- 1Institute of Sport Science, Sichuan University, Chengdu, China
- 2College of Applied Technology, Sichuan Normal University, Chengdu, China
Faced with a constant inundation of information and increasing pressures brought by the continuous development of modern civilization, people are increasingly faced with mental health challenges that are only now being actively researched. Mental illness is caused by brain dysfunction due to internal and external pathogenic factors that destroy the integrity of the human brain and alter its function. Regular participation in physical exercise can stimulate the cerebral cortex and simultaneously increase the supply of oxygen and nutrients, helping to preserve or restore normal functioning of the nervous system. In conjunction with other systems of the body, the nervous system constitutes the neuro-humoral regulation system responsible for maintaining the stable state of the human body. This paper is a systematic review of studies investigating the effects of exercise intervention on several common neuropsychological diseases, including depression, anxiety disorder, autism, and attention-deficit/hyperactivity disorder. Furthermore, we discuss possible physiological mechanisms underlying exercise-induced benefits and study limitations that must be addressed by future research. In many cases, drug therapy is ineffective and brings unwanted side effects. Based on the literature, we conclude that exercise intervention plays a positive role and that certain standards must be established in the field to make physical activity consistently effective.
Introduction
Neuropsychology investigates the relationships between brain processes and mechanisms on one hand and cognition and behavioral control on the other (Berlucchi, 2009). The rapid development of modern society has improved people’s living standards but has also taken a toll on their physical and mental health. The mortality rate of patients with severe neuropsychological disorders is two to three times higher than that of the general population (Saha et al., 2007; Walker et al., 2015). A meta-analysis determined that 32.6% of patients with severe mental disorders also suffer from metabolic syndrome (Vancampfort et al., 2015). Co-morbidities, mainly cardiovascular disease, are found in about 60% of people who die from severe neuropsychological diseases (Lawrence et al., 2013).
Exercise is associated with a range of health benefits: it can improve physical as well as mental health. People who exercise generally report improved quality of life, reduced psychological stress, and improved physical function (Fiuza-Luces et al., 2013; Schuch et al., 2016b, 2015; Vera-Garcia et al., 2015). In addition, exercise intervention has almost no negative side effects. Conversely, the negative effects of lack of exercise are manifold. Harmful effects on health and personal well-being include increased incidence of coronary heart disease, diabetes, certain cancers, obesity, and high blood pressure (Booth et al., 2012). Cross-sectional and prospective longitudinal studies have shown that a lack of physical activity is associated with depression and anxiety symptoms (Bhui and Fletcher, 2000; Goodwin, 2003Abu-Omar et al., 2004; Haarasilta et al., 2004; Motl et al., 2004).
According to studies on both animals and humans, physical exercise can bring lasting benefits, such as improved cognitive function, increased cerebral blood flow, reduced oxidative stress response, increased neurotransmitter levels and plasticity, and improved ability to concentrate and process information (Radak et al., 2001; Ferris et al., 2007; Hillman et al., 2008; Stroth et al., 2009). Additionally, physical exercise can release stress (Tsatsoulis and Fountoulakis, 2006) and reduce negative psychology in patients with neuropsychological diseases, such as anxiety (Binder et al., 2004) and depression (McKercher et al., 2009; Lepage and Crowther, 2010).
Exercise training can improve the neurocognitive ability of patients with mental disorders, such as schizophrenia or depression (Oertel-Knochel et al., 2014; Greer et al., 2015). Given the great potential of exercise for improving physical and mental health, exercise could be developed specifically for cross-diagnosis and treatment of patients with neuropsychological disorders. Due to the current frequency and seriousness of mental diseases, an up-to-date and objective understanding of the therapeutic role of physical activity is needed.
Based on our findings, we put forth the recommendation that exercise may be exploited to reduce morbidity and mortality associated with mental illness. Our recommendation is based on some review of the available literature about the effects of exercise intervention on several of the most common neuropsychological diseases among children, adolescents, and adults in modern society (Mishra et al., 2018; Durbeej et al., 2019; Zablotsky et al., 2019): depression, anxiety disorder, autism, and attention-deficit/hyperactivity disorder (ADHD). We examined interventions, their possible therapeutic mechanisms, and limitations.
Literature Search
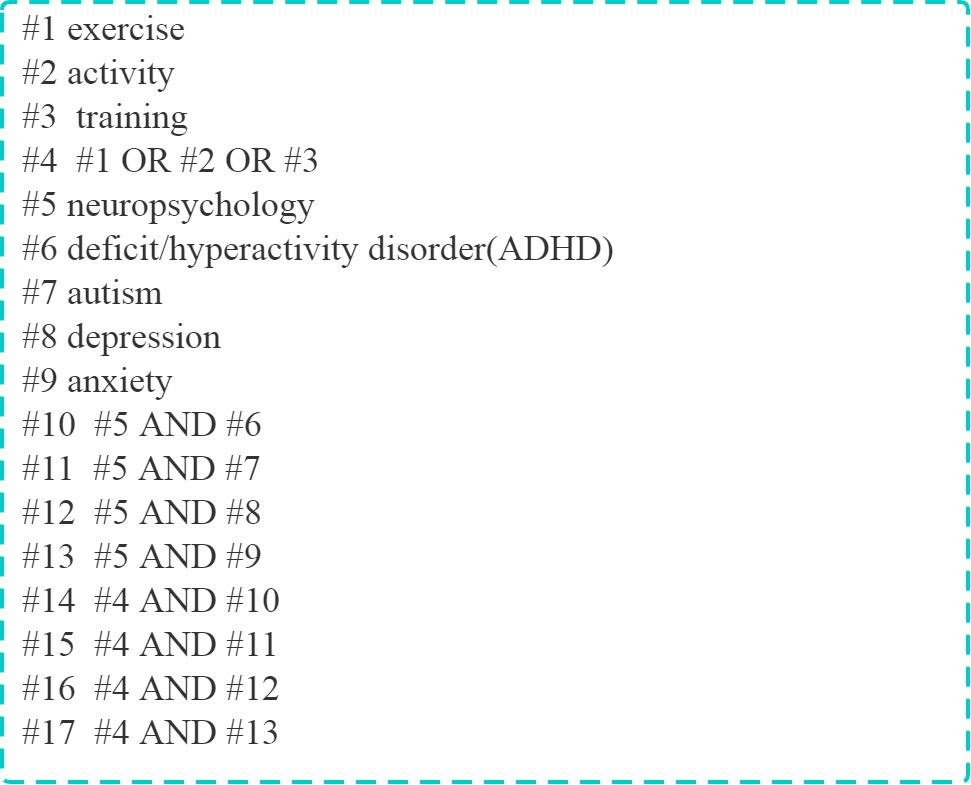
The following electronic databases were systematically searched for relevant literature from inception to January 1, 2020: PubMed, Embase, the Cochrane Library, Web of Science, China Biology Medicine Disk, WanFang Data, and China National Knowledge Infrastructure. Eligible articles were also screened from reference lists of included studies. The following search strings were used: (“exercise” OR “activity” OR “training”) AND (“neuropsychology” OR “ADHD” OR “autism” OR “depression” OR “anxiety”). Additionally, the language restriction was set as English. An example of a retrieval strategy in PubMed is shown in Figure 1. A total of 167 publications were scrutinized.
Common Neuropsychological Diseases and Exercise Interventions
ADHD
Attention-deficit/hyperactivity disorder is one of the most common neurodevelopmental disorders in children and adolescents, with a prevalence rate of 8–10% worldwide (Colvin and Stern, 2015; Faraone et al., 2003; Polanczyk et al., 2007; Thomas et al., 2015). Symptoms develop over time and include inattention, excessive activity, and impulsiveness (Polanczyk et al., 2007). Over half (57%) of children diagnosed with ADHD struggle with symptoms into adulthood (Biederman et al., 2010; Fayyad et al., 2017), which severely impacts their individual learning, communication, normal life, and social ability (Coelho et al., 2010).
At present, ADHD is treated mainly with drugs (Ng, 2017) and behavioral or psychological intervention (Pliszka and Issues, 2007). Early administration of drugs or psychological intervention often adversely affects the child’s growth and development. For example, short-term use of stimulants may cause headaches, insomnia, anorexia, and nausea; long-term use may stunt growth (Greenhill et al., 2001; Hansen and Hansen, 2006; LeBlanc-Duchin and Taukulis, 2007; Scherer et al., 2010; Martinez-Raga et al., 2013; Childress and Sallee, 2014; Wang et al., 2013). Although stimulants such as methylphenidate can be effective, 20–25% of ADHD patients do not respond to such drugs (Childress and Sallee, 2014). Treatment duration and complexity can make life difficult for patients and their families (Jensen et al., 2007). ADHD treatment is marred by many deficiencies that must be urgently addressed through alternative therapies. Exercise offers a potential alternative as it is a natural and essential part of development.
Effects of Exercise Intervention on Children and Adolescents With ADHD
Cognitive ability and executive function appear to be hindered in ADHD patients, manifesting as lack of attention, forgetfulness, impulsiveness, and lack of organizational ability and perseverance (Willcutt et al., 2005; Diamond, 2013; Coghill et al., 2014; Silverstein et al., 2020). Indeed, evidence suggests that ADHD develops in patients as a result of a lack of executive function (Willcutt et al., 2005) and motivation (Nigg, 2005). The cognitive and executive ability of ADHD patients significantly improves with moderate- to high-intensity exercise, which may be indirectly reflected through improved academic performance (Castelli et al., 2007; Medina et al., 2010; Chang et al., 2012; Grassmann et al., 2017). In addition, physical exercise can reduce dependence on ADHD drugs (Katz et al., 2010). One review (Den Heijer et al., 2017) summarized several studies that revealed that physical exercise may represent an effective treatment option that could be combined with other treatment approaches for ADHD, but it highlighted that more well-controlled studies are needed in both children and adults. Therefore, exercise may directly and indirectly benefit ADHD-related mental and physical symptomology. Basic information regarding studies in recent years exploring the role of exercise intervention in patients with ADHD is shown in Table 1.
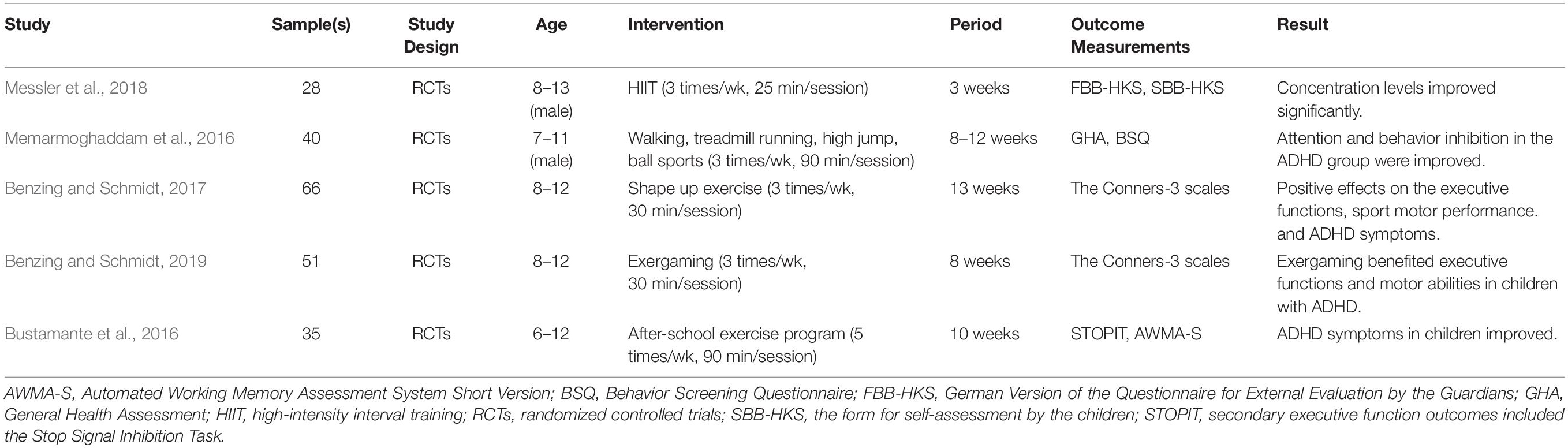
Table 1. Studies of the Effects of Exercise Intervention on Children with Attention-Deficit/Hyperactivity Disorder (ADHD).
Possible Mechanism of Exercise Intervention in the Treatment of ADHD
Attention deficit/hyperactivity disorder may potentially benefit from exercise-related increases in noradrenaline (NE), dopamine (DA), and 5-hydroxytryptamine (5-HT) levels in the prefrontal cortex, hippocampus, and striatum (Smith et al., 2013; Verret et al., 2012). Norepinephrine is involved in the control of executive function and impulses (Robinson, 2012). DA is essential for normal motor and cognitive function of the brain (Cropley et al., 2006) and is found widely lacking in the prefrontal cortex of ADHD patients (Russell, 2002). Increases in 5-hydroxytryptamine and endogenous opioid peptide levels after exercise can further strengthen attention and emotional processing (Hillman et al., 2008). Therefore, exercise produces physiological effects similar to stimulant drugs used to treat ADHD, thereby alleviating symptoms.
Depression
Depression is a life-threatening and disabling mental illness that is affecting more and more people around the world at an alarming rate (Global Burden of Disease Study, 2015). In extreme cases, depression can even compromise someone’s health more than physical disease (Moussavi et al., 2007). In patients suffering from somatic diseases, such as cancer, cardiovascular disease, and infection, depression further increases the risk of death. Not only can depression lead to emotional changes and reduced activity, but as many as two-thirds of patients also suffered from cognitive impairment—which can last even after symptoms have been alleviated (Behnken et al., 2010; Rock et al., 2014; Chakrabarty et al., 2016).
Cognitive defects are an important determinant of psychosocial function, and their persistence weakens the capacity for psychosocial rehabilitation (Reppermund et al., 2009). One meta-analysis concluded that cognitive impairment should be the core of diagnosis and treatment (Rock et al., 2014). Since psychotropic antidepressants have almost no regulatory effect on cognitive function in patients with depression (McIntyre et al., 2013), non-pharmacological methods are becoming increasingly important in the treatment of cognitive impairment.
Effects of Exercise Intervention on Depression
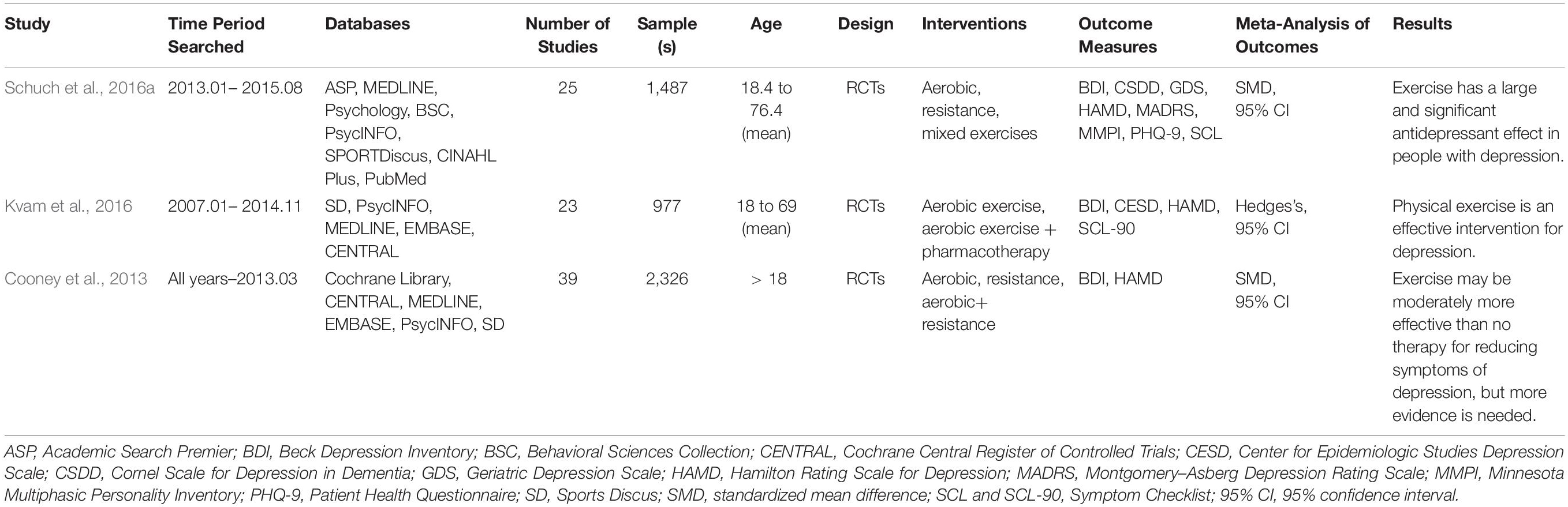
Compared to non-depressed patients, patients with depression initiate less physical activity, and their health deteriorates faster (Andersson et al., 2015). Exercise is positively correlated with improvement of mental health. A meta-analysis including 25 randomized controlled trials (RCTs) confirmed that exercise intervention is a good method for the treatment of depression (Schuch et al., 2016a), and it may also function as adjuvant therapy combined with antidepressant drugs (Kvam et al., 2016). Exercise intervention induces antidepressant effects among patients with depression (Cooney et al., 2013; Schuch et al., 2016a) that are, in some cases, comparable to those of antidepressant drugs or psychotherapy (Brosse et al., 2002; Blumenthal et al., 2007). Cognitive ability and other psychiatric indicators were improved in depressed patients after 4 weeks of aerobic endurance training (Oertel-Knochel et al., 2014), while a meta-analysis found that aerobic exercise significantly alleviated severe depressive symptoms in adults (Morres et al., 2019). In a study conducted on 13 adolescent patients with depression, gradual increases in aerobic exercise intensity over 12 weeks significantly alleviated depressive symptoms (Dopp et al., 2012). In this way, a large number of studies have confirmed that exercise intervention can reduce the symptoms of depression. Three meta-analyses about exercise intervention as treatment for depression are shown in Table 2. Considering the recurrent and serious effects of depression, timely understanding and full application of exercise intervention is necessary for better treatment.
Possible Mechanism of Exercise Intervention in the Treatment of Depression
Imaging studies show that structural changes in the hippocampus, amygdala, striatum, and frontal cortex—areas of the brain with high connectivity—are associated with early depression (Bjornebekk et al., 2005; Nguyen et al., 2019). The most consistent finding associated with depression is atrophy of the hippocampal region. Antidepressant drugs treat depression by promoting neurogenesis of the brain (Park, 2019). Likewise, exercise hypothetically promotes hippocampal neurogenesis through up-regulation of up to four factors: endorphins, vascular endothelial growth factor, brain-derived neurotrophic factor, and 5-hydroxytryptamine (Ernst et al., 2006).
Exercise may improve mood through other mechanisms as well. For example, exercise increases endocannabinoid levels, which are associated with analgesia, anxiety, and well-being (De Moor et al., 2006). Exercise is also associated with changes in the hypothalamic–pituitary–adrenal (HPA) axis, including an increase in corticotropin and a decrease in cortisol, two actions that together contribute to positive mood changes (Duclos and Tabarin, 2016). Finally, exercise improves the self-concept of patients with depression, and it may also promote the relief of depressive symptoms (Knapen et al., 2015).
Anxiety Disorder
Anxiety disorder is a common, heterogeneous mental health disorder. Globally, the incidence of anxiety disorders in various countries ranges from 3.8% to 25%, and it is as high as 70% among people with chronic diseases (Remes et al., 2016). Anxiety disorders are divided into generalized anxiety disorder, social phobia, panic disorder, phobia, agoraphobia, separation anxiety disorder, and selective mutism (Kessler et al., 1994). These widespread mental diseases negatively impact people’s daily body function, quality of life, and health. In addition, anxiety disorders can easily coexist with other mental disorders, such as depression, which can hinder treatment (Kessler et al., 2008). Furthermore, anxiety disorders are associated with increased risk of cardiovascular disease (Tully et al., 2013; Batelaan et al., 2016) and premature mortality (Tully et al., 2008; Janszky et al., 2010).
Anxiety disorders are traditionally treated by pharmacotherapy (e.g., selective 5-hydroxytryptamine reuptake inhibitors and benzodiazepines) (Baldwin et al., 2005, 2011), cognitive behavioral therapy (Carpenter et al., 2018), or both (Ori et al., 2015). Although traditional therapy usually has good therapeutic effects, there are several downfalls. Nearly one-third of patients do not respond to treatment (Hofmann and Smits, 2008; de Vries et al., 2016), and even those who do may experience adverse side effects (Baldwin et al., 2005). Behavioral cognitive therapy is expensive and requires highly specialized professionals (Gunter and Whittal, 2010). Current treatments for anxiety disorders are not effective or even accessible to everyone; thus, more practical approaches should be explored.
Effects of Exercise Intervention on Anxiety Disorder
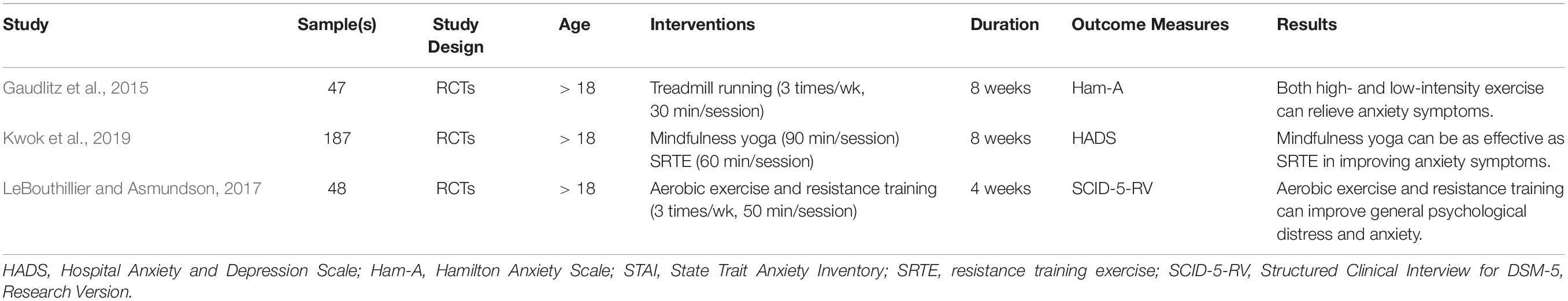
Exercise intervention is an effective treatment for a variety of mental diseases (Ahlskog et al., 2011; Firth et al., 2017; Gordon et al., 2017). For people with anxiety disorders, exercise intervention may be a promising, affordable, and accessible treatment option free of side effects. People who do not exercise reportedly suffer from a significantly higher risk of suffering anxiety and severity of panic disorder (Smits and Zvolensky, 2006). Sedentary lifestyles increase the risk of developing anxiety disorders (Teychenne et al., 2015) or other mental disorders such as depression (Schuch et al., 2018). Indeed, one study confirmed that the degree of anxiety in the exercise group was much lower than that in the control group that did not exercise (Wipfli et al., 2008). In addition, exercise training can reduce the anxiety symptoms of sedentary people with chronic diseases (Herring et al., 2010). Studies of the general population found that physically active people were at a lower risk of developing anxiety disorders or showed fewer symptoms of severe anxiety disorders (De Mello et al., 2013; Lindwall et al., 2014). Stonerock’s review and Bartley’s meta-analysis indicated that exercise may be a useful treatment for anxiety (Bartley et al., 2013; Stonerock et al., 2015). However, those analyses highlighted that definitive conclusions about the efficacy of exercise require additional rigorous, methodologically sound RCTs, larger samples, and comparisons that control for exercise time. Studies in recent years about exercise intervention in patients with anxiety disorders are summarized in Table 3.
Possible Mechanism of Exercise Intervention in the Treatment of Anxiety Disorder
Exercise intervention may regulate the stress response through the HPA axis or glucocorticoid circulation (Anderson and Shivakumar, 2013), increasing cell proliferation and levels of brain-derived neurotrophic factor responsible for reducing anxiety. Exercise intervention may also work by up-regulating the endogenous cannabinoid system. Circulating cannabinoids produce anti-anxiety effects by regulating other neurotransmitters such as DA (Tantimonaco et al., 2014). These data strongly argue that exercise intervention can play an important role in the treatment of anxiety disorders.
Autism
Autism is a highly heritable disease that usually occurs in infancy and childhood and follows a stable process without remission. According to the new edition of the Diagnostic and Statistical Manual of Mental Disorders from the American Psychiatric Association, people with autism have deficiencies in social interaction and communication skills and show repetitive, restrictive, and stereotyped behavior patterns and interest in activities. All these characteristic manifestations have an important impact on a child’s growth and the daily life of their family. The number of people diagnosed with autism is rapidly growing around the world. In Chinese children under the age of 15, about 1.61% of children are affected along the autism spectrum (Wong and Hui, 2008). Compared with the general population, children and adults with autism have a higher risk of other mental and medical diseases (Bradley and Bolton, 2006; Bauman, 2010; Croen et al., 2015), such as obesity and cardiovascular disease (McCoy et al., 2016). Autistic patients also have lower health indices than their normally developing peers, including cardiovascular endurance, upper and abdominal muscle strength, endurance, and lower limb flexibility (Pan et al., 2016). Surveys from parents reveal that their autistic children engage in significantly fewer types of physical activities and for less time annually than do their normal peers (Bandini et al., 2013).
The main purpose behind the treatment of people with autism is to improve their quality of life and reduce related defects and family suffering. Treatment is usually based on the needs of the child, but there is no single treatment that is sufficient to control all symptoms (Myers et al., 2007). Currently, there are no known medications that can relieve the core symptoms of autism, especially communication and social disorders (Myers et al., 2007). Although there is still no cure for autism, some treatments and interventions can help autistic children with daily functioning.
Effects of Exercise Intervention on Autism
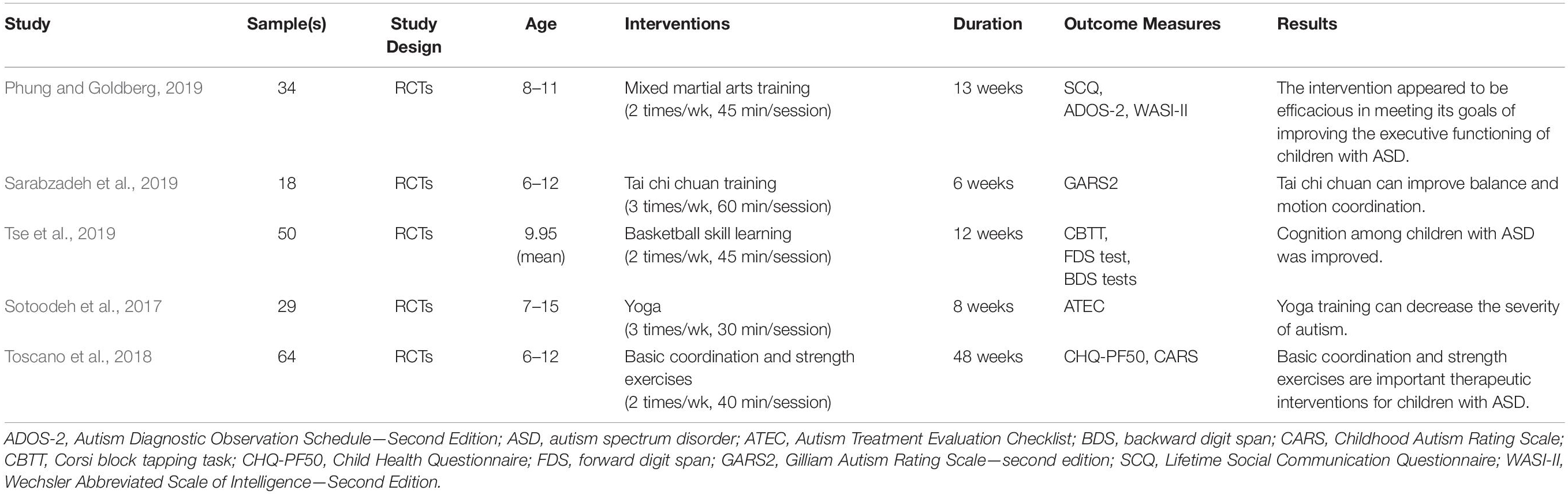
Physical activity is especially important for children because it can not only strengthen their bodies but also improve their self-esteem, social skills, and behavior (Fisher et al., 2011). Conversely, many studies have pointed out the potential problems that can arise due to lack of exercise, especially for children with disabilities (Dobbins et al., 2013; Donnelly et al., 2016; Saunders et al., 2016; Pate et al., 2019). Due to the lack of social and communication skills, autistic children have little opportunity to play with their peers and participate in physical activities (Pan and Frey, 2006). Participation in physical activity allows autistic children to experience interesting activities with their peers and develop interpersonal skills (Srinivasan et al., 2014). Moreover, specific patterns of exercise intervention positively impact the social and communication skills of autistic children and increase their rapid response and frequency of expression (Zhao and Chen, 2018). In one study, ball games, fun games, and orienteering games all improved the perceptual motor skills of autistic adolescents (Rafie et al., 2017). In another study, 12 weeks of ping-pong training significantly improved the motor skill proficiency and executive function of autistic children (Pan et al., 2017). Although high-intensity aerobic exercise may aggravate the stereotypical behavior of autistic children, low- to moderate-intensity exercise can significantly reduce the occurrence of stereotyped behavior (Schmitz Olin et al., 2017). Basic information from recent studies about exercise intervention in patients with autism is shown in Table 4. Overall, exercise intervention appears to benefit the development of physical health and social communication skills, including operating skills, motor skills, muscle strength, and endurance for youth with autism (Healy et al., 2018). These studies establish that exercise intervention may be a feasible treatment for autism.
Possible Mechanism of Exercise Intervention in the Treatment of Autism
Autism involves structural defects in the brain, including a decrease in forebrain volume and a disruption of neural networks between the limbic system and other cortical regions (Sairanen et al., 2005). Exercise intervention can increase the volume of hippocampal tissue and promote the production of nerves and blood vessels in patients with autism by increasing brain-derived neurotrophic factor in the cerebral cortex (Vaynman et al., 2004). It can also promote the production of neurotrophic factors, including nerve growth factor and fibroblast growth factor-2, which can improve the neuropsychological function of autistic children (Courchesne et al., 2001; Croen et al., 2008). In animal models of autism, exercise intervention stimulated the signaling pathway involving phosphatidylinositol-3-kinase (PI3K), protein kinase B (Akt), and extracellular signal-regulated protein kinases 1 and 2 (ERK 1/2), leading to inhibition of neuronal apoptosis in the brain and thereby improving spatial learning, memory, and decision making as well as neurogenesis in the hippocampus (Seo et al., 2013). In addition, exercise intervention improves the cognitive ability of people with autism and reduces repetitive behaviors (Anderson-Hanley et al., 2011). Other evidence shows that exercise intervention can enhance memory function in people with autism (Chan et al., 2015). In summary, studies support exercise intervention for mitigating the symptoms of autism.
Potential Mechanisms of Exercise Intervention in Improving Neuropsychological Diseases
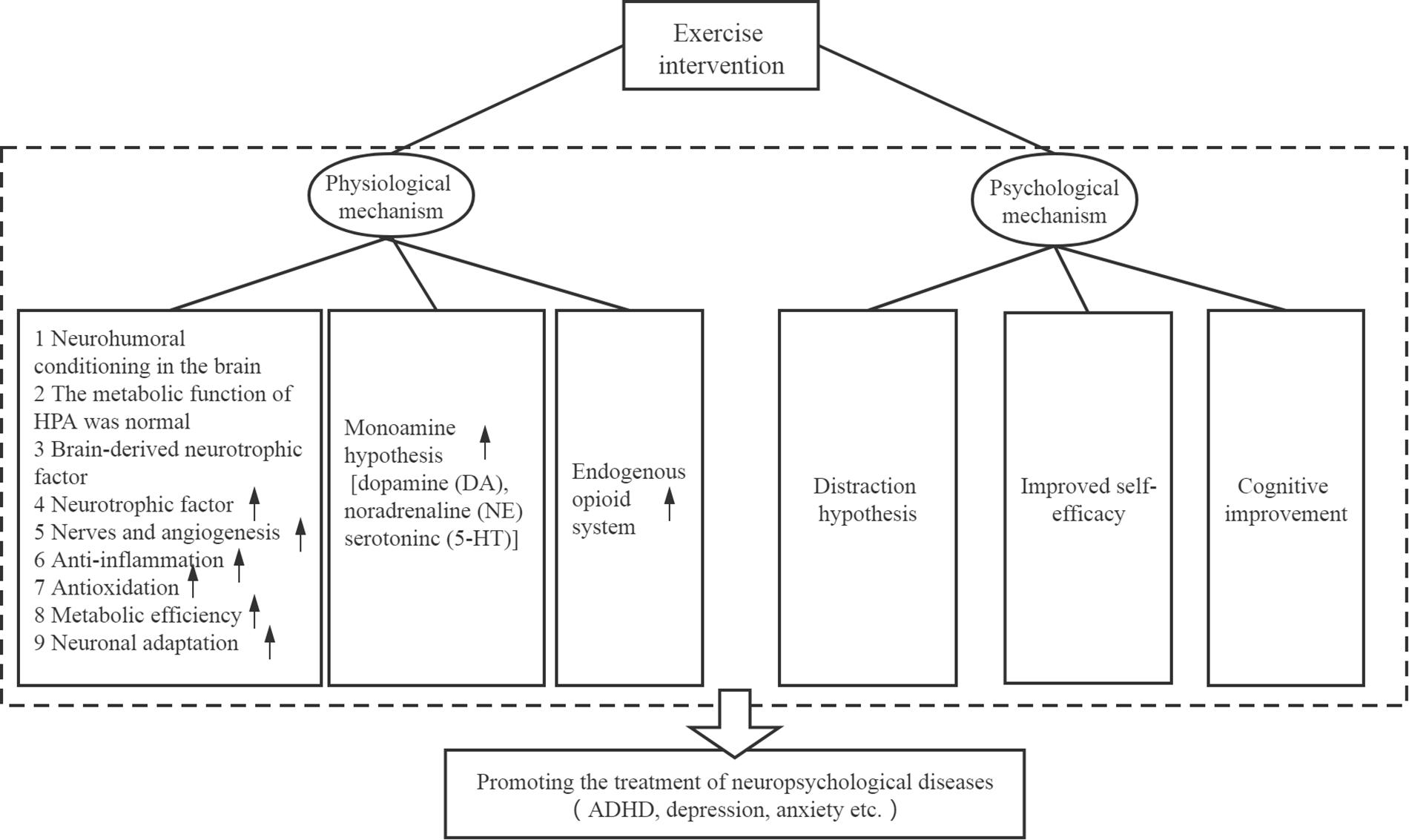
Exercise intervention is hypothesized to alleviate symptoms of neuropsychological diseases through a series of different physiological and psychological mechanisms. These mechanisms are shown in Figure 2 and described in greater detail below.
Proposed Physiological Mechanisms
Neuro-humoral regulation in the brain is one proposed physiological mechanism. Regular aerobic exercise is associated with lower activity of the sympathetic nervous system and HPA cascade (Jackson and Dishman, 2006; Rimmele et al., 2007). The HPA cascade plays a key role in coping with physical and psychological stress, whereas a disordered reaction is related to the occurrence of depression and anxiety (Swaab et al., 2005). Exercise changes the release of corticotropin-releasing factor in the hypothalamus and corticotropin in the anterior pituitary (Salmon, 2001; Droste et al., 2003). These findings suggest that changes in the HPA cascade response induced by exercise can regulate the stress response, anxiety, and depression in humans.
Exercise intervention can also stimulate a series of neurogenic processes that are important for normal function of the brain: it up-regulates growth factors and brain-derived neurotrophic factors, stimulating neurogenesis and angiogenesis (Voss et al., 2013; Kandola et al., 2016). Brain-derived neurotrophic factor is the most abundant neurotrophic factor in the brain, and it is related to anxiety and depression. Stress-induced depression and anxiety behavior are associated with decreased levels of neurotrophic factors in the brain, especially in the hippocampus (Duman and Monteggia, 2006). People with depression have reduced hippocampal volume (Campbell et al., 2004), and 3 months of regular exercise can increase hippocampal volume and improve memory (Pajonk et al., 2010). It is indeed possible that physical activity has a direct positive effect on the hippocampus.
The monoamine hypothesis holds that exercise enhances brain aminergic synaptic transmission (Swaab et al., 2005). DA, NE, and serotonin (5-HT) are the three major monoamine neurotransmitters that are known to be modulated by exercise (Lin and Kuo, 2013). Antidepressant medications are thought to work by improving aminergic transmission, which appears to be impaired in depressive disorders due to defects in production, transmission, reuptake, or metabolism (Pajonk et al., 2010). Another hypothesis postulates that exercise activates the endogenous opioid system. Endogenous opioids can regulate emotion and emotional response (Bodnar and Klein, 2006). Exercise-induced increases in activity of endogenous opioids in the central and peripheral nervous system simultaneously cause feelings of euphoria and relieve pain (Dinas et al., 2011).
Some studies revealed that antioxidant indicators tended to increase and pro-oxidant indicators tended to decrease after exercise training (de Sousa et al., 2017). Exercise training also has been shown to enhance brain function and ameliorate brain disorders by inducing neuroplasticity, increasing metabolic efficiency, enhancing neuronal adaptation, and improving anti-oxidative capacity (Gomez-Cabrera et al., 2008; Lin et al., 2012; Nagamatsu et al., 2014). Moreover, physical exercise can modulate microglial activation in the central nervous system and thereby prevent neuroinflammation in the central nervous system (Mee-Inta et al., 2019). Thus, it is suggested that people, regardless of their health condition, participate in certain kinds of exercise in order to balance the redox state and improve health-related outcomes.
Proposed Psychological Mechanisms
Exercise can make us forget the troubles of daily life for a period of time, which supports the distraction hypothesis. In this theory, diverting attention from unpleasant stimuli or painful physical complaints via exercise can improve mood or simulate an antidepressant-like effect (Carek et al., 2011; Crush et al., 2018). In contrast, the popular “self-efficacy theory” originally proposed by Bandura (Bandura, 1977) suggests that a person’s sense of self-efficacy is positively correlated with his/her ability to control potential threats. Those who believe in their ability to manage potential threats (high self-efficacy) will not be bothered by worrying thoughts or experience low-level anxiety. In essence, if a treatment can rebuild the sense of self-efficacy by providing the experience of self-control, then it will succeed. Exercise itself can improve self-efficacy by providing experience in successfully dealing with stress (Guszkowska, 2004). In one study, the score of self-efficacy was closely related to the current exercise stage, while people who did not exercise lacked confidence in their exercise ability (Jonsson et al., 2018). Improvement in physical fitness results in more endurance and less pain, and it may contribute to positive ideologies. Successful regular physical activity can improve mood, enhance self-confidence, and enhance the ability to deal with challenging mental health events (Chu et al., 2014). These studies have shown that appropriate exercise intervention can improve self-efficacy.
Limitations of Exercise Intervention
Formulating Appropriate Types and Intensities of Exercise Interventions Against Different Psychological Disorders
Studies of exercise intervention may give different results depending on the type of training (e.g., running, walking, or cycling), as well as its duration and intensity. Future research should maintain a consistent and strict definition of aerobic exercise, which would greatly benefit the implementation of correct and effective exercise intervention. A good starting point might be the guidelines proposed by the American Heart Association: lower limb endurance training for 20–60 min, three to five times a week (Fletcher et al., 2001). Then intervention programs could be specifically tailored to suit the needs of individuals with different neuropsychological diseases.
However, an important caveat to consider is that excessive physical activity may be harmful to physical and mental health. Overtraining may cause a neurophysiological disorder and is associated with hyperglucocorticoidemia and hypothalamic dysfunction caused by insulin-induced hypoglycemia (Raglin, 1990; Angeli et al., 2004). Furthermore, excessive exercise decreases libido, retards psychomotor function, and induces other depressive states (Morgan et al., 1987). The boundary between adequate and excessive exercise patterns can be subtle for many people, so future research should examine how to define training intensities for different populations. In the case of ADHD patients, many studies have examined the effectiveness of only short-term exercise intervention in improving behavioral symptoms and neuropsychological function. Future research should include long-term aerobic training and measurements of executive function in order to confirm the long-term effectiveness of exercise intervention.
Considering Patient Differences and Objective Measures
Most experimental designs have not taken into account the influence of gender and age, both of which may be associated with the risk of mental disorders. For example, the incidence of ADHD in boys (7.9%) is four times higher than that in girls (1.8%) (Schlack et al., 2007).
Considering the pessimism of patients with depression and the fact that exercise demands time and energy, many patients seem reluctant to participate in studies of how exercise may benefit them. In fact, lack of interest is a key symptom of depression and the main obstacle to treatment of mental illness more generally (Legrand and Neff, 2016). Clinical staff may find it difficult to stimulate a patient’s interest in exercise. This means that the results obtained in exercise studies of volunteers with depression cannot be broadly extrapolated to all people with depression.
Most studies of exercise intervention against psychological disorders have not applied an acceptable standardized set of measures, they often lack control groups, and they suffer from methodological bias. For example, clinical scoring relies heavily on self-report by the subjects, making it impossible to rule out subjectivity. The best way to minimize this potential deviation is to apply double blinding, but few studies have applied this design.
Future studies should examine whether particular subgroups of patients are more likely than others to benefit from exercise interventions. It may be necessary to optimize interventions for a given disease based on patients’ clinicodemographic characteristics.
Conclusion
The universality of neuropsychological diseases highlights the necessity of diversified treatments. Pharmacological or behavioral interventions are not appropriate or effective for many patients. Clinical and animal studies and meta-analyses strongly support the benefits of exercise intervention for alleviating neuropsychological symptoms and overall disease. These positive impacts occur via several physiological and psychological mechanisms. Especially since people with neuropsychological disorders are at significantly greater risk of potentially serious co-morbidities (Tyler et al., 2011), such as obesity in autistic children, more work is urgently needed to study and establish exercise intervention as a standard of care in the treatment of neuropsychological diseases and coexisting health problems.
Author Contributions
WL conceived the study. WL and ZC searched the literature and selected studies to analyze closely. GY and WL drafted the manuscript, which all authors revised and approved for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank SL (Institute of Sport Science, Sichuan University) for stimulating discussions.
References
Abu-Omar, K., Rutten, A., and Lehtinen, V. (2004). Mental health and physical activity in the European Union. Soz. Praventivmed. 49, 301–309. doi: 10.1007/s00038-004-3109-8
Ahlskog, J. E., Geda, Y. E., Graff-Radford, N. R., and Petersen, R. C. (2011). Physical exercise as a preventive or disease-modifying treatment of dementia and brain aging. Mayo Clin. Proc. 86, 876–884. doi: 10.4065/mcp.2011.0252
Anderson, E., and Shivakumar, G. (2013). Effects of exercise and physical activity on anxiety. Front. Psychiatry 4:27. doi: 10.3389/fpsyt.2013.00027
Anderson-Hanley, C., Tureck, K., and Schneiderman, R. L. (2011). Autism and exergaming: effects on repetitive behaviors and cognition. Psychol. Res. Behav. Manage. 4, 129–137. doi: 10.2147/PRBM.S24016
Andersson, E., Hovland, A., Kjellman, B., Taube, J., and Martinsen, E. (2015). [Physical activity is just as good as CBT or drugs for depression]. Lakartidningen 112:DP4E.
Angeli, A., Minetto, M., Dovio, A., and Paccotti, P. (2004). The overtraining syndrome in athletes: a stress-related disorder. J. Endocrinol. Invest. 27, 603–612. doi: 10.1007/BF03347487
Baldwin, D. S., Anderson, I. M., Nutt, D. J., Bandelow, B., Bond, A., Davidson, J. R., et al. (2005). Evidence-based guidelines for the pharmacological treatment of anxiety disorders: recommendations from the British Association for Psychopharmacology. J. Psychopharmacol. 19, 567–596. doi: 10.1177/0269881105059253
Baldwin, D. S., Waldman, S., and Allgulander, C. (2011). Evidence-based pharmacological treatment of generalized anxiety disorder. Int. J. Neuropsychopharmacol. 14, 697–710. doi: 10.1017/S1461145710001434
Bandini, L. G., Gleason, J., Curtin, C., Lividini, K., Anderson, S. E., Cermak, S. A., et al. (2013). Comparison of physical activity between children with autism spectrum disorders and typically developing children. Autism 17, 44–54. doi: 10.1177/1362361312437416
Bandura, A. (1977). Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 84, 191–215. doi: 10.1037//0033-295x.84.2.191
Bartley, C. A., Hay, M., and Bloch, M. H. (2013). Meta-analysis: aerobic exercise for the treatment of anxiety disorders. Prog. Neuropsychopharmacol. Biol. Psychiatry 45, 34–39. doi: 10.1016/j.pnpbp.2013.04.016
Batelaan, N. M., Seldenrijk, A., Bot, M., van Balkom, A. J., and Penninx, B. W. (2016). Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br. J. Psychiatry 208, 223–231. doi: 10.1192/bjp.bp.114.156554
Bauman, M. L. (2010). Medical comorbidities in autism: challenges to diagnosis and treatment. Neurotherapeutics 7, 320–327. doi: 10.1016/j.nurt.2010.06.001
Behnken, A., Schoning, S., Gerss, J., Konrad, C., de Jong-Meyer, R., Zwanzger, P., et al. (2010). Persistent non-verbal memory impairment in remitted major depression - caused by encoding deficits? J. Affect. Disord. 122(1-2), 144–148. doi: 10.1016/j.jad.2009.07.010 -
Benzing, V., and Schmidt, M. (2017). Cognitively and physically demanding exergaming to improve executive functions of children with attention deficit hyperactivity disorder: a randomised clinical trial. BMC Pediatr. 17:8. doi: 10.1186/s12887-016-0757-9
Benzing, V., and Schmidt, M. (2019). The effect of exergaming on executive functions in children with ADHD: a randomized clinical trial. Scand. J. Med. Sci. Sports 29, 1243–1253. doi: 10.1111/sms.13446
Berlucchi, G. (2009). “Neuropsychology: theoretical basis,” Encyclopedia of Neuroscience. Amsterdam: Elsevier Ltd. 1001–1006. doi: 10.1016/B978-008045046-9.00996-7
Bhui, K., and Fletcher, A. (2000). Common mood and anxiety states: gender differences in the protective effect of physical activity. Soc. Psychiatry Psychiatr. Epidemiol. 35, 28–35. doi: 10.1007/s001270050005
Biederman, J., Petty, C. R., Evans, M., Small, J., and Faraone, S. V. (2010). How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res. 177, 299–304. doi: 10.1016/j.psychres.2009.12.010
Binder, E., Droste, S. K., Ohl, F., and Reul, J. M. (2004). Regular voluntary exercise reduces anxiety-related behaviour and impulsiveness in mice. Behav. Brain Res. 155, 197–206. doi: 10.1016/j.bbr.2004.04.017
Bjornebekk, A., Mathe, A. A., and Brene, S. (2005). The antidepressant effect of running is associated with increased hippocampal cell proliferation. Int. J. Neuropsychopharmacol. 8, 357–368. doi: 10.1017/S1461145705005122
Blumenthal, J. A., Babyak, M. A., Doraiswamy, P. M., Watkins, L., Hoffman, B. M., Barbour, K. A., et al. (2007). Exercise and pharmacotherapy in the treatment of major depressive disorder. Psychosom. Med. 69, 587–596. doi: 10.1097/PSY.0b013e318148c19a
Bodnar, R. J., and Klein, G. E. (2006). Endogenous opiates and behavior: 2005. Peptides 27, 3391–3478. doi: 10.1016/j.peptides.2006.07.011
Booth, F. W., Roberts, C. K., and Laye, M. J. (2012). Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2, 1143–1211. doi: 10.1002/cphy.c110025
Bradley, E., and Bolton, P. (2006). Episodic psychiatric disorders in teenagers with learning disabilities with and without autism. Br. J. Psychiatry 189, 361–366. doi: 10.1192/bjp.bp.105.018127
Brosse, A. L., Sheets, E. S., Lett, H. S., and Blumenthal, J. A. (2002). Exercise and the treatment of clinical depression in adults: recent findings and future directions. Sports Med. 32, 741–760. doi: 10.2165/00007256-200232120-00001
Bustamante, E. E., Davis, C. L., Frazier, S. L., Rusch, D., Fogg, L. F., Atkins, M. S., et al. (2016). Randomized Controlled Trial of Exercise for ADHD and Disruptive Behavior Disorders. Med. Sci. Sports Exerc. 48, 1397–1407. doi: 10.1249/MSS.0000000000000891
Campbell, S., Marriott, M., Nahmias, C., and MacQueen, G. M. (2004). Lower hippocampal volume in patients suffering from depression: a meta-analysis. Am. J. Psychiatry 161, 598–607. doi: 10.1176/appi.ajp.161.4.598
Carek, P. J., Laibstain, S. E., and Carek, S. M. (2011). Exercise for the treatment of depression and anxiety. Int. J. Psychiatry Med. 41, 15–28. doi: 10.2190/PM.41.1.c
Carpenter, J. K., Andrews, L. A., Witcraft, S. M., Powers, M. B., Smits, J. A. J., and Hofmann, S. G. (2018). Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress. Anxiety 35, 502–514. doi: 10.1002/da.22728
Castelli, D. M., Hillman, C. H., Buck, S. M., and Erwin, H. E. (2007). Physical fitness and academic achievement in third- and fifth-grade students. J. Sport Exerc. Psychol. 29, 239–252. doi: 10.1123/jsep.29.2.239
Chakrabarty, T., Hadjipavlou, G., and Lam, R. W. (2016). Cognitive dysfunction in major depressive disorder: assessment, impact, and management. Focus 14, 194–206. doi: 10.1176/appi.focus.20150043
Chan, A. S., Han, Y. M., Sze, S. L., and Lau, E. M. (2015). Neuroenhancement of memory for children with autism by a mind-body exercise. Front. Psychol. 6:1893. doi: 10.3389/fpsyg.2015.01893
Chang, Y. K., Liu, S., Yu, H. H., and Lee, Y. H. (2012). Effect of acute exercise on executive function in children with attention deficit hyperactivity disorder. Arch. Clin. Neuropsychol. 27, 225–237. doi: 10.1093/arclin/acr094
Childress, A. C., and Sallee, F. R. (2014). Attention-deficit/hyperactivity disorder with inadequate response to stimulants: approaches to management. CNS Drugs 28, 121–129. doi: 10.1007/s40263-013-0130-6
Chu, A. H., Koh, D., Moy, F. M., and Muller-Riemenschneider, F. (2014). Do workplace physical activity interventions improve mental health outcomes? Occup. Med. 64, 235–245. doi: 10.1093/occmed/kqu045
Coelho, L., Chaves, E., Vasconcelos, S., Fonteles, M., De Sousa, F., and Viana, G. (2010). [Attention deficit hyperactivity disorder (ADHD) in children: neurobiological aspects, diagnosis and therapeutic approach]. Acta Med. Port. 23, 689–696.
Coghill, D. R., Seth, S., and Matthews, K. (2014). A comprehensive assessment of memory, delay aversion, timing, inhibition, decision making and variability in attention deficit hyperactivity disorder: advancing beyond the three-pathway models. Psychol. Med. 44, 1989–2001. doi: 10.1017/S0033291713002547
Colvin, M. K., and Stern, T. A. (2015). Diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder. J. Clin. Psychiatry 76:e1148. doi: 10.4088/JCP.12040vr1c
Cooney, G. M., Dwan, K., Greig, C. A., Lawlor, D. A., Rimer, J., Waugh, F. R., et al. (2013). Exercise for depression. Cochrane Database Syst. Rev. CD004366. doi: 10.1002/14651858.CD004366.pub6
Courchesne, E., Karns, C. M., Davis, H. R., Ziccardi, R., Carper, R. A., Tigue, Z. D., et al. (2001). Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology 57, 245–254. doi: 10.1212/wnl.57.2.245
Croen, L. A., Goines, P., Braunschweig, D., Yolken, R., Yoshida, C. K., Grether, J. K., et al. (2008). Brain-derived neurotrophic factor and autism: maternal and infant peripheral blood levels in the Early Markers for Autism (EMA) study. Autism Res. 1, 130–137. doi: 10.1002/aur.14
Croen, L. A., Zerbo, O., Qian, Y., Massolo, M. L., Rich, S., Sidney, S., et al. (2015). The health status of adults on the autism spectrum. Autism 19, 814–823. doi: 10.1177/1362361315577517
Cropley, V. L., Fujita, M., Innis, R. B., and Nathan, P. J. (2006). Molecular imaging of the dopaminergic system and its association with human cognitive function. Biol. Psychiatry 59, 898–907. doi: 10.1016/j.biopsych.2006.03.004
Crush, E. A., Frith, E., and Loprinzi, P. D. (2018). Experimental effects of acute exercise duration and exercise recovery on mood state. J. Affect. Disord. 229, 282–287. doi: 10.1016/j.jad.2017.12.092
De Mello, M. T., Lemos Vde, A., Antunes, H. K., Bittencourt, L., Santos-Silva, R., and Tufik, S. (2013). Relationship between physical activity and depression and anxiety symptoms: a population study. J. Affect. Disord. 149, 241–246. doi: 10.1016/j.jad.2013.01.035
De Moor, M. H., Beem, A. L., Stubbe, J. H., Boomsma, D. I., and De Geus, E. J. (2006). Regular exercise, anxiety, depression and personality: a population-based study. Prev. Med. 42, 273–279. doi: 10.1016/j.ypmed.2005.12.002
de Sousa, C. V., Sales, M. M., Rosa, T. S., Lewis, J. E., de Andrade, R. V., and Simoes, H. G. (2017). The antioxidant effect of exercise: a systematic review and meta-analysis. Sports Med. 47, 277–293. doi: 10.1007/s40279-016-0566-1
de Vries, Y. A., de Jonge, P., van den Heuvel, E., Turner, E. H., and Roest, A. M. (2016). Influence of baseline severity on antidepressant efficacy for anxiety disorders: meta-analysis and meta-regression. Br. J. Psychiatry 208, 515–521. doi: 10.1192/bjp.bp.115.173450
Den Heijer, A. E., Groen, Y., Tucha, L., Fuermaier, A. B., Koerts, J., Lange, K. W., et al. (2017). Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review. J. Neural Transm. 124(Suppl. 1), 3–26. doi: 10.1007/s00702-016-1593-7
Diamond, A. (2013). Executive functions. Annu. Rev. Psychol. 64, 135–168. doi: 10.1146/annurev-psych-113011-143750
Dinas, P. C., Koutedakis, Y., and Flouris, A. D. (2011). Effects of exercise and physical activity on depression. Ir. J. Med. Sci. 180, 319–325. doi: 10.1007/s11845-010-0633-9
Dobbins, M., Husson, H., DeCorby, K., and LaRocca, R. L. (2013). School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. CD007651. doi: 10.1002/14651858.CD007651.pub2
Donnelly, J. E., Hillman, C. H., Castelli, D., Etnier, J. L., Lee, S., Tomporowski, P., et al. (2016). Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Med. Sci. Sports Exerc. 48, 1197–1222. doi: 10.1249/MSS.0000000000000901
Dopp, R. R., Mooney, A. J., Armitage, R., and King, C. (2012). Exercise for adolescents with depressive disorders: a feasibility study. Depress. Res. Treat. 2012:257472. doi: 10.1155/2012/257472
Droste, S. K., Gesing, A., Ulbricht, S., Muller, M. B., Linthorst, A. C., and Reul, J. M. (2003). Effects of long-term voluntary exercise on the mouse hypothalamic-pituitary-adrenocortical axis. Endocrinology 144, 3012–3023. doi: 10.1210/en.2003-0097
Duclos, M., and Tabarin, A. (2016). Exercise and the Hypothalamo-Pituitary-Adrenal Axis. Front. Horm. Res. 47, 12–26. doi: 10.1159/000445149
Duman, R. S., and Monteggia, L. M. (2006). A neurotrophic model for stress-related mood disorders. Biol. Psychiatry 59, 1116–1127. doi: 10.1016/j.biopsych.2006.02.013
Durbeej, N., Sorman, K., Noren Selinus, E., Lundstrom, S., Lichtenstein, P., Hellner, C., et al. (2019). Trends in childhood and adolescent internalizing symptoms: results from Swedish population based twin cohorts. BMC Psychol. 7:50. doi: 10.1186/s40359-019-0326-8
Ernst, C., Olson, A. K., Pinel, J. P., Lam, R. W., and Christie, B. R. (2006). Antidepressant effects of exercise: evidence for an adult-neurogenesis hypothesis? J. Psychiatry Neurosci. 31, 84–92.
Faraone, S. V., Sergeant, J., Gillberg, C., and Biederman, J. (2003). The worldwide prevalence of ADHD: is it an American condition? World Psychiatry 2, 104–113.
Fayyad, J., Sampson, N. A., Hwang, I., Adamowski, T., Aguilar-Gaxiola, S., Al-Hamzawi, A., et al. (2017). The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten. Defic. Hyperact. Disord. 9, 47–65. doi: 10.1007/s12402-016-0208-3
Ferris, L. T., Williams, J. S., and Shen, C. L. (2007). The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med. Sci. Sports Exerc. 39, 728–734. doi: 10.1249/mss.0b013e31802f04c7
Firth, J., Stubbs, B., Rosenbaum, S., Vancampfort, D., Malchow, B., Schuch, F., et al. (2017). Aerobic exercise improves cognitive functioning in people with Schizophrenia: a systematic review and meta-analysis. Schizophr. Bull. 43, 546–556. doi: 10.1093/schbul/sbw115
Fisher, A., Saxton, J., Hill, C., Webber, L., Purslow, L., and Wardle, J. (2011). Psychosocial correlates of objectively measured physical activity in children. Eur. J. Public Health 21, 145–150. doi: 10.1093/eurpub/ckq034
Fiuza-Luces, C., Garatachea, N., Berger, N. A., and Lucia, A. (2013). Exercise is the real polypill. Physiology 28, 330–358. doi: 10.1152/physiol.00019.2013
Fletcher, G. F., Balady, G. J., Amsterdam, E. A., Chaitman, B., Eckel, R., Fleg, J., et al. (2001). Exercise standards for testing and training: a statement for healthcare professionals from the American Heart Association. Circulation 104, 1694–1740. doi: 10.1161/hc3901.095960
Gaudlitz, K., Plag, J., Dimeo, F., and Strohle, A. (2015). Aerobic exercise training facilitates the effectiveness of cognitive behavioral therapy in panic disorder. Depress. Anxiety 32, 221–228. doi: 10.1002/da.22337
Global Burden of Disease Study (2015). Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 386, 743–800. doi: 10.1016/S0140-6736(15)60692-4
Gomez-Cabrera, M. C., Domenech, E., and Vina, J. (2008). Moderate exercise is an antioxidant: upregulation of antioxidant genes by training. Free Radic. Biol. Med. 44, 126–131. doi: 10.1016/j.freeradbiomed.2007.02.001
Goodwin, R. D. (2003). Association between physical activity and mental disorders among adults in the United States. Prev. Med. 36, 698–703. doi: 10.1016/s0091-7435(03)00042-2
Gordon, B. R., McDowell, C. P., Lyons, M., and Herring, M. P. (2017). The Effects of resistance exercise training on anxiety: a meta-analysis and meta-regression analysis of randomized controlled trials. Sports Med. 47, 2521–2532. doi: 10.1007/s40279-017-0769-0
Grassmann, V., Alves, M. V., Santos-Galduroz, R. F., and Galduroz, J. C. (2017). Possible cognitive benefits of acute physical exercise in children with ADHD. J. Atten. Disord. 21, 367–371. doi: 10.1177/1087054714526041
Greenhill, L. L., Swanson, J. M., Vitiello, B., Davies, M., Clevenger, W., Wu, M., et al. (2001). Impairment and deportment responses to different methylphenidate doses in children with ADHD: the MTA titration trial. J. Am. Acad. Child Adolesc. Psychiatry 40, 180–187. doi: 10.1097/00004583-200102000-00012
Greer, T. L., Grannemann, B. D., Chansard, M., Karim, A. I., and Trivedi, M. H. (2015). Dose-dependent changes in cognitive function with exercise augmentation for major depression: results from the TREAD study. Eur. Neuropsychopharmacol. 25, 248–256. doi: 10.1016/j.euroneuro.2014.10.001
Gunter, R. W., and Whittal, M. L. (2010). Dissemination of cognitive-behavioral treatments for anxiety disorders: overcoming barriers and improving patient access. Clin. Psychol. Rev. 30, 194–202. doi: 10.1016/j.cpr.2009.11.001
Guszkowska, M. (2004). [Effects of exercise on anxiety, depression and mood]. Psychiatr. Pol. 38, 611–620.
Haarasilta, L. M., Marttunen, M. J., Kaprio, J. A., and Aro, H. M. (2004). Correlates of depression in a representative nationwide sample of adolescents (15-19 years) and young adults (20-24 years). Eur. J. Public Health 14, 280–285. doi: 10.1093/eurpub/14.3.280
Hansen, D. L., and Hansen, E. H. (2006). Caught in a balancing act: parents’ dilemmas regarding their ADHD child’s treatment with stimulant medication. Qual. Health Res. 16, 1267–1285. doi: 10.1177/1049732306292543
Healy, S., Nacario, A., Braithwaite, R. E., and Hopper, C. (2018). The effect of physical activity interventions on youth with autism spectrum disorder: a meta-analysis. Autism Res. 11, 818–833. doi: 10.1002/aur.1955
Herring, M. P., O’Connor, P. J., and Dishman, R. K. (2010). The effect of exercise training on anxiety symptoms among patients: a systematic review. Arch. Intern. Med. 170, 321–331. doi: 10.1001/archinternmed.2009.530
Hillman, C. H., Erickson, K. I., and Kramer, A. F. (2008). Be smart, exercise your heart: exercise effects on brain and cognition. Nat. Rev. Neurosci. 9, 58–65. doi: 10.1038/nrn2298
Hofmann, S. G., and Smits, J. A. (2008). Cognitive-behavioral therapy for adult anxiety disorders: a meta-analysis of randomized placebo-controlled trials. J. Clin. Psychiatry 69, 621–632. doi: 10.4088/jcp.v69n0415
Jackson, E. M., and Dishman, R. K. (2006). Cardiorespiratory fitness and laboratory stress: a meta-regression analysis. Psychophysiology 43, 57–72. doi: 10.1111/j.1469-8986.2006.00373.x
Janszky, I., Ahnve, S., Lundberg, I., and Hemmingsson, T. (2010). Early-onset depression, anxiety, and risk of subsequent coronary heart disease: 37-year follow-up of 49,321 young Swedish men. J. Am. Coll. Cardiol. 56, 31–37. doi: 10.1016/j.jacc.2010.03.033
Jensen, P. S., Arnold, L. E., Swanson, J. M., Vitiello, B., Abikoff, H. B., Greenhill, L. L., et al. (2007). 3-year follow-up of the NIMH MTA study. J. Am. Acad. Child Adolesc. Psychiatry 46, 989–1002. doi: 10.1097/CHI.0b013e3180686d48
Jonsson, T., Ekvall Hansson, E., Thorstensson, C. A., Eek, F., Bergman, P., and Dahlberg, L. E. (2018). The effect of education and supervised exercise on physical activity, pain, quality of life and self-efficacy - an intervention study with a reference group. BMC Musculoskelet. Disord. 19:198. doi: 10.1186/s12891-018-2098-3
Kandola, A., Hendrikse, J., Lucassen, P. J., and Yucel, M. (2016). Aerobic exercise as a tool to improve hippocampal plasticity and function in humans: practical implications for mental health treatment. Front. Hum. Neurosci. 10:373. doi: 10.3389/fnhum.2016.00373
Katz, D. L., Cushman, D., Reynolds, J., Njike, V., Treu, J. A., Walker, J., et al. (2010). Putting physical activity where it fits in the school day: preliminary results of the ABC (Activity Bursts in the Classroom) for fitness program. Prev. Chronic Dis. 7:A82.
Kessler, R. C., Gruber, M., Hettema, J. M., Hwang, I., Sampson, N., and Yonkers, K. A. (2008). Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychol. Med. 38, 365–374. doi: 10.1017/S0033291707002012
Kessler, R. C., McGonagle, K. A., Zhao, S., Nelson, C. B., Hughes, M., Eshleman, S., et al. (1994). Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 51, 8–19. doi: 10.1001/archpsyc.1994.03950010008002
Knapen, J., Vancampfort, D., Morien, Y., and Marchal, Y. (2015). Exercise therapy improves both mental and physical health in patients with major depression. Disabil. Rehabil. 37, 1490–1495. doi: 10.3109/09638288.2014.972579
Kvam, S., Kleppe, C. L., Nordhus, I. H., and Hovland, A. (2016). Exercise as a treatment for depression: a meta-analysis. J. Affect. Disord. 202, 67–86. doi: 10.1016/j.jad.2016.03.063
Kwok, J. Y. Y., Kwan, J. C. Y., Auyeung, M., Mok, V. C. T., Lau, C. K. Y., Choi, K. C., et al. (2019). Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with Parkinson disease: a randomized clinical trial. JAMA Neurol. 76, 755–763. doi: 10.1001/jamaneurol.2019.0534
Lawrence, D., Hancock, K. J., and Kisely, S. (2013). The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 346:f2539. doi: 10.1136/bmj.f2539
LeBlanc-Duchin, D., and Taukulis, H. K. (2007). Chronic oral methylphenidate administration to periadolescent rats yields prolonged impairment of memory for objects. Neurobiol. Learn. Mem. 88, 312–320. doi: 10.1016/j.nlm.2007.04.010
LeBouthillier, D. M., and Asmundson, G. J. G. (2017). The efficacy of aerobic exercise and resistance training as transdiagnostic interventions for anxiety-related disorders and constructs: a randomized controlled trial. J. Anxiety Disord. 52, 43–52. doi: 10.1016/j.janxdis.2017.09.005
Legrand, F. D., and Neff, E. M. (2016). Efficacy of exercise as an adjunct treatment for clinically depressed inpatients during the initial stages of antidepressant pharmacotherapy: An open randomized controlled trial. J. Affect. Disord. 191, 139–144. doi: 10.1016/j.jad.2015.11.047
Lepage, M. L., and Crowther, J. H. (2010). The effects of exercise on body satisfaction and affect. Body Image 7, 124–130. doi: 10.1016/j.bodyim.2009.12.002
Lin, T. W., Chen, S. J., Huang, T. Y., Chang, C. Y., Chuang, J. I., Wu, F. S., et al. (2012). Different types of exercise induce differential effects on neuronal adaptations and memory performance. Neurobiol. Learn. Mem. 97, 140–147. doi: 10.1016/j.nlm.2011.10.006
Lin, T. W., and Kuo, Y. M. (2013). Exercise benefits brain function: the monoamine connection. Brain Sci. 3, 39–53. doi: 10.3390/brainsci3010039
Lindwall, M., Gerber, M., Jonsdottir, I. H., Borjesson, M., and Ahlborg, G. Jr. (2014). The relationships of change in physical activity with change in depression, anxiety, and burnout: a longitudinal study of Swedish healthcare workers. Health Psychol. 33, 1309–1318. doi: 10.1037/a0034402
Martinez-Raga, J., Knecht, C., Szerman, N., and Martinez, M. I. (2013). Risk of serious cardiovascular problems with medications for attention-deficit hyperactivity disorder. CNS Drugs 27, 15–30. doi: 10.1007/s40263-012-0019-9
McCoy, S. M., Jakicic, J. M., and Gibbs, B. B. (2016). Comparison of obesity, physical activity, and sedentary behaviors between adolescents with autism spectrum disorders and without. J. Autism. Dev. Disord. 46, 2317–2326. doi: 10.1007/s10803-016-2762-0
McIntyre, R. S., Cha, D. S., Soczynska, J. K., Woldeyohannes, H. O., Gallaugher, L. A., Kudlow, P., et al. (2013). Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress. Anxiety 30, 515–527. doi: 10.1002/da.22063
McKercher, C. M., Schmidt, M. D., Sanderson, K. A., Patton, G. C., Dwyer, T., and Venn, A. J. (2009). Physical activity and depression in young adults. Am. J. Prev. Med. 36, 161–164. doi: 10.1016/j.amepre.2008.09.036
Medina, J. A., Netto, T. L., Muszkat, M., Medina, A. C., Botter, D., Orbetelli, R., et al. (2010). Exercise impact on sustained attention of ADHD children, methylphenidate effects. Atten. Defic. Hyperact. Disord. 2, 49–58. doi: 10.1007/s12402-009-0018-y
Mee-Inta, O., Zhao, Z. W., and Kuo, Y. M. (2019). Physical exercise inhibits inflammation and microglial activation. Cells 8:691. doi: 10.3390/cells8070691
Memarmoghaddam, M., Torbati, H. T., Sohrabi, M., Mashhadi, A., and Kashi, A. (2016). Effects of a selected exercise programon executive function of children with attention deficit hyperactivity disorder. J. Med. Life 9, 373–379.
Messler, C. F., Holmberg, H. C., and Sperlich, B. (2018). Multimodal therapy involving high-intensity interval training improves the physical fitness, motor skills, social behavior, and quality of life of boys with ADHD: a randomized controlled study. J. Atten. Disord. 22, 806–812. doi: 10.1177/1087054716636936
Mishra, S. K., Srivastava, M., Tiwary, N. K., and Kumar, A. (2018). Prevalence of depression and anxiety among children in rural and suburban areas of Eastern Uttar Pradesh: a cross-sectional study. J. Family Med. Prim. Care 7, 21–26. doi: 10.4103/jfmpc.jfmpc_248_17
Morgan, W. P., Brown, D. R., Raglin, J. S., O’Connor, P. J., and Ellickson, K. A. (1987). Psychological monitoring of overtraining and staleness. Br. J. Sports Med. 21, 107–114. doi: 10.1136/bjsm.21.3.107
Morres, I. D., Hatzigeorgiadis, A., Stathi, A., Comoutos, N., Arpin-Cribbie, C., Krommidas, C., et al. (2019). Aerobic exercise for adult patients with major depressive disorder in mental health services: a systematic review and meta-analysis. Depress. Anxiety 36, 39–53. doi: 10.1002/da.22842
Motl, R. W., Birnbaum, A. S., Kubik, M. Y., and Dishman, R. K. (2004). Naturally occurring changes in physical activity are inversely related to depressive symptoms during early adolescence. Psychosom. Med. 66, 336–342. doi: 10.1097/01.psy.0000126205.35683.0a
Moussavi, S., Chatterji, S., Verdes, E., Tandon, A., Patel, V., and Ustun, B. (2007). Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370, 851–858. doi: 10.1016/S0140-6736(07)61415-9
Myers, S. M., and Johnson, C. P., and American Academy of Pediatrics Council on Children With D (2007). Management of children with autism spectrum disorders. Pediatrics 120, 1162–1182.
Nagamatsu, L. S., Flicker, L., Kramer, A. F., Voss, M. W., Erickson, K. I., Hsu, C. L., et al. (2014). Exercise is medicine, for the body and the brain. Br. J. Sports Med. 48, 943–944. doi: 10.1136/bjsports-2013-093224
Ng, Q. X. (2017). A systematic review of the use of Bupropion for Attention-Deficit/Hyperactivity Disorder in children and adolescents. J. Child Adolesc. Psychopharmacol. 27, 112–116. doi: 10.1089/cap.2016.0124
Nguyen, L., Kakeda, S., Katsuki, A., Sugimoto, K., Otsuka, Y., Ueda, I., et al. (2019). Relationship between VEGF-related gene polymorphisms and brain morphology in treatment-naive patients with first-episode major depressive disorder. Eur. Arch. Psychiatry Clin. Neurosci. 269, 785–794. doi: 10.1007/s00406-018-0953-8
Nigg, J. T. (2005). Neuropsychologic theory and findings in attention-deficit/hyperactivity disorder: the state of the field and salient challenges for the coming decade. Biol. Psychiatry 57, 1424–1435. doi: 10.1016/j.biopsych.2004.11.011
Oertel-Knochel, V., Mehler, P., Thiel, C., Steinbrecher, K., Malchow, B., Tesky, V., et al. (2014). Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. Eur. Arch. Psychiatry Clin. Neurosci. 264, 589–604. doi: 10.1007/s00406-014-0485-9
Ori, R., Amos, T., Bergman, H., Soares-Weiser, K., Ipser, J. C., and Stein, D. J. (2015). Augmentation of cognitive and behavioural therapies (CBT) with d-cycloserine for anxiety and related disorders. Cochrane Database Syst. Rev. CD007803. doi: 10.1002/14651858.CD007803.pub2
Pajonk, F. G., Wobrock, T., Gruber, O., Scherk, H., Berner, D., Kaizl, I., et al. (2010). Hippocampal plasticity in response to exercise in schizophrenia. Arch. Gen. Psychiatry 67, 133–143. doi: 10.1001/archgenpsychiatry.2009.193
Pan, C. Y., Chu, C. H., Tsai, C. L., Sung, M. C., Huang, C. Y., and Ma, W. Y. (2017). The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism 21, 190–202. doi: 10.1177/1362361316633562
Pan, C. Y., and Frey, G. C. (2006). Physical activity patterns in youth with autism spectrum disorders. J. Autism. Dev. Disord. 36, 597–606. doi: 10.1007/s10803-006-0101-6
Pan, C. Y., Tsai, C. L., Chu, C. H., Sung, M. C., Ma, W. Y., and Huang, C. Y. (2016). Objectively measured physical activity and health-related physical fitness in secondary school-aged male students with autism spectrum disorders. Phys. Ther. 96, 511–520. doi: 10.2522/ptj.20140353
Park, S. C. (2019). Neurogenesis and antidepressant action. Cell Tissue Res. 377, 95–106. doi: 10.1007/s00441-019-03043-5
Pate, R. R., Hillman, C. H., Janz, K. F., Katzmarzyk, P. T., Powell, K. E., Torres, A., et al. (2019). Physical activity and health in children younger than 6 years: a systematic review. Med. Sci. Sports Exerc. 51, 1282–1291. doi: 10.1249/MSS.0000000000001940
Phung, J. N., and Goldberg, W. A. (2019). Promoting executive functioning in children with Autism Spectrum Disorder through mixed martial arts training. J. Autism. Dev. Disord. 49, 3669–3684. doi: 10.1007/s10803-019-04072-3
Pliszka, S., and Issues AWGoQ. (2007). Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 46, 894–921. doi: 10.1097/chi.0b013e318054e724
Polanczyk, G., de Lima, M. S., Horta, B. L., Biederman, J., and Rohde, L. A. (2007). The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am. J. Psychiatry 164, 942–948. doi: 10.1176/ajp.2007.164.6.942
Radak, Z., Kaneko, T., Tahara, S., Nakamoto, H., Pucsok, J., Sasvari, M., et al. (2001). Regular exercise improves cognitive function and decreases oxidative damage in rat brain. Neurochem. Int. 38, 17–23. doi: 10.1016/s0197-0186(00)00063-2
Rafie, F., Ghasemi, A., Zamani Jam, A., and Jalali, S. (2017). Effect of exercise intervention on the perceptual-motor skills in adolescents with autism. J. Sports Med. Phys. Fitness 57, 53–59. doi: 10.23736/S0022-4707.16.05919-3
Raglin, J. S. (1990). Exercise and mental health. Beneficial and detrimental effects. Sports Med. 9, 323–329. doi: 10.2165/00007256-199009060-00001
Remes, O., Brayne, C., van der Linde, R., and Lafortune, L. (2016). A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. 6:e00497. doi: 10.1002/brb3.497
Reppermund, S., Ising, M., Lucae, S., and Zihl, J. (2009). Cognitive impairment in unipolar depression is persistent and non-specific: further evidence for the final common pathway disorder hypothesis. Psychol. Med. 39, 603–614. doi: 10.1017/S003329170800411X
Rimmele, U., Zellweger, B. C., Marti, B., Seiler, R., Mohiyeddini, C., Ehlert, U., et al. (2007). Trained men show lower cortisol, heart rate and psychological responses to psychosocial stress compared with untrained men. Psychoneuroendocrinology 32, 627–635. doi: 10.1016/j.psyneuen.2007.04.005
Robinson, E. S. (2012). Blockade of noradrenaline re-uptake sites improves accuracy and impulse control in rats performing a five-choice serial reaction time tasks. Psychopharmacology 219, 303–312. doi: 10.1007/s00213-011-2420-3
Rock, P. L., Roiser, J. P., Riedel, W. J., and Blackwell, A. D. (2014). Cognitive impairment in depression: a systematic review and meta-analysis. Psychol. Med. 44, 2029–2040. doi: 10.1017/S0033291713002535
Russell, V. A. (2002). Hypodopaminergic and hypernoradrenergic activity in prefrontal cortex slices of an animal model for attention-deficit hyperactivity disorder–the spontaneously hypertensive rat. Behav. Brain Res. 130, 191–196. doi: 10.1016/s0166-4328(01)00425-9
Saha, S., Chant, D., and McGrath, J. (2007). A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch. Gen. Psychiatry 64, 1123–1131. doi: 10.1001/archpsyc.64.10.1123
Sairanen, M., Lucas, G., Ernfors, P., Castren, M., and Castren, E. (2005). Brain-derived neurotrophic factor and antidepressant drugs have different but coordinated effects on neuronal turnover, proliferation, and survival in the adult dentate gyrus. J. Neurosci. 25, 1089–1094. doi: 10.1523/JNEUROSCI.3741-04.2005
Salmon, P. (2001). Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin. Psychol. Rev. 21, 33–61. doi: 10.1016/s0272-7358(99)00032-x
Sarabzadeh, M., Azari, B. B., and Helalizadeh, M. (2019). The effect of six weeks of Tai Chi Chuan training on the motor skills of children with Autism Spectrum Disorder. J. Bodyw. Mov. Ther. 23, 284–290. doi: 10.1016/j.jbmt.2019.01.007
Saunders, T. J., Gray, C. E., Poitras, V. J., Chaput, J. P., Janssen, I., Katzmarzyk, P. T., et al. (2016). Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl. Physiol. Nutr. Metab. 41(6 Suppl. 3), S283–S293. doi: 10.1139/apnm-2015-0626
Scherer, E. B., da Cunha, M. J., Matte, C., Schmitz, F., Netto, C. A., and Wyse, A. T. (2010). Methylphenidate affects memory, brain-derived neurotrophic factor immunocontent and brain acetylcholinesterase activity in the rat. Neurobiol. Learn. Mem. 94, 247–253. doi: 10.1016/j.nlm.2010.06.002
Schlack, R., Holling, H., Kurth, B. M., and Huss, M. (2007). [The prevalence of attention-deficit/hyperactivity disorder (ADHD) among children and adolescents in Germany. Initial results from the German Health Interview and Examination Survey for Children and Adolescents (KiGGS)]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 50, 827–835. doi: 10.1007/s00103-007-0246-2
Schmitz Olin, S., McFadden, B. A., Golem, D. L., Pellegrino, J. K., Walker, A. J., Sanders, D. J., et al. (2017). The effects of exercise dose on stereotypical behavior in children with Autism. Med. Sci. Sports Exerc. 49, 983–990. doi: 10.1249/MSS.0000000000001197
Schuch, F. B., Vancampfort, D., Firth, J., Rosenbaum, S., Ward, P. B., Silva, E. S., et al. (2018). Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am. J. Psychiatry 175, 631–648. doi: 10.1176/appi.ajp.2018.17111194
Schuch, F. B., Vancampfort, D., Richards, J., Rosenbaum, S., Ward, P. B., and Stubbs, B. (2016a). Exercise as a treatment for depression: a meta-analysis adjusting for publication bias. J. Psychiatr. Res. 77, 42–51. doi: 10.1016/j.jpsychires.2016.02.023
Schuch, F. B., Vancampfort, D., Rosenbaum, S., Richards, J., Ward, P. B., and Stubbs, B. (2016b). Exercise improves physical and psychological quality of life in people with depression: a meta-analysis including the evaluation of control group response. Psychiatry Res. 241, 47–54. doi: 10.1016/j.psychres.2016.04.054
Schuch, F. B., Vasconcelos-Moreno, M. P., Borowsky, C., Zimmermann, A. B., Rocha, N. S., and Fleck, M. P. (2015). Exercise and severe major depression: effect on symptom severity and quality of life at discharge in an inpatient cohort. J. Psychiatr. Res. 61, 25–32. doi: 10.1016/j.jpsychires.2014.11.005
Seo, T. B., Cho, H. S., Shin, M. S., Kim, C. J., Ji, E. S., and Baek, S. S. (2013). Treadmill exercise improves behavioral outcomes and spatial learning memory through up-regulation of reelin signaling pathway in autistic rats. J. Exerc. Rehabil. 9, 220–229. doi: 10.12965/jer.130003
Silverstein, M. J., Faraone, S. V., Leon, T. L., Biederman, J., Spencer, T. J., and Adler, L. A. (2020). The relationship between executive function deficits and DSM-5-Defined ADHD symptoms. J. Atten. Disord. 24, 41–51. doi: 10.1177/1087054718804347
Smith, A. L., Hoza, B., Linnea, K., McQuade, J. D., Tomb, M., Vaughn, A. J., et al. (2013). Pilot physical activity intervention reduces severity of ADHD symptoms in young children. J. Atten. Disord. 17, 70–82. doi: 10.1177/1087054711417395
Smits, J. A., and Zvolensky, M. J. (2006). Emotional vulnerability as a function of physical activity among individuals with panic disorder. Depress. Anxiety 23, 102–106. doi: 10.1002/da.20146
Sotoodeh, M. S., Arabameri, E., Panahibakhsh, M., Kheiroddin, F., Mirdoozandeh, H., and Ghanizadeh, A. (2017). Effectiveness of yoga training program on the severity of autism. Complement Ther. Clin. Pract. 28, 47–53. doi: 10.1016/j.ctcp.2017.05.001
Srinivasan, S. M., Pescatello, L. S., and Bhat, A. N. (2014). Current perspectives on physical activity and exercise recommendations for children and adolescents with Autism Spectrum Disorders. Phys. Ther. 94, 875–889. doi: 10.2522/ptj.20130157
Stonerock, G. L., Hoffman, B. M., Smith, P. J., and Blumenthal, J. A. (2015). Exercise as treatment for anxiety: systematic review and analysis. Ann. Behav. Med. 49, 542–556. doi: 10.1007/s12160-014-9685-9
Stroth, S., Hille, K., Spitzer, M., and Reinhardt, R. (2009). Aerobic endurance exercise benefits memory and affect in young adults. Neuropsychol. Rehabil. 19, 223–243. doi: 10.1080/09602010802091183
Swaab, D. F., Bao, A. M., and Lucassen, P. J. (2005). The stress system in the human brain in depression and neurodegeneration. Ageing Res. Rev. 4, 141–194. doi: 10.1016/j.arr.2005.03.003
Tantimonaco, M., Ceci, R., Sabatini, S., Catani, M. V., Rossi, A., Gasperi, V., et al. (2014). Physical activity and the endocannabinoid system: an overview. Cell. Mol. Life Sci. 71, 2681–2698. doi: 10.1007/s00018-014-1575-6
Teychenne, M., Costigan, S. A., and Parker, K. (2015). The association between sedentary behaviour and risk of anxiety: a systematic review. BMC Public Health 15:513. doi: 10.1186/s12889-015-1843-x
Thomas, R., Sanders, S., Doust, J., Beller, E., and Glasziou, P. (2015). Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics 135, e994–e1001. doi: 10.1542/peds.2014-3482
Toscano, C. V. A., Carvalho, H. M., and Ferreira, J. P. (2018). Exercise effects for children with Autism Spectrum Disorder: metabolic health, autistic traits, and quality of life. Percept. Mot. Skills 125, 126–146. doi: 10.1177/0031512517743823
Tsatsoulis, A., and Fountoulakis, S. (2006). The protective role of exercise on stress system dysregulation and comorbidities. Ann. N.Y. Acad. Sci. 1083, 196–213. doi: 10.1196/annals.1367.020
Tse, C. Y. A., Lee, H. P., Chan, K. S. K., Edgar, V. B., Wilkinson-Smith, A., and Lai, W. H. E. (2019). Examining the impact of physical activity on sleep quality and executive functions in children with autism spectrum disorder: a randomized controlled trial. Autism 23, 1699–1710. doi: 10.1177/1362361318823910
Tully, P. J., Baker, R. A., and Knight, J. L. (2008). Anxiety and depression as risk factors for mortality after coronary artery bypass surgery. J. Psychosom. Res. 64, 285–290. doi: 10.1016/j.jpsychores.2007.09.007
Tully, P. J., Cosh, S. M., and Baune, B. T. (2013). A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychol. Health Med. 18, 627–644. doi: 10.1080/13548506.2012.749355
Tyler, C. V., Schramm, S. C., Karafa, M., Tang, A. S., and Jain, A. K. (2011). Chronic disease risks in young adults with autism spectrum disorder: forewarned is forearmed. Am. J. Intellect. Dev. Disabil. 116, 371–380. doi: 10.1352/1944-7558-116.5.371
Vancampfort, D., Stubbs, B., Mitchell, A. J., De Hert, M., Wampers, M., Ward, P. B., et al. (2015). Risk of metabolic syndrome and its components in people with schizophrenia and related psychotic disorders, bipolar disorder and major depressive disorder: a systematic review and meta-analysis. World Psychiatry 14, 339–347. doi: 10.1002/wps.20252
Vaynman, S., Ying, Z., and Gomez-Pinilla, F. (2004). Hippocampal BDNF mediates the efficacy of exercise on synaptic plasticity and cognition. Eur. J. Neurosci. 20, 2580–2590. doi: 10.1111/j.1460-9568.2004.03720.x
Vera-Garcia, E., Mayoral-Cleries, F., Vancampfort, D., Stubbs, B., and Cuesta-Vargas, A. I. (2015). A systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with Schizophrenia: an update. Psychiatry Res. 229, 828–839. doi: 10.1016/j.psychres.2015.07.083
Verret, C., Guay, M. C., Berthiaume, C., Gardiner, P., and Beliveau, L. (2012). A physical activity program improves behavior and cognitive functions in children with ADHD: an exploratory study. J. Atten. Disord. 16, 71–80. doi: 10.1177/1087054710379735
Voss, M. W., Vivar, C., Kramer, A. F., and van Praag, H. (2013). Bridging animal and human models of exercise-induced brain plasticity. Trends Cogn. Sci. 17, 525–544. doi: 10.1016/j.tics.2013.08.001
Walker, E. R., McGee, R. E., and Druss, B. G. (2015). Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 72, 334–341. doi: 10.1001/jamapsychiatry.2014.2502
Wang, G. J., Volkow, N. D., Wigal, T., Kollins, S. H., Newcorn, J. H., Telang, F., et al. (2013). Long-term stimulant treatment affects brain dopamine transporter level in patients with attention deficit hyperactive disorder. PLoS One 8:e63023. doi: 10.1371/journal.pone.0063023
Willcutt, E. G., Doyle, A. E., Nigg, J. T., Faraone, S. V., and Pennington, B. F. (2005). Validity of the executive function theory of attention-deficit/hyperactivity disorder: a meta-analytic review. Biol. Psychiatry 57, 1336–1346. doi: 10.1016/j.biopsych.2005.02.006
Wipfli, B. M., Rethorst, C. D., and Landers, D. M. (2008). The anxiolytic effects of exercise: a meta-analysis of randomized trials and dose-response analysis. J. Sport Exerc. Psychol. 30, 392–410. doi: 10.1123/jsep.30.4.392
Wong, V. C., and Hui, S. L. (2008). Epidemiological study of autism spectrum disorder in China. J. Child Neurol. 23, 67–72. doi: 10.1177/0883073807308702
Zablotsky, B., Black, L. I., Maenner, M. J., Schieve, L. A., Danielson, M. L., Bitsko, R. H., et al. (2019). Prevalence and trends of developmental disabilities among children in the United States: 2009-2017. Pediatrics 144:e20190811. doi: 10.1542/peds.2019-0811
Keywords: exercise intervention, neuropsychological disease, ADHD, depression, anxiety, autism
Citation: Chen Z, Lan W, Yang G, Li Y, Ji X, Chen L, Zhou Y and Li S (2020) Exercise Intervention in Treatment of Neuropsychological Diseases: A Review. Front. Psychol. 11:569206. doi: 10.3389/fpsyg.2020.569206
Received: 03 June 2020; Accepted: 14 September 2020;
Published: 22 October 2020.
Edited by:
Guangyu Zhou, Peking University, ChinaReviewed by:
Antonia Meyer, University Hospital of Basel, SwitzerlandDalila Burin, Tohoku University School of Medicine, Japan
Copyright © 2020 Chen, Lan, Yang, Li, Ji, Chen, Zhou and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shanshan Li, Mjc1NjgxOTJAcXEuY29t
†These authors have contributed equally to this work
 Zichao Chen
Zichao Chen Wencen Lan
Wencen Lan Guifen Yang2†
Guifen Yang2† Shanshan Li
Shanshan Li