
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 28 January 2020
Sec. Psychology for Clinical Settings
Volume 11 - 2020 | https://doi.org/10.3389/fpsyg.2020.00075
This article is part of the Research Topic Mind the Heart – Psychosocial Risk Factors and Cognitive Functioning in Cardiovascular Disease View all 13 articles
Objective: Research on psychosocial risk factors in cardiovascular disease (CVD) has identified traumatic stress and attachment style as independent risk factors for the development of CVD and poor prognosis for those with established CVD. Exploring the interrelationships between these variables will inform psychosocial risk factor modeling and potential avenues for intervention. Therefore, the hypothesis that attachment style is related to health outcomes among CR patients and that traumatic stress mediates this relationship was tested.
Methods: Patients in a cardiac rehabilitation program (n = 201) completed validated self-report measures of traumatic stress and attachment style at baseline (program intake). Health outcomes were assessed at baseline and 3 months, including anxiety, depression, quality of life, fasting blood glucose, glycated hemoglobin (HbA1c), and cholesterol (HDL ratio). Multivariate structural equation modeling was used to fit the data.
Results: Of the 201 participants, 42 (21%) had trauma scores indicating the probable presence of posttraumatic stress disorder. Via greater levels of traumatic stress, greater attachment anxiety at baseline was indirectly related to greater anxiety, depression, fasting blood glucose, and HbA1c, and poorer physical and mental quality of life. There were no significant indirect effects on HDL ratios.
Conclusion: Greater attachment anxiety predicted greater traumatic stress; this, in turn, predicted poorer health outcomes. Screening and treatment for these constructs in CVD patients is warranted.
Cardiovascular disease (CVD) includes a host of different disorders of the heart and blood vessels, such as coronary artery disease and hypertension, and symptoms typically manifest only after the disease has progressed to an advanced stage (Perk et al., 2012). Prevalence rates of CVD in the United States (Mozaffarian et al., 2015) and Canada (Government of Canada, 2019) are very high (6.2 and 7.8%, respectively), especially for an ostensibly preventable disease (Mozaffarian et al., 2015), and these rates are associated with a significant societal financial burden (Trogdon et al., 2007; Mozaffarian et al., 2015). As the population of people with CVD in developed countries continues to increase, so does the need for preventative medicine (Yazdanyar and Newman, 2009).
The promotion of health behavior change is central to CVD prevention efforts. These changes focus on reducing or moderating specific risk factors; these can be behavioral in nature, such as managing weight loss, quitting smoking, or eating healthier (Mozaffarian et al., 2015), they can be physiological, such as targeting specific CVD markers like hypertension, high cholesterol, or lack of exercise (Lee et al., 2012), or, these risk factors can psychological, such as elevated anxiety and depression (Rothenbacher et al., 2007; Whalley et al., 2014; Blumenthal et al., 2016), insecure attachment (Maunder and Hunter, 2001), and lower levels of psychological well-being (Boehm and Kubzansky, 2012).
Interest in attenuating psychological risk factors has grown in recent years, as some targeted psychosocial interventions have proven effective in reducing cardiac events (Whalley et al., 2014; Blumenthal et al., 2016; Richards et al., 2018), which is positive, as individuals with CVD are known to have elevated rates of anxiety (Frasure-Smith and Lespérance, 2008; Bunevicius et al., 2013) and depression (Frasure-Smith and Lespérance, 2008; Lichtman et al., 2008). Stress and depression directly contribute to poorer cardiovascular health by increasing blood pressure (Rothenbacher et al., 2007), vascular inflammation, and endothelial dysfunction (Williams and Steptoe, 2007). Indirectly, greater anxiety and depression promote other unhealthy behaviors (e.g., sedentary behavior, smoking) that exacerbate CVD risk.
One potential psychosocial risk factor for CVD that has not yet been fully explored is insecure attachment, a construct that has been associated with increased prevalence of illness and disease (Maunder and Hunter, 2001; McWilliams and Bailey, 2010; Pietromonaco et al., 2013; Pietromonaco and Collins, 2017). Attachment was first described in the literature over four decades ago; it is defined as the tendency for human beings to develop strong emotional bonds with significant people in their lives, referred to as “attachment figures,” as a principal means of emotion regulation in the face of stress or potential danger (Bowlby, 1958, 2005; Ainsworth and Bell, 1970). Secure attachment refers to the tendency to seek out emotional support and comfort from an attachment figure in situations of stress or emotional pain. Securely attached individuals perceive others as safe and trustworthy (Bowlby, 1980); thus, they are able to receive comfort and reassurance when they need it to reduce stress. Insecure attachment, however, is characterized by the tendency to either avoid seeking out emotional support and closeness from others (i.e., avoidant attachment) or exist in a near-constant state of reassurance-seeking that often leaves one feeling distressed and vulnerable, rather can calm and safe (i.e., anxious attachment; Bartholomew and Horowitz, 1991; Simpson and Rholes, 2017).
Instead of deriving reassurance and comfort from their relationships with attachment figures, people who are insecurely attached are more likely to worry and to feel uneasy about these relationships. This is highly stressful and is thought to contribute to the onset and course of chronic disease (Maunder and Hunter, 2001; McWilliams and Bailey, 2010; Pietromonaco et al., 2013; Pietromonaco and Collins, 2017). More specifically, the theorized mechanisms by which insecure attachment relates to increased disease risk include higher cortisol levels during times of stress (Luecken, 1998; Quirin et al., 2008; Pierrehumbert et al., 2012), augmented blood pressure during social interactions (Gallo and Matthews, 2006), and heavier reliance on external regulators for emotions, including alcohol and tobacco (Maunder and Hunter, 2001).
Although there is a known link between a lack of social relationships and increased mortality in general (Cerhan and Wallace, 1997; Holt-Lunstad et al., 2010; Barger, 2013), only a handful of studies have examined the impact of attachment style on heart health (Vilchinsky et al., 2010; Pietromonaco et al., 2013; Peleg et al., 2017; Pietromonaco and Collins, 2017). This may indicate an important gap in the literature, as the studies that have been conducted suggest a connection between insecure attachment and poor health (West et al., 1995; Bohachick et al., 2002; McWilliams and Bailey, 2010; Pietromonaco and Collins, 2017). For example, in one sample of the general population (N = 5645), insecure attachment was identified as a risk factor for the development of chronic illness, especially conditions related to the cardiovascular system (McWilliams and Bailey, 2010). Likewise, a follow-up study of heart transplant patients revealed that those with insecure attachment had worse functional outcomes 6 months after the procedure than did patients with secure attachment (Bohachick et al., 2002). A recent investigation found similar results; the researchers found insecure attachment styles were significantly more prevalent among people with coronary artery disease compared to healthy controls (Oladi and Dargahi, 2018).
There are known mechanistic links between attachment and CVD risk factors; for example, inflammation has been identified as a major contributor to the onset of heart disease, and there is evidence that both avoidant and anxious attachment are related to the production of the IL-6 in stressful situations such as conflict discussions between spouses and even CABG surgery (Kidd et al., 2014; Ehrlich, 2019). Despite some anti-inflammatory properties that have been noted, IL-6 is generally considered atherogenic, to the point where some researchers have suggested targeting it as a treatment for atherosclerosis (Reiss et al., 2017). Cardiovascular reactivity is another risk factor that researchers have linked to attachment and the development of CVD. Compared to when doing a cold pressor task alone, securely attached participants had significantly reduced systolic and diastolic blood pressure when their primary attachment figures were present or when they were instructed to think about them (Bourassa et al., 2019). Greater reductions in heart rate variability have also been detected during this stress task among participants with high levels of attachment avoidance (Bryant and Hutanamon, 2018). Once again, greater attachment security was related to less cardiovascular risk, and vice versa. Lastly, attachment insecurity has also been linked to primary hypertension. One group of researchers observed that 88% of hypertensive patients presented as insecurely attached, as compared to 50% in non-clinical populations (Balint et al., 2016).
Insecure attachment throughout the lifespan is also a robust predictor of psychopathology. For example, Stovall-McClough and Dozier (2016) noted in a comprehensive review of the literature that anxious, avoidant, and disorganized (i.e., sometimes anxious, sometimes avoidant) attachment styles detected during childhood play a key role in the development of major depression, anxiety disorders, dissociative disorders, and personality disorders later in life. The findings of more recent studies corroborate these results; insecure attachment (anxious and avoidant) has been linked to major depression comorbid with generalized anxiety disorder (GAD), panic disorder, and PTSD in adults (Huang et al., 2019), whereas fear of rejection by romantic partners and fearful attachment in general has also predicted the presence of mental-health problems among adults (Alonso et al., 2018). Taken together, these findings suggest that the subjective sense of loneliness typical of people with insecure attachment styles might contribute to the onset and course of psychological problems. This makes sense considering that, according to attachment theory, the perceived emotional unavailability of an attachment figure, especially in times of stress, is inherently traumatizing for human beings (Johnson, 2020), with all of the physical and psychological implications that the experience of trauma can have.
Symptoms of traumatic stress can also occur following a cardiac event; in fact, a systematic review of PTSD induced by a cardiac event revealed an average prevalence of about 12% of cardiac samples across 150 studies and noted that pre-existing psychological risk factors were important predictors in developing PTSD in this manner (Vilchinsky et al., 2017). Symptoms of PTSD, generally, include intrusive thoughts or images (flashbacks, nightmares), avoidance of triggering stimuli, emotional numbing, hyperarousal, sleep difficulties, and negative cognitions and mood (American Psychiatric Association, 2013). A diagnosis of PTSD is made when symptoms of traumatic stress are significant enough to disrupt an individual’s functioning or to cause them clinically significant distress. A recent systematic review of 21 studies of attachment and post-traumatic stress in the general population revealed that insecure attachment consistently had mediating and moderating effects on the link between the experience of a traumatic stressor and the onset of symptoms of post-traumatic stress (Barazzone et al., 2019). The more insecurely attached a person is, the more likely he or she appears to develop PTSD in the face of a traumatic event. Potential reasons for this correlation might be that people with insecure attachment perceive a lack of emotional support and are therefore less resilient to trauma. Those with anxious attachment also report greater distress than do those with secure or avoidant attachment, indicating that they may be more focused on, and sensitive to, threatening stimuli.
With respect to cardiovascular functioning, chronic traumatic stress is detrimental to the heart; it is linked to increased heart rate, blood pressure, and substance abuse (Bedi and Arora, 2007; Coughlin, 2011); as well as greater risk of developing CVD (Kubzansky et al., 2007, 2009; Boscarino, 2008) and negative physical and mental health outcomes in patients with CVD (Whitehead et al., 2006; Edmondson and Cohen, 2013; Ginzburg et al., 2016). In one study of over 1000 patients with CVD followed over 7.5 years, exposure to traumatic events throughout the lifespan predicted greater mortality and a greater number of adverse cardiovascular events (Hendrickson et al., 2013). Moreover, the experience of potentially fatal cardiovascular events (e.g., myocardial infarction) has been shown to induce PTSD in some patients (Spindler and Pedersen, 2005; Edmondson et al., 2011, 2012; Edmondson and Cohen, 2013), and PTSD symptoms after such an event, in turn, are linked to subsequent cardiac health problems (Wikman et al., 2008; Edmondson et al., 2011) and all-cause mortality (Edmondson et al., 2011). To our knowledge, no one has yet examined the role of both attachment insecurity and traumatic stress in a CVD population, despite the potential for attachment insecurity to explain some of the well-documented effects of trauma on the heart.
The main objective of this study was to test a model predicting health outcomes measured at 3 months in a CR population using baseline measures of attachment style and traumatic stress. Multivariate SEM was used to test the following hypotheses: (1) insecure attachment (i.e., avoidant or anxious attachment) would be associated with greater traumatic stress symptoms, (2) elevated traumatic stress and insecure attachment would each be independently associated with poorer cardiac-related physical and mental health outcomes, and (3) traumatic stress would mediate the relationship between insecure attachment and poorer physical and mental health outcomes.
Patients enrolled in the cardiac rehabilitation program (CR) at the UOHI were assessed at baseline (program intake) and 3 months (end-of-program). The CR program consists of exercise, education, and allied health services (e.g., nurses, physiotherapists, vocational rehabilitation). Patients are automatically referred to CR following discharge from hospital (Tiller et al., 2013). Only those who were unable to speak/read in English or French were excluded from the study. This study was approved by the Ottawa Health Science Network Research Ethics Board.
A power analysis was conducted using the software G∗Power 3 (Faul et al., 2007) in order to calculate the minimum sample size required to achieve sufficient power for the statistical analyses involved. With a power level a 0.80 and an alpha of 0.05, it was estimated that a sample size of 200 would be required. This is also in keeping with the minimum suggested sample size for SEM (i.e., N = 200), suggested by Kline (2011).
Individuals participating in the CR program at the UOHI were recruited at the patient’s standard intake into the program. A healthcare professional in the prospective participant’s circle of care provided an overview of the study and obtained consent for research staff to approach the patient. Research personnel obtained written informed consent and administered baseline questionnaires on-site. Physiological variables [fasting blood glucose concentration (mmol/L), glycated hemoglobin (HbA1c;%), HDL cholesterol ratios] were assessed at baseline by CR staff as part of standard intake procedure and then again at 3 months when participants returned for on-site follow-up appointments as part of standard care at the CR program. With respect to psychosocial variables, anxiety, depression, and quality of life were assessed at baseline and 3 months, while attachment and traumatic stress were assessed at baseline only. For those variables measured at 3 months, follow-up questionnaires (3 months) were mailed to participants along with a prepaid return envelope so that participants could mail back completed questionnaires.
At baseline, participants reported their age, sex, ethnicity, and marital status (see Table 1). Compliance with CR was calculated as the percentage of prescribed CR appointments patients attended. Participants’ cardiac diagnoses and relevant cardiac procedures are also provided in Table 1.
Attachment style was measured using the validated (Fraley et al., 2000) and reliable (Sibley et al., 2005) Experiences in Close Relationships-Revised (ECR-R). The ECR-R has 36 items designed to measure two individual factors of attachment: attachment anxiety (i.e., the degree to which a person worries their attachment figures will not be available or supportive when they need them) and attachment avoidance (i.e., the degree to which a person distrusts their attachment figures and achieves self-assurance by maintaining emotional distance). Each item consists of a statement regarding how the respondent feels in emotionally intimate relationships. Responses are indicated on a 7-point Likert-type scale (1 = Strongly Disagree; 7 = Strongly Agree) and the summed total of all items in each attachment style represents the score for that attachment style. Higher values indicate stronger affiliation with a particular attachment style.
Traumatic stress was measured using the validated (Horowitz et al., 1979) and reliable (Rash et al., 2008), 22-item Impact of Event Scale-Revised (IES-R). On the IES-R, respondents are asked questions about how they have been feeling over the last week with reference to their traumatic event (participants were asked specifically to refer to their cardiac event). Responses are indicated on a 5-point Likert-type scale (0 = Not at All; 4 = Extremely) and the summed total of all items serves as the total score. Higher scores indicate greater traumatic stress and scores of 33 or higher are indicative of a probable diagnosis of PTSD. The IES-R has been previously validated in a CVD population (Eslami, 2017).
The HADS (Zigmond and Snaith, 1983) is a 14-item self-report measure of anxiety (seven items) and depression (seven items) that has been used often in clinical populations, including with cardiac patients (Tulloch et al., 2018; Lemay et al., 2019). The HADS examines a range of anxious (e.g., muscle tension, panic-like symptoms, constantly worrying) and depressive (e.g., decreased mood, loss of interest, lack of motivation) symptoms. Symptoms statements are rated on a scale from 0 to 3. The HADS produces separate total scores for anxiety and depression (scores range from 0 to 21), with higher scores indicating greater levels of anxiety or depression; scores of 5 (depression) and 7 (anxiety) or greater are considered the cut-offs for clinical screening (Singer et al., 2009). The validity (Bjelland et al., 2002) and reliability (Boxley et al., 2016) of this measure has been demonstrated.
Physical and mental quality of life was measured using the Short Form Health Survey Questionnaire, Version 1 (SF-36, V.1; Ware and Sherbourne, 1992), a self-report questionnaire containing 36 items. For the physical health (i.e., summed total of scale scores for “physical functioning,” “physical role functioning,” “bodily pain,” and “general health perceptions”) and mental health (i.e., summed total of scale scores for “vitality,” “emotional role functioning,” “social role functioning,” and “mental health”) total scores, higher values indicate better perceived physical or mental quality of life, respectively. This measure has been validated previously in a CVD population (Muller-Nordhorn, 2004) and has demonstrated reliability (Bunevicius, 2017).
Blood samples were drawn to assess physiological health outcomes, including fasting blood glucose concentration (mmol/L), glycated hemoglobin (HbA1c;%), and cholesterol information, including HDL ratios (total cholesterol/HDL), which have been shown to be superior predictors of poor cardiovascular health than other indicators of cholesterol (Lemieux et al., 2001); higher cholesterol is a risk factor for CVD as it indicates greater risk of arterial plaque deposits. Greater fasting blood glucose or HbA1c are indicative or greater risk of CVD, and can indicate prediabetes or diabetes.
Missing data were evaluated following the procedures outlined by Tabachnick and Fidell (2007), and were imputed using multiple imputation (i.e., missing values replaced with means of 5 repeated imputations; Rubin, 1996). The effect of participating in the CR program on all dependent variables was assessed using a repeated-measures MANOVA. For the multivariate SEM analyses, the following parameters were used to determine excellent model fit: non-significant χ2, CFI ≥ 0.95, RMSEA < 0.07, and values ranging from 2 to 3 for CMIN/df (Hooper et al., 2008). Modification indices were examined to identify instances where variables and error terms were highly correlated; these relationships were allowed to covary within the model to improve fit. The main theoretical model consisted of baseline attachment anxiety and attachment avoidance, predicting traumatic stress, with traumatic stress in turn predicting all end-of-intervention health outcomes (see Figure 1). Compliance and baseline measures of health outcome variables were included in the model as controls. For all standardized indirect coefficients, the bias-corrected percentile method of generating two tailed significance values was used. Indirect effects were calculated using 2000 bootstrap samples.
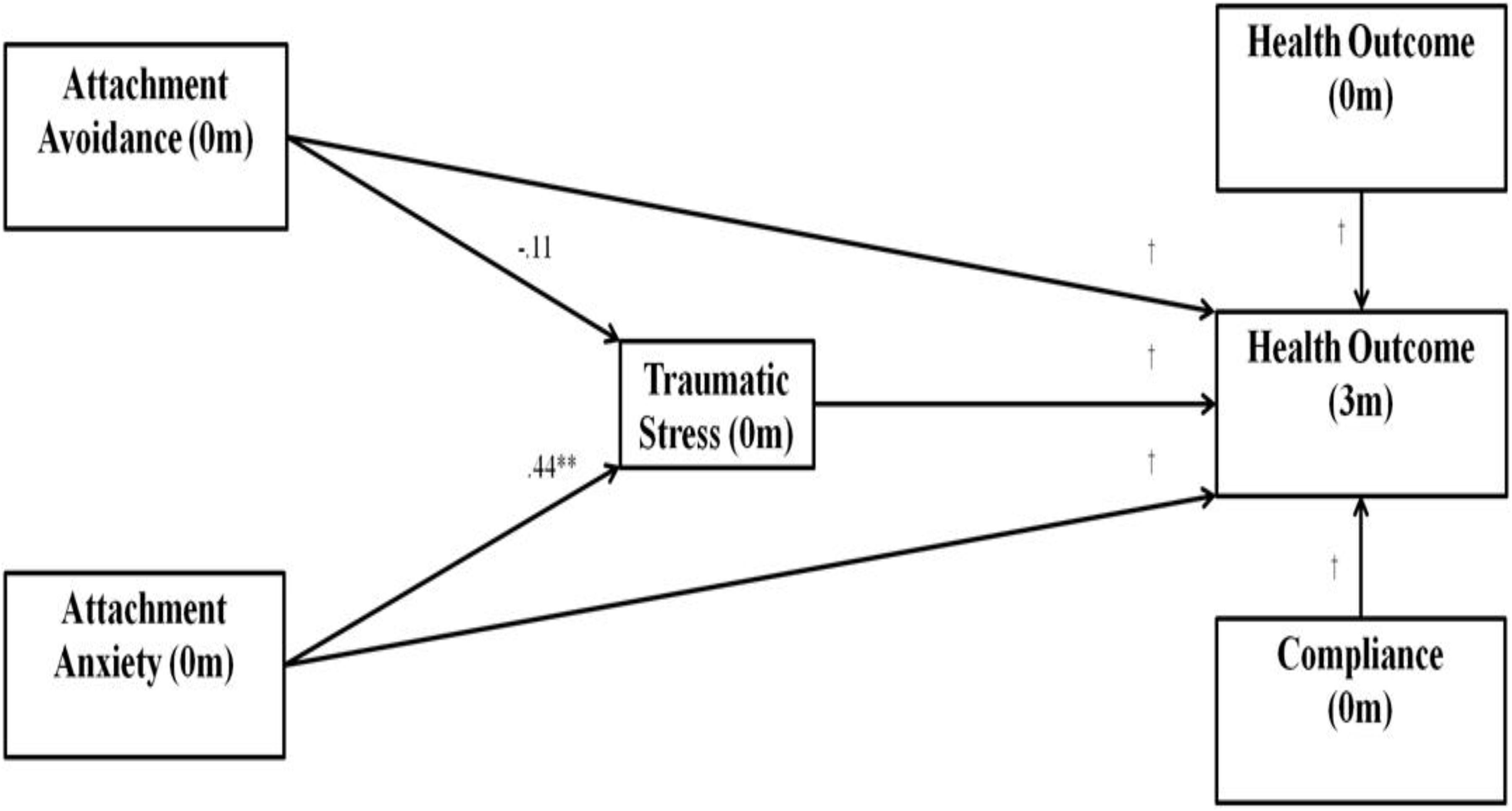
Figure 1. Multivariate structural equation model used for path analysis. Hypothesized pathways included attachment anxiety and avoidance having indirect effects on health outcome variables through traumatic stress. m, months.
All variables were normally distributed. For baseline data, 9 and 10% of the data were missing for attachment anxiety and attachment avoidance subscales respectively, while 8% of the data were missing for the IES-R. Regarding information collected at baseline and 3 months, HADS scores were missing 1 and 23%, respectively, SF-36 scores were missing 0 and 33%, fasting blood glucose values were missing 2 and 21%, glycated hemoglobin (HbA1c) values were missing 4 and 29%, and HDL ratio values were missing 1 and 20%. Compliance data were missing 10%. Missing values were found to be missing at random, Little’s MCAR (747) = 42.87, p = 0.999.
We approached 410 patients for the study. Of those, 409 were eligible (1 was not eligible due to language barrier), 288 agreed to participate (70% of eligible patients), and 201 completed the baseline questionnaires (70% of consented patients). Between baseline and follow-up, 2 patients died, 2 were out of the country, 9 dropped out of the study (2 said they felt it was not relevant to them, 2 had insufficient time, and 5 stated they were no longer interested), and 23 were unreachable, leaving 165 participants (82%) with completed 3-month data.
A demographic summary is presented in Table 1. The participants (n = 201) ranged in age from 24 to 89 years (M = 62.08, SD = 10.87) and were predominately male (n = 160, 80%), white (n = 189, 94%), and married (n = 150, 75%). Regarding traumatic stress, 42 (21%) scored above 33 on the IES-R, suggesting the probable presence of PTSD. On the HADS at baseline, a minority of individuals with scores above the cut-offs on anxiety (n = 86, 43%) and depression (n = 75, 37%); at 3 months, the number of those who scored high on the anxiety subscale had dropped moderately (n = 55, 27%) while those above the depression cut-off dropped off to a lesser degree (n = 61, 30%). The sample mean for fasting blood glucose concentration was above the normal range of 3.9 – 5.6 mmol/L (The Emerging Risk Factors Collaboration, 2010) at both baseline and 3 months and the sample mean for HbA1c was above the normal range of 3.8–5.9% (Cavalot et al., 2006) at both baseline and 3 months. The sample mean for HDL ratio was below the highest risk cut-off of 5 at both baseline (M = 3.25, SD = 0.96) and 3 months (M = 2.99, SD = 0.79) (Manninen et al., 1992). Compliance was high (M = 82.42%, SD = 25.17); about a third of participants attended every session (n = 73, 36.3%).
A repeated measures MANOVA on all dependent variables was significant, F(7,194) = 29.78, p < 0.001, Wilk’s λ = 0.48, partial η2 = 0.52. Depression (p = 0.003), anxiety (p < 0.001), and HDL ratio (p < 0.001), were all significantly lower at 3 months compared to baseline; physical quality of life (p < 0.001) and mental quality of life (p < 0.001) were significantly higher at 3 months compared to baseline. There was no significant change in fasting blood glucose or HbA1c values between baseline and 3 months. See Table 2 for all means, standard deviations, and zero-order correlations between variables.
The multivariate SEM model (with standardized estimates) can be found in Figure 2. The model fit statistics indicated the hypothesized model was a good fit of the data; the chi-square test was not significant [χ2(74) = 91.30, p = 0.084], and the measures of approximate fit were: RMSEA = 0.03 (CI90% = 0.00,0.06), CFI = 0.99, CMIN/df = 1.23.
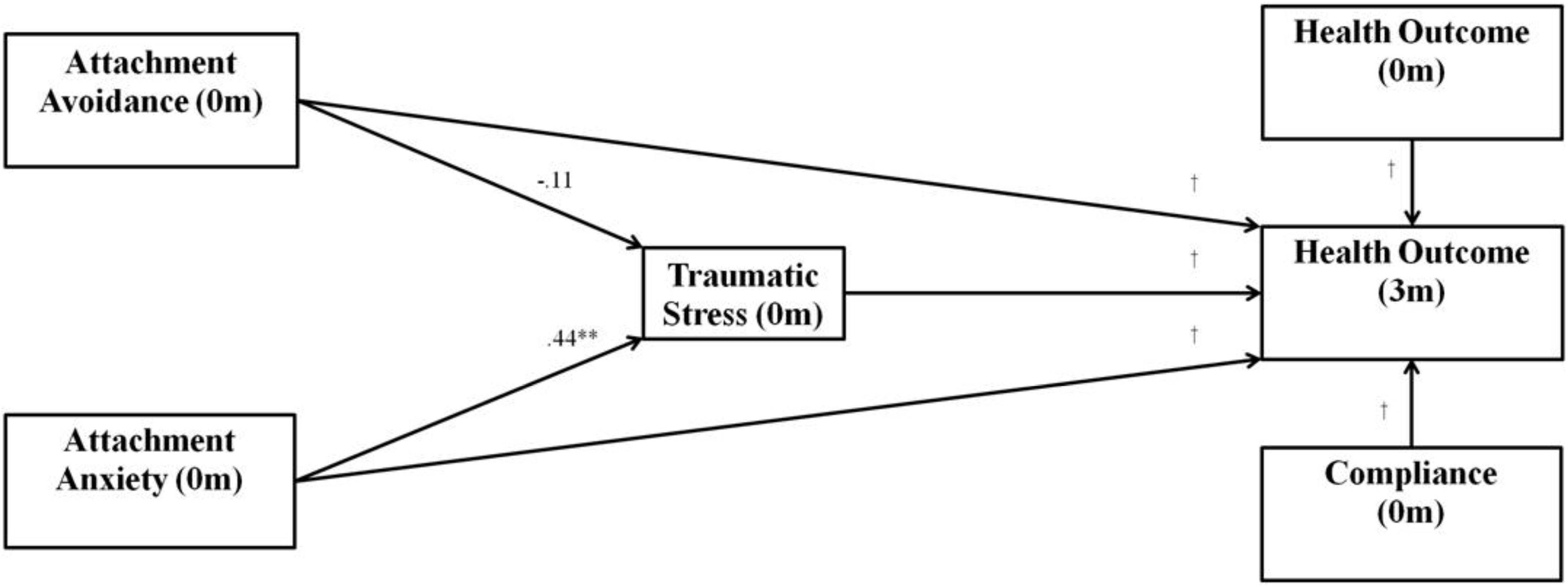
Figure 2. Multivariate structural equation model used for path analysis with values representing standardized regression coefficients. The hypothesized pathways include attachment anxiety and avoidance having indirect effects on health outcome variables through traumatic stress. ∗∗p < 0.01, m, months, †values are presented in Table 2. Indirect effects for model are shown in Table 3.
The results of the path analysis were that baseline attachment anxiety had a significant, positive indirect effect (via traumatic stress) on depression, anxiety, fasting blood glucose, and HbA1c, and a significant, negative indirect effect on mental quality of life and physical quality of life (see direct effects in Table 3 and indirect effects in Table 4). The indirect effect of baseline attachment anxiety on HDL ratio was not significant; however, greater baseline attachment anxiety directly predicted significantly greater HDL ratios. There were no significant indirect effects of baseline attachment avoidance on any outcome variable.
The purpose of the present study was to test a model predicting physical and mental health outcomes in CVD patients using measures of attachment style and traumatic stress. To this end, CR patients were assessed at baseline (program intake) and 3-month follow-up (end-of-program) on a variety of outcomes.
The first hypothesis was that insecure attachment (i.e., attachment anxiety or avoidance) would be positively associated with traumatic stress. In support of this, the zero-order correlations (see Table 2) between attachment anxiety, attachment avoidance, and traumatic stress were all significant and positive. The SEM results, however, supported this hypothesis only for attachment anxiety; attachment avoidance did not significantly predict traumatic stress (see Figure 2).
One reason why attachment anxiety might associate with greater traumatic stress is that individuals with anxious attachment appear to be more sensitive to detecting threatening stimuli (Barazzone et al., 2019). This focus on potential threat, coupled with generally less perceived social support compared to securely attached individuals, may make those with anxious attachment less resilient to trauma. Perceived social support is known to be among the most important buffers against symptoms of PTSD (e.g., Guay et al., 2006; Stanley et al., 2018). It follows logically that insecurely attached people would be more susceptible to the effects of trauma than would securely attached people.
It has also been proposed that traumatic experiences, such as an acute cardiac event, activate the attachment system. Although both securely attached and anxiously attached individuals are likely to seek out reassurance and comfort from their attachment figures, those who are anxiously attached are less likely to perceive and to integrate the emotional support that is offered. This drives them to persist in their bids for reassurance, which might strain their close relationships and add additional barriers against processing trauma effectively (Mikulincer et al., 2007, 2015).
Alternatively, our finding that attachment avoidance did not significantly predict traumatic stress is not without precedent. For example, in one meta-analysis, there was no relationship between attachment avoidance and traumatic stress, though the authors noted that this may have been due to the tendency to underreport, especially when completing self-report measures (Woodhouse et al., 2015). Psychophysiological measures that tap into adrenocortical activity, skin conductance, and heart rate, are generally more sensitive indicators of stress among people with avoidant attachment styles (Gander and Buchheim, 2015). For this reason, it is likely that the lack of a link between attachment avoidance and traumatic stress may be more related to a lack of reporting than to true resilience against trauma. Individuals with an avoidant attachment style tend to dismiss or compartmentalize trauma without seeking support from others, which seems to disrupt the ability to process trauma effectively (Mikulincer et al., 2007). In addition, there is some evidence that individuals with avoidant attachment express fewer positive and negative psychological symptoms, tending to experience psychological symptoms that are negative to neutral (Kerr et al., 2003). In accordance with this, almost all zero-order correlations in the present study between attachment scores and outcome variables were greater for anxious attachment than they were for avoidant attachment. Future research is required to fully understand the relationships between trauma and both types of insecure attachment; however, it is possible our theoretical model is only appropriate for those with anxious attachment.
Second, it was hypothesized that insecure attachment (i.e., greater attachment anxiety and avoidance) and greater traumatic stress would each independently predict poorer health outcomes. Again, this hypothesis was partially supported (see Table 3).
While greater attachment anxiety directly predicted several poorer health outcomes, attachment avoidance predicted significantly higher fasting blood glucose values only. This, as well as the finding that attachment anxiety had significant indirect effects on many outcome variables and attachment avoidance had none (see Table 4), suggests that attachment anxiety, not avoidance, may drive the previously observed relationship between insecure attachment and poorer health (Maunder and Hunter, 2001).
The third hypothesis was that traumatic stress would mediate the relationship between insecure attachment and poorer physical and mental health outcomes. The results of the multivariate SEM supported this hypothesis for attachment anxiety only.
Greater baseline attachment anxiety was indirectly related to greater anxiety, depression, fasting blood glucose, and HbA1c levels at 3 months, and poorer physical and mental quality of life at 3 months. There were no significant indirect effects of attachment avoidance on any outcome measure; however, our findings are the first evidence that attachment anxiety is associated with poorer health outcomes in CVD patients via the experience of traumatic stress, which is an important finding. It is the first substantial empirical evidence of the notion that people with an anxious attachment style may be so preoccupied with their attachment relationships that it puts their health at risk.
In previous research, attachment anxiety has been linked to greater cortisol levels in times of stress (Quirin et al., 2008), and augmented diastolic and systolic blood pressure during social interactions (Gallo and Matthews, 2006). Our findings complement these and demonstrate that attachment anxiety is highly predictive of negative outcomes in people with heart disease. People with an anxious attachment style experience a great deal of interpersonal stress throughout most of their lives (Simpson and Rholes, 2017); their intense fear of losing meaningful attachment relationships and the accompanying hyperactivation of the attachment system might reach chronic levels similar to the hypervigilance that characterizes PTSD, with all of the health risks this can pose.
Although attachment anxiety was directly and indirectly linked to poor physical and mental health outcomes, attachment avoidance was not. The only finding related to CVD risk factors that was observed for attachment avoidance was that greater attachment avoidance at baseline was directly related to greater fasting blood glucose levels at 3 months. Regarding relationships with mediating factors in the SEM model, greater attachment avoidance predicted significantly lower levels of traumatic stress, which is at odds with previous findings (Clark and Owens, 2012). One possibility is that attachment avoidance may provide some measure of protection or resiliency against traumatic stress, but at the cost of fewer people who could potentially provide positive support. Alternatively, those who score higher in attachment avoidance tend to have less insight into and ability to express their own emotional experiences, otherwise known as alexithymia (Fantini-Hauwel et al., 2012). They might underreport traumatic stress, which may be the more plausible interpretation of this finding.
The present study is not without limitations. Our CR patients were diverse in terms of cardiac diagnoses (see Table 1), meaning our relatively small sample size (N = 201) precluded diagnosis-based analyses of our data. Furthermore, we lacked some important variables (e.g., length of time since cardiac event, duration of hospitalization, etc.) that are important in the context of understanding the nature of traumatic stress. In many ways, our sample may be considered a relatively small subsample of the overall cardiac population; larger cohort studies could provide additional evidence regarding the relationship between attachment style and traumatic stress in specific cardiac subgroups. Understanding whether there are differences in terms of cardiac diagnoses would inform screening and treatment considerations in these groups.
Although diverse in terms of CVD, our sample was quite homogenous in other ways, further limiting the degree to which our findings may generalize to other settings. Our group of participants were mainly white, married, and highly educated; while this reflects the nature of who attends CR in our clinical setting and thus has clinical validity here, it makes examining relationships between study variables and sample variables (e.g., ethnicity) very difficult with a sample this size, disqualifying some potentially interesting analyses.
Finally, future studies could conduct longer-term follow up (i.e., compared to the 3 months presented here), and more thorough data collection (e.g., length of time since cardiac event, as listed above). The design of the present study was made with the structure of the current CR program in mind; alternative studies in a less clinical setting could prioritize more rigorous follow-up procedures, longer-term data-collection window, and greater control over the type of data collected from participants.
In the present sample of patients participating in a CR program, greater attachment anxiety predicted greater traumatic stress; this, in turn, predicted poorer physical and mental health outcomes. Via traumatic stress, baseline attachment anxiety was indirectly linked with a host of negative outcomes at 3 months, including greater anxiety, depression, fasting blood glucose, and HbA1c levels. Stated differently, people who tend to fear emotional abandonment and loss appear to be more susceptible to traumatic stress in the context of heart disease, which in turn seems to have negative effects on their mental and physical health, itself known to further worsen CVD (e.g., Williams and Steptoe, 2007).
Screening and interventions designed to target elevated attachment anxiety and traumatic stress should be considered for future study. Attachment-focused therapies such as Emotionally Focused Individual Therapy (EFIT; Johnson, 2019), Emotionally Focused Therapy (EFT) for couples (Johnson, 2020), or interpersonal psychodynamic approaches (Yalom, 1995) are interventions that might be particularly effective with the CVD population, due to their emphasis on helping clients develop and maintain secure attachment bonds to the most significant people in their lives. Another program that has shown promise among people with heart disease and their partner is Healing Hearts Together (Tulloch et al., 2016, 2017), which is heavily based on the principles of attachment theory and EFT. Whatever the intervention, our findings suggest that a key component ought to be the strength and quality of the personal relationships of patients with heart disease.
The datasets generated for this study are available on request to the corresponding author.
The studies involving human participants were reviewed and approved by the Ottawa Health Science Network Research Ethics Board. The patients/participants provided their written informed consent to participate in this study.
All authors contributed to the writing and conceptualization of the manuscript. AH and HT completed the statistical analyses.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
CABG, coronary artery bypass grafting; CFI, Comparative Fit Index; CR, cardiac rehabilitation; CVD, cardiovascular disease; ECR-R, Experiences in Close Relationships – Revised; HADS, Hospital Anxiety and Depression Scale; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; ICD, implantable cardioverter defibrillator; IES-R, Impact of Event Scale – Revised; IL-6, cytokine interleukin 6; MANOVA, multivariate analysis of variance; MCAR, Missing Completely at Random; PCI, percutaneous coronary intervention; PTSD, posttraumatic stress disorder; RMSEA, root mean square error of approximation; SEM, structural equation modeling; SF-36, 36-Item Short Form Survey; UOHI, University of Ottawa Heart Institute.
Ainsworth, M. D. S., and Bell, S. M. (1970). Attachment, exploration, and separation: illustrated by the behavior of one-year-olds in a strange situation. Child Dev. 41, 49–67.
Alonso, Y., Fernández, J., Fontanil, Y., Ezama, E., and Gimeno, A. (2018). Contextual determinants of psychopathology. The singularity of attachment as a predictor of mental dysfunction. Psychiatry Res. 261, 338–343. doi: 10.1016/j.psychres.2018.01.010
Balint, E. M., Gander, M., Pokorny, D., Funk, A., Waller, C., and Buchheim, A. (2016). High prevalence of insecure attachment in patients with primary hypertension. Front. Psychol. 7:1087. doi: 10.3389/fpsyg.2016.01087
Barazzone, N., Santos, I., McGowan, J., and Donaghay-Spire, E. (2019). The links between adult attachment and post-traumatic stress: a systematic review. Psychol. Psychother. 92, 131–147. doi: 10.1111/papt.12181
Barger, S. D. (2013). Social integration, social support and mortality in the US national health interview survey. Psychosom. Med. 75, 510–517. doi: 10.1097/PSY.0b013e318292ad99
Bartholomew, K., and Horowitz, L. M. (1991). Attachment styles among young adults: a test of a four-category model. J. Pers. Soc. Psychol. 61, 226–244. doi: 10.1037/0022-3514.61.2.226
Bedi, U. S., and Arora, R. (2007). Cardiovascular manifestations of posttraumatic stress disorder. J. Natl. Med. Assoc. 99, 642–649.
Bjelland, I., Dahl, A. A., Haug, T. T., and Neckelmann, D. (2002). The validity of the hospital anxiety and depression scale: an updated literature review. J. Psychosom. Res. 52, 69–77.
Blumenthal, J. A., Sherwood, A., Smith, P. J., Watkins, L., Mabe, S., Kraus, W. E., et al. (2016). Enhancing cardiac rehabilitation with stress management training: a randomized, clinical efficacy trial. Circulation 133, 1341–1350. doi: 10.1161/CIRCULATIONAHA.115.018926
Boehm, J. K., and Kubzansky, L. D. (2012). The heart’s content: the association between positive psychological well-being and cardiovascular health. Psychol. Bull. 138, 655–691. doi: 10.1037/a0027448
Bohachick, P., Taylor, M. V., Sereika, S., Reeder, S., and Anton, B. B. (2002). Social support, personal control, and psychosocial recovery following heart transplantation. Clin. Nurs. Res. 11, 34–51. doi: 10.1177/105477380201100104
Boscarino, J. A. (2008). A prospective study of PTSD and early-age heart disease mortality among Vietnam veterans: implications for surveillance and prevention. Psychosom. Med. 70, 668–676. doi: 10.1097/PSY.0b013e31817bccaf
Bourassa, K. J., Ruiz, J. M., and Sbarra, D. A. (2019). The impact of physical proximity and attachment working models on cardiovascular reactivity: comparing mental activation and romantic partner presence. Psychophysiology 56:e13324. doi: 10.1111/psyp.13324
Bowlby, J. (1980). Attachment and Loss. Separation, Anxiety and Anger, Vol. II. New York, NY: Basic Books.
Bowlby, J. (2005). A Secure Base: Clinical Applications of Attachment Theory. London: Taylor & Francis.
Boxley, L., Flaherty, J. M., Spencer, R. J., Drag, L. L., Pangilinan, P. H., and Bieliauskas, L. A. (2016). Reliability and factor structure of the hospital anxiety and depression scale in a polytrauma clinic. J. Rehabil. Res. Dev. 53, 873–880. doi: 10.1682/JRRD.2015.05.0088
Bryant, R. A., and Hutanamon, T. (2018). Activating attachments enhances heart rate variability. PLoS One 13:e0151747. doi: 10.1371/journal.pone.0151747
Bunevicius, A. (2017). Reliability and validity of the SF-36 Health Survey Questionnaire in patients with brain tumors: a cross-sectional study. Health Qual. Life Outcomes 15:92. doi: 10.1186/s12955-017-0665-1
Bunevicius, A., Staniute, M., Brozaitiene, J., Pop, V. J. M., Neverauskas, J., and Bunevicius, R. (2013). Screening for anxiety disorders in patients with coronary artery disease. Health Qual. Life Outcomes 11:37. doi: 10.1186/1477-7525-11-37
Cavalot, F., Petrelli, A., Traversa, M., Bonomo, K., Fiora, E., Conti, M., et al. (2006). Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study. J. Clin. Endocrinol. Metab. 91, 813–819. doi: 10.1210/jc.2005-1005
Cerhan, J. R., and Wallace, R. B. (1997). Change in social ties and subsequent mortality in rural elders. Epidemiology 8, 475–481.
Clark, A. A., and Owens, G. P. (2012). Attachment, personality characteristics, and posttraumatic stress disorder in U.S. Veterans of Iraq and Afghanistan. J. Trauma. Stress 25, 657–664. doi: 10.1002/jts.21760
Coughlin, S. S. (2011). Post-traumatic stress disorder and cardiovascular disease. Open Cardiovasc. Med. J. 5, 164–170. doi: 10.2174/1874192401105010164
Edmondson, D., and Cohen, B. E. (2013). Posttraumatic stress disorder and cardiovascular disease. Prog. Cardiovasc. Dis. 55, 548–556. doi: 10.1016/j.pcad.2013.03.004
Edmondson, D., Richardson, S., Falzon, L., Davidson, K. W., Mills, M. A., and Neria, Y. (2012). Posttraumatic stress disorder prevalence and risk of recurrence in acute coronary syndrome patients: a meta-analytic review. PLoS One 7:e38915. doi: 10.1371/journal.pone.0038915
Edmondson, D., Rieckmann, N., Shaffer, J. A., Schwartz, J. E., Burg, M. M., Davidson, K. W., et al. (2011). Posttraumatic stress due to an acute coronary syndrome increases risk of 42-month major adverse cardiac events and all-cause mortality. J. Psychiatr. Res. 45, 1621–1626. doi: 10.1016/j.jpsychires.2011.07.004
Ehrlich, K. B. (2019). Attachment and psychoneuroimmunology. Curr. Opin. Psychol. 25, 96–100. doi: 10.1016/j.copsyc.2018.03.012
Eslami, B. (2017). Correlates of posttraumatic stress disorder in adults with congenital heart disease. Congenit. Heart Dis. 12, 357–363. doi: 10.1111/chd.12452
Fantini-Hauwel, C., Boudoukha, A. H., and Arciszewski, T. (2012). Adult attachment and emotional awareness impairment: a multimethod assessment. Socioaffect. Neurosci. Psychol. 2:10744. doi: 10.3402/snp.v2i0.10744
Faul, F., Erdfelder, E., Lang, A. G., and Buchner, A. (2007). G∗Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 39, 175–191. doi: 10.3758/bf03193146
Fraley, R. C., Waller, N. G., and Brennan, K. A. (2000). An item response theory analysis of self-report measures of adult attachment. J. Pers. Soc. Psychol. 78, 350–365. doi: 10.1037/0022-3514.78.2.350
Frasure-Smith, N., and Lespérance, F. (2008). Depression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery disease. Arch. Gen. Psychiatry 65, 62–71. doi: 10.1001/archgenpsychiatry.2007.4
Gallo, L. C., and Matthews, K. A. (2006). Adolescents attachment orientation influences ambulatory blood pressure responses to everyday social interactions. Psychosom. Med. 68, 253–261. doi: 10.1097/01.psy.0000204633.33599.81
Gander, M., and Buchheim, A. (2015). Attachment classification, psychophysiology and frontal EEG asymmetry across the lifespan: a review. Front. Hum. Neurosci. 9:79. doi: 10.3389/fnhum.2015.00079
Ginzburg, K., Kutz, I., Koifman, B., Roth, A., Kriwisky, M., David, D., et al. (2016). Acute stress disorder symptoms predict all-cause mortality among myocardial infarction patients: a 15-year longitudinal study. Ann. Behav. Med. 50, 177–186. doi: 10.1007/s12160-015-9744-x
Government of Canada (2019). Canadian Chronic Disease Surveillance System. Available at: https://health-infobase.canada.ca/ccdss/data-tool/ (accessed December 23, 2019).
Guay, S., Billette, V., and Marchand, A. (2006). Exploring the links between posttraumatic stress disorder and social support: processes and potential research avenues. J. Trauma. Stress 19, 327–338. doi: 10.1002/jts.20124
Hendrickson, C. M., Neylan, T. C., Na, B., Regan, M., Zhang, Q., and Cohen, B. E. (2013). Lifetime trauma exposure and prospective cardiovascular events and all-cause mortality: findings from the heart and soul study. Psychosom. Med. 75, 849–855. doi: 10.1097/PSY.0b013e3182a88846
Holt-Lunstad, J., Smith, T. B., and Layton, J. B. (2010). Social relationships and mortality risk: a meta-analytic review. PLoS Med. 7:e1000316. doi: 10.1371/journal.pmed.1000316
Hooper, D., Coughlan, J., and Mullen, M. R. (2008). Structural equation modelling: guidelines for determining model fit. Electron. J. Bus. Res. Methods 6, 53–60. doi: 10.1016/j.acap.2015.07.001
Horowitz, M., Wilner, N., and Alvarez, W. (1979). Impact of Event Scale: a measure of subjective stress. Psychosom. Med. 41, 209–218. doi: 10.1097/00006842-197905000-00004
Huang, Y.-C., Lee, Y., Lin, P.-Y., Hung, C.-F., Lee, C.-Y., and Wang, L.-J. (2019). Anxiety comorbidities in patients with major depressive disorder: the role of attachment. Int. J. Psychiatry Clin. Pract. 23, 286–292. doi: 10.1080/13651501.2019.1638941
Johnson, S. M. (2019). Attachment Theory in Practice: Emotionally Focused Therapy (EFT) with Individuals, Couples, and Families. New York, NY: Guilford Publications.
Johnson, S. M. (2020). The Practice of Emotionally Focused Couple Therapy: Creating Connection, 3rd Edn. Philadelphia, PA: Brunner-Routledge.
Kerr, S. L., Melley, A. M., Travea, L., and Pole, M. (2003). The relationship of emotional expression and experience to adult attachment style. Individ. Differ. Res. 1, 108–123.
Kidd, T., Poole, L., Leigh, E., Ronaldson, A., Jahangiri, M., and Steptoe, A. (2014). Attachment anxiety predicts IL-6 and length of hospital stay in coronary artery bypass graft surgery (CABG) patients. J. Psychosom. Res. 77, 155–157. doi: 10.1016/j.jpsychores.2014.06.002
Kline, R. B. (2011). Principles and Practice of Structural Equation Modeling, 3rd Edn. New York, NY: Guilford Press.
Kubzansky, L. D., Koenen, K. C., Jones, C., and Eaton, W. W. (2009). A prospective study of posttraumatic stress disorder symptoms and coronary heart disease in women. Health Psychol. 28, 125–130. doi: 10.1037/0278-6133.28.1.125
Kubzansky, L. D., Koenen, K. C., Spiro, A., Vokonas, P. S., and Sparrow, D. (2007). Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the normative aging study. Arch. Gen. Psychiatry 64, 109–116.
Lee, D. C., Sui, X., Church, T. S., Lavie, C. J., Jackson, A. S., and Blair, S. N. (2012). Changes in fitness and fatness on the development of cardiovascular disease risk factors: hypertension, metabolic syndrome, and hypercholesterolemia. J. Am. Coll. Cardiol. 59, 665–672. doi: 10.1016/j.jacc.2011.11.013
Lemay, K. R., Tulloch, H. E., Pipe, A. L., and Reed, J. L. (2019). Establishing the minimal clinically important difference for the hospital anxiety and depression scale in patients with cardiovascular disease. J. Cardiopulm. Rehabil. Prev. 39, E6–E11. doi: 10.1097/HCR.0000000000000379
Lemieux, I., Lamarche, B., Couillard, C., Pascot, A., Cantin, B., Bergeron, J., et al. (2001). Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men. Arch. Intern. Med. 161, 2685–2692.
Lichtman, J. H., Bigger, J. T., Blumenthal, J. A., Frasure-Smith, N., Kaufmann, P. G., Lesperance, F., et al. (2008). Depression and coronary heart disease. Circulation 118, 1768–1775.
Luecken, L. J. (1998). Childhood attachment and loss experiences affect adult cardiovascular and cortisol function. Psychosom. Med. 60, 765–772. doi: 10.1097/00006842-199811000-00021
Manninen, V., Tenkanen, L., Koskinen, P., Huttunen, J. K., Mänttäri, M., Heinonen, O. P., et al. (1992). Joint effects of serum triglyceride and LDL cholesterol and HDL cholesterol concentrations on coronary heart disease risk in the Helsinki Heart Study. Implications for treatment. Circulation 85, 37–45. doi: 10.1161/01.cir.85.1.37
Maunder, R. G., and Hunter, J. J. (2001). Attachment and psychosomatic medicine: developmental contributions to stress and disease. Psychosom. Med. 63, 556–567. doi: 10.1097/00006842-200107000-00006
McWilliams, L. A., and Bailey, S. J. (2010). Associations between adult attachment ratings and health conditions: evidence from the national comorbidity survey replication. Health Psychol. 29, 446–453. doi: 10.1037/a0020061
Mikulincer, M., Shaver, P. R., and Horesh, N. (2007). “Attachment bases of emotion regulation and posttraumatic adjustment,” in Emotion Regulation in Couples and Families: Pathways to Dysfunction and Health, eds D. K. Snyder, J. Simpson, and J. N. Hughes, (Washington, DC: American Psychological Association), 77–99. doi: 10.1037/11468-004
Mikulincer, M., Shaver, P. R., and Solomon, Z. (2015). “An attachment perspective on traumatic and posttraumatic reactions,” in Future Directions in Post-Traumatic Stress Disorder, eds M. P. Safir, H. S. Wallach, and A. S. Rizzo, (Berlin: Springer Science+Business Media), 76–96.
Mozaffarian, D., Benjamin, E. J., Go, A. S., Arnett, D. K., Blaha, M. J., Cushman, M., et al. (2015). Heart disease and stroke statistics–2015 update: a report from the American heart association. Circulation 131, e29–e322.
Muller-Nordhorn, J. (2004). Comparison of the short form (SF)-12 health status instrument with the SF-36 in patients with coronary heart disease. Heart 90, 523–527. doi: 10.1136/hrt.2003.013995
Oladi, F., and Dargahi, M. (2018). The comparison of attachment styles in people with and without coronary artery disease. J. Res. Med. Sci. 20:e60106.
Peleg, S., Vilchinsky, N., Fisher, W. A., Khaskia, A., and Mosseri, M. (2017). Personality makes a difference: attachment orientation moderates theory of planned behavior prediction of cardiac medication adherence. J. Pers. 85, 867–879. doi: 10.1111/jopy.12294
Perk, J., De Backer, G., Gohlke, H., Graham, I., Reiner, Ž., Verschuren, M., et al. (2012). European guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur. Heart J. 33, 1635–1701.
Pierrehumbert, B., Torrisi, R., Ansermet, F., Borghini, A., and Halfon, O. (2012). Adult attachment representations predict cortisol and oxytocin responses to stress. Attach. Hum. Dev. 14, 453–476. doi: 10.1080/14616734.2012.706394
Pietromonaco, P. R., and Collins, N. L. (2017). Interpersonal mechanisms linking close relationships to health. Am. Psychol. 72, 531–542. doi: 10.1037/amp0000129
Pietromonaco, P. R., Uchino, B., and Dunkel Schetter, C. (2013). Close relationship processes and health: implications of attachment theory for health and disease. Health Psychol. 32, 499–513. doi: 10.1037/a0029349
Quirin, M., Pruessner, J. C., and Kuhl, J. (2008). HPA system regulation and adult attachment anxiety: individual differences in reactive and awakening cortisol. Psychoneuroendocrinology 33, 581–590. doi: 10.1016/j.psyneuen.2008.01.013
Rash, C. J., Coffey, S. F., Baschnagel, J. S., Drobes, D. J., and Saladin, M. E. (2008). Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict. Behav. 33, 1039–1047. doi: 10.1016/j.addbeh.2008.04.006
Reiss, A. B., Siegart, N. M., and De Leon, J. (2017). Interleukin-6 in atherosclerosis: atherogenic or atheroprotective? Clin. Lipidol. 12, 14–23.
Richards, S. H., Anderson, L., Jenkinson, C. E., Whalley, B., Rees, K., Davies, P., et al. (2018). Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Eur. J. Prev. Cardiol. 25, 247–259. doi: 10.1177/2047487317739978
Rothenbacher, D., Hahmann, H., Wüsten, B., Koenig, W., and Brenner, H. (2007). Symptoms of anxiety and depression in patients with stable coronary heart disease: prognostic value and consideration of pathogenetic links. Eur. J. Cardiovasc. Prev. Rehabil. 14, 547–554. doi: 10.1097/hjr.0b013e3280142a02
Rubin, D. B. (1996). Multiple imputation after 18+ years. J. Am. Stat. Assoc. 91, 473–489. doi: 10.1080/01621459.1996.10476908
Sibley, C. G., Fischer, R., and Liu, J. H. (2005). Reliability and validity of the revised Experiences in Close Relationships (ECR-R) self-report measure of adult romantic attachment. Pers. Soc. Psychol. Bull. 31, 1524–1536. doi: 10.1177/0146167205276865
Simpson, J. A., and Rholes, W. S. (2017). Adult attachment, stress, and romantic relationships. Curr. Opin. Psychol. 13, 19–24. doi: 10.1016/j.copsyc.2016.04.006
Singer, S., Kuhnt, S., Götze, H., Hauss, J., Hinz, A., Liebmann, A., et al. (2009). Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br. J. Cancer 100, 908–912. doi: 10.1038/sj.bjc.6604952
Spindler, H., and Pedersen, S. S. (2005). Posttraumatic stress disorder in the wake of heart disease: prevalence, risk factors, and future research directions. Psychosom. Med. 67, 715–723. doi: 10.1097/01.psy.0000174995.96183.9b
Stanley, I. H., Hom, M. A., Chu, C., Dougherty, S. P., Gallyer, A. J., Spencer-Thomas, S., et al. (2018). Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: a multistudy investigation. Psychol. Serv. 16, 543–555. doi: 10.1037/ser0000240
Stovall-McClough, K. C., and Dozier, M. (2016). “Attachment states of mind and psychopathology in adulthood,” in Handbook of Attachment: Theory, Research, and Clinical Applications, 3rd Edn, eds J. Cassidy and P. R. Shaver, (New York, NY: The Guilford Press), 715–738.
Tabachnick, B. G., and Fidell, L. S. (2007). Using Multivariate Statistics. Using Multivariate Statistics, 5th Edn. New York, NY: Pearson.
The Emerging Risk Factors Collaboration (2010). Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet 375, 2215–2222. doi: 10.1016/S0140-6736(10)60484-9
Tiller, S., Leger-Caldwell, L., O’Farrell, P., Pipe, A. L., and Mark, A. E. (2013). Cardiac rehabilitation: beginning at the bedside. J. Cardiopulm. Rehabil. Prev. 33, 180–184. doi: 10.1097/HCR.0b013e31827e14da
Trogdon, J. G., Finkelstein, E. A., Nwaise, I. A., Tangka, F. K., and Orenstein, D. (2007). The economic burden of chronic cardiovascular disease for major insurers. Health Promot. Pract. 8, 234–242. doi: 10.1177/1524839907303794
Tulloch, H. E., Greenman, P., Demidenko, N., and Johnson, S. M. (2017). Healing Hearts Together Relationship Education Program: Facilitators Guide for Small Groups. Ottawa, ON: International Centre for Excellence in Emotionally Focused Therapy.
Tulloch, H. E., Heenan, A., Cupper, L., Pelletier, R., O’Farrell, P., and Pipe, A. (2018). Depression and anxiety screening and triage protocol for cardiac rehabilitation programs. J. Cardiopulm. Rehabil. Prev. 38, 159–162. doi: 10.1097/HCR.0000000000000276
Tulloch, H. E., Johnson, S., Greenman, P., Demidenko, N., and Clyde, M. (2016). “Healing hearts together: a pilot intervention program for cardiac patients and their partners,” in Proceedings of the Canadian Association of Cardiac Prevention and Rehabilitation, Montreal.
Vilchinsky, N., Ginzburg, K., Fait, K., and Foa, E. B. (2017). Cardiac-disease-induced PTSD (CDI-PTSD): a systematic review. Clin. Psychol. Rev. 55, 92–106. doi: 10.1016/j.cpr.2017.04.009
Vilchinsky, N., Haze-Filderman, L., Leibowitz, M., Reges, O., Khaskia, A., and Mosseri, M. (2010). Spousal support and cardiac patients’ distress: the moderating role of attachment orientation. J. Family Psychol. 24, 508–512. doi: 10.1037/a0020009
Ware, J. E. J., and Sherbourne, C. D. (1992). The MOS 36-ltem short-form health survey (SF-36): I. conceptual framework and item selection. Med. Care 30, 473–483. doi: 10.1097/00005650-199206000-00002
West, M., Sarah Rose, M., and Brewis, C. S. (1995). Anxious attachment and psychological distress in cardiac rehabilitation patients. J. Clin. Psychol. Med. Settings 2, 167–178. doi: 10.1007/BF01988641
Whalley, B., Thompson, D. R., and Taylor, R. S. (2014). Psychological interventions for coronary heart disease: Cochrane systematic review and meta-analysis. Int. J. Behav. Med. 21, 109–121. doi: 10.1007/s12529-012-9282-x
Whitehead, D. L., Perkins-Porras, L., Strike, P. C., and Steptoe, A. (2006). Post-traumatic stress disorder in patients with cardiac disease: predicting vulnerability from emotional responses during admission for acute coronary syndromes. Heart 92, 1225–1229. doi: 10.1136/hrt.2005.070946
Wikman, A., Bhattacharyya, M., Perkins-Porras, L., and Steptoe, A. (2008). Persistence of posttraumatic stress symptoms 12 and 36 months after acute coronary syndrome. Psychosom. Med. 70, 764–772. doi: 10.1097/PSY.0b013e3181835c07
Williams, E. D., and Steptoe, A. (2007). The role of depression in the etiology of acute coronary syndrome. Curr. Psychiatry Rep. 9, 486–492. doi: 10.1007/s11920-007-0066-y
Woodhouse, S., Ayers, S., and Field, A. P. (2015). The relationship between adult attachment style and post-traumatic stress symptoms: a meta-analysis. J. Anxiety Disord. 35, 103–117. doi: 10.1016/j.janxdis.2015.07.002
Yalom, I. D. (1995). The Theory and Practice of Group Psychotherapy. New York, NY: Basic Books (AZ).
Yazdanyar, A., and Newman, A. B. (2009). The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin. Geriatr. Med. 25, 563–577. doi: 10.1016/j.cger.2009.07.007
Keywords: cardiovascular disease, attachment anxiety, traumatic stress, health outcomes, attachment avoidance
Citation: Heenan A, Greenman PS, Tassé V, Zachariades F and Tulloch H (2020) Traumatic Stress, Attachment Style, and Health Outcomes in Cardiac Rehabilitation Patients. Front. Psychol. 11:75. doi: 10.3389/fpsyg.2020.00075
Received: 23 October 2019; Accepted: 10 January 2020;
Published: 28 January 2020.
Edited by:
Noa Vilchinsky, Bar-Ilan University, IsraelReviewed by:
Sivan George Levi, Peres Academic Center, IsraelCopyright © 2020 Heenan, Greenman, Tassé, Zachariades and Tulloch. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Heather Tulloch, aGV0dWxsb2NoQG90dGF3YWhlYXJ0LmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.