
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 23 March 2021
Sec. Psychopathology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.638831
Fear is a common and potentially distressful psychological response to the current COVID-19 pandemic. The factors associated with such fear remains relatively unstudied among older adults. We investigated if fear of COVID-19 could be associated with a combination of psychological factors such as anxiety and depressive symptoms, and risk perception of COVID-19, and demographic factors in a community sample of older adults. Older adults (N = 413, Mage = 69.09 years, SD = 5.45) completed measures of fear of COVID-19, anxiety and depressive symptoms, and risk perception of COVID-19, during a COVID-19 lockdown. These variables, together with demographics, were fitted to a structural equation model. Anxiety and depressive symptoms were highly correlated with each other and were combined into the higher order latent variable of affective symptoms for analyses. The final model revealed that fear of COVID-19 was positively associated with psychological factors of affective symptoms and risk perception. Older age was associated with greater fear of COVID-19. Our findings showed that fear of COVID-19 can be a projection of pre-existing affective symptoms and inflated risk perceptions and highlighted the need to address the incorrect risk perceptions of COVID-19 and socio-affective issues among older adults in the community.
The novel coronavirus disease (COVID-19) was first discovered in Wuhan, China in December 2019, and has since been declared a global pandemic by the World Health Organization in March 2020 (World Health Organization, 2020b). In response to the health crisis, countries worldwide have implemented a series of public health and social distancing measures to curb the spread of COVID-19.
Singapore saw its first confirmed COVID-19 case on January 23, 2020, and the emergence of its first cluster of community cases on February 04, 2020 (Goh, 2020). As the threat of COVID-19 grew, the government raised its Disease Outbreak Response System Condition1 level from yellow to orange on February 7, which signaled to the public that COVID-19 is severe and spreads easily, with moderate disruptions to daily life (Khalik, 2020). Shortly after, panic buying was observed in the community, with household items such as toilet paper and instant noodles being wiped out in supermarkets (Baker, 2020).
The COVID-19 situation began to worsen, and Singapore reported the first two local COVID-19 deaths on March 21. Eventually, on April 3, a “circuit breaker” measure (gov.sg, 2020a; Ministry of Health, 2020) was put in place to prevent further spread of the disease. The circuit breaker was implemented from April 07 to June 01, 2020, which comprised a series of measures such as a nationwide partial lockdown and closure of non-essential workplaces. Wearing of masks was mandatory and gathering in groups was banned. During this period, confirmed cases of COVID-19 in local communities still continued to rise substantially, and new clusters started to form and spread rapidly among foreign workers’ dormitories. On April 20, Singapore reached its peak of 1,426 new COVID-19 cases, with the majority of them coming from dormitories (Baker, 2020).
Following the circuit breaker, a “Phase 1” measure was implemented from June 02 to 18, 2020 (gov.sg, 2020b). Phase 1 was part of a three-phased approach aimed to progressively lift the circuit breaker measures, to ensure that transmission rates of COVID-19 remain under control (gov.sg, 2020b). While there was gradual re-opening of some businesses and activities, many restrictions in Phase 1 were largely similar to those in the circuit breaker.
With the backdrop of high COVID-19 cases and the constantly evolving situation locally and globally, it is imperative to examine the psychological and mental health impacts COVID-19 brings to individuals. One psychological response commonly reported is fear toward COVID-19 (Ahorsu et al., 2020a; Pakpour and Griffiths, 2020; Schimmenti et al., 2020). Fear is an adaptive emotion fundamental for survival, which serves to prepare the individual for behavioral responses to potential threats (Garcia, 2017). Fear may occur in response to specific stimuli in the present environment, or in anticipation of future or imagined events that pose a threat to oneself.
In the context of the COVID-19 pandemic, fear may be beneficial as it motivates preventive behavior such as hand-washing and social distancing (Harper et al., 2020). However, fear can become maladaptive when it is excessive, leading to significant levels of distress and irrational behaviors at both the individual and population level. For the former, fear of COVID-19 may exacerbate pre-existing mental health conditions (Ho et al., 2020), while in several cases, fear may lead to suicidal behavior (Dsouza et al., 2020; Mamun and Griffiths, 2020; Sher, 2020). For the latter, fear predicts panic buying (Arafat et al., 2020) as well as racist and discriminatory responses (Devakumar et al., 2020). As such, it is important to investigate the variables associated with fear of COVID-19, in order to ensure fear is well-managed and that detrimental consequences resulting from excessive fear is minimized.
Fear of COVID-19 is associated with some major psychological factors, according to the existing literature. First, affective symptoms such as those of depression and anxiety may be associated with fear. Depression refers to a state of low mood characterized by general negative views of the self, world and the future (Beck, 1979), while anxiety is an emotion characterized by internal feelings of tension and worry, which may be accompanied with physical responses such as sweating and increased heart rate (American Psychological Association, 2021). Symptoms of depression and anxiety are common psychological reactions to COVID-19 (Rajkumar, 2020), and correlational evidence thus far suggests that fear of COVID-19 is positively associated with depression and anxiety (Harper et al., 2020; Satici et al., 2020). Further, another study found that depression and anxiety, amongst other variables, play a mediating role between fear of COVID-19 and positivity (Bakioğlu et al., 2020). Given an unprecedented time with high infection and transmission rates of COVID-19, the co-occurrence and association between fear, anxiety and depression are not surprising. Hence, based on the aforementioned evidence in the literature, we would expect fear of COVID-19 to be associated with both depressive and anxiety symptoms.
Another related psychological factor may be risk perception. Risk perception is a subjective judgment an individual makes on the likelihood of negative occurrences (Paek and Hove, 2017), and it is often influenced by cognitive, emotional, social, and cultural factors (Douglas and Wildavsky, 1983; Slovic, 2000; Loewenstein et al., 2001; Van der Linden, 2015). While literature on risk perception from previous infectious diseases remains scant (De Zwart et al., 2007), many laboratory studies suggest an interplay between emotions and heightened risk perception, with fearful individuals exhibiting increased risk perception of negative outcomes following fear-relevant stimuli. This association has been found in various groups of individuals, such as those with fears of snakes and spiders (Tomarken et al., 1989; Amin and Lovibond, 1997; Kennedy et al., 1997), fear of contamination (Olatunji et al., 2006), and socially anxious individuals (de Jong et al., 1998). Additionally, a field experiment on the terrorist attack on September 11, 2001 has shown that fearful individuals had higher risk estimates and more plans for precautionary actions (Lerner et al., 2003).
While studies have shown known associations between risk perception and fear, it is important to note that they are of conceptually different constructs. Inflated risk perceptions may not always be accompanied by increased fear levels. For example, repeated prolonged exposure to the fear stimulus may ultimately reduce or eliminate fear entirely, but judgment of risks may still remain the same as before (as risk can be influenced by factors other than emotional ones). Nonetheless, in the context of the COVID-19 pandemic where there is no previous prolonged exposure, we would expect risk perception and fear of COVID-19 to be positively related. Individuals with increased risk perception may also have higher fear levels of COVID-19.
Given these previous fear-related findings, we put together a model of fear of COVID-19 which explores the relationships with anxiety and depressive symptoms, and risk perception of COVID-19. We tested this model using structural equation modeling on cross-sectional data collected from community-dwelling older adults during a COVID-19 lockdown in Singapore. A secondary aim of our study was to investigate potential demographic factors associated with fear of COVID-19, which would be useful to identify potential demographical subgroups who are more fearful of COVID-19.
Participants in our study were recruited from the Community Health and Intergenerational study, an existing cohort study involving community-dwelling older adults in Singapore (Lee R. Z. Y. et al., 2020). These participants were recruited via door-to-door recruitment within various housing estates in the Western region of Singapore. Participants from the Community Health and Intergenerational study were invited to join the current study based on the following inclusion criteria: (a) age between 60 and 99 years, (b) literate in either English or Mandarin, and (c) no diagnosis of Dementia. These participants must also have indicated their consent to be re-contacted for future studies, and to donate their coded data for future research in the Community Health and Intergenerational study’s consent form. A total of 582 older adults fulfilled the inclusion criteria and were contacted over the phone for their interest in the current study.
Participation to the current study was voluntary, and consent (verbal or written) was obtained from all participants before enrolment. Of the 582 contacted, 454 older adults provided consent to participate. However, 40 failed to submit responses, resulting in a response rate of 91.2%. 1 had missing data and were excluded from further analysis. This resulted in a final sample of 413 participants. The socio-demographic characteristics of the sample are illustrated in Table 1.
Participants completed the study questionnaires in either English or Mandarin, on an online survey platform (Qualtrics) or through mail. Participants who completed all questionnaires were remunerated with $10. The study received ethics approval by the National University of Singapore Institutional Review Board (S-20-118E). Data collection took place from May 11 to June 05, 2020.
The COVID-19 Fear Inventory is a newly constructed 13-item scale developed by the authors to assess fear of COVID-19 and its associated concerns. The inventory was adapted from the Ebola Fear Inventory (Blakey et al., 2015) and the Swine Flu Anxiety Items (Wheaton et al., 2012), which were used to assess Ebola and H1N1 (swine flu) fears respectively. Participants rated their agreement with each item on a 5-point Likert scale ranging from 1 (“not at all”) to 5 (“very much”). Higher scores corresponded to higher fear levels of COVID-19. The full list of items in the COVID-19 Fear Inventory is presented in Supplementary Table 1.
The GDS-15 (Yesavage and Sheikh, 1986) is a shortened version of the Geriatric Depression Scale used to assess depressive symptoms among older adults. Participants responded “yes” or “no” to 15 items, with 1 point awarded to each response indicative of depressive symptoms. Higher scores corresponded to higher levels of depressive symptoms. The scale demonstrated good psychometric validity in the local context (Nyunt et al., 2009), achieving the optimal cut-off of 4/5 used in most studies (Wancata et al., 2006).
The GAI-SF (Byrne and Pachana, 2011) is a shortened version of the Geriatric Anxiety Inventory (GAI), which consists of 5 items that measures anxiety symptoms among older adults. Participants were asked to indicate “agree” or “disagree” for each item, with higher scores suggesting higher levels of anxiety symptoms. The GAI-SF was found to have good psychometric properties for assessing anxiety symptoms and may be used as a useful alternative to the original GAI (Johnco et al., 2015).
The Risk of Infection Questionnaire is a 10-item scale constructed by the authors which aimed to assess perceived risk of COVID-19 infection. Participants rated the likelihood of being infected with COVID-19 under different situations (e.g., in a train) or from contact with commonplace objects (e.g., lift buttons). Each item was rated on a 4-point Likert scale ranging from 1 (“very unlikely”) to 4 (“very likely”). Higher scores indicated heightened risk perception of COVID-19 infection. The full list of items in the questionnaire can be found in Supplementary Table 2. At the point of study conceptualization, there were no similar scales available for the purpose of measuring perceived risk of COVID-19 infection.
First, we conducted a confirmatory factor analysis (CFA) to establish the factor structure of the COVID-19 Fear Inventory and Risk of Infection Questionnaire. As both scales were newly developed, it was important to ensure that the included items for analysis fit a hypothesized measurement model as well as to partial out measurement error. Individual items from each scale were fitted into latent variables (i.e., fear and risk perception latent variable), which were then used for further analysis. Likewise, latent variables for depressive and anxiety symptoms were constructed from items in GDS and GAI-SF, respectively, to partial out their measurement error.
Next, we used structural equation modeling (SEM) to model the relationship between fear, anxiety, and depressive symptoms, and risk perception, with age, gender, and years of education included as demographic covariates. The latent variables for depressive and anxiety symptoms were loaded on to a higher-level latent variable—affective symptoms, which was used to predict fear, instead of having anxiety and depressive symptoms predict fear individually. Using SEM for our data analysis strategy was appropriate as the SEM approach is versatile enough for us to concurrently fit items into a measurement model, and to explore the relationships between the fitted latent variables.
For both CFA and SEM, robust maximum likelihood was used for parameters estimation, with analyses being carried out with the R package lavaan (Rosseel, 2012). The Root Mean Square Error of Approximation (RMSEA), Comparative Fit Index (CFI), Standardized Root Mean square Residual (SRMR), Akaike Information Criterion (AIC) and Bayesian Information Criterion (BIC) were used to assess model fit. CFI values > 0.90 were considered an acceptable fit (Hair et al., 2010), while SRMR and RMSEA values < 0.08 were indicative of an acceptable model (Hu and Bentler, 1999). Lower information criterion values correspond to better fit. The χ2 test of difference was used to compare the fit between models.
Correlations between fear and other continuous variables were examined using Pearson correlation coefficients. Statistical significance was set at p < 0.05. A post hoc power analysis on the R package SemPower (Moshagen and Erdfelder, 2016) was also conducted to determine the achieved power of the final SEM model. All analyses were performed in R 4.0.0. The R code for executing these analyses is available at https://osf.io/byfc4.
As COVID-19 Fear Inventory is a newly developed scale, we first employed CFA to evaluate its factor structure. Items 7, 8, 10 and 11 were excluded from analysis due to low factor loadings and other theoretical considerations. For instance, items 7 and 8 relate to the threat of COVID-19 influencing one to practice social distancing and use protective supplies. As these actions were made compulsory by the government (Ang and Phua, 2020; The Straits Times, 2020), it may be possible that individuals were motivated to follow these measures as a result of fear and obedience to the rules, not by fear alone. For item 10 [“To what extent do you engage in panic buying (i.e., buying large amounts of protective supplies and other essential items because of the threat of COVID-19)?”], panic buying only occurred during the early stages of the pandemic, and it was not prevalent during the period of data collection. Item 11 relates to the fear of one’s household income being affected due to the threat of COVID-19. As household income was supplemented with government financial packages (gov.sg, 2020c), this item would not be very relevant. Taken together, these items may not be true measures of fear, and were removed from the model. This resulted in a 9-item scale with unstandardized factor loadings ranging from 0.55 to 1.0 (p < 0.001). The results also indicated that a single factor best fits the model. Supplementary Table 3 shows the fit indices of the tested CFA models.
Similarly, CFA was conducted to validate the factor structure of the Risk of Infection Questionnaire. The results showed that items 2 (“pressing the lift buttons”) and 9 (“being around doctors, nurses and other hospital staff”) had relatively lower factor loadings. Furthermore, situations described in items 2 and 9 have some overlaps with those in items 3 and 10 (i.e., items 2 and 3 both depict a lift setting, while items 9 and 10 both depict a hospital setting). Because of the above considerations, items 2 and 9 were excluded from subsequent analysis, thus resulting in a final 8-item scale with unstandardized factor loadings ranging from 1.0 to 1.3 (p < 0.001). The results indicated that a single factor best fits the model. Fit indices of the tested CFA models can be found in Supplementary Table 3.
Table 2 presents the mean scores, standard deviations, and Cronbach’s alpha for the total scores of the study measures included for analysis in the SEM model. Pearson correlations were conducted to examine the relationships among them. Table 3 presents the results obtained. As shown, there were significant positive correlations between fear and age, depressive symptoms, anxiety symptoms, and risk perception; no significant correlations were found between fear and years of education.
The latent variables and covariates were fitted into a baseline model which is illustrated in Figure 1. Our findings revealed that age was significantly associated with fear. As expected, anxiety and depressive symptoms were seen to be highly associated with each other (p < 0.01). Model fit indices of the model was unsatisfactory [χ2(693) = 1259.30, p < 0.001; RMSEA = 0.05; CFI = 0.86; SRMR = 0.06].
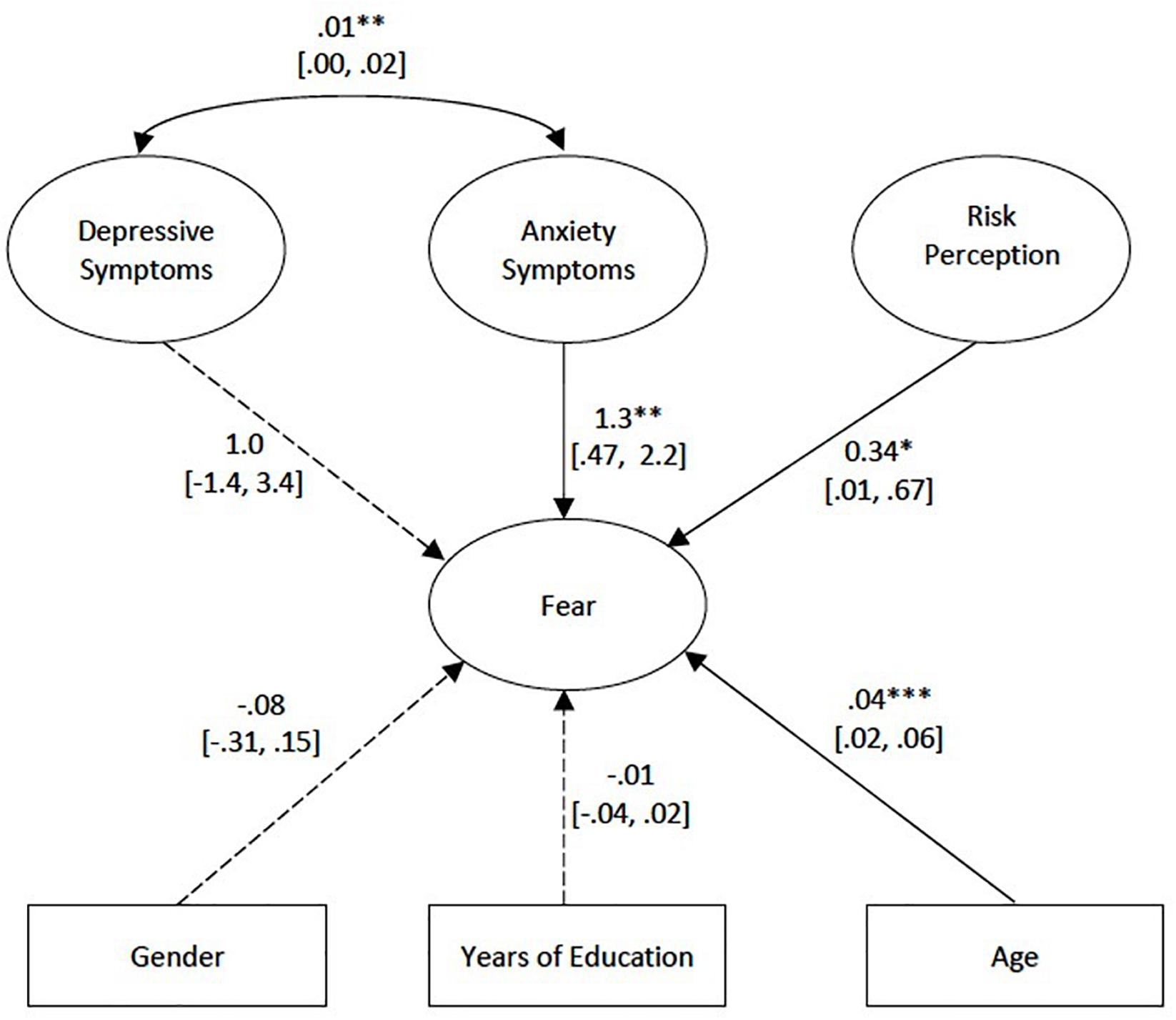
Figure 1. Baseline model. Unstandardized regression estimates are shown. Solid lines are significant at p < 0.05, while dotted lines are non-significant. Ovals represent latent variables, while rectangles represent observed variables. Individual indicators in the questionnaires are omitted in the figures for simplicity. Figures in brackets represent the Confidence Intervals. *p < 0.05, **p < 0.01, ***p < 0.001.
A second model was constructed to improve the model fit. In this model, only variables that were significantly associated with fear (i.e., age, affective symptoms of anxiety and depression, and risk perception) were included. Evaluation of model fit indices for the second model revealed that it did not have a reasonable fit [χ2(624) = 1100.13, p < 0.001; RMSEA = 0.05; CFI = 0.87; SRMR = 0.06].
Modification indices were examined to determine whether the model fit could be improved. This resulted in a final model, which included three correlated errors from the COVID-19 Fear Inventory based on statistical and theoretical considerations. The first pair of error terms was items 1 (“To what extent are you afraid of being infected with COVID-19?”) and 2 (“If you are infected with COVID-19, to what extent are you afraid that you will be severely ill, or die?”). Correlated errors were expected as both items assessed fears of COVID-19 infecting the self. Similarly, there were overlaps between items 3 (“To what extent are you afraid that your loved ones will be infected with COVID-19?”) and 4 (“If your loved ones are infected with COVID-19, to what extent are you afraid that they will be severely ill, or die?”) as both items assessed fears of COVID-19 infecting loved ones. The last pair of error terms was items 12 (“To what extent are you worried that the threat of COVID-19 could affect your personal relationships?”) and 13 [“To what extent has the threat of COVID-19 influenced you to experience more negative emotions than usual (e.g., fear, worry, panic, etc.)?”]. Both items related to socio-emotional fears arising from COVID-19—strains on personal relationships may also affect one’s emotions in a negative manner.
With the inclusion of the correlated errors, the model resulted in satisfactory fit indices [χ2(621) = 982.01, p < 0.001; RMSEA = 0.04; CFI = 0.91; SRMR = 0.06]. Furthermore, the χ2 test of difference between the models with and without the correlated errors was significant (Δχ2 = 72.94, Δdf = 3, p < 0.001), thus suggesting that the inclusion of the correlated errors significantly improved the model fit. Our post hoc power analyses on the model indicated that the sample size of N = 413 was associated with a power larger than >99.99% to reject a wrong model (with df = 621) with an amount of misspecification corresponding to RMSEA = 0.04 on alpha = 0.05. The results of the final model are presented in Figure 2.
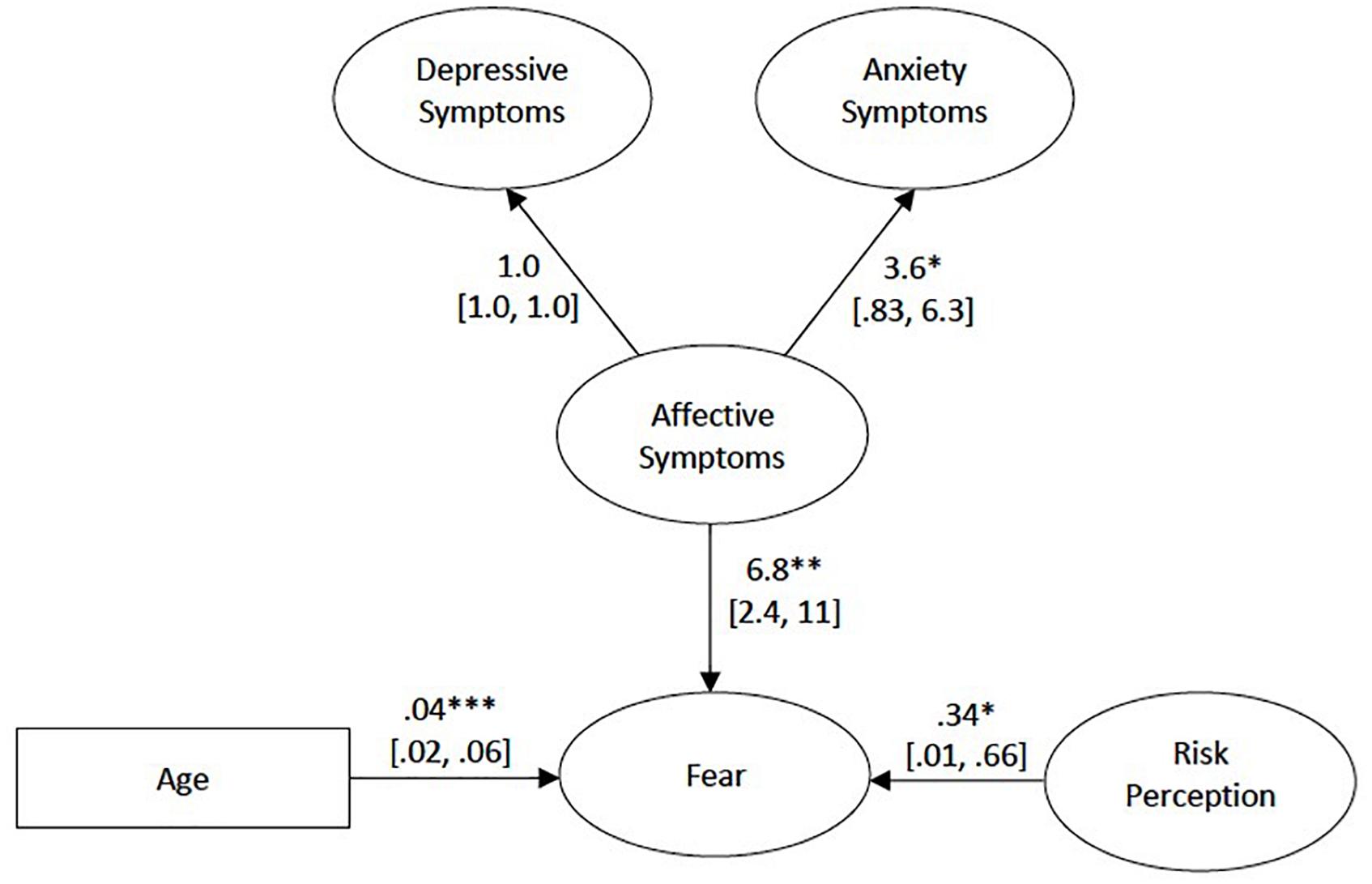
Figure 2. Final model. Unstandardized regression estimates are shown. Ovals represent latent variables, while the rectangle represents the observed variable. Correlated errors among the items in the COVID-19 Fear Inventory are not shown for clarity. Statistical significance for the path between depressive and affective symptoms was not tested as it was set to 1. Figures in brackets represent the Confidence Intervals. *p < 0.05, **p < 0.01, ***p < 0.001.
The current study examined the association between psychological factors and fear of COVID-19 among community-dwelling older adults during a COVID-19 lockdown in Singapore. We also investigated potential demographic factors which could be related to fear of COVID-19. Our results indicated that affective symptoms (which include both depressive and anxiety symptoms), risk perception, and old age were associated with heightened fear of COVID-19.
Our findings revealed a strong interrelation between fear of COVID-19 and affective symptoms, suggesting the significant effect COVID-19 has on psychological well-being and mental health. While the relationship between fear and psychological distress is explored and well-supported in various studies (Bakioğlu et al., 2020; Harper et al., 2020; Satici et al., 2020), few studies (Ahorsu et al., 2020b) have explored this relationship specifically on the older adult population. Given that older adults are a high-risk group due to their increased physical and mental health vulnerabilities (Lee K. et al., 2020), more effort and attention should be given to explore COVID-19-related psychological distress among older adults.
The relationship between fear of COVID-19 and affective symptoms could be attributed to catastrophizing (Beck, 1979), a cognitive distortion commonly associated with anxiety and depression. Catastrophizing is a negative thinking style where one expects the worst possible outcome in a given situation. In the context of the COVID-19 pandemic, the negative outlook on reality could be accompanied with negative moods and emotions, including the experience of heightened fear levels. Speculatively, the association among the three variables seems to suggest the presence of a negative reinforcing loop; increased negativity may lead to higher fear levels toward COVID-19, which may in turn contribute to higher levels of depressive and anxiety symptoms (Bakioğlu et al., 2020; Satici et al., 2020). Given the cross-sectional nature of the current study, this hypothesis needs to be tested with future longitudinal datasets.
Our results indicated that higher fear levels of COVID-19 were associated with higher risk perceptions. Though the association has not been explored extensively in past epidemics, our finding was consistent with a previous study which investigated this association during the Ebola outbreak (Yang and Chu, 2018). Various theories in the existing literature have consistently pointed to the strong influence of emotions on risk assessment and decision-making. According to the appraisal-tendency framework, emotions influence one’s judgment and decision-making due to the different appraisals and cognitive responses accompanying emotions (Lerner and Keltner, 2000). Similarly, the risk-as-feelings hypothesis highlights the dominance of emotions in decision-making (Loewenstein et al., 2001). Both emotional reactions and cognitive assessments determine risk assessment; however, when conflict between the two arises, emotional reactions often override cognitive assessments and drive the eventual risk assessment and decision-making (Loewenstein et al., 2001). Based on the aforementioned theories, fearful individuals would perceive the COVID-19 pandemic as a high-risk event due to appraisals of lack of individual control, uncertainty, and unpleasantness (Smith and Ellsworth, 1985; Lazarus, 1991). In addition, the intense, immediate response and high mental imagery of fear (Loewenstein et al., 2001) would outweigh the cognitive evaluation of the actual threat posed by COVID-19. This suggests that fearful individuals are more likely to make inflated risk perceptions which are unrepresentative of actual risk levels.
As can be seen from our findings, older age was associated with greater fear of COVID-19. This could be attributed to the increased vulnerability to COVID-19 among the oldest-old. Clinical evidence thus far suggests that both COVID-19 mortality and fatality rates are associated with old age (Leung, 2020; Verity et al., 2020; Wang et al., 2020), with risks being especially high for the oldest-old. For example, studies in China and Italy reported that the case-fatality rate (CFR) of those 80 years and above was the highest at 14.8–20.2% (Novel Coronavirus Pneumonia Emergency Response Epidemiology, 2020; Onder et al., 2020). This was significantly higher than the CFR reported at 3.5–3.6% for older adults aged 60–69 years, and 8.0–12.8% for those aged 70 to 79 years (Novel Coronavirus Pneumonia Emergency Response Epidemiology, 2020; Onder et al., 2020). Considering the higher health risks posed to the oldest-old, it is not surprising to find that higher fear levels were found in this subgroup of older adults.
The findings have several implications. First, they highlighted the characteristics of individuals who are more likely to react fearfully toward COVID-19, such as those with more severe affective symptoms (anxiety and depressive) and inflated risk perception, as well as those who are older. It is imperative that intervention programs take these factors into account, to help individuals alleviate and manage their fears.
Second, the present study highlights the concerns surrounding heightened risk perception of COVID-19. While existing research has demonstrated risk perception as an important tool in promoting protective and preventive behaviors during pandemics (e.g., hand-washing, wearing a surgical mask, and social distancing), incorrect and exaggerated perceptions of risk may potentially hinder the adoption of such behaviors (Dryhurst et al., 2020). Furthermore, heighted risk perceptions may lead to other serious and undesirable outcomes such as hoarding of essential health (e.g., medications) and protective supplies (e.g., personal protective equipment), resulting in a shortage of such supplies (Abrams and Greenhawt, 2020). Steps should be taken to ensure that risk perceptions are accurate and proportionate to the actual risk levels involved in COVID-19. Some appropriate risk communication methods include maintaining various platforms for active engagement between the public and healthcare professionals, and addressing common misunderstandings and misinformation through various means like public education, health hotlines, healthcare workers, and the community (World Health Organization, 2020a). Appropriate guidance is needed to prevent inflated risk perceptions of COVID-19 among individuals.
Third, our findings point to the need to address and alleviate the negative mental health consequences associated with fear of COVID-19. The affective symptoms of anxiety and depression should not be overlooked; if prolonged, these mental health consequences may result in longer-term problems than the pandemic itself (Ornell et al., 2020). In the current climate where offline, face-to-face contact is discouraged, it is important to consider other psychological interventions that allow individuals to continue to meet their mental health needs. Strategies include provision of online counseling services, health education programs (Liu et al., 2020), and telemental health services (Zhou et al., 2020).
The present study has a few limitations. First, due to the cross-sectional design of our study, we are unable to make inferences on the directionality of the relationships between studied variables. Second, as data were collected through self-reports, it may be possible that the data may be influenced by social desirability bias. Third, the lockdown conditions enforced during the circuit breaker may be unique to Singapore and may not be generalizable or comparable to those in other countries. While a complete lockdown was implemented in other countries, where individuals were not allowed to head out entirely, a partial lockdown was enforced in Singapore. Individuals could still head out for essential activities.
In conclusion, our results show that fear of COVID-19 was positively associated with the affective symptoms of anxiety and depression, risk perception, and old age. Care needs to be given to these factors when designing intervention programs aimed to manage fears of COVID-19 among individuals. The results also highlight the importance of addressing incorrect risk perceptions of COVID-19, and the continual need to provide psychological interventions to individuals at risk of adverse mental health consequences.
The datasets generated for this study are not readily available because the conditions of our ethics approval do not permit public archiving of the data supporting this study. Interested researchers seeking access to the anonymized data should contact the corresponding authors and complete a formal data sharing agreement. Access will be granted in accordance with ethical procedures governing the reuse of data. Requests to access the datasets should be directed to MH, cGNtaGZ5bUBudXMuZWR1LnNn or JY, cGNteWpAbnVzLmVkdS5zZw==.
The studies involving human participants were reviewed and approved by National University of Singapore Institutional Review Board. The patients/participants provided their verbal or written informed consent to participate in this study.
MH, RM, and JY were involved in the study design and data collection. MH conducted all data analyses and drafted the manuscript. RM and JY provided input for the manuscript. JY took on a supervisory role in data analyses. All authors contributed to the article and approved the submitted version.
This work was supported by Research Donations from Kwan Im Thong Hood Cho Temple, Lee Kim Tah Holdings Pte Ltd., and The Hongkong and Shanghai Banking Corporation, under the Mind Science Centre, Department of Psychological Medicine, National University of Singapore.
The authors declare that this study received funding from Research Donations from Kwan Im Thong Hood Cho Temple, Lee Kim Tah Holdings Pte Ltd., and the Hongkong and Shanghai Banking Corporation. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
The authors would like to thank Ms. Savannah Siew, Ms. Lim Xin Ying, Ms. Yap Ai Che, Ms. Ng Siew Yee, and Ms. Adena Peh for their help and dedication to the study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.638831/full#supplementary-material
Abrams, E. M., and Greenhawt, M. (2020). Risk communication during COVID-19. J. Allergy Clin. Immunol. Pract. 8, 1791–1794. doi: 10.1016/j.jaip.2020.04.012
Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., and Pakpour, A. H. (2020a). The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict. 1–9.
Ahorsu, D. K., Lin, C.-Y., and Pakpour, A. H. (2020b). The association between health status and insomnia, mental health, and preventive behaviors: the mediating role of fear of COVID-19. Gerontol. Geriatr. Med. 6:2333721420966081. doi: 10.1177/2333721420966081
American Psychological Association (2021). Anxiety. Washington, DC: American Psychological Association.
Amin, J. M., and Lovibond, P. F. (1997). Dissociations between covariation bias and expectancy bias for fear-relevant stimuli. Cogn. Emot. 11, 273–289. doi: 10.1080/026999397379926
Ang, H. M., and Phua, R. (2020). COVID-19: Compulsory to Wear Mask When Leaving the House, Says Lawrence Wong. Singapore: CNA.
Arafat, S. Y., Kar, S. K., Marthoenis, M., Sharma, P., Apu, E. H., and Kabir, R. (2020). Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. 289:113061. doi: 10.1016/j.psychres.2020.113061
Baker, J. A. (2020). Singapore’s Circuit Breaker and Beyond: Timeline of the COVID-19 Reality. Singapore: Channel News Asia.
Bakioğlu, F., Korkmaz, O., and Ercan, H. (2020). Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00331-y
Blakey, S. M., Reuman, L., Jacoby, R. J., and Abramowitz, J. S. (2015). Tracing “Fearbola”: psychological predictors of anxious responding to the threat of ebola. Cogn. Ther. Res. 39, 816–825. doi: 10.1007/s10608-015-9701-9
Byrne, G. J., and Pachana, N. A. (2011). Development and validation of a short form of the geriatric anxiety inventory-the GAI-SF. Int. Psychogeriatr. 23, 125–131. doi: 10.1017/S1041610210001237
de Jong, P. J., Merckelbach, H., Bögels, S., and Kindt, M. (1998). Illusory correlation and social anxiety. Behav. Res. Ther. 36, 1063–1073. doi: 10.1016/S0005-7967(98)00099-0
De Zwart, O., Veldhuijzen, I. K., Elam, G., Aro, A. R., Abraham, T., Bishop, G. D., et al. (2007). Avian influenza risk perception, Europe and Asia. Emerg. Infect. Dis. 13, 290–293. doi: 10.3201/eid1302.060303
Devakumar, D., Shannon, G., Bhopal, S. S., and Abubakar, I. (2020). Racism and discrimination in COVID-19 responses. Lancet 395:1194. doi: 10.1016/S0140-6736(20)30792-3
Douglas, M., and Wildavsky, A. (1983). Risk and Culture: An Essay on the Selection of Technological and Environmental Dangers. California, MA: University of California Press.
Dryhurst, S., Schneider, C. R., Kerr, J., Freeman, A. L., Recchia, G., Van Der Bles, A. M., et al. (2020). Risk perceptions of COVID-19 around the world. J. Risk Res. 23, 994–1006. doi: 10.1080/13669877.2020.1758193
Dsouza, D. D., Quadros, S., Hyderabadwala, Z. J., and Mamun, M. A. (2020). Aggregated COVID-19 suicide incidences in India: fear of COVID-19 infection is the prominent causative factor. Psychiatry Res. 290:113145. doi: 10.1016/j.psychres.2020.113145
Garcia, R. (2017). Neurobiology of fear and specific phobias. Learn. Mem. 24, 462–471. doi: 10.1101/lm.044115.116
Goh, T. (2020). Six Months of Covid-19 in Singapore: A Timeline. Available: https://www.straitstimes.com/singapore/six-months-of-covid-19-in-singapore-a-timeline (accessed August 28, 2020).
gov.sg. (2020a). Circuit Breaker Extension and Tighter Measures: What You Need to Know. Available: https://www.gov.sg/article/circuit-breaker-extension-and-tighter-measures-what-you-need-to-know (accessed August 2, 2020).
gov.sg. (2020b). Ending Circuit Breaker: Phased Approach to Resuming Activities Safely [Online]. Singapore. Available: https://www.gov.sg/article/ending-circuit-breaker-phased-approach-to-resuming-activities-safely (accessed August 6, 2020).
gov.sg. (2020c). Financial Support to Help Singaporeans Affected by COVID-19 [Online]. Available: https://www.gov.sg/article/financial-support-to-help-singaporeans-affected-by-covid-19 (accessed August 5, 2020).
Hair, J. F., Black, W. C., Babin, B. J., and Anderson, R. E. (2010). Multivariate Data Analysis: International Version. New Jersey: Pearson.
Harper, C. A., Satchell, L. P., Fido, D., and Latzman, R. D. (2020). Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00281-5
Ho, C. S., Chee, C. Y., and Ho, R. C. (2020). Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singapore 49, 1–3.
Hu, L. T., and Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 6, 1–55. doi: 10.1080/10705519909540118
Johnco, C., Knight, A., Tadic, D., and Wuthrich, V. M. (2015). Psychometric properties of the Geriatric Anxiety Inventory (GAI) and its short-form (GAI-SF) in a clinical and non-clinical sample of older adults. Int. Psychogeriatr. 27, 1089–1097. doi: 10.1017/S1041610214001586
Kennedy, S. J., Rapee, R. M., and Mazurski, E. J. (1997). Covariation bias for phylogenetic versus ontogenetic fear-relevant stimuli. Behav. Res. Ther. 35, 415–422. doi: 10.1016/s0005-7967(96)00128-3
Khalik, S. (2020). Singapore Raises Coronavirus Outbreak Alert to Orange: What Does it Mean?. Singapore: The Straits Times.
Lee, K., Jeong, G.-C., and Yim, J. (2020). Consideration of the psychological and mental health of the elderly during COVID-19: a theoretical review. Int. J. Environ. Res. Public Health 17:8098. doi: 10.3390/ijerph17218098
Lee, R. Z. Y., Yu, J., Rawtaer, I., Allen, P. F., Bao, Z., Feng, L., et al. (2020). CHI study: protocol for an observational cohort study on ageing and mental health in community-dwelling older adults. BMJ Open 10:e035003. doi: 10.1136/bmjopen-2019-035003
Lerner, J. S., Gonzalez, R. M., Small, D. A., and Fischhoff, B. (2003). Effects of fear and anger on perceived risks of terrorism: a national field experiment. Psychol. Sci. 14, 144–150. doi: 10.1111/1467-9280.01433
Lerner, J. S., and Keltner, D. (2000). Beyond valence: toward a model of emotion-specific influences on judgement and choice. Cogn. Emot. 14, 473–493. doi: 10.1080/026999300402763
Leung, C. (2020). Risk factors for predicting mortality in elderly patients with COVID-19: a review of clinical data in China. Mech. Age. Dev. 2020:111255. doi: 10.1016/j.mad.2020.111255
Liu, S., Yang, L., Zhang, C., Xiang, Y.-T., Liu, Z., Hu, S., et al. (2020). Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry 7, e17–e18. doi: 10.1016/S2215-0366(20)30077-8
Loewenstein, G. F., Weber, E. U., Hsee, C. K., and Welch, N. (2001). Risk as feelings. Psychol. Bull. 127, 267–286. doi: 10.1037/0033-2909.127.2.267
Mamun, M. A., and Griffiths, M. D. (2020). First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J. Psychiatr. 51:102073. doi: 10.1016/j.ajp.2020.102073
Ministry of Health (2020). Circuit Breaker to Minimize Further Spread of COVID-19. Available: https://www.moh.gov.sg/news-highlights/details/circuit-breaker-to-minimise-further-spread-of-covid-19 (accessed August 2, 2020).
Moshagen, M., and Erdfelder, E. (2016). A new strategy for testing structural equation models. Struct. Equ. Model. 23, 54–60. doi: 10.1080/10705511.2014.950896
Novel Coronavirus Pneumonia Emergency Response Epidemiology (2020). The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China [in Chinese]. Zhonghua Liu Xing Bing Xue Za Zhi 41, 145–151. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003
Nyunt, M. S. Z., Fones, C., Niti, M., and Ng, T.-P. (2009). Criterion-based validity and reliability of the Geriatric Depression Screening Scale (GDS-15) in a large validation sample of community-living Asian older adults. Aging Ment. Health 13, 376–382. doi: 10.1080/13607860902861027
Olatunji, B. O., Lohr, J. M., Willems, J. L., and Sawchuk, C. N. (2006). Expectancy bias for disgust and emotional responding in contamination-related obsessive-compulsive disorder. Anxiety Stress Coping 19, 383–396. doi: 10.1080/10615800601055964
Onder, G., Rezza, G., and Brusaferro, S. (2020). Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 323, 1775–1776. doi: 10.1001/jama.2020.4683
Ornell, F., Schuch, J. B., Sordi, A. O., and Kessler, F. H. P. (2020). “Pandemic fear” and COVID-19: mental health burden and strategies. Braz. J. Psychiatry 42, 232–235. doi: 10.1590/1516-4446-2020-0008
Paek, H.-J., and Hove, T. (2017). “Risk perceptions and risk characteristics,” in Oxford Research Encyclopedia of Communication (Oxford: Oxford University press).
Pakpour, A., and Griffiths, M. (2020). The fear of COVID-19 and its role in preventive behaviors. J. Concurr. Disord. 2, 58–63.
Rajkumar, R. P. (2020). COVID-19 and mental health: a review of the existing literature. Asian J. Psychiatr. 52:102066. doi: 10.1016/j.ajp.2020.102066
Rosseel, Y. (2012). Lavaan: an R package for structural equation modeling and more. Version 0.5-12 (BETA). J. Stat. Softw. 48, 1–36. doi: 10.18637/jss.v048.i02
Satici, B., Gocet-Tekin, E., Deniz, M. E., and Satici, S. A. (2020). Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 1–9. doi: 10.1007/s11469-020-00294-0
Schimmenti, A., Billieux, J., and Starcevic, V. (2020). The four horsemen of fear: an integrated model of understanding fear experiences during the COVID-19 pandemic. Clin. Neuropsychiatry 17, 41–45. doi: 10.36131/CN20200202
Sher, L. (2020). The impact of the COVID-19 pandemic on suicide rates. QJM 113, 707–712. doi: 10.1093/qjmed/hcaa202
Smith, C. A., and Ellsworth, P. C. (1985). Patterns of cognitive appraisal in emotion. J. Pers. Soc. Psychol. 48, 813–838. doi: 10.1037/0022-3514.48.4.813
The Straits Times (2020). Coronavirus: Safe Distancing Rules Kick in, Failure to Sit or Queue 1m Apart from Others Could Land You a Fine or Jail Term. Available: https://www.straitstimes.com/singapore/coronavirus-safe-distancing-rules-kick-in-failure-to-sit-or-queue-1m-apart-from-others (accessed August 5, 2020).
Tomarken, A. J., Mineka, S., and Cook, M. (1989). Fear-relevant selective associations and covariation bias. J. Abnorm. Psychol. 98:381. doi: 10.1037/0021-843X.98.4.381
Van der Linden, S. (2015). The social-psychological determinants of climate change risk perceptions: towards a comprehensive model. J. Environ. Psychol. 41, 112–124. doi: 10.1016/j.jenvp.2014.11.012
Verity, R., Okell, L. C., Dorigatti, I., Winskill, P., Whittaker, C., Imai, N., et al. (2020). Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect. Dis. 20, 669–677. doi: 10.1016/S1473-3099(20)30243-7
Wancata, J., Alexandrowicz, R., Marquart, B., Weiss, M., and Friedrich, F. (2006). The criterion validity of the geriatric depression scale: a systematic review. Acta Psychiatr. Scand. 114, 398–410. doi: 10.1111/j.1600-0447.2006.00888.x
Wang, D., Hu, B., Hu, C., Zhu, F., Liu, X., Zhang, J., et al. (2020). Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069. doi: 10.1001/jama.2020.1585
Wheaton, M. G., Abramowitz, J. S., Berman, N. C., Fabricant, L. E., and Olatunji, B. O. (2012). Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit. Ther. Res. 36, 210–218. doi: 10.1007/s10608-011-9353-3
World Health Organization (2020a). Risk Communication and Community Engagement Readiness and Response to Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020. Geneva: World Health Organization.
World Health Organization (2020b). WHO Announces COVID-19 Outbreak a Pandemic [Online]. Available: https://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic (accessed July 19, 2020).
Yang, J. Z., and Chu, H. (2018). Who is afraid of the Ebola outbreak? The influence of discrete emotions on risk perception. J. Risk Res. 21, 834–853. doi: 10.1080/13669877.2016.1247378
Yesavage, J. A., and Sheikh, J. I. (1986). 9/Geriatric depression scale (GDS) recent evidence and development of a shorter version. Clin. Gerontol. 5, 165–173.
Keywords: COVID-19, fear, depression, anxiety, risk perception, older adults
Citation: Han MFY, Mahendran R and Yu J (2021) Associations Between Fear of COVID-19, Affective Symptoms and Risk Perception Among Community-Dwelling Older Adults During a COVID-19 Lockdown. Front. Psychol. 12:638831. doi: 10.3389/fpsyg.2021.638831
Received: 07 December 2020; Accepted: 04 March 2021;
Published: 23 March 2021.
Edited by:
Anders Hakansson, Lund University, SwedenReviewed by:
Amir H. Pakpour, Qazvin University of Medical Sciences, IranCopyright © 2021 Han, Mahendran and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Madeline F. Y. Han, cGNtaGZ5bUBudXMuZWR1LnNn; Junhong Yu, cGNteWpAbnVzLmVkdS5zZw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.