
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 05 May 2021
Sec. Movement Science
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.625354
This article is part of the Research TopicFutsal research and challenges for sport developmentView all 23 articles
 Marcos Roberto Queiroga1*
Marcos Roberto Queiroga1* Danilo Fernandes da Silva2
Danilo Fernandes da Silva2 Sandra Aires Ferreira1
Sandra Aires Ferreira1 Vinícius Müller Reis Weber3
Vinícius Müller Reis Weber3 Daniel Zanardini Fernandes3
Daniel Zanardini Fernandes3 Timothy Gustavo Cavazzotto1
Timothy Gustavo Cavazzotto1 Bruno Sergio Portela1
Bruno Sergio Portela1 Marcus Peikriszwili Tartaruga1
Marcus Peikriszwili Tartaruga1 Matheus Amarante Nascimento4
Matheus Amarante Nascimento4 Edgar Ramos Vieira5
Edgar Ramos Vieira5We aimed to characterize the age of onset of training, age at menarche, menstrual periodicity, and performance perception during the menstrual cycle and examined the impact of these reproductive variables on body composition, morphology, and body weight satisfaction in Brazilian elite futsal players. The study consisted of 115 female Brazilian elite futsal players from the top national teams. Data were collected during the twentieth Women’s Brazil Futsal Cup. Players were interviewed and self-reported their age of onset of training, age at menarche, menstrual periodicity, and the menstrual period, where they performed best. We also asked for what they considered to be their ideal body weight as well as information related to their training (i.e., volume and frequency). Subsequently, anthropometric measurements (i.e., body mass, height, circumferences, diameters, and skinfold thickness) were performed to estimate the body composition and determine morphological characteristics (e.g., somatotype). Fifty-nine (53.2%) players were postmenarche-trained and 52 (46.8%) were premenarche-trained. Eighteen (16.2%), 65 (58.6%), and 28 (25.2%) were classified as early, normal, and late menarche, respectively. Only 11 (9.6%) and 1 (0.9%) had irregular menstrual cycles and were amenorrheic, respectively. Seventy-three (69.5%), 23 (21.9%), and 9 (8.6%) reported that their game performance was the best at the follicular phase, menses, and luteal phase of the menstrual cycle, respectively. No associations between the four reproductive-related variables were found. Postmenarche-trained players had significant lower age at menarche and higher percentage body fat. The somatotype profile registered lower ectomorphy rate for the postmenarche-trained participants after controlling for covariates. Early menarche group presented higher sum of six skinfold thickness and endomorphy rate compared to normal and late menarche groups. No differences were found when menstrual periodicity groups and best performance groups were compared, except for higher femur width in the regular menstrual cycle group compared to the irregular one. The association between body weight satisfaction and the four reproductive-related variables were not observed. Premenarche-trained Brazilian elite futsal players had the menarche later than the postmenarche-trained athletes. Most of the participants had menarche age classified as “normal,” presented “regular” menstrual cycles and perceived to perform better during the follicular phase of the menstrual cycle.
Exercise training can directly impact female reproductive health. Over 40 years of research have shown that female athletes are susceptible to oligomenorrhea and amenorrhea when compared to non-athletic populations (Dale et al., 1979; Frisch, 1980; Calthorpe et al., 2019). Moreover, a recent systematic review with meta-analysis revealed that age at menarche is 1.13 (95% CI: 0.80–1.47) years later in trained vs. non-trained girls (Calthorpe et al., 2019). It is worth mentioning that none of the included studies had team sport female athletes involved (Calthorpe et al., 2019).
Irregular menstrual cycle may pose as a risk for female reproductive health (Ackerman and Misra, 2018). However, later menarche can be protective against some chronic diseases when compared to having an early menarche. Epidemiological research has suggested that early age at menarche is associated with increased risk of cancer (Werneck et al., 2018a), higher blood pressure (Werneck et al., 2018b), gestational diabetes mellitus (Schoenaker and Mishra, 2017), and all-cause mortality (Tamakoshi et al., 2011). With regards to exercise performance, there is evidence that later menarche is associated with superior athletic performance (Stager et al., 1984), although the field of alterations related to the menstrual cycle and athletic performance has considerable controversial findings (e.g., no impact or some impact being previously reported; McNulty et al., 2020).
One factor that seems to influence later menarche is the onset of exercise training. Menstrual disturbances have been reported to be relatively more common in athletes who began training before the menarche. The premenarche-trained athletes reported a higher incidence of menstrual cycle irregularities than the athletes who began training after the menarche (Toriola, 1988). Frisch (1980) found that each year of training before menarche has accounted for 5 months of delay in the menarche in college athletes. Furthermore, premenarche-trained athletes presented high rates of irregular menstrual cycle (61%) and amenorrhea (22%; Frisch, 1980).
Menstrual dysfunctions can be caused by low energy availability or energy deficiency (Mountjoy et al., 2014; Ackerman and Misra, 2018). Low energy availability is linked with a disbalance between energy intake and energy expenditure, which can ultimately lead to lower body fat content (Loucks, 2004). Thus, low body fat, as a result of a disbalanced energy storage, can lead to changes in the menstrual cycle (Mountjoy et al., 2014) and may be a common characteristic of women with menstrual dysfunctions (Carlberg et al., 1983). Psychological aspects, such as eating disorder behaviors, can also influence female reproductive health by altering body weight and body fat content. Rates of eating disorders and body image alterations are 13.3 and 24.4% in female team sport athletes including futsal players (Kravchychyn et al., 2013).
The association between physical training and reproductive health issues, particularly in elite athletes, is a big concern of the sport and exercise scientific community. With regards to elite futsal players, to the best of our knowledge, the rates of menstrual dysfunctions have yet to be described. In fact, there is a lack of reproductive health-related information available in the team sport literature (Findlay et al., 2020). One potential explanation for a reduced focus on team sports is that research tends to focus on sports, which encourage leanness (Bruinvels et al., 2017), assuming that lower body fat and an ectomorphic somatotype would be potentially linked with higher rates of menstrual dysfunction (Mountjoy et al., 2014). To further explore this assumption, the present study aimed to characterize the age of onset of training, age at menarche, menstrual periodicity, and performance perception during the menstrual cycle and examined the impact of these reproductive variables on body composition, morphology, and body weight satisfaction in Brazilian elite futsal players. We hypothesized that premenarche-trained, late menarche, and athletes with irregular menstrual cycles would have greater rates of menstrual dysfunction, lower body fat, higher ectomorphy morphological profile, and greater dissatisfaction with body weight. We also hypothesized the study outcomes would not differ between menstrual periods when participants perceive to perform best.
Study design is cross-sectional. One-hundred and fifteen female Brazilian elite futsal players from the top national teams were recruited for the present study. The recruitment process was conducted through the Brazilian Confederation of Futsal with the support of the coaches of the teams. Eligibility criteria were checked and validated by the leading research investigator. The inclusion criterion was being registered for the twentieth Women’s Brazil Futsal Cup. No exclusion criteria were applied. The sample comprehended the population of female Brazilian elite futsal players. Since 1992, this national competition is a yearly event organized by the Brazilian Futsal Confederation1 between the 10 top teams in the country. One represents the host city and the other nine are champions from other Brazilian states. The study was approved by the Local Ethics Board (Process n. 039/2011) and complies with the Resolution of the National Health Council of the Brazilian Ministry of Health and the Declaration of Helsinki on human research. All players were fully informed about the purpose of the study and signed the consent form before any procedure took place.
All measurements were conducted by the leading research investigator. The twentieth Women’s Brazil Futsal Cup format allowed each team to take 1 day off. In this way, data collection was performed in a room, in the same place, where the games were played and coincided with this day off of the teams, which allowed a minimum interval of 15 h between the last game and the evaluation. Thus, all the assessments were performed in a single day. Before performing the anthropometrical measurements, participants were interviewed following a structure interview with close-ended question and self-reported four reproductive-related variables:
1. Age of onset of training (years). This was measured based on a close-ended question (what was your age, in years, of onset of training?). Depending on the age at menarche, athletes were classified as premenarche-trained and postmenarche-trained (Frisch, 1980);
2. Age at menarche (years). This was measured based on a close-ended question (what was your age, in years, at menarche?). This variable was classified as early menarche (<12 years), normal menarche (12–14 years), and late menarche (>14 years; Day et al., 2015);
3. Menstrual periodicity. This was measured based on a close-ended question (for the most part of your reproductive years, what is your menstrual cycle periodicity? Options: 10–13 cycles/year; 3–9 cycles/year; and 0–2 cycles/year). Regular menstrual cycles were considered between 10 and 13 cycles/year, irregular menstrual cycles between 3 and 9 cycles/year and amenorrheic 0–2 cycles/year (Frisch, 1980);
4. Menstrual period when they performance best. This variable was obtained based on a close-ended question (based on your perception, which menstrual period do you perform the best? Options: Menses; Luteal Phase; and Follicular Phase). Based on their own perception, they answered one of the three options.
Besides that, they were also asked:
5. Ideal body weight (kg) and body weight satisfaction (classified as “Satisfied,” “No, increase,” and “No, decrease”). Ideal body weight was asked as a close-ended question (what is your ideal body weight in kg?). Body weight satisfaction was also a close-ended question (are you satisfied with your body weight? Options: Yes; No, increase; and No, decrease).
6. Information related to their training (i.e., volume and frequency). These data were also obtained with a close-ended question (what is your training volume? and what is your training frequency?). They were asked to report training volume in hours/week, minutes/week, or hours:minutes/week. We converted all answers in minutes/week before moving to data analysis. Training frequency was reported in times/week.
Anthropometric variables were checked in duplicate in the right hemisphere of the body. If the difference was greater than 0.2 mm for skinfolds or 0.5 cm for other variables, a third measurement was performed. The final result used for data analysis was the average of two or three measurements. All anthropometric measurements were performed with athletes wearing no shoes and only light clothing, in accordance with standardized procedures (Marfell-Jones et al., 2006). They have been already described in more details elsewhere (Queiroga et al., 2019). Measurements were taken in a private room at approximately the same time of the day for all participants during a period of 5 days. Body mass was assessed by a 100-g precision anthropometric scale (Welmy™ São Paulo, Brazil) and height was measured by a 0.1-cm precision wall-mounted stadiometer. Body mass index (BMI) was calculated as body mass (kg)/height squared (m2). Biceps girth (mid-upper-arm) and calf girth (cm) were measured using a non-elastic tape to the nearest 0.1 cm (Mabis™ Curitiba, Brazil). The Biceps girth (cm) was obtained with the arm in a tensed position, while calf girth (cm) was measured in a seated position with legs on the ground. Biepicondylar humerus and femur width were measured to the nearest 0.1 cm with a metal caliper (Somet™ Curitiba, Brazil).
Skinfold thickness (SKFT) was measured at six sites (triceps, subscapular, supraspinal, suprailiac, midthigh, and medial calf) to the nearest 0.1 mm with a Cescorf caliper (Cescorf™ Porto Alegre, Brazil).
The sum of three skinfold thicknesses (3SKFT; triceps + suprailiac + midthigh) determined body density (Jackson et al., 1980). Body fat percentage (%BF) was subsequently estimated (Siri, 1961). Fat mass (FM) and lean body mass (LBM) were calculated in kg: FM = (%BF/100) × body mass; LBM = body mass − FM. The three somatotype components (i.e., endomorphy, mesomorphy, and ectomorphy) were determined according to the Heath and Carter Anthropometric Somatotyping Method (Carter and Health, 1990). All variables were measured in duplicate in the right side of the body. A third measure was taken if a difference greater than 0.2 mm for skinfold thickness or 0.5 cm difference for all the other variables was recorded. The final score used in the data analysis was the mean of the two scores or the median of three scores. The technical error of measurement of the leading research investigator who conducted all the measurements was between 2.9 and 3.5% for SKFT and between 0.1 and 1.8% for the other anthropometric measurements. The intra-class correlation for the measurements varied between 0.98 and 0.99 for SKFT and between 0.95 and 0.99 for the other measurements.
Data were descriptively analyzed using mean ± standard deviation (SD), frequencies, and percentages. The associations between the four reproductive-related variables and body weight satisfaction were tested with Chi-square test. When more than 20% of cells had expected count less than 5, the Likelihood Ratio correction was applied. Cramer’s V was calculated as an effect size measurement of the associations.
Body composition and morphological variables were compared according to the four reproductive-related variables with one-way ANCOVA adjusting for the time of experience in the sport, training volume, and frequency. Effect sizes for comparisons were computed using partial eta squared (η2). Bonferroni correction was applied when significant differences were captured in the adjusted one-way ANCOVA. Significance was set at p < 0.05 for all analyses.
One-hundred and fifteen female Brazilian elite futsal players (age: 22.0 ± 3.9 years; body weight: 58.6 ± 7.6 kg; height: 161.8 ± 6.5 cm; BMI: 22.3 ± 2.2 kg/m2; and body fat: 22.2 ± 5.0%) were evaluated; however, four did not report the age at menarche. The average of their age at menarche was 13.1 ± 1.8 years, the time of experience was 9.0 ± 4.3 years, the training volume was 171.9 ± 77.4 min/week, and the training frequency was 5.2 ± 1.8 times/week.
Fifty-nine (53.2%) players were postmenarche-trained and 52 (46.8%) were premenarche-trained. Eighteen (16.2%), 65 (58.6%), and 28 (25.2%) were classified as early, normal, and late menarche, respectively. Only 11 (9.6%) and 1 (0.9%) had irregular menstrual cycles and were amenorrheic, respectively. Seventy-three (69.5%), 23 (21.9%), and 9 (8.6%) reported that their game performance was the best at the follicular phase, menses, and luteal phase of the menstrual cycle, respectively. No associations between the four reproductive-related variables were found (Table 1).
After adjusting for the time of experience in the sport, training volume, and frequency, postmenarche-trained players had significant higher age and lower age at menarche than premenarche-trained players. They also presented higher body fat (kg). The somatotype profile registered lower ectomorphy rate for the postmenarche-trained participants (Table 2).
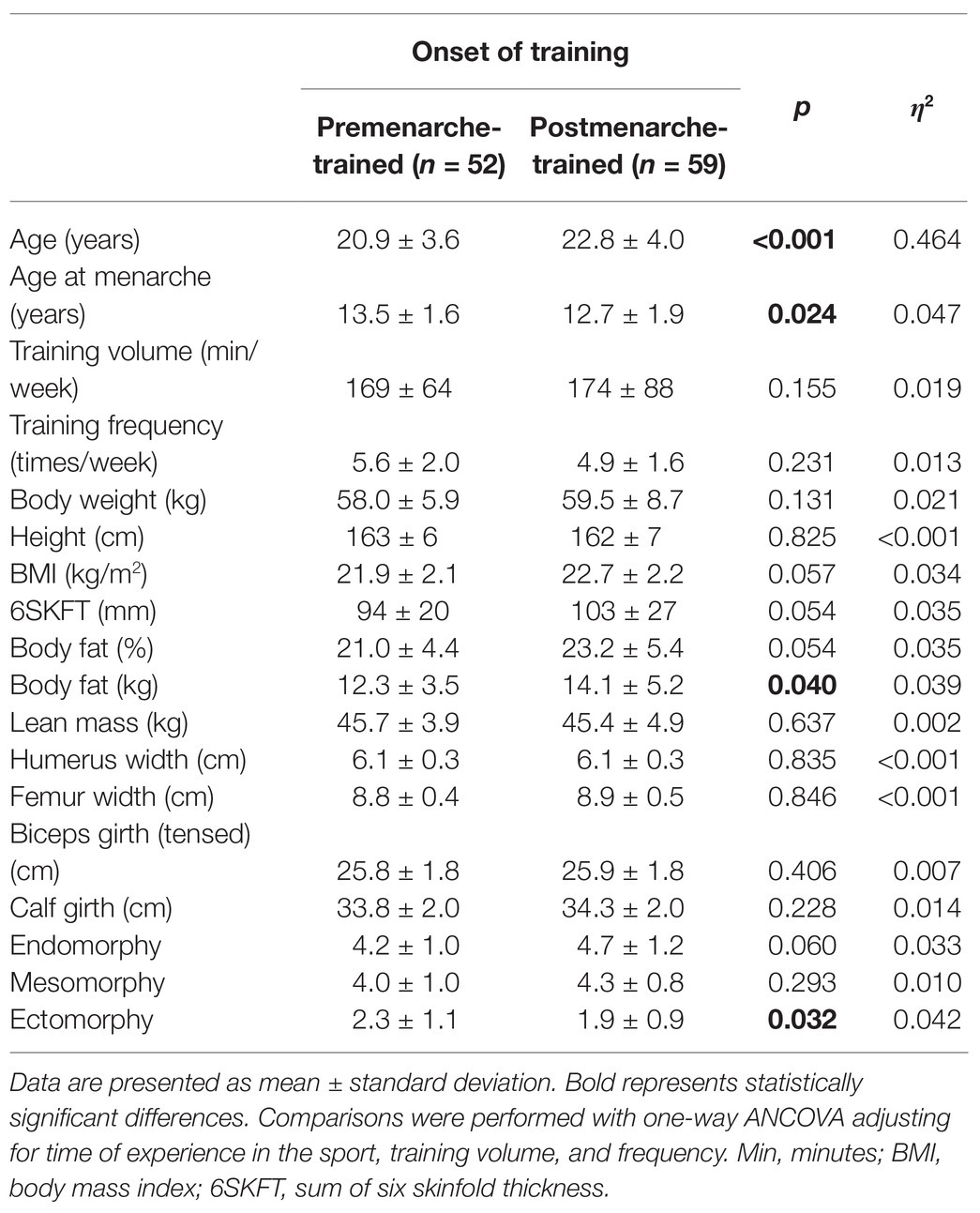
Table 2. Age, training, and anthropometric characteristics of premenarche-trained and postmenarche-trained female Brazilian elite futsal players.
When women with early, normal, and late menarche were compared, applying the same adjustments, we observed higher of sum of the six SKFT and endomorphy rate for the early menarche group compared to both normal and late menarche groups (Table 3). No significant results were evidenced in the comparison between women with regular vs. irregular menstrual cycle, except for higher femur width in the regular menstrual cycle group (Table 4). Women who perceived their performance to be the best at menses compared to follicular phase or luteal phase also did not differ for any anthropometric variable (Table 5).
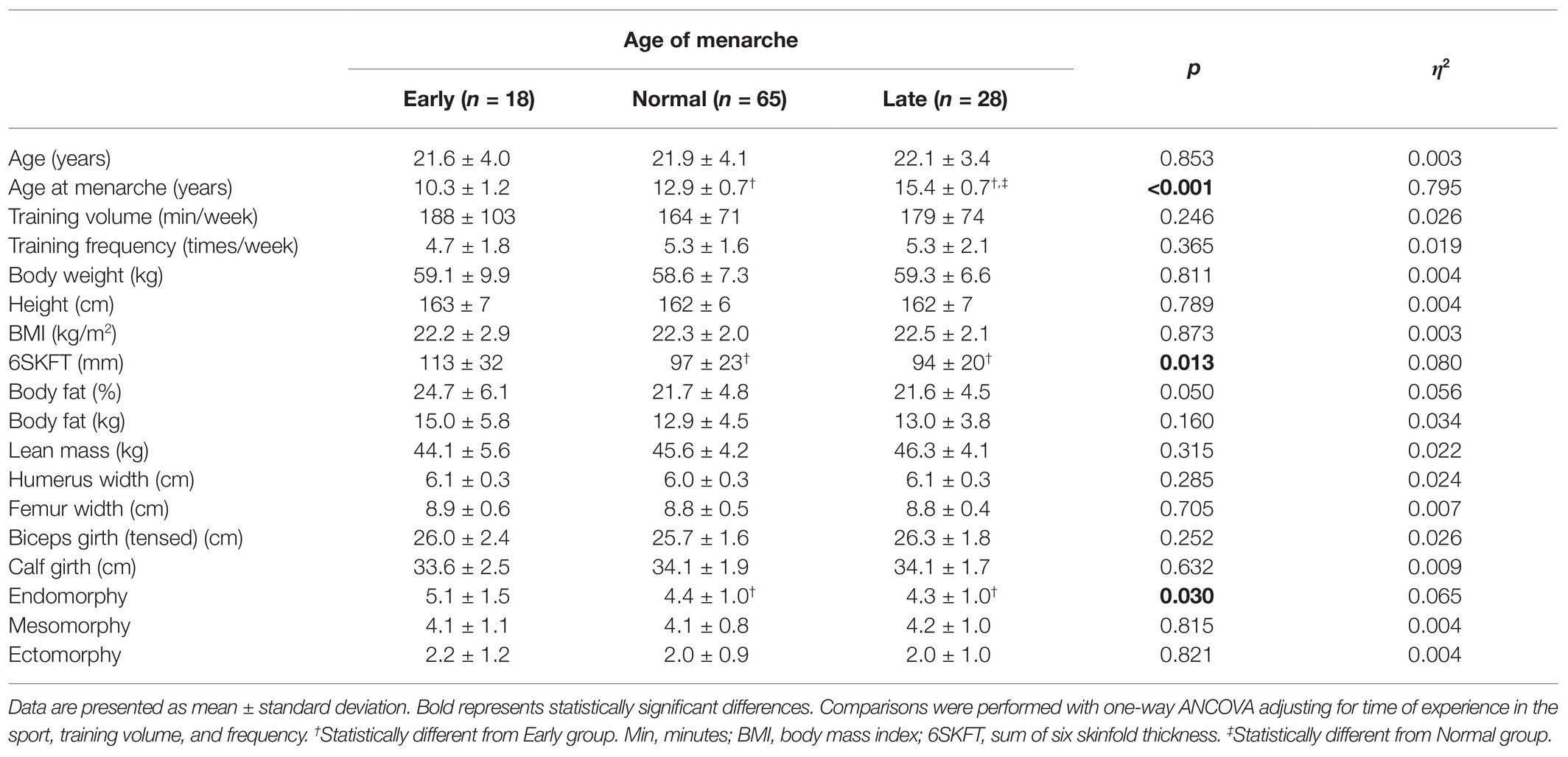
Table 3. Age, training, and anthropometric characteristics of female Brazilian elite futsal players classified as early, normal, and late menarche.
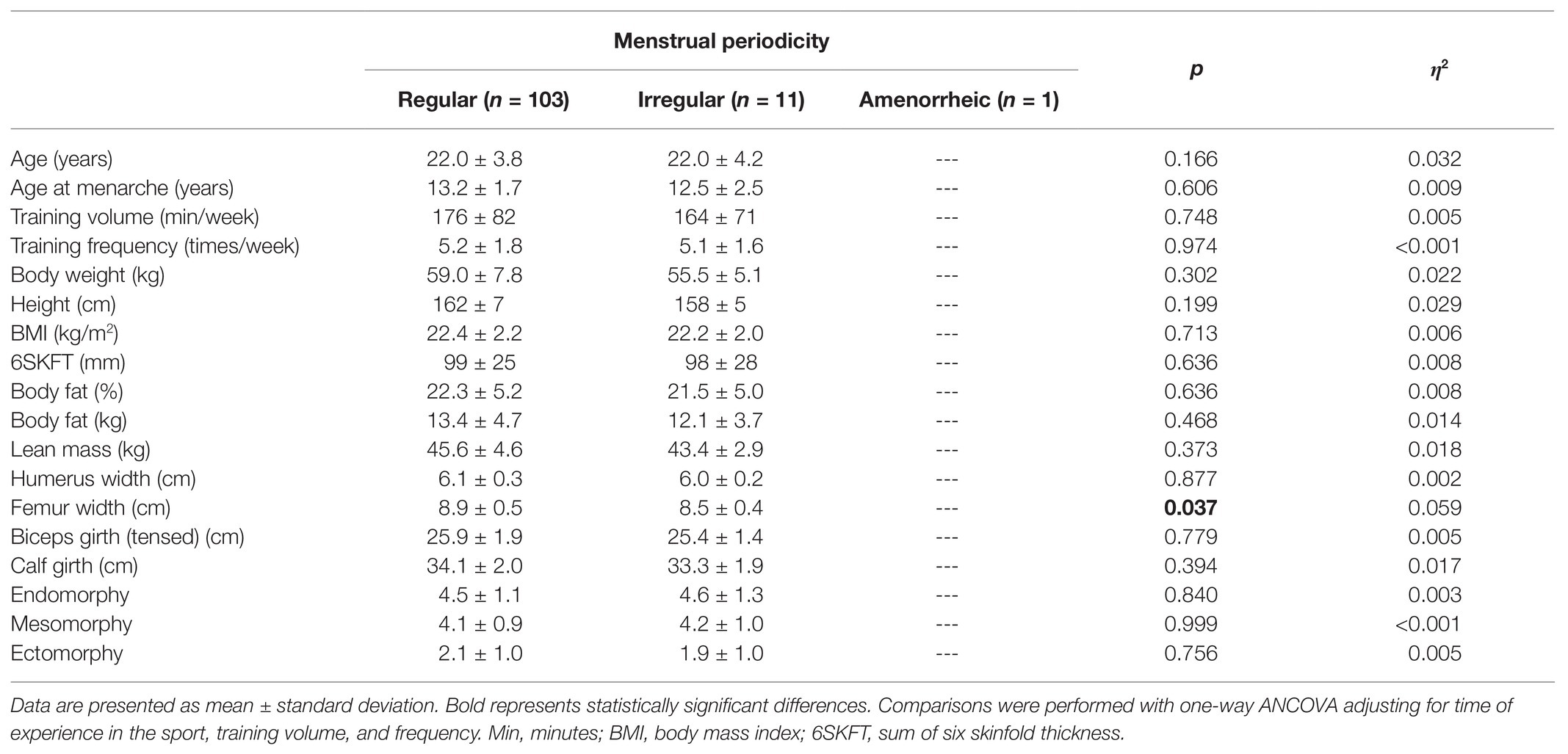
Table 4. Age, training, and anthropometric characteristics of female Brazilian elite futsal players classified as regular and irregular menstrual cycle.
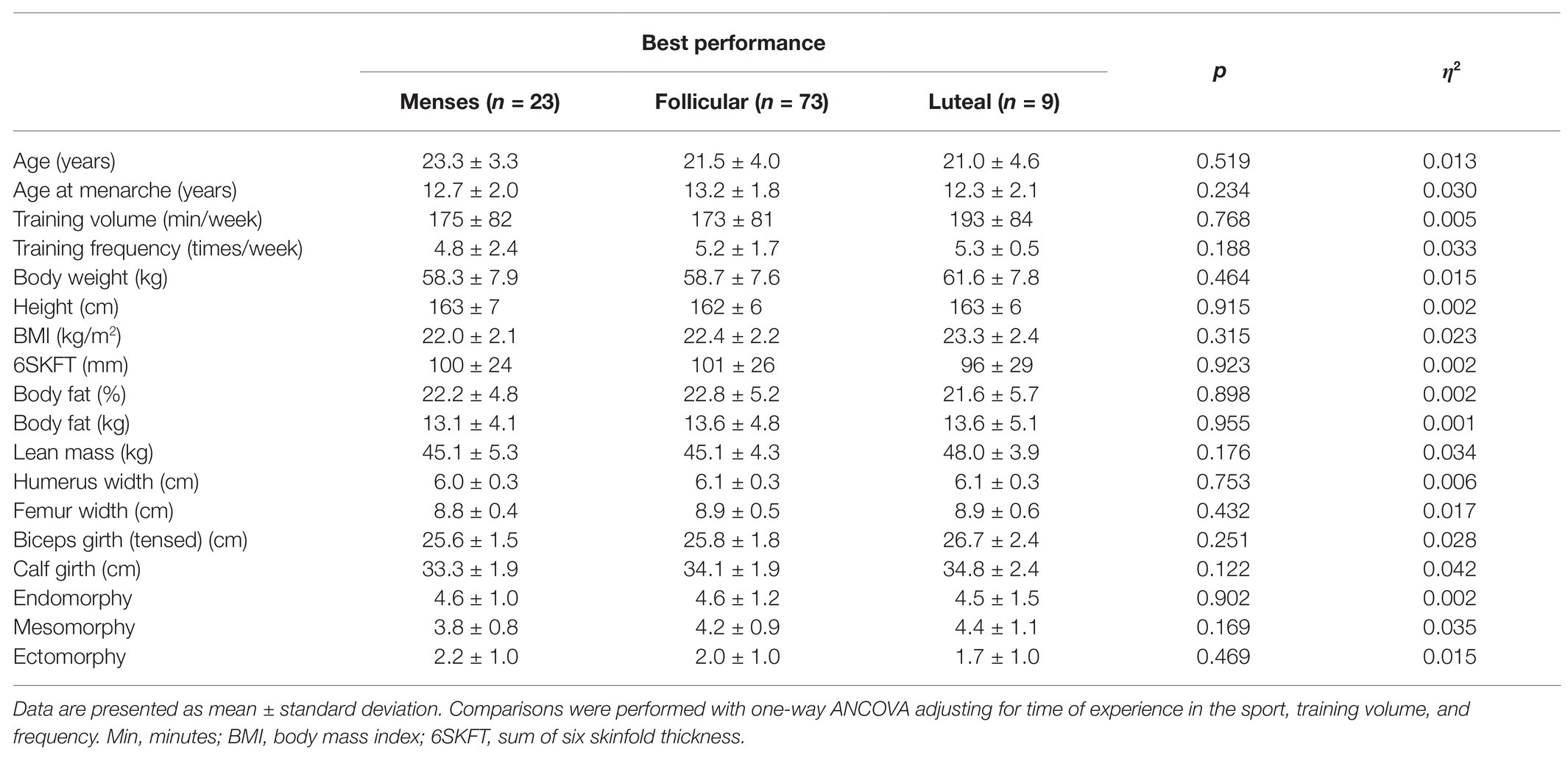
Table 5. Age, training, and anthropometric characteristics of female Brazilian elite futsal players according to the menstrual phase that they perceive to perform best.
After adjusting for time of experience in the sport, training volume, and frequency, the perception of ideal body weight and difference between ideal and real body weight were not different between categories of onset of training, age of menarche, menstrual periodicity, and menstrual period when athletes reported to perform best (Table 6).
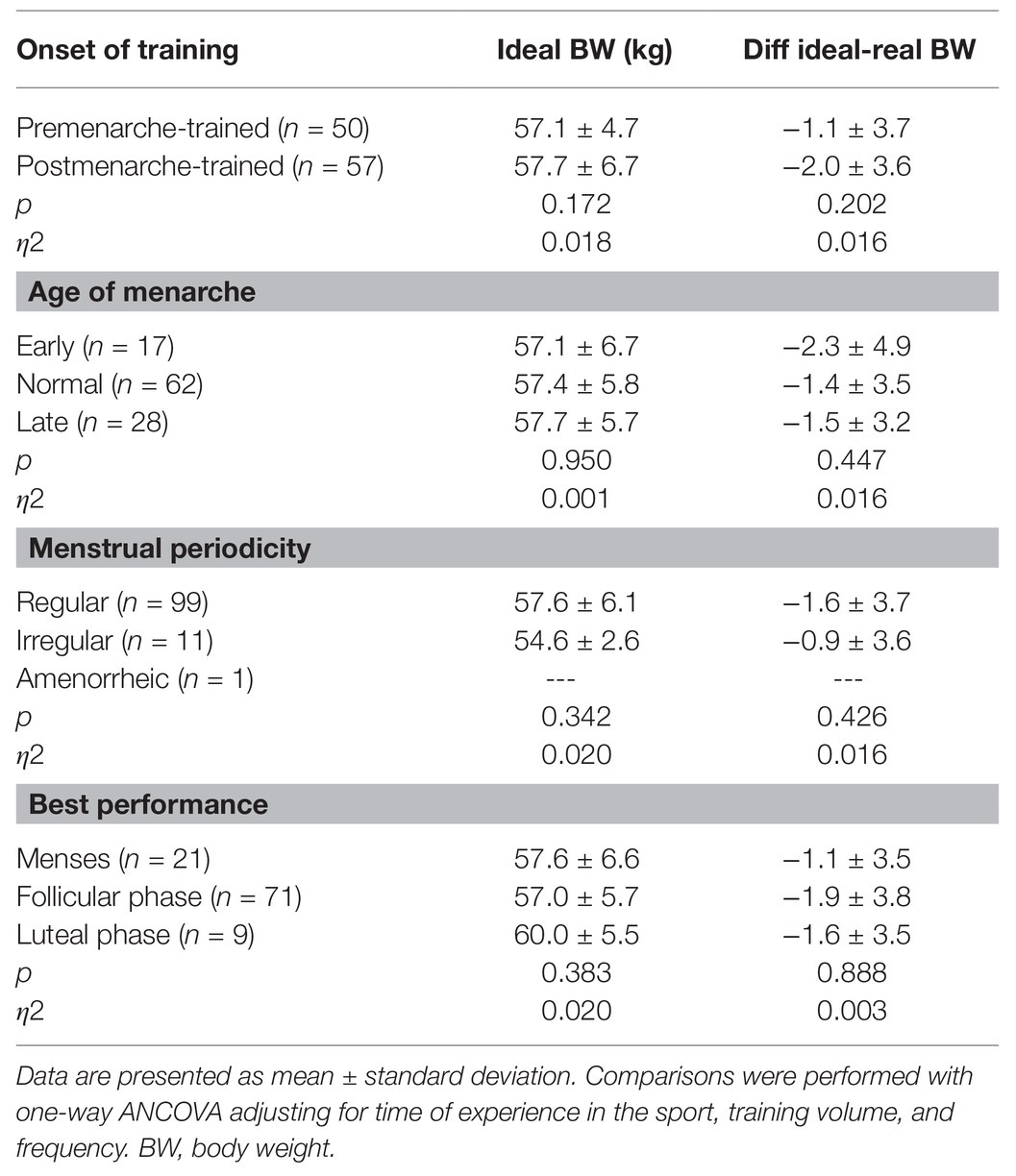
Table 6. Perception of ideal body weight and difference between ideal and real body weight according to categories of onset of training, age of menarche, menstrual periodicity, and menstrual period when athletes reported to perform best.
The association between body weight satisfaction and the four reproductive-related variables is represented in Figures 1A–D. No significant results were found.
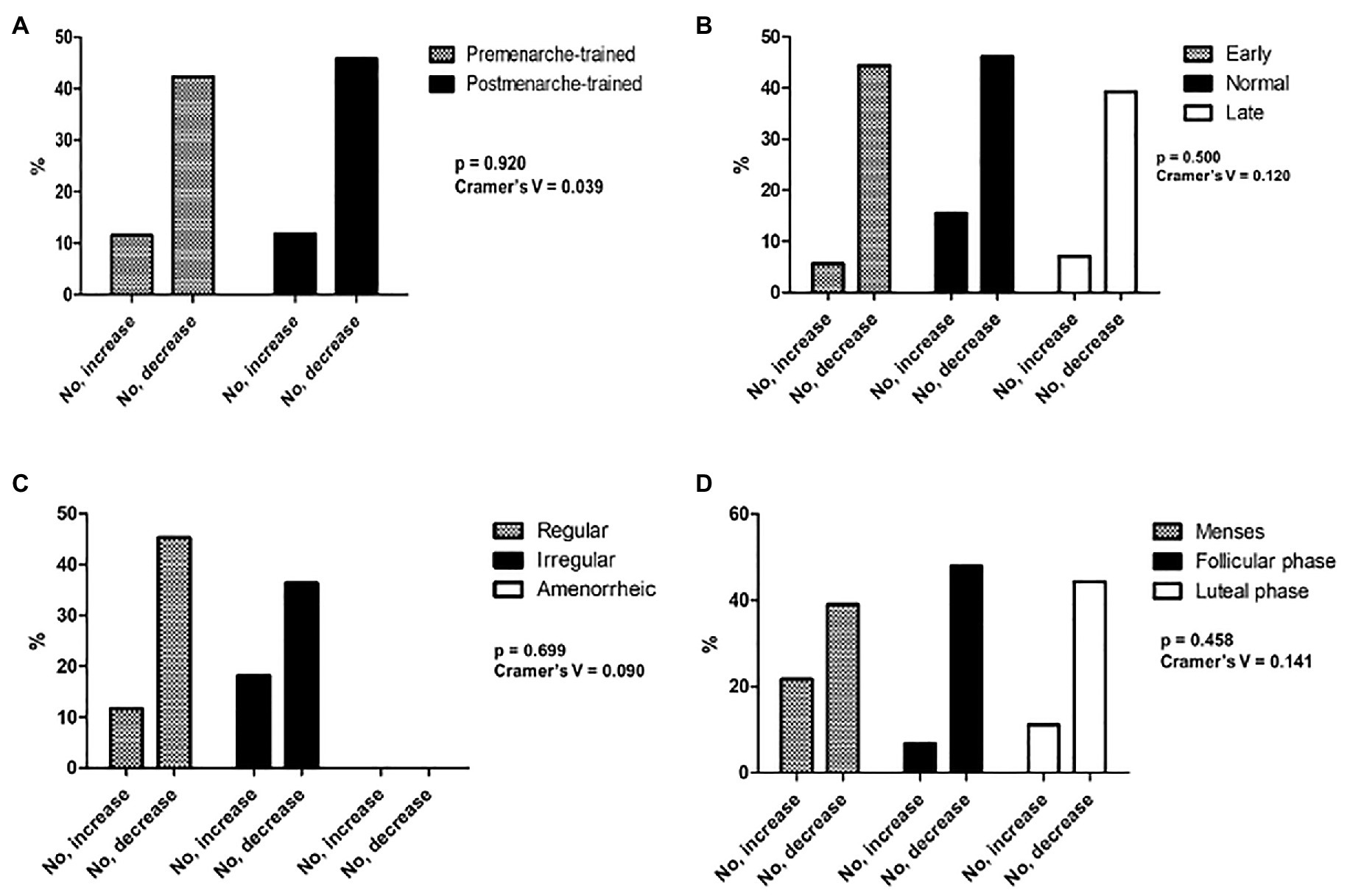
Figure 1. Association between body weight satisfaction and the four reproductive-related variables (A–D).
The purpose of this study was to characterize the age of onset of training, age at menarche, menstrual periodicity, and performance perception during the menstrual cycle and examined the impact of these reproductive variables on body composition, morphology, and body weight satisfaction in Brazilian elite futsal players.
The main findings of this research were that the number of female futsal players who engaged on the sport before menarche is balanced with the number of women who embarked on futsal training after the menarche. Those who engaged before the menarche had the menarche significantly later than those who started training after the menarche. Premenarche-trained players had lower body fat (kg) and greater ectomorphy profile after controlling for time of experience in the sport, training volume, and frequency. In addition, our descriptive analysis showed that most of the participants of the present study had their menarche age classified as “normal,” presented a “regular” menstrual cycle and perceived to perform better during the follicular phase of the menstrual cycle. Nonetheless, these factors did not associate with each other.
Intense training has been found to delay the onset of puberty in females by altering normal hormonal development (Theintz, 1994; Matina and Rogol, 2011; Malina et al., 2013). A systematic review with meta-analysis has shown that age at menarche is 1.13 (95% CI: 0.80–1.47) years later in trained vs. non-trained girls (Calthorpe et al., 2019). The age difference between premenarche-trained vs. postmenarche-trained in the present study is about 1.9 years.
Besides later menarche, female athletes are known to be more susceptible to oligomenorrhea and amenorrhea when compared to non-athletic populations (Dale et al., 1979; Frisch, 1980; Calthorpe et al., 2019). A relevant biological causal factor for the menstrual dysfunctions is low energy availability (Ackerman and Misra, 2018). Although we did not measure energy intake or energy balance, premenarche-trained futsal players had lower body fat (kg) than their postmenarche-trained counterparts. The ranges of body fat in our study are within the range from other studies with female futsal players of different performance levels (i.e., elite, sub-elite, and amateur; Barbero-Alvarez et al., 2015; Ramos-Campo et al., 2016; Beato et al., 2018; Palucci Vieira et al., 2020).
Also, our study demonstrated that women with early menarche presented higher sum of six SKFT and endomorphy rate compared to women whose menarche was classified as normal and late. The relationship between early age at menarche and higher adiposity is not completely elucidated; however, three factors have been suggested: (i) early menarche girls have longer exposure to a positive energy balance and (ii) endocrine factors, such as high levels of estrogen and GnRH, may accelerate pubertal development and increase subcutaneous body fat accumulation (Garn et al., 1986; Cole, 2003).
On the other hand, no differences in body fat were found in the comparison between groups related to menstrual periodicity (i.e., regular vs. irregular) and menstrual period when performance is perceived to be the best (i.e., menses, follicular, or luteal phases). Other anthropometric, body composition, and morphology variables did not differ between the four reproductive-related variables in Brazilian elite futsal players, except for femur width that was higher in the group with regular menstrual cycles compared to the irregular menstrual cycle group. Despite the significant results, this difference was only about 0.4 cm, which does not seem to be clinically important. Thus, our findings suggest that changes in reproductive variables are not related to relevant physical changes in this population. This agrees with Merzenich et al. (1993) who showed that exposure to exercise training may affect age at menarche through pathways that may go beyond adiposity.
Moreover, the percentage of women with normal age range menarche and regular menstrual cycle was much higher (58.6% for normal age range at menarche and 89.5% for regular menstrual cycle) in the present study compared to others. Frisch (1980) found that 61 and 22% of the premenarche-trained swimmers and runners had irregular menstrual cycle and were amenorrheic, and 60% of the postmenarche-trained swimmers and runners had regular menstrual cycles. In our study, 92.3% of the premenarche-trained and 86.4% of the postmenarche-trained had regular menstrual cycle. The reason for high rates of regular menstrual cycle can be related to the training volume of Brazilian female futsal players. Both groups had low training volume. Delayed age at the first menarche has been reported in young girls involved in athletic training for at least 15 h/week (Thomis et al., 2005). In the present study, the post-menarche-trained and pre-menarche-trained reported a much lower training volume, which was 174 ± 88 min and 164 ± 64 min (≈3 h/week – 2–6 h/week), respectively. Thus, the low training volume of the present sample is probably a strong contributor of the low rates of menstrual dysfunctions in Brazilian elite futsal players.
Another factor previously associated with menstrual dysfunctions is eating disorder behaviors (Mountjoy et al., 2014; Ackerman and Misra, 2018). A previous study with female athletes of team sports, including futsal, noticed that 13.3% of the sample had eating disorders (Kravchychyn et al., 2013). The authors also found that 24.4% of the sample presented body image distortion, and the team sport athletes of higher BMI and percentage body fat had greater risk for body image distortion (Kravchychyn et al., 2013). In the present study, we did not find associations between body weight satisfaction and the four reproductive-related variables. However, our data demonstrate large rates of body weight dissatisfaction, with most of the participants willing to decrease their body weight.
The majority of our sample perceived their performance to be the best in the follicular phase of the menstrual cycle and only a few participants said that the luteal phase was their best period for performing. This can be supported by physical and physiological data, indicating a reduction in maximal endurance performance during the luteal phase of the menstrual cycle in nine sub elite female soccer players (Julian et al., 2017). However, these authors did not find the same effect or jumping and sprint performance (Julian et al., 2017). Evidence suggests that maximum endurance performance during the menstrual cycle is at its lowest during menstruation and/or the luteal phase (Janse de Jonge, 2003). With regards to strength-related variables, a systematic review that investigated changes in strength-related variables during different phases of the menstrual cycle in eumenorrheic women recommends caution in the interpretation of results due to the methodological shortcomings identified by the quality assessment (Blagrove et al., 2020). Strength-related measures appear to be minimally altered (g ≤ 0.35) by the fluctuations in ovarian sex hormones that occur during the menstrual cycle (Blagrove et al., 2020). Given the aerobic predominance of futsal, it is expected that women would perceive the follicular phase as the best to perform. The physiological mechanism behind the explanation for a greater performance perception in the follicular phase can be related to the link between the follicular phase with reduced sympathetic autonomic activity and lower emotional stress (Tada et al., 2017). Recent research has suggested that greater parasympathetic activity is associated with increased performance in futsal players (Nakamura et al., 2020). Nonetheless, women who perceived their performance to be the best during the follicular phase compared to the other menstrual phases did not differ in the onset of training, anthropometric characteristics, and the perception of ideal body weight.
Our study has four important strengths. First, we characterized reproductive-related variables and menstrual dysfunctions in elite futsal players. In addition, we assessed women who participate in the largest futsal competition in Brazil, which allow us to have a representative sample of female Brazilian elite futsal players. The third strength is the strong and standard methodological procedures to determine anthropometric variables and, subsequently, body composition and morphological variables. The last point is the inclusion of relevant physical aspects (i.e., anthropometric variables) and a perceptual aspect (i.e., body weight satisfaction) that could be linked with menstrual dysfunctions. We also have limitations. Although we were able to access a large cohort of Brazilian elite futsal players, the lack of a longitudinal design (i.e., only a cross-sectional study design) represents an important limitation. Age at menarche and age at the onset of training are susceptible to recall bias. However, previous investigations have indicated that woman’s first menstrual bleed is a widely used measure of puberty timing, a distinct and notable event in their lives, and is well-recalled (Koo and Rohan, 1997; Bosetti et al., 2001; Must et al., 2002). We could not include more sophisticated measurements of body composition (i.e., DEXA scans and pletismography) due to the design of the study and the lack of time and resources to account for these measurements in real-world settings. Only doubly indirect measurements were included (i.e., anthropometry). Body weight satisfaction was not determined with validated questionnaires and is based on the instrument developed by the leading investigator for this study. Finally, other factors that might influence menstrual dysfunctions were not included in our analysis, such as socioeconomic conditions, nutritional assessment, and access to preventive health care, that may influence the timing and progression of puberty and reproductive health (Baxter-Jones and Maffulli, 2002; American Academy of Pediatrics Committee on Adolescence et al., 2006). Although not the ideal variable to represent socioeconomic conditions, we have found that 69.6% of our sample received a salary as a futsal player and receiving a salary was associated with being a premenarche-trained athlete and greater rates of late menarche (data not shown).
Considering the low effect size for almost all the analysis, we cannot provide general clinical/practical guidance and an anthropometric profile based on reproductive-related factors in female futsal players. Rather than that, monitoring these reproductive factors and accounting for their impact on futsal athletes should be done using an individualized approach and considering each athlete’s needs. Future research should longitudinally account for the impact of reproductive-related variables in performance and the body composition markers of female futsal players.
Brazilian elite futsal players who engaged before the menarche had the menarche significantly later than those who started training after the menarche. Postmenarche-trained players had significant higher body fat and lower ectomorphy rate after controlling for covariates. Early menarche group presented higher sum of six skinfold thickness and endomorphy rate compared to normal and late menarche groups. No differences were found when menstrual periodicity groups and menstrual period, when performance is the best groups, were compared, except for higher femur width in the regular menstrual cycle group compared to the irregular one. Most of the participants of the present study had their menarche age classified as “normal,” presented a “regular” menstrual cycle and perceived to perform better during the follicular phase of the menstrual cycle. However, this perception was neither associated with other reproductive-related variables nor differed in anthropometric characteristics.
The datasets presented in this article are not readily available because of ethical reasons.
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the Midwest State University (UNICENTRO), process number 039/2011. The patients/participants provided their written informed consent to participate in this study.
MQ, DS, SF, MN, BP, MT, and EV: concept and design, methodology, the preparation of manuscript, the interpretation of data, formal analysis, and writing – review and editing. DS, TC, DF, and VW: formal analysis, the interpretation of data, writing and review, and the preparation of manuscript. MQ and SF: acquisition of subjects and data and writing and review. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ackerman, K. E., and Misra, M. (2018). Amenorrhoea in adolescent female athletes. Lancet Child Adolesc. Health. 2, 677–688. doi: 10.1016/S2352-4642(18)30145-7
American Academy of Pediatrics Committee on Adolescence American College of Obstetricians and Gynecologists Committee on Adolescent Health Care Diaz, A., Laufer, M. R., and Breech, L. L. (2006). Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics 118, 2245–2250. doi: 10.1542/peds.2006-2481
Barbero-Alvarez, J. C., Subiela, J. V., Granda-Vera, J., Castagna, C., Gómez, M., and Del Coso, J. (2015). Aerobic fitness and performance in elite female futsal players. Biol. Sport 32, 339–344. doi: 10.5604/20831862.1189200
Baxter-Jones, A. D., and Maffulli, N. (2002). Intensive training in elite young female athletes. Br. J. Sports Med. 36, 13–15. doi: 10.1136/bjsm.36.1.13
Beato, M., Bianchi, M., Coratella, G., Merlini, M., and Drust, B. (2018). Effects of plyometric and directional training on speed and jump performance in elite youth soccer players. J. Strength Cond. Res. 32, 289–296. doi: 10.1519/JSC.0000000000002371
Blagrove, R. C., Bruinvels, G., and Pedlar, C. R. (2020). Variations in strength-related measures during the menstrual cycle in eumenorrheic women: a systematic review and meta-analysis. JSAMS 12, 1220–1227. doi: 10.1016/j.jsams.2020.04.022
Bosetti, C., Tavani, A., Negri, E., Trichopoulos, D., and La Vecchia, C. (2001). Reliability of data on medical conditions, menstrual and reproductive history provided by hospital controls. J. Clin. Epidemiol. 54, 902–906. doi: 10.1016/S0895-4356(01)00362-6
Bruinvels, G., Burden, R. J., McGregor, A. J., Ackerman, K. E., Dooley, M., Richards, T., et al. (2017). Sport, exercise and the menstrual cycle: where is the research? Br. J. Sports Med. 51, 487–488. doi: 10.1136/bjsports-2016-096279
Calthorpe, L., Brage, S., and Ong, K. K. (2019). Systematic review and meta-analysis of the association between childhood physical activity and age at menarche. Acta Paediatr. 108, 1008–1015. doi: 10.1111/apa.14711
Carlberg, K. A., Buckman, M. T., Peake, G. T., and Riedesel, M. L. (1983). Body composition of oligo/amenorrheic athletes. Med. Sci. Sports Exerc. 15, 215–217.
Carter, J. E. L., and Health, B. H. (1990). Somatotyping: Development and Applications. Cambridge: Cambridge University Press.
Cole, T. J. (2003). The secular trend in human physical growth: a biological view. Econ. Hum. Biol. 1, 161–168. doi: 10.1016/S1570-677X(02)00033-3
Dale, E., Gerlach, D. H., and Wilhite, A. L. (1979). Menstrual dysfunction in distance runners. Obstet. Gynecol. 54, 47–53. doi: 10.1097/00006250-197907000-00013
Day, F., Elks, C., Murray, A., Ong, K. K., and Perry, J. R. B. (2015). Puberty timing associated with diabetes, cardiovascular disease and also diverse health outcomes in men and women: the UK Biobank study. Sci. Rep. 5:11208. doi: 10.1038/srep11208
Findlay, R. J., Macrae, E. H. R., Whyte, I. Y., Easton, C., and Whyte, L. J. F. N. (2020). How the menstrual cycle and menstruation affect sporting performance: experiences and perceptions of elite female rugby players. Br. J. Sports Med. 54, 1108–1113. doi: 10.1136/bjsports-2019-101486
Frisch, R. E. (1980). Pubertal adipose tissue: is it necessary for normal sexual maturation? Evidence from the rat and human female. Fed. Proc. 39, 2395–2400.
Garn, S. M., LaVelle, M., Rosenberg, K. R., and Hawthorne, V. M. (1986). Maturational timing as a factor in female fatness and obesity. Am. J. Clin. Nutr. 43, 879–883. doi: 10.1093/ajcn/43.6.879
Jackson, A. S., Pollock, M. L., and Ward, A. (1980). Generalized equations for predicting body density of women. Med. Sci. Sports Exerc. 12, 175–181.
Janse de Jonge, X. A. (2003). Effects of the menstrual cycle on exercise performance. Sports Med. 33, 833–851. doi: 10.2165/00007256-200333110-00004
Julian, R., Hecksteden, A., Fullagar, H. H., and Meyer, T. (2017). The effects of menstrual cycle phase on physical performance in female soccer players. PLoS One 12:e0173951. doi: 10.1371/journal.pone.0173951
Koo, M. M., and Rohan, T. E. (1997). Accuracy of short-term recall of age at menarche. Ann. Hum. Biol. 24, 61–64. doi: 10.1080/03014469700004782
Kravchychyn, A. C. P., da Silva, D. F., and Machado, F. A. (2013). Relação entre estado nutricional, adiposidade corporal, percepção de autoimagem corporal e risco para transtornos alimentares em atletas de modalidades coletivas do gênero feminino. Rev. Bras. Educ. Fís Esporte 27, 459–466. doi: 10.1590/S1807-55092013000300012
Loucks, A. B. (2004). Energy balance and body composition in sports and exercise. J. Sports Sci. 22, 1–14. doi: 10.1080/0264041031000140518
Malina, R. M., Baxter-Jones, A. D., Armstrong, N., Beunen, G. P., Caine, D., Daly, R. M., et al. (2013). Role of intensive training in the growth and maturation of artistic gymnasts. Sports Med. 43, 783–802. doi: 10.1007/s40279-013-0058-5
Marfell-Jones, M., Olds, T., Stewart, A., and Carter, L. (2006). International Standards for Anthropometric Assessment. Potchefstroom: International Society for the Advancement of Kinanthropometry-ISAK, Potchefstroom.
Matina, R. M., and Rogol, A. D. (2011). Sport training and the growth and pubertal maturation of young athletes. Pediatr. Endocrinol. Rev. 9, 441–455.
McNulty, K. L., Elliot-Sale, K. J., Dolan, E., Swinton, P. A., Ansdell, P., Goodall, S., et al. (2020). The effects of menstrual cycle phase on exercise performance in Eumenorrheic women: a systematic review and meta-analysis. Sports Med. 50, 1813–1827. doi: 10.1007/s40279-020-01319-3
Merzenich, H., Boeing, H., and Wahrendorf, J. (1993). Dietary fat and sports activity as determinants for age at menarche. Am. J. Epidemiol. 138, 217–224. doi: 10.1093/oxfordjournals.aje.a116850
Mountjoy, M., Sundgot-Borgen, J., Burke, L., Carter, S., Constantini, N., Lebrun, C., et al. (2014). The IOC consensus statement: beyond the female athlete triad--relative energy deficiency in sport (RED-S). Br. J. Sports Med. 48, 491–497. doi: 10.1136/bjsports-2014-093502
Must, A., Phillips, S. M., Naumova, E. N., Blum, M., Harris, S., Dawson-Hughes, B., et al. (2002). Recall of early menstrual history and menarcheal body size: after 30 years, how well do women remember? Am. J. Epidemiol. 155, 672–679. doi: 10.1093/aje/155.7.672
Nakamura, F. Y., Antunes, P., Nunes, C., Costa, J. A., Esco, M. R., and Travassos, B. (2020). Heart rate variability changes from traditional vs. ultra-short-term recordings in relation to preseason training load and performance in futsal players. J. Strength Cond. Res. 34, 2974–2981. doi: 10.1519/JSC.0000000000002910
Palucci Vieira, L. H., Arins, F. B., Guglielmo, L. G. A., de Lucas, R. D., Carminatti, L. J., and Santiago, P. R. P. (2020). Game running performance and fitness in women's futsal. Int. J. Sports Med. doi: 10.1055/a-1202-1496, [Epub ahead of print]
Queiroga, M. R., Ferreira, S. A., Cavazzotto, T. G., Portela, B. S., Tartaruga, M. P., Nascimento, M. A., et al. (2019). Comparison between two generations to verify the morphological changes in female futsal athletes in a period of 10 years. Rev. Bras. Cineantropom. Desempenho Hum. 21:e56970. doi: 10.5007/1980-0037.2019v21e56970
Ramos-Campo, D. J., Rubio-Arias, J. A., Carrasco-Poyatos, M., and Alcaraz, P. E. (2016). Physical performance of elite and subelite Spanish female futsal players. Biol. Sport 33, 297–304. doi: 10.5604/20831862.1212633
Schoenaker, D. A. J. M., and Mishra, G. D. (2017). Association between age at menarche and gestational diabetes mellitus: the Australian longitudinal study on women's health. Am. J. Epidemiol. 185, 554–561. doi: 10.1093/aje/kww201
Siri, W. E. (1961). “Body Composition From Fluid Spaces and Density: Analysis of Methods,” in Techniques for Measuring Body Composition. eds. J. Brozek and A. Henschel (Washington, DC: National Academy of Sciences), 223–224.
Stager, J. M., Robertshaw, D., and Miescher, E. (1984). Delayed menarche in swimmers in relation to age at onset of training and athletic performance. Med. Sci. Sports Exerc. 16, 550–555.
Tada, Y., Yoshizaki, T., Tomata, Y., Yokoyama, Y., Sunami, A., Hida, A., et al. (2017). The impact of menstrual cycle phases on cardiac autonomic nervous system activity: an observational study considering lifestyle (diet, physical activity, and sleep) among female college students. J. Nutr. Sci. Vitaminol. 63, 249–255. doi: 10.3177/jnsv.63.249
Tamakoshi, K., Yatsuya, H., and Tamakoshi, A., JACC Study Group (2011). Early age at menarche associated with increased all-cause mortality. Eur. J. Epidemiol. 26, 771–778. doi: 10.1007/s10654-011-9623-0
Theintz, G. E. (1994). Endocrine adaptation to intensive physical training during growth. Clin. Endocrinol. 41, 267–272. doi: 10.1111/j.1365-2265.1994.tb02543.x
Thomis, M., Claessens, A. L., Lefevre, J., Philippaerts, R., Beunen, G. P., and Malina, R. M. (2005). Adolescent growth spurts in female gymnasts. J. Pediatr. 146, 239–244. doi: 10.1016/j.jpeds.2004.09.026
Toriola, A. L. (1988). Survey of menstrual function in young Nigerian athletes. Int. J. Sports Med. 9, 29–34. doi: 10.1055/s-2007-1024974
Werneck, A. O., Coelho-e-Silva, M. J., Padilha, C. S., Ronque, E. R. V., Cyrino, E. S., Szwarcwald, C. L., et al. (2018a). Age at menarche and cancer risk at adulthood. Ann. Hum. Biol. 45, 369–372. doi: 10.1080/03014460.2018.1470670
Keywords: female athletes, sports medicine, early puberty, five-a-side football, reproductive health, menstrual cycle, soccer, women
Citation: Queiroga MR, da Silva DF, Ferreira SA, Weber VMR, Fernandes DZ, Cavazzotto TG, Portela BS, Tartaruga MP, Nascimento MA and Vieira ER (2021) Characterization of Reproductive and Morphological Variables in Female Elite Futsal Players. Front. Psychol. 12:625354. doi: 10.3389/fpsyg.2021.625354
Received: 02 November 2020; Accepted: 06 April 2021;
Published: 05 May 2021.
Edited by:
Fábio Yuzo Nakamura, Instituto Universitário da Maia (ISMAI), PortugalReviewed by:
Rafael Dos Santos Henrique, Federal University of Pernambuco, BrazilCopyright © 2021 Queiroga, da Silva, Ferreira, Weber, Fernandes, Cavazzotto, Portela, Tartaruga, Nascimento and Vieira. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marcos Roberto Queiroga, cXVlaXJvZ2FtckBob3RtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.