
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 01 July 2021
Sec. Psychology for Clinical Settings
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.612338
This article is part of the Research Topic Sensory Stimulation and Oxytocin: Their Roles in Social Interaction and Health Promotion View all 20 articles
 Claudia Carmassi1
Claudia Carmassi1 Donatella Marazziti1,2*
Donatella Marazziti1,2* Federico Mucci3,4
Federico Mucci3,4 Alessandra Della Vecchia1
Alessandra Della Vecchia1 Filippo Maria Barberi1
Filippo Maria Barberi1 Stefano Baroni1
Stefano Baroni1 Gino Giannaccini5
Gino Giannaccini5 Lionella Palego5
Lionella Palego5 Gabriele Massimetti1
Gabriele Massimetti1 Liliana Dell’Osso1
Liliana Dell’Osso1Introduction: Although the pathophysiology of post-traumatic stress disorder (PTSD) is still unclear, growing preclinical evidences suggest that oxytocin (OT), a pleiotropic hormone, is possibly involved. However, direct studies on OT levels or clinical trials with this exogenous hormone in patients with PTSD led to inconsistent findings. Therefore, the aim of the present study was at exploring and comparing the plasma OT levels in a group of patients with PTSD and matched healthy subjects as the control group.
Materials and Methods: Twenty-six outpatients (13 men, 13 women, mean age: 40.3 ± 11.5 years) suffering from PTSD, according to the Diagnostic and Statistical Manual for Mental Disorders, fifth edition (DSM-5), and 26 healthy subjects (13 men, 13 women, mean age: 43.8 ± 12.7 years) were included. The patients were assessed through the structured clinical interview for DSM-5 research version, patient edition (SCID-I/P), and the Impact for Event Scale revised (IES-R). All fasting subjects underwent three venous blood samples for the subsequent oxytocin radioimmunoassay. We used unpaired Student’s t-test to assess OT levels and the intergroup difference of demographic characteristics, while anxiety, avoidance, and hyperarousal scores were compared among groups adjusting for the effect of gender and age by means of analysis of covariance (ANCOVA). The correlations between different variables were investigated by Pearson’s method.
Results: The most common traumatic events of patients with PTSD were the following: severe car accident, physical violence, sexual violence, sudden death of a loved one, and natural disaster. The IES total score was 55 ± 15. Student’s t-test revealed that the patients showed significantly lower OT levels (mean ± SD, pg/ml) than healthy control subjects (4.37 ± 1.61 vs 5.64 ± 2.17, p < 0.001). We detected no correlation between the IES total score, subscales, or single items and OT plasma levels. Again, no difference between men and women was detected in the patients’ group, while healthy control women showed higher OT levels than men.
Discussion: Our study, while reporting the presence of decreased plasma OT levels in outpatients with PTSD of both sexes, as compared with healthy control subjects, would support the possible involvement of OT in the pathophysiology of PTSD. However, given the complexity of the clinical picture, future investigations are necessary to better deepen the role and level of OT in PTSD.
Post-traumatic stress disorder (PTSD) was initially classified within the category of anxiety disorders. However, in the fifth (and latest) edition of the Diagnostic and Statistical Manual for mental disorders (DSM-5) published in 2013 (American Psychiatric Association, 2013), PTSD was given a different diagnostic dignity and included within a brand new nosological category named “trauma- and stress-related disorders.” PTSD is diagnosed if patients experienced or witnessed events that include death or threatened death, actual or threatened physical injury, or actual or threatened sexual violation. They would also need symptoms in four separate categories including recurrence of intrusive and distressing memories or dreams that are related to the traumatic events, dissociative reactions (such as flashbacks), avoidance of thoughts and/or situations associated with the trauma, numbing of emotional responsiveness, negative alteration of cognition, and increased arousal (such as increased tendency to irritability and/or disruption of sleep pattern) (American Psychiatric Association, 2013).
Given the complexity of the clinical picture, the pathophysiology of PTSD is still unclear and mainly focused on the stress response.
Oxytocin (OT) is a pleiotropic hormone synthesized within the paraventricular and supraoptic nuclei of the hypothalamus, and is released into systemic circulation via the posterior pituitary and into the brain via widely distributed pathways (Pittman et al., 1981; Knobloch, 2014). Besides the “classical” functions attributed to OT, namely, uterine contractions during labor and milk ejection during nursing (Argiolas and Gessa, 1991; Fuchs et al., 1991), this hormone would promote social contacts between conspecifics, different types of attachment, and pair-bonding (Carter, 1992; Pedersen et al., 1992; Kendrick, 2000; Lim and Young, 2006; Marazziti et al., 2006; Macdonald and Macdonald, 2010; Anacker and Beery, 2013; Jones et al., 2017). In addition, it acts as a potent modulator of the immune system and shows anti-inflammatory properties (Clodi et al., 2008; Oliveira-Pelegrin et al., 2013; Li et al., 2017; Garrido-Urbani et al., 2018; Buemann et al., 2020). Oxytocin is released during stress response and seems to be an important modulator of anxiety and fear processes, mainly with anxiolytic effect (Jezová et al., 1996; McCarthy et al., 1996; Kirsch et al., 2005; Uvnås-Moberg and Petersson, 2005; Marazziti et al., 2006; Carter, 2017). Evidence shows that OT may decrease the response of the hypothalamic–pituitary–adrenal (HPA) axis in rodents and primates (Windle et al., 2004; Parker et al., 2005). Other physiological OT activities, including the attenuation of memory consolidation and retrieval, facilitation of the extinctions of an activated avoidance response, and attenuation of passive avoidance behavior (Bohus et al., 1978a,b; Amico, 1985), would support its potential role in PTSD neurobiology.
The first evidence of a possible involvement of the OT in some aspects of PTSD pathophysiology derived from animal experiments (Buijs, 1978). Converging studies showed that the exogenous OT administration modulated anxiety and fear responses in threatening situations (Landgraf and Neumann, 2004) and mitigated the activation of the HPA axis and the sympathetic system by reducing heart rate, blood pressure, and cortisol levels (Björkstrand et al., 1996; Petersson et al., 1996, 1999; Windle et al., 1997, 2004; Uvnäs-Moberg, 1998; Petersson and Uvnäs-Moberg, 2003; Parker et al., 2005). Studies on rats also suggested that the main target of OT anxiolytic effect would be the central amygdala, and that OT, together with dopamine, could act in reducing fear and anxiety arising from social and environmental stressors in order to promote appropriate behavioral responses (Bale et al., 2001; Neumann, 2001, 2002).
Different studies in humans showed a significant relationship between reduced endogenous OT concentrations and traumatic experiences and/or PTSD following early severe and recurrent abuse during childhood. These data suggested that alterations in stress response, including OT modulation, could explain the increased risk for impaired brain development following severe traumatic experience in children, for PTSD (Mirescu et al., 2004; Heim et al., 2009; Chatzittofis et al., 2014; Mohiyeddini et al., 2014) and, in general, for psychopathological disorders (Teicher et al., 2002; Ozbay et al., 2008; Gonzalez et al., 2009; Nicolson et al., 2010; Goldman-Mellor et al., 2012), perhaps related to increased emotional suppression (Opacka-Juffry and Mohiyeddini, 2012). On the contrary, the OT levels were increased in children exposed to minor traumas who lived in safe environments (Mizuki and Fujiwara, 2015). Increased OT levels also seem to be typical of women exposed to traumatic/stressful situations to perhaps promote pro-social and supporting behaviors (Taylor et al., 2006; Weisman et al., 2013). Interestingly, under acute stressful conditions, previously abused women showed increased OT concentrations (Seltzer et al., 2014). Such differences could be explained considering that estrogens influence OT release and OT receptor (OTRs) expression (Williams et al., 1985; Wigger and Neumann, 1999) and also by the recent report that basically women have higher OT levels than men (Marazziti et al., 2019).
The studies on the direct evaluation of plasma OT levels in patients with PTSD are few. Male policemen who developed PTSD after a severe trauma showed lower levels of salivary OT than colleagues without the disorder (Frijling et al., 2015). This might be due to increased activity of the prolyl-endopeptidase (PEP), a cleavage enzyme involved in the degradation of many behaviorally active oligopeptides such as OT, as shown in those patients with PTSD with a concomitant major depression (Welches et al., 1993; Maes et al., 1999).
The administration of exogenous OT in subjects exposed to trauma experiences or suffering from PTSD led to inconclusive or opposite results (Finkelhor et al., 1990; Heim et al., 2000; Heinrichs et al., 2004; Kirsch et al., 2005; Domes et al., 2007; Gamer et al., 2010; Seng et al., 2014; Koch S.B. et al., 2016; Koch S.B.J. et al., 2016), given the possible interplay of different factors (sex, context, acute or chronic trauma) (Fan et al., 2014; Frijling et al., 2014, 2016a,b; Grimm et al., 2014; Rilling et al., 2014; Eidelman-Rothman et al., 2015; Nawijn et al., 2016, 2017; Sack et al., 2017; van Zuiden et al., 2017).
Finally, genetic association studies showed that some OTR gene polymorphisms might be related to increased risk of developing traumatic experiences and psychiatric disorders, such as PTSD, anxiety, and depression (Cochran et al., 2013; Lucas-Thompson and Holman, 2013; McQuaid et al., 2013; Tollenaar et al., 2017), while other OTR gene polymorphisms might have a protective function (Cicchetti and Rogosch, 2012). The most studied one, the OTR rs53576 GG genotype was associated with insecure attachments, poor response to social support, emotional dysregulation, and less resilience to stress (Bradley et al., 2011; Cicchetti and Rogosch, 2012; Sippel et al., 2017b), all factors resulting in a greater vulnerability to psychiatric disorders related to traumatic experiences (Feldman et al., 2016) and to environmental context (Champagne and Curley, 2009; Olff et al., 2013; Dannlowski et al., 2016).
Since PTSD is characterized by impairments in anxiety/stress regulation, memory, and social skills, and that OT is possibly involved in these functions, OT seems to represent a worthy target to be investigated and/or also to possibly develop future drugs to treat some symptoms of this condition (Olff et al., 2010; Sippel et al., 2017a).
Therefore, since the findings on this topic are still inconclusive and the available data in humans are meager, with this investigation, we explored and compared the plasma levels of OT in a group of patients with PTSD and matched healthy subjects as the control group. The possible sex-related difference in OT was examined as well, given the recent report showing higher plasma OT concentrations in healthy women than in men (Marazziti et al., 2019).
Twenty-six outpatients (13 men, 13 women, mean age: 40.3 ± 11.5), recruited at the psychiatric outpatient unit of the Department of Clinical and Experimental Medicine, Section of Psychiatry, University of Pisa from a large cohort, were consecutively enrolled in the study. All patients were at their first psychiatric consultation and were affected by PTSD diagnosed according to the Diagnostic and Statistical Manual for Mental Disorders, fourth edition revised (DSM-5) (American Psychiatric Association, 2013). All subjects were first assessed by a clinical evaluation with the ensuing diagnoses subsequently to be supported by the structured clinical interview for DSM-5, research version, patient edition (SCID-I/P) (First et al., 2015). The severity of PTSD was assessed by the Impact for Event Scale revised (IES-R) (Weiss and Marmar, 1996). No patients were depressed, as shown by their total score at the Hamilton Rating Scale for Depression (HRSD), which was <8 (Hamilton, 1960). All patients were drug-free; only five were occasionally taking benzodiazepines.
Twenty-six matched healthy subjects (13 men, 13 women, mean age: 43.8 ± 12.7), who volunteered for the study, were selected as the control group among clinicians or residents at the Specialty School of Psychiatry, at the University of Pisa. No subject had a family or personal history of any major psychiatric disorder or had ever taken regularly psychotropic drugs, as assessed by a detailed psychiatric interview conducted by one of the senior authors (DM). All subjects were free of physical illness, were neither heavy cigarette smokers, nor belonged to groups of high-risk HIV individuals, nor did take any regular medication or drug of addiction. The women had normal menstrual cycles and did not take contraceptive pills; their blood was drawn in the early follicular phase (between the second and the fifth day of the menses). The men had no history of genital disease or hypogonadism. All these pieces of information derived from the medical history collected by one of the authors (DM). All subjects provided their written informed consent to participate in the study that was approved by the Ethics Committee at Pisa University.
It is a multiple-item questionnaire used to provide an indication of depression and as a guide to evaluate recovery. The patient is rated on 17 to 29 items scored either on a 3- or 5-point Likert-type scale. For the 17-item version, a score of 0–7 is considered to be normal, while a score of 20 or higher (indicating at least moderate severity) is usually required for entry into a clinical trial.
The IES-R is a self-assessment questionnaire of 22 items investigating subjective reactions to traumatic events (Horowitz et al., 1979). In this revised version, seven items were added with particular reference to the hyperarousal symptom not considered in the previous version. Subjects should recognize a specific stressful life event and rate the perceived level of their personal distress during the past 7 days. Items are rated on a 5-point Likert scale ranging from 0 (“not at all”) to 4 (“extremely”). The clinician calculates the IES-R total (from 0 to 88) and subscale (intrusion, avoidance, and hyperarousal) scores.
Thirty milliliters of venous blood was drawn from fasting subjects who were sitting and relaxing in the same room at a constant temperature in the period January–June, and between 8 and 9 am. The blood for OT assay (10 ml) was transferred in vacutainers containing EDTA (anticoagulant), then to centrifuge tubes containing aprotinin (Sigma, Milan, Italy) (0.6 TIU/ml of blood), and mixed at different times to inhibit the proteinase activity. Blood was then centrifuged at 1,600 × g for 15 min at 4°C, and the ensuing plasma was collected and kept at −70°C until the assay.
On the day of the assay, 6 ml of each sample of plasma was acidified with 6 ml of buffer A (1% trifluoroacetic acid in H2O) and centrifuged at 17,000 × g for 20 min at 4°C; after this centrifugation, the supernatant was collected. C-18 sep-columns were equilibrated by washing them with 1 ml of buffer B (60% acetonitrile in 1% trifluoroacetic acid) followed by buffer A (3 ml, three times). The acidified plasma solution was loaded into the pre-treated C-18 Sep-column; the column was washed slowly with buffer A (3 ml, twice), and the washing liquid was discarded. Oxytocin was then eluted with buffer B (3 ml, once) and collected into a polystyrene tube. The eluate was evaporated in a centrifugal concentrator (Speedvac), and the remaining product was lyophilized by a freeze dryer.
Radioimmunoassay was performed by a Phoenix Pharmaceuticals Oxytocin RIA kit (Belmont, CA, United States) according to a method developed by us (Marazziti et al., 2006). The cross-reactivity of the OT antibody was 100% with OT and null with Lys-vasopressin, Arg-vasopressin, GH, alpha-ANP, Met-Enkephalin, GRF, somatostatin, TRH, VIP, and Pacap 27-NH2. The sensitivity of the assay, measured as IC50, was 10–30 pg/tube. The intra-assay and inter-assay values were 9 and 11%, respectively. Lyophilized samples and standard OT were rehydrated with an RIA buffer, and dilutions of standard oxytocin were prepared (from 1 to 128 pg/tube). Primary rabbit anti-OT antibodies were added to each sample and each standard, except for the nonspecific binding tubes, and then the mixtures were stored for 24 h at 4°C. 125I-Oxytocin was added to the mixtures, which were subsequently stored for 24 h at 4°C. Goat antirabbit Ig G serum and normal rabbit serum were added to each tube; subsequently, the tubes were centrifuged at 1,700 × g for 20 min at 4°C. All the supernatant was carefully aspirated, and the pellets were counted by a gamma-counter (Wizard, Perkin Elmer, Milan, Italy). All samples were assayed in duplicate. Standard curve and calculations of unknown samples were performed by means of the Graphpad Prism3 software.
The intergroup differences of age and OT levels were assessed by unpaired Student’s t-test. Analysis of covariance (ANCOVA) was used to compare anxiety, avoidance, and hyperarousal scores among groups adjusting for the effect of gender and age. The correlations between different variables were explored using Pearson’s method. Statistical analyses were carried out using SPSS, Version 12.0.1 (SPSS Inc., 2003).
The demographic characteristics of the study sample are shown in Table 1. Fifteen patients (seven men and eight women) were married, six (three men and three women) patients were single, two widowed (one man and one woman), and three divorced (two men and one woman). Fourteen healthy control subjects (7 men and 7 women) were married, 10 (6 men and 4 women) were single, and 2 (1 man and 1 woman) were divorced. Ten patients graduated, 10 had completed the high school, and 6 had completed the primary school. Twenty control subjects graduated and six had completed high school.
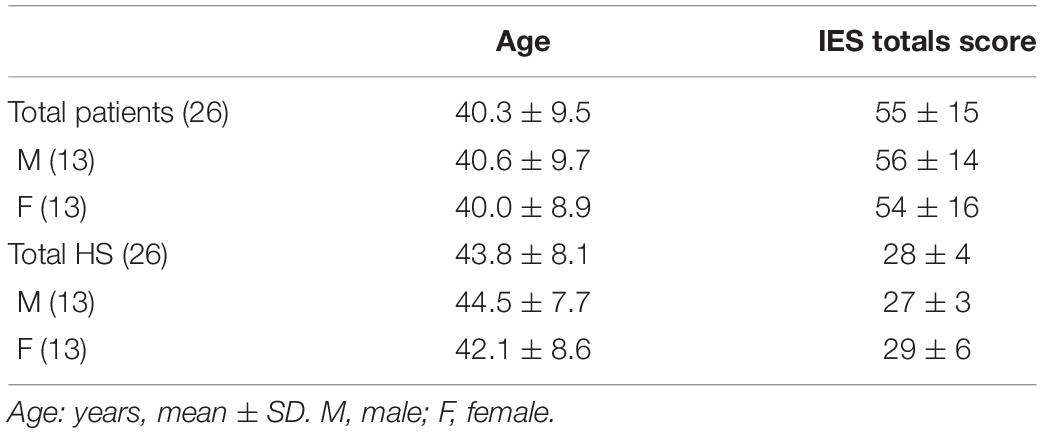
Table 1. Demographic data of PTSD patients and healthy subjects (HS) (in the total sample and in the two sexes).
The traumatic events reported by the sample were severe car accident (seven), physical violence (five), sexual violence (three), sudden death of a loved one (eight), and natural disaster (three).
The IES total score was 55 ± 15.
The OT levels (mean ± SD, pg/ml) were significantly lower in the patients than in the control subjects (4.37 ± 1.61 vs 5.64 ± 2.17, p < 0.001) (Table 2).
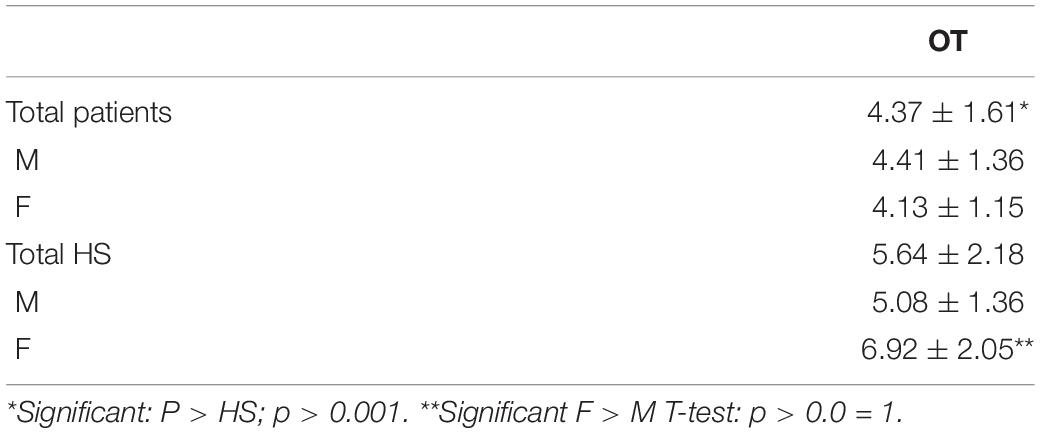
Table 2. Plasma oxytocin (OT) levels (pg/ml, mean+SD) in patients with PTSD and healthy subjects (HS) (in the total sample and in the two sexes).
No correlations were found between the IES total score, subscales, or single items and OT plasma levels.
No difference between men and women was detected in the patients’ group, while healthy control women showed higher OT levels than men (Table 2). There was a trend toward higher IES total and subscale scores in female than in male patients.
The present study aimed at providing information about the possible involvement of OT in some processes involved in PTSD through the assessment of its plasma levels in a group of patients suffering from PTSD as compared with matched healthy control subjects.
Although the reliability of plasma OT concentrations as a peripheral marker of those present in the CNS is still disputed (Neumann and Landgraf, 2012; Leng and Ludwig, 2016), nevertheless, parallel modifications in plasma or liquor and central OT have been reported (Carter, 1992; Bale et al., 1995; Smeltzer et al., 2006), supporting the peripheral model as a “window” of the central parameter (Scantamburlo et al., 2007; Agmo et al., 2008; Carson et al., 2015). While keeping in mind this limitation (that is common and applicable to a variety of markers in biological psychiatry), our findings highlighted significantly lower plasma concentrations of OT in patients with PTSD than in healthy control subjects. To our knowledge, this is the first description of decreased OT levels in adult patients with PTSD of both sexes. Our findings are consistent with a previous report of decreased salivary OT levels in a group of Dutch male policemen (Frijling et al., 2015). On the contrary, individual variations in plasma OT and vasopressin levels did not seem to be related to the development of combat-related PTSD in a large military group. However, this might be also probably due to the peculiarities of this sample, which was composed by men only and assessed before and after the deployment to a combat zone (Reijnen et al., 2017). Another study explored the predictive value of serum OT levels on PTSD, depression, and anxiety symptoms after a motor vehicle accident, while reporting negative results (Nishi et al., 2015). In any way, in our sample, we could not detect any difference in OT levels between the two sexes in the patients, probably for the small sample size, while healthy women showed higher OT levels than men, as already reported (Marazziti et al., 2019). For the same problem, we could not assess the possible impact of different traumatic events on OT concentrations.
It is undoubted that sex matters on OT, but available studies seldom explored this problem that still requires to be more thoroughly investigated in relation to psychopathology (Sippel et al., 2017a). Indeed, the majority of psychiatric disorders show a net dimorphism (Breslau et al., 1999; Kessler et al., 2003; Mezulis et al., 2010; Hellmuth et al., 2013; Bangasser and Wicks, 2017). Although controversies do exist, it has been hypothesized that some genetic polymorphisms may alter OT or OTRs, while increasing in women the risk to develop psychopathological disorders related to traumas, PTSD, anxiety, and depression (Bradley et al., 2011; Cicchetti and Rogosch, 2012; Lucas-Thompson and Holman, 2013; McQuaid et al., 2013; Altemus et al., 2014; Sippel et al., 2017b; Tollenaar et al., 2017; Ramikie and Ressler, 2018; Carter et al., 2020).
According to us, our findings of lower OT levels in PTSD patients might be interpreted as an unspecific biomarker of a condition of chronic stress (Olff et al., 2005; Abdallah et al., 2019).
Indeed, decreased OT concentrations have been observed in patients with autism and with OCD, where they increased after serotonergic treatments (Guastella et al., 2010; Humble et al., 2013; Husarova et al., 2016). Elevated plasma OT levels have been described in both depressed patients (Meynen et al., 2007; Parker et al., 2010) and OCD patients (Marazziti et al., 2015) and related with stress/anxiety symptoms or emotional distress (Costa et al., 2009; Thompson et al., 2011; Oh et al., 2018). However, it should be underlined that the validity of the methods used to measure OT levels is put into question, given their high variability (Szeto et al., 2011; McCullough et al., 2013; Leng and Ludwig, 2016), so that studies carried out in different laboratories are not easily comparable.
The data on the possible usefulness of exogenous, mainly intranasal OT in patients with PTSD or subjects with other trauma-related disorders are similarly controversial, possibly for the heterogeneity in trauma, social context, and sex (Finkelhor et al., 1990; Heim et al., 2000, 2009; Heinrichs et al., 2004; Kirsch et al., 2005; Domes et al., 2007; Gamer et al., 2010; Opacka-Juffry and Mohiyeddini, 2012; Chatzittofis et al., 2014; Frijling et al., 2014, 2015; Mohiyeddini et al., 2014; Seng et al., 2014; Mizuki and Fujiwara, 2015; Nishi et al., 2015; Koch S.B. et al., 2016; Koch S.B.J. et al., 2016). In addition, while the acute administration of OT to exposed subjects without PTSD resulted mainly in greater anxiety, reactivity, and worsening of post-traumatic symptoms (Fan et al., 2014; Grimm et al., 2014; Frijling et al., 2016a,b), in PTSD subjects, OT seemed to improve the overall clinical picture, especially the avoidance symptoms, in both acute and repeated administration (Eidelman-Rothman et al., 2015; Koch S.B. et al., 2016; Nawijn et al., 2016, 2017; Sack et al., 2017; van Zuiden et al., 2017). A recent systematic review concluded that long-term use of OT might decrease, although not at a statistical level, PTSD in relation with the severity of acute symptoms (Di Lorenzo et al., 2020).
Although, with no doubt, OT seems to represent a potentially innovative and “natural” psychotropic drug, further clinical and controlled studies, taking into account all possible confounding factors, including the sexually dimorphic effects of intranasal OT (Palgi et al., 2016; Sippel et al., 2017a), are necessary to ascertain its real therapeutic role on specific symptoms or symptom clusters, such as fear memory, compassion, and social skills in at least some subsets of stressed/traumatized patients (Palgi et al., 2016; Wang et al., 2018; Le Dorze et al., 2020).
To summarize, the findings of the present study showing decreased plasma OT levels in a group of outpatients with PTSD of both sexes, as compared with healthy control subjects, support the notion that OT might be involved in the modulation of some processes altered in PTSD, specifically the stress response, anxiety, memory, and social contacts.
Future studies should be helpful to disentangle the question of what are the most specific symptomatic domains or dimensions regulated by OT, as well as the therapeutic impact of treatment with OT or OT analogs or antagonists. Indeed, it is now evident that OT is a pleiotropic hormone fundamental for health, stress response, social behaviors, healing, and resilience through its effects on the brain, peripheral tissues, and the immune system (Carter et al., 2020). However, well-designed, controlled, and long-term studies are urgently warranted to understand the potential of OT that currently seems a sort of “chica de moda” or a panacea for a variety of different disorders.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Ethics Committee of the AOU Pisana. The patients/participants provided their written informed consent to participate in this study.
DM, LD, and CC planned and organized the study. FM, AD, and FB selected and assessed the patients: all diagnoses were confirmed by senior psychiatrists (DM and CC). SB, GG, and LP carried out the biological assays. GM performed the statistical analyses. DM reviewed the specific literature and wrote the manuscript. All the authors revised and commented on the manuscript and agreed to publish it.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abdallah, C. G., Averill, L. A., Akiki, T. J., Raza, M., Averill, C. L., Gomaa, H., et al. (2019). The neurobiology and pharmacotherapy of posttraumatic stress disorder. Ann. Rev. Pharmacol. Toxicol. 6, 171–189. doi: 10.1146/annurev-pharmtox-010818-021701
Agmo, A., Choleris, E., Kavaliers, M., Pfaff, D. W., and Ogawa, S. (2008). Social and sexual incentive properties of estrogen receptor alpha, estrogen receptor beta, or oxytocin knockout mice. Genes Brain Behav. 7, 70–77. doi: 10.1111/j.1601-183X.2007.00327.x
Altemus, M., Sarvaiya, N., and Neill Epperson, C. (2014). Sex differences in anxiety and depression: clinical perspectives. Front. Neuroendocrinol. 35:320–330. doi: 10.1016/j.yfrne.2014.05.004
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Washington, DC: American Psychiatric Association.
Anacker, A. M. J., and Beery, A. K. (2013). Life in groups: the roles of oxytocin in mammalian sociality. Front. Behav. Neurosci. 7:185. doi: 10.3389/fnbeh.2013.00185
Argiolas, A., and Gessa, G. L. (1991). Central functions of oxytocin. Neurosci. Biobehav. Rev. 15, 217–231. doi: 10.1016/s0149-7634(05)80002-8
Bale, T. L., Davis, A. M., Auger, A. P., Dorsa, D. M., and McCarthy, M. M. (2001). CNS region-specific oxytocin receptor expression: importance in regulation of anxiety and sex behavior. J. Neurosci. 21, 2546–2552. doi: 10.1523/jneurosci.21-07-02546.2001
Bale, T. L., Dorsa, D. M., and Johnston, C. A. (1995). Oxytocin receptor mRNA expression in the ventromedial hypothalamus during the estrous cycle. J. Neurosci. 15(7 Pt 1), 5058–5064. doi: 10.1523/jneurosci.15-07-05058.1995
Bangasser, D. A., and Wicks, B. (2017). Sex-specific mechanisms for responding to stress. J. Neurosci. Res. 95, 75–82. doi: 10.1002/jnr.23812
Björkstrand, E., Eriksson, M., and Uvnäs-Moberg, K. (1996). Evidence of a peripheral and a central effect of oxytocin on pancreatic hormone release in rats. Neuroendocrinology 63, 377–383. doi: 10.1159/000126978
Bohus, B., Kovács, G. L., and de Wied, D. (1978a). Oxytocin, vasopressin and memory: opposite effects on consolidation and retrieval processes. Brain Res. 157, 414–417. doi: 10.1016/0006-8993(78)90052-5
Bohus, B., Urban, I., Van Wimersma Greidanus, T. B., and De Wied, D. (1978b). Opposite effects of oxytocin and vasopressin on avoidance behaviour and hippocampal theta rhythm in the rat. Neuropharmacology 17, 239–247. doi: 10.1016/0028-3908(78)90107-7
Bradley, B., Westen, D., Mercer, K. B., Binder, E. B., Jovanovic, T., Crain, D., et al. (2011). Association between childhood maltreatment and adult emotional dysregulation in a low-income, urban. Afr. Am. Sample Moderat. Oxytocin Receptor Gene. Dev. Psychopathol. 23, 439–452. doi: 10.1017/s0954579411000162
Breslau, N., Chilcoat, H. D., Kessler, R. C., Peterson, E. L., and Lucia, V. C. (1999). Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol. Med. 29, 813–821. doi: 10.1017/s0033291799008612
Buemann, B., Marazziti, D., and Uvnäs-Moberg, K. (2020). Can intravenous oxytocin infusion counteract hyperinflammation in COVID-19 infected patients? World J. Biol. Psychiatry. doi: 10.1080/15622975.2020.1814408 [Epub ahead of print].
Buijs, R. M. (1978). Intra- and extrahypothalamic vasopressin and oxytocin pathways in the rat. pathways to the limbic system, medulla oblongata and spinal cord. Cell Tissue Res. 192, 423–435. doi: 10.1007/bf00212323
Carson, D. S., Berquist, S. W., Trujillo, T. H., Garner, J. P., Hannah, S. L., Hyde, S. A., et al. (2015). Cerebrospinal fluid and plasma oxytocin concentrations are positively correlated and negatively predict anxiety in children. Mol. Psychiatry 20, 1085–1090. doi: 10.1038/mp.2014.132
Carter, C. S. (1992). Oxytocin and sexual behavior. Neurosci. Biobehav. Rev. 16, 131–144. doi: 10.1016/s0149-7634(05)80176-9
Carter, C. S. (2017). The oxytocin-vasopressin pathway in the context of love and fear. Front. Endocrinol. 8:356. doi: 10.3389/fendo.2017.00356
Carter, C. S., Kenkel, W. M., MacLean, E. L., Wilson, S. R., Perkeybile, A. M., Yee, J. R., et al. (2020). Is oxytocin “nature’s medicine”? Pharmacol. Rev. 72, 829–861. doi: 10.1124/pr.120.019398
Champagne, F. A., and Curley, J. P. (2009). Epigenetic mechanisms mediating the long-term effects of maternal care on development. Neurosci. Biobehav. Rev. 33, 593–600. doi: 10.1016/j.neubiorev.2007.10.009
Chatzittofis, A., Nordström, P., Uvnäs-Moberg, K., Asberg, M., and Jokinen, J. (2014). CSF and plasma oxytocin levels in suicide attempters, the role of childhood trauma and revictimization. Neuroendocrinol. Lett. 35, 213–217.
Cicchetti, D., and Rogosch, F. A. (2012). Gene × environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Dev. Psychopathol. 24, 411–427. doi: 10.1017/s0954579412000077
Clodi, M., Vila, G., Geyeregger, R., Riedl, M., Stulnig, T. M., Struck, J., et al. (2008). Oxytocin alleviates the neuroendocrine and cytokine response to bacterial endotoxin in healthy men. Am. J. Physiol. Endocrinol. Metabolism 295, E686–E691. doi: 10.1152/ajpendo.90263.2008
Cochran, D. M., Fallon, D., Hill, M., and Frazier, J. A. (2013). The role of oxytocin in psychiatric disorders: a review of biological and therapeutic research findings. Harvard Rev. Psychiatry 21, 219–247. doi: 10.1097/HRP.0b013e3182a75b7d
Costa, B., Pini, S., Gabelloni, P., Abelli, M., Lari, L., Cardini, A., et al. (2009). Oxytocin receptor polymorphisms and adult attachment style in patients with depression. Psychoneuroendocrinology 34, 1506–1514. doi: 10.1016/j.psyneuen.2009.05.006
Dannlowski, U., Kugel, H., Grotegerd, D., Redlich, R., Opel, N., Dohm, K., et al. (2016). Disadvantage of social sensitivity: interaction of oxytocin receptor genotype and child maltreatment on brain structure. Biol. Psychiatry 80, 398–405. doi: 10.1016/j.biopsych.2015.12.010
Di Lorenzo, G., Longo, L., Jannini, T. B., Niolu, C., Rossi, R., and Siracusano, A. J. P. (2020). Oxytocin in the prevention and the treatment of post-traumatic stress disorder: a systematic review of randomized controlled trials. J. Psychopathol. 26, 107–118.
Domes, G., Heinrichs, M., Gläscher, J., Büchel, C., Braus, D. F., and Herpertz, S. C. (2007). Oxytocin attenuates amygdala responses to emotional faces regardless of valence. Biol. Psychiatry 62, 1187–1190. doi: 10.1016/j.biopsych.2007.03.025
Eidelman-Rothman, M., Goldstein, A., Levy, J., Weisman, O., Schneiderman, I., Mankuta, D., et al. (2015). Oxytocin affects spontaneous neural oscillations in trauma-exposed war veterans. Front. Behav. Neurosci. 9:165. doi: 10.3389/fnbeh.2015.00165
Fan, Y., Herrera-Melendez, A. L., Pestke, K., Feeser, M., Aust, S., Otte, C., et al. (2014). Early life stress modulates amygdala-prefrontal functional connectivity: implications for oxytocin effects. Hum. Brain Mapping 35, 5328–5339. doi: 10.1002/hbm.22553
Feldman, R., Monakhov, M., Pratt, M., and Ebstein, R. P. (2016). Oxytocin pathway genes: evolutionary ancient system impacting on human affiliation, sociality, and psychopathology. Biol. Psychiatry 79, 174–184. doi: 10.1016/j.biopsych.2015.08.008
Finkelhor, D., Hotaling, G., Lewis, I. A., and Smith, C. (1990). Sexual abuse in a national survey of adult men and women: prevalence, characteristics, and risk factors. Child Abuse Neglect 14, 19–28. doi: 10.1016/0145-2134(90)90077-7
First, M. B., Williams, J. B., Karg, R. S., and Spitzer, R. L. (2015). SCID-5-CV: Structured Clinical Interview for DSM-5 Disorders; Research Version. Arlington, TX: American Psychiatric Association Publishing.
Frijling, J. L., van Zuiden, M., Koch, S. B. J., Nawijn, L., Goslings, J. C., Luitse, J. S., et al. (2014). Efficacy of oxytocin administration early after psychotrauma in preventing the development of PTSD: study protocol of a randomized controlled trial. BMC Psychiatry 14:92. doi: 10.1186/1471-244X-14-92
Frijling, J. L., van Zuiden, M., Koch, S. B. J., Nawijn, L., Veltman, D. J., and Olff, M. (2016a). Effects of intranasal oxytocin on amygdala reactivity to emotional faces in recently trauma-exposed individuals. Soc. Cognit. Affect. Neurosci. 11, 327–336. doi: 10.1093/scan/nsv116
Frijling, J. L., van Zuiden, M., Koch, S. B., Nawijn, L., Veltman, D. J., and Olff, M. (2016b). Intranasal oxytocin affects amygdala functional connectivity after trauma script-driven imagery in distressed recently trauma-exposed individuals. Neuropsychopharmacology 41, 1286–1296. doi: 10.1038/npp.2015.278
Frijling, J. L., van Zuiden, M., Nawijn, L., Koch, S. B., Neumann, I. D., Veltman, D. J., et al. (2015). Salivary oxytocin and vasopressin levels in police officers with and without post-traumatic stress disorder. J. Neuroendocrinol. 27, 743–751. doi: 10.1111/jne.12300
Fuchs, A.-R., Romero, R., Keefe, D., Parra, M., Oyarzun, E., and Behnke, E. (1991). Oxytocin secretion and human parturition: pulse frequency and duration increase during spontaneous labor in women. Am. J. Obst. Gynecol. 165, 1515–1523. doi: 10.1016/S0002-9378(12)90793-0
Gamer, M., Zurowski, B., and Büchel, C. (2010). Different amygdala subregions mediate valence-related and attentional effects of oxytocin in humans. Proc. Natl. Acad. Sci. U.S.A. 107, 9400–9405. doi: 10.1073/pnas.1000985107
Garrido-Urbani, S., Deblon, N., Poher, A. L., Caillon, A., Ropraz, P., Rohner-Jeanrenaud, F., et al. (2018). Inhibitory role of oxytocin on TNFα expression assessed in vitro and in vivo. Diabetes Metabolism 44, 292–295. doi: 10.1016/j.diabet.2017.10.004
Goldman-Mellor, S., Hamer, M., and Steptoe, A. (2012). Early-life stress and recurrent psychological distress over the lifecourse predict divergent cortisol reactivity patterns in adulthood. Psychoneuroendocrinology 37, 1755–1768. doi: 10.1016/j.psyneuen.2012.03.010
Gonzalez, A., Jenkins, J. M., Steiner, M., and Fleming, A. S. (2009). The relation between early life adversity, cortisol awakening response and diurnal salivary cortisol levels in postpartum women. Psychoneuroendocrinology 34, 76–86. doi: 10.1016/j.psyneuen.2008.08.012
Grimm, S., Pestke, K., Feeser, M., Aust, S., Weigand, A., Wang, J., et al. (2014). Early life stress modulates oxytocin effects on limbic system during acute psychosocial stress. Soc. Cognit. Affect. Neurosci. 9, 1828–1835. doi: 10.1093/scan/nsu020
Guastella, A. J., Einfeld, S. L., Gray, K. M., Rinehart, N. J., Tonge, B. J., Lambert, T. J., et al. (2010). Intranasal oxytocin improves emotion recognition for youth with autism spectrum disorders. Biol. Psychiatry 67, 692–694. doi: 10.1016/j.biopsych.2009.09.020
Hamilton, M. (1960). A.rating scale for depression. J. Neurol. Neurosurg. Psychiatry 23, 56–62. doi: 10.1136/jnnp.23.1.56
Heim, C., Newport, D. J., Heit, S., Graham, Y. P., Wilcox, M., Bonsall, R., et al. (2000). Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA 284, 592–597. doi: 10.1001/jama.284.5.592
Heim, C., Young, L. J., Newport, D. J., Mletzko, T., Miller, A. H., and Nemeroff, C. B. (2009). Lower CSF oxytocin concentrations in women with a history of childhood abuse. Mol. Psychiatry 14, 954–958. doi: 10.1038/mp.2008.112
Heinrichs, M., Meinlschmidt, G., Wippich, W., Ehlert, U., and Hellhammer, D. H. (2004). Selective amnesic effects of oxytocin on human memory. Physiol. Behav. 83, 31–38. doi: 10.1016/j.physbeh.2004.07.020
Hellmuth, J. C., Jaquier, V., Young-Wolff, K., and Sullivan, T. P. (2013). Posttraumatic stress disorder symptom clusters, alcohol misuse, and women’s use of intimate partner violence. J. Traumatic Stress 26, 451–458. doi: 10.1002/jts.21829
Horowitz, M., Wilner, N., and Alvarez, W. (1979). Impact of event scale: a measure of subjective stress. Psychosomatic Med. 41, 209–218. doi: 10.1097/00006842-197905000-00004
Humble, M. B., Uvnäs-Moberg, K., Engström, I., and Bejerot, S. (2013). Plasma oxytocin changes and anti-obsessive response during serotonin reuptake inhibitor treatment: a placebo controlled study. BMC Psychiatry 13:344. doi: 10.1186/1471-244X-13-344
Husarova, V. M., Lakatosova, S., Pivovarciova, A., Babinska, K., Bakos, J., Durdiakova, J., et al. (2016). Plasma oxytocin in children with autism and its correlations with behavioral parameters in children and parents. Psychiatry Investigast. 13, 174–183. doi: 10.4306/pi.2016.13.2.174
Jezová, D., Juránková, E., Mosnárová, A., Kriska, M., and Skultétyová, I. (1996). Neuroendocrine response during stress with relation to gender differences. Acta Neurobiol. Exp. 56, 779–785.
Jones, C., Barrera, I., Brothers, S., Ring, R., and Wahlestedt, C. (2017). Oxytocin and social functioning. Dialogues Clin. Neurosci. 19, 193–201. doi: 10.31887/dcns.2017.19.2/cjones
Kendrick, K. M. (2000). Oxytocin, motherhood and bonding. Exp. Physiol. 85, 111s–124s. doi: 10.1111/j.1469-445x.2000.tb00014.x
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Koretz, D., Merikangas, K. R., et al. (2003). The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA 289, 3095–3105. doi: 10.1001/jama.289.23.3095
Kirsch, P., Esslinger, C., Chen, Q., Mier, D., Lis, S., Siddhanti, S., et al. (2005). Oxytocin modulates neural circuitry for social cognition and fear in humans. J. Neurosci. 25, 11489–11493. doi: 10.1523/jneurosci.3984-05.2005
Knobloch, H. S. (2014). Grinevch v: evolution if oxytocin pathwayin the brain of verebrates. Front. Behav. Neurosci. 14:31. doi: 10.3389/fnbeh.2014.00031
Koch, S. B. J., van Zuiden, M., Nawijn, L., Frijling, J. L., Veltman, D. J., and Olff, M. (2016). Intranasal oxytocin normalizes amygdala functional connectivity in posttraumatic stress disorder. Neuropsychopharmacology 41, 2041–2051. doi: 10.1038/npp.2016.1
Koch, S. B., van Zuiden, M., Nawijn, L., Frijling, J. L., Veltman, D. J., and Olff, M. (2016). Intranasal oxytocin administration dampens amygdala reactivity towards emotional faces in male and female PTSD patients. Neuropsychopharmacology 41, 1495–1504. doi: 10.1038/npp.2015.299
Landgraf, R., and Neumann, I. D. (2004). Vasopressin and oxytocin release within the brain: a dynamic concept of multiple and variable modes of neuropeptide communication. Front. Neuroendocrinol. 25:150–176. doi: 10.1016/j.yfrne.2004.05.001
Le Dorze, C., Borreca, A., Pignataro, A., Ammassari-Teule, M., and Gisquet-Verrier, P. (2020). Emotional remodeling with oxytocin durably rescues trauma-induced behavioral and neuro-morphological changes in rats: a promising treatment for PTSD. Trans. Psychiatry 10:27. doi: 10.1038/s41398-020-0714-0
Leng, G., and Ludwig, M. (2016). Intranasal oxytocin: myths and delusions. Biol. Psychiatry 79, 243–250. doi: 10.1016/j.biopsych.2015.05.003
Li, T., Wang, P., Wang, S. C., and Wang, Y.-F. (2017). Approaches mediating oxytocin regulation of the immune system. Front. Immunol. 7:693. doi: 10.3389/fimmu.2016.00693
Lim, M. M., and Young, L. J. (2006). Neuropeptidergic regulation of affiliative behavior and social bonding in animals. Hormones Behav. 50, 506–517. doi: 10.1016/j.yhbeh.2006.06.028
Lucas-Thompson, R. G., and Holman, E. A. (2013). Environmental stress, oxytocin receptor gene (OXTR) polymorphism, and mental health following collective stress. Hormones Behav. 63, 615–624. doi: 10.1016/j.yhbeh.2013.02.015
Macdonald, K., and Macdonald, T. M. (2010). The peptide that binds: a systematic review of oxytocin and its prosocial effects in humans. Harvard Rev. Psychiatry 18, 1–21. doi: 10.3109/10673220903523615
Maes, M., Lin, A.-H., Bonaccorso, S., Goossens, F., Van Gastel, A., Pioli, R., et al. (1999). Higher serum prolyl endopeptidase activity in patients with post-traumatic stress disorder. J. Affect. Dis. 53, 27–34. doi: 10.1016/S0165-0327(98)00086-X
Marazziti, D., Baroni, S., Giannaccini, G., Catena-Dell’Osso, M., Piccinni, A., Massimetti, G., et al. (2015). Plasma oxytocin levels in untreated adult obsessive-compulsive disorder patients. Neuropsychobiology 72, 74–80. doi: 10.1159/000438756
Marazziti, D., Baroni, S., Mucci, F., Piccinni, A., Moroni, I., Giannaccini, G., et al. (2019). Sex-related differences in plasma oxytocin levels in humans. Clin. Pract. Epidemiol. Mental Health 15, 58–63. doi: 10.2174/1745017901915010058
Marazziti, D., Dell’Osso, B., Baroni, S., Mungai, F., Catena, M., Rucci, P., et al. (2006). A relationship between oxytocin and anxiety of romantic attachment. Clin. Pract. Epidemiol. Mental Health 2:28. doi: 10.1186/1745-0179-2-28
McCarthy, M. M., McDonald, C. H., Brooks, P. J., and Goldman, D. (1996). An anxiolytic action of oxytocin is enhanced by estrogen in the mouse. Physiol. Behav. 60, 1209–1215. doi: 10.1016/s0031-9384(96)00212-0
McCullough, M. E., Churchland, P. S., and Mendez, A. J. (2013). Problems with measuring peripheral oxytocin: can the data on oxytocin and human behavior be trusted? Neurosci. Biobehav. Rev. 37, 1485–1492. doi: 10.1016/j.neubiorev.2013.04.018
McQuaid, R. J., McInnis, O. A., Stead, J. D., Matheson, K., and Anisman, H. (2013). A paradoxical association of an oxytocin receptor gene polymorphism: early-life adversity and vulnerability to depression. Front. Neurosci. 7:128. doi: 10.3389/fnins.2013.00128
Meynen, G., Unmehopa, U. A., Hofman, M. A., Swaab, D. F., and Hoogendijk, W. J. (2007). Hypothalamic oxytocin mRNA expression and melancholic depression. Mol. Psychiatry 12, 118–119. doi: 10.1038/sj.mp.4001911
Mezulis, A. H., Funasaki, K. S., Charbonneau, A. M., and Hyde, J. S. (2010). Gender differences in the cognitive vulnerability-stress model of depression in the transition to adolescence. Cognit. Ther. Res. 34, 501–513. doi: 10.1007/s10608-009-9281-7
Mirescu, C., Peters, J. D., and Gould, E. (2004). Early life experience alters response of adult neurogenesis to stress. Nat. Neurosci. 7, 841–846. doi: 10.1038/nn1290
Mizuki, R., and Fujiwara, T. (2015). Association of oxytocin level and less severe forms of childhood maltreatment history among healthy Japanese adults involved with child care. Front. Behav. Neurosci. 9:138. doi: 10.3389/fnbeh.2015.00138
Mohiyeddini, C., Opacka-Juffry, J., and Gross, J. J. (2014). Emotional suppression explains the link between early life stress and plasma oxytocin. Anxiety Stress Coping 27, 466–475. doi: 10.1080/10615806.2014.887696
Nawijn, L., van Zuiden, M., Koch, S. B. J., Frijling, J. L., Veltman, D. J., and Olff, M. (2017). Intranasal oxytocin increases neural responses to social reward in post-traumatic stress disorder. Soc. Cognit. Affect. Neurosci. 12, 212–223. doi: 10.1093/scan/nsw123
Nawijn, L., van Zuiden, M., Koch, S. B., Frijling, J. L., Veltman, D. J., and Olff, M. (2016). Intranasal oxytocin enhances neural processing of monetary reward and loss in post-traumatic stress disorder and traumatized controls. Psychoneuroendocrinology 66, 228–237. doi: 10.1016/j.psyneuen.2016.01.020
Neumann, I. D. (2001). Alterations in behavioral and neuroendocrine stress coping strategies in pregnant, parturient and lactating rats. Progr. Brain Res. 133, 143–152. doi: 10.1016/s0079-6123(01)33011-x
Neumann, I. D. (2002). Involvement of the brain oxytocin system in stress coping: interactions with the hypothalamo-pituitary-adrenal axis. Progr. Brain Res. 139, 147–162. doi: 10.1016/s0079-6123(02)39014-9
Neumann, I. D., and Landgraf, R. (2012). Balance of brain oxytocin and vasopressin: implications for anxiety, depression, and social behaviors. Trends Neurosci. 35, 649–659. doi: 10.1016/j.tins.2012.08.004
Nicolson, N. A., Davis, M. C., Kruszewski, D., and Zautra, A. J. (2010). Childhood maltreatment and diurnal cortisol patterns in women with chronic pain. Psychosom. Med. 72, 471–480. doi: 10.1097/PSY.0b013e3181d9a104
Nishi, D., Hashimoto, K., Noguchi, H., Kim, Y., and Matsuoka, Y. (2015). Serum oxytocin, posttraumatic coping and C-reactive protein in motor vehicle accident survivors by gender. Neuropsychobiology 71, 196–201. doi: 10.1159/000382021
Oh, K.-S., Kim, E.-J., Ha, J.-W., Woo, H.-Y., Kwon, M.-J., Shin, D.-W., et al. (2018). The relationship between plasma oxytocin levels and social anxiety symptoms. Psychiatry Investigat. 15, 1079–1086. doi: 10.30773/pi.2018.08.31
Olff, M., Frijling, J. L., Kubzansky, L. D., Bradley, B., Ellenbogen, M. A., Cardoso, C., et al. (2013). The role of oxytocin in social bonding, stress regulation and mental health: an update on the moderating effects of context and interindividual differences. Psychoneuroendocrinology 38, 1883–1894. doi: 10.1016/j.psyneuen.2013.06.019
Olff, M., Langeland, W., and Gersons, B. P. (2005). Effects of appraisal and coping on the neuroendocrine response to extreme stress. Neurosci. Biobehav. Rev. 29, 457–467. doi: 10.1016/j.neubiorev.2004.12.006
Olff, M., Langeland, W., Witteveen, A., and Denys, D. (2010). A.psychobiological rationale for oxytocin in the treatment of posttraumatic stress disorder. CNS Spectrums 15, 522–530. doi: 10.1017/s109285290000047x
Oliveira-Pelegrin, G. R., Saia, R. S., Cárnio, E. C., and Rocha, M. J. (2013). Oxytocin affects nitric oxide and cytokine production by sepsis-sensitized macrophages. Neuroimmunomodulation 20, 65–71. doi: 10.1159/000345044
Opacka-Juffry, J., and Mohiyeddini, C. (2012). Experience of stress in childhood negatively correlates with plasma oxytocin concentration in adult men. Stress 15, 1–10. doi: 10.3109/10253890.2011.560309
Ozbay, F., Fitterling, H., Charney, D., and Southwick, S. (2008). Social support and resilience to stress across the life span: a neurobiologic framework. Curr. Psychiatry Rep. 10, 304–310. doi: 10.1007/s11920-008-0049-7
Palgi, S., Klein, E., and Shamay-Tsoory, S. G. (2016). Oxytocin improves compassion toward women among patients with PTSD. Psychoneuroendocrinology 64, 143–149. doi: 10.1016/j.psyneuen.2015.11.008
Parker, K. J., Buckmaster, C. L., Schatzberg, A. F., and Lyons, D. M. (2005). Intranasal oxytocin administration attenuates the ACTH stress response in monkeys. Psychoneuroendocrinology 30, 924–929. doi: 10.1016/j.psyneuen.2005.04.002
Parker, K. J., Kenna, H. A., Zeitzer, J. M., Keller, J., Blasey, C. M., Amico, J. A., et al. (2010). Preliminary evidence that plasma oxytocin levels are elevated in major depression. Psychiatry Res. 178, 359–362. doi: 10.1016/j.psychres.2009.09.017
Pedersen, C. A., Caldwell, J. D., Peterson, G., Walker, C. H., and Mason, G. A. (1992). Oxytocin activation of maternal behavior in the rats. Ann. N. Y. Acad. Sci. 652, 58–69. doi: 10.1111/j.1749-6632.1992.tb34346
Petersson, M., Alster, P., Lundeberg, T., and Uvnäs-Moberg, K. (1996). Oxytocin causes a long-term decrease of blood pressure in female and male rats. Physiol. Behav. 60, 1311–1315. doi: 10.1016/s0031-9384(96)00261-2
Petersson, M., and Uvnäs-Moberg, K. (2003). Systemic oxytocin treatment modulates glucocorticoid and mineralocorticoid receptor mRNA in the rat hippocampus. Neurosci. Lett. 343, 97–100. doi: 10.1016/s0304-3940(03)00334-3
Petersson, M., Hulting, A. L., and Uvnäs-Moberg, K. (1999). Oxytocin causes a sustained decrease in plasma levels of corticosterone in rats. Neurosci. Lett. 264, 41–44. doi: 10.1016/s0304-3940(99)00159-7
Pittman, Q. J., Blume, H. W., and Renaud, L. P. (1981). Connections of the hypothalamic paraventricular nucleus with the neurohypophysis, median eminence, amygdala, lateral septum and midbrain periaqueductal gray: an electrophysiological study in the rat. Brain Res. 215, 15–28. doi: 10.1016/0006-8993(81)90488-1
Ramikie, T. S., and Ressler, K. J. (2018). Mechanisms of sex differences in fear and posttraumatic stress disorder. Biol. Psychiatry 83, 876–885. doi: 10.1016/j.biopsych.2017.11.016
Reijnen, A., Geuze, E., and Vermetten, E. (2017). Individual variation in plasma oxytocin and vasopressin levels in relation to the development of combat-related PTSD in a large military cohort. J. Psychiatric Res. 94, 88–95. doi: 10.1016/j.jpsychires.2017.06.010
Rilling, J. K., DeMarco, A. C., Hackett, P. D., Chen, X., Gautam, P., Stair, S., et al. (2014). Sex differences in the neural and behavioral response to intranasal oxytocin and vasopressin during human social interaction. Psychoneuroendocrinology 39, 237–248. doi: 10.1016/j.psyneuen.2013.09.022
Sack, M., Spieler, D., Wizelman, L., Epple, G., Stich, J., Zaba, M., et al. (2017). Intranasal oxytocin reduces provoked symptoms in female patients with posttraumatic stress disorder despite exerting sympathomimetic and positive chronotropic effects in a randomized controlled trial. BMC Med. 15:40. doi: 10.1186/s12916-017-0801-0
Scantamburlo, G., Hansenne, M., Fuchs, S., Pitchot, W., Maréchal, P., Pequeux, C., et al. (2007). Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology 32, 407–410. doi: 10.1016/j.psyneuen.2007.01.009
Seltzer, L. J., Ziegler, T., Connolly, M. J., Prososki, A. R., and Pollak, S. D. (2014). Stress-induced elevation of oxytocin in maltreated children: evolution, neurodevelopment, and social behavior. Child Dev. 85, 501–512. doi: 10.1111/cdev.12136
Seng, J. S., D’Andrea, W., and Ford, J. D. (2014). Complex mental health sequelae of psychological trauma among women in prenatal care. Psychological. Trauma. 6, 41–49. doi: 10.1037/a0031467
Sippel, L. M., Allington, C. E., Pietrzak, R. H., Harpaz-Rotem, I., Mayes, L. C., and Olff, M. (2017a). Oxytocin and stress-related disorders: neurobiological mechanisms and treatment opportunities. Chronic Stress 1, 2470547016687996. doi: 10.1177/2470547016687996
Sippel, L. M., Han, S., Watkins, L. E., Harpaz-Rotem, I., Southwick, S. M., Krystal, J. H., et al. (2017b). Oxytocin receptor gene polymorphisms, attachment, and PTSD: Results from the national health and resilience in veterans study. J. Psychiatric Res. 94, 139–147. doi: 10.1016/j.jpsychires.2017.07.008
Smeltzer, M. D., Curtis, J. T., Aragona, B. J., and Wang, Z. (2006). Dopamine, oxytocin, and vasopressin receptor binding in the medial prefrontal cortex of monogamous and promiscuous voles. Neurosci. Lett. 394, 146–151. doi: 10.1016/j.neulet.2005.10.019
Szeto, A., McCabe, P. M., Nation, D. A., Tabak, B. A., Rossetti, M. A., McCullough, M. E., et al. (2011). Evaluation of enzyme immunoassay and radioimmunoassay methods for the measurement of plasma oxytocin. Psychosomatic Med. 73, 393–400. doi: 10.1097/PSY.0b013e31821df0c2
Taylor, S. E., Gonzaga, G. C., Klein, L. C., Hu, P., Greendale, G. A., and Seeman, T. E. (2006). Relation of oxytocin to psychological stress responses and hypothalamic-pituitary-adrenocortical axis activity in older women. Psychosomatic Med. 68, 238–245. doi: 10.1097/01.psy.0000203242.95990.74
Teicher, M. H., Andersen, S. L., Polcari, A., Anderson, C. M., and Navalta, C. P. (2002). Developmental neurobiology of childhood stress and trauma. Psychiatric Clin. North Am. 25, 397–426,vii–viii. doi: 10.1016/s0193-953x(01)00003-x
Thompson, R. J., Parker, K. J., Hallmayer, J. F., Waugh, C. E., and Gotlib, I. H. (2011). Oxytocin receptor gene polymorphism (rs2254298) interacts with familial risk for psychopathology to predict symptoms of depression and anxiety in adolescent girls. Psychoneuroendocrinology 36, 144–147. doi: 10.1016/j.psyneuen.2010.07.003
Tollenaar, M. S., Molendijk, M. L., Penninx, B. W. J. H., Milaneschi, Y., and Antypa, N. (2017). The association of childhood maltreatment with depression and anxiety is not moderated by the oxytocin receptor gene. Eur. Arch. Psychiatry Clin. Neurosci. 267, 517–526. doi: 10.1007/s00406-017-0784-z
Uvnäs-Moberg, K. (1998). Antistress Pattern Induced by Oxytocin. News Physiol. Sci. 13, 22–25. doi: 10.1152/physiologyonline.1998.13.1.22
Uvnås-Moberg, K., and Petersson, M. (2005). Oxytocin, a mediator of anti-stress, well-being, social interaction, growth and healing. Zeitschrift fur Psychosomatische Medizin und Psychotherapie 51, 57–80. doi: 10.13109/zptm.2005.51.1.57
van Zuiden, M., Frijling, J. L., Nawijn, L., Koch, S. B. J., Goslings, J. C., Luitse, J. S., et al. (2017). Intranasal oxytocin to prevent post-traumatic stress disorder symptoms: a randomized controlled trial in emergency department patients. Biol. Psychiatry 81, 1030–1040. doi: 10.1016/j.biopsych.2016.11.012
Wang, S.-C., Lin, C.-C., Chen, C.-C., Tzeng, N.-S., and Liu, Y.-P. (2018). Effects of oxytocin on fear memory and neuroinflammation in a rodent model of posttraumatic stress disorder. Int. J. Mol. Sci. 19:3848. doi: 10.3390/ijms19123848
Weisman, O., Zagoory-Sharon, O., Schneiderman, I., et al. (2013). Plasma oxytocin distributions in a large cohort of women and men and their gender-specific associations with anxiety. Psychoneuroendocrinology 38, 694–697. doi: 10.1016/j.psyneuen.2012.08.01
Weiss, D. S., and Marmar, C. R. (1996). “The impact of event scale - revised,” in Assessing Psychological Trauma and PTSD, eds J. P. Wilson and T. M. Keane (New York, NY: Guilford Press), 399–411.
Welches, W. R., Brosnihan, K. B., and Ferrario, C. M. (1993). A comparison of the properties and enzymatic activities of three angiotensin processing enzymes: angiotensin converting enzyme, prolyl endopeptidase and neutral endopeptidase 24.11. Life Sci. 52, 1461–1480. doi: 10.1016/0024-3205(93)90108-f
Wigger, A., and Neumann, I. D. (1999). Periodic maternal deprivation induces gender-dependent alterations in behavioral and neuroendocrine responses to emotional stress in adult rats. Physiol. Behav. 66, 293–302. doi: 10.1016/s0031-9384(98)00300-x
Williams, T. D., Carter, D. A., and Lightman, S. L. (1985). Sexual dimorphism in the posterior pituitary response to stress in the rat. Endocrinology 116, 738–740. doi: 10.1210/endo-116-2-738
Windle, R. J., Kershaw, Y. M., Shanks, N., Wood, S. A., Lightman, S. L., and Ingram, C. D. (2004). Oxytocin attenuates stress-induced c-fos mRNA expression in specific forebrain regions associated with modulation of hypothalamo-pituitary-adrenal activity. J. Neurosci. 24, 2974–2982. doi: 10.1523/JNEUROSCI.3432-03.2004
Keywords: PTSD, pathophysiology, stress system, oxytocin, biomarkers, therapeutic targets
Citation: Carmassi C, Marazziti D, Mucci F, Della Vecchia A, Barberi FM, Baroni S, Giannaccini G, Palego L, Massimetti G and Dell’Osso L (2021) Decreased Plasma Oxytocin Levels in Patients With PTSD. Front. Psychol. 12:612338. doi: 10.3389/fpsyg.2021.612338
Received: 30 September 2020; Accepted: 24 March 2021;
Published: 01 July 2021.
Edited by:
Henri Julius, Universität Rostock, GermanyReviewed by:
Kathleen Ann Kendall-Tackett, Texas Tech University Health Science Center Amarillo, United StatesCopyright © 2021 Carmassi, Marazziti, Mucci, Della Vecchia, Barberi, Baroni, Giannaccini, Palego, Massimetti and Dell’Osso. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Donatella Marazziti, ZG1hcmF6emlAcHNpY28ubWVkLnVuaXBpLml0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.