- 1Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, China
- 2Mental Health Institute, Second Xiangya Hospital, Central South University, Changsha, China
Background: As one of the most widely researched consequence of traumatic events, the prevalence of post-traumatic stress symptoms (PTSS) among people exposed to the trauma resulting from infectious disease outbreak varies greatly across studies. This review aimed at examining the pooled prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak, summarizing the possible causes of the inconsistencies in the current estimates.
Methods: Systematic searches of databases were conducted for literature published on PubMed, EMBASE, Web of Science, the Cochrane Library, PsycArticles, and Chinese National Knowledge Infrastructure (CNKI) until 14 October 2020. Statistical analyses were performed using R software (registration number: CRD42020182366).
Results: About 106 studies were included. The results showed that the pooled prevalence of PTSS among the general population exposed to the trauma resulting from infectious disease outbreak was 24.20% (95% CI: 18.54–30.53%), the pooled prevalence of PTSS among healthcare workers was 24.35% (95% CI: 18.38–1.51%), the pooled prevalence of PTSS among patients with infectious disease was 28.83% (95% CI: 18.53–44.86%), and the pooled prevalence of PTSS among suspected cases of infectious disease was 25.04% (95% CI: 18.05–34.73%). Mortality rate was a significant contributor to heterogeneity.
Conclusions: Evidence suggests that PTSS were very common among people exposed to the trauma resulting from infectious disease outbreak. Health policymakers should consider both short-term and long-term preventive strategy of PTSS.
Background
Infectious disease poses a serious threat to public health. Over the past two decades, novel viruses continuing to emerge, the number of reported outbreaks of highly pathogenic or highly transmitted infectious diseases has increased, such as severe acute respiratory syndrome (SARS) in 2003, 2009 influenza A (H1N1) in 2009, and Ebola virus disease (Ebola) in 2014
(Houlihan and Whitworth, 2019). At the end of 2019, a new type of infectious disease emerged, which is known as coronavirus disease 2019 (COVID-19). As of December 10, 2020, over 66.2 million cases of COVID-19 and about 1.5 million deaths have been reported to the WHO (WHO, 2020). The outbreak of infectious disease can spread rapidly, causing enormous losses to individual health, national economy, and social well-being (Steele et al., 2016).
The psychological effects of infectious disease outbreak can be deleterious and far-reaching. Previous research indicates high prevalence rates of clinically relevant post-traumatic stress symptoms (PTSS) among people exposed to the trauma resulting from infectious disease outbreak (such as the outbreak of SARS; Gardner and Moallef, 2015). Patients with post-traumatic stress disorder (PTSD)-related symptoms live under the shadow of past trauma. According to the Diagnostic and Statistics of Mental Disorders, the fifth edition (DSM-5), the clinical features of PTSD include persistent intrusion symptoms, persistent avoidance of stimuli, negative alterations in cognition or mood, and marked alterations in arousal and reactivity, all of which are related to traumatic events (Association, 2013). PTSS could cause clinically significant distress or impairment in social, occupational, or other important areas of functioning (Greene et al., 2016). When an infectious disease breaks out, people may experience many types of psychological trauma, such as directly suffering from the symptoms and traumatic treatment, witness of suffering, and struggling and dying of patients (Fiorillo and Gorwood, 2020). Additionally, individuals may experience the fear of realistic or unrealistic of infection, social isolation, exclusion, and stigmatization, as patients, care and help providers, or even the general public (Kisely et al., 2020; Morganstein and Ursano, 2020). As one of the most widely researched consequence of traumatic events, the prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak varies greatly across studies (Lancee et al., 2008; Jung et al., 2020). In order to provide more reliable prevention, it is necessary to determine a more accurate estimation of the prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak and to explore the possible causes of the inconsistencies in the current estimates.
Currently, control of the epidemic of COVID-19 is still the dominant task of the whole world, millions of people are scared and even panic of the possible loss of health, life, and wealth (Dutheil et al., 2020). A few epidemic studies reported that experience and witness of the suffering related to COVID-19 resulted in a high prevalence of PTSD-related symptoms (Kisely et al., 2020; Rogers et al., 2020). Although it is too early to predict how many people worldwide will be infected with the virus, it is believed that the numbers of case and death will continue to increase in the following months. Some psychologists draw attention toward PTSD as the second tsunami of the COVID-19 pandemic (Dutheil et al., 2020). For taking effective measures to reduce the psychological sequelae caused by COVID-19 across the world, understanding how infectious disease outbreak cause PTSD and who might be vulnerable are essential. This review aimed at examining the pooled prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak (including infectious diseases over the past 20 years and COVID-19), summarizing the possible causes of the inconsistencies in the current estimates, and examining potentially vulnerable populations, try to provide a reference for COVID-19 and possible outbreak of infectious diseases in the future.
Materials and Methods
This review was reported in accordance with the PRISMA guideline and the Meta-analyses Of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al., 2000; Moher et al., 2009). The protocol of this review is registered in the International Prospective Register of Systematic Reviews (registration number: CRD42020182366). See Supplementary Material for the details.
Search Strategy
PubMed, EMBASE, Web of Science, the Cochrane Library, PsycArticle, and Chinese National Knowledge Infrastructure (CNKI) were independently searched by two reviewers (DQ and YLL), with no restrictions on date or language of publication up until 25 April 2020, and an update search was conducted on 14 October 2020. The following search terms were used: “Infectious disease” (including “infection,” “infectious,” “infectious disease,” “public health emergency,” “public health event,” “SARS,” “Severe Acute Respiratory Syndrome,” “H1N1,” “flu,” “influenza,” “Ebola,” “MERS,” “Middle East Respiratory Syndrome Coronavirus,” “coronavirus,” and “COVID-19”); “Post-traumatic stress disorder” (including “Posttraumatic stress disorder,” “posttraumatic syndrome,” “PTSD,” “stress disorder,” “post-traumatic,” and “post traumatic syndrome”). See Supplementary Table 1 for a full search strategy.
Study Selection
Studies were included if they meet the following criteria: (1) the study was observational study; (2) information about the prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak; (3) the full article was written in English or Chinese; and (4) these outbreaks were SARS, H1N1, H7N9, MERS, Ebola virus disease, Zika virus disease, and COVID-19. Studies were excluded if: (1) the report was a review, comments, meta-analysis, or protocol; (2) the participants with comorbid symptoms or chronic disease (such as mental illness, cancer, etc.); and (3) the report was duplicate results.
Data Extraction
Two reviewers (DQ and YLL) checked the titles, abstracts, and full texts of the initial search results independently. Data were extracted on first author, year of publication, country or area, type of disease, population, survey period, sample size, response rate, percentage of male participants, average age of participants, instruments used to identify PTSS, prevalence of PTSS, and quality score of the included studies. Any discrepancies that emerged in these procedures were discussed and resolved by involving a third reviewer (SYX).
Quality Assessment
Two independent reviewers (JH and FYOY) used the established guidelines, the Loney criteria, to evaluate the methodological quality of the included studies, which has been widely used to evaluate observational studies (Loney et al., 1998; Sanderson et al., 2007). The included papers were scored according to eight criteria, such as definition of participants, study design, sampling method, response rate, sample size, and appropriateness of measurement and analysis. The scores range from 0 to 8, with a score of 0–3 as low quality, 4–6 as moderate, and 7–8 as high (Qiu et al., 2020). See Supplementary Table 3 for details on the quality assessment.
Statistical Analyses
When data were available for three or more studies, the prevalence was combined. When there were 10 or more studies, the quantitative subgroup analysis was conducted. All the statistical analyses were performed using the “meta” (4.12-0) and “metafor” package (2.4-0) of R version 4.0.0. Between-study heterogeneity was evaluated by Cochran's Q-test and quantified by the I2 statistic, with values 50% or more indicating possible heterogeneity (Higgins et al., 2003; Ades et al., 2005). The pooled prevalence of PTSS was combined using the Logit transformation method or Log transformation method by a random effects model if significant heterogeneity was observed across studies (when p < 0.05, I2 > 50%). If more than one dataset was reported for the same group of participants, the outcomes that were assessed at the baseline were used. In order to compare the prevalence from different studies, the subgroup meta-analysis was conducted. Because the subgroup analyses should be interpreted with caution (Jike et al., 2018), we planned a priori to limit our subgroup analyses to a small number of baseline characteristics including area, sample size, type of disease, mortality rate of disease, survey time after the outbreak, gender, age, assessment tool, and quality score. The difference between subgroups was examined using the Cochran's Q chi-square tests. Mixed-model meta-regression analyses were performed by using the Freeman–Tukey double arcsine method to explore potential moderators on the heterogeneity. Publication bias was investigated by Egger's test. To evaluate the consistency of the results, sensitivity analysis was performed by removing each study individually. All the statistical tests were two-sided, with a significance threshold of p < 0.05.
Results
Literature Search
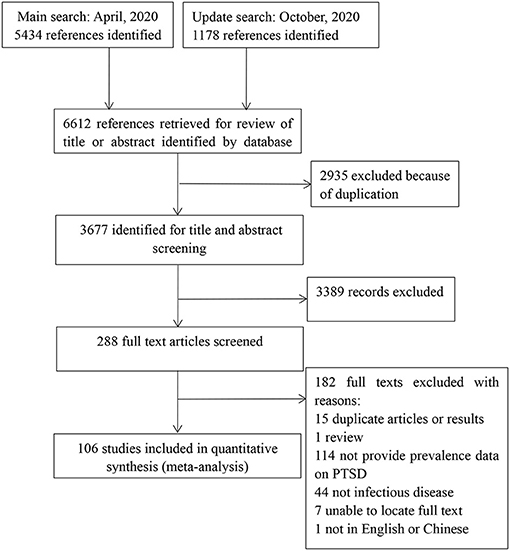
As shown in Figure 1, a total of 6,612 references were identified. Among them, 2,953 duplicates were removed. By screening titles and abstracts, 3,019 irrelevant articles were excluded. A total of 288 potentially relevant full-text articles were independently assessed based on the selection criteria. Further, 182 studies were excluded because of the following reasons: duplicate articles or results (n = 15), review (n = 1), did not provide data on PTSS (n = 114), not infectious disease (n = 44), unable to locate full text (n = 7), and not in English or Chinese (n = 1). Finally, 106 eligible studies were included in this review. See Figure 1 for the details.
Study Characteristics
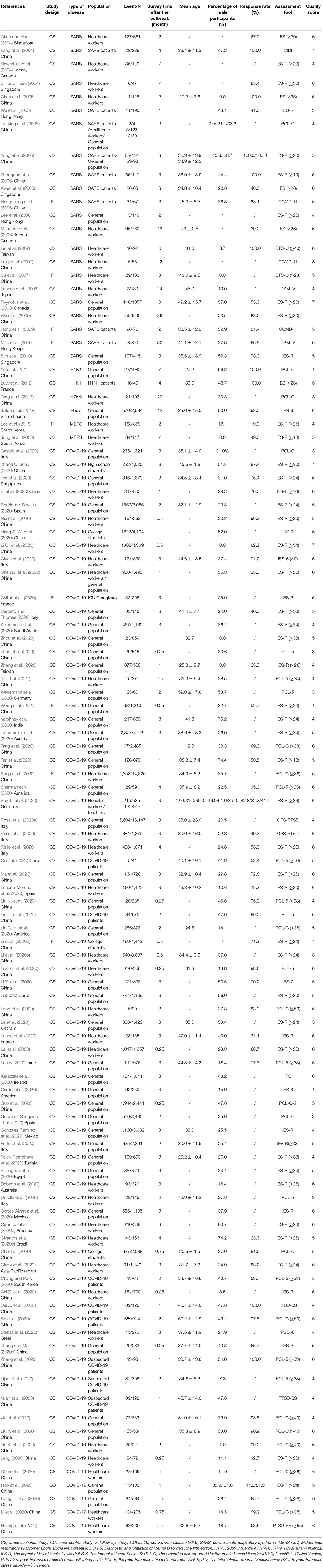
One hundred and six papers met the inclusion criteria. Of the included studies, 78 were of COVID-19 (Alkhamees et al., 2020; Barbato and Thomas, 2020; Blekas et al., 2020; Bo et al., 2020; Caillet et al., 2020; Cai X. et al., 2020; Cai Z. et al., 2020; Cardel et al., 2020; Castelli et al., 2020; Chang and Park, 2020; Chen B. et al., 2020; Chen et al., 2020; Chew et al., 2020; Chi et al., 2020; Civantos et al., 2020a,b; Cortes-Alvarez et al., 2020; Di Tella et al., 2020; Dobson et al., 2020; El-Zoghby et al., 2020; Fekih-Romdhane et al., 2020; Forte et al., 2020; Giusti et al., 2020; Gonzalez Ramirez et al., 2020; Gonzalez-Sanguino et al., 2020; Guo et al., 2020; Hao et al., 2020; Huang et al., 2020; Karatzias et al., 2020; Lahav, 2020; Lai et al., 2020; Lange et al., 2020; Le et al., 2020; Leng, 2020; Leng et al., 2020; Li, 2020; Liang L. et al., 2020; Liang S. W. et al., 2020; Li et al., 2020,a,b; Li G. et al., 2020; Lijun et al., 2020; Liu C. H. et al., 2020; Liu D. et al., 2020; Liu N. et al., 2020; Liu Y. et al., 2020; Li X. C. et al., 2020; Li X. et al., 2020; Luceno-Moreno et al., 2020; Ma et al., 2020; Nie et al., 2020; Qi et al., 2020; Riello et al., 2020; Rodriguez-Rey et al., 2020; Rossi et al., 2020a,b; Seyahi et al., 2020; Sherman et al., 2020; Si et al., 2020; Song et al., 2020; Tan et al., 2020; Tang et al., 2020; Tee et al., 2020; Traunmuller et al., 2020; Varshney et al., 2020; Wang et al., 2020; Wesemann et al., 2020; Xie et al., 2020; Yin et al., 2020; Yuan et al., 2020; Zhang and Ma, 2020a,b; Zhang C. et al., 2020; Zhang et al., 2020; Zhao et al., 2020; Zhou et al., 2020) (Alkhamees et al., 2020; Barbato and Thomas, 2020; Blekas et al., 2020; Bo et al., 2020; Caillet et al., 2020; Cai X. et al., 2020; Cai Z. et al., 2020; Cardel et al., 2020; Castelli et al., 2020; Chang and Park, 2020; Chen B. et al., 2020; Chen et al., 2020; Chew et al., 2020; Chi et al., 2020; Civantos et al., 2020a,b; Cortes-Alvarez et al., 2020; Di Tella et al., 2020; Dobson et al., 2020; El-Zoghby et al., 2020; Fekih-Romdhane et al., 2020; Forte et al., 2020; Giusti et al., 2020; Gonzalez Ramirez et al., 2020; Gonzalez-Sanguino et al., 2020; Guo et al., 2020; Karatzias et al., 2020; Lahav, 2020; Lange et al., 2020; Le et al., 2020; Leng, 2020; Leng et al., 2020; Li, 2020; Liang S. W. et al., 2020; Li et al., 2020a,b; Li G. et al., 2020; Lijun et al., 2020; Liu C. H. et al., 2020; Liu D. et al., 2020; Liu Y. et al., 2020; Li X. C. et al., 2020; Li X. et al., 2020; Luceno-Moreno et al., 2020; Ma et al., 2020; Nie et al., 2020; Qi et al., 2020; Riello et al., 2020; Rodriguez-Rey et al., 2020; Rossi et al., 2020a,b; Seyahi et al., 2020; Sherman et al., 2020; Si et al., 2020; Song et al., 2020; Tan et al., 2020; Tee et al., 2020; Traunmuller et al., 2020; Varshney et al., 2020; Wesemann et al., 2020; Xie et al., 2020; Yuan et al., 2020; Zhang and Ma, 2020a,b; Zhang C. et al., 2020; Zhang et al., 2020; Zhao et al., 2020; Zhou et al., 2020), two of Middle East Respiratory Syndrome (MERS) (Lee et al., 2018; Jung et al., 2020), one of Ebola virus disease (Jalloh et al., 2018), one of H7N9 (Tang et al., 2017), two of H1N1 (Xu et al., 2011; Luyt et al., 2012), and the remaining 22 of SARS (Chan and Huak, 2004; Fang et al., 2004; Hawryluck et al., 2004; Sin and Huak, 2004; Chen et al., 2005; Tie-ying et al., 2005; Wu et al., 2005, 2009; Yong et al., 2005; Hongsheng et al., 2006; Kwek et al., 2006; Lee et al., 2006; Maunder et al., 2006; Zhongguo et al., 2006; Laiqi et al., 2007; Lin et al., 2007; Su et al., 2007; Lancee et al., 2008; Reynolds et al., 2008; Hong et al., 2009; Mak et al., 2010; Sim et al., 2010). Six papers were in Chinese, and the remainder in English. Of these, 93 were cross-sectional studies, nine were longitudinal designs, and four were case control studies. Most of the included studies were from Asia, such as China, Singapore, and South Korea. See Table 1 for the details. From the 106 papers, five (4.72%) studies were rated as high quality, 93 (87.73%) were rated as moderate, and eight (7.55%) were rated as low quality. Details of the methodological quality assessments of all 106 studies are showed in Supplementary Table 3.
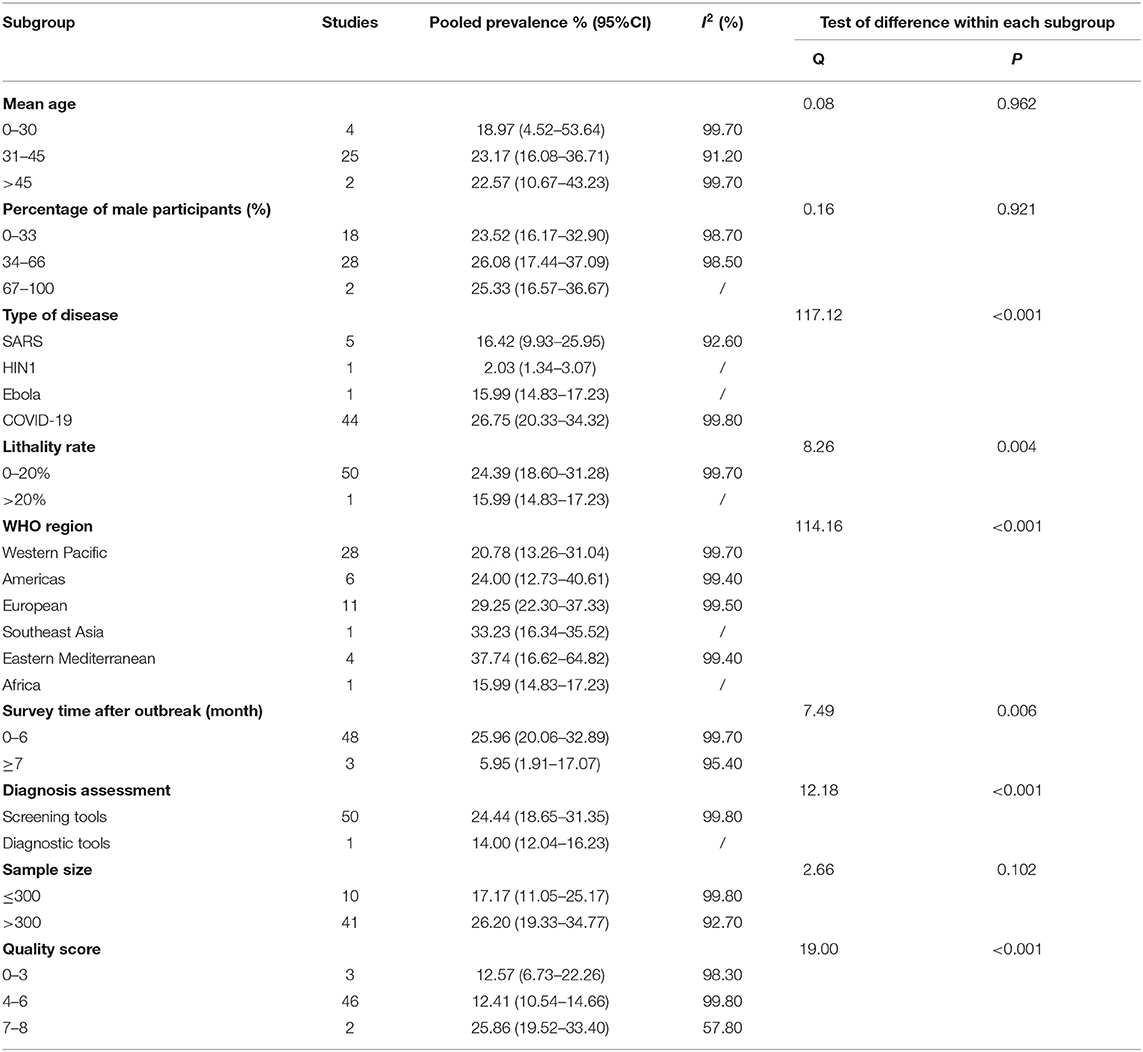
Pooled Prevalence of Post-traumatic Stress Symptoms Among the General Population
There were 51 studies reported the prevalence of PTSS among the general population. The forest plot in Figure 2 depicts the details. A total of 78,459 people exposed to the trauma resulting from an epidemic of infectious disease were identified in the 51 articles, of which 25,826 were reported with PTSS. The random effects model was used to determine the pooled prevalence (I2 = 99.70%, p < 0.001), the pooled prevalence of PTSS among people exposed to the trauma resulting from infectious disease outbreak was 24.20%, with a 95% CI of 18.54–30.53%.
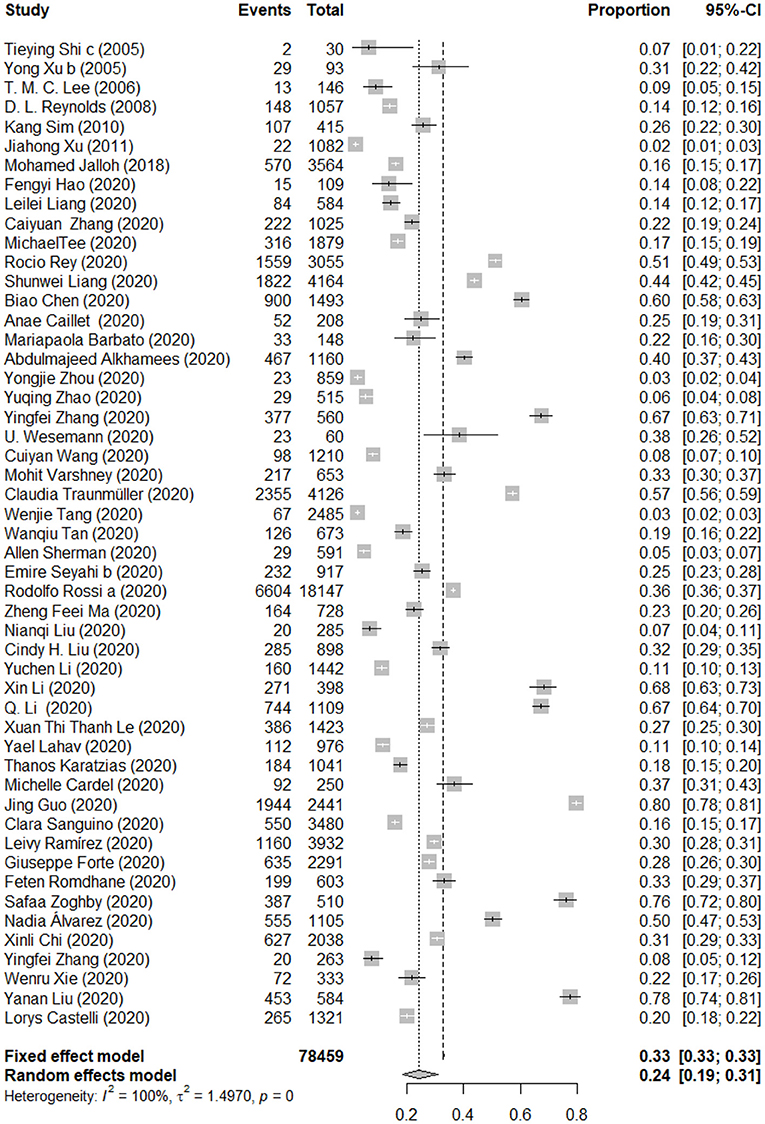
Figure 2. Forest plots of pooled prevalence of post-traumatic stress symptoms among the general population.
The details of subgroup analyses are presented in Table 2. There were no significant differences in the prevalence of PTSS between age and gender (Q = 0.08 and 0.16, p > 0.05). Significant difference in the prevalence of PTSS between different types of disease was observed, the pooled prevalence of PTSS among people influenced by COVID-19 was higher than that for people influenced by SARS, Ebola and H1N1 (26.75 vs. 16.42 vs. 15.99 vs. 2.03%; Q = 117.12, p < 0.05). In addition, a higher mortality rate is associated with a lower prevalence of PTSS (24.39 vs. 15.99%; Q = 8.26, p < 0.05). The pooled prevalence of PTSS among people in the Eastern Mediterranean region was higher than people in the Western Pacific region, the Southeast Asia region, the America region, the European region, and the Africa region (37.74 vs. 33.23 vs. 29.25 vs. 24.00 vs. 20.78 vs. 15.99%; Q = 114.16, p < 0.05). Furthermore, there were significant differences in the prevalence of PTSS between different survey time after the outbreak; closer survey time to the point of infectious disease outbreak was associated with a higher prevalence of PTSS (25.96 vs. 5.95%; Q = 7.49, p < 0.05). There were significant differences in the prevalence of PTSS between studies used different assessment tools (24.44 vs. 14.00%; Q = 12.18, p < 0.05). In addition, significant difference in the prevalence of PTSS between studies with different quality scores was observed, articles with the highest quality scores showed a high prevalence (12.57 vs. 12.41 vs. 25.86%; Q = 19.00, p < 0.05). A multivariate meta-regression was carried out to explore the origin of heterogeneity accounted for by the variables, such as type of disease and survey time after the outbreak. However, no significant contributor was found. See Table 5 for the details.
The results of the Egger's test showed that publication bias was not found in this study (t = −2.425, p = 0.208). When each study was excluded one by one, the recalculated combined results did not change significantly. The pooled prevalence of PTSS ranged from 23.29% (95% CI: 17.91–29.70%) to 25.13% (95% CI: 19.43–31.85%), and the I2 statistic varied from 99.70% to 99.80%. The results indicate that no individual study significantly influenced the overall results.
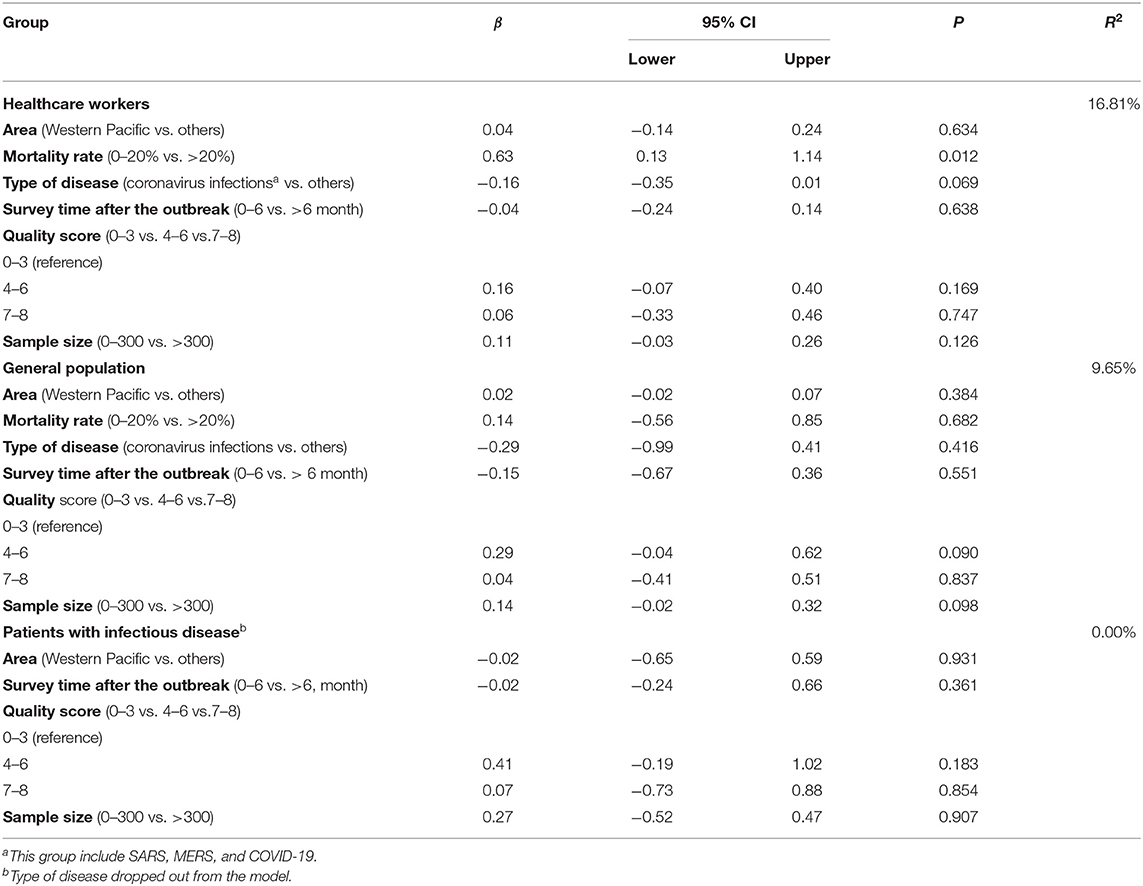
Pooled Prevalence of Post-traumatic Stress Symptoms Among the Healthcare Workers
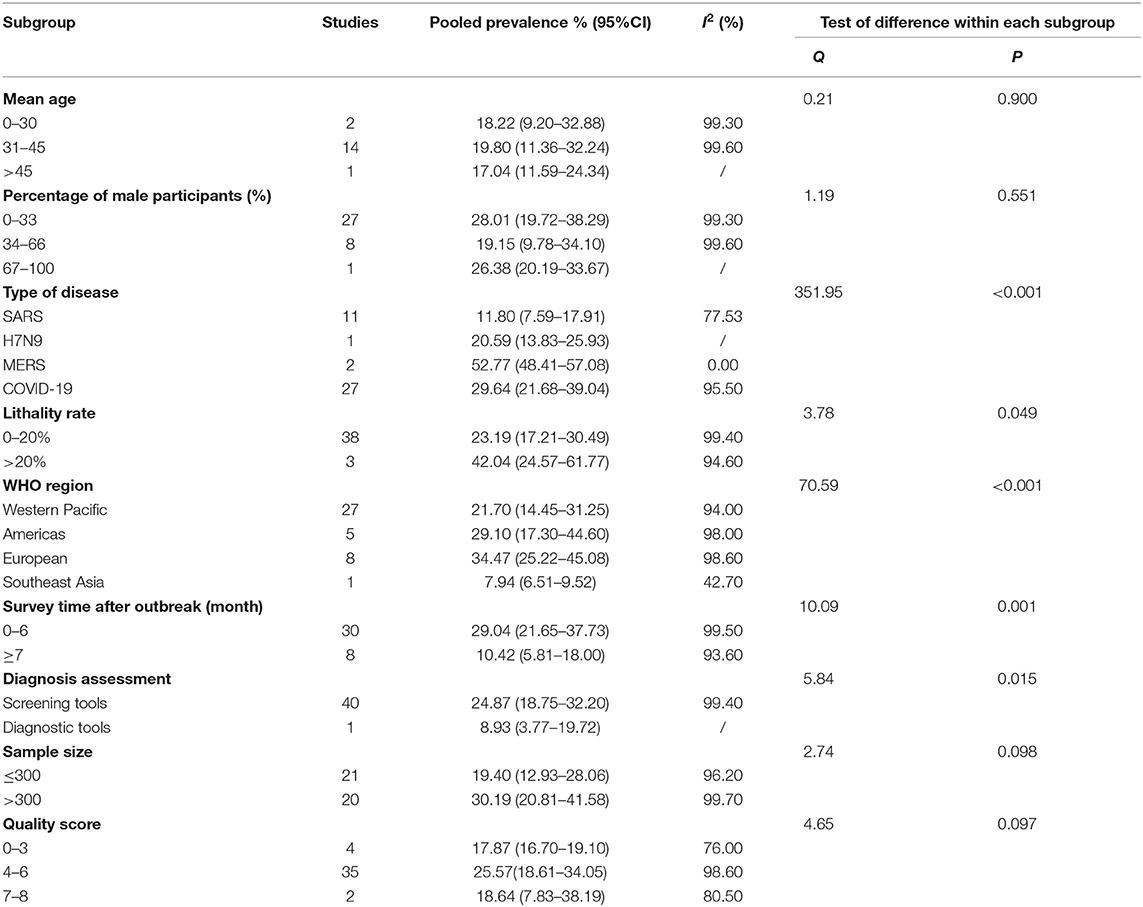
A total of 41 studies reported the prevalence of PTSS among the healthcare workers. The forest plot in Figure 3 depicts the details. A total of 38,250 healthcare workers exposed to the trauma resulting from an epidemic of infectious disease were identified in the 41 articles, of which 9,071 were reported with PTSS. The random effects model was used to determine the pooled prevalence (I2 = 99.40%, p < 0.001), the pooled prevalence of PTSS among healthcare workers exposed to the trauma resulting from infectious disease outbreak was 24.35%, with a 95% CI of 18.38–31.51%.
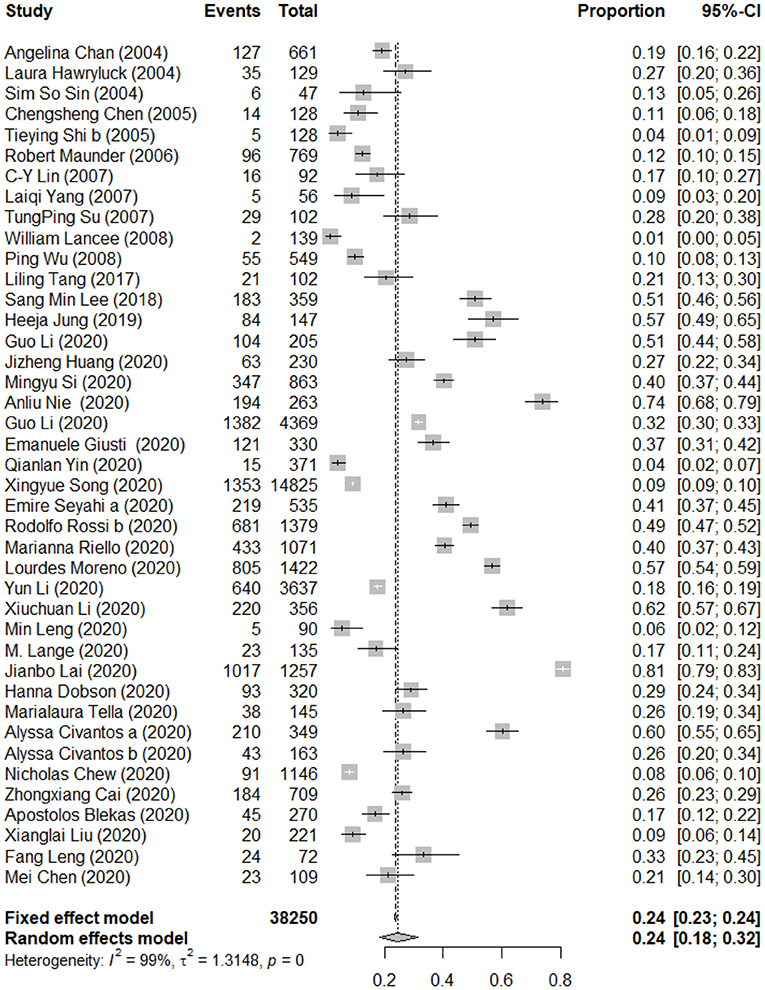
Figure 3. Forest plots of pooled prevalence of post-traumatic stress symptoms among healthcare workers.
The details of subgroup analyses are presented in Table 3. There were no significant differences in the prevalence of PTSS between age, gender, mortality rate of disease, sample size, and quality score (Q = 0.21, 0.19, 3.78, 2.54, and 4.65, p > 0.05). Significant difference in the prevalence of PTSS between different types of disease was observed, and the pooled prevalence of PTSS among people influenced by MERS was higher than that for the people influenced by COVID-19, H7N9, and SARS (52.77 vs. 29.64 vs. 20.59 vs. 11.80%; Q = 351.95, p < 0.05). In addition, a higher mortality rate is associated with a higher prevalence of PTSS (23.19 vs. 42.04%; Q = 3.78, p < 0.05). The pooled prevalence of PTSS among people in the European region was higher than people in the America region, the Western Pacific region, and the Southeast Asia region (34.47 vs. 29.10 vs. 21.70 vs. 7.94%; Q = 70.59, p < 0.05). Furthermore, there were significant differences in the prevalence of PTSS between different survey time after the outbreak, and closer survey time to the point of infectious disease outbreak is associated with a higher prevalence of PTSS (29.04 vs. 10.42%; Q = 10.09, p < 0.05). There were significant differences in the prevalence of PTSS between studies used different assessment tools (24.87 vs. 8.93%; Q = 5.84, p < 0.05). A multivariate meta-regression was carried out to explore the origin of heterogeneity accounted for by the variables including type of disease, mortality rate, survey time after the outbreak, age, gender, quality score, and sample size. The results of meta-regression showed that mortality rate of disease was a significant contributor to heterogeneity (accounted for 16.81% of the heterogeneity). See Table 5 for the details.
The results of the Egger's test showed that publication bias was not found in this study (t = 0.728, p = 0.470). When each study was excluded one by one, the recalculated combined results did not change significantly. The pooled prevalence of PTSS ranged from 23.22% (95% CI: 17.69–29.84%) to 25.62% (95% CI: 19.68–32.62%), and the I2 statistic varied from 99.20 to 99.40%. The results indicate that no individual study significantly influenced the overall results.
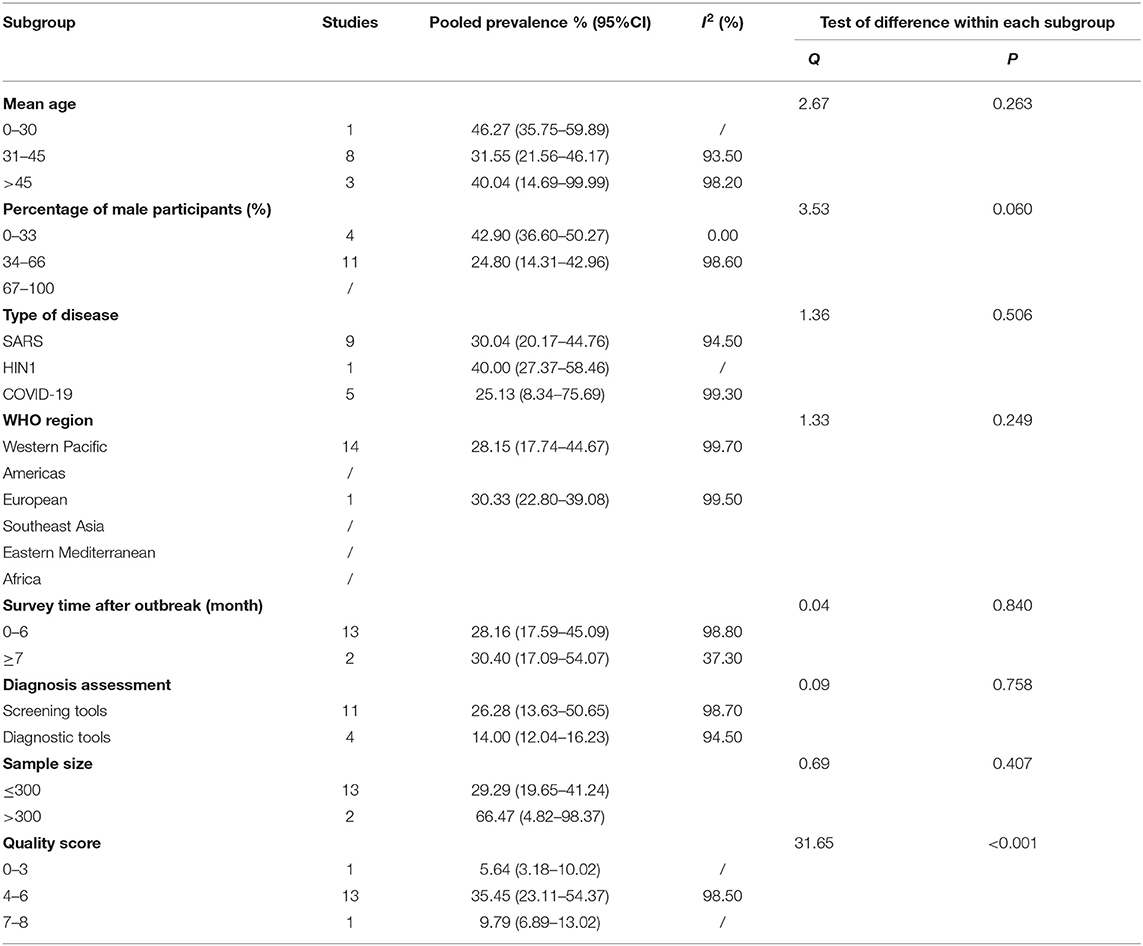
Pooled Prevalence of Post-traumatic Stress Symptoms Among Patients With Infectious Disease
A total of 15 studies reported the prevalence of PTSS among the patients. The forest plot in Figure 4 depicts the details. A total of 2,666 patients with infectious disease were identified in the 15 articles, of which 1,125 were reported with PTSS. The random effects model was used to determine the pooled prevalence (I2 = 98.60%, p < 0.001), and the pooled prevalence of PTSS among patients with infectious disease was 28.83%, with a 95% CI of 18.53–44.86%.
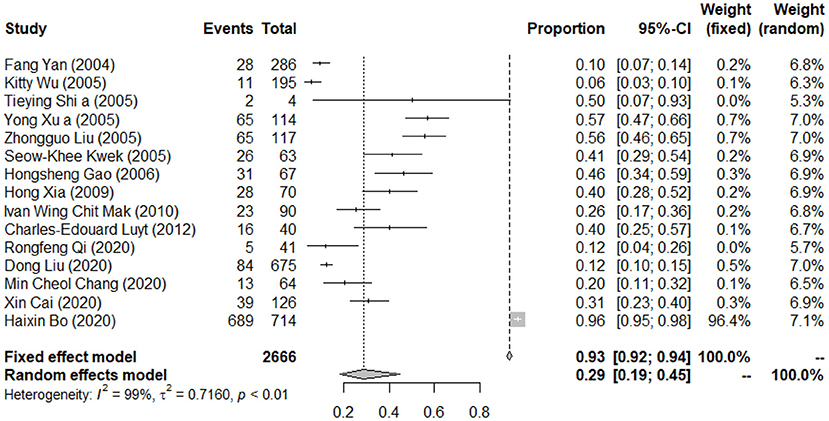
Figure 4. Forest plots of pooled prevalence of post-traumatic stress symptoms among patients with infectious disease.
The details of subgroup analyses are presented in Table 4. There were no significant differences in the prevalence of PTSS between age, gender, type of disease, region, survey time after outbreak, diagnosis tool, sample size, and quality score (p > 0.05). A significant difference in the prevalence of PTSS between studies with different quality scores was observed (5.64 vs. 35.45 vs. 9.79%; Q = 31.65, p < 0.05). A multivariate meta-regression was carried out to explore the origin of heterogeneity accounted for by the variables, such as type of disease and survey time after the outbreak. However, no significant contributor was found. See Table 5 for the details.
The results of the Egger's test showed that publication bias was not found in this study (t = −6.138, p = 3.553). When each study was excluded one by one, the recalculated combined results did not change significantly. The pooled prevalence of PTSS ranged from 23.22% (95% CI: 17.69–29.84%) to 32.23% (95% CI: 20.75–50.05%), and the I2 statistic varied from 95.40 to 98.7%. The results indicate that no individual study significantly influenced the overall results.
Pooled Prevalence of Post-traumatic Stress Symptoms Among the Suspected Cases of Infectious Disease
A total of three studies reported the prevalence of PTSS among the suspected cases. The forest plot in Figure 5 depicts the details. A total of 525 suspected cases of infectious disease exposed to the trauma resulting from an epidemic of infectious disease were identified in the three articles, of which 139 were reported with PTSS. The random effects model was used to determine the pooled prevalence (I2 = 74.50%, p < 0.001), the pooled prevalence of PTSS among suspected cases exposed to the trauma resulting from infectious disease outbreak was 25.04%, with a 95% CI of 18.05–34.73%.
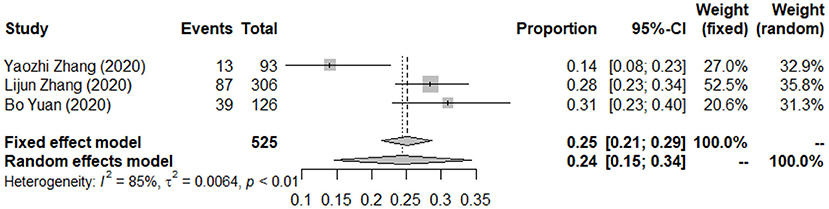
Figure 5. Forest plots of pooled prevalence of post-traumatic stress symptoms among suspected cases.
Discussion
Key Findings
This review has highlighted the importance of considering the psychological impacts of people exposed to the trauma resulting from infectious disease outbreak. The results showed that the pooled prevalence of PTSS among the general population was 24.20% (95% CI: 18.54–30.53%), the pooled prevalence of PTSS among the healthcare workers was 24.35% (95% CI: 18.38–31.51%), the pooled prevalence of PTSS among patients with infectious disease was 28.83% (95% CI: 18.53–44.86%), and the pooled prevalence of PTSS among the suspected cases of infectious disease was 25.04% (95% CI: 18.05–34.73%), and several factors including type of disease, mortality rate of disease, region, survey time after outbreak, assessment tool, sample size, and quality score were associated with PTSS. Mortality rate of disease was a significant moderator for heterogeneity. Further research is needed to identify effective strategies for preventing and treating PTSS among people exposed to the trauma resulting from infectious disease outbreak.
Comparison With the Literature
The pooled prevalence of PTSS among different population exposed to the trauma resulting from infectious disease outbreak in this study ranged from 24.20 to 28.83%, which was higher than flood survivors (15.74%) and hurricane survivors (Liu et al., 2017; Wang et al., 2019), but similar to earthquake survivors (Dai et al., 2016) and civilian war survivors (23.66–26.00%) (Morina et al., 2018). Compared with infectious diseases, some natural disasters, such as flood and hurricane, can be predicted, whereas earthquakes and infectious disease were often happened suddenly and without a warning and pose a huge threat to health and property of people in a short period of time (Dai et al., 2016). Therefore, earthquakes might have caused more damage to mental health of people. Relative to natural disasters, wars often last longer, and survivors directly exposed to trauma continuously (Morina et al., 2018). Furthermore, the pooled prevalence of PTSS among patients with infectious disease was much higher than healthcare workers, the general population, and suspected cases of infectious diseases, which were consistent with previous studies (Neria et al., 2008). The possible reason is that patients with infectious disease experience higher level of severity of disaster exposure. Patients often directly suffer from the symptoms and traumatic treatment (such as dyspnea, respiratory failure, alteration of conscious states, and tracheotomy), and after being cured, they were more vulnerable to social discrimination than other groups (Neria et al., 2008).
The pooled prevalence of PTSS in different types of diseases was different, and different mortality rates of those infectious diseases also affect the prevalence of PTSS. Among the healthcare workers, mortality rate of infectious diseases was a significant moderator for heterogeneity, higher mortality rate was associated with a higher prevalence of PTSS. Previous studies have shown that when the mortality rate of infectious diseases is high, the impact on mental health of people may be greater (Spoorthy et al., 2020). Therefore, we think the mortality rate of these infectious diseases should be considered when formulating psychological interventions for people influenced by infectious diseases. In addition, the pooled prevalence of PTSS is relatively high in Europe and the Americas, but relatively low in Asia and Africa. The possible reason is that the epidemic situation is more serious in the first two places (WHO, 2020). In addition, the pooled prevalence of PTSS assessed in different time points was different. PTSS among the general population and the healthcare workers were higher in the immediate aftermath of the infectious disease outbreak (0–6 months), which was in line with other studies (Heron-Delaney et al., 2013; Dai et al., 2016; Righy et al., 2019; Benfante et al., 2020). However, in patients with infectious disease, no significant difference was found, and the prevalence of PTSS among patients was still high even after 6 months. This difference in the prevalence estimates among different population may be explained by the fact that patients are exposed to greater trauma than other population, they need more time to recover (Xiao et al., 2020). Furthermore, we found that the pooled prevalence of PTSS among healthcare workers and the general population identified by screening tools was significantly higher than that identified by diagnostic tools, which was consistent with previous researches (Edmondson et al., 2013). It is reported that studies with poor methodological quality or small sample size generally yielded more extreme prevalence estimates (Mata et al., 2015), the current study showed similar results. However, after controlling for other factors, the results of meta-regression showed that the influence of methodological quality and sample size on the prevalence of PTSS is no longer significant. Hence, the results for quality score and sample size in the subgroup analyses require further clarification.
Implications for the Future
Epidemiological studies have demonstrated a rather high prevalence of mental health problems among different population after an epidemic of infectious disease (Catalan et al., 2011; Tucci et al., 2017). While most of these mental health problems will fade out after the epidemic, symptoms of PTSD may last for a prolonged time and result in severe distress and disability (Vyas et al., 2016). In terms of applicability to COVID-19, evidence suggests that the symptoms of PTSD were very common and persist in patients with infectious disease even higher after 6 months (Hong et al., 2009). Thus, healthcare policies need to take into account both short-term and long-term preventive strategies of PTSD. The information available suggests that the prevalence of PTSS is higher among patients with infectious disease, lower among suspected cases, related workers, and yet even lower in the general population. These three types of samples studied are likely to represent different levels of severity of disaster exposure, with different levels of the PTSS prevalence (Neria et al., 2008). However, there is little doubt that there is a dose–response relationship between the degree of trauma and the mental health burden of disasters (Neria et al., 2008). This relation may not necessarily mean that the principal mental health burden of people exposed to the trauma resulting from infectious disease outbreak is among those who were most directly affected by the disease (Galea and Resnick, 2005). It will be important to establish whether indirect exposure to a trauma during a COVID-19 pandemic was correlated with higher risk of PTSS. In addition, it is necessary to assess the relation between exposure to multiple traumas and risk of PTSS in the future. Additionally, the mortality rate of these infectious diseases should be considered when formulating psychological interventions for people influenced by infectious diseases. Lastly, we think a large multicenter prospective study using a single validated measure of PTSS and measuring possible confounding factors in randomly selected participants is needed in the future, which would provide a more accurate estimate of PTSS among people influenced by infectious diseases.
Limitations
First, although subgroup analyses and meta-regression analyses were conducted to control many moderating factors for the pooled prevalence of PTSS, heterogeneity was still retained in this review. It is reported that heterogeneity is difficult to avoid in meta-analysis of epidemiological surveys (Winsper et al., 2013), suggesting the need for caution when drawing inferences about estimates of PTSS in post-disaster research. In addition, the follow-up time varies greatly among the included longitudinal studies, which hinder comparability. Additionally, although our study included relevant studies across 30 countries, more than half of the eligible studies were from upper-high income countries. Prevalence studies were scarce for many countries, especially for low-income countries. Considering the inconsistency of the healthcare environment and socioeconomic status across the world, more prevalence studies in low-income countries are needed to understand the panorama of PTSS among people influenced by infectious diseases. Lastly, we noticed that most of the included studies were used screening tools to assess PTSS, only 5.71% of studies used diagnostic tools. It is possible that the pooled prevalence of PTSS caused by infectious diseases was overestimated in this review. Thus, we think ongoing surveillance is essential.
Conclusion
Evidence suggests that PTSS were very common among people exposed to the trauma resulting from infectious disease outbreak, and the pooled prevalence among different population ranged from 24.20 to 28.83%. Several factors, including type of disease, mortality rate of disease, region, survey time after outbreak, assessment tool, sample size, and quality score, were associated with PTSS. Mortality rate of disease was a significant moderator for heterogeneity. Further research is needed to identify effective strategies for preventing and treating PTSS among people exposed to the trauma resulting from infectious diseases outbreak.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
DQ, SX, and YL contributed to the design of the study. DQ and YL screened the text. DQ and LL extracted and analyzed the data. JH and FO conducted the quality assessment. DQ wrote the first draft of the manuscript with input from SX. All authors approved the final manuscript.
Funding
This research was supported by the Ministry of Science and Technology of China (Grant No.: 2016YFC0900802). The funding agency did not take part in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.668784/full#supplementary-material
Abbreviations
COVID-19, coronavirus disease 2019; SARS, severe acute respiratory syndrome; MERS-CoV, Middle East respiratory syndrome; Ebola, Ebola virus disease; PTSD, post-traumatic stress disorder; DSM-5, Diagnostic and Statistics of Mental Disorders the fifth edition; H1N1, 2009 influenza A(H1N1); H7N9, H7N9 avian influenza.
References
Ades, A. E., Lu, G., and Higgins, J. P. (2005). The interpretation of random-effects meta-analysis in decision models. Med. Decis. Making 25, 646–654. doi: 10.1177/0272989X05282643
Alkhamees, A. A., Alrashed, S. A., Alzunaydi, A. A., Almohimeed, A. S., and Aljohani, M. S. (2020). The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Compr. Psychiatry. 102:152192. doi: 10.1016/j.comppsych.2020.152192
Association, A. P. (2013). Diagnostic and Statistical Manual of Mental Disorder, 5th Edn. Washington, DC: American Psychiatric Publishing.
Barbato, M., and Thomas, J. (2020). Far from the eyes, close to the heart: psychological impact of COVID-19 in a sample of Italian foreign workers. Psychiatry Res. 290:113113. doi: 10.1016/j.psychres.2020.113113
Benfante, A., Di Tella, M., Romeo, A., and Castelli, L. (2020). Traumatic stress in healthcare workers during COVID-19 pandemic: a review of the immediate impact. Front. Psychol. 11:569935. doi: 10.3389/fpsyg.2020.569935
Blekas, A., Voitsidis, P., Athanasiadou, M., Parlapani, E., Chatzigeorgiou, A. F., Skoupra, M., et al. (2020). COVID-19: PTSD symptoms in Greek health care professionals. Psychol. Trauma. 12, 812–819. doi: 10.1037/tra0000914
Bo, H. X., Li, W., Yang, Y., Wang, Y., Zhang, Q., Cheung, T., et al. (2020). Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020, 1–2. doi: 10.1017/S0033291720000999
Cai, X., Hu, X. P., Ekumi, I. O., Wang, J. C., An, Y. W., Li, Z. W., et al. (2020). Psychological distress and its correlates among COVID-19 survivors during early convalescence across age groups. Am. J. Geriat. Psychiat. 28, 1030–1039. doi: 10.1016/j.jagp.2020.07.003
Cai, Z., Cui, Q., Liu, Z., Li, J., Gong, X., Liu, J., et al. (2020). Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. J. Psychiatr. Res. 131, 132–137. doi: 10.1016/j.jpsychires.2020.09.007
Caillet, A., Coste, C., Sanchez, R., and Allaouchiche, B. (2020). Psychological Impact of COVID-19 on ICU Caregivers. Anaesth. Crit. Care Pain Med. 2020:6. doi: 10.1016/j.accpm.2020.08.006
Cardel, M. I., Manasse, S., Krukowski, R. A., Ross, K., Shakour, R., Miller, D. R., et al. (2020). COVID-19 impacts mental health outcomes and ability/desire to participate in research among current research participants. Obesity. 2020:23016. doi: 10.1002/oby.23016
Castelli, L., Di Tella, M., Benfante, A., and Romeo, A. (2020). The spread of COVID-19 in the Italian population: anxiety, depression, and post-traumatic stress symptoms. Can. J. Psychiatry. 65, 731–732. doi: 10.1177/0706743720938598
Catalan, J., Harding, R., Sibley, E., Clucas, C., Croome, N., and Sherr, L. (2011). HIV infection and mental health: suicidal behaviour–systematic review. Psychol. Health Med. 16, 588–611. doi: 10.1080/13548506.2011.582125
Chan, A. O., and Huak, C. Y. (2004). Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. 54, 190–196. doi: 10.1093/occmed/kqh027
Chang, M. C., and Park, D. (2020). Incidence of post-traumatic stress disorder after coronavirus disease. Healthcare 8:40373. doi: 10.3390/healthcare8040373
Chen, B., Li, Q. X., Zhang, H., Zhu, J. Y., Yang, X., Wu, Y. H., et al. (2020). The psychological impact of COVID-19 outbreak on medical staff and the general public. Curr. Psychol. 2020, 1–9. doi: 10.21203/rs.3.rs-21213/v1
Chen, C. S., Wu, H. Y., Yang, P., and Yen, C. F. (2005). Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr. Serv. 56, 76–79. doi: 10.1176/appi.ps.56.1.76
Chen, M., Yue, F., and Liu, G. (2020). Investigation and study on mental status among first line nurses against new type coronavirus pneumonia epidemic under systematic support. J. Mod. Med. Health 36, 2671–2674. doi: 10.3969/j.issn.1009-5519.2020.17.005
Chew, N. W. S., Ngiam, J. N., Tan, B. Y. Q., Tham, S. M., Tan, C. Y. S., Jing, M. X., et al. (2020). Asian-Pacific perspective on the psychological well-being of healthcare workers during the evolution of the COVID-19 pandemic. Bjpsych Open 6:98. doi: 10.1192/bjo.2020.98
Chi, X. L., Becker, B., Yu, Q., Willeit, P., Jiao, C., Huang, L. Y., et al. (2020). Prevalence and psychosocial correlates of mental health outcomes among chinese college students during the coronavirus disease (COVID-19) pandemic. Front. Psychiatr. 11:803. doi: 10.3389/fpsyt.2020.00803
Civantos, A. M., Bertelli, A., Gonçalves, A., Getzen, E., Chang, C., Long, Q., et al. (2020b). Mental health among head and neck surgeons in Brazil during the COVID-19 pandemic: a national study. Am. J. Otolaryngol. 41:102694. doi: 10.1016/j.amjoto.2020.102694
Civantos, A. M., Byrnes, Y., Chang, C. G., Prasad, A., Chorath, K., Poonia, S. K., et al. (2020a). Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck-J. Sci. Spec. 42, 1597–1609. doi: 10.1002/hed.26292
Cortes-Alvarez, N. Y., Pineiro-Lamas, R., and Vuelvas-Olmos, C. R. (2020). Psychological effects and associated factors of COVID-19 in a Mexican sample. Disast. Med. Publ. 14, 413–424. doi: 10.1017/dmp.2020.215
Dai, W., Chen, L., Lai, Z., Li, Y., Wang, J., and Liu, A. (2016). The incidence of post-traumatic stress disorder among survivors after earthquakes:a systematic review and meta-analysis. BMC Psychiatr. 16:188. doi: 10.1186/s12888-016-0891-9
Di Tella, M., Romeo, A., Benfante, A., and Castelli, L. (2020). Mental health of healthcare workers during the COVID-19 pandemic in Italy. J. Eval. Clin. Pract. 26, 1583–1587. doi: 10.1111/jep.13444
Dobson, H., Malpas, C. B., Burrell, A. J. C., Gurvich, C., Chen, L., Kulkarni, J., et al. (2020). Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Austral. Psychiatr. 2020:1039856220965045. doi: 10.1177/1039856220965045
Dutheil, F., Mondillon, L., and Navel, V. (2020). PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol. Med. 2020, 1–2. doi: 10.1017/S0033291720001336
Edmondson, D., Richardson, S., Fausett, J. K., Falzon, L., Howard, V. J., and Kronish, I. M. (2013). Prevalence of PTSD in survivors of stroke and transient ischemic attack: a meta-analytic review. PLoS ONE 8:e66435. doi: 10.1371/journal.pone.0066435
El-Zoghby, S. M., Soltan, E. M., and Salama, H. M. (2020). Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Commun. Health 45, 689–695. doi: 10.1007/s10900-020-00853-5
Fang, Y., Zhe, D., and Shuran, L. (2004). Survey on mental status of subjects recovered from SARS. Chin. Ment. Health J. 18, 675–677. doi: 10.3321/j.issn:1000-6729.2004.10.001
Fekih-Romdhane, F., Ghrissi, F., Abbassi, B., Cherif, W., and Cheour, M. (2020). Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatr. Res. 290:113131. doi: 10.1016/j.psychres.2020.113131
Fiorillo, A., and Gorwood, P. (2020). The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry 63:e32. doi: 10.1192/j.eurpsy.2020.35
Forte, G., Favieri, F., Tambelli, R., and Casagrande, M. (2020). The enemy which sealed the world: effects of COVID-19 diffusion on the psychological state of the Italian Population. J. Clin. Med. 9:jcm9061802. doi: 10.3390/jcm9061802
Galea, S., and Resnick, H. (2005). Posttraumatic stress disorder in the general population after mass terrorist incidents: considerations about the nature of exposure. CNS Spectr. 10, 107–115. doi: 10.1017/S1092852900019441
Gardner, P. J., and Moallef, P. (2015). Psychological impact on SARS survivors: critical review of the English language literature. Can. Psychol. 56, 123–135. doi: 10.1037/a0037973
Giusti, E. M., Pedroli, E., D'Aniello, G. E., Stramba Badiale, C., Pietrabissa, G., Manna, C., et al. (2020). The psychological impact of the COVID-19 outbreak on health professionals: a cross-sectional study. Front. Psychol. 11:1684. doi: 10.3389/fpsyg.2020.01684
Gonzalez Ramirez, L. P., Martinez Arriaga, R. J., Hernandez-Gonzalez, M. A., and De la Roca-Chiapas, J. M. (2020). Psychological distress and signs of post-traumatic stress in response to the COVID-19 health emergency in a Mexican sample. Psychol. Res. Behav. Manag. 13, 589–597. doi: 10.2147/PRBM.S259563
Gonzalez-Sanguino, C., Ausin, B., Castellanos, M. A., Saiz, J., Lopez-Gomez, A., Ugidos, C., et al. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 87, 172–176. doi: 10.1016/j.bbi.2020.05.040
Greene, T., Neria, Y., and Gross, R. (2016). Prevalence, detection and correlates of PTSD in the primary care setting: a systematic review. J. Clin. Psychol. Med. Sett. 23, 160–180. doi: 10.1007/s10880-016-9449-8
Guo, J., Feng, X. L., Wang, X. H., and van IJzendoorn, M. H. (2020). Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in chinese adults. Int. J. Env. Res. Pub. He. 17:113857. doi: 10.3390/ijerph17113857
Hao, F., Tan, W., Jiang, L., Zhang, L., Zhao, X., Zou, Y., et al. (2020). Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020:69. doi: 10.1016/j.bbi.2020.04.069
Hawryluck, L., Gold, W. L., Robinson, S., Pogorski, S., Galea, S., and Styra, R. (2004). SARS control and psychological effects of quarantine, Toronto, Canada. Emerg. Infect. Dis. 10, 1206–1212. doi: 10.3201/eid1007.030703
Heron-Delaney, M., Kenardy, J., Charlton, E., and Matsuoka, Y. (2013). A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury 44, 1413–1422. doi: 10.1016/j.injury.2013.07.011
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hong, X., Currier, G. W., Zhao, X., Jiang, Y., Zhou, W., and Wei, J. (2009). Posttraumatic stress disorder in convalescent severe acute respiratory syndrome patients: a 4-year follow-up study. Gen. Hosp. Psychiatr. 31, 546–554. doi: 10.1016/j.genhosppsych.2009.06.008
Hongsheng, G., Wuli, H., Xiaoxia, L., Jie, W., Yilan, H., Ru, L., et al. (2006). A follow-up study of post-traumatic stress disorder of SARS patients after discharge. Chin. J. Rehabil. Med. 21, 1003–1004. doi: 10.3969/j.issn.1001-1242.2006.11.018
Houlihan, C. F., and Whitworth, J. A. (2019). Outbreak science: recent progress in the detection and response to outbreaks of infectious diseases. Clin. Med. 19, 140–144. doi: 10.7861/clinmedicine.19-2-140
Huang, J. Z., Han, M. F., Luo, T. D., Ren, A. K., and Zhou, X. P. (2020). Mental health survey of medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao DongWei Sheng Zhi Ye Bing Za Zhi. 38, 192–195. doi: 10.3760/cma.j.cn121094-20200219-00063
Jalloh, M. F., Li, W., Bunnell, R. E., Ethier, K. A., O'Leary, A., Hageman, K. M., et al. (2018). Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob. Health 3:e000471. doi: 10.1136/bmjgh-2017-000471
Jike, M., Itani, O., Watanabe, N., Buysse, D. J., and Kaneita, Y. (2018). Long sleep duration and health outcomes: a systematic review, meta-analysis and meta-regression. Sleep Med. Rev. 39, 25–36. doi: 10.1016/j.smrv.2017.06.011
Jung, H., Jung, S. Y., Lee, M. H., and Kim, M. S. (2020). Assessing the presence of post-traumatic stress and turnover intention among nurses post-middle east respiratory syndrome outbreak: the importance of supervisor support. Workplace Health Saf. 2020:2165079919897693. doi: 10.1177/2165079919897693
Karatzias, T., Shevlin, M., Murphy, J., McBride, O., Ben-Ezra, M., Bentall, R. P., et al. (2020). Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J. Trauma Stress 2020:22565. doi: 10.1002/jts.22565
Kisely, S., Warren, N., McMahon, L., Dalais, C., Henry, I., and Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta-analysis. BMJ 369:m1642. doi: 10.1136/bmj.m1642
Kwek, S. K., Chew, W. M., Ong, K. C., Ng, A. W., Lee, L. S., Kaw, G., et al. (2006). Quality of life and psychological status in survivors of severe acute respiratory syndrome at 3 months postdischarge. J. Psychosom. Res. 60, 513–519. doi: 10.1016/j.jpsychores.2005.08.020
Lahav, Y. (2020). Psychological distress related to COVID-19 - the contribution of continuous traumatic stress. J. Affect Disord. 277, 129–137. doi: 10.1016/j.jad.2020.07.141
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., Wei, N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. J. Am. Med. Assoc. Netw. Open 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Laiqi, Y., Xingqu, W., Yan, Z., Ming, L., Guangxiong, L., Yongli, G., et al. (2007). Mental health status of medical staffs fighting SARS: a long-dated investigation. China J. Health Psychol. 15, 567–569. doi: 10.3969/j.issn.1005-1252.2007.06.030
Lancee, W. J., Maunder, R. G., and Goldbloom, D. S. (2008). Prevalence of psychiatric disorders among toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Servic. 59, 91–95. doi: 10.1176/ps.2008.59.1.91
Lange, M., Joo, S., Couette, P. A., de Jaegher, S., Joly, F., and Humbert, X. (2020). Impact on mental health of the COVID-19 outbreak among community pharmacists during the sanitary lockdown period. Ann. Pharm. Fr. 78, 459–463. doi: 10.1016/j.pharma.2020.09.002
Le, X. T. T., Dang, A. K., Toweh, J., Nguyen, Q. N., Le, H. T., Do, T. T. T., et al. (2020). Evaluating the psychological impacts related to COVID-19 of Vietnamese people under the first nationwide partial lockdown in Vietnam. Front. Psychiatr. 11:824. doi: 10.3389/fpsyt.2020.00824
Lee, S. M., Kang, W. S., Cho, A.-R., Kim, T., and Park, J. K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Comprehens. Psychiatr. 87, 123–127. doi: 10.1016/j.comppsych.2018.10.003
Lee, T. M., Chi, I., Chung, L. W., and Chou, K. L. (2006). Ageing and psychological response during the post-SARS period. Aging Ment. Health 10, 303–311. doi: 10.1080/13607860600638545
Leng, F. (2020). Correlation analysis of anxiety, depression and post-traumatic stress disorder among frontline nurses fighting against new coronavirus pneumonia. J. Clin. Nurs. 19, 14–17. doi: 10.3969/j.issn.1671-8933.2020.03.005
Leng, M., Wei, L. L., Shi, X. H., Cao, G. R., Wei, Y. L., Xu, H., et al. (2020). Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs. Crit. Care. 2020:12528. doi: 10.1111/nicc.12528
Li, C., Mi, Y., Chu, J., Zhu, L., Zhang, Z., Liang, L., et al. (2020). Post-traumatic stress disorder of frontline nurses for COVID-19. J. Nurs. Train. 35, 615–618. doi: 10.16821/j.cnki.hsjx.2020.25.003
Li, G., Miao, J., Wang, H., Xu, S., Sun, W., Fan, Y., et al. (2020). Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatr. 91, 895–897. doi: 10.1136/jnnp-2020-323134
Li, Q. (2020). Psychosocial and coping responses toward 2019 coronavirus diseases (COVID-19): a cross-sectional study within the Chinese general population. QJM 113, 731–738. doi: 10.1093/qjmed/hcaa226
Li, X., Lu, P. X., Hu, L. T., Huang, T. H., and Lu, L. (2020). Factors associated with mental health results among workers with income losses exposed to COVID-19 in China. Int. J. Env. Res. Pub. He. 17:155627. doi: 10.3390/ijerph17155627
Li, X. C., Zhou, Y., and Xu, X. Y. (2020). Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: a predictive study. J. Nurs. Manag. 2020:13146. doi: 10.1111/jonm.13146
Li, Y., Qin, Q., Sun, Q., Sanford, L. D., Vgontzas, A. N., and Tang, X. (2020a). Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 16, 1417–1418. doi: 10.5664/jcsm.8524
Li, Y., Wang, Y., Jiang, J., Valdimarsdottir, U. A., Fall, K., Fang, F., et al. (2020b). Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 2020, 1–3. doi: 10.1017/S0033291720001555
Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z., Li, C., et al. (2020). The effect of COVID-19 on youth mental health. Psychiatr. Q. 2020:3. doi: 10.1007/s11126-020-09744-3
Liang, S. W., Chen, R. N., Liu, L. L., Li, X. G., Chen, J. B., Tang, S. Y., et al. (2020). The psychological impact of the COVID-19 epidemic on Guangdong College students: the difference between seeking and not seeking psychological help. Front. Psychol. 11:2231. doi: 10.3389/fpsyg.2020.02231
Lijun, Z., Sheng, C., Lei, Y., Qi, W., and Hongzhi, Y. (2020). A study on post-traumatic stress reaction to the first-line medical staffs against COVID-19. Health Med. Res. Pract. 17, 15–18. doi: 10.11986/j.issn.1673-873X.2020.04.004
Lin, C. Y., Peng, Y. C., Wu, Y. H., Chang, J., Chan, C. H., and Yang, D. Y. (2007). The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg. Med. J. 24, 12–17. doi: 10.1136/emj.2006.035089
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S., and Hahm, H. C. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatr. Res. 290:113172. doi: 10.1016/j.psychres.2020.113172
Liu, D., Baumeister, R. F., Veilleux, J. C., Chen, C., Liu, W., Yue, Y., et al. (2020). Risk factors associated with mental illness in hospital discharged patients infected with COVID-19 in Wuhan, China. Psychiatr. Res. 292:113297. doi: 10.1016/j.psychres.2020.113297
Liu, H., Petukhova, M. V., Sampson, N. A., Aguilar-Gaxiola, S., Alonso, J., Andrade, L. H., et al. (2017). Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the world health organization world mental health surveys. J. Am. Med. Assoc. Psychiatr. 74, 270–281. doi: 10.1001/jamapsychiatry.2016.3783
Liu, N., Zhang, F., Wei, C., Jia, Y., Shang, Z., Sun, L., et al. (2020). Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatr. Res. 287:112921. doi: 10.1016/j.psychres.2020.112921
Liu, X., Lin, Z., Zhu, H., Zhan, D., Han, T., and Yao, Q. (2020). Investigation of mental health status of medical stuff from Hainan who aided Hubei province to fight against COVID-19. Johnal Hanan Med. Univ. 26, 1285–1228. doi: 10.13210/j.cnki.jhmu.2020622.02
Liu, Y., Jiang, P., Cao, Y., Zhou, Y., and Li, Y. (2020). Investigation on the psychological stress of nursing staff during the novel coronavirus pneumonia epidemic and analysis of related factors. Nurs. Integr. Tradition. Chin. Western Med. 6, 179–183. doi: 10.11997/nitcwm.202008042
Loney, P. L., Chambers, L. W., Bennet, K. J., Roberts, J. G., and Stratford, P. W. (1998). Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis. Can. 19, 170–176.
Luceno-Moreno, L., Talavera-Velasco, B., Garcia-Albuerne, Y., and Martin-Garcia, J. (2020). Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish Health Personnel during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 17:155514. doi: 10.3390/ijerph17155514
Luyt, C. E., Combes, A., Becquemin, M. H., Beigelman-Aubry, C., Hatem, S., Brun, A. L., et al. (2012). Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest 142, 583–592. doi: 10.1378/chest.11-2196
Ma, Z. F., Zhang, Y. T., Luo, X. Q., Li, X. L., Li, Y. S., Liu, S. C., et al. (2020). Increased stressful impact among general population in mainland China amid the COVID-19 pandemic: a nationwide cross-sectional study conducted after Wuhan city's travel ban was lifted. Int. J. Soc. Psychiatr. 66, 770–779. doi: 10.1177/0020764020935489
Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., Ho, S. C., and Chan, V. L. (2010). Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatr. 32, 590–598. doi: 10.1016/j.genhosppsych.2010.07.007
Mata, D. A., Ramos, M. A., Bansal, N., Khan, R., Guille, C., Di Angelantonio, E., et al. (2015). Prevalence of depression and depressive symptoms among resident physicians a systematic review and meta-analysis. J. Am. Med. Assoc. 314, 2373–2383. doi: 10.1001/jama.2015.15845
Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., Borgundvaag, B., Evans, S., et al. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 12, 1924–1932. doi: 10.3201/eid1212.060584
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Morganstein, J. C., and Ursano, R. J. (2020). Ecological disasters and mental health: causes, consequences, and interventions. Front. Psychiatr. 11:1. doi: 10.3389/fpsyt.2020.00001
Morina, N., Stam, K., Pollet, T. V., and Priebe, S. (2018). Prevalence of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J. Affect. Disord. 239, 328–338. doi: 10.1016/j.jad.2018.07.027
Neria, Y., Nandi, A., and Galea, S. (2008). Post-traumatic stress disorder following disasters: a systematic review. Psychol. Med. 38, 467–480. doi: 10.1017/S0033291707001353
Nie, A., Su, X., Zhang, S., Guan, W., and Li, J. (2020). Psychological impact of COVID-19 outbreak on frontline nurses: a cross-sectional survey study. J. Clin. Nurs. 2020:15454. doi: 10.1111/jocn.15454
Qi, R., Chen, W., Liu, S., Thompson, P. M., Zhang, L. J., Xia, F., et al. (2020). Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv 2020. doi: 10.1101/2020.05.08.20031666
Qiu, D., Yu, Y., Li, R. Q., Li, Y. L., and Xiao, S. Y. (2020). Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Med. 67, 258–266. doi: 10.1016/j.sleep.2019.01.047
Reynolds, D. L., Garay, J. R., Deamond, S. L., Moran, M. K., Gold, W., and Styra, R. (2008). Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol. Infect. 136, 997–1007. doi: 10.1017/S0950268807009156
Riello, M., Purgato, M., Bove, C., MacTaggart, D., and Rusconi, E. (2020). Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. Roy Soc. Open Sci. 7:200880. doi: 10.1098/rsos.200880
Righy, C., Rosa, R. G., da Silva, R. T. A., Kochhann, R., Migliavaca, C. B., Robinson, C. C., et al. (2019). Prevalence of post-traumatic stress disorder symptoms in adult critical care survivors: a systematic review and meta-analysis. Crit. Care. 23:213. doi: 10.1186/s13054-019-2489-3
Rodriguez-Rey, R., Garrido-Hernansaiz, H., and Collado, S. (2020). Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 11:1540. doi: 10.3389/fpsyg.2020.01540
Rogers, J. P., Chesney, E., Oliver, D., Pollak, T. A., McGuire, P., Fusar-Poli, P., et al. (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatr. 7, 611–627. doi: 10.1016/S2215-0366(20)30203-0
Rossi, R., Socci, V., Pacitti, F., Di Lorenzo, G., Di Marco, A., Siracusano, A., et al. (2020a). Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. J. Am. Med. Assoc. Netw. Open 3:10185. doi: 10.1001/jamanetworkopen.2020.10185
Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., et al. (2020b). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatr. 11:790. doi: 10.3389/fpsyt.2020.00790
Sanderson, S., Tatt, I. D., and Higgins, J. P. (2007). Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int. J. Epidemiol. 36, 666–676. doi: 10.1093/ije/dym018
Seyahi, E., Poyraz, B. C., Sut, N., Akdogan, S., and Hamuryudan, V. (2020). The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40, 1229–1238. doi: 10.1007/s00296-020-04626-0
Sherman, A. C., Williams, M. L., Amick, B. C., Hudson, T. J., and Messias, E. L. (2020). Mental health outcomes associated with the COVID-19 pandemic: prevalence and risk factors in a southern US state. Psychiatr. Res. 293:113476. doi: 10.1016/j.psychres.2020.113476
Si, M. Y., Su, X. Y., Jiang, Y., Wang, W. J., Gu, X. F., Ma, L., et al. (2020). Psychological impact of COVID-19 on medical care workers in China. Infect. Dis. Poverty 9:113. doi: 10.1186/s40249-020-00724-0
Sim, K., Huak Chan, Y., Chong, P. N., Chua, H. C., and Wen Soon, S. (2010). Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J. Psychosom. Res. 68, 195–202. doi: 10.1016/j.jpsychores.2009.04.004
Sin, S. S., and Huak, C. Y. (2004). Psychological impact of the SARS outbreak on a Singaporean rehabilitation department. Int. J. Therapy Rehabil. 11, 417–424. doi: 10.12968/ijtr.2004.11.9.19589
Song, X., Fu, W., Liu, X., Luo, Z., Wang, R., Zhou, N., et al. (2020). Mental health status of medical staff in emergency departments during the Coronavirus disease 2019 epidemic in China. Brain Behav. Immun. 88, 60–65. doi: 10.1016/j.bbi.2020.06.002
Spoorthy, M. S., Pratapa, S. K., and Mahant, S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic-a review. Asian J. Psychiatr. 51:102119. doi: 10.1016/j.ajp.2020.102119
Steele, L., Orefuwa, E., and Dickmann, P. (2016). Drivers of earlier infectious disease outbreak detection: a systematic literature review. Int. J. Infect. Dis. 53, 15–20. doi: 10.1016/j.ijid.2016.10.005
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. J. Am. Med. Assoc. 283, 2008–2012. doi: 10.1001/jama.283.15.2008
Su, T. P., Lien, T. C., Yang, C. Y., Su, Y. L., Wang, J. H., Tsai, S. L., et al. (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 41, 119–130. doi: 10.1016/j.jpsychires.2005.12.006
Tan, W., Hao, F., McIntyre, R. S., Jiang, L., Jiang, X., Zhang, L., et al. (2020). Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 87, 84–92. doi: 10.1016/j.bbi.2020.04.055
Tang, L., Pan, L., Yuan, L., and Zha, L. (2017). Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int. J. Nurs. Sci. 4, 63–67. doi: 10.1016/j.ijnss.2016.12.002
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., et al. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020:9. doi: 10.1016/j.jad.2020.05.009
Tee, M. L., Tee, C. A., Anlacan, J. P., Aligam, K. J. G., Reyes, P. W. C., Kuruchittham, V., et al. (2020). Psychological impact of COVID-19 pandemic in the Philippines. J. Affect Disord. 277, 379–391. doi: 10.1016/j.jad.2020.08.043
Tie-ying, S., Chaojia, J., Qi-gui, J. Z., and Xiang-yu, Q. (2005). Post-traumatic stress disorder and related factors following the severe acute respiratory syndrome. Chin. J. Clin. Rehabil. 9, 9–13. doi: 10.3321/j.issn:1673-8225.2005.44.012
Traunmuller, C., Stefitz, R., Gaisbachgrabner, K., and Schwerdtfeger, A. (2020). Psychological correlates of COVID-19 pandemic in the Austrian population. BMC Public Health 20:1395. doi: 10.1186/s12889-020-09489-5
Tucci, V., Moukaddam, N., Meadows, J., Shah, S., Galwankar, S. C., and Kapur, G. B. (2017). The forgotten plague: psychiatric manifestations of ebola, zika, and emerging infectious diseases. J. Glob. Infect. Dis. 9, 151–156. doi: 10.4103/jgid.jgid_66_17
Varshney, M., Parel, J. T., Raizada, N., and Sarin, S. K. (2020). Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE 15:e0233874. doi: 10.1371/journal.pone.0233874
Vyas, K. J., Delaney, E. M., Webb-Murphy, J. A., and Johnston, S. L. (2016). Psychological impact of deploying in support of the U.S. Response to ebola: a systematic review and meta-analysis of past outbreaks. Mil. Med. 181, e1515–e1531. doi: 10.7205/MILMED-D-15-00473
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020:28. doi: 10.1016/j.bbi.2020.04.028
Wang, Z., Wu, X., Dai, W., Kaminga, A. C., Wu, X., Pan, X., et al. (2019). The prevalence of posttraumatic stress disorder among survivors after a typhoon or hurricane: a systematic review and meta-analysis. Disast. Med. Public Health Prep. 13, 1065–1073. doi: 10.1017/dmp.2019.26
Wesemann, U., Hadjamu, N., Willmund, G., Dolff, S., Vonderlin, N., Wakili, R., et al. (2020). Influence of COVID-19 on general stress and posttraumatic stress symptoms among hospitalized high-risk patients. Psychol. Med. 2020, 1–2. doi: 10.1017/S0033291720003165
WHO. (2020). Coronavirus disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update 2020. Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ (accessed December 10, 2020).
Winsper, C., Ganapathy, R., Marwaha, S., Large, M., Birchwood, M., and Singh, S. P. (2013). A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatr. Scand. 128, 413–421. doi: 10.1111/acps.12113
Wu, K. K., Chan, S. K., and Ma, T. M. (2005). Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J. Traumat. Stress 18, 39–42. doi: 10.1002/jts.20004
Wu, P., Fang, Y., Guan, Z., Fan, B., Kong, J., Yao, Z., et al. (2009). The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatr. 54, 302–311. doi: 10.1177/070674370905400504
Xiao, S. Y., Luo, D., and Xiao, Y. (2020). Survivors of COVID-19 are at high risk of posttraumatic stress disorder. Glob. Health Res. Pol. 5:2. doi: 10.1186/s41256-020-00155-2
Xie, R., Zhu, X., and Huang, X. (2020). Anxiety state of ordinary residents under novel coronavirus pneumonia epidemic situation and related factors of emergency level. China J. Health Psychol. 28, 1670–1674. doi: 10.13342/j.cnki.cjhp.2020.11.014
Xu, J., Zheng, Y., Wang, M., Zhao, J., Zhan, Q., Fu, M., et al. (2011). Predictors of symptoms of posttraumatic stress in Chinese university students during the 2009 H1N1 influenza pandemic. Med. Sci. Monit. 17, PH60–PH64. doi: 10.12659/MSM.881836
Yin, Q., Sun, Z., Liu, T., Ni, X., Deng, X., Jia, Y., et al. (2020). Posttraumatic stress symptoms of health care workers during the corona virus disease 2019 (COVID-19). Clin. Psychol. Psychother. 2020:2477. doi: 10.1002/cpp.2477
Yong, X., Ke-rang, Z., and Hong, Y. (2005). Difference of posttraumatic stress disorder between severe acute respiratory syndrome patients and the public in epidemic area. Chin. J. Clin. Rehabil. 9, 214–215. doi: 10.3321/j.issn:1673-8225.2005.16.020
Yuan, B., Cai, X., Wang, J., Hu, X., Li, Z., Lu, T., et al. (2020). Investigation of psychological stress state of during early convalescence of patients with coronavirus disease 2019 and analysis of its influencing factors. Chin. J. Clin. Neurosurg. 25, 531–534. doi: 10.13798/j.issn.1009-153X.2020.08.011
Zhang, C., Ye, M., Fu, Y., Yang, M., Luo, F., Yuan, J., et al. (2020). The psychological impact of the COVID-19 pandemic on teenagers in China. J. Adolesc. Health 67, 747–755. doi: 10.1016/j.jadohealth.2020.08.026
Zhang, Y., Liu, X., Xue, M., Luo, L., He, G., Feng, P., et al. (2020). The correlation between post-traumatic stress disorder and perceived stress in suspected COVID-19 patients quarantined in hospital. Chin. J. Respir. Crit. Care Med. 19, 325-329. doi: 10.7507/1671-6205.202005021
Zhang, Y. F., and Ma, Z. F. (2020a). Psychological responses and lifestyle changes among pregnant women with respect to the early stages of COVID-19 pandemic. Int. J. Soc. Psychiatr. 67, 344–350. doi: 10.1177/0020764020952116
Zhang, Y. F., and Ma, Z. F. (2020b). Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Env. Res. Pub. He. 17:72381. doi: 10.3390/ijerph17072381
Zhao, Y. Q., An, Y. Y., Tan, X., and Li, X. H. (2020). Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma 25, 580–593. doi: 10.1080/15325024.2020.1761592
Zhongguo, L., Zuxun, L., Yong, X., and Kerang, Z. (2006). Investigation on posttraumatic stress reactions in SARS patients. J. Shanxi Med. Univ. 37, 56–58. doi: 10.3969/j.issn.1007-6611.2006.01.019
Keywords: infectious disease outbreak, systematic review, meta-analysis, COVID-19, post-traumatic stress symptoms
Citation: Qiu D, Li Y, Li L, He J, Ouyang F and Xiao S (2021) Infectious Disease Outbreak and Post-Traumatic Stress Symptoms: A Systematic Review and Meta-Analysis. Front. Psychol. 12:668784. doi: 10.3389/fpsyg.2021.668784
Received: 17 February 2021; Accepted: 05 July 2021;
Published: 05 August 2021.
Edited by:
Rubén N. Muzio, Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), ArgentinaReviewed by:
Agata Benfante, University of Turin, ItalySeockhoon Chung, University of Ulsan, South Korea
Ferdinando Franzoni, University of Pisa, Italy
Copyright © 2021 Qiu, Li, Li, He, Ouyang and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuiyuan Xiao, eGlhb3N5QGNzdS5lZHUuY24=
 Dan Qiu
Dan Qiu Yilu Li1
Yilu Li1 Shuiyuan Xiao
Shuiyuan Xiao