
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 31 August 2021
Sec. Quantitative Psychology and Measurement
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.614193
 Ligai Liu1†
Ligai Liu1† Xin Wang2†
Xin Wang2† Yiwei Hao3†
Yiwei Hao3† Jingming Yang2
Jingming Yang2 Di Yang4
Di Yang4 Xuefei Duan5
Xuefei Duan5 Gaoli Fang6
Gaoli Fang6 Bing Han4
Bing Han4 Chunguo Jiang7
Chunguo Jiang7 Junnan Li8
Junnan Li8 Yao Liu9
Yao Liu9 Yang Wang10
Yang Wang10 Rui Song4*
Rui Song4*Objective: To analyze the discrepancy between self-rating and professional evaluation of mental health status in coronavirus disease 2019 (COVID-19) cluster cases.
Method: A total of 65 COVID-19 cluster cases admitted to Beijing Ditan Hospital Capital Medical University from June 14, 2020 to June 16, 2020 were included in the study. Mental health assessment was completed by self-rating and professional evaluation. The gaps between self-rating and professional evaluation in different demographic characteristics were compared.
Results: The results of self-rating were inconsistent with those of professional evaluation. The gap was statistically different among certain demographic subgroups. As for anxiety, the gaps had remarkable statistics differences in subgroups of sex, monthly income, infection way, and anxiety/depression medical history. Similarly, in the terms of depression, the gaps had significant statistic differences in the subgroups of the medical history of anxiety/depression, history of physical disease, employment status and the insurance type, marriage, education (year), residing in Beijing (year), and the monthly income.
Conclusion: Compared to the professional evaluation, patients had a higher self-rating, which may be related to some demographic characteristics. It suggests that screening can be conducted in patients with COVID-19 by self-rating first, and then professional evaluation should be carried out in the patients with suspicious or positive results.
Since the coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) had been reported in December 2019 (Zhu et al., 2020), it has gained wide attention rapidly. SARS-CoV-2 is highly contagious (Fang et al., 2020), and it could develop into a severe even fatal respiratory system disease (Guan et al., 2020; Huang et al., 2020), as well as develop neurological disorders (Wenting et al., 2020; Taquet et al., 2021).
Studies show clear signs of the harmful consequences, both mentally and psychologically, of COVID-19 in the general population (e.g., anxiety and depression; World Health Organization, 2020; de Vroege and van den Broek, 2021).
Being similar to other coronaviruses (Mak et al., 2009), patients with COVID-19 might show mental pressure, anxiety and depression syndromes, psychiatric dysfunction, and other such problems (Li et al., 2020a; Liu et al., 2020; Pappa et al., 2020; Qi et al., 2020; Torales et al., 2020; Zhang et al., 2020), even in the long term after the disease (Taquet et al., 2021). It is possibly because the patients experienced fear of the consequences of severe disease and the contagion (Xiang et al., 2020). Furthermore, strict quarantine and mandatory contact-tracing policy by the health authorities could cause societal rejection, financial loss, discrimination, and stigmatization (Balsamo and Carlucci, 2020; Brooks et al., 2020; Carlucci et al., 2020; Shigemura et al., 2020; Vindegaard and Benros, 2020). Some patients even committed suicide after experiencing anxiety and insomnia in the beginning of the hospitalization. In Italy, since the beginning of the COVID-19 quarantine, domestic homicides, and murder suicides registered to date increased (Balsamo and Carlucci, 2020). But it remains unclear whether the risks are attributable to viral infections per se or the host immune response (Troyer et al., 2020).
Therefore, accurate assessment of the mental status of patients is especially important (Epstein et al., 2020), which can avoid wastage of the limited mental health resources, and patients can be supported through less intense ways. On the contrary, it can also reduce the burden of medical workers. Previous studies showed that there were differences between self-rating and professional evaluation results, and the depression rate reported through self-rating scale was significantly higher than those through clinical interview (Lim et al., 2018). For the slightly depression conditions, more depression symptoms can be generated through self-rating (Rush et al., 1987).
Professional evaluation and self-rating are two common clinical scales, and can provide important information for clinical doctors (Möller, 2000). Self-rating, which is economical and practical, is widely used for survey and screening procedures, especially for slight diseases such as anxiety (Maier et al., 1990). The problem is the self-awareness of the patients may not reflect reality. It's hard to complete for some patients lack of reading ability (Hamilton, 1976). While professional evaluation is a comprehensive evaluation to the symptoms of the patients by clinically trained professionals with experience, which is still the golden standard for mental disorder diagnosis (Dunstan et al., 2017).
The self-rating anxiety scale (SAS) and self-rating depression scale (SDS) of Zung are the widely used for anxiety and depression evaluation (Zung, 1965, 1971; Möller, 2000). The Hamilton Anxiety (HAMA) and the Hamilton Depression (HAMD) rating scales are commonly used in evaluating anxiety and depression (Hamilton, 1959, 1960). They are the golden standard in the depression evaluation (Bagby et al., 2004). During the COVID-19 pandemic, it was widely used to investigate the psychological status of the different population (Li et al., 2020b).
Most of the researches on the psychological evaluation of patients with COVID-19 used self-rating scales (Guo et al., 2020), and the application of the professional evaluations is rare. Besides, the rare research has reported the difference between self-rating and professional evaluation in the patients with COVID-19. This study conducted that both self-rating and professional evaluation in COVID-19 cluster cases, and compared the results obtained by these two methods.
There were 65 cluster patients with COVID-19 enrolled in this study. All of them were admitted to Beijing Ditan Hospital from June 14, 2020 to 16 June 16, 2020, including 38 male patients, aging from 21 to 65 (42.29 ± 12.344). This is a cross-sectional observational study that is approved by the Ethics Committee of Beijing Ditan Hospital affiliated to Capital Medical University.
The inclusion criteria were: (i) age >18, (ii) diagnosed as COVID-19 (mild-type to normal-type), which was based on the COVID-19 diagnosis protocol (trial version 7) issued by the State Health Committee, and (iii) patient informed consent.
The exclusion criteria were: (i) had a recent history of travel and residence overseas or in other high-risk areas, (ii) had severe psychological trauma recently, (iii) having severe heart, liver, kidney, or nervous system diseases, and (iv) failed to cooperate to complete the self-rating and the professional evaluation.
Demographic data were collected, including sex, age, marital status, educational background, length of residence in Beijing in the years, employment status, monthly income, insurance type, infection way, family member infected or not, smoking history, psychological disease, and other physical disease history.
This study, through online survey, conducted self-evaluation by using SAS and SDS. The Chinese norm shows that the cut-off value of the SAS standard score is 50. From 50 to 59 points was slightly anxiety, 60 to 69 points were medium anxiety, and above 70 points is heavily anxiety. The Chinese norm shows that the cut-off value of the SDS standard score is 53. From 53 to 62 is slightly depression, 63 to 72 is medium depression, and above 72 is heavily depression.
In addition, the mental health of the patients was assessed by the two trained attending psychiatrists, who passed the consistency evaluation, through with HAMA and HAMD.
Hamilton Anxiety rating scale items were concluded into two dimensions: (i) mental anxiety and (ii) somatic anxiety. HAMD items were concluded into seven dimensions: (i) Anxiety/somatization: consisting of mental anxiety, physical anxiety, digestive symptoms, hypochondria, and insight, (ii) Weight: weight loss item, (iii) Cognitive disorder: consisting of self-guilt, suicidal, intense, depersonalization and derealization, paranoid symptoms, and obsessive compulsive symptoms, (iv) Diurnal variation: only this item, (v) Retardation: consisting of the depressive emotions, work and hobby, retardation, and sex symptoms, (vi) Sleeping disorder: consisting of the difficulty falling into sleep, sleep light and early wakeup, (vii) Desperation: consisting of the sense of diminished ability, desperation and sense of inferiority. HAMA ≥7, anxiety symptoms exist and HAMD ≥8, depression symptoms exist.
The SPSS 17.0 software was used to analyze the data. Quantitative data with normal distribution were expressed using the format mean ± SD ( ± s). The t-test for the two isolated samples was used to make comparison between the two groups. One-way ANOVA was used to compare multiple groups. Mann–Whitney U-test was used to make comparison between two quantitative data groups with non-normal distribution. The Kruskal–Wallis test was used to make comparison among multiple isolated samples with non-normal distribution, and p < 0.05 was considered statistically significant.
We calculate the gaps between the self-rating scale and professional evaluation in the same dimension. However, the self-rating scale and professional evaluation have completely different measurement and the scoring system. So, 0–1 normalization process is used to standardize the scores in each dimension, which makes the dimension scores comparable between the self-rating scale and the professional evaluation. The 0–1 normalization process of the ith question for the jth patient is calculated as follow:
Standardi is the standardized scores for the ith question, scoreij is the initial score of the ith question for the jth patient in the HAMD scale. Max(scorei) and min(scorei) are the theoretical maximum and minimum values of the scores in the ith question. Take the HAMD scores as an example, max(scorei)−min(scorei) = 4 − 0 = 4. We conduct this process for all the questions in the HAMD scale, and then calculate the average standardize scores in each dimension. By this way, we get the standard scores in seven dimensions in the HAMD scale. After the 0–1 normalization, the maximum standard score becomes 1 and the standard minimum score becomes 0. The exactly same process is also conducted in the SDS scale and their anxiety evaluation counterparts. Although the self-rating scale and the professional evaluation have different measurement in both the anxiety and depression evaluation, the 0–1 normalization process makes it possible to make a compare of one particular dimension between the self-rating scale and the professional evaluation. The gap between self-rating and professional evaluation within one particular dimension is calculated by the standard professional evaluation score minus standard self-rating score.
All the data collected by the scales were stored in the database. Then, the calculation functions in the database could help to finish the 0–1 normalization process, and the statistical analysis was running based on these data. So, the methods allow for the replication studies.
A total of 65 patients participated in this study, and 58 patients had finished both the self-rating and the professional evaluation.
The self-rating is inconsistent with the professional evaluation as Figure 1 shows Kappa Consistence.
The SAS score was (31.79 ± 4.742), with anxiety symptoms 0 case. The HAMA score was (4.16 ± 4.043), 12 cases (20.7%) had anxiety symptoms. The scores of two dimensions of SAS were both higher than HAMA (Figure 2), and the differences were statistically significant (p = 0.001, p = 0.018).
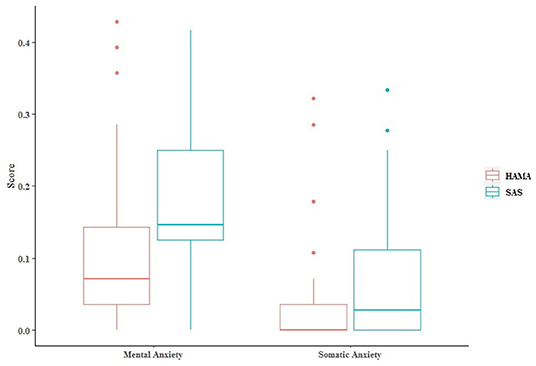
Figure 2. The SAS was divided and matched by referring to the two dimensions of somatic anxiety and mental anxiety in HAMA, and the scores of the same dimension were compared.
The value of p < 0.05 indicates that the factors are the reason for the significant difference in the gaps, and that may be the reason for the difference between the results of SAS and HAMA (Table 1). Among/between the subgroups of sex, monthly, and anxiety/depression medical history, the mental anxiety gap had significant difference. Between the subgroups of the infection way, the somatic anxiety gap had significant difference.
The SDS score was (38.55 ± 8.664), 24 cases (41.4%) had depression symptoms, including 19 cases of mild depression, and 5 cases of moderate depression. The HAMD score was (6.10 ± 4.734), 16 cases (27.6%) had depressive symptoms, all were slightly depressed. The SDS scores on seven dimensions were all higher than HAMD (Figure 3), and the differences were statistically significant, p < 0.05.
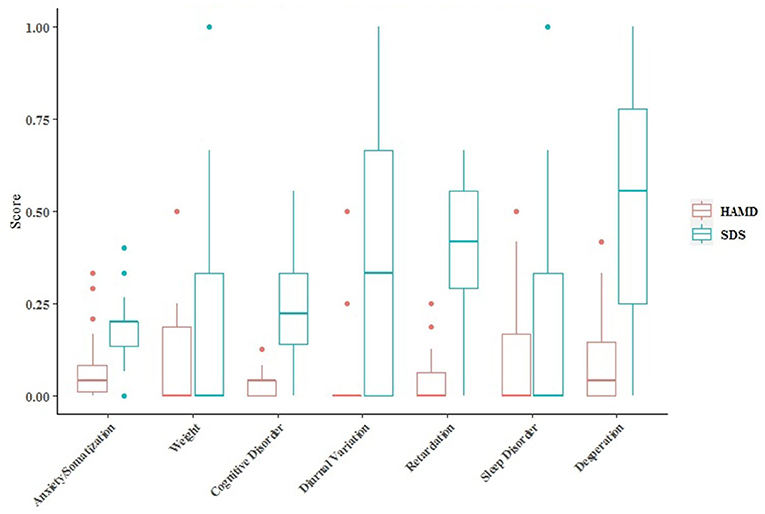
Figure 3. The SDS scale was divided and matched according to the seven dimensions of HAMD, and the scores of the same dimension were compared.
The value of p < 0.05 indicates that the factors are the reason for the significant difference in the gaps, and that may be the reason for the difference between the results of the SDS and HAMD (Table 2).
Among the subgroups of the insurance type, the anxiety/somatization gap had significant difference. Between the subgroups of the history of physical disease, the cognitive gap had significant difference. Among/between the subgroups of marriage, education (year), and residing in Beijing (year), the retardation gap had significant difference. Among the subgroups of education (year) and monthly, the desperation gap had significant difference. Among the subgroups of monthly, the diurnal variation gap had significant difference. Between the subgroups of the employment status and anxiety/depression medical history, the sleeping gap had significant difference.
By introducing the concept of gap, this study discussed the discrepancy between self-rating and professional evaluation in the COVID-19 cluster cases for the first time. It showed that SAS and SDS scores in the same dimension were significantly higher than the HAMA and HAMD, indicating that there were significant differences between the self-rating and the professional evaluation. This was consistent with the previous reports (Rush et al., 1987; Enns et al., 2014; Krebber et al., 2014; Lim et al., 2018).
Moreover, the male subgroup and the subgroup with higher income had higher self-rating scores in the mental anxiety dimension, which might be due to the fact that they assume more family and social responsibilities, so that they were more likely to worry about the impact of illness on themselves, family life, and the career. Notably, as compared with the indirect contact with Xinfadi, where COVID-19 broke out, the patients with direct contact had higher self-rating of the somatic anxiety, who might be more in need of the attention of doctors (Troyer et al., 2020), which is possibly because the cluster disease increased their feelings of fear and guilt to some extent.
In terms of depression, patients who were non-insured were more likely to have higher self-rating of anxiety/somatic status, which might be due to their fear of bearing high-medical costs. The patients without a history of physical disease had a higher self-rating of cognitive, which might be due to the greater psychological burden of the hospitalization because they had not been hit by the disease. Compared with the patients who were divorced and widowed, the patients who were unmarried and married had higher self-rating of retardation, which might be due to their concern about the impact on their relationship or the family life. The patients with higher education level had higher self-rating of cognitive and desperation status. It was probably because the patients with better education background had better reading ability and could complete the questionnaire accurately, and also knew more about COVID-19 and understood the risk of novel coronavirus infection, which increased their depression mood. The patients with the higher income made a higher self-rating of desperation and diurnal variation, which might be caused by the fear of the disease affecting career and work, and the inability to maintain the current income level. It seemed incomprehensible that the patients without a history of depression tend to have a higher self-rating of sleeping disorder. The patients with a history of depression were able to make a more objective self-rating when they developed insomnia symptoms after being infected with the SARS-CoV-2, which was probably because they had severe insomnia before, and in particular, they had filled the similar rating scales often ever before.
Those differences may be associated with the personality and demography of the patients, which is consistent with the previous studies (Enns et al., 2014). So, when planning to assess the mental health of the patients with COVID-19 by self-rating, it is necessary to pay attention to the age, gender, work status, monthly, education level, employment status, medical history, and infection way of the patients. There may be an unobjective evaluation. For instance, the scores of the two dimensions of anxiety self-rating were both higher than those of the professional evaluation, but the patients with anxiety were not found according to the anxiety self-rating standard, which was not in accordance with the actual situation. We supposed that the SAS diagnostic threshold may need to be adjusted or improved the self-rating questionnaire when used.
Therefore, in the clinical practice, we suggest that screening can be conducted by self-rating first, then the professional evaluation should be carried for the patients with suspicious or positive results, so as to reduce unnecessary contact with the patients and the workload of the medical workers (de Vroege and van den Broek, 2021).
The limitations are the limited number of cases included in the study and the lack of a control group. Fortunately, the included cases were cluster cases, all from Xinfadi where COVID-19 broke, with relatively consistent background and mild condition. As a result those cases are highly homogeneous. It, to some extent, proves something. However, whether self-rating can accurately and effectively assess mental status of the patients and the reasons for the difference between the self-rating and professional evaluation will likely require the closer examination.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by the Ethics Committee of Beijing Ditan Hospital affiliated to Capital Medical University. The patients/participants provided their written informed consent to participate in this study.
RS developed the ideas in the paper and provided feedback on several drafts of the paper. LL collected the data of demographic and self-rating, and wrote the paper. XW and JY evaluated the patients by HAMA and HAMD. YH conducted statistical analysis of the data in this study. DY, XD, GF, BH, CJ, JL, YL, and YW introduced the study to the patients and obtain their consent. All authors contributed to the article and approved the submitted version.
This article was funded by Capital's Funds for Health Improvement and Research (CFH), Fund number 2021-1G-4091.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Bagby, R. M., Ryder, A. G., Schuller, D. R., and Marshall, M. B. (2004). The Hamilton Depression Rating Scale: has the gold standard become a lead weight? Am. J. Psychiatry 161, 2163–2177. doi: 10.1176/appi.ajp.161.12.2163
Balsamo, M., and Carlucci, L. (2020). Italians on the age of COVID-19: the self-reported depressive symptoms through web-based survey. Front. Psychol. 11:569276. doi: 10.3389/fpsyg.2020.569276
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Carlucci, L., D'Ambrosio, I., and Balsamo, M. (2020). Demographic and attitudinal factors of adherence to quarantine guidelines during COVID-19: the Italian model. Front Psychol. 11:559288. doi: 10.3389/fpsyg.2020.559288
de Vroege, L., and van den Broek, A. (2021). Results of mental support for health care professionals and mental care during the COVID-19 pandemic. J. Public Health 27:fdaa278. doi: 10.1093/pubmed/fdaa278
Dunstan, D. A., Scott, N., and Todd, A. K. (2017). Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry 17:329. doi: 10.1186/s12888-017-1489-6
Enns, M. W., Larsen, D. K., and Cox, B. J. (2014). Discrepancies between self and observer ratings of depression. The relationship to demographic, clinical and personality variables. J. Affect. Disord. 161, 144–149. doi: 10.1016/s0165-0327(99)00156-1
Epstein, D., Andrawis, W., Lipsky, A. M., Ziad, H. A., and Matan, M. (2020). Anxiety and suicidality in a hospitalized patient with COVID-19 infection. Eur. J. Case Rep. Intern. Med. 7:001651. doi: 10.12890/2020_001651
Fang, Y., Nie, Y., and Penny, M. (2020). Transmission dynamics of the COVID-19 outbreak and effectiveness of government interventions: a data-driven analysis. J. Med. Virol. 92, 645–659. doi: 10.1002/jmv.25750
Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., et al. (2020). Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382, 1708–1720. doi: 10.1056/NEJMoa2002032
Guo, Q., Zheng, Y., Shi, J., Wang, J., Li, G., Li, C., et al. (2020). Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 88, 17–27. doi: 10.1016/j.bbi.2020.05.038
Hamilton, M. (1960). A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. doi: 10.1136/jnnp.23.1.56
Hamilton, M. (1976). Comparative value of rating scales. Br. J. Clin. Pharmacol. 3(1 Suppl. 1), 58–60. doi: 10.1111/j.1365-2125.1976.tb03714.x
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. doi: 10.1016/S0140-6736(20)30183-5
Krebber, A. M., Buffart, L. M., Kleijn, G., Riepma, I. C., de Bree, R., Leemans, C. R., et al. (2014). Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology 23, 121–130. doi: 10.1002/pon.3409
Li, W., Yang, Y., Liu, Z. H., Zhao, Y. J., Zhang, Q., Zhang, L., et al. (2020a). Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 16, 1732–1738. doi: 10.7150/ijbs.45120
Li, W., Zhang, C., Luo, J., Zhang, H., Wu, H., Yang, B., et al. (2020b). Psychological status among different populations during COVID-19 epidemic: a systematic review and meta-analysis (in Chinese). J. Tongji Univers. 41, 147–154. doi: 10.16118/j.1008-0392.2020.02.002
Lim, G. Y., Tam, W. W., Lu, Y., Ho, C. S., Zhang, M. W., and Ho, R. C. (2018). Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 8:2861. doi: 10.1038/s41598-018-21243-x
Liu, K., Chen, Y., Wu, D., Lin, R., Wang, Z., and Pan, L. (2020). Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Pract. 39:101132. doi: 10.1016/j.ctcp.2020.101132
Maier, W., Albus, M., Buller, R., Nutzinger, D., Shera, D., and Bech, P. (1990). Self- and observer assessment in anxiolytic drug trials: a comparison of their validity. Eur. Arch. Psychiatry Clin. Neurosci. 240, 103–108. doi: 10.1007/BF02189979
Mak, I. W., Chu, C. M., Pan, P. C., Yiu, M. G., and Chan, V. L. (2009). Long-term psychiatric morbidities among SARS survivors. Gen. Hosp. Psychiatry 31, 318–326. doi: 10.1016/j.genhosppsych.2009.03.001
Möller, H. J. (2000). Rating depressed patients- observer- vs self-assessment. Eur. Psychiatry 15, 160–172. doi: 10.1016/s0924-9338(00)00229-7
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907. doi: 10.1016/j.bbi.2020.05.026
Qi, R., Chen, W., Liu, S., Thompson, P. M., Zhang, L. J., Xia, F., et al. (2020). Psychological morbidities and fatigue in patients with confirmed COVID-19 during disease outbreak: prevalence and associated biopsychosocial risk factors. medRxiv [Preprint]. doi: 10.1101/2020.05.08.20031666
Rush, A. J., Hiser, W., and Giles, D. E. (1987). A comparison of self-reported versus clinician-related symptoms in depression. J. Clin. Psychiatry 48, 246–248.
Shigemura, J., Ursano, R. J., Morganstein, J. C., Kurosawa, M., and Benedek, D. M. (2020). Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: mental health consequences and target populations. Psychiatry Clin. Neurosci. 74, 281–282. doi: 10.1111/pcn.12988
Taquet, M., Geddes, J. R., Husain, M., Luciano, S., and Harrison, P. J. (2021). 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8, 416–427. doi: 10.1016/S2215-0366(21)00084-5
Torales, J., Olla, V., Giannakasaldelli-Maia, J. M., and Ventriglio, A. (2020). The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 66, 317–320. doi: 10.1177/0020764020915212
Troyer, E. A., Kohn, J. N., and Hong, S. (2020). Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 87, 34–39. doi: 10.1016/j.bbi.2020.04.027
Vindegaard, N., and Benros, M. E. (2020). COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89, 531–542. doi: 10.1016/j.bbi.2020.05.048
Wenting, A., Gruters, A., van Os, Y., Verstraeten, S., Valentijn, S., Ponds, R., et al. (2020). COVID-19 neurological manifestations and underlying mechanisms: a scoping review. Front. Psychiatry 11:860. doi: 10.3389/fpsyt.2020.00860
World Health Organization (2020). Facing Mental Health Fallout From the Coronavirus Pandemic. Available online at: https://www.who.int/news-room/feature-stories/detail/facing-mental-health-fallout-from-the-coronavirus-pandemic (accessed June 20, 2021).
Xiang, Y.-T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Zhang, J., Lu, H., Zeng, H., Zhang, S., Du, Q., Jiang, T., et al. (2020). The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 87, 49–50. doi: 10.1016/j.bbi.2020.04.031
Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., et al. (2020). A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733. doi: 10.1056/NEJMoa2001017
Zung, W. W. (1965). A self-rating depression scale. Arch. Gen. Psychiatry 12, 63–70. doi: 10.1001/archpsyc.1965.01720310065008
Keywords: SARS-CoV-2, COVID-19, self-rating scale, professional evaluation, mental health assessment
Citation: Liu LG, Wang X, Hao YW, Yang JM, Yang D, Duan XF, Fang GL, Han B, Jiang CG, Li JN, Liu Y, Wang Y and Song R (2021) The Gaps Between the Self and Professional Evaluation in Mental Health Assessment of COVID-19 Cluster Cases. Front. Psychol. 12:614193. doi: 10.3389/fpsyg.2021.614193
Received: 05 October 2020; Accepted: 13 July 2021;
Published: 31 August 2021.
Edited by:
Michela Balsamo, University of Studies G. d'Annunzio Chieti and Pescara, ItalyReviewed by:
Rubén López-Bueno, National Research Centre for the Working Environment, DenmarkCopyright © 2021 Liu, Wang, Hao, Yang, Yang, Duan, Fang, Han, Jiang, Li, Liu, Wang and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Rui Song, c29uZ3J1aWlAaG90bWFpbC5jb20=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.