
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol., 03 May 2021
Sec. Psycho-Oncology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.621850
This article is part of the Research TopicUncertainty, Anxiety, and Fear of Cancer RecurrenceView all 26 articles
 Kate Anderson1,2*
Kate Anderson1,2* Allan ‘Ben' Smith3
Allan ‘Ben' Smith3 Abbey Diaz1,2
Abbey Diaz1,2 Joanne Shaw4
Joanne Shaw4 Phyllis Butow4
Phyllis Butow4 Louise Sharpe4
Louise Sharpe4 Afaf Girgis3
Afaf Girgis3 Sophie Lebel5
Sophie Lebel5 Haryana Dhillon4
Haryana Dhillon4 Linda Burhansstipanov6
Linda Burhansstipanov6 Boden Tighe1,2
Boden Tighe1,2 Gail Garvey1,2
Gail Garvey1,2While cancer survivors commonly experience fear and anxiety, a substantial minority experience an enduring and debilitating fear that their cancer will return; a condition commonly referred to as fear of cancer recurrence (FCR). Despite recent advances in this area, little is known about FCR among people from Indigenous or other ethnic and racial minority populations. Given the high prevalence and poor outcomes of cancer among people from these populations, a robust understanding of FCR among people from these groups is critical. The current review identified and aggregated existing literature on FCR amongst adult cancer survivors from Indigenous and minority populations. The protocol of this review was registered with PROSPERO in July 2020 (Registration number: CRD42020161655). A systematic search of bibliographic databases was conducted for relevant articles published from 1997 to November 2019. Data from eligible articles were extracted and appraised for quality by two independent reviewers. Nineteen articles from four countries (United States of America, Canada, Australia and the United Kingdom) met the inclusion criteria, including 14 quantitative, 4 qualitative and 1 mixed-methods study. Only one article reported on an Indigenous population. Few studies reported on FCR prevalence (n = 3) or severity (n = 9). While the variation in tools used to measure FCR hindered a robust estimate of severity, results suggested some differences in FCR severity between minority and dominant populations, although these may have been due to study metholodological differences. Few factors were reported as being associated with FCR in minorities across multiple studies. The qualitative synthesis found five themes associated with the lived experience of FCR: (i) variations in the lived experience of FCR; (ii) spirituality and worldview impacting on FCR; (iii) the importance of staying positive; (iv) complexities around support; and (v) increasing cancer knowledge. The findings of this review highlight differences in FCR across cultures and contexts, which reinforces the need for culturally-specific approaches to this condition. The dearth of research in this area is of concern given the significant burden of cancer in these populations. A deeper understanding of this condition among Indigenous and minority populations is critical to developing and delivering appropriate and effective psychosocial care for cancer survivors from these groups. Systematic Review Registration: identifier [CRD42020161655].
Increasing clinical and research attention over the past two decades has produced a growing evidence base around fear of cancer recurrence (FCR) in people with different cancer types and from diverse populations including some vulnerable groups (Thewes et al., 2012a; Crist and Grunfeld, 2013; Koch et al., 2013; Simard et al., 2013; Almeida et al., 2019). FCR is defined as “the fear, worry or concern relating to the possibility that cancer will come back or progress” (Lebel et al., 2016). While some degree of FCR is considered a normal response to the experience of having cancer, estimates suggest that 40–70% of cancer survivors experience a level of FCR that is enduring and debilitating (Thewes et al., 2012a). FCR is associated with varied adverse outcomes in cancer survivors, including: psychological distress; impaired social functioning, and coping with work; reduced quality of life and level of enjoyment; and increased healthcare usage and costs (Avis et al., 2005; Hodges and Humphris, 2009; Lebel et al., 2013; Otto et al., 2018). Moreover, cancer survivors identify FCR as one of their major concerns (Simard et al., 2013).
Several factors are associated with a higher prevalence of FCR, including: younger age; female gender; greater burden of physical symptoms; and psychological factors (Härtl et al., 2003; Simard et al., 2013). Progress has also been made in screening for and assessing FCR (Simard and Savard, 2009), as well as in the development of psychological interventions to reduce FCR, which have been demonstrated to be effective predominantly in patients with early stage cancers treated with curative intent (Sharpe et al., 2017; Hall et al., 2018; Butow et al., 2019; Tauber et al., 2019). Despite these advances, little is known about FCR among cancer survivors from Indigenous, ethnic and racial minority populations and it is unclear whether existing programs and interventions aimed at reducing FCR are appropriate or effective for cancer survivors from these groups. This is surprising, given that cancer is a leading cause of illness and death among many Indigenous populations (United Nations Permanent Forum on Indigenous Issues, 2009; de Souza et al., 2016), and minority populations experience significantly poorer cancer outcomes than other groups with respect to risk factor prevalence, cancer incidence, stage at diagnosis and disease outcomes (United Nations Permanent Forum on Indigenous Issues, 2009; de Souza et al., 2016; Wild et al., 2020), including psychosocial outcomes (Garvey et al., 2020).
Indigenous peoples are recognized as the original inhabitants of a country or geographical region and are known as First Peoples or in some countries by more specific terms such as “Native American” in the US, “First Nations” in Canada, and “Aboriginal” and “Torres Strait Islander” in Australia. While there are no globally agreed definitions, the United Nations describes Indigenous peoples as “inheritors and practitioners of unique cultures and ways of relating to people and the environment. They have retained social, cultural, economic, and political characteristics that are distinct from those of the dominant societies in which they live” (United Nations, 2020). Similarly, definitions of ethnic and racial minorities are manifold, however, the terms generally refer to ethnic or racial groups in a given country in which they are in a non-dominant position in relation to the dominant population (United Nations, 1992). While there are clear and important distinctions between Indigenous peoples and ethnic and other racial minority populations (hereon respectfully referred to as a collective as IM populations), these groups similarly experience significant disparities in cancer outcomes and share many barriers to accessing and engaging with cancer care (United Nations Permanent Forum on Indigenous Issues, 2009; de Souza et al., 2016).
The current review aimed to explore the following questions:
1. What is the prevalence and severity of FCR among IM populations? Are there differences between IM and dominant populations?
2. What demographic, clinical, social and psychological factors are associated with FCR in IM populations?
3. What are the lived experiences of FCR among IM populations?
The establishment of an evidence base in this specific area will facilitate the evaluation and tailoring of programs and interventions to reduce FCR for cancer survivors from IM populations.
A protocol for this systematic review was published on the PROSPERO: International prospective register of systematic reviews website in July 2020 [Registration number: CRD42020161655].
The search aimed to identify peer-reviewed literature reporting new empirical data from qualitative, quantitative and mixed-methods studies with a focus on FCR in one or more IM population. The search strategy adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009). The literature search included studies published between 1997 and November 2019. Articles published in scientific journals were identified by searching the bibliographic databases CINAHL, EMBASE, PsycINFO, and PubMed. The search aimed to identify any paper about FCR in adults (18 years or older) from IM populations who have been diagnosed with cancer. There was no restriction on cancer type, cancer stage, time since diagnosis, treatment type, or country/region of residence (see Appendix A for a detailed description of the search strategy).
The search string for Indigenous populations was adapted from a previously published systematic review of Indigenous populations (Angell et al., 2016). The search string for minority populations was adapted from a previously published systematic reviews of minority populations (Dawson et al., 2018).
Studies were included if they were: peer-reviewed; published in English; published from 1997 (this start date was chosen as FCR research began to emerge in the literature from this date) to November 2019; report original data from quantitative, qualitative or mixed method studies; involve cancer survivors; and report on the experiences of FCR and/or measures of FCR (e.g., mean FCR score; proportion of participants reporting any/high levels of FCR) separately for at least one IM population, as identified below. All eligible articles were included in the review regardless of quality assessment rating.
Studies were excluded if they were: systematic reviews, meta- and pooled- analyses, reported relative measures only, case studies, case series, commentary, editorial and other opinion papers, even if peer-reviewed; books or book chapters, narrative reviews, conference abstracts, dissertations, and other gray literature; published in languages other than English; or published prior to 1997.
All citations identified in the search were downloaded into Rayyan Online Software (Ouzzani et al., 2016). After removal of duplicates, the titles and abstracts were screened separately by two independent reviewers (KA and HH). Reference lists of systematic reviews found in the search were screened to identify other relevant articles for the review. Reviewers resolved disagreements through discussion and evaluation against inclusion/exclusion criteria. Full-text records were retrieved for studies that could not be excluded based on title and abstract alone.
Data extraction was completed by three authors (KA, ABS, and AD), which included: publication information (authors, year of publication, country, region); participant characteristics [IM population(s), cancer type, total number of participants, number of participants per IM group, age, sex]; study characteristics (study design; data collection method, study setting). Study outcomes for the quantitative studies and relevant findings of mixed methods papers were extracted by one author (AD) [FCR measure/s used, statistical tests used, proportion, mean, standard deviation (SD), range, effect size, clinically significant cut offs]. Qualitative and mixed methods papers were imported into NVivo 12 (NVivo qualitative data analysis software; QSR International Pty Ltd. Version 12, 2018) for coding and aggregation by one author (KA).
Three authors (KA, ABS, and BT) conducted a critical appraisal of the included articles using the Mixed Methods Appraisal Tool (MMAT) VERSION 2018 (Hong et al., 2018). An overall score out of five was calculated for each article, by tallying how many quality criteria each study was determined to have met.
The quantitative and qualitative syntheses were conducted and presented separately, with the relevant components of any identified mixed methods studies presented in both. Two authors (ABS and AD) synthesized the quantitative data regarding the prevalence, severity, and associated factors of FCR among cancer survivors from IM populations compared to dominant populations (review questions 1 and 2). A meta-synthesis of the qualitative data relating to the lived experiences of FCR among cancer survivors from IM populations was conducted by one author (KA).
Of the 304 records retrieved, 302 were identified in the search and two were identified through a handsearch. From these, 108 duplicates were removed, and 197 records were screened by title and abstract. Of those screened by title and abstract, 136 full-text articles were assessed for eligibility, and 19 records were subsequently considered eligible for inclusion (see Figure 1).
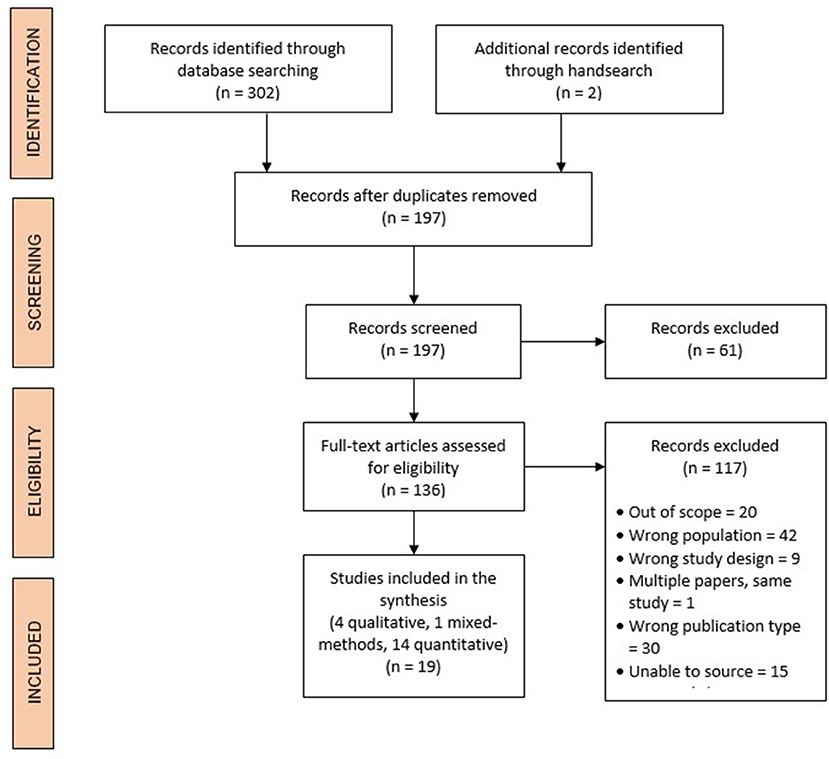
Figure 1. Study selection and PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
A total of 19 studies met inclusion criteria (Braun et al., 2002; Ashing-Giwa et al., 2004; Gill et al., 2004; Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011, 2016; Liu et al., 2011; Pandya et al., 2011; Bache et al., 2012; Taylor et al., 2012; Butow et al., 2013; Singh-Carlson et al., 2013; Best et al., 2015; Sam, 2016; Ashing et al., 2017; Nápoles et al., 2017; Cho et al., 2018; McMullen et al., 2019). Sixteen studies were conducted in the United States (Braun et al., 2002; Ashing-Giwa et al., 2004; Gill et al., 2004; Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011, 2016; Liu et al., 2011; Pandya et al., 2011; Taylor et al., 2012; Best et al., 2015; Sam, 2016; Ashing et al., 2017; Nápoles et al., 2017; Cho et al., 2018; McMullen et al., 2019), one in Australia (Butow et al., 2013), Canada (Singh-Carlson et al., 2013) and the United Kingdom (Bache et al., 2012). Fourteen studies were quantitative (Gill et al., 2004; Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011, 2016; Liu et al., 2011; Pandya et al., 2011; Taylor et al., 2012; Butow et al., 2013; Best et al., 2015; Sam, 2016; Ashing et al., 2017; Cho et al., 2018; McMullen et al., 2019), four were qualitative (Braun et al., 2002; Ashing-Giwa et al., 2004; Bache et al., 2012; Singh-Carlson et al., 2013) and one was mixed-methods (Nápoles et al., 2017). One study included participants from an Indigenous population (Native Hawaiian) (Braun et al., 2002) and all other studies included participants who identified as belonging to one or more minority populations [Latino = 7 (Janz et al., 2011, 2016; Pandya et al., 2011; Sam, 2016; Ashing et al., 2017; Nápoles et al., 2017; McMullen et al., 2019), African American = 11, (Gill et al., 2004; Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011, 2016; Pandya et al., 2011; Taylor et al., 2012; Best et al., 2015; Sam, 2016; McMullen et al., 2019). Asian American = 4 (Ashing-Giwa et al., 2004; Ashing et al., 2017; Cho et al., 2018; McMullen et al., 2019) and unspecified “non-White” = 1 (Liu et al., 2011) in the United States; first-generation immigrants from various ethnic groups = 1 (Butow et al., 2013) in Australia; South Asian = 1 (Singh-Carlson et al., 2013) in Canada; and African and Black Caribbean = 1 (Bache et al., 2012) in the United Kingdom]. Eleven studies included only breast cancer survivors (Ashing-Giwa et al., 2004; Gill et al., 2004; Janz et al., 2011, 2016; Liu et al., 2011; Taylor et al., 2012; Singh-Carlson et al., 2013; Ashing et al., 2017; Nápoles et al., 2017; Cho et al., 2018); one study each included gynecological (Sam, 2016); colorectal (McMullen et al., 2019); and prostate cancer survivors (Krupski et al., 2005); and five studies included cancer survivors with multiple cancer types (Braun et al., 2002; Deimling et al., 2006; Bache et al., 2012; Butow et al., 2013; Best et al., 2015). The detailed characteristics of the included studies are presented in Table 1 (quantitative studies), Table 2 (qualitative and mixed methods studies). Most quantitative studies used a relevant sampling strategy (12/15) and appropriate statistical analysis (13/15). It was unclear whether the sample was representative of the target population in 10/15 studies, risk of non-response bias was high in 7/15 studies, and only 7/15 studies used a validated FCR measure (see Appendix B for results of the quality appraisal).
Seven studies reported FCR prevalence for IM populations (see Table 3) (Pandya et al., 2011; Taylor et al., 2012; Janz et al., 2016; Ashing et al., 2017; Nápoles et al., 2017; McMullen et al., 2019). The prevalence of FCR ranged widely, from 14% (8/57) of Non-Hispanic Black breast cancer survivors who were 4 years post-diagnosis (Janz et al., 2016) to 67% (34/51) of African American breast cancer survivors at on average 7 years post cancer diagnosis (Taylor et al., 2012) and 67% (20/30) of Hispanic leukemia survivors (Pandya et al., 2011).
Three studies compared FCR prevalence in minority cancer populations to their Non-Hispanic White/Caucasian counterparts (Pandya et al., 2011; Janz et al., 2016; McMullen et al., 2019), although only two reported FCR prevalence by specific minority group (Pandya et al., 2011; Janz et al., 2016). In these studies, FCR was reported by a greater proportion of Hispanic/Latina people with cancer [Leukemia: (Pandya et al., 2011) 67%; Breast cancer: (Janz et al., 2016) 37% in high acculturated Latina and 50% in low acculturated Latina] than their Non-Hispanic White counterparts [Leukemia 30%; (Pandya et al., 2011). Breast Cancer: (Janz et al., 2016) 27%] (Table 3). Conversely, Janz et al. reported less FCR in Non-Hispanic Black breast cancer survivors compared to Non-Hispanic White breast cancer survivors (14.0 vs. 27.1%) (Janz et al., 2016). While Pandya et al. reported a higher prevalence of FCR in African American than Caucasian Leukemia patients (40 vs. 30%); it is important to note that this study only recruited five African American people (Pandya et al., 2011).
FCR was the most prevalent health/lifestyle concern, emotional concern or symptom among colorectal cancer survivors (McMullen et al., 2019), among Latina breast cancer survivors (Nápoles et al., 2017), and was the highest unmet supportive care need among a mixed sample of immigrant IM cancer survivors (Butow et al., 2013).
Nine studies reported on the severity of FCR for IM populations (Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011; Liu et al., 2011; Taylor et al., 2012; Best et al., 2015; Sam, 2016; Ashing et al., 2017; Cho et al., 2018), while one reported on the mean number of triggers of FCR experienced (Gill et al., 2004). FCR was often measured using purpose-designed items, often a single item, making judgements regarding severity difficult, although most mean scores were in the low/moderate range (Table 3). Several studies used the Concerns About Recurrence Scale (CARS) with mean scores ranging from 2.00 (SD = 1.35) in “Non-white” early stage breast cancer survivors (Liu et al., 2011) to 2.65 out of 6.00 (SD = 1.44) in African American breast cancer survivors (Taylor et al., 2012).
Assessment of FCR in distinct IM groups indicate that Hispanic people may experience more severe FCR compared to non-Hispanic Whites. This was observed in older long-term cancer survivors from several cancer groups (Deimling et al., 2006) and survivors of breast cancer (Janz et al., 2011), however no difference was observed between Hispanic and non-Hispanic White non-metastatic prostate cancer survivors (Krupski et al., 2005). In contrast, non-Hispanic Black cancer survivors experienced similar (Best et al., 2015) or less severe (Krupski et al., 2005; Deimling et al., 2006; Janz et al., 2011). FCR compared to non-Hispanic White cancer survivors. One study found Chinese American women reported significantly lower FCR than “other Asian” American women (M = 2.76 years post-diagnosis) (Ashing et al., 2017).
Two studies assessed longitudinal changes in FCR (Janz et al., 2016; Ashing et al., 2017). Higher FCR levels in Hispanic vs. non-Hispanic women 9 months after a breast cancer diagnosis were still evident 4 years post-diagnosis (Janz et al., 2016). Similarly, higher levels of FCR among non-Chinese vs. Chinese Asian-American breast cancer survivors were still evident 1 year post-baseline (Ashing et al., 2017).
Factors associated with FCR in cancer patients and survivors from minority populations were explored in six studies (Taylor et al., 2012; Butow et al., 2013; Best et al., 2015; Sam, 2016; Ashing et al., 2017; Cho et al., 2018).
Few consistent relationships emerged between minority peoples' FCR and their demographic or clinical characteristics. Associations with age were assessed in four studies (Taylor et al., 2012; Best et al., 2015; Sam, 2016; Ashing et al., 2017). Age was not associated with FCR in Asian-American breast cancer survivors (Ashing et al., 2017) or overall FCR in African American breast cancer survivors (Taylor et al., 2012), but was negatively correlated with FCR health worries, role worries and death worries domains (Taylor et al., 2012). Age was also negatively correlated with FCR in a heterogenous group of non-White cancer survivors, more so than in Whites (Sam, 2016). Longer time since diagnosis was associated with lower FCR in African American breast cancer survivors (Taylor et al., 2012), but not African Americans with a mix of cancer types (Best et al., 2015) or Non-white gynecological cancer survivors (Sam, 2016). More advanced cancer stage was associated with higher FCR in minority peoples with breast cancer (Ashing et al., 2017), but not in a mixed sample of cancer survivors (Best et al., 2015).
Various aspects of minority peoples' perceptions of their illness and its treatment were found to be associated with FCR, although no factors were identified in more than one study. There were a few notable differences in relationships between FCR and psychological variables in White vs. non-White people. Best et al. found a significant negative association between meaning and FCR in African American survivors but not in non-African American survivors (Best et al., 2015). Gill et al. found that African American breast cancer survivors were less likely than other survivors to have FCR triggered by external factors, namely hearing about somebody else's cancer, environmental triggers or cancer-related media coverage or controversy (Gill et al., 2004). In Australian immigrant minority cancer survivors, more severe unmet FCR-related needs were significantly associated with the need for an interpreter and poorer understanding of the healthcare system (Butow et al., 2013). Among Asian Americans, greater healthcare satisfaction predicted lower subsequent FCR (Ashing et al., 2017). FCR was also found to mediate the impact of pain interference and fatigue on emotional wellbeing (i.e., greater pain interference and fatigue were associated with higher FCR, which was further related to poorer emotional wellbeing) in Chinese American breast cancer survivors (Cho et al., 2018).
Several studies found that minority peoples' FCR was associated with worse psychological distress (Butow et al., 2013; Sam, 2016), physical, emotional, functional quality of life and breast cancer specific quality of life (Taylor et al., 2012; Butow et al., 2013; Ashing et al., 2017). Two studies compared outcomes of FCR across minority and dominant populations (Butow et al., 2013; Sam, 2016). FCR and psychological distress demonstrated positive correlations that were moderate in “non-white” and strong in “white” gynecological cancer survivors (Sam, 2016). FCR-related unmet needs and worse anxiety, depression and quality of life were strongly correlated in immigrant Arabic cancer survivors, and moderately correlated in Anglo-Australian and immigrant Chinse and Greek cancer survivors (Butow et al., 2013).
Of the four qualitative studies (Braun et al., 2002; Ashing-Giwa et al., 2004; Bache et al., 2012; Singh-Carlson et al., 2013) and one mixed-method study (Nápoles et al., 2017) in this review, two were from the USA [California (Ashing-Giwa et al., 2004) and Hawaii] (Braun et al., 2002), one from Canada (British Columbia) (Singh-Carlson et al., 2013) and one from the UK (London) (Bache et al., 2012). The Hawaiian study was the only study in the review that reported on Indigenous participants (Braun et al., 2002). The meta-synthesis undertaken on the qualitative findings reported in these papers revealed five synthesized findings around the lived experience of FCR: (i) variations in the lived experience of FCR; (ii) spirituality and worldview impacting on FCR; (iii) the importance of staying positive and not dwelling on illness; (iv) complexities around family and community support; and (v) increasing cancer knowledge. These synthesized findings are described below, and the meta-synthesis is presented with illustrative quotes in Table 4.
There were some accounts from cancer survivors from IM populations in these studies about their experiences of FCR, which were contrasted against the experiences of relevant dominant populations and/or other IM groups. Many survivors detailed their experiences of fear, suspense, anxiety and sadness about the thought of their cancer returning (Ashing-Giwa et al., 2004; Singh-Carlson et al., 2013).
Ashing-Giwa et al. found that while cancer survivors from dominant populations in the USA expressed concerns about recurrence associated with incapacitation and loss of autonomy, survivors from African American, Asian American and Latina populations were more concerned about their ability to care for their family if their cancer returned (Ashing-Giwa et al., 2004). Moreover, Ashing-Giwa et al. and Napoles et al. both found that cancer survivors from IM populations in the USA were more likely than dominant populations to experience FCR when obtaining follow up care, including check-ups and mammograms (Ashing-Giwa et al., 2004; Nápoles et al., 2017).
Singh-Carlson et al. found that among female cancer survivors from South Asian populations in Canada, younger women commonly experienced FCR relating to uncertainty around their future, whereas for middle-aged women the FCR centered around what would happen to their children, and older women were not troubled by FCR (Singh-Carlson et al., 2013).
Singh-Carlson et al. reported that IM survivors in Canada were prone to experiencing FCR when hearing stories about other people who are dying from cancer (Singh-Carlson et al., 2013). Ashing-Giwa et al. also found that physical sensations of pain and dizziness were also triggering for FCR among survivors from IM populations in the USA (Ashing-Giwa et al., 2004).
Cancer survivors from IM populations reported spiritual and/or fatalistic beliefs regarding the outcomes of their cancer and their future, which were identified as pivotal in moderating survivors' FCR and fostering psychological adjustment to uncertainties of life after cancer (Braun et al., 2002; Ashing-Giwa et al., 2004; Bache et al., 2012; Singh-Carlson et al., 2013). Across the studies, God was commonly described by cancer survivors from IM populations as a source of comfort and as the ultimate decider of one's fate (Bache et al., 2012). Additionally, participation in religious practices, such as attending church services and religious support groups, provided emotional support and distraction, which strengthened cancer survivors' ability to cope with their illness (Bache et al., 2012). Ashing-Giwa et al. found that Asian American survivors relied on their personal sense of faith in managing their fear, African American survivors relied heavily on their prayers and support from their faith community, and Latino-American survivors relied on a combination of faith, prayers and support from their faith community (Ashing-Giwa et al., 2004).
Singh-Carlson et al. found that South Asian cancer survivors in Canada demonstrated a quiet acceptance of their cancer experience (Singh-Carlson et al., 2013). This was regarded as reflective of Eastern spiritual beliefs that discourage fighting against suffering and discomfort and instead encourage acceptance and endurance of one's negative experiences (Singh-Carlson et al., 2013). The authors found that among South Asian cancer survivors, belief in faith and karma were commonly reported to moderate apprehension and reduce fear about their cancer returning (Singh-Carlson et al., 2013).
Similarly, Braun et al. found that Native Hawaiian cancer survivors expressed fatalistic views regarding the outcomes of their cancers, which was thought to foster acceptance and likely reduce FCR (Braun et al., 2002). Ashing-Giwa et al. found that many of the African American survivors drew emotional strength from the long legacy of resilience and survivorship in the history of African Americans (Ashing-Giwa et al., 2004).
Several of the studies in this review found that cancer survivors from IM populations expressed beliefs that maintaining a positive attitude and not dwelling on one's illness are important factors, not just in coping with FCR, but also in overcoming their cancer.
Ashing-Giwa et al. found that a common belief shared across cultural groups was that accepting their illness, but not dwelling on it, was important for coping with cancer (Ashing-Giwa et al., 2004). In order to avoid ruminating on their cancer, older and/or newly emigrated cancer survivors from IM populations, who were often reluctant to seek psychosocial support, distracted themselves from emotional overwhelm with household duties (Ashing-Giwa et al., 2004). Bache et al. also found this to be the case among cancer survivors from IM populations in the United Kingdom (Bache et al., 2012). Survivors attributed emotional and physical resilience to maintaining a positive outlook; and that over-contemplation of illness was thought to accelerate the progression of the cancer (Bache et al., 2012). The researchers postulate that the common avoidance of contemplating cancer, which can lead to missing check-ups and screening and increasing late-detection of cancers, might also be an important component in psychological resilience and a defense against FCR (Bache et al., 2012).
Braun et al. found that many Native Hawaiian cancer survivors had relatives who had died of cancer, which occasioned increased FCR for those people (Braun et al., 2002). This made it difficult to stay positive and some participants took issue with the word recovery, as they said: “You never know. once you get cancer, you might get a recurrence or you might get cancer somewhere else” (Braun et al., 2002).
Asian and Latina cancer survivors in Ashing-Giwa et al.'s study reported a reliance on inner strength and an emotional response of displacement (e.g., focusing their energy on their families and their household responsibilities) to cope with fear and anxiety around their cancer (Ashing-Giwa et al., 2004). This contrasted with the Caucasian survivors who predominantly drew on a sense of personal empowerment, individual responsibility and knowledge as their source of resiliency (Ashing-Giwa et al., 2004).
While family and community were identified across the studies as providing critical support for cancer survivors from IM backgrounds to cope with their cancer experiences, there were also commonly identified stressors associated with these relationships.
Two of the included studies reported African American cancer survivors often found strength and emotional support in family and church communities to cope emotionally with their cancer (Ashing-Giwa et al., 2004; Bache et al., 2012). However, Singh-Carlson et al. found that South Asian cancer survivors were ambivalent about receiving emotional support from family and community (Singh-Carlson et al., 2013). The common stigma around cancer in their communities and the prevalent view of cancer as a death-sentence meant that survivors from IM populations were often unwilling to disclose their cancer diagnosis to family and community (Singh-Carlson et al., 2013). This occasioned feelings of isolation and depression among survivors, which heightened rumination and FCR. People who sought support from other cancer survivors had improved hounsla (morale) and increased hope for the future (Singh-Carlson et al., 2013).
While support from family was important for many cancer survivors, some studies reported cancer survivors felt great pressure from their families to be positive and well, as they were relied upon to be the traditional caregiver in the family (Braun et al., 2002; Ashing-Giwa et al., 2004; Singh-Carlson et al., 2013). Two studies reported that family and community members did not want to discuss the illness or the survivor's experience with them, and the survivor felt isolated and unsupported (Ashing-Giwa et al., 2004; Singh-Carlson et al., 2013). Braun et al. also found that Native Hawaiian cancer survivors reported stigma and shame around a cancer diagnosis, which caused some people to hide their diagnosis (Braun et al., 2002). These pressures on cancer survivors to not express their negative thoughts and emotions about their cancer to family members sometimes intensified cancer survivors' rumination and FCR.
While the involvement of family and community members occasioned complex and often competing emotional issues, support groups were described by some cancer survivors from IM populations as important to emotionally cope with their illness. Ashing-Giwa et al. reported that these groups offered survivors support via a shared understanding of the experience with other survivors, a lack of pressure to suppress fears and negative feelings, and the stories of survival from cancer providing hope (Ashing-Giwa et al., 2004). These opportunities to share gave survivors some relief from their anxieties and accounts of good cancer outcomes on which they could reflect.
For some survivors from IM populations, increasing their knowledge about cancer was seen as important in coping and managing FCR—for some people this was via biomedical knowledge and for others it was via traditional medicines and knowledge. Ashing-Giwa et al. found that some cancer survivors relied on alternative medicine and word of mouth rather than rather than Western doctors' recommendations (Ashing-Giwa et al., 2004). Asian American survivors reported that being informed about their illness and maintaining their treatment regimen was beneficial to their recovery from cancer (Ashing-Giwa et al., 2004). Similarly, Bache et al. found that some cancer survivors from IM populations reduced their anxiety by increasing their knowledge about cancer—although it was not known whether such knowledge was philosophically, socially or biomedically based (Bache et al., 2012).
The findings of this review highlight diversity in FCR across different IM populations, which might reflect measurement differences, as well as underlying group differences. While this review found some evidence that FCR might be less prevalence in IM populations that other populations, the lack of culturally-specific FCR measures could account for this apparent difference. The current findings also reveal variability in the factors associated with FCR across IM populations, as well as differences in the lived experience of FCR between different IM populations. Most notably, the findings of our review underscore the paucity of research investigating FCR in IM populations, particularly around the reasons for the varying experiences and outcomes of FCR in minority populations and the near absence of such research for Indigenous populations.
The quantitative synthesis found few consistencies across studies in terms of methods for assessing FCR. The most commonly used validated tool was the Concerns About Recurrence Scale (CARS) (Vickberg, 2003), whilst others used purpose-designed items. There have been no attempts to develop culturally appropriate measures or to validate existing measures of FCR for any IM populations in these studies. It is notable that the FCRI (Simard and Savard, 2009), which is considered one of the most psychometrically sound FCR measures and has been validated in several different languages (Thewes et al., 2012b), was not used in any of these studies.
The prevalence of FCR in IM populations across the studies ranged from 14 to 67%, which is lower than that reported more broadly (39–97%), but still suggests a substantial proportion of IM cancer survivors suffer from FCR (Simard et al., 2013). Direct comparisons of FCR levels between IM groups and dominant groups were limited, but there was some evidence suggesting higher FCR in Hispanic and lower FCR in African American people compaired with non-Hispanic whites. However, differences between IM and dominant groups were not consistent across studies, which could be due to the different tools used to measure FCR (and lack of validation in IM populations), different ways of grouping ethnicities and races for comparison, different countries and contexts, and different cancer types.
Few consistent relationships were evident between IM populations' FCR and their demographic or clinical characteristics, which is consistent with the FCR literature generally (Smith et al., 2018). There were, however, several psychological factors associated with FCR that were notably different for IM compared with dominant cancer survivors, including meaning and trigger factors. The sense of life meaning and purpose associated with the religious/spiritual beliefs held by many IM survivors may help them engage in more goal-directed action consistent with their values, enabling them to disengage from worries about recurrence (Fardell et al., 2016). Additionally, unmet needs and healthcare satisfaction were associated with FCR differently for some IM populations, as was the mediating effect of FCR on pain interference and fatigue on emotional well-being. It appears that the difficulties navigating the healthcare system and lower levels of healthcare satisfaction experienced more commonly by IM cancer survivors may be exacerbating their FCR, perhaps through the greater sense of general uncertainty that this creates (Fardell et al., 2016; Lebel et al., 2018). The identification of factors associated with FCR in these studies was limited by the fact that the majority of quantitative studies in this review were cross-sectional studies. While some of these were large, they often included only a small IM sub-sample.
The findings of the qualitative meta-synthesis suggest some notable differences in the experience of FCR between cancer survivors across IM groups. This finding is broadly consistent with current thinking that FCR might not be a unique/simple fear but rather a set of different fears, which are often experienced differently between people (Almeida et al., 2019). Despite the many differences, there were some noteworthy parallels in the experience of FCR among cancer survivors across IM populations.
Our qualitative findings suggest that FCR in cancer survivors from IM populations might be commonly moderated via spiritual and/or fatalistic worldviews regarding the outcomes of their cancer and their future. While the particular characteristics of such views differed across cultural groups and individuals, some commonality in the psychological strength and solace that they afforded IM cancer survivors was apparent. While this issue has received little research attention in other populations (Almeida et al., 2019), there is some evidence that a sense of connectedness, which has been characterized as spirituality, helps some breast cancer survivors to adjust and cope post-treatment (Shachar Siman-Tov, 2008). Additionally, our review findings suggest that there is a commonly held belief among IM cancer survivors that maintaining a positive attitude is an important factor in coping with FCR and in overcoming their cancer more generally. This type of thinking is sometimes called the tyranny of positivity as it is widely accepted that promoting unsupported beliefs regarding maintaining a positive outlook and avoiding stress will prevent or lessen a person's chances of serious illness are dangerous and likely lead to victim-blaming of those who are ill for not being positive enough (Aspinwall and Tedeschi, 2010). While staying positive may assist coping and reduce FCR for some IM cancer survivors, the promotion of positivity to IM survivors should be balanced with consideration of the potential negative effects of overemphasizing its import.
Our qualitative findings around the complexities associated with family and community support for cancer survivors from IM populations were notable. Strong family and community networks are commonly identified as important supports for cancer patients in many IM populations, the pressure and stigma that these networks can occasion for cancer survivors might sometimes serve to heighten FCR, as it prevents cancer survivors from expressing their fears in order to protect those around them (Soriano et al., 2018). Sharing concerns with social supports may help normalize concerns, while internalization of fears may lead to greater rumination and worsening of FCR.
Taken together, the results of our review revealed that FCR is experienced differently across IM populations, which is perhaps unsurprising, considering the diversity of cultural groups, geographic and social contexts and study methods, as well as the documented variability in FCR levels across other populations generally (Almeida et al., 2019). Spirituality, family and community support, and need for cancer information have such marked but variable roles in the experience of FCR for cancer survivors from different IM populations that approaches to reducing FCR must be flexible and adaptable enough to meet each survivor's individual circumstances and needs.
Our review highlights important considerations for future FCR research and practice addressing key priorities [e.g., better FCR detection/screening and more accessible FCR treatment models (Shaw et al., 2021)], to ensure that IM experiences and needs regarding FCR are accommodated. To enable FCR screening in IM populations, further work is needed to validate brief FCR measures in IM populations and adapt them where needed. To date, no interventions specifically targeting FCR in an IM population have been trialed (Tauber et al., 2019). To make FCR interventions accessible and engaging for IM populations it is essential that their diverse cultural beliefs and norms be considered. For instance, interventions incorporating elements of acceptance and commitment therapy may appeal more to IM populations where spiritual beliefs around acceptance are common. Given the importance of community support for many IM populations, but occasionally negative impact of community expectations, delivery of interventions focused on normalizing and coping with FCR, not just for survivors, but also their caregivers and communities, may be beneficial. Our findings make clear that effective measurement and treatment of FCR must take into account the individual and cultural circumstances of cancer survivors. While patient-reported outcome measures are commonly translated for culturally and linguistically diverse respondents, this approach fails to capture critical issues relevant to specific populations. Measures of FCR that include items developed by and with people from IM populations will offer the most effective means of identifying IM patients' concerns associated with this condition. Considering the variable experience of FCR across different IM populations, it is essential that researchers and clinicians partner with representatives of the specific IM communities they are serving, to ensure research and clinical practice is culturally responsive.
There are methodological limitations of our review that must be noted. The heterogeneity in the study designs, samples, cancers and methods for assessing FCR across the studies included in this review only enable the aggregation of descriptive statistics. Further, limited evidence was available regarding factors associated with FCR and how these differed between IM and majority populations. This limits the strength of the evidence that can be presented and elicits more questions than answers. As this review aims to establish an evidence base within an under-researched area, this limitation is to be expected.
Most studies included in this review were conducted in the US, which highlights the need for greater research attention to this issue in other countries. The single study reporting on FCR for Indigenous people (also from the US), while offering a valuable insight into the condition for this particular group, cannot reflect the experience of survivors across different Indigenous populations. Given this limitation, it is tenuous to make any generalizations about FCR for other Indigenous populations.
This review is a first attempt to draw attention to the dearth of literature around FCR for cancer survivors from IM populations. The findings of this review are intended to identify the areas in greatest need of research attention. Most notable is the lack of research into FCR among Indigenous cancer survivors. The fact that all papers identified in our review were in Anglophile countries highlights the paucity of FCR research internationally. Fortunately, the number of articles published on FCR in IM populations appears to be increasing, with an updated search in March 2021 finding seven further relavent papers. We hope this review will stimulate further research in the area and that an update of this review would incorporate many more papers. The development of culturally-appropriate measures of FCR, or the validation of existing measures of FCR for IM populations, would also aid further research. Ensuring that research in this space is conducted by and/or with researchers from IM populations is imperative.
This review highlights the potential impact of culture and context on FCR and reinforces the need for a culturally-specific lens to be used in consideration and measurement of this condition. The paucity of research investigating FCR among cancer survivors from Indigenous groups requires urgent attention.
This paper presents findings from our synthesis of previously reported findings. Each study included in our review is included in our reference list. For original data enquiries, please contact the corresponding authors of these papers.
KA, ABS, and AD participated in research design, writing of the paper, performance of the research, and data analysis. JS, LS, AG, SL, HD, LB, and PB participated in research design and writing of the paper. BT participated in writing of the paper and data analysis. GG participated in research design, writing of the paper, performance of the research, and data analysis. All authors contributed to the article and approved the submitted version.
This study was supported by the NHMRC-funded Center of Research Excellence in Targeted Approaches To Improve Cancer Services for Aboriginal and Torres Strait Islander Australians (TACTICS CRE; #1153027). AD was funding by the TACTICS CRE. GG was supported by an NHMRC Investigator grant (#1176651).
The views expressed in this publication are those of the authors and do not necessarily reflect the views of the funders.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Thank you to Professor Joan Cunningham for reviewing the manuscript. Thank you to Ms. Hana Hoburg, Ms. Elaina Elder-Robinson, and Ms. Rachael Jaenke for assisting with administration of this review.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.621850/full#supplementary-material
Almeida, S. N., Elliott, R., Silva, E. R., and Sales, C. M. D. (2019). Fear of cancer recurrence: a qualitative systematic review and meta-synthesis of patients' experiences. Clin. Psychol. Rev. 68, 13–24. doi: 10.1016/j.cpr.2018.12.001
Angell, B., Muhunthan, J., Eades, A. M., Cunningham, J., Garvey, G., Cass, A., et al. (2016). The health-related quality of life of indigenous populations: a global systematic review. Qual. Life Res. 25, 2161–2178. doi: 10.1007/s11136-016-1311-9
Ashing, K. T., Cho, D., Lai, L., Yeung, S., Young, L., Yeon, C., et al. (2017). Exploring characteristics, predictors, and consequences of fear of cancer recurrence among Asian-American breast cancer survivors. Psychooncology 26, 2253–2260. doi: 10.1002/pon.4350
Ashing-Giwa, K. T., Padilla, G., Tejero, J., Kraemer, J., Wright, K., Coscarelli, A., et al. (2004). Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psychooncology 13, 408–428. doi: 10.1002/pon.750
Aspinwall, L. G., and Tedeschi, R. G. (2010). Of babies and bathwater: a reply to Coyne and Tennen's views on positive psychology and health. Ann. Behav. Med. 39, 27–34. doi: 10.1007/s12160-010-9155-y
Avis, N. E., Smith, K. W., McGraw, S., Smith, R. G., Petronis, V. M., and Carver, C. S. (2005). Assessing quality of life in adult cancer survivors (QLACS). Qual. Life Res. 14, 1007–1023. doi: 10.1007/s11136-004-2147-2
Bache, R. A., Bhui, K. S., Dein, S., and Korszun, A. (2012). African and Black Caribbean origin cancer survivors: a qualitative study of the narratives of causes, coping and care experiences. Ethn. Health 17, 187–201. doi: 10.1080/13557858.2011.635785
Best, A. L., Alcaraz, K. I., McQueen, A., Cooper, D. L., Warren, R. C., and Stein, K. (2015). Examining the mediating role of cancer-related problems on spirituality and self-rated health among African American cancer survivors: a report from the American Cancer Society's Studies of Cancer Survivors-II. Psychooncology 24, 1051–1059. doi: 10.1002/pon.3720
Braun, K. L., Mokuau, N., Hunt, G. H., Kaanoi, M., and Gotay, C. C. (2002). Supports and obstacles to cancer survival for Hawaii's native people. Cancer Pract. 10, 192–200. doi: 10.1046/j.1523-5394.2002.104001.x
Butow, P., Williams, D., Thewes, B., Tesson, S., Sharpe, L., Smith, A. B., et al. (2019). A psychological intervention (ConquerFear) for treating fear of cancer recurrence: views of study therapists regarding sustainability. Psychooncology 28, 533–539. doi: 10.1002/pon.4971
Butow, P. N., Bell, M. L., Aldridge, L. J., Sze, M., Eisenbruch, M., Jefford, M., et al. (2013). Unmet needs in immigrant cancer survivors: a cross-sectional population-based study. Support. Care Cancer 21, 2509–2520. doi: 10.1007/s00520-013-1819-2
Cho, D., Chu, Q., and Lu, Q. (2018). Associations among physical symptoms, fear of cancer recurrence, and emotional well-being among Chinese American breast cancer survivors: a path model. Support. Care Cancer 26, 1755–1761. doi: 10.1007/s00520-017-4010-3
Crist, J. V., and Grunfeld, E. A. (2013). Factors reported to influence fear of recurrence in cancer patients: a systematic review. Psychooncology 22, 978–986. doi: 10.1002/pon.3114
Dawson, S., Campbell, S. M., Giles, S. J., Morris, R. L., and Cheraghi-Sohi, S. (2018). Black and minority ethnic group involvement in health and social care research: a systematic review. Health Expect. 21, 3–22. doi: 10.1111/hex.12597
de Souza, J. A., Hunt, B., Asirwa, F. C., Adebamowo, C., and Lopes, G. (2016). Global health equity: cancer care outcome disparities in high-, middle-, and low-income countries. J. Clin. Oncol. 34, 6–13. doi: 10.1200/JCO.2015.62.2860
Deimling, G. T., Bowman, K. F., Sterns, S., Wagner, L. J., and Kahana, B. (2006). Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology 15, 306–320. doi: 10.1002/pon.955
Fardell, J. E., Thewes, B., Turner, J., Gilchrist, J., Sharpe, L., Smith, A., et al. (2016). Fear of cancer recurrence: a theoretical review and novel cognitive processing formulation. J. Cancer Surviv. 10, 663–673. doi: 10.1007/s11764-015-0512-5
Garvey, G., Cunningham, J., Mayer, C., Letendre, A., Shaw, J., Anderson, K., et al. (2020). Psychosocial aspects of delivering cancer care to indigenous people: an overview. JCO Global Oncol. 6, 148–154. doi: 10.1200/JGO.19.00130
Gill, K. M., Mishel, M., Belyea, M., Germino, B., Germino, L. S., Porter, L., et al. (2004). Triggers of uncertainty about recurrence and long-term treatment side effects in older African American and Caucasian breast cancer survivors. Oncol. Nurs. Forum. 31, 633–639. doi: 10.1188/04.ONF.633-639
Hall, D. L., Luberto, C. M., Philpotts, L. L., Song, R., Park, E. R., and Yeh, G. Y. (2018). Mind-body interventions for fear of cancer recurrence: a systematic review and meta-analysis. Psychooncology 27, 2546–2558. doi: 10.1002/pon.4757
Härtl, K., Janni, W., Kästner, R., Sommer, H., Strobl, B., Rack, B., et al. (2003). Impact of medical and demographic factors on long-term quality of life and body image of breast cancer patients. Ann. Oncol. 14, 1064–1071. doi: 10.1093/annonc/mdg289
Hodges, L. J., and Humphris, G. M. (2009). Fear of recurrence and psychological distress in head and neck cancer patients and their carers. Psychooncology 18, 841–848. doi: 10.1002/pon.1346
Hong, Q. N., Pluye, P., Fàbregues, S., Bartlett, G., Boardman, F., Cargo, M., et al. (2018). Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of Copyright (#1148552). Montreal, QC: Canadian Intellectual Property Office.
Janz, N. K., Hawley, S. T., Mujahid, M. S., Griggs, J. J., Alderman, A., Hamilton, A. S., et al. (2011). Correlates of worry about recurrence in a multiethnic population-based sample of women with breast cancer. Cancer 117, 1827–1836. doi: 10.1002/cncr.25740
Janz, N. K., Li, Y., Beesley, L. J., Wallner, L. P., Hamilton, A. S., Morrison, R. A., et al. (2016). Worry about recurrence in a multi-ethnic population of breast cancer survivors and their partners. Support. Care Cancer 24, 4669–4678. doi: 10.1007/s00520-016-3314-z
Koch, L., Jansen, L., Brenner, H., and Arndt, V. (2013). Fear of recurrence and disease progression in long-term (≥5 years) cancer survivors—a systematic review of quantitative studies. Psychooncology 22, 1–11. doi: 10.1002/pon.3022
Krupski T. L. Sonn G. Kwan L. Maliski S. Fink A. Litwin M. S. Ethnic variation in health-related quality of life among low-income men with prostate cancer. Ethn Dis. (2005) 15:461–8.
Lebel, S., Maheu, C., Tomei, C., Bernstein, L. J., Courbasson, C., Ferguson, S., et al. (2018). Towards the validation of a new, blended theoretical model of fear of cancer recurrence. Psychooncology 27, 2594–2601. doi: 10.1002/pon.4880
Lebel, S., Ozakinci, G., Humphries, G., Mutasers, B., Thewes, B., Prins, J., et al. (2016). From normal response to clinical problem: definition and clinical features of fear of cancer recurrence. Support. Care Cancer. 24, 3265–3268. doi: 10.1007/s00520-016-3272-5
Lebel, S., Tomei, C., Feldstain, A., Beattie, S., and McCallum, M. (2013). Does fear of cancer recurrence predict cancer survivors' health care use? Support. Care Cancer. 21, 901–906. doi: 10.1007/s00520-012-1685-3
Liu, Y., Pérez, M., Schootman, M., Aft, R. L., Gillanders, W. E., and Jeffe, D. B. (2011). Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Res. Treat. 130, 165–173. doi: 10.1007/s10549-011-1551-x
McMullen, C., Bulkley, J., Corley, D. A., Madrid, S., Davis, A. Q., Hesselbrock, R., et al. (2019). Health care improvement and survivorship priorities of colorectal cancer survivors: findings from the PORTAL colorectal cancer cohort survey. Support. Care Cancer 27, 147–156. doi: 10.1007/s00520-018-4299-6
Moher, D., Liberati, A., Tetzlaff, J., and Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br. Med. J. 339:b2535. doi: 10.1136/bmj.b2535
Nápoles, A. M., Ortiz, C., Santoyo-Olsson, J., Stewart, A. L., Lee, H. E., Duron, Y., et al. (2017). Post-treatment survivorship care needs of Spanish-speaking Latinas with breast cancer. J. Commun. Support Oncol. 15, 20–27. doi: 10.12788/jcso.0325
Otto, A. K., Soriano, E. C., Siegel, S. D., LoSavio, S. T., and Laurenceau, J.-P. (2018). Assessing the relationship between fear of cancer recurrence and health care utilization in early-stage breast cancer survivors. J. Cancer Survivorship 12, 775–785. doi: 10.1007/s11764-018-0714-8
Ouzzani, M., Hammady, H., Fedorowicz, Z., and Elmagarmid, A. (2016). Rayyan — a web and mobile app for systematic reviews. Syst. Rev. 5:210. doi: 10.1186/s13643-016-0384-4
Pandya, D. M., Patel, S., Ketchum, N. S., Pollock, B. H., and Padmanabhan, S. (2011). A comparison of races and leukemia subtypes among patients in different cancer survivorship phases. Clin. Lymphoma Myeloma Leuk. 11(Suppl. 1), S114–S118. doi: 10.1016/j.clml.2011.05.036
Sam, A. V. (2016). Relationship between illness perception and fear of cancer recurrence and psychological distress among survivors of gynecologic cancer. J. Oncol. Navigat. Survivorship. 7.
Shachar Siman-Tov, E. (2008). The Experience and the Role of Spirituality Among Women Who Have had Breast Cancer and Who Have Completed Their Medical Treatments. University of Hartford.
Sharpe, L., Thewes, B., and Butow, P. (2017). Current directions in research and treatment of fear of cancer recurrence. Curr. Opin. Support. Palliat. Care 11, 191–196. doi: 10.1097/SPC.0000000000000288
Shaw, J., Kamphuis, H., Sharpe, L., Lebel, S., Smith, A. B., Hulbert-Williams, N., et al. (2021). Setting an international research agenda for fear of cancer recurrence: an online delphi consensus study. Front. Psychol. 12:e596682. doi: 10.3389/fpsyg.2021.596682
Simard, S., and Savard, J. (2009). Fear of cancer recurrence inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support. Care Cancer 17, 241–251. doi: 10.1007/s00520-008-0444-y
Simard, S., Thewes, B., Humphries, G., Dixon, M., Hayden, C., Mireskandari, S., et al. (2013). Fear of cancer recurrence in adult cancer survivors: a systematic review of quantitative studies. J. Cancer Survivorship 7, 300–322. doi: 10.1007/s11764-013-0272-z
Singh-Carlson, S., Wong, F., Martin, L., and Nguyen, S. K. A. (2013). Breast cancer survivorship and South Asian women: understanding about the follow-up care plan and perspectives and preferences for information post treatment. Curr. Oncol. 20, e63–79. doi: 10.3747/co.20.1066
Smith, A., Sharpe, L., Thewes, B., Turner, J., Gilchrist, J., Fardell, J. E., et al. (2018). Medical, demographic and psychological correlates of fear of cancer recurrence (FCR) morbidity in breast, colorectal and melanoma cancer survivors with probable clinically significant FCR seeking psychological treatment through the ConquerFear study. Support. Care Cancer 26, 4207–4216. doi: 10.1007/s00520-018-4294-y
Soriano, E. C., Pasipanodya, E. C., LoSavio, S. T., Otto, A. K., Perndorfer, C., Siegel, S. D., et al. (2018). Social constraints and fear of recurrence in couples coping with early stage breast cancer. Health Psychol. 37, 874–884. doi: 10.1037/hea0000649
Tauber, N. M., O'Toole, M. S., Dinkel, A., Galica, J., Humphries, G., Lebel, S., et al. (2019). Effect of psychological intervention on fear of cancer recurrence: a systematic review and meta-analysis. J. Clin. Oncol. 37, 2899–2915. doi: 10.1200/JCO.19.00572
Taylor, T. R., Huntley, E. D., Sween, J., Makambi, K., Mellman, T. A., Williams, C. D., et al. (2012). An exploratory analysis of fear of recurrence among African-American breast cancer survivors. Int. J. Behav. Med. 19, 280–287. doi: 10.1007/s12529-011-9183-4
Thewes, B., Butow, P., Bell, M. L., Beith, J., Stuart-Harris, R., Grossi, M., et al. (2012a). Fear of cancer recurrence in young women with a history of early-stage breast cancer: a cross-sectional study of prevalence and association with health behaviours. Support. Care Cancer 20, 2651–2659. doi: 10.1007/s00520-011-1371-x
Thewes, B., Butow, P., Zacharie, R., Christensen, S., Simard, S., and Gotay, C. (2012b). Fear of cancer recurrence: a systematic literature review of self-report measures. Psychooncology 21, 571–587. doi: 10.1002/pon.2070
United Nations (1992). Declaration on the Rights of Persons Belonging to National or Ethnic, Religious and Linguistic Minorities. Geneva: United Nations. Available online at: https://www.ohchr.org/en/professionalinterest/pages/minorities.aspx (accessed September 22, 2020).
United Nations (2020). Indigenous Peoples at the UN. Available online at: https://www.un.org/development/desa/indigenouspeoples/about-us.html (accessed February 19, 2020).
United Nations Permanent Forum on Indigenous Issues (2009). Statistical Division. State of the World's Indigenous Peoples. New York, NY: United Nations Publications.
Vickberg, S. M. (2003). The concerns about recurrence scale (CARS): A systematic measure of women's fears about the possibility of breast cancer recurrence. Ann. Behav. Med. 25, 16–24. doi: 10.1207/S15324796ABM2501_03
Keywords: fear of cancer recurrence, cancer, oncology, review—systematic, minority, Indigenous people
Citation: Anderson K, Smith AB, Diaz A, Shaw J, Butow P, Sharpe L, Girgis A, Lebel S, Dhillon H, Burhansstipanov L, Tighe B and Garvey G (2021) A Systematic Review of Fear of Cancer Recurrence Among Indigenous and Minority Peoples. Front. Psychol. 12:621850. doi: 10.3389/fpsyg.2021.621850
Received: 27 October 2020; Accepted: 22 March 2021;
Published: 03 May 2021.
Edited by:
Sigrun Vehling, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Rebecca Philipp, University Medical Center Hamburg-Eppendorf, GermanyCopyright © 2021 Anderson, Smith, Diaz, Shaw, Butow, Sharpe, Girgis, Lebel, Dhillon, Burhansstipanov, Tighe and Garvey. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kate Anderson, a2F0ZS5hbmRlcnNvbkBtZW56aWVzLmVkdS5hdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.