
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol. , 01 March 2021
Sec. Health Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.611954
This article is part of the Research Topic Psychosocial Adjustment to Illness: Positive Adaptation and the Role of Body Image View all 3 articles
The experience of breast cancer and related treatments has notable effects on women's mental health. Among them, the subjective perception of the body or body image (BI) is altered. Such alterations deserve to be properly treated because they augment the risk for depression and mood disorders, and impair intimate relationships. A number of studies revealed that focused psychological interventions are effective in reducing BI issues related to breast cancer. However, findings are inconsistent regarding the dimension of such effects. This meta-analysis synthesizes and quantifies the efficacy of psychological interventions for BI in breast cancer patients and survivors. Additionally, since sexual functioning emerged as a relevant aspect in the BI distortions, we explored the efficacy of psychological interventions on sexual functioning related to BI in breast cancer patients and survivors. The literature search for relevant contributions was carried out in March 2020 through the following electronic databases: Scopus, PsycINFO, and ProQUEST. Only articles available in English and that featured psychological interventions for body image in breast cancer patients or survivors with controls were included. Seven articles with 17 dependent effect sizes were selected for this meta-analysis. Variables were grouped into: Body Image (six studies, nine dependent effect sizes) and Sexual Functioning Related to the Body Image in breast cancer patients and survivors (four studies, eight dependent effect sizes). The three-level meta-analysis showed a statistically significant effect for Body Image [g = 0.50; 95% CI (0.08; 0.93); p < 0.05] but no significant results for Sexual Functioning Related to Body Image [g = 0.33; 95% CI (−0.20; 0.85); p = 0.19]. These results suggest that psychological interventions are effective in reducing body image issues but not in reducing sexual functioning issues related to body image in breast cancer patients and survivors. Future review efforts may include gray literature and qualitative studies to better understand body image and sexual functioning issues in breast cancer patients. Also, high-quality studies are needed to inform future meta-analyses.
Breast cancer is one of the most common tumors among women (Ferlay et al., 2015; Andreis et al., 2018). Standard intervention approach includes surgery, adjuvant therapies, chemotherapy, hormonotherapy, and radiotherapy (Early Breast Cancer Trialists' Collaborative Group, 2011; Serletti et al., 2011). Despite a fairly good prognosis, cancer diagnosis and treatments concur to both negative physical and psychological long term-side effects that affect patients' and survivors' quality of life (QOL; Sterba et al., 2014; Ahmad et al., 2015; Williams and Jeanetta, 2016). Undesirable appearance-related side effects [i.e., loss or deformities in the breast(s), visible scarring, hair loss, skin discoloration, alopecia, muscle weakness, and weight fluctuation] alter the perception of Body Image (BI) and develop intensive negative feelings (Gorini et al., 2015; Fioretti et al., 2017; Yang et al., 2017).
BI is generally defined as “internal representation of one's own outer appearance” (Thompson et al., 1999, p. 4) that involves the mental representation of one's own body and related emotions within an overall sense of bodily self (Lewis-Smith et al., 2018; Sebri et al., 2020b). Perceptual (i.e., accuracy of estimated body size), attitudinal (i.e., subjective satisfaction about one's own body), cognitive (i.e., involvement in appearance belief about the body), affective (i.e., sensations and emotions), and behavioral dimensions (i.e., compensatory behaviors such as dieting and physical activity) are involved (Cash and Smolak, 2011). BI construct is indeed relevant because of impacts on the quality of life (Torres et al., 2020). Consequently, breast cancer patients and survivors' evaluation of their own physical appearance as well as attitudes toward the body notably change, especially in terms of femininity and sexuality (Maass et al., 2015; Sherman et al., 2018). Mastectomy surgery or conservation, for example, may threaten overall self-satisfaction and evoke multiple changes in body perception mediated by sensations within breast and chest never experienced before (Falbjork et al., 2013; Paterson et al., 2015). BI issues are strictly related to sexual functioning in breast cancer survivors. Sexual dysfunctions (i.e., sexual arousal, dyspareunia, fatigue, and loss or decrease in sexual desire and pleasure) occur frequently even beyond the acute phase of treatments, leading to dissatisfaction that becomes one of the most problematic aspects of survivors' life (Emilee et al., 2010; Male et al., 2016). Patients' and survivors' BI in terms of sexuality is altered by the fear of loss of fertility, induced menopause, and perception of sexual unattractiveness, linked also to perceived partner's greater difficulties to understand their feelings (Woertman and Van den Brink, 2012).
The subjective changed experience within one's own BI and related emotions impact on patients' and survivors' social relationships too (Dua et al., 2015; Triberti et al., 2019b). In general, women constantly self-scrutinize themselves compared to cultural stereotypes of physical appearance (Triberti et al., 2017a,b). Following the Self Discrepancy Theory by Higgins (1987), the discrepancy between one's own current and desired self-representations leads to feelings of dissatisfaction and emotional distress and promotes habitual self-surveillance and evaluation, according to theories of self-objectification (Fredrickson and Roberts, 1997). As a result, patients and survivors severely worry about physical appearance and develop the belief that others observe and evaluate their bodies continually (Hunter, 2015). In this regard, the construction of femininity and sexuality after illness depends not only on patients' and survivors' post-treatment experiences but also on the intrapsychic negotiation within their social and relational context (Male et al., 2016).
To sum up, a growing body of literature evidences that the experience of breast cancer seriously infringes patients' and survivors' BI and the general sense of self (Boquiren et al., 2013; Jabłoński et al., 2019) until years after diagnosis and treatments (Falk Dahl et al., 2010). For this reason, several psychological interventions have been proposed that address breast cancer survivors' BI issues and sexual functioning (Park et al., 2015). Most of these are programs based on cognitive-behavioral/existential, educational, supportive emotionally expressive, interpersonal, and psychosocial approaches (Blanco et al., 2014). Their main objectives are to decrease psychological distress providing problem-solving methods and relaxation and to modify the perception of one's own body. Furthermore, literature shows the efficacy of novel and mixed approaches including psychotherapy-based interventions, physical exercise, and art/dance therapy to improve well-being in cancer patients and survivors (Björneklett et al., 2013), as well as cosmetic educational programs to promote self-esteem (Park et al., 2015). For example, mixed interventions featuring psychological support and physical activity (aerobic and resistance training especially) promote personal strength and quality of life (Fong et al., 2012; Benton et al., 2014) as well as improvements in cognitive abilities such as attention, working memory, and decision making (Sebri et al., 2019, 2020a). Regarding type of session, structured group, couple intervention, and formal one-to-one psychotherapy are the main formats of support within clinical settings (Fingeret et al., 2014). Among different methodological approaches, Cognitive Behavioral Therapy (CBT) has been found particularly promising as a time-limited and goal-oriented psychotherapeutic approach (Fingeret et al., 2014).
With the aim of evaluating the usefulness of different programs and approaches, Lewis-Smith et al. (2018) highlighted that breast cancer patients and survivors perceive psychological interventions as acceptable, feasible, and effective to address BI issues (McLean et al., 2011). Nevertheless, evaluations of psychological interventions' long-term impact are limited due to a general lack of methodological rigor across studies (Lewis-Smith et al., 2016, 2018). Most psychological interventions do not adopt an exclusive focus on BI, which tends to be addressed as a small component of larger interventions. Also, there is no clear, unified information about the dimension of such positive effects in the literature. For this reason, a meta-analytic approach to the issue is in order.
The aim of this study is to evaluate the efficacy of different kinds of psychological interventions on BI and sexual functioning in breast cancer patients and breast cancer survivors. Specifically, this study assessed which typology of psychological intervention is the most effective to improve BI in breast cancer patients and survivors. Based on the existing literature, we expected that psychological interventions would promote benefits on BI and sexual functioning related to BI in cancer patients and survivors.
The literature search for relevant contributions was carried out in March 2020 through an electronic computer-based search on the following databases: Scopus, PsycINFO, and ProQUEST. The PICOS model was used as a tool for developing search strategies for this meta-analysis and eligibility criteria. This model includes the patient or problem (P), the intervention or exposure (I), the comparison intervention or exposure (C), and the clinical outcome of interest (O) (Eriksen and Frandsen, 2018), and (S) Study type. Following this model, records were searched using “psychological intervention” OR “psychological therapy” OR “psychological support” OR “psychotherapy” AND “body esteem” OR “bodily self” OR “body image” OR “body consciousness” AND “breast cancer” as key terms in the title or in the abstract of the manuscripts. Only articles available in English were included. The authors did place a priori restrictions by excluding “gray literature” such as conference abstracts, other non-peer-reviewed sources, and doctoral dissertation in the attempt to improve review manageability (Beatty et al., 2018). No other limitations were placed in reference to age of participants, statistical presentation of results, time period of publications, or study type. Studies were included in meta-analysis if they met the following criteria: (1) studies that examined the efficacy of psychological interventions for BI on cancer patients or survivors compared with a control group; (2) studies that included a measure of BI that was consistent with any dimension of BI (e.g., subjective evaluation and/or perceptual); (3) between-group outcome data of mixed-method design studies or between-group research studies. If different times were analyzed in the study, we considered only the last outcome point available; (4) studies written in English. Previous studies showed that there was nearly no evidence of a systematic bias from English language restriction in meta-analyses (e.g., Morrison et al., 2012; McKenzie et al., 2019; see Table 1 for a detailed description of the search strategy and eligibility criteria).
The effect sizes (Hedges' g) were reported or computed based on the information provided in the article. If an article did not provide appropriate statistics to compute effect sizes, it was excluded from this meta-analysis. Of note, since we only aimed to explore the efficacy of psychological interventions for BI in breast cancer patients and survivors, we decided to exclude studies that did not use psychological interventions, studies that explicitly state in the article that the intervention was not conducted by trained psychologists, or studies in which the psychological intervention is not used alone, but was administered in combination with other educational techniques (which makes it difficult to understand the effectiveness of the psychological interventions). This meta-analysis has been registered with the International Prospective Register for Systematic Reviews with ID number CRD42020203021 (available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020203021).
During the first screening stage, two researchers (VS and ID) independently coded the studies. After removing duplicates, the titles and abstracts of 180 articles (20% of 903 articles potentially relevant for inclusion) were independently screened based on the inclusion criteria, in order to exclude irrelevant studies for this meta-analysis. Inter-rater agreement coefficient (Cohen's k; McHugh, 2012) was equal to 0.91. Discrepancies between the raters were resolved by referring back to the original article and through discussions with the third author (ST) to reach a consensus. In the next stage, 20% of 32 full-text articles assessed for eligibility (six articles) were independently screened by researchers to assess their relevance. Inter-rater agreement coefficient (Cohen's k) was equal to 1.00.
For each of the selected study, two researchers extracted in a blinded manner (1) the basic information (e.g., authors, publication year), (2) the type of psychological intervention, (3) the type of control group (alternative intervention vs. no intervention), (4) the format of the intervention (individuals, groups, couples), (5) the sample size and sample characteristics [i.e., participants (patients or survivors); mean age of participants], and (6) the instruments used in the study and the variables explored. Inter-rater reliability analysis revealed a perfect agreement between researchers was reached.
For what regard the studies included in the meta-analysis, the assessment of study quality was conducted by the first two authors of this manuscript independently. Discrepancies were resolved through discussions with the third author. We adapted the eight-criteria defined by Cuijpers et al. (2010) and already used in other meta-analyses for assessing study quality (David et al., 2018; Hoppen and Morina, 2020). We also included three additional items to further explore the quality of the studies included in this meta-analysis (see Table 2).
Independent assessments of the methodological quality of each study were conducted by three researchers (VS, ID, and ST) using the Cochrane risk of bias tool, version 2 (RoB 2; Higgins et al., 2011). The RbB 2 is based on some domains related to the quality appraisal of the studies and their biases (Sterne et al., 2019). For each study, the results of the risk of bias were differentiated as “low risk,” “some concerns,” and “high risk” by assessing each domain and its related specific risks. The overall risk of the study is considered low if the risk assessment of all the domains resulted in low (Higgins et al., 2011). Discrepancies in the quality of the studies were resolved through discussions between researchers.
Data analyses were conducted via the software R (the rma.mv function of the metafor package; Viechtbauer and Viechtbauer, 2015) and the SPSS Statistical Software 20.0.
We conducted six major sets of analyses:
1) First of all, an outlier analysis was conducted on the effect sizes included in this meta-analysis. An outlying effect was present when standardized z values exceeded +3.29 (Tabachnick and Fidell, 2013);
2) Hedges' g was computed for each comparison between the experimental and control groups using means and standard deviations. Hedges' g was interpreted as small (≤ 0.20), medium (=0.50), or large (≥0.80) (Cohen, 1988; Chalmers et al., 2014). Positive values indicate that the outcome is higher in breast cancer patients or survivors who received psychological interventions compared to participants who did not receive a psychological intervention;
3) Meta-analyses were run in order to assess the efficacy of psychological interventions on Body Image (Outcome 1) and Sexual Functioning Related to Body Image (Outcome 2) in breast cancer patients and survivors. In traditional meta-analysis, an important assumption is the independence between the included effect sizes (Rosenthal and Rubin, 1986; Assink and Wibbelink, 2016). This allows avoidance of overconfidence in the results and “inflated” estimates (Van den Noortgate et al., 2013; Assink and Wibbelink, 2016). Since this important precondition is violated in this meta-analysis, we used a three-level analysis (Assink and Wibbelink, 2016; Assink et al., 2018; van der Put et al., 2018; van der Put et al., 2020);
4) To deal with dependency of effect sizes (Van den Noortgate et al., 2013; Cheung, 2014), three levels of the model were included in the analysis:
a) Level 1 variance: It refers to the sampling variance of the individual effect sizes;
b) Level 2 variance: It refers to the variance between effect sizes from the same study;
c) Level 3 variance: It refers to the differences between studies.
5) (Level 2 and Level 3 variances are included as random terms in the model);
6) Publication bias was explored by inspecting the funnel plot graphs' asymmetry (Sterne and Egger, 2001) conducted with the trim-and-fill method and .rma function. If publication bias is absent, the funnel plot should assume a symmetric funnel shape. We also assessed whether small effects were underrepresented and whether large effects were missing (a great number of “missing” effect sizes suggested a bias to a greater extent; Assink et al., 2018) observing the white dots in the funnel plot (Higgins and Thompson, 2002).
7) Lastly, the presence or absence of heterogeneity across studies was tested by the Q statistic (Hedges and Olkin, 1985). The extent of such heterogeneity across studies was assessed using the I2 index (Higgins and Thompson, 2002). I2 index of 25, 50, and 75% indicate low, moderate, and high heterogeneity, respectively (Higgins et al., 2003). We also examined how the total variance was distributed over the three levels (Level 1, Level 2, and Level 3; Cheung 2014, formula 14, p. 2015). In order to determine whether the variance in Level 2 and in Level 3 were significant, we performed two separate one-tailed log-likelihood-ratio-tests. In these analyses the outcome of the full model was compared to the outcome of a model excluding one of the variance parameters. The model parameters were estimated using the restricted maximum likelihood estimation method. Lastly, we computed a prediction interval analysis (e.g., IntHout et al., 2016) in order to explore an approximate 95% range of underlying effects.
The meta-analysis was conducted following the guidelines and checklist of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA; Liberati et al., 2009; Moher et al., 2009; Figure 1). Table 3 summarizes the Participants, Interventions, Control group intervention, and Outcome measures included in this meta-analysis. The initial search process returned 921 potentially relevant articles. After removing duplicates, 903 studies remained. Two researchers reviewed and screened these studies by reading the title and abstract, and based on the inclusion criteria, 32 were full-text screened. This selection procedure yielded a subset of seven usable empirical studies (Table 4). These studies were published between 2008 and 2014 and included a total sample size of 366 participants and 17 individual effect sizes. Each variable assessed in the selected studies was carefully analyzed by the authors and classified in the Body Image outcome (Outcome 1). Since the BI issues are strictly related to sexual functioning in breast cancer patients and survivors and sexual dysfunctions occur frequently even beyond the acute phase of treatments, we decided to explore also the effect of psychological interventions on Sexual Functioning Related to Body Image in breast cancer patients and survivors (Outcome 2).
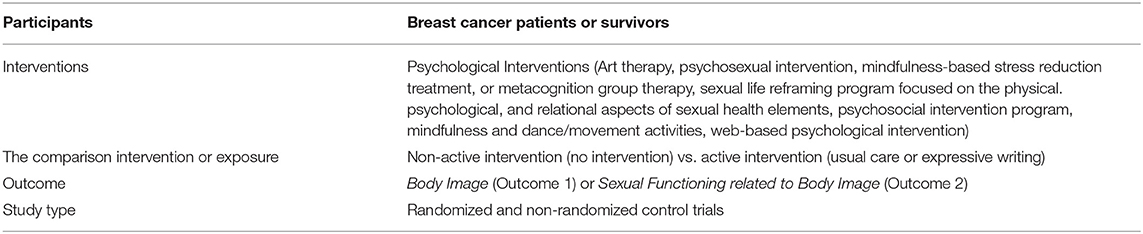
Table 3. Description of the studies included in the meta-analysis following the PICOS model, The PICOS measure.
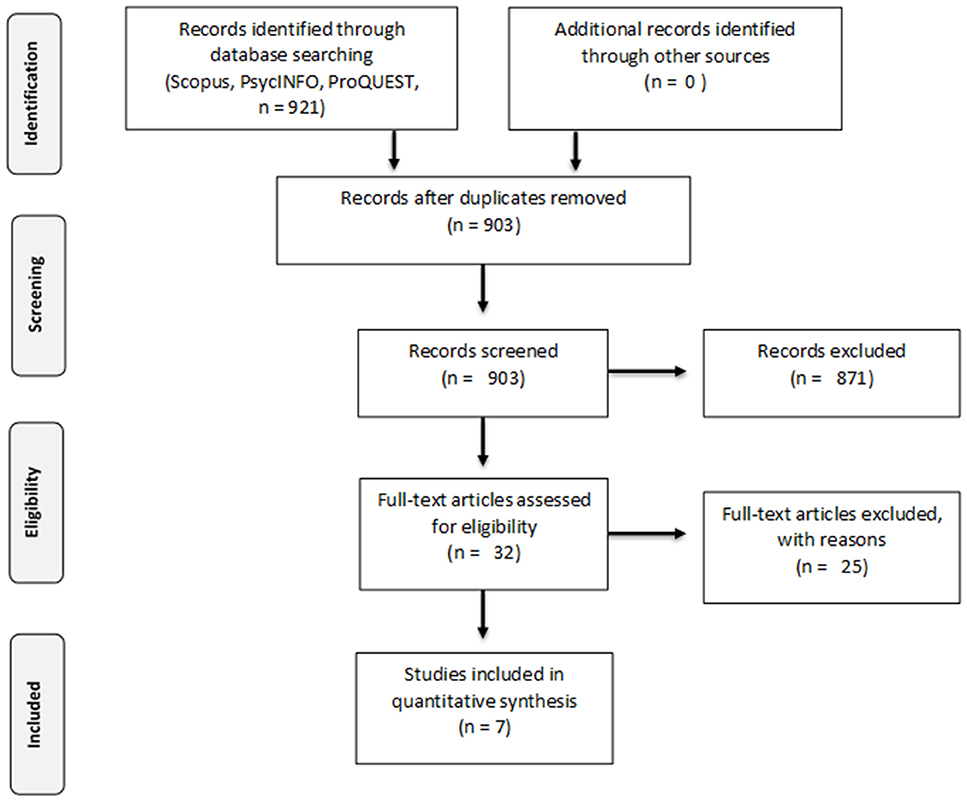
Figure 1. PRISMA flow diagram (Moher et al., 2009).
Outcome 1 includes six studies and nine dependent effect sizes on personal satisfaction with BI when naked or when dressed, BI distress, and BI appreciation. Outcome 2 includes four studies and eight dependent effect sizes related to sexual functioning, feeling attractive, sexual desire frequency, sexual interest, sexual dysfunction, and sexual satisfaction.
Details of each study included in the meta-analysis as well as descriptions of the effect sizes are provided in Tables 4, 5.
The assessment of study quality revealed that most studies had an adequate quality (5 or more points out of 10 points). The details of the assessment of study quality included in this meta-analysis are reported in Table 6.
The quality appraisal of the selected studies was assessed through the Cochrane risk of bias tool, version 2 (RoB 2; Higgins et al., 2011). The researchers reached an overall consensus on the quality appraisal evaluation of the seven selected studies and the results are reported in Table 7. Only one (Sebastián et al., 2008) of the included studies had high risk of bias in sequence generation. Randomization methods of the other studies were clear, even if they did not explain how participants were allocated. About the blinding of participants and personnel, only Sherman et al. (2018) specified it. Sebastián et al. (2008) claimed the blinding of outcome data, while in the other studies it is unclear. Three of seven studies (Sebastián et al., 2008; Crane-Okada et al., 2012; Sherman et al., 2018) reported attrition bias because they had a dropout rate. No selective reporting bias was detected in included studies. Finally, three of seven studies (Kalaitzi et al., 2007; Svensk et al., 2009; Rahmani et al., 2014) reported other biases in their experimental studies. Other studies are unclear or the risk of bias was assessed as low.
The outlier analysis conducted on all the dependent effect sizes included in this meta-analysis highlighted that standardized z values not exceeded ±3.29 (Table 5). Thus, all the effect sizes were included in the analyses.
The first meta-analysis explored the efficacy of psychological intervention on breast cancer patients' and survivors' Body Image (Table 8). Six studies and nine non-independent effect sizes were included in the analysis (Figure 2).
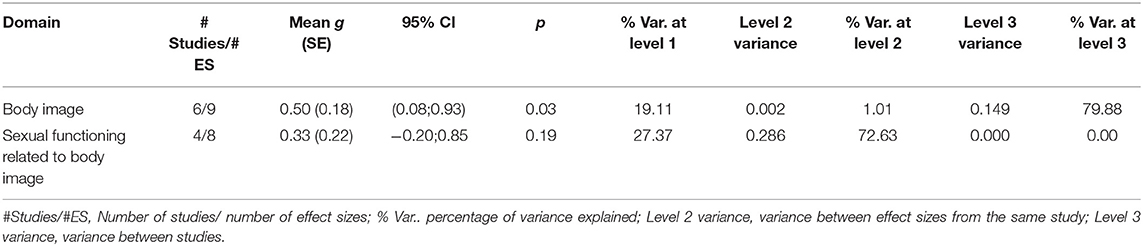
Table 8. Results for the overall mean effect sizes of the two outcomes (body image and sexual functioning).
The random effect three-level analysis showed a medium, statistically significant effect of psychological interventions on breast cancer patients' and survivors' BI [g = 0.50; 95% CI (0.08; 0.93); p < 0.05].
The funnel plot with trim and fill function shows no visual asymmetry and suggests a low probability of publication bias (Figure 3).
The heterogeneity was significant [Q (8) = 33.75, p < 0.001, I2 = 80.89]. The 19.11% of the total variance can be attributed to the sampling variance, 1.01% can be attributed to within studies variance (the differences between effect sizes within studies, and 79.88% can be attributed to between-studies variance (differences between studies). Log-likelihood tests revealed a non-statistically significant variance within-study (p = 0.89), and between-study (p = 0.07). The prediction interval is within −0.49 to 1.50.
The second meta-analysis explored the efficacy of psychological intervention on breast cancer patients' and survivors' Sexual Functioning Related to Body Image (Table 8). The dataset was composed by four studies and eight dependent effect sizes (Figure 4).
The three-level meta-analysis showed a non-statistical significant effect size {g = 0.33 [95% CI (−0.20; 0.85); p = 0.19]}, suggesting that psychological interventions do not have an impact on breast cancer patients and survivors' Sexual Functioning Related to Body Image. Interestingly, one study highlighted a negative effect size in sexual functioning (g = −0.84) (Rahmani et al., 2014).
The funnel plot with trim and fill method (Figure 5) reveals only one missing effect size in the (bottom) right side of the graph, suggesting a low probability of publication bias.
The heterogeneity was significant [Q (7) = 23.60, p < 0.01, I2 = 72.63]. The 27.37% of the total variance can be attributed to the sampling variance, 72.63% can be attributed to within-studies variance, and 0% can be attributed to between-studies variance. Log-likelihood tests revealed a statistically significant variance within-study (p = 0.02), and a no-statistically significant variance between-study (p = 1.00). The prediction interval ranged between a large negative and a large positive effect size (−1.04 to 1.69).
The current study reviewed the literature prior to March 2020 about the efficacy of psychological interventions for BI and sexual functioning related to BI in breast cancer patients and survivors using meta-analytic techniques. BI is a crucial component of the experience of cancer, and especially of breast cancer. Indeed, patients' and survivors' bodies are not only affected by the disease but also by the secondary consequences of treatment such as surgery and chemotherapy (Munzone et al., 2019; Oliveri et al., 2020). Psycho-oncologists are well aware that alterations of BI go way beyond a mere “self-appreciation” issue: the body is felt as less whole, less feminine, and as a source of danger and betrayal (Rubin and Tanenbaum, 2011; Triberti et al., 2019a). Women are directly affected by this perception in their intimacy and sexual life, as well as in their perceived ability to give birth and nurture (Markopoulos et al., 2009; Faccio et al., 2020). Since body image affects patients and survivors' quality of life strongly, relevant changes in BI impact on psychological well-being in terms, for example, of self-esteem and social life. Identifying psychological interventions which impact on patients' and survivors' BI is relevant to sustain the adjustment to illness, especially to chronic illness as breast cancer. Findings suggested that different types of psychological interventions are effective for breast cancer patients' and survivors' BI with a medium effect size. This suggests that the improvements are not modality-specific but there are various explanations for the benefits in the studies reviewed. However, in this meta-analysis, cognitive, social, and sexual interventions as well as art therapy, mindfulness, and web-based treatments are assessed as types of psychological interventions. In addition, except for the single session in the web-based psychological treatment by Sherman et al. (2018), psychological interventions are extended and consistent over time (from 5 to 14 weeks for each intervention). Moreover, in these studies professionals delivering psychological interventions are psychologists and draw on their training to propose mixed methods to engage many aspects of BI linked to psychological, emotional, and social changes. This may enable breast cancer patients and survivors to address various aspects of BI without self-fragmentation. Although BI received attention in the psycho-oncology literature in the last few decades, a first issue regarding BI conceptualization in breast cancer patients and survivors. Given the complexity of BI definition as a multidimensional construct, positive outcomes on BI do not depend on specific characteristics of psychological interventions but in meeting patients and survivors needs and preferences, as affirmed by Möller et al. (2019). Personalized interventions and collaborative psychological interventions (e.g., Smith and George, 2012; Aschieri et al., 2015; Durosini et al., 2017) are needed to deal with BI issues taking into account any individual breast cancer patient's or survivor's situation and experiences. Referring to sexual functioning, literature reveals the association between BI and sexual functioning in breast cancer patients and survivors (Woertman and Van den Brink, 2012). BI issues interfere with sexual functioning due to the connection between how a woman perceives her own body and sexuality (Seal, Andrea and Cindy). This could be particularly relevant for breast cancer patients and survivors who have to cope with an ill body during and/or after oncological treatments. However, in this meta-analysis sexual functioning does not show improvement among the reviewed contributions. One possible explanation might be related to the typology of psychological interventions in which sexual functioning is not the main objective of interest. Moreover, some studies, such as the art therapy program by Svensk et al. (2009) in the field of cognitive-based interventions and the study of Rahmani et al. (2014), do not focus on sexual issues specifically. Without a specific focus on sexuality, it is possible that this contribution's intervention was not effective in this regard.
In addition, it has been suggested that BI is extensively entwined with social ideals in a particular place and time (Perdue et al., 2018). The comparison between the actual and ideal appearance can increase the self-objectification that is strongly connected to disease in sexual functioning (Bishop, 2015). This is particularly evident in breast cancer patients and survivors because tumor experience affects cognitions and perceptions about BI with direct influences on, for example, perception of being attractive and sexual desire (Benoit, 2020). Relevant changes in the body can be both visible (e.g., scarring and hair loss) and not apparent (e.g., interoception or the inner perception of the body). This suggests that sexual functioning has to be assessed as one of the main aspects of interest related to BI, especially in breast cancer patients and survivors. Finally, the low number of available studies focused on BI issues shows that BI has not yet been explored enough in the current literature and sustains the need to promote psychological interventions in this field.
Drawing researchers' attention to the multiple characteristics associated with BI, this study aimed to explore the efficacy of psychological interventions by involving both individual and relational aspects of BI. Findings show the positive outcomes on BI, thanks to both individual and group psychological interventions conducted by trained professionals. The usage of strict criteria for data selection and cultural differences could be limitations of this meta-analysis. Additionally, keywords related to specific types of psychological interventions were not used as well as gray literature and doctoral dissertation were excluded from the selected studies. Thus, it is possible that some studies were not identified as fulfilling the selection criteria adequately and the literature search might be not sufficient to provide a comprehensive and full picture of the evidence. In the same line, only three databases were used for the study research without relevant medical databases related to breast cancer issues. Furthermore, the authors suggest a cautious evaluation of the funnel plot and the trim-and-fill method due to their low sensitivity to detect publication bias when the number of studies is small as in this meta-analysis. At the same time, the high statistical variance across study designs, as result of different levels of clinical and methodological diversity (e.g., the inclusion of a non-randomized trial), is a limitation of the study.
Regarding future directions, research may feature more psychological characteristics, improve measurements, and change inclusion criteria of study selection. Additionally, it may be interesting to explore the effectiveness of psychological interventions on cancer patients and survivors moderated by the type of psychological intervention and the typology of participants. Third, qualitative studies could be reviewed to assess the individual perceptions of patients and survivors with the aim to explore BI dimensions and implement personalized psychological interventions centered on the lived illness. Recommendation for clinical practice suggests that psychological interventions have to assess BI and related constructs in terms of BI appreciation as well as sexual functioning. Therefore, these findings highlight the foundation for individualized aids in meeting breast cancer patients' and survivors' needs, given more space to sexual functioning and their issues linked to cognitive and social processes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
VS and ID conceived the ideas presented in the article and wrote the first draft. VS, ID, and ST performed the literature search. ID performed the meta-analysis. ST contributed to the interpretation of the data, provided comments on the ideas presented, and edited the manuscript. GP contributed with important intellectual contents and supervised the whole process. All listed authors gave final approval of the version to be published.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5 × 1,000 funds for IEO European Institute of Oncology IRCCS. VS is a Ph.D. student within the European School of Molecular Medicine (SEMM). ID was supported by Fondazione Umberto Veronesi.
Ahmad, S., Fergus, K., and McCarthy, M. (2015). Psychosocial issues experienced by young women with breast cancer: the minority group with the majority of need. Curr. Opin. Support. Palliat. Care 9, 271–278. doi: 10.1097/SPC.0000000000000162
Andreis, F., Meriggi, F., Codignola, C., Frigoli, I., Prochilo, T., Mutti, S., et al. (2018). Impact of a psycho-educational team in early breast cancer patients' coping strategies: the Venere project. Rev. Recent Clin. Trials 13, 274–280. doi: 10.2174/1574887113666180409152025
Aschieri, F., De Saeger, H., and Durosini, I. (2015). L'évaluation thérapeutique et collaborative: preuves empiriques. Prat. Psychol. 21, 307–317. doi: 10.1016/j.prps.2015.09.005
Assink, M., Spruit, A., Schuts, M., Lindauer, R., van der Put, C. E., and Stams, G. J. J. (2018). The intergenerational transmission of child maltreatment: a three-level meta-analysis. Child Abuse Neglect. 84, 131–145. doi: 10.1016/j.chiabu.2018.07.037
Assink, M., and Wibbelink, C. J. (2016). Fitting three-level meta-analytic models in R: a step-by-step tutorial. Quant. Methods Psychol. 12, 154–174. doi: 10.20982/tqmp.12.3.p154
Avalos, L., Tylka, T. L., and Wood-Barcalow, N. (2005). The body appreciation scale: development and psychometric evaluation. Body Image 2, 285–297. doi: 10.1016/j.bodyim.2005.06.002
Beatty, L., Kemp, E., Butow, P., Girgis, A., Schofield, P., Turner, J., et al. (2018). A systematic review of psychotherapeutic interventions for women with metastatic breast cancer: context matters. Psycho-oncology 27, 34–42. doi: 10.1002/pon.4445
Benoit, L. M. (2020). Young adult breast cancer survivors' experiences with body image changes (Ph.D. thesis). Oregon State University, Oregon, United States.
Benton, M. J., Schlairet, M. C., and Gibson, D. R. (2014). Change in quality of life among breast cancer survivors after resistance training: is there an effect of age? J. Aging Phys. Act., 22, 178–185. doi: 10.1123/japa.2012-0227
Bishop, D. M. (2015). The consequences of self-objectification: Investigating the impact of body image on female sexual functioning (BA), Ball State University, Muncie, United States.
Björneklett, H. G., Rosenblad, A., Lindemalm, C., Ojutkangas, M. L., Letocha, H., Strang, P., et al. (2013). Long-term follow-up of a randomized study of support group intervention in women with primary breast cancer. J. Psychosom. Res. 74, 346–353. doi: 10.1016/j.jpsychores.2012.11.005
Blanco, C., Markowitz, J. C., Hershman, D. L., Levenson, J. A., Wang, S., and Grann, V. R. (2014). A pilot study of interpersonal psychotherapy for depressed women with breast cancer. Am. J. Psychother. 68, 489–495. doi: 10.1176/appi.psychotherapy.2014.68.4.489
Boquiren, V. M., Esplen, M. J., Wong, J., Toner, B., and Warner, E. (2013). Exploring the influence of gender-role socialization and objectified body consciousness on body image disturbance in breast cancer survivors. Psycho-oncology 22, 2177–2185. doi: 10.1002/pon.3271
Cash, T. F., and Smolak, L. (Eds.). (2011). Body Image: A Handbook of Science, Practice, and Prevention. New York, NY: Guilford Press.
Chalmers, J. A., Quintana, D. S., Abbott, M. J., and Kemp, A. H. (2014). Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front. Psychiatry 5:80. doi: 10.3389/fpsyt.2014.00080
Cheung, M. W. L. (2014). Modeling dependent effect sizes with three-level meta- analyses: a structural equation modeling approach. Psychol. Methods 19, 211–229. doi: 10.1037/a0032968
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences, 2nd Edn. Hillsdale, NJ: Erlbaum.
Crane-Okada, R., Kiger, H., Sugerman, F., Uman, G. C., Shapiro, S. L., Wyman-McGinty, W., et al. (2012). Mindful movement program for older breast cancer survivors: a pilot study. Cancer Nurs. 35, E1–E13. doi: 10.1097/NCC.0b013e3182280f73
Cuijpers, P., van Straten, A., Bohlmeijer, E., Hollon, S. D., and Andersson, G. (2010). “The effects of psychotherapy for adult depression are overestimated: a meta-analysis of study quality and effect size,” in Database of Abstracts of Reviews of Effects (DARE): Quality-Assessed Reviews. Centre for Reviews and Dissemination (UK). doi: 10.1017/S0033291709006114
David, D., Cotet, C., Matu, S., Mogoase, C., and Stefan, S. (2018). 50 years of rational-emotive and cognitive-behavioral therapy: a systematic review and meta-analysis. J. Clin. Psychol. 74, 304–318. doi: 10.1002/jclp.22514
Dua, P., Heiland, M. F., and Kracen, A. C. (2015). Cancer-related hair loss: a selective review of the alopecia research literature. Psycho-Oncology 26, 438–443. doi: 10.1002/pon.4039
Durosini, I., Tarocchi, A., and Aschieri, F. (2017). Therapeutic assessment with a client with persistent complex bereavement disorder: a single-case time-series design. Clin. Case Stud. 16, 295–312. doi: 10.1177/1534650117693942
Early Breast Cancer Trialists' Collaborative Group (2011). Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials. Lancet 378, 1707–1716. doi: 10.1016/S0140-6736(11)61629-2
Emilee, G., Ussher, J. M., and Perz, J. (2010). Sexuality after breast cancer: a review. Maturitas 66, 397–407. doi: 10.1016/j.maturitas.2010.03.027
Eriksen, M. B., and Frandsen, T. F. (2018). The impact of patient, intervention, comparison, outcome (PICO) as a search strategy tool on literature search quality: a systematic review. J. Med. Libr. Assoc. 106:420. doi: 10.5195/JMLA.2018.345
Faccio, F., Mascheroni, E., Ionio, C., Pravettoni, G., Peccatori, F. A., Pisoni, C., et al. (2020). Motherhood during or after breast cancer diagnosis: a qualitative study. Eur. J. Cancer Care 29:e13214. doi: 10.1111/ecc.13214
Falbjork, U., Rasmussen, B. H., Karlsson, S., and Salander, P. (2013). Aspects of body image after mastectomy due to breast cancer—a two-year follow-up study. Eur. J. Oncol. Nurs. 17, 340–345. doi: 10.1016/j.ejon.2012.09.002
Falk Dahl, C. A., Reinertsen, K. V., Nesvold, I. L., Fosså, S. D., and Dahl, A. A. (2010). A study of body image in long–term breast cancer survivors. Cancer 116, 3549–3557. doi: 10.1002/cncr.25251
Ferlay, J., Soerjomataram, I., Dikshit, R., Eser, S., Mathers, C., Rebelo, M., et al. (2015). Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 136, E359–E386. doi: 10.1002/ijc.29210
Fingeret, M. C., Teo, I., and Epner, D. E. (2014). Managing body image difficulties of adult cancer patients: lessons from available research. Cancer 120, 633–641. doi: 10.1002/cncr.28469
Fioretti, C., Mazzocco, K., and Pravettoni, G. (2017). “Psychological support in breast cancer patients: a personalized approach,” in Breast Cancer, eds U. Veronesi, A. Goldhirsch, P. Veronesi, O. D. Gentilini, and M. C. Leonardi (Cham: Springer), 841–847. doi: 10.1007/978-3-319-48848-6_73
Fong, D. Y., Ho, J. W., Hui, B. P., Lee, A. M., Macfarlane, D. J., Leung, S. S., et al. (2012). Physical activity for cancer survivors: meta-analysis of randomised controlled trials. BMJ (Clin. Res. Ed.), 344:e70. doi: 10.1136/bmj.e70
Fredrickson, B. L., and Roberts, T. A. (1997). Objectification theory: toward understanding women's lived experiences and mental health risks. Psychol. Women Q. 21, 173–206. doi: 10.1111/j.1471-6402.1997.tb00108.x
Galiano-Castillo, N., Ariza-García, A., Cantarero-Villanueva, I., Fernández-Lao, C., Díaz-Rodríguez, L., and Arroyo-Morales, M. (2014). Depressed mood in breast cancer survivors: associations with physical activity, cancer-related fatigue, quality of life, and fitness level. Eur. J. Oncol. Nurs. 18, 206–210. doi: 10.1016/j.ejon.2013.10.008
Ganz, P. A., Schag, C. A. C., Lee, J. J., and Sim, M. S. (1992). The CARES: a generic measure of health-related quality of life for patients with cancer. Qual. Life Res. 1, 19–29. doi: 10.1007/BF00435432
Gorini, A., Mazzocco, K., Gandini, S., Munzone, E., McVie, G., and Pravettoni, G. (2015). Development and psychometric testing of a breast cancer patient-profiling questionnaire. Breast Cancer 7:133. doi: 10.2147/BCTT.S80014
Hedges, L. V., and Olkin, I. (1985). Statistical Methods for Metaanalysis. Orlando, FL: Academic Press.
Higgins, E. T. (1987). Self-discrepancy: a theory relating self and affect. Psychol. Rev. 94, 319–340. doi: 10.1037/0033-295X.94.3.319
Higgins, J. P., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 343:d5928. doi: 10.1136/bmj.d5928
Higgins, J. P., and Thompson, S. G. (2002). Quantifying heterogeneity in a meta-analysis. Stat. Med. 21, 1539–1558. doi: 10.1002/sim.1186
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Hoppen, T. H., and Morina, N. (2020). Is high-quality of trials associated with lower treatment efficacy? A meta-analysis on the association between study quality and effect sizes of psychological interventions for pediatric PTSD. Clin. Psychol. Rev. 78:101855. doi: 10.1016/j.cpr.2020.101855
Hopwood, P., Fletcher, I., Lee, A., and Al Ghazal, S. (2001). A body image scale for use with cancer patients. Eur. J. Cancer 37, 189–197. doi: 10.1016/S0959-8049(00)00353-1
Hunter, R. (2015). Changes in body image and sexuality in rural breast cancer survivors during a weight loss and weight maintenance intervention (Ph.D. dissertation). University of Kansas, Kanas, United States.
IntHout, J., Ioannidis, J. P., Rovers, M. M., and Goeman, J. J. (2016). Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open 6:7. doi: 10.1136/bmjopen-2015-010247
Jabłoński, M. J., Mirucka, B., Streb, J., Słowik, A. J., and Jach, R. (2019). Exploring the relationship between the body self and the sense of coherence in women after surgical treatment for breast cancer. Psycho-Oncology 28, 54–60. doi: 10.1002/pon.4909
Jun, E. Y., Kim, S., Chang, S. B., Oh, K., Kang, H. S., and Kang, S. S. (2011). The effect of a sexual life reframing program on marital intimacy, body image, and sexual function among breast cancer survivors. Cancer Nurs. 34, 142–149. doi: 10.1097/NCC.0b013e3181f1ab7a
Kalaitzi, C., Papadopoulos, V. P., Michas, K., Vlasis, K., Skandalakis, P., and Filippou, D. (2007). Combined brief psychosexual intervention after mastectomy: effects on sexuality, body image, and psychological well-being. J. Surg. Oncol. 96, 235–240. doi: 10.1002/jso.20811
Lewis-Smith, H., Diedrichs, P. C., and Harcourt, D. (2018). A pilot study of a body image intervention for breast cancer survivors. Body Image 27, 21–31. doi: 10.1016/j.bodyim.2018.08.006
Lewis-Smith, H., Diedrichs, P. C., Rumsey, N., and Harcourt, D. (2016). A systematic review of interventions on body image and disordered eating outcomes among women in midlife. Int. J. Eat. Disord. 49, 5–18. doi: 10.1002/eat.22480
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., et al. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 62, e1–e34. doi: 10.1016/j.jclinepi.2009.06.006
Maass, S. W., Roorda, C., Berendsen, A. J., Verhaak, P. F., and de Bock, G. H. (2015). The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: a systematic review. Maturitas 82, 100–108. doi: 10.1016/j.maturitas.2015.04.010
Male, D. A., Fergus, K. D., and Cullen, K. (2016). Sexual identity after breast cancer: sexuality, body image, and relationship repercussions. Curr. Opin. Support. Palliat. Care 10, 66–74. doi: 10.1097/SPC.0000000000000184
Markopoulos, C., Tsaroucha, A. K., Kouskos, E., Mantas, D., Antonopoulou, Z., and Karvelis, S. (2009). Impact of breast cancer surgery on the self-esteem and sexual life of female patients. J. Int. Med. Res. 37, 182–188. doi: 10.1177/147323000903700122
McHugh, M. L. (2012). Interrater reliability: the kappa statistic. Biochem. Med. 22, 276–282. doi: 10.11613/BM.2012.031
McKenzie, J. E., Brennan, S. E., Ryan, R. E., Thomson, H. J., Johnston, R. V., and Thomas, J. (2019). Chapter 3: defining the criteria for including studies and how they will be grouped for the synthesis. Cochrane Handbook for Systematic Reviews of Interventions Version, 6. doi: 10.1002/9781119536604.ch3
McLean, S. A., Paxton, S. J., and Wertheim, E. H. (2011). A body image and disordered eating intervention for women in midlife: a randomized controlled trial. J. Consult. Clin. Psychol. 79, 751–758. doi: 10.1037/a0026094
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and The P RISMA Group (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Möller, U. O., Beck, I., Ryden, L., and Malmström, M. (2019). A comprehensive approach to rehabilitation interventions following breast cancer treatment-a systematic review of systematic reviews. BMC Cancer 19:472. doi: 10.1186/s12885-019-5648-7
Munzone, E., Bagnardi, V., Campenn,ì, G., Mazzocco, K., Pagan, E., Tramacere, A., et al. (2019). Preventing chemotherapy-induced alopecia: a prospective clinical trial on the efficacy and safety of a scalp-cooling system in early breast cancer patients treated with anthracyclines. Br. J. Cancer 121, 325–331. doi: 10.1038/s41416-019-0520-8
Oliveri, S., Ongaro, G., Durosini, I., Curigliano, G., and Pravettoni, G. (2020). Breast implant-associated anaplastic large cell lymphoma: emotional impact and guidelines for psychological support. Breast Cancer Res. Treat. 181, 221–224. doi: 10.1007/s10549-020-05601-w
Park, H. Y., Kim, J. H., Choi, S., Kang, E., Oh, S., Kim, J. Y., et al. (2015). Psychological effects of a cosmetic education programme in patients with breast cancer. Eur. J. Cancer Care 24, 493–502. doi: 10.1111/ecc.12290
Paterson, C. L., Lengacher, C. A., Donovan, K. A., Kip, K. E., and Tofthagen, C. S. (2015). Body image in younger breast cancer survivors: a systematic review. Cancer Nurs. 39, E39–58 [Epub ahead of print]
Perdue, T. O., Schreier, A., Swanson, M., Neil, J., and Carels, R. (2018). Evolving self view and body image concerns in female postoperative bariatric surgery patients. J. Clin. Nurs. 27, 4018–4027. doi: 10.1111/jocn.14527
Rahmani, S., Talepasand, S., and Ghanbary-Motlagh, A. (2014). Comparison of effectiveness of the metacognition treatment and the mindfulness-based stress reduction treatment on global and specific life quality of women with breast cancer. Iran. J. Cancer Prev. 7:184.
Rosenthal, R., and Rubin, D. B. (1986). Meta-analytic procedures for combining studies with multiple effect sizes. Psychol. Bull. 99, 400–406. doi: 10.1037/0033-2909.99.3.400
Rubin, L. R., and Tanenbaum, M. (2011). “Does that make me a woman?” Breast cancer, mastectomy, and breast reconstruction decisions among sexual minority women. Psychol. Women Q. 35, 401–414. doi: 10.1177/0361684310395606
Seal, B. N., Andrea, B., and Cindy, M. The association between body esteem sexual desire among college women. Arch. Sex. Behav. 38 866–872. doi: 10.1007/s10508-008-9467-1
Sebastián, J., Manos, D., Bueno, M., and Mateos, N. (2008). Body image and self esteem in women with breast cancer participating in a psychosocial intervention program. Psychol. Spain 12, 13–25.
Sebri, V., Savioni, L., Triberti, S., Durosini, I., Mazzocco, K., and Pravettoni, G. (2020a). Do you transfer your skills? From sports to health management in cancer patients. Front. Psychol. 11:546. doi: 10.3389/fpsyg.2020.00546
Sebri, V., Savioni, L., Triberti, S., Mazzocco, K., and Pravettoni, G. (2019). How to train your health: Sports as a resource to improve cognitive abilities in cancer patients. Front. Psychol. 10:2096. doi: 10.3389/fpsyg.2019.02096
Sebri, V., Triberti, S., and Pravettoni, G. (2020b). Injured self: autobiographical memory, self-concept, and mental health risk in breast cancer survivors. Front. Psychol. 11:607514. doi: 10.3389/fpsyg.2020.607514
Serletti, J. M., Fosnot, J., Nelson, J. A., Disa, J. J., and Bucky, L. P. (2011). Breast reconstruction after breast cancer. Plast. Reconstr. Surg. 127, 124e−135e. doi: 10.1097/PRS.0b013e318213a2e6
Sherman, K. A., Przezdziecki, A., Alcorso, J., Kilby, C. J., Elder, E., Boyages, J., et al. (2018). Reducing body image–related distress in women with breast cancer using a structured online writing exercise: results from the my changed body randomized controlled trial. J. Clin. Oncol. 36, 1930–1940. doi: 10.1200/JCO.2017.76.3318
Smith, J. D., and George, C. (2012). Therapeutic assessment case study: treatment of a woman diagnosed with metastatic cancer and attachment trauma. J. Pers. Assess. 94, 331–344. doi: 10.1080/00223891.2012.656860
Sprangers, M. A. G., Groenvold, M., Arraras, J. I., Franklin, J., te Velde, A., Muller, M., et al. (1996). The European Organisation for Research and Treatment of Cancer: breast cancer specific quality of life questionnaire module: first results from a three-country field study. J. Clin. Oncol. 14, 2756–2768. doi: 10.1200/JCO.1996.14.10.2756
Sterba, K. R., Burris, J. L., Heiney, S. P., Ruppel, M. B., Ford, M. E., and Zapka, J. (2014). “We both just trusted and leaned on the Lord”: a qualitative study of religiousness and spirituality among African American breast cancer survivors and their caregivers. Qual. Life Res. 23, 1909–1920. doi: 10.1007/s11136-014-0654-3
Sterne, J. A., and Egger, M. (2001). Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J. Clin. Epidemiol. 54, 1046–1055. doi: 10.1016/S0895-4356(01)00377-8
Sterne, J. A. C., Savović, J., Page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., et al. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:14898. doi: 10.1136/bmj.l4898
Svensk, A. C., Öster, I., Thyme, K. E., Magnusson, E., Sjödin, M., Eisemann, M., et al. (2009). Art therapy improves experienced quality of life among women undergoing treatment for breast cancer: a randomized controlled study. Eur. J. Cancer Care 18, 69–77. doi: 10.1111/j.1365-2354.2008.00952.x
Thompson, J. K., Heinberg, L. J., Altabe, M., and Tantleff-Dunn, S. (1999). Exacting Beauty: Theory, Assessment, and Treatment of Body Image Disturbance. Washington, DC: American Psychological Association. doi: 10.1037/10312-000
Torres, S., Sales, C., Guerra, M. P., Simões, M. P., Pinto, M., and Vieira, F. M. (2020). Emotion-focused cognitive behavioral therapy in comorbid obesity with binge eating disorder: a Pilot study of feasibility and long-term outcomes. Front. Psychol. 11:343. doi: 10.3389/fpsyg.2020.00343
Triberti, S., Durosini, I., Aschieri, F., Villani, D., and Riva, G. (2017a). Changing avatars, changing selves? The influence of social and contextual expectations on digital rendition of identity. Cyberpsychol. Behav. Soc. Netw. 20, 501–507. doi: 10.1089/cyber.2016.0424
Triberti, S., Durosini, I., Aschieri, F., Villani, D., and Riva, G. (2017b). A frame effect in avatar customization: how users' attitudes towards their avatars may change depending on virtual context. Ann. Rev. CyberTher. Telemed. 15, 92–97.
Triberti, S., Gorini, A., Savioni, L., Sebri, V., and Pravettoni, G. (2019a). Avatars and the disease: Digital customization as a resource for self-perception assessment in breast cancer patients. Cyberpsychol. Behav. Soc. Netw. 22, 558–564. doi: 10.1089/cyber.2018.0461
Triberti, S., Savioni, L., Sebri, V., and Pravettoni, G. (2019b). eHealth for improving quality of life in breast cancer patients: a systematic review. Cancer Treat. Rev. 74, 1–14. doi: 10.1016/j.ctrv.2019.01.003
Van den Noortgate, W., López-López, J. A., Marín-Martínez, F., and Sánchez-Meca, J. (2013). Three-level meta-analysis of dependent effect sizes. Behav. Res. Methods 45, 576–594. doi: 10.3758/s13428-012-0261-6
van der Put, C. E., Assink, M., Gubbels, J., and van Solinge, N. F. B. (2018). Identifying effective components of child maltreatment interventions: a meta-analysis. Clin. Child Fam. Psychol. Rev. 21, 171–202. doi: 10.1007/s10567-017-0250-5
van der Put, C. E., Boekhout van Solinge, N. F., Stams, G. J., Hoeve, M., and Assink, M. (2020). Effects of awareness programs on juvenile delinquency: a three-level meta-analysis. Int. J. Offender Ther. Comp. Criminol. 65, 68–91. doi: 10.1177/0306624X20909239
Viechtbauer, W., and Viechtbauer, M. W. (2015). Package “metafor”. The Comprehensive R Archive Network. Package ‘metafor’. Available online at: https://cran.r-project.org/web/packages/metafor/metafor.pdf (accessed September, 2020).
Williams, F., and Jeanetta, S. C. (2016). Lived experiences of breast cancer survivors after diagnosis, treatment and beyond: qualitative study. Health Expect. 19, 631–642. doi: 10.1111/hex.12372
Woertman, L., and Van den Brink, F. (2012). Body image and female sexual functioning and behavior: a review. J. Sex Res. 49, 184–211. doi: 10.1080/00224499.2012.658586
Yang, Y., Wen, Y., Bedi, C., and Humphris, G. (2017). The relationship between cancer patient's fear of recurrence and chemotherapy: a systematic review and meta-analysis. J. Psychosom. Res. 98, 55–63. doi: 10.1016/j.jpsychores.2017.05.002
Keywords: breast cancer, body image, sexual functioning, psychological interventions, cancer survivors
Citation: Sebri V, Durosini I, Triberti S and Pravettoni G (2021) The Efficacy of Psychological Intervention on Body Image in Breast Cancer Patients and Survivors: A Systematic-Review and Meta-Analysis. Front. Psychol. 12:611954. doi: 10.3389/fpsyg.2021.611954
Received: 29 September 2020; Accepted: 29 January 2021;
Published: 01 March 2021.
Edited by:
Kylee Miller, Oregon Health & Science University, United StatesReviewed by:
Julio Sánchez-Meca, University of Murcia, SpainCopyright © 2021 Sebri, Durosini, Triberti and Pravettoni. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Valeria Sebri, dmFsZXJpYS5zZWJyaUB1bmltaS5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.