
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 25 May 2021
Sec. Health Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.622973
 Rejane Coan Ferretti Mayer
Rejane Coan Ferretti Mayer Maíra Ramos Alves
Maíra Ramos Alves Sueli Miyuki Yamauti
Sueli Miyuki Yamauti Marcus Tolentino Silva
Marcus Tolentino Silva Luciane Cruz Lopes*
Luciane Cruz Lopes*Context: People with mental disorders can acquire long-term disabilities, which could impair their functioning and quality of life (QoL), requiring permanent care and social support. Systematic data on QoL and functioning, which could support a better management of these people, were not available.
Objective: To analyze the QoL, level of functioning and their association with sociodemographic and clinical factors of people with mental disorders who underwent deinstitutionalization using assisted living facilities.
Methods: A Cross-sectional study was conducted between July 2018 and July 2019, through interviews using the World Health Organization Quality of Life (WHOQOL-BREF) to determine the QoL scores, and the World Health Organization Disability Assessment Schedule (WHODAS 2.0) to determine the level of functioning. All adults (≥18 years old) with mental disorders, who underwent deinstitutionalization, users of assisted living facilities and assisted by the Psychosocial Assistance Centers III, in a city in the state of São Paulo, Brazil, were selected. For statistical analysis of the associated factors, Student’s t-test was used for dichotomous variables and ANOVA for polynomial variables. Pearson correlation coefficient was used to measure the association between QoL and functioning scores.
Results: Out of 359 people who underwent deinstitutionalization with mental disorders, 147 met the eligibility criteria. The mean total score for the WHOQOL-BREF was 66.5 ± 13.4 and the mean score for WHODAS 2.0 was 10.4 ± 7.6. An association was found between people who were studying (n = 65.8; 95%CI, 63.5–68.1 vs. n = 73.9; 95%CI, 67.5–80.3; p = 0.04) and better WHOQOL-BREF QoL scores or WHODAS 2.0 levels of functioning (n = 10.9; 95%CI, 9.6–12.2 vs. n = 5.1; 95%CI, 2.5–7.7; p = 0.01). A weak negative correlation (r = 0.41) emerged between higher QoL scores and functioning improvement.
Conclusion: This study indicates that the QoL of the sample is associated by their functioning levels, which, in turn, may reflect on their social interactions. Public policies that favor interventions increasing socialization of this population can result in better health outcomes. The QoL and functioning scores provide valuable insights to develop public policies more suited to this population profile.
Mental disorders can be defined as a group of signs and symptoms that clinically affect physical, psychological, behavioral, and cognitive aspects of a person (American Psychiatric Association, 2014). In some cases, they can cause long term incapacities, leading to impairments in people’s functioning and quality of life (QoL) and are responsible for 34% of the existing disabilities in the Americas (Hiany et al., 2018; Pan American Health Organization, 2018). People with severe mental disorders may need permanent care and social support in the community (World Health Organization and the Gulbenkian Global Mental Health Platform, 2014).
Deinstitutionalization movements first started in developed countries (Thornicroft and Bebbington, 1989; Yohanna, 2013; Hudson, 2019). In the United States, the decrease in hospital beds and changes toward community-based mental health services started in the 1950’s and a similar thing has happened with the United Kingdom (Thornicroft and Bebbington, 1989; Hudson, 2019). In Italy, this process took place in the 1960’s with a special focus on the experiences of Franco Basaglia, a pioneer in the anti-asylum movements in Italy, which had a significant impact on the deinstitutionalization movements in Brazil (Thornicroft and Bebbington, 1989; Amarante and Nunes, 2018). Since the deinstitutionalization process, mental health policies around the world passed through reformulations to provide care to the people who underwent deinstitutionalization recently (Shen and Snowden, 2014).
The Brazilian process diverged from these other countries, both because of the period — started the anti-asylum movements in the 1970’s and consolidated the deinstitutionalization laws in the 2000’s — and because of its structure. The mental health policy, introduced by the Psychiatric Reform Law (Brasil, 2001), is structured based on the humanization principles of the Brazilian Unified Health System and built in the form of a network (Ministério da Saúde, 2005, 2014; Santos et al., 2015; Sampaio and Bispo Júnior, 2021). It upheld the care in freedom and the reestablishment of the citizenship of people with mental disorders who underwent deinstitutionalization and were guided by the creation and maintenance, by the State, of services that substituted the asylum model, such as the Psychosocial Assistance Centers (in Portuguese, Centros de Atenção Psicossocial - CAPS) and assisted living facilities (Passos et al., 2013; Trape and Campos, 2017).
The assisted living facilities1 are dwellings, located in urban centers, aimed at sheltering people with mental disorders that, after a long period of hospitalization, have passed through the process of deinstitutionalization and lack familiar or community support. These services play an important role in retaking citizenship and reinserting the user into society, as it is through the symbolic and material appropriation of the dwelling and its surroundings that the rehabilitation process begins (Argiles et al., 2013; Cortes and Barros, 2017). Clinical care and individualized treatment plans are developed and applied at CAPS (Ministério da Saúde, 2004).
QoL comprises the individual’s relationships and perceptions, influenced by cultural determinants in relation to personal and social values under which the person lives (The WHOQOL Group, 1996). In addition, QoL encompasses important aspects of resocialization, environmental adaptation, and care for the individual (Costa et al., 2014; Passos and Portugal, 2015; Silva and Rosa, 2015).
The functioning of these people is also an important monitoring indicator. Functioning is understood as the bodily functions, the activities performed and the person’s participation, in relationship with environmental factors (barriers and enablers) (World Health Organization, 2007). In contrast, disabilities refer to impairments, limitations and restrictions to activities and participation, in relationship with the environment.
The functioning assessment and limitations of the person with mental disorders is important to identify the consequences related to the disorder, contributing to the choice of more effective interventions and priority areas for public resource allocation (Silveira et al., 2013).
QoL and functioning can be used as important parameters in the development of mental healthcare strategies, health condition monitoring and social reinsertion of these people, supporting the new assisted living facility implementations and improvement of existent ones.
This study analyzed the QoL, functioning and their relationship with sociodemographic and clinical aspects of people with mental disorder who underwent deinstitutionalization using the assisted living facilities in Brazil. In addition, the current study highlights the uniqueness of the Brazilian process, offering quantitative data about this population.
A cross-sectional study was conducted between July 2018 and July 2019, through interviews using the World Health Organization Quality of Life instrument (WHOQOL-BREF) (The WHOQOL Group, 1996) to determine QoL scores and the World Health Organization Disability Assessment Schedule (WHODAS 2.0 – 12 items) to assess the levels of functioning (World Health Organization, 2010).
This study employed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (Appendix 1) for the more precise and complete description of observational studies (Vandenbroucke et al., 2007).
The study was conducted in the city of Sorocaba, state of São Paulo, Brazil, in the CAPS III and the assisted living facilities.
Sorocaba is an important city in Brazilian mental health, because of the Vera Cruz Psychiatric Hospital, which, after years of operation, became a deinstitutionalization pole by the end of its activities (Prefeitura de Sorocaba, 2019). The city’s mental health plan, organized by the State Health Secretariat encompasses ten CAPS in total, one of each type for each Health Regional of the city. There are three CAPS of the type III. These offer specialized care to people with mental disorders and work with multidisciplinary teams including psychiatrists, nurses, nursing technicians, occupational therapists, psychologists, and social workers. They operate 24 h, having beds for nocturnal shelter and capacity to assist more than 1,000 people per month (Ministério da Saúde, 2014; Blog da Saúde, 2014).
There are 40 assisted living facilities in the city, with a capacity of ten, where people who underwent deinstitutionalization could return to live in the society, acquire responsibility, freedom, and autonomy over their daily routines, taking care of domestic activities and sharing houses with other people. Some facilities can have a caregiver, depending on the need and severity of the disorder of the residents.
The participants were extracted from a population of 359 people who underwent deinstitutionalization living in assisted living facilities at Sorocaba city and assisted by the CAPS III unities, from July 2018 to July 2019. 114 failed to sign the informed consent form, leading to the availability of 245 people who were willing to participate in the research.
Participants were selected if they underwent deinstitutionalization, were older than 18 years of age, users of assisted living facilities, assisted by the CAPS III in Sorocaba and had signed the informed consent form.
Participants were excluded if they failed to finish or refused to respond the questionnaires.
The instruments were applied in the assisted living facilities, by two psychologists, RM and MA, with previous scheduling, both in the same day. The residents were reunited in their living room and invited to participate, in the presence of their trusted person, usually the caregiver or the technical reference of the house.
In addition to the interviews, other complementary information was obtained from the medical records.
From the medical records, sociodemographic data (gender; age; marital status; education; financial autonomy; family ties) and clinical data (psychiatric hospital of origin; current diagnosis; diagnosis from hospitalization; comorbidities; time of hospitalization; time of deinstitutionalization; number of hospitalizations in psychiatric beds, CAPS beds and general hospital beds after deinstitutionalization; drug therapy) were extracted.
In the absence of any of this information above within the medical record, the health team was consulted. The team and the participant validated the missing or incomplete information in the medical record, to reduce the memory bias in this type of research design.
WHOQOL-BREF and WHODAS 2.0-12 items were applied both in the same day and only once to the participants.
WHOQOL-BREF (The WHOQOL Group, 1996) is a QoL questionnaire developed by the World Health Organization, composed of 24 items clustered into four domains: Physical health, Psychological, Social relationships, and Environment; and two items referring to the Self-evaluation of the QoL, totaling 26 items (Fleck et al., 2000; Pedroso et al., 2010). It was developed by specialists from different cultures as a generic intercultural instrument that could be used by different professionals (Angelim et al., 2015).
When compared to other widely used instruments, such as the 36-item Form Constructed to Survey Health Status (SF-36), EUROQOL (EQ-5D), Medical Outcomes Studies 36-item Short-Form (MOS SF-36) and Medical Outcomes Studies 12-item Short-Form (MOS SF-12), WHOQOL-BREF stands out for presenting the Social relationships and Environment domains, in addition to Physical health and Psychological domains (Almeida-Brasil et al., 2017; Skevington and Epton, 2018). This makes it possible to assess issues related to the person’s subjective perception over its contexts, distinctly from other instruments, which evaluate issues related to the functioning consequences of a given health condition (Almeida-Brasil et al., 2017).
These characteristics make WHOQOL-BREF a broader instrument about QoL perception and can be used in different knowledge areas (Castro et al., 2014; Skevington and Epton, 2018). It presents both low user bounce and data loss rates which makes it a more precise instrument (Skevington and Epton, 2018).
The WHODAS 2.0-12 items were used to assess the functioning outcome variable. The full version WHODAS 2.0 instrument has 36 items and is scored on a scale of 0-40, with higher scores indicating poor levels of functioning. It evaluates the functioning levels in six domains: Cognition, Mobility, Self-care, Getting along, Life Activities and Participation, which composes the domains of the International Classification of Functioning (World Health Organization, 2007). The 12-item instrument is a shortened version for assessments limited in time or because of other reasons that can cause an impediment to the 36-item instrument use (Ćwirlej-Sozańska et al., 2020). The WHODAS 2.0 - 12 items version used in the current study limits the calculation of scores by domains and scores range on a scale of 12-60 (World Health Organization, 2010).
Validation studies of the WHODAS 2.0 – 12 items showed that the instrument displays reliability to score functioning and health conditions, especially when applied to populations with mental disorders. In addition, because of its quick and easy application, its use has been recommended with this population (Carlozzi et al., 2015; Axelsson et al., 2017; Ćwirlej-Sozańska et al., 2020). Non-parametric analysis shows that the 12-item instrument works well within the different levels of disablement and it presented no differences when applied to both genders (Luciano et al., 2010). It has also been adapted and validated for the Brazilian context (Silveira et al., 2013).
To avoid information bias and systematic errors related to data collection, high quality validated instruments were used. The researchers that collected data were trained to apply the instruments, following the orientations within each manual, to guarantee a standardized application, also avoiding observation, instrument assessment, and verification biases.
Possible recall bias within the data collection through interviews, due to the influence of the disorder severity and memory problems resulting from the temporal distance in which the questioned event occurred (the questionnaires asked about events occurred 2 weeks prior to its application), was reduced confronting the data with the person’s care team.
The quantitative data consisted of sociodemographic data and outcome variables, which were tabulated and compared. The scores obtained for each instrument, WHOQOL-BREF and WHODAS 2.0 – 12 items, were calculated following each respective manual instruction (The WHOQOL Group, 1996; World Health Organization, 2010).
For the WHOQOL-BREF scores, first a simple mean was calculated for the Likert-scored answers. Then, they were transformed into a score of 4-20 points and later transformed again into a scale of 0-100 points, in which scores closer to 100 indicate better QoL (The WHOQOL Group, 1996).
For WHODAS 2.0 – 12 items, we used the simple scoring method described in the manual. In this type of score, recommended for the 12 items version, the values assigned to each answer are summed, wherein “none” = 1, “mild” = 2, “moderate” = 3, “severe” = 4 and “extreme” = 5 (World Health Organization, 2010).
Statistical descriptive analysis was performed for the studied variables measured. Frequency was calculated for the categorical variables and means and standard deviations for the continuous variables. The association with the sociodemographic and clinical factors was assessed using the student’s t-test for the dichotomous variables and analysis of variance (ANOVA) for polynomial variables, using STATA (14.2 version) statistical program. The 95% confidence interval was standardized, and the level of significance was set at 5%.
A dispersion graph was plotted to show the correlation between QoL and functioning, that was assessed by Pearson correlation coefficient.
Out of 359 people who underwent deinstitutionalization living in assisted living facilities at Sorocaba city, 114 failed to sign the informed consent form, resulting in 245 people who were willing to participate in the research. During the WHOQOL-BREF application, 98 failed to finish or refused to respond the questionnaire and were excluded, resulting in 147 people who had completed the QoL assessment. In the WHODAS 2.0 – 12 items application, 102 failed to finish or refused to respond the questionnaire and were excluded, resulting in 143 people who had completed the functioning assessment (Figure 1).
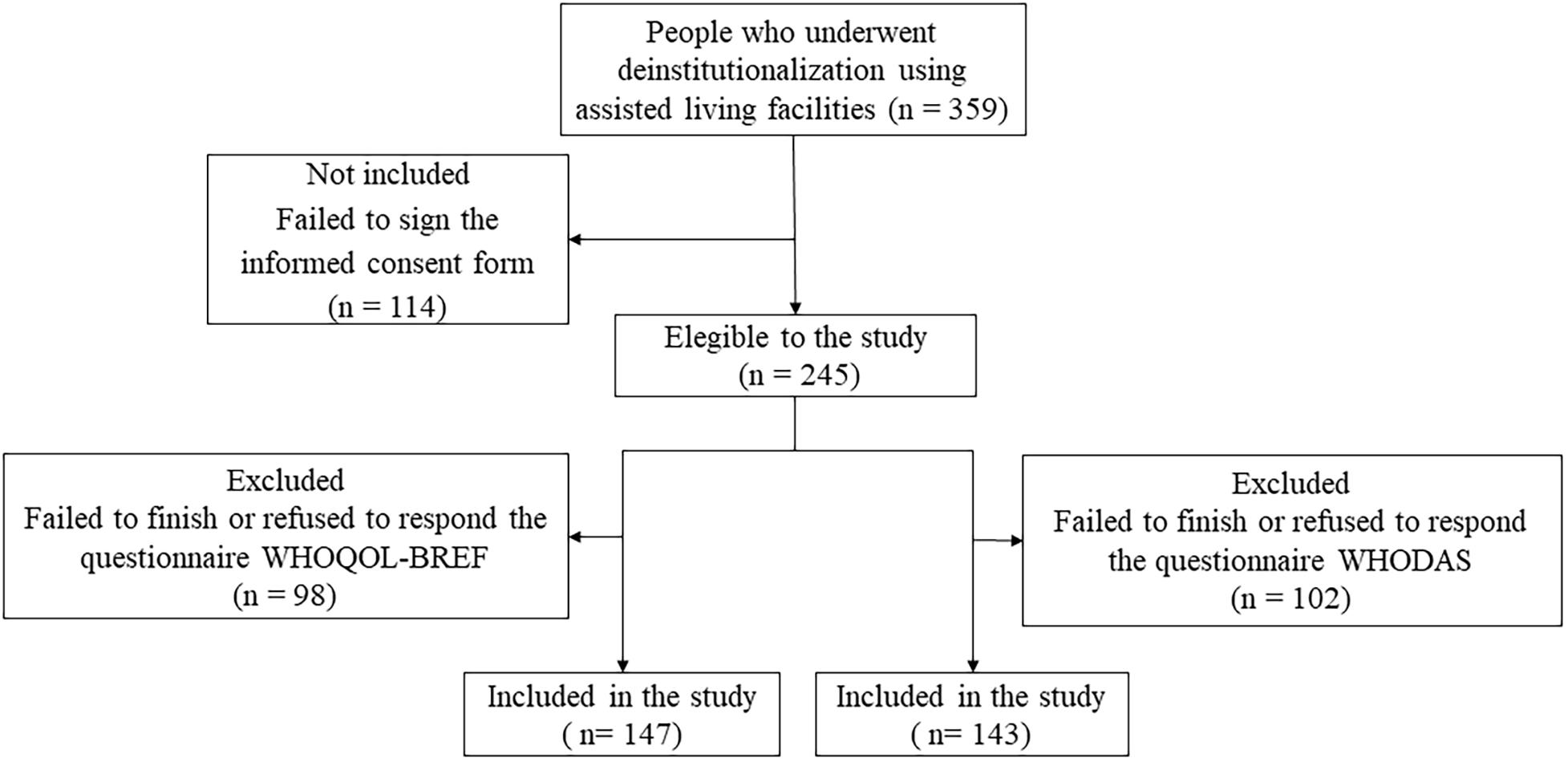
Figure 1. Flowchart of Sample Composition. WHOQOL-BREF, World Health Organization Quality of Life. WHODAS 2.0, World Health Organization Disability Assessment Schedule.
About the population’s sociodemographic characteristics: the participants (n = 147) displayed a mean age of 51.5 ± 10.6 years, were predominantly male (n = 83, 56.5%), single (n = 136, 92.5%), not literate (n = 98, 66.7%), without paid work (n = 145, 98.6%), and beneficiaries of social programs (n = 135, 91.8%) (Table 1).
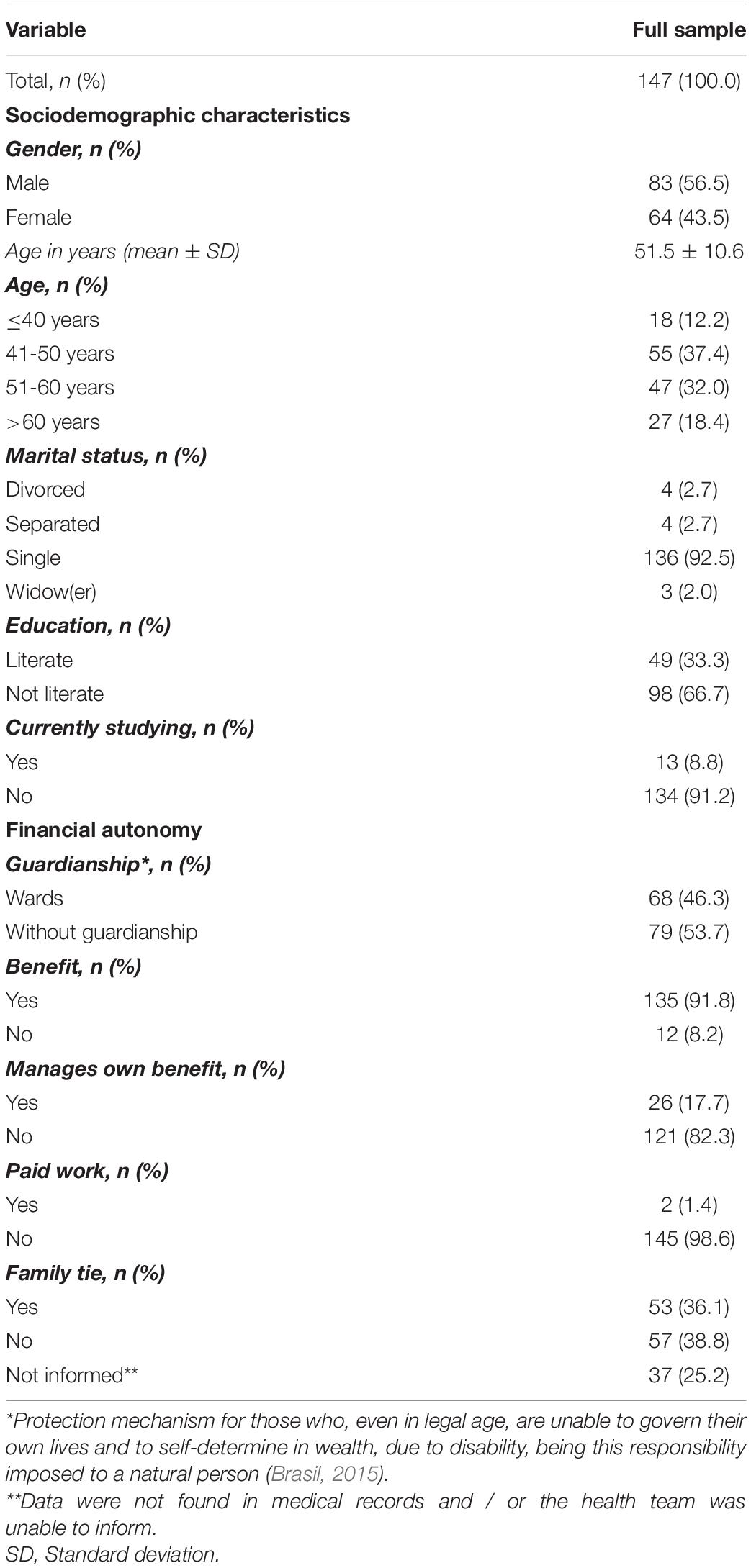
Table 1. Sociodemographic characteristics of people with mental disorders who underwent deinstitutionalization using assisted living facilities, Sorocaba city, 2019.
Schizophrenia spectrum disorders (n = 63, 42.9%) were the most prevalent diagnosis of mental disorders, followed by intellectual disabilities (n = 41, 27.9%). The mean time of hospitalization in psychiatric hospitals was 16.9 ± 8.8 years. Most of them were not admitted to a psychiatric bed (n = 143, 97.2%) and/or CAPS bed (n = 136, 92.5%) after deinstitutionalization (Table 2).
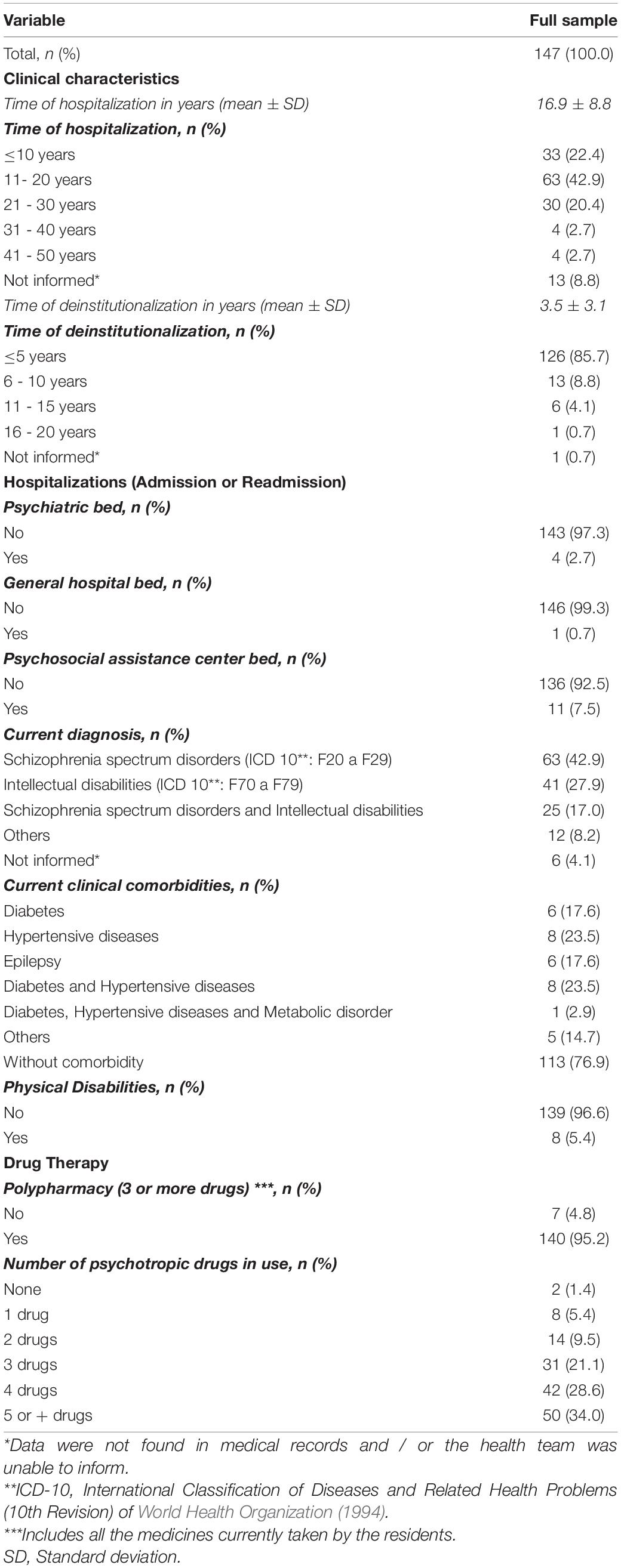
Table 2. Clinical characteristics of people with mental disorders who underwent deinstitutionalization using assisted living facilities, Sorocaba city, 2019.
About the level of functioning variable, we have only measured the global functioning score for our sample, since the WHODAS 2.0 – 12 items do not allow the calculation of scores by domains. The mean functioning score obtained was 10.4 ± 7.6.
The mean total score for the WHOQOL-BREF questionnaire was 66.5 ± 13.4. Between the domains, the greater mean score was for the QoL Self-evaluation domain (69.8 ± 21.8) and the lowest for the Psychological domain (63.7 ± 19.0) (Table 3).
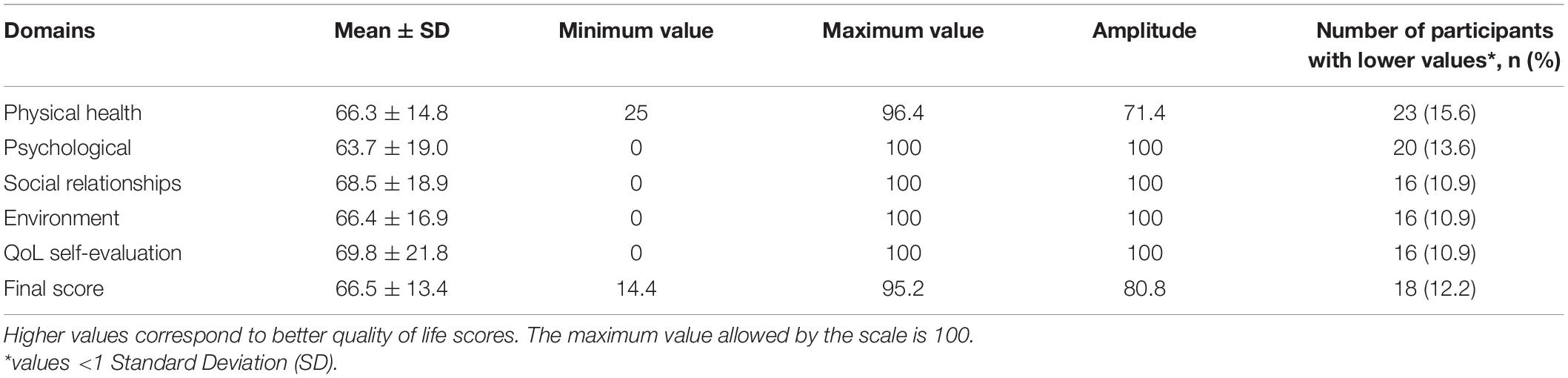
Table 3. Mean transformed scores (0-100 scale) of WHOQOL-BREF obtained by the application in people with mental disorders who underwent deinstitutionalization using assisted living facilities, Sorocaba city, 2019.
Statistically significant associated factors related to sociodemographic and clinical variables and QoL or levels of functioning were not found, except for the “currently studying” variable (Tables 4, 5).
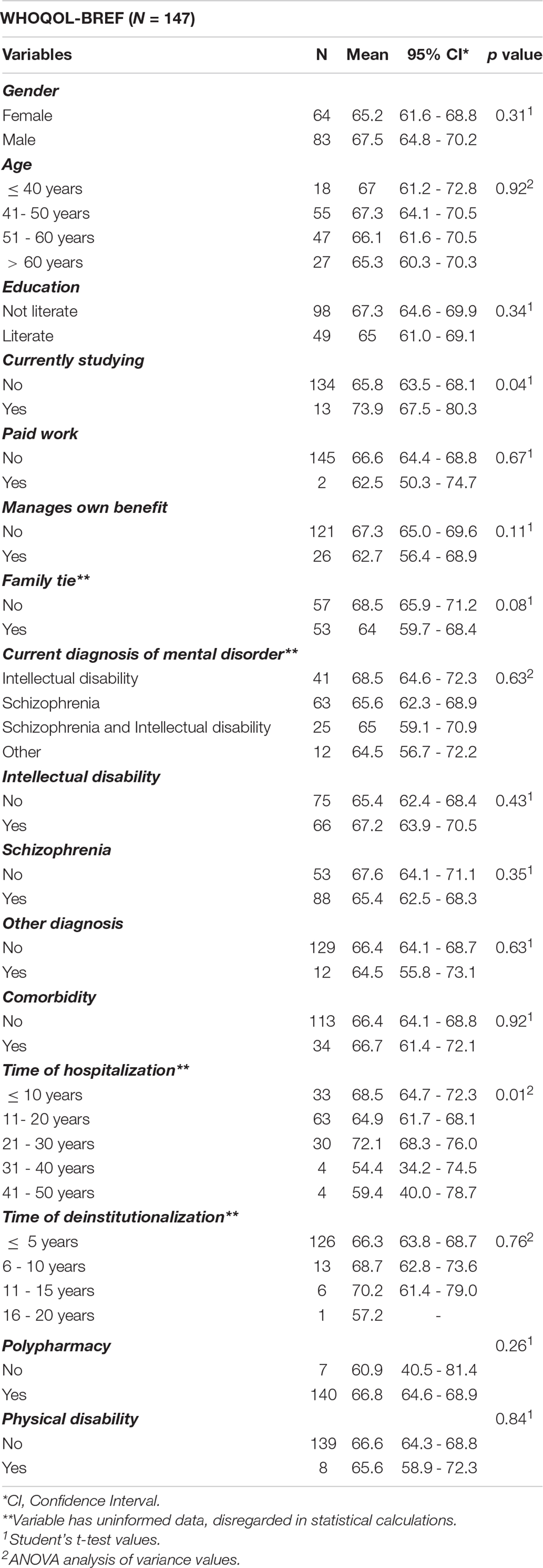
Table 4. Distribution of people with mental disorders who underwent deinstitutionalization using assisted living facilities by sociodemographic and clinical characteristics according to WHOQOL-BREF, 2019, n = 147.
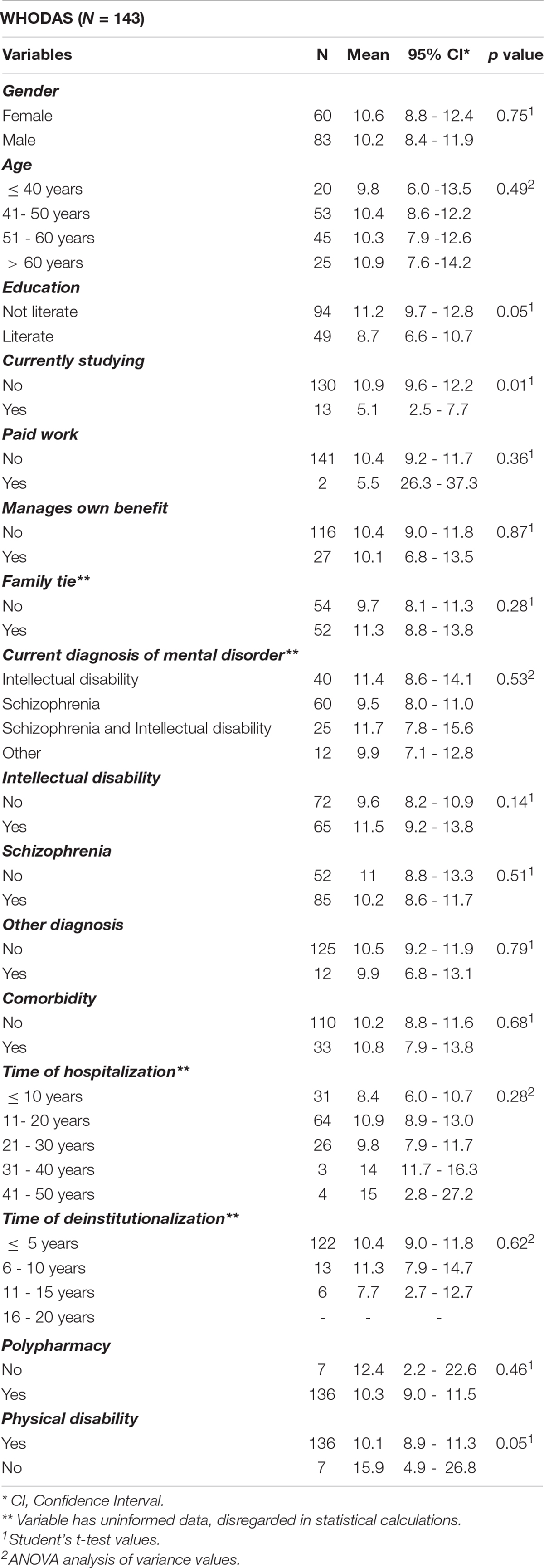
Table 5. Distribution of people with mental disorders who underwent deinstitutionalization using assisted living facilities by sociodemographic and clinical characteristics according to WHODAS 2.0, 2019, n = 143.
A weak negative linear correlation emerged (r = 0.4) between the QoL and functioning scores such that the higher the decrease in the level of functioning, the lower the QoL scores (Figure 2).
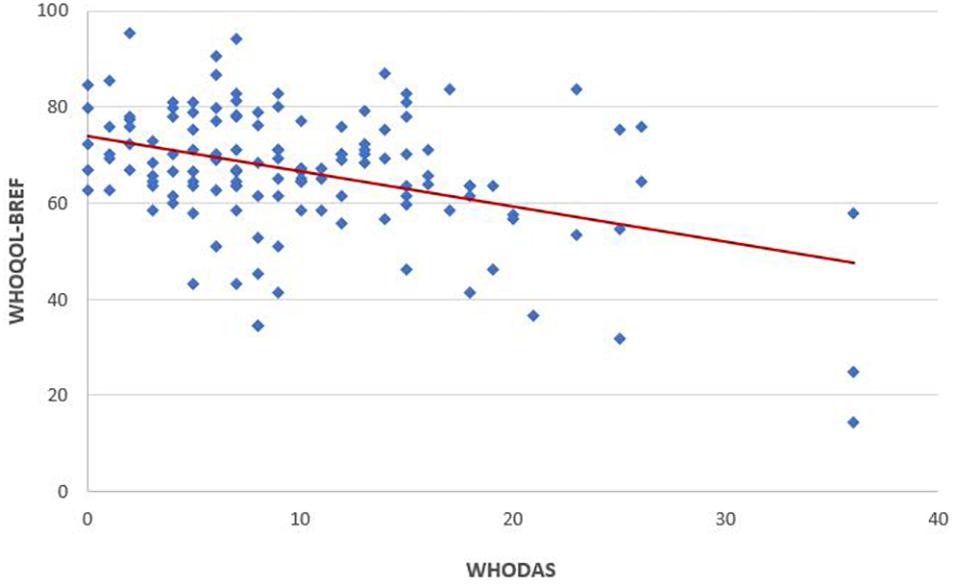
Figure 2. Correlation of quality of life (WHOQOL-BREF) to levels of functioning (WHODAS). Pearson correlation analysis shows a weak negative correlation of WHODAS versus WHOQOL-BREF (Pearson r = 0.41; n = 135). Line represents linear regression of data (y = –0.74x + 73.94; r2 = 0.1651).
The study results indicated that in people with mental disorders who underwent deinstitutionalization using the assisted living facilities in Sorocaba, Brazil, the prevalent characteristics include middle-aged men, single, not literate, unemployed, without family ties or children, mainly with schizophrenia spectrum disorder or intellectual disabilities with a history of long years of hospitalization and a short time of deinstitutionalization. There seems to be an association between people who were currently studying, education and better levels of functioning and QoL scores. In addition, an association between physical disabilities and worst levels of functioning was observed. Furthermore, a weak negative linear correlation between QoL and functioning emerged. Other variables were not associated with the improvement of QoL or level of functioning.
A few studies that used the WHOQOL-BREF instrument in people with schizophrenia obtained QoL mean scores higher than 80 (Mas-Exposito et al., 2011; Mohandoss, 2017), 20 points higher than the obtained by our sample. The QoL of the general population can be affected by factors related to gender, age, family ties, employment, social interaction, health conditions, among other factors (Gomez et al., 2017; Wang et al., 2017; Sum et al., 2018). Although these factors can influence the general population’s QoL, studies conducted in people with schizophrenia were not consistent regarding the existence of associated factors (Souza and Coutinho, 2006).
The prevalence of sociodemographic characteristics such as single middle-aged men, not literate, and unemployed, were also found in studies conducted in Rio de Janeiro (Alves et al., 2010), Piauí (Lago et al., 2014) and Pernambuco (França et al., 2017). However, these factors were not associated with lower QoL or functioning scores in our sample.
In addition to the mental disorder itself, which contributes to interpersonal difficulties, the isolation caused by a long hospitalization period reinforces social impairment and the need for reintegration, that could contribute to an improvement in QoL and functioning. These factors can explain, in part, the low score obtained in the Physical health and Psychological domains, since these domains cover issues about body health, energy, feelings, capacity perception, body perception and self-esteem (The WHOQOL Group, 1996; Pedroso et al., 2010).
The lack of employment, a prevalent characteristic in this sample, was also captured in previous studies (Alves et al., 2010; Lago et al., 2014; França et al., 2017) and could be related to stigma and prejudice, that is present in the employment sector, and in the society in general (Assunção et al., 2017). Our sample showed moderately low functioning mean values compared to other population studies (Ferrer et al., 2019). This can also partially explain the lack of employment.
To people with mental disorders, work can be therapeutic, an incentive to socialize and improve QoL, social recognition, and the development of abilities (Melo et al., 2015; Fernandes et al., 2017). A study conducted with 268 people with schizophrenia, using the WHOQOL-BREF, showed a positive association (p = 0.020) between being employed and better QoL scores (Pinho et al., 2018). Similarly, the associations found between people currently studying and better functioning and QoL scores show the importance of these sociodemographic aspects to elaborate intervention strategies that could develop abilities and functioning capacities of people with mental disorders. In addition, they might draw support from education and employment and, consequently, decrease their functioning disabilities (Picco et al., 2018).
However, although our sample has few family ties, the high mean scores obtained for the social relationship domain was surprising. A linear positive relationship between the support of the companions and friendships and an improvement in the QoL scores was observed (Portugal et al., 2016). One hypothesis to explain these findings is that, in assisted living facilities, the housemates become the new family, what ends up supplying the lack of fundamental support that can be offered by the family in the care (Costa et al., 2014; Dadalte et al., 2017).
It is worth mentioning that although the general QoL score was lower than the mean scores found in other populations (Cruz et al., 2011; Almeida-Brasil et al., 2017), the perception of QoL in this study, measured by the Self-evaluation domain of WHOQOL-BREF instrument, proved to be high. These high QoL perceptions scores could be explained by the fact that assisted living facilities are structured following the principles of humanized assistance of the Brazilian Unified Health System (Santos et al., 2015) and that, as stated by the World Health Organization (2001), the community-based mental health care, outside the psychiatric hospitals, have a positive effect in the clinical outcomes and QoL of people with chronic mental disorders, in addition to respecting human rights.
This study presents original data about a vulnerable population that is directly affected by the care provided by the health system and by the severity of the mental disorder. The sociodemographic and clinical variables description used to verify the associated factors, represent important information to health professionals and local managers, to face the problem at this stage of the deinstitutionalization process. Data about QoL and functioning of people who underwent deinstitutionalization with mental disorders, users of assisted living facilities, since the Psychiatric Reform in Brazil (Brasil, 2001), were not available. These findings can contribute to better care management and amendment of public policies for this population.
Notwithstanding the fact that the sample can be considered epidemiologically small, it corresponds to the majority (∼70%) currently assisted by the assisted living facilities, in one of the cities in the region considered in the past, the largest asylum pole in the country. The prevalence of the diagnoses of complex severity and significant cognitive impairment helps to understand, in part, the profile of those previously institutionalized people, as well as the absence of bonds and family abandonment. In addition, this was a limiting factor for the person’s participation in the interviews about QoL and functioning since the cognitive impairment in about 40% of the people prevented them from understanding the questionnaire. Consequently, these people were excluded from this analysis. As a result, the data expressed here, although current on QoL and functioning, are not representative of a portion of the people who used assisted living facilities.
The design type of this study can be considered as a limitation for the result assessments since descriptive cross-sectional studies only show the prevalence of a given factor or characteristic, but do not establish cause-effect relationships, once the outcome and the exposure are assessed at the same time (Venancio, 2017).
The QoL of people with mental disorders in this study was associated to their level of functioning, which in turn, can be reflected on the low employment rates and social interactions. Considering that this is a middle-aged population, that in a couple of years will become an elderly population, the mental health care should develop strategies that promote QoL and improve functioning of the people with mental disorders who use assisted living facilities, benefiting them and the society. Although the Brazilian mental health policy has been debatable, and the implementation process is incomplete, there is still room to rescue the financial, occupational, physical, and educational autonomy of the people with mental disorders, so that they can enjoy the social interaction benefits from which they were previously deprived.
The QoL and functioning scores in this study provide valuable data to develop public policies more suited to this population profile. Studies of national inquiry, comparing the QoL scores of these people, users of assisted living facilities, and those who returned to live with their families, and the type of care they receive in psychosocial attention networks could provide important information for interventions aimed at these people and better inform implementation of public policy.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The study protocol was approved by the Brazilian Research Ethics Committee (protocol n° 2.600.954/2018) and by the Municipal Government of Sorocaba City (protocol n° 26022018). All subjects gave written informed consent in accordance with the Declaration of Helsinki.
LL and RM contributed to the study conception and design. MA and RM organized the database. MS and RM performed the statistical analysis. RM wrote the first draft of the manuscript. MA, SY, LL, and RM wrote sections of the manuscript. All authors contributed to the manuscript revisions, readings, and approved the submitted version.
RM is supported by University of Sorocaba scholarship. The funding source had no part in choosing the topic, in the systematic scoping review or in the decision to submit the article for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.622973/full#supplementary-material
Almeida-Brasil, C. C., Silveira, M. R., Silva, K. R., Lima, M. G., Faria, C., Cardoso, C. L., et al. (2017). Quality of life and associated characteristics: application of WHOQOL-BREF in the context of primary health care. Cien. Saúde Colet. 22, 1705–1716. doi: 10.1590/1413-81232017225.20362015
Alves, C., Coutinho, I., Reis, T., and Mello, R. (2010). Perfil dos pacientes de três residências terapêuticas de um hospital psiquiátrico municipalizado do estado do Rio de Janeiro. Revista de Pesquisa: Cuidado é Fundamental Online. 2, 149–152. doi: 10.9789/2175-5361.rpcfo.v0.848
Amarante, P., and Nunes, M. O. (2018). A reforma psiquiátrica no SUS e a luta por uma sociedade sem manicômios. Cien. Saúde Colet. 23, 2067–2074. doi: 10.1590/1413-81232018236.07082018
American Psychiatric Association (2014). DSM5: Manual diagnóstico e estatístico de transtornos mentais. Nascimento, M.I.C., Machado, P.H., Garcez, R.M., Pizzato, R. and Rosa, S.M.M., translators. Porto Alegre: Artmed.
Angelim, R. C. M., Figueiredo, T. R., Correia, P. P., Bezerra, S. M. M. S., Baptista, R. S., and Abrão, F. M. S. (2015). Avaliação da qualidade de vida por meio do WHOQOL: Análise bibliométrica da produção de enfermagem. Rev. Baiana Enferm. 29, 400–410. doi: 10.18471/rbe.v29i4.11857
Argiles, C. T. L., Kantorski, L. P., Willrich, J. Q., Antonacci, M. H., and Coimbra, V. C. C. (2013). Redes de sociabilidade: construções a partir do serviço residencial terapêutico. Ciênc. Saúde Coletiva. 18, 2049–2058. doi: 10.1590/S1413-81232013000700020
Assunção, A. A., Lima, E. P., and Guimaraes, M. D. (2017). Mental disorders and participation in the labor market: a multicenter national study in Brazil. Cad. Saúde Pública 33:e00166815. doi: 10.1590/0102-311X00166815
Axelsson, E., Lindsäter, E., Ljótsson, B., Andersson, E., and Hedman-Lagerlöf, E. (2017). The 12-item Self-Report World Health Organization Disability Assessment Schedule (WHODAS) 2.0 administered via the internet to individuals with anxiety and stress disorders: a psychometric investigation based on data from two clinical trials. JMIR Ment Health 4:e58. doi: 10.2196/mental.7497
Blog da Saúde (2014). Sorocaba Recebe Primeiro CAPS III, Com Atendimento 24 Horas. Brasília: Ministério da Saúde.
Brasil. (2001). Lei n° 10.216, de 6 de abril de 2001. Dispõe sobre a proteção e os direitos das pessoas portadoras de transtornos mentais e redireciona o modelo assistencial em saúde Mental. Brasília: Diário Oficial da União.
Brasil (2015). Lei n° 13.105, de 16 de março de 2015. Código de processo Civil. Brasília: Diário Oficial da União.
Carlozzi, N. E., Kratz, A. L., Downing, N. R., Goodnight, S., Miner, J. A., Migliore, N., et al. (2015). Validity of the 12-item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) in individuals with Huntington disease (HD). Qual. Life Res. 24, 1963–1971. doi: 10.1007/s11136-015-0930-x
Castro, P. C., Driusso, P., and Oishi, J. (2014). Convergent validity between SF-36 and WHOQOL-BREF in older adults. Rev. Saúde Pública 48, 63–67. doi: 10.1590/S0034-8910.2014048004783
Cortes, H. M., and Barros, S. (2017). Reabilitação psicossocial de moradores de um serviço residencial terapêutico. J.Nurs.Health 7:148. doi: 10.15210/jonah.v7i2.12313
Costa, G. M. d., Pessôa, C. K. L., Soares, C. A., and Rocha, S. A. M. (2014). A importância da família nas práticas de cuidado no campo da Saúde Mental. Cadernos ESP 8, 41–57.
Cruz, L. N., Polanczyk, C. A., Camey, S. A., Hoffmann, J. F., and Fleck, M. P. (2011). Quality of life in Brazil: normative values for the WHOQOL-bref in a southern general population sample. Qual. Life Res. 20, 1123–1129. doi: 10.1007/s11136-011-9845-3
Ćwirlej-Sozańska, A., Sozański, B., Kotarski, H., Wilmowska-Pietruszyńska, A., and Wiśniowska-Szurlej, A. (2020). Psychometric properties and validation of the polish version of the 12-item WHODAS 2.0. BMC Public Health 20:1203. doi: 10.1186/s12889-020-09305-0
Dadalte, A. C., Soares, E. J. P., and Pedrão, L. J. (2017). The residents’ perception about the residential therapeutic services. SMAD Rev. Eletrônica Saúde Ment. Álcool e Drogas. 13, 213–220. doi: 10.11606/issn.1806-6976.v13i4p213-220
Fernandes, M. A., Branco, G. S. C., Costa, A. S., Silva, J. S., and Feitosa, C. D. A. (2017). The relationship between mental health and work: integrated mental health outpatient center study. J. Nurs. UFPE Online 11(Suppl.10) 4191–4198. doi: 10.5205/reuol.10712-95194-3-SM.1110sup201724
Ferrer, M. L. P., Perracini, M. R., Rebustini, F., and Buchalla, C. M. (2019). WHODAS 2.0-BO: normative data for the assessment of disability in older adults. Rev. Saúde Pública 53:19. doi: 10.11606/S1518-8787.2019053000586
Fleck, M. P., Louzada, S., Xavier, M., Chachamovich, E., Vieira, G., Santos, L., et al. (2000). Aplicação da versão em português do instrumento abreviado de avaliação da qualidade de vida “WHOQOL-bref”. Rev. Saúde Pública 34, 178–183. doi: 10.1590/S0034-89102000000200012
França, V. V., Alves, M. P., Silva, A. L. M. A., Guedes, T. G., and Frazão, I. S. (2017). Who are the residents of therapeutic residential services? Profile of de-institutionalized patients with mental disorders. Saúde Debate. 41, 872–884. doi: 10.1590/0103-1104201711416
Gomez, Y. F., Rodriguez, M. A. A., and Lopez, M. I. G. (2017). Personal and macro-systemic factors as predictors of quality of life in chronic schizophrenia. Psicothema 29, 160–165. doi: 10.7334/psicothema2016.179
Hiany, N., Vieira, M. A., Gusmão, R. O. M., and Barbosa, S. F. A. (2018). Perfil Epidemiológico dos Transtornos Mentais na População Adulta no Brasil: uma revisão integrativa. Rev. Enferm. Atual 86:24.
Hudson, C. G. (2019). Deinstitutionalization of mental hospitals and rates of psychiatric disability: an international study. Health Place 56, 79–79.
Lago, E. A., Machado, R. S., Vieira, T. S., and Monteiro, C. F. S. (2014). Profile of residents of therapeutic home services. REUFPI 3, 10–17. doi: 10.26694/reufpi.v3i1.1113
Luciano, J. V., Ayuso-Mateos, J. L., Aguado, J. L., Fernandez, A., Serrano-Blanco, A., Roca, M., et al. (2010). RTehseaerc h1 a2rti-clietem World Health Organization Disability Assessment Schedule II (WHO-DAS II): a nonparametric item response analysis. BMC Med. Res. Methodol. 10:45. doi: 10.1186/1471-2288-10-45
Mas-Exposito, L., Amador-Campos, J. A., Gomez-Benito, J., and Lalucat-Jo, L. (2011). The World Health Organization Quality of life scale brief version: a validation study in patients with schizophrenia. Qual. Life Res. 20, 1079–1089. doi: 10.1007/s11136-011-9847-1
Melo, M. C., Albuquerque, S. G., Luz, J. H., Quental, P. T., Sampaio, A. M., and Lima, A. B. (2015). Perfil clínico e psicossocial dos moradores em hospitais psiquiátricos no estado do Ceará. Brasil. Ciênc. Saúde Coletiva 20, 343–352. doi: 10.1590/1413-81232015202.2062013
Ministério da Saúde (2004). Residências terapêuticas: o que são, para que servem. Brasília: Ministério da Saúde.
Ministério da Saúde (2005). Reforma psiquiátrica e política de saúde mental no Brasil. Documento apresentado à Conferência Regional de Reforma dos Serviços de Saúde Mental: 15 anos depois de Caracas. Brasília: OPAS.
Ministério da Saúde (2014). Portaria n° 2.840, de 29 de dezembro de 2014. Cria o Programa de Desinstitucionalização integrante do componente Estratégias de Desinstitucionalização da Rede de Atenção Psicossocial (RAPS), no âmbito do Sistema Único de Saúde (SUS), e institui o respectivo incentivo financeiro de custeio mensal. Brasília: Diário Oficial da União.
Mohandoss, A. A. (2017). Quality of life in schizophrenic patients: Comparative study from South India. J. Dr. NTR Univ. Health Sci. 6:224. doi: 10.4103/2277-8632.221523
Pan American Health Organization (2018). The Burden of Mental Disorders in the Region of the Americas, 2018. Washington, DC: PAHO.
Passos, E., Palombini, A. d. L., Campos, R. O., Rodrigues, S. E., Melo, J., Maggi, P. M., et al. (2013). Autonomia e cogestão na prática em saúde mental: o dispositivo da gestão autônoma da medicação (GAM). Aletheia 41, 24–38.
Passos, R. G., and Portugal, S. (2015). Breve balanço da política de saúde mental: análise comparativa Brasil e Portugal a partir da experiência das residências terapêuticas. R. Pol. Públ. 19, 91–102. doi: 10.18764/2178-2865.v19n1p91-102
Pedroso, B., Pilatti, L. A., Gutierrez, G. L., and Picinin, C. T. (2010). Cálculo dos escores e estatística descritiva do WHOQOL-bref através do Microsoft Excel. Rev. Bras. Qualidade Vida 2, 31–36. doi: 10.3895/s2175-08582010000100004
Picco, L., Lau, Y. W., Pang, S., Jeyagurunathan, A., Vaingankar, J. A., Abdin, E., et al. (2018). Predictors of general functioning and correlates of quality of life: a cross-sectional study among psychiatric outpatients. Ann. Acad. Med. Singapore 47, 3–12.
Pinho, L. M. G., Pereira, A. M. S., and Chaves, C. (2018). Quality of life in schizophrenic patients: the influence of sociodemographic and clinical characteristics and satisfaction with social support. Trends Psychiatry Psychother. 40, 202–209. doi: 10.1590/2237-6089-2017-0002
Portugal, F. B., Campos, M. R., Gonçalves, D. A., Mari, J. J., and Fortes, S. L. C. L. (2016). Qualidade de vida em pacientes da atenção primária do Rio de Janeiro e São Paulo, Brasil: associações com eventos de vida produtores de estresse e saúde mental. Ciênc. Saúde Coletiva 21, 497–508. doi: 10.1590/1413-81232015212.20032015
Prefeitura de Sorocaba (2019). Sorocaba completa um ano do fechamento de hospitais psiquiátricos na cidade. Available online at: https://agencia.sorocaba.sp.gov.br/sorocaba-completa-um-ano-do-fechamento-de-hospitais-psiquiatricos/ accessed June 4, 2020.
Sampaio, M. L., and Bispo Júnior, J. P. (2021). Entre o enclausuramento e a desinstitucionalização: a trajetória da saúde mental no Brasil. Trabalho Educação e Saúde 19:e00313145. doi: 10.1590/1981-7746-sol00313
Santos, N. M., Silva, E. R. M., Santos Filho, J. N. B., and Câmara, J. J. C. (2015). Práticas e estratégias de reinserção na sociedade de um Serviço Residencial Terapêutico em São Luís. Maranhão. Rev. Pesq. Saúde. 16, 71–74.
Shen, G. C., and Snowden, L. R. (2014). Institutionalization of deinstitutionalization: a cross-national analysis of mental health system reform. Int J Ment Health Syst 8:47. doi: 10.1186/1752-4458-8-47
Silva, S. L. C., and Rosa, L. C. S. (2015). “Residências Terapêuticas: uma política pública como expressão da luta antimanicomial,” in VII Jornada Internacional Políticas Públicas (São Luís: Universidade Federal do Maranhão).
Silveira, C., Parpinelli, M. A., Pacagnella, R. C., Camargo, R. S., Costa, M. L., Zanardi, D. M., et al. (2013). Cross-cultural adaptation of the World Health Organization Disability Assessment Schedule (WHODAS 2.0) into Portuguese. Rev. Assoc. Med. Bras. 59, 234–240. doi: 10.1016/j.ramb.2012.11.005
Skevington, S. M., and Epton, T. (2018). How will the sustainable development goals deliver changes in well-being? A systematic review and meta-analysis to investigate whether WHOQOL-BREF scores respond to change. BMJ Glob. Health. 3(Suppl. 1):e000609. doi: 10.1136/bmjgh-2017-000609
Souza, L. A., and Coutinho, E. S. F. (2006). Fatores associados à qualidade de vida de pacientes com esquizofrenia. Rev. Bras. Psiquiatr. 28, 50–58. doi: 10.1590/S1516-44462006000100011
Sum, M. Y., Tay, K. H., Sengupta, S., and Sim, K. (2018). Neurocognitive functioning and quality of life in patients with and without deficit syndrome of schizophrenia. Psychiatry Res. 263, 54–60. doi: 10.1016/j.psychres.2018.02.025
The WHOQOL Group (1996). WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment. Geneva: WHO.
Thornicroft, G., and Bebbington, P. (1989). Deinstitutionalisation–from hospital closure to service development. Br. J. Psychiatry 155, 739–753. doi: 10.1192/bjp.155.6.739
Trape, T. L., and Campos, R. O. (2017). The mental health care model in Brazil: analyses of the funding, governance processes, and mechanisms of assessment. Rev. Saúde Pública 51:19. doi: 10.1590/S1518-8787.2017051006059
Vandenbroucke, J. P., von Elm, E., Altman, D. G., Gotzsche, P. C., Mulrow, C. D., Pocock, S. J., et al. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann. Intern. Med. 147, W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1
Venancio, S. I. (2017). “Desenhos de estudos epidemiológicos,” in Avaliação de Tecnologias de Saúde & Políticas Informadas por Evidências, eds T. S. Toma, T. V. Pereira, T. Vanni, and J. O. M. Barreto (São Paulo: Instituto de Saúde), 51–68.
Wang, X. Q., Petrini, M. A., and Morisky, D. E. (2017). Predictors of quality of life among Chinese people with schizophrenia. Nurs. Health Sci. 19, 142–148. doi: 10.1111/nhs.12286
World Health Organization (1994). International Classification of Diseases and Related Health Problems: ICD-10. Geneva: WHO.
World Health Organization (2001). The World health report 2001. Mental health: New Understanding, New Hope. Geneva: WHO.
World Health Organization (2007). International Classification of Functioning, Disability and Health: Children & Youth Version: ICF-CY. Geneva: WHO.
World Health Organization (2010). Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. Geneva: WHO.
World Health Organization and the Gulbenkian Global Mental Health Platform (2014). Innovation in deinstitutionalization: a WHO expert survey. Geneva: WHO.
Keywords: mental health, quality of life, disability evaluation, deinstitutionalization, assisted living facilities
Citation: Mayer RCF, Alves MR, Yamauti SM, Silva MT and Lopes LC (2021) Quality of Life and Functioning of People With Mental Disorders Who Underwent Deinstitutionalization Using Assisted Living Facilities: A Cross-Sectional Study. Front. Psychol. 12:622973. doi: 10.3389/fpsyg.2021.622973
Received: 29 October 2020; Accepted: 19 April 2021;
Published: 25 May 2021.
Edited by:
Roberto Cattivelli, Istituto Auxologico Italiano (IRCCS), ItalyReviewed by:
Gioia Mura, University of Cagliari, ItalyCopyright © 2021 Mayer, Alves, Yamauti, Silva and Lopes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luciane Cruz Lopes, bHVjaWFuZS5sb3Blc0Bwcm9mLnVuaXNvLmJy
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.