
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 10 July 2020
Sec. Psychology for Clinical Settings
Volume 11 - 2020 | https://doi.org/10.3389/fpsyg.2020.01684
This article is part of the Research TopicCoronavirus Disease (COVID-19): Psychological, Behavioral, Interpersonal Effects, and Clinical Implications for Health SystemsView all 204 articles
 Emanuele Maria Giusti1,2*
Emanuele Maria Giusti1,2* Elisa Pedroli3,4
Elisa Pedroli3,4 Guido E. D'Aniello2
Guido E. D'Aniello2 Chiara Stramba Badiale3
Chiara Stramba Badiale3 Giada Pietrabissa1,2
Giada Pietrabissa1,2 Chiara Manna1,2
Chiara Manna1,2 Marco Stramba Badiale5
Marco Stramba Badiale5 Giuseppe Riva1,3
Giuseppe Riva1,3 Gianluca Castelnuovo1,2 and Enrico Molinari1,2
Gianluca Castelnuovo1,2 and Enrico Molinari1,2Background: The COVID-19 pandemic had a massive impact on health care systems, increasing the risks of psychological distress in health professionals. This study aims at assessing the prevalence of burnout and psychopathological conditions in health professionals working in a health institution in the Northern Italy, and to identify socio-demographic, work-related and psychological predictors of burnout.
Methods: Health professionals working in the hospitals of the Istituto Auxologico Italiano were asked to participate to an online anonymous survey investigating socio-demographic data, COVID-19 emergency-related work and psychological factors, state anxiety, psychological distress, post-traumatic symptoms and burnout. Predictors of the three components of burnout were assessed using elastic net regression models.
Results: Three hundred and thirty health professionals participated to the online survey. Two hundred and thirty-five health professionals (71.2%) had scores of state anxiety above the clinical cutoff, 88 (26.8%) had clinical levels of depression, 103 (31.3%) of anxiety, 113 (34.3%) of stress, 121 (36.7%) of post-traumatic stress. Regarding burnout, 107 (35.7%) had moderate and 105 (31.9%) severe levels of emotional exhaustion; 46 (14.0%) had moderate and 40 (12.1%) severe levels of depersonalization; 132 (40.1%) had moderate and 113 (34.3%) severe levels of reduced personal accomplishment. Predictors of all the three components of burnout were work hours, psychological comorbidities, fear of infection and perceived support by friends. Predictors of both emotional exhaustion and depersonalization were female gender, being a nurse, working in the hospital, being in contact with COVID-19 patients. Reduced personal accomplishment was also predicted by age.
Conclusions: Health professionals had high levels of burnout and psychological symptoms during the COVID-19 emergency. Monitoring and timely treatment of these conditions is needed.
At the end of 2019, the coronavirus disease (COVID-19) first appeared in China, in particular in Whang City, in Hubei province (Wang et al., 2020a). In March 2020, due to the global spread of the disease, COVID-19 was declared as a pandemic, causing widespread concern (World Health Organization, 2020b). In fact, COVID-19 is an international public health emergency unprecedented in modern history and it causes several health and psychological problems among general population including high level of anxiety, depression and stress (Ornell et al., 2020).
As of the first half of May, 2020, Italy was one of the most affected countries during this outbreak, counting over 223,000 individuals infected by COVID-19 and more than 31,000 casualties (World Health Organization, 2020a). The high prevalence of the disease in the Northern regions of the country led to a national reorganization of the hospital network and caused sudden changes in the personal and professional lives of healthcare professionals.
Epidemic studies proved that previous infectious diseases caused long-term and persistent psychopathological consequences among this category (Tam et al., 2004; Lee et al., 2007). For example, during and after the Severe Acute Respiratory Syndrome (SARS) outbreak in 2003, frontline healthcare professionals self-reported lack of support in the workplace and consequently severe psychological symptoms as acute distress (Tam et al., 2004). Also, in 2015, during the Middle East respiratory syndrome (MERS) outbreak, the medical staff showed an increased long-term risk of developing post-traumatic stress disorder (PTSD), leading to a boost in absenteeism from work (Lee et al., 2018). SARS and MERS experiences crucially compromised healthcare professionals' well-being. In fact, during epidemic emergencies, as it is happening during COVID-19, frontline care workers experience an unexpected increase in workload in a context of uncertainty and powerlessness, and are more vulnerable to the infection due to their direct contact with patients, which also increases in turn their concerning about infecting their families and colleagues (Liu et al., 2020; Ran et al., 2020). As of the end of April 2020, about 12,000 between doctors and nurses were infected by COVID-19, and 228 doctors and 26 nurses had died (Fusaroli et al., 2020; Manzoni and Milillo, 2020). Non-frontline healthcare workers are also at risk for increased stress due to reduced accessibility to formal psychological support, less first-hand medical information on the outbreak, less intensive training on personal protective equipment and infection control measures (Tan et al., 2020a).
During pandemics, general population have been safeguarded with several precautionary measures including shutdown or slowdown in daily activities, social distancing, reductions in interactions between people, wearing face masks and have good ventilation to reduce the possibility of new infections (Tan et al., 2020b; Wang et al., 2020b; Wilder-Smith and Freedman, 2020). On the contrary, healthcare professionals were exposed to longer work shifts, in order to manage the growth of health care demand (Huang et al., 2020; Ornell et al., 2020). These critical conditions are exacerbated by the need of wearing personal protective equipment which cause discomfort and difficulties in breathing.
At the beginning of the spreading of the virus, hospitals had limited availability of personal protective equipment and guidelines or treatment were not well-established (Xiang et al., 2020). Therefore, many professionals felt confused and unprepared to treat adequately patients infected by the new virus (Huang et al., 2020). As a consequence, they perceived feelings of uncertainty, helplessness, alienation, isolation and difficulties in managing the workload. Furthermore, operators had to face loneliness, perception of stigma and rigid expectations, which can lead to several emotional and psychological outcomes as anger, anxiety, insomnia, and stress related to the uncertainty of the outbreak (Ran et al., 2020; Zhang et al., 2020). All the above-mentioned risk factors can induce more likely the onset of burnout (Ornell et al., 2020).
Burnout can be defined as a psychological syndrome characterized by chronic exhaustion, cynicism and ineffectiveness and it emerges as a response to the presence of highly stressful conditions in the workplace (Maslach and Goldberg, 1998). The presence of burnout among health operators, in particular but not limited to doctors and nurses, has a very strong impact both on their physical and psychological health and on the efficiency of their organization and work (Portoghese et al., 2014; Low et al., 2019; Woo et al., 2020). Usually, burnout occurs following long-term exposition to organizational risk factors but critical emergences, like pandemics, can easily trigger emotional exhaustion (Kim and Choi, 2016).
During pandemics or other critical situations, protective factors can help healthcare professionals to cope with the emergency. For instance, after SARS, health professionals reported that clear directiveness and support from the supervisors, adequate training, precautionary measures, social, religious, and familiar support were the most effective coping strategies (Chan and Huak, 2004; Cheng and Wong, 2005; Maunder et al., 2006). Personality traits also proved to influence health professionals' responses to the pandemics. In fact, during SARS emergence, optimism, resilience and altruism reduced psychological distress among healthcare workers (Bai et al., 2004; Lee et al., 2007).
Furthermore, after MERS, medical staff sustained that several factors including strict protective measures and guidance, the presence of a cohesive team, positive attitudes in the workplace and the recognition of their efforts by the hospital helped them to face the situation (Khalid et al., 2016).
Recent scientometric analysis found that the most common research topics include emergency care and surgical, viral pathogenesis, and global responses in the COVID-19 pandemic but there is a lack of mental health research and only few studies addressed the impact of the COVID-19 pandemic on healthcare professionals' well-being (Tran et al., 2020). Therefore, the main objective of this study is to identify the prevalence of burnout and psychological distress in health professionals during the early phases of the pandemic. The secondary objective of this study is to assess the demographic, psychological, and work-related predictors of burnout.
This study is part of a broader project, the COV-BHP study, which is a prospective cohort study aimed at identifying the prevalence and predictors of burnout and psychological distress in health professionals working in the Hospitals of the Istituto Auxologico Italiano. The Istituto Auxologico Italiano is a scientific and clinical institution operating with three main hospitals in Lombardy and Piedmont (Northern Italy), the regions with the higher transmission rates and mortality in Italy (Dipartimento della Protezione Civile, 2020). About 800 health professionals work in this Institution. All of them were informed about the study through an institutional e-mail message, which also reported an anonymous link that enabled to be enrolled in the study after giving an informed consent. The e-mail was sent on April 16, 2020 and data collection was discontinued on May 11, 2020. The whole study was performed using online questionnaires implemented using the Qualtrics software, version 03/2020 (Qualtrics, Provo, UT). The study was approved by the Institutional Ethical Committee.
Data collected in the survey included:
• Socio-demographic and clinical factors: gender, age, occupation, current working situation (full-time working in the Hospital, part-time working in the Hospital, working from home, being quarantined), medical or psychopathological comorbidities;
• COVID-19 emergency-related work factors: number of hours per week spent working, exposure to COVID-19 cases (no exposure, exposure to suspect COVID-19 cases, exposure to confirmed COVID-19 cases), working in wards dedicated exclusively to the care of patients with COVID-19 patients, number of days since the professional's working situation changed because of COVID-19;
• COVID-19 emergency-related psychological factors: single items measured through a cursor on a pointed scale from 0 to 100, adapted from a previous study on MERS epidemic (Kim and Choi, 2016). COVID-19 emergency-related psychological factors included fear of COVID-19 infection due to work-related exposure (“I am afraid of being infected with COVID-19 since I deal with COVID-19 patients”), perceived support from family and friends (“My family supports me even if my work carries risks of infection,” “My friends supports me even if my work carries risks of infection”)of for caring for COVID-19 patients”); chances to find spiritual comfort (“In facing the COVID-19 crisis, I find comfort in spirituality”);
• State Anxiety: State-Trait Anxiety Inventory—State form (STAI-S) (Spielberger et al., 1983). The STAI-S measures participant's state anxiety, i.e., the transitory state of fear and emotional tension as a response to a perceived threatening situation. The STAI-S includes 20 items on a 4-points Likert scale (not at all, somewhat, moderately so, very much so), with higher values indicating higher state anxiety. Examples of its items are “I am tense” and “I am worried.” The cut-off value of 40 was employed to identify participants with clinical levels of anxiety (Spielberger et al., 1983). This scale has been widely validated and its Italian translation has shown good psychometric properties (Pedrabissi and Santinello, 1989);
• Psychological distress: Depression, Anxiety and Stress Scale-21 (DASS) (Lovibond and Lovibond, 1995). This scale includes 21 items measured on a 4- points Likert scale (never, sometimes, often, almost always) which measure the three psychological subdimensions of psychological distress, namely anxiety (e.g., “I felt I was close to panic”), depression (e.g., “I felt that I had nothing to look forward to”) and stress (e.g., “I found it difficult to relax”). Higher values indicate higher psychological distress. Clinical levels of depression, anxiety and stress were detected identifying values above the 75° percentile based on normative data (Henry and Crawford, 2005). This scale has been validated in Italian and provides reliable and valid measurements of psychological distress in health workers (Bottesi et al., 2015);
• Post-traumatic symptoms: Impact of Event Scale—Revised-−6 items version (IES-6) (Weiss, 2007). The IES-6 is a reduced version of the 22-items IES-R instrument. It is a self-report questionnaire assessing psychological distress in response to a traumatic event. It includes 3 subscales, representing symptoms clusters of post-traumatic stress: intrusion (e.g., “I thought about it when I didn't mean to”), avoidance (e.g., “I tried not to think about it”) and hyperarousal (e.g., “I felt watchful or on guard”). Respondents are asked to indicate on a 5-point Likert scale ranging from never (score 0) to often (score 4) how frequently each symptom was experienced during the past week. The cut-off of 9 was used to dichotomize the total score (Thoresen et al., 2009). The Italian translation showed psychometric features similar to the original version (Giorgi et al., 2015);
• Burnout: Maslach Burnout Inventory (MBI) (Maslach et al., 1997). The MBI is a 22-items questionnaire on a 5-points Likert scale which assesses the three theoretical components of burnout syndrome, namely emotional exhaustion (“I feel emotionally drained from my work,” depersonalization (“I feel I treat some patients as if they were impersonal objects”) and personal accomplishment (“I deal very effectively with the problems of my patients). Higher scores in the emotional exhaustion and depersonalization scales indicate greater burnout, whereas higher scores in the personal accomplishment subscale indicate less burnout. Cutoffs for moderate and severe emotional exhaustion were ≥17 and ≥27, for moderate and severe depersonalization ≥7 and ≥13, and for moderate and severe reduced personal accomplishment ≤38 and ≤21 (Maslach et al., 1997). The MBI Italian translation has been validated for its use on health workers (Sirigatti et al., 1988).
Descriptive statistics are presented as counts and proportions for categorical variables and means and standard deviations for continuous variables. For descriptive purposes, scores of the burnout and psychological distress questionnaires were categorized using the appropriate cut-offs. Associations between categorical variables and burnout components were assessed using point-biserial correlations, whereas associations between continuous variables and burnout components calculating Person's r coefficient. Predictors of the burnout components, analyzed as continuous variables, were then assessed using elastic net linear regressions. Briefly, elastic net regression is a penalized linear regression analysis technique which enables to address multicollinearity between the predictors and to select the most important ones. This is done by regularizing (shrinking) their estimated β coefficients applying a penalization based on two hyperparameters. The first hyperparameter is α, which identifies the type of penalty, which ranges from a ridge penalty (based on the squared magnitude of the coefficients) when α approaches 0 to a lasso penalty (based on the absolute magnitude of the coefficients) when α approaches 1. The second hyperparameter is λ, which identifies the amount of penalization (Zou and Hastie, 2005).
We used 10-fold repeated (10 times) cross-validation to train and tune our model over a grid of α and λ hyperparameters on half of the sample, which constituted the training dataset. The model was refit on the training dataset with the best performing hyperparameters to calculate the final penalized β coefficients. The model was then applied to the other half of the sample, which constituted the testing dataset, to calculate model performance. The above procedure was repeated for each of the three dependent outcome variables. Elastic net regression was performed using the R (version 3.5.1) packages caret (Kuhn, 2015) and glmnet (Friedman et al., 2010).
Three hundred and thirty out of the about 800 health professionals working in the Institution participated to the online survey. Table 1 reports the demographic, work-related and psychological characteristics of the participants of this research.
Figure 1 represents the prevalence of burnout and psychological distress in the participants. Two hundred and thirty-five health professionals (71.2%) had state anxiety scores above the cutoff. Regarding burnout, 107 (35.7%) had moderate and 105 (31.9%) severe levels of emotional exhaustion; 46 (14.0%) had moderate and 40 (12.1%) severe levels of depersonalization; 132 (40.1%) had moderate and 113 (34.3%) severe levels of reduced personal accomplishment. Clinical levels of depression were identified in 88 participants (26.8%), clinical levels of anxiety in 103 (31.3%) and clinical levels of stress in 113 participants (34.3%). Finally, 121 (36.7%) reported symptoms of post-traumatic stress.
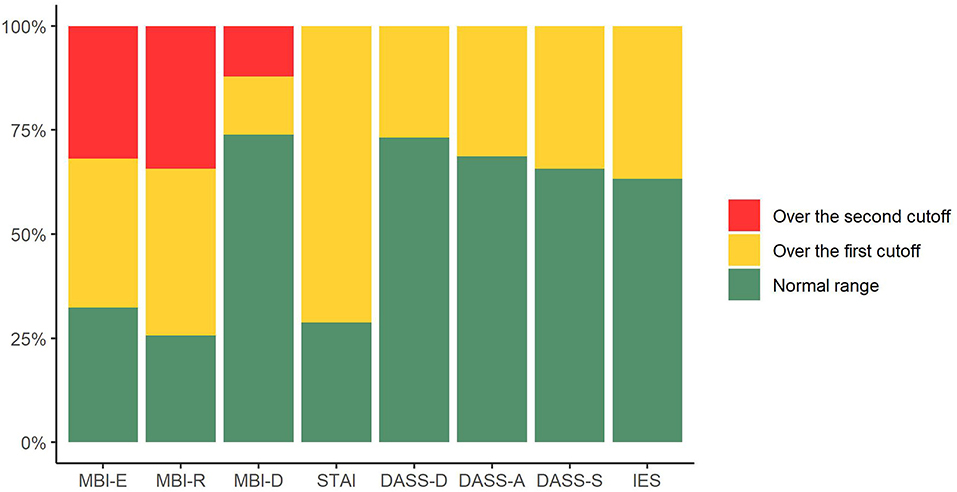
Figure 1. Prevalence of burnout, state anxiety, trait anxiety, depression, stress, and post-traumatic symptoms in health professionals participating to the study. MBI-E, Maslach Burnout Inventory-Emotional Exhaustion; MBI-R, Maslach Burnout Inventory-Reduced personal accomplishment; MBI-D, Maslach Burnout Inventory-Depersonalization; STAI, State-Trait Anxiety Inventory; DASS-D, Depression Anxiety Stress Scales 21-Depression; DASS-A, Depression Anxiety Stress Scales 21-Anxiety; DASS-D, Depression Anxiety Stress Scales 21-Stress; IES, Impact of Event Scale-6.
The associations between categorical and continuous predictors and burnout components are plotted in Figure 2. Variables with association coefficients > 0.3, corresponding to a weak or moderate effect, were age, occupation, being home, work hours, psychological comorbidities, contact with COVID-19 patients, fear of infection, support from family and support from friends.
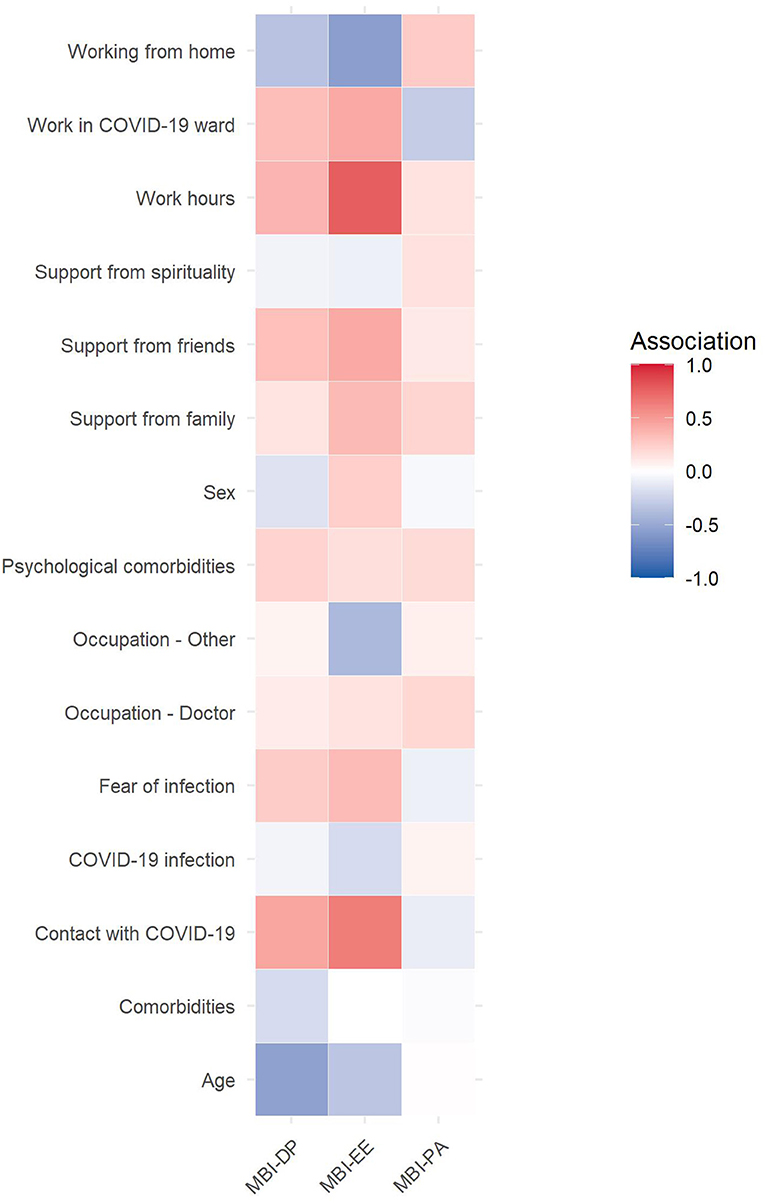
Figure 2. Heatmap of the association between socio-demographic, COVID-19-related, and psychological factors and burnout components. Note. Association between categorical variables and burnout were assessed using point-biserial correlation, association between continuous variables and burnout calculating Pearson's r coefficients.
Finally, elastic net regressions were performed. After model tuning, the best hyperparameter for the Emotional Exhaustion subscale were α = 0.21 and β = 0.17; for the Depersonalization subscale were α = 0.28 and β = 0.17; for the Personal Accomplishment subscale were α = 0.16 and β = 0.60. Selected predictors and their coefficients are reported in Table 2.
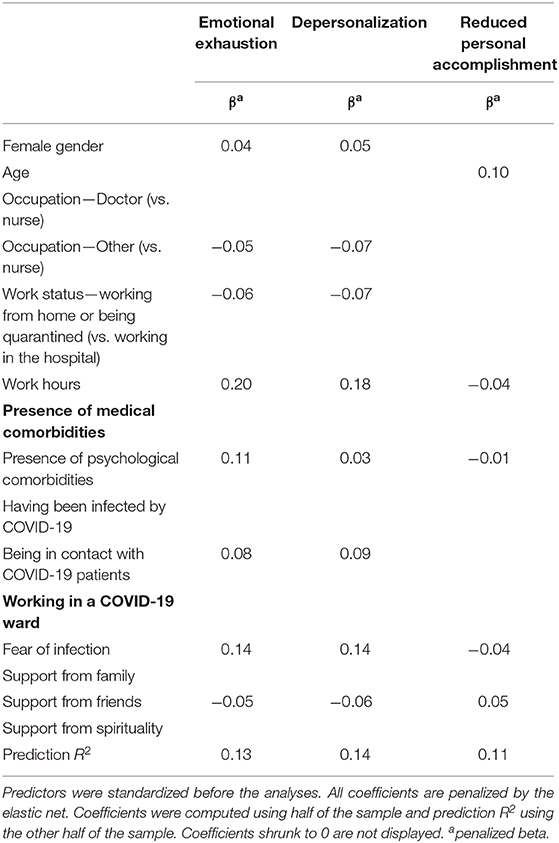
Table 2. Results of the elastic net regression models investigating the predictors of the components of burnout.
The main aims of this study were to assess the prevalence of burnout among health professionals during the COVID-19 pandemic and to evaluate its predictors. Results show that severe levels of burnout and psychopathological symptoms had high prevalence, and that the work-related and psychological factors associated with the necessity to cope with the COVID-19 emergency increase the risks of negative psychological consequences.
Moderate to severe levels of emotional exhaustion and reduced personal accomplishment were present in more than 60% of the sample, and moderate to severe levels of depersonalization in more than 25% of the sample. These results are novel since, to our knowledge, prevalence of burnout among health professionals during the COVID-19 pandemic has not been studied before. More importantly, these results have clear implications for both the professionals' health and efficiency of the health care systems. From the perspective of the professionals, burnout is associated with increased risks of both physical and psychological long-term detrimental consequences (Salvagioni et al., 2017). From the perspective of the health care systems, burnout is associated with increase in sick leave, absenteeism, job withdrawal and poor work efficiency (Salvagioni et al., 2017). Given the potential extended duration of the pandemic (Giordano et al., 2020), the negative impact of the high prevalence of burnout might worsen and reduce the capacity of health systems to cope with the increased demand of care that is likely to occur both in the short- and in the long-term (Boukhris et al., 2020; Leocani et al., 2020; Liebensteiner et al., 2020).
Analysis of burnout was complemented with the assessment of other psychological disorders. This helped to overcome the limitations of the cutoffs of burnout measures (Schaufeli and Van Dierendonck, 1995; Bianchi, 2015). In particular, prevalence of clinical levels of depression, anxiety, stress was higher than 25% in our sample. A previous rapid review with meta-analysis on 12 studies performed in China and one study performed in Singapore found that anxiety, depression and insomnia prevalence among health professionals during the COVID-19 outbreak was 23.2, 22.8, and 38.9%, respectively (Pappa et al., 2020). Taken together, these findings confirm that the impact of the pandemic on the health professionals' psychological health is massive. The respondents also showed very high levels of state anxiety, which might suggest the presence of a pervasive state of tension that could help the development or worsening of burnout and psychological distress symptoms. In addition, more than one participant out of four also showed post-traumatic symptoms. Previous studies performed after the SARS pandemic show conflicting results regarding the presence of post-traumatic symptoms among health workers, potentially attributable to the preparedness to face the emergency (Chan and Huak, 2004; Lee et al., 2007). The high prevalence of these symptoms that was found in this study might suggest the lack of preparation to face the emergency, and that the COVID-19 emergency has the potential to trigger traumatizing experiences for health professionals.
The regression models clearly show that the increased workload, the constant contact with COVID-19 patients and the psychological aspects related to their care are related to the levels of burnout. On the one hand, this calls for political and organizational decisions. Although the main focus of health care systems is on minimizing transmission, treating the infection, and saving lives, attention should be made to reduce the work-related burden on health professionals. Attention should be focused on promoting positive and protective strategies to cope with the emergency developed with the support of a dedicated psychologist.
On the other hand, these results show that presence of previous psychological comorbidities, fear of infection and feelings of isolation due to perceived lack of support from friends should be taken into account by interventions aimed at preventing the development of burnout in health professionals.
Timely recognition of this problem should help implement adequate prevention or rehabilitation strategies. In their review, Wiederhold et al. (2018) highlight that a successful intervention for burnout should take into account the broad range of causes and should incorporate a variety of different therapeutic tools. For this reason, it is necessary to promote monitoring of the health status, including mental health, of health workers during these moments of crisis. Several strategies could be implemented during and after the emergency to support health professionals working with COVID-19 patients, which include work-hour regulation programs, the implementation of strategies to reduce the pressure of difficult decision-making, planning official and unofficial rewards, providing individual or group psychological support programs, promoting focus groups to advance proposals for improvement of the organization of the work, providing individual and group skill training programs as well as online cognitive behavior therapy or mindfulness-based therapy (Ho et al., 2020).
The main limitation of this study is the heterogeneity of the sample. Although the inclusion of health professionals with different occupations and working in different wards allowed to provide a more complete picture of the impact of the pandemic, the variety of the respondents' characteristics. In addition, similarly to other studies performed during epidemics (Maunder et al., 2006; Lee et al., 2007), the respondent rate was low, indicating the risk of the auto-selection of the sample. Moreover, the cross-sectional nature of this study limits our understanding of the risk factors of burnout and suggests that longitudinal studies are needed for this purpose. Finally, the assessment of burnout, psychological distress and post-traumatic symptoms was performed using self-reported instruments which were not confirmed by medical records or specialistic evaluations.
In conclusion, this study shows that health professionals have a high risk of incurring in burnout or psychological conditions due to the COVID-19 pandemic. Continuous monitoring and timely treatment of these conditions is needed to preserve the professionals' health and to enhance the healthcare systems preparedness to face the medium- and long-term consequences of the outbreak.
The datasets presented in this article are not readily available because due to the nature of this research, participants of this study did not agree for their data to be shared publicly, so supporting data is not available. Requests to access the datasets should be directed to ZS5naXVzdGlAYXV4b2xvZ2ljby5pdA==.
The studies involving human participants were reviewed and approved by Comitato Etico dell'Istituto Auxologico Italiano. The participants provided their electronic informed consent to participate in this study.
EG, EP, CS, and CM were responsible for drafting the manuscript. All authors critically revised it for important intellectual content, gave final approval to the finished manuscript, and agreed to be accountable for all aspects of the work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We would like to express our deepest appreciation to all the health professionals who kindly participated in this study for donating their effort and time in a period of global emergency to help scientific research to continue.
Bai, Y. M., Lin, C. C., Lin, C. Y., Chen, J. Y., Chue, C. M., and Chou, P. (2004). Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 55, 1055–1057. doi: 10.1176/appi.ps.55.9.1055
Bianchi, R. (2015). What is “severe burnout” and can its prevalence be assessed? Intens. Care Med. 41:166. doi: 10.1007/s00134-014-3534-y
Bottesi, G., Ghisi, M., Altoè, G., Conforti, E., Melli, G., and Sica, C. (2015). The Italian version of the depression anxiety stress scales-21: factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 60, 170–181. doi: 10.1016/j.comppsych.2015.04.005
Boukhris, M., Hillani, A., Moroni, F., Annabi, M. S., Addad, F., Ribeiro, M. H., et al. (2020). Cardiovascular implications of the COVID-19 pandemic: a global perspective. Can. J. Cardiol. doi: 10.1016/j.cjca.2020.05.018. [Epub ahead of print].
Chan, A. O. M., and Huak, C. Y. (2004). Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup. Med. 54, 190–196. doi: 10.1093/occmed/kqh027
Cheng, S. K. W., and Wong, C. W. (2005). Psychological intervention with sufferers from severe acute respiratory syndrome (SARS): lessons learnt from empirical findings. Clin. Psychol. Psychother. 12, 80–86. doi: 10.1002/cpp.429
Dipartimento della Protezione Civile (2020). COVID-19 Scheda Regioni 20200523. Available online at: https://github.com/pcm-dpc/COVID-19/blob/master/schede-riepilogative/regioni/dpc-covid19-ita-scheda-regioni-20200523.pdf
Friedman, J., Hastie, T., and Tibshirani, R. (2010). Regularization paths for generalized linear models via coordinate descent. J. Stat. Softw. 33:1. doi: 10.18637/jss.v033.i01
Fusaroli, P., Balena, S., and Lisotti, A. (2020). On the death of 100 + Italian doctors from COVID-19. Infection 1–2. doi: 10.1007/s15010-020-01436-1. [Epub ahead of print].
Giordano, G., Blanchini, F., Bruno, R., Colaneri, P., Di Filippo, A., Di Matteo, A., et al. (2020). Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nat. Med. 26, 855–860. doi: 10.1038/s41591-020-0883-7
Giorgi, G., Fiz Perez, F. S., Castiello D'Antonio, A., Mucci, N., Ferrero, C., Cupelli, V., et al. (2015). Psychometric properties of the Impact of Event Scale-6 in a sample of victims of bank robbery. Psychol. Res. Behav. Manag. 8, 99–104. doi: 10.2147/PRBM.S73901
Henry, J. D., and Crawford, J. R. (2005). The short-form version of the depression anxiety stress scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 44, 227–239. doi: 10.1348/014466505X29657
Ho, C. S., Chee, C. Y., and Ho, R. C. (2020). Mental health strategies to combat the psychological impact of covid-19 beyond paranoia and panic. Ann. Acad. Med. Singapore 49, 155–160.
Huang, J. Z., Han, M. F., Luo, T. D., Ren, A. K., and Zhou, X. P. (2020). Mental health survey of 230 medical staff in a tertiary infectious disease hospital for COVID-19. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 38, 192–195. doi: 10.3760/cma.j.cn121094-20200219-00063
Khalid, I., Khalid, T. J., Qabajah, M. R., Barnard, A. G., and Qushmaq, I. A. (2016). Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin. Med. Res. 14, 7–14. doi: 10.3121/cmr.2016.1303
Kim, J. S., and Choi, J. S. (2016). Factors influencing emergency nurses' burnout during an outbreak of middle east respiratory syndrome Coronavirus in Korea. Asian Nurs. Res. 10, 295–299. doi: 10.1016/j.anr.2016.10.002
Kuhn, M. (2015). caret: Classification and Regression Training. Astrophysics Source Code Library. Available online at: https://ui.adsabs.harvard.edu/abs/2015ascl.soft05003K (accessed May 03, 2020).
Lee, A. M., Wong, J. G., McAlonan, G. M., Cheung, V., Cheung, C., Sham, P. C., et al. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry 52, 233–240. doi: 10.1177/070674370705200405
Lee, S. M., Kang, W. S., Cho, A. R., Kim, T., and Park, J. K. (2018). Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 87, 123–127. doi: 10.1016/j.comppsych.2018.10.003
Leocani, L., Diserens, K., Moccia, M., and Caltagirone, C. (2020). Disability through COVID-19 pandemic: neurorehabilitation cannot wait. Eur. J. Neurol. doi: 10.1111/ene.14320. [Epub ahead of print].
Liebensteiner, M. C., Khosravi, I., Hirschmann, M. T., Heuberer, P. R., Thaler, M., Board of the AGA-Society of Arthroscopy Joint-Surgery, and Thaler, M. (2020). Massive cutback in orthopaedic healthcare services due to the COVID-19 pandemic. Knee Surg. Sports Traumatol. Arthrosc. 28, 1705–1711. doi: 10.1007/s00167-020-06032-2
Liu, Q., Luo, D., Haase, J. E., Guo, Q., Wang, X. Q., Liu, S., et al. (2020). The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study. Lancet Glob. Heal. 8, e790–e798. doi: 10.1016/S2214-109X(20)30204-7
Lovibond, P. F., and Lovibond, S. H. (1995). The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343. doi: 10.1016/0005-7967(94)00075-U
Low, Z. X., Yeo, K. A., Sharma, V. K., Leung, G. K., McIntyre, R. S., Guerrero, A., et al. (2019). Prevalence of burnout in medical and surgical residents: a meta-analysis. Int. J. Environ. Res. Public Health 16:1479. doi: 10.3390/ijerph16091479
Manzoni, P., and Milillo, C. (2020). Covid-19 mortality in Italian doctors. J. Infect. doi: 10.1016/j.jinf.2020.05.034. [Epub ahead of print].
Maslach, C., and Goldberg, J. (1998). Prevention of burnout: new perspectives. Appl. Prev. Psychol. 7, 63–74. doi: 10.1016/S0962-1849(98)80022-X
Maslach, C., Jackson, S., and Leiter, M. (1997). “The Maslach burnout inventory manual,” in Evaluating Stress: A Book of Resources (Palo Alto, CA: Consulting Psychologists Press), 191–218.
Maunder, R. G., Lancee, W. J., Balderson, K. E., Bennett, J. P., Borgundvaag, B., Evans, S., et al. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 12, 1924–1932. doi: 10.3201/eid1212.060584
Ornell, F., Schuch, J. B., Sordi, A. O., and Kessler, F. H. P. (2020). “Pandemic fear” and COVID-19: mental health burden and strategies. Braz. J. Psychiatry 42, 232–235. doi: 10.1590/1516-4446-2020-0008
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain. Behav. Immun. doi: 10.1016/j.bbi.2020.05.026. [Epub ahead of print].
Pedrabissi, L., and Santinello, M. (1989). Verifica della validità dello STAI forma Y di Spielberger. [Verification of the validity of the STAI, Form Y, by Spielberger.]. Giunti Organ. Spec. 191–192, 11–14.
Portoghese, I., Galletta, M., Coppola, R. C., Finco, G., and Campagna, M. (2014). Burnout and Workload among health care workers: the moderating role of job control. Saf. Health Work 5, 152–157. doi: 10.1016/j.shaw.2014.05.004
Ran, L., Chen, X., Wang, Y., Wu, W., Zhang, L., and Tan, X. (2020). Risk Factors of Healthcare Workers with Corona Virus Disease 2019: A Retrospective Cohort Study in a Designated Hospital of Wuhan in China. Clin. Infect. Dis. ciaa287. doi: 10.1093/cid/ciaa287. [Epub ahead of print].
Salvagioni, D. A. J., Melanda, F. N., Mesas, A. E., González, A. D., Gabani, F. L., and Andrade, S. M. de (2017). Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS ONE 12:e0185781–e0185781. doi: 10.1371/journal.pone.0185781
Schaufeli, W. B., and Van Dierendonck, D. (1995). A cautionary note about the cross-national and clinical validity of cut-off points for the Maslach Burnout Inventory. Psychol. Rep. 76, 1083–1090. doi: 10.2466/pr0.1995.76.3c.1083
Sirigatti, S., Stefanile, C., and Menoni, E. (1988). Per un adattamento italiano del Maslach Burnout Inventory (MBI) [Toward an Italian version of the Maslach Burnout Inventory (MBI)]. Boll. di Psicol. Appl. 187–188, 33–39.
Spielberger, C., Gorsuch, R., Lushene, R., Vagg, P. R., and Jacobs, G. (1983). Manual for the State-Trait Anxiety Inventory (Form Y1 – Y2). Palo Alto, CA: Consulting Psychologists Press.
Tam, C. W. C., Pang, E. P. F., Lam, L. C. W., and Chiu, H. F. K. (2004). Severe acute respiratory syndrome (SARS) in Hongkong in 2003: stress and psychological impact among frontline healthcare workers. Psychol. Med. 34, 1197–1204. doi: 10.1017/S0033291704002247
Tan, B. Y. Q., Chew, N. W. S., Lee, G. K. H., Jing, M., Goh, Y., Yeo, L. L. L., et al. (2020a). Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. M20–M1083. doi: 10.7326/M20-1083
Tan, W., Hao, F., McIntyre, R. S., Jiang, L., Jiang, X., Zhang, L., et al. (2020b). Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain. Behav. Immun. 87, 84–92. doi: 10.1016/j.bbi.2020.04.055
Thoresen, S., Tambs, K., Hussain, A., Heir, T., Johansen, V., and Bisson, J. (2009). Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc. Psychiatry Psychiatr. Epidemiol. 45, 405–412. doi: 10.1007/s00127-009-0073-x
Tran, B. X., Ha, G. H., Nguyen, L. H., Vu, G. T., Hoang, M. T., Le, H. T., et al. (2020). Studies of Novel Coronavirus Disease 19 (COVID-19) pandemic: a global analysis of literature. Int. J. Environ. Res. Public Health. 17:4095. doi: 10.3390/ijerph17114095
Wang, C., Horby, P. W., Hayden, F. G., and Gao, G. F. (2020a). A novel coronavirus outbreak of global health concern. Lancet 395, 470–473. doi: 10.1016/S0140-6736(20)30185-9
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020b). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain. Behav. Immun. 87, 40–48. doi: 10.1016/j.bbi.2020.04.028
Weiss, D. S. (2007). “The impact of event scale: revised BT,” in Cross-Cultural Assessment of Psychological Trauma and PTSD, eds J. P. Wilson and C. S. Tang (Boston, MA: Springer US, 219–238.
Wiederhold, B. K., Cipresso, P., Pizzioli, D., Wiederhold, M., and Riva, G. (2018). Interventions for physician burnout: a systematic review of systematic reviews. Int. J. Prev. Med. 9, 253–263. doi: 10.1515/med-2018-0039
Wilder-Smith, A., and Freedman, D. O. (2020). Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J. Travel Med. 27:taaa020. doi: 10.1093/jtm/taaa020
Woo, T., Ho, R., Tang, A., and Tam, W. (2020). Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J. Psychiatr. Res. 123, 9–20. doi: 10.1016/j.jpsychires.2019.12.015
World Health Organization (2020a). Coronavirus Disease 2019 (COVID-19) Situation Report - 116. Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200515-covid-19-sitrep-116.pdf
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Zhang, C., Yang, L., Liu, S., Ma, S., Wang, Y., Cai, Z., et al. (2020). Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry. 11:306. doi: 10.3389/fpsyt.2020.00306
Keywords: COVID-19, burnout, depression, anxiety, post-traumatic stress, predictors, clinical psychology, cross-sectional study
Citation: Giusti EM, Pedroli E, D'Aniello GE, Stramba Badiale C, Pietrabissa G, Manna C, Stramba Badiale M, Riva G, Castelnuovo G and Molinari E (2020) The Psychological Impact of the COVID-19 Outbreak on Health Professionals: A Cross-Sectional Study. Front. Psychol. 11:1684. doi: 10.3389/fpsyg.2020.01684
Received: 29 May 2020; Accepted: 22 June 2020;
Published: 10 July 2020.
Edited by:
Konstantinos Papazoglou, Yale University, United StatesReviewed by:
Roger C. Ho, National University of Singapore, SingaporeCopyright © 2020 Giusti, Pedroli, D'Aniello, Stramba Badiale, Pietrabissa, Manna, Stramba Badiale, Riva, Castelnuovo and Molinari. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Emanuele Maria Giusti, ZS5naXVzdGlAYXV4b2xvZ2ljby5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.