
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 11 December 2019
Sec. Health Psychology
Volume 10 - 2019 | https://doi.org/10.3389/fpsyg.2019.02775
This article is part of the Research TopicExperimental Approaches to Body Image, Representation and PerceptionView all 24 articles
This study conducted a cross-sectional investigation of facial appearance dissatisfaction between patients before undergoing orthognathic surgery and a non-surgical sample to evaluate the potential influencing factors of facial appearance dissatisfaction. A sample of 354 participants completed a set of questionnaires concerning facial appearance dissatisfaction, interpersonal pressure, media pressure, and fear of negative appearance evaluation (112 patients, 242 controls). The patients reported higher facial appearance dissatisfaction, more media pressure, more interpersonal pressure, and a greater fear of negative appearance evaluation among others than the control group. Moreover, regression analyses identified interpersonal pressure and fear of negative appearance evaluation as the main predictors of facial appearance dissatisfaction whether in the orthognathic patients or the control groups. The associations between the perceptions of interpersonal pressure, fear of negative appearance evaluation, and facial appearance dissatisfaction support the possible utility of strengthening social experiences and psychological intervention in preventing and treating these appearance-concerns, especially for the orthognathic patients.
Individuals’ satisfaction with their appearance is of central importance to their psychological well-being and health. Previous research has demonstrated negative associations between appearance satisfaction and depression, social avoidance, and low quality of life, both within the general population (Wilson et al., 2013; Griffiths et al., 2017) and among clinical samples with dentofacial deformities who are thought to be particularly vulnerable to dissatisfaction with their facial appearance (Frejman et al., 2013; Feragen and Stock, 2016, 2017). Epidemiological surveys show that about 40% of the population has malocclusion, about 5% of which is due to abnormal skeletal malformation caused by abnormal jaw development, i.e., dentofacial deformity (Qiu, 2008). Dentofacial deformities are changes or irregularities that primarily affect the jaws and teeth. However, multiple craniofacial structures may also be affected (Ong, 2004). In most cases, they are the result of moderate or severe genetic distortions that occurred during the normal development process (such as mandibular prognathism, bimaxillary prognathism or retrognathism, and maxillary vertical excess) and can be corrected using an integrated treatment of orthodontics and orthognathic surgery in adults (Leite et al., 2004).
Facial attractiveness is highly valued in modern society and plays a central role in social activities, such as choosing a partner (Morgan and Kisley, 2014). However, dentofacial deformities cause facial attractiveness to deviate from the sociocultural norms of beauty and attractiveness. This often causes people with dentofacial deformities to feel that they are different from their peers in terms of facial appearance and to suffer from facial appearance dissatisfaction, which may lead to other psychosocial problems such as feelings of hopelessness, interpersonal problems, and low self-esteem (Cadogan and Bennun, 2011; Alanko et al., 2014; Gomes et al., 2019). It has been reported that orthognathic patients have a better personal facial appearance evaluation after orthognathic surgery than before, and their social functioning and self-confidence have improved. These patients also exhibit positive life changes and reduced anxiety (Soh and Narayanan, 2014; Al-Asfour et al., 2018). Although satisfaction with orthognathic treatment is generally high, a small but important group of patients is dissatisfied with the outcome, often despite technically good results (Lee et al., 2007; Ryan et al., 2012). This phenomenon may be caused by psychological factors. Therefore, it is important to investigate psychological factors that may affect patients’ satisfaction with treatment outcomes before offering orthognathic surgery treatment. Therefore, knowledge concerning the specific factors thought to affect the development of subjective facial appearance evaluations among orthognathic patients is essential.
Mass media represents a powerful source of perceived societal values and standards, especially concerning “ideal beauty,” weight, food, and fashion (Levine and Harrison, 2009). An experimental study by Newton and Minhas (2005) demonstrated that female orthognathic patients display more dissatisfaction with their facial appearance after viewing idealized images of facial photographs than females who were not orthognathic patients. Some studies have illustrated that patients with dentofacial deformities perceived social pressure which is created by the media and its representation of “ideal beauty,” but none of these studies have specifically addressed the impact of this pressure on the facial appearance satisfaction of orthognathic patients. Moreover, in the research field of body dissatisfaction, a large number of studies have shown that perceived media pressure can exacerbate an individual’s body dissatisfaction (Robinson et al., 2017; Want and Saiphoo, 2017). Therefore, it is important to discover what the impact of perceived mass media pressure on orthognathic patients’ facial appearance dissatisfaction is.
In addition to mass media, researchers have theorized that messages about appearance-related standards of beauty can also be transmitted by modeling and appearance-related feedback from family members, friends, and romantic partners (Schaefer and Salafia, 2014; Girard et al., 2018). In the field of body dissatisfaction, these messages are often transmitted covertly (e.g., a mother may project a certain message to her daughter about body weight and shape through her dieting habits) or overtly (e.g., a sibling calling their sibling “fat”). Both these messages increase interpersonal pressure for individuals to change their appearance (Chng and Fassnacht, 2016; Thogersen-Ntoumani et al., 2016). This illustrates how weight-related pressure and criticism serves to promote adherence to societal norms concerning weight and shape, further contributing to the individual’s body dissatisfaction. Similarly, associations between interpersonal experiences and subjective appearance evaluations have been described in numerous cross-sectional and quantitative studies within the cleft lip and/or palate (CL/P) literature (Berger and Dalton, 2011; Searle et al., 2017). However, there are no studies comparing the perceived interpersonal pressure regarding facial appearance for people with and without dentofacial deformities. It is reasonable to speculate that due to their unusual facial appearance, orthognathic patients will perceive more interpersonal pressure than those without dentofacial deformities. Furthermore, interpersonal pressure can predict one’s facial appearance dissatisfaction.
Generally, fear of negative evaluation (FNE) can be understood as a type of social anxiety or apprehension about being negatively judged by others and avoidance of situations in which these negative evaluations may occur (Watson and Friend, 1969). Few studies have found a negative correlation between FNE and satisfaction with the appearance in adults with a congenital craniofacial anomaly. Adults with a congenital craniofacial anomaly were more dissatisfied with their facial appearance when they reported an increased FNE (Versnel et al., 2010; Roberts and Mathias, 2013). Importantly, fear of negative appearance evaluation, a domain-specific FNE—which is defined as social anxiety and distress based on having one’s appearance negatively evaluated (Hart et al., 2008)—may also be associated with facial appearance dissatisfaction. Claes et al. (2012) found that fear of negative appearance evaluation was positively correlated with body dissatisfaction in women diagnosed with an eating disorder. Besides, Levinson and Rodebaugh (2012) found that fear of negative appearance evaluation could predict an individual’s body dissatisfaction. However, no research has yet focused on the impact of fear of negative appearance evaluation on facial appearance dissatisfaction.
In summary, psychological factors may play an important role in orthognathic patients’ perception of their facial appearance. According to previous studies on body dissatisfaction, media pressure, interpersonal pressure, and fear of negative appearance evaluation may be the three psychological factors most likely to affect the facial appearance dissatisfaction of clinical patients with dentofacial deformities. However, the first limitation of current research is that no study has focused on the differences between orthognathic patients and a non-surgical sample without dentofacial deformities in facial appearance dissatisfaction, media pressure, interpersonal pressure, and fear of negative appearance evaluation. Moreover, there is limited research that has focused on the role of psychological influences on individuals’ perception of facial appearance to seek better psychological interventions for improving orthognathic patients’ satisfaction with orthognathic surgery treatment outcomes. The current study thus aimed to compare orthognathic patients (patients before undergoing orthognathic surgery) and a non-surgical sample (the controls) in the levels of facial appearance dissatisfaction, appearance pressure from interpersonal relationships and mass media, and negative appearance evaluation fears, as well as to investigate the predictors of facial appearance dissatisfaction among the two groups. In line with previous findings, we hypothesized that (1) the patients would have a higher level of facial appearance dissatisfaction than the controls. Furthermore, relative to the control sample, patients were expected to report more appearance pressure from interpersonal relationships and mass media, and greater negative appearance evaluation fears. We also hypothesized that (2) among the patients and control groups, media pressure, interpersonal pressure, and fear of negative appearance evaluation would be predictors of facial appearance dissatisfaction, and the predictive effect was more significant in patients’ facial appearance dissatisfaction.
The initial sample consisted of 381 participants (136 patients and 245 controls). Twenty-seven participants (7.09%) were excluded from the sample for being younger than 18 years of age. The final sample consisted of 354 participants [patients: 112 (31.64%), controls: 242 (68.36%)], ranging from 18 to 35 years of age (M = 20.78 years, SD = 3.04 years). The patient sample included 112 individuals (females: 76 males: 36) and their ages ranged from 18 to 35 (M = 22.79 years, SD = 4.20 years). The patients’ inclusion criteria were: adult patients (more than 18 years old), the presence of skeletal deformity affecting patients’ appearance, is scheduled to undergo orthognathic surgery. The patients’ exclusion criteria were: trauma or previous orthognathic surgery, syndromic patients, cleft lip and palate patients, distraction osteogenesis cases, and patients who had undergone isolated genioplasty procedures. The control group consisted of 242 college students (females: 163, males: 79) who did not have any facial skeletal discrepancies. Additionally, these individuals were not orthodontic patients. Their ages ranged from 18 to 27 years (M = 19.85, SD = 1.63). All the participants were from mainland China. Similar to the ethnic group composition of the general population, the great majority of the participants (80.20%) was Han (national minorities: 19.80%). There were no gender differences between the patients and controls, χ2 (1) = 0.01, p = 0.93. Furthermore, there was a significant difference in age between the two groups; t(155) = 7.14, p < 0.001.
This study was approved by the ethics committee for human research at Southwest University. A doctor’s assistant from the Stomatological Hospital of Chongqing Medical University was instructed thoroughly concerning the study and contacted the orthognathic patients from the Stomatological Hospital of Chongqing Medical University. The patients would receive a survey packet that included a brief research overview, an informed consent agreement, and self-report measures described below. The patients were asked to complete a set of questionnaires carefully. The patient completed the questionnaire 2 days before the surgery. The controls were college students from Zunyi Medical College who did not undergo orthognathic surgery, completed the questionnaires in school hours. This study was carried out from December 2015 to February 2017.
All measures and questionnaires of this study were in Chinese. Several scales (the Sociocultural Attitudes Toward Appearance Scale-3, the Perceived Sociocultural Pressure Scale, and Fear of Negative Appearance Evaluation) were translated into Chinese and back-translated into English in previously published works (e.g., Jackson and Chen, 2010, 2011; Chen and Jackson, 2012). The Negative Physical Self-Face Scale has had a Chinese vision (see Chen et al., 2006).
Participants were asked to provide their age, gender, income levels, relationship status, and nation information.
Facial appearance dissatisfaction was assessed using the Facial Appearance Concern subscale of the Negative Physical Self Scale (NPSS; Chinese version: Chen et al., 2006; Chen and Jackson, 2007). The Facial Appearance Concern subscale consists of 11 items and is comprised of three sub-dimensions: cognition-affect (e.g., “I am depressed about how my face looks”), behavior (e.g., “If it is possible, I will change the way my face looks”), and projection (e.g., “People around me do not like the way my face looks”). All items were rated on a 5-point scale ranging from 0 (never) to 4 (always). Items were averaged to form a total score, with higher scores indicating more facial appearance dissatisfaction. The Facial Appearance Concern subscale has a stable factor structure as well as good reliability and validity among Chinese samples (Chen et al., 2006; Jackson and Chen, 2008; Wang et al., 2019). For the current study, the Cronbach’s alpha values were 0.91 among the patients and 0.90 among the controls.
Reported appearance pressure from mass media was calculated by adding the eight items from the Pressure subscale of the Sociocultural Attitudes Toward Appearance Scale-3 (SATAQ-3; Thompson et al., 2004; Chinese version: Chen and Jackson, 2012). Each statement was assessed on a Likert-type scale that ranged from 1 (totally disagree) to 5 (totally agree). An example item is “I have felt pressure from TV or magazines to change my appearance.” However, four items about thinness (e.g., “I have felt pressure from TV and magazines to be thin”) were removed, as they are not relevant to the research theme. The final score was calculated by the sum of the responses, with higher scores indicating more media pressure. The subscale has satisfactory reliability and validity in Chinese samples (Chen and Jackson, 2012). The Cronbach’s alpha values of the 4-item version of the subscale for the present study sample were 0.91 among patients and 0.81 among the controls.
Six items of the Perceived Sociocultural Pressure Scale-Interpersonal (PSPS-I; Stice and Agras, 1998; Chinese version: Jackson and Chen, 2008) were used to assess appearance pressure from friends (e.g., “I have felt pressure from my friends to change my physical appearance”), family (e.g., “I have felt pressure from my family to change my physical appearance”) and prospective romantic partner (“I have felt pressure from people that I am interested in dating to change my physical appearance”). Each item was rated from 1 (none) to 5 (a lot). For the Chinese samples, items have been modified slightly to reflect pressure to “change my physical appearance” or “have a certain physical appearance” rather than pressure to be thin (e.g., Jackson and Chen, 2008). Concerning the “romantic partner” items, these were changed to include the respondent’s “current romantic partner or people I would like to date” to increase applicability to all respondents, including those not currently dating. The final score was calculated by the sum of the responses, with higher scores indicating more interpersonal pressure. Chen and Jackson (2012) found all six interpersonal PSPS items loaded on one component in Chinese samples of each gender. The Cronbach’s alpha values for this variable were 0.86 for patients and 0.79 for the controls.
The six-item fear of negative appearance evaluation (FNAE, Lundgren et al., 2004; Chinese version: Jackson and Chen, 2011) assessed the frequency of concerns that others will judge one’s physical appearance negatively. Sample items included “I worry that people will find fault with the way I look” and “I am afraid other people will notice my physical flaws.” Each item was rated from 1 (never) to 5 (almost always true). The final score was calculated by the sum of the responses, with higher scores indicating a greater FNAE. The questionnaire showed good reliability for Chinese adolescents (Jackson and Chen, 2011). The Cronbach’s alpha values were 0.90 for patients and 0.84 for controls.
The statistical analyses were performed using SPSS 22. Descriptive analyses were conducted to obtain the ranges, means, and standard deviations of the two study groups (Table 1). Next, we performed a multivariate analysis of covariance (MANCOVA) controlling for age (covariates) between the patients and the controls for there was a significant difference in age between the two groups. To explore the relationships among facial appearance dissatisfaction, and risk factors (media pressure, interpersonal pressure, and fear of negative appearance evaluation), the correlations among the variables were initially examined in patients and controls separately by using a Pearson correlation (Table 2). We used a recommended guideline by Gignac and Szodorai (2016) for interpreting the magnitude of correlations (0.15 = small, 0.25 = medium, and 0.35 = large). Hierarchical multiple regression analyses were also conducted to determine the contribution of the variables of interest on facial appearance dissatisfaction, controlling the model with the age and gender of the patients and controls separately (Table 3). Multicollinearity was examined using tolerance and VIF statistics and found to be acceptable in all cases. Highest VIF values were 2.26, and lowest tolerance values were 0.44.
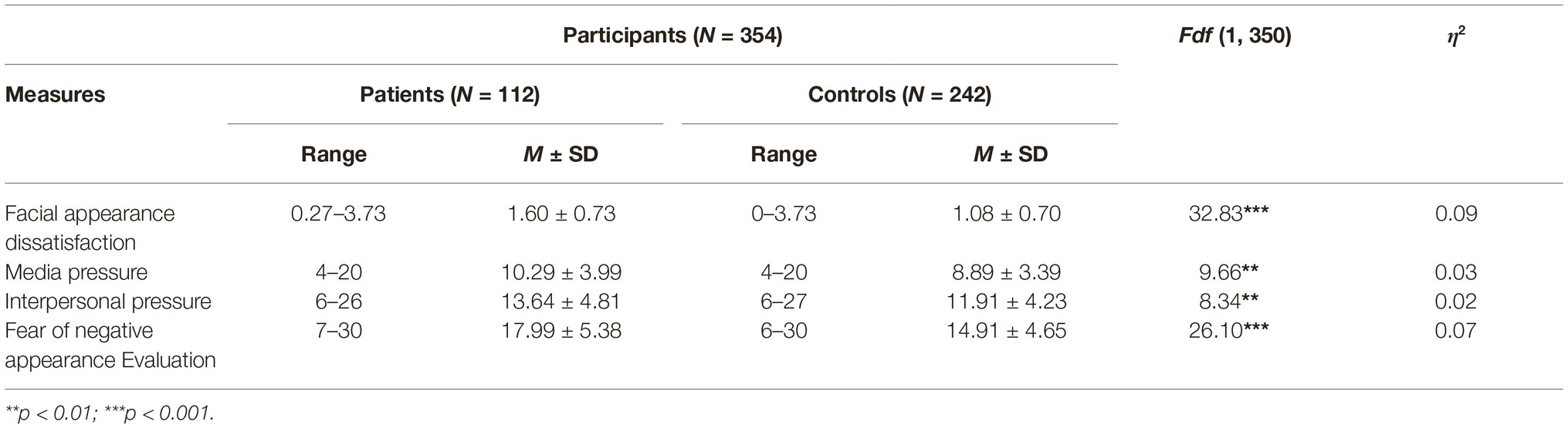
Table 1. Scale range, mean, and standard deviation (SD) for study variables among orthognathic patients and the control group.
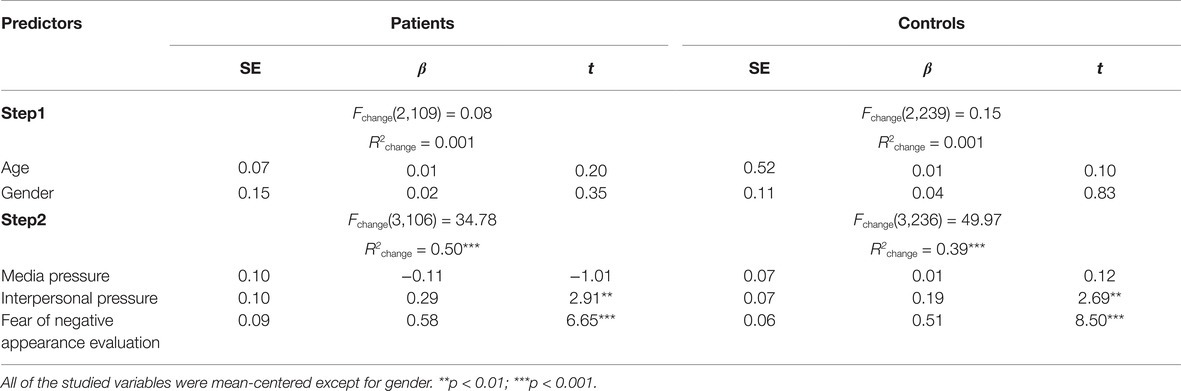
Table 3. Hierarchical multiple regression analyses of risk factors predicting facial appearance dissatisfaction for orthognathic patients and the control group.
Table 1 presents the scale range, mean values, and standard deviations (SD) of the study variables among the orthognathic patients and the control group.
In accordance with our first research question, the multivariate analysis of covariance revealed significant differences in the combined variables, F (4, 347) = 9.13, p < 0.001, η2 = 0.10; Pillai’s trace = 0.10. An examination of the univariate values of F indicated that compared to the control group, the patients reported higher facial appearance dissatisfaction, more media pressure, more interpersonal pressure, and a greater fear of negative appearance evaluation among others (Table 1).
The bivariate correlations among all the study variables for both samples are presented in Table 2. For both the patients and control groups, the pattern of correlations confirmed the expected relationships between the study variables. Furthermore, the findings concerning the bivariate correlations reveal that in both samples, facial appearance dissatisfaction has a strong association with media pressure (patients: r = 0.44, p < 0.01; controls: r = 0.39, p < 0.01), interpersonal pressure (patients: r = 0.52, p < 0.01; controls: r = 0.43, p < 0.01), and fear of negative appearance evaluation (patients: r = 0.67, p < 0.01; controls: r = 0.60, p < 0.01).
Starting with these significant associations, we conducted hierarchical multiple regression analyses with facial appearance dissatisfaction as a dependent variable (Table 3). We also proposed independent models for patients and the controls. Because previous analyses revealed age- and gender-related variations in body dissatisfaction (Menzel et al., 2010; Chng and Fassnacht, 2016), to exclude the influence of irrelevant variables in this study, we accounted for the baseline level of these demographic variables in the first step.
For the orthognathic patients, after the age and gender analyses, the predictors explained 50% of the variance in facial appearance dissatisfaction changes (Table 3). The significant predictors were interpersonal pressure (β = 0.29, p < 0.01) and fear of negative appearance evaluation (β = 0.58, p < 0.001). Moreover, fear of negative appearance evaluation was the strongest predictor of facial appearance dissatisfaction for orthognathic patients. In this model, media pressure had no significant influence (p > 0.05).
Concerning the control group, the hypothesized predictors accounted for 39% of the variance in facial appearance dissatisfaction changes after controlling for age and gender (Table 3). The significant predictors were interpersonal pressure (β = 0.19, p < 0.01) and fear of negative appearance evaluation (β = 0.51, p < 0.001). Moreover, fear of negative appearance evaluation was considered to be the strongest predictor of facial appearance dissatisfaction, with media pressure again having no significant effect (p > 0.05).
In light of our original research question, these results suggest that while for both groups the results of hierarchical multiple regression analyses are the same, the associations between interpersonal pressure and fear of negative appearance evaluation and facial appearance dissatisfaction are stronger in orthognathic patients than in the control group (see Table 3).
This study is the first to investigate the relationship between psychological factors and facial appearance dissatisfaction when considering orthognathic patients and a non-surgical sample group. First, we determined the differences between the two groups concerning facial appearance dissatisfaction, media pressure, interpersonal pressure, and fear of negative appearance evaluation. Second, the findings contribute to our knowledge of interpersonal pressure and fear of negative appearance evaluation and their relationships with facial appearance dissatisfaction for both orthognathic patients and the control group.
The findings revealed that the orthognathic patients felt more dissatisfied with their facial appearance than the comparison groups. This is consistent with earlier research on the topic which has found patients who pursue orthognathic surgery were more concerned about their dentofacial appearance and general body image compared with the individuals who did not have skeletal discrepancies (Sar et al., 2015). Furthermore, the patients perceived more media pressure, interpersonal pressure, and reported greater fear of negative appearance evaluation than the controls. These findings are consistent with the patients’ situation before orthognathic surgery. The patients feel that their dentofacial deformities make them look different from the peers and reduce their facial attractiveness, affecting many aspects of their lives, such as social interactions, their possible success when seeking employment, being chosen as a romantic partner, and not least, their personality and characteristics (Eslamipour et al., 2017). These differences between patients and the controls indicate that it is essential to investigate the risk factors concerning patients’ facial appearance dissatisfaction and the related psychosocial factors, rather than only investigating the biological influence.
The predictive effects of the risk factors concerning facial appearance dissatisfaction in patients and controls were examined separately and the findings partially answered our research question. Generally, the patients and the controls showed the same pattern of results.
For both groups, interpersonal pressure reliably predicted concerns regarding facial appearance, suggesting that interpersonal pressure may have a negative influence on an individual’s facial appearance satisfaction. This finding is consistent with similar research in body dissatisfaction literature, which presented that direct interpersonal influences can predict body dissatisfaction (Johnson et al., 2015). The interpersonal pressure may come from daily life communication overtly (e.g., appearance teasing from peers, parental comments regarding facial appearance) or covertly (e.g., parents worry that their children are disadvantaged in society because of facial appearance), and these pressures may profoundly affect the development and construction of individuals’ facial appearance dissatisfaction.
The expected relationship between fear of negative appearance evaluation and facial appearance dissatisfaction was confirmed for both patients and controls. The result showed that fear of negative appearance evaluation was the most predictive variable on facial appearance dissatisfaction, highlighting the centrality of this variable for facial appearance dissatisfaction. The observations in this study are consistent with that of Lundgren et al. (2004), who found that appearance evaluation fears predicted body image concerns. Similarly, Jackson and Chen (2011) found that fear of negative appearance evaluation was among the strongest predictors of changes in eating pathology for Chinese girls. Our results suggest that elevated fear of negative appearance evaluation may be a risk factor for the development of facial appearance dissatisfaction.
The lack of significance of the media in predicting facial appearance dissatisfaction among both patients and the non-surgical sample in this study is also of interest. There was a positive correlation between media pressure and facial appearance dissatisfaction for both groups. Contrary to our results, there is a substantial body of research that indicates that the media was the main source of influence on body dissatisfaction (Robinson et al., 2017; Want and Saiphoo, 2017). The sample size of orthognathic patients and non-clinical samples in this study is small, which may affect the statistical significance of media pressure. Another possible explanation is the difference in the findings may relate to mass media playing an important role in conveying body shape and weight ideals, rather than specifically facial features (e.g., Thompson et al., 1999; Thompson and Smolak, 2001). Contrary to body shape and weight ideals, there is no “gold standard” for facial beauty for the perceptions vary among various people (Rhodes, 2006), which may weaken the effect of media pressure. However, on the other hand, experimental research showed that exposure to idealized images of facial photographs transmitted by mass media can increase facial appearance dissatisfaction in female orthognathic patients (Newton and Minhas, 2005). There may be some discrepancies between the media pressure of self-report and the pressure caused by direct media exposure.
A particular strength of this research is that we extended our research beyond body dimensions to facial characteristics to investigate the risk factors of facial appearance dissatisfaction among orthognathic patients and the controls. However, several limitations also need to be recognized. The first of these limitations is that it is not possible to conclude the direction of the relationship between the factors investigated due to the cross-sectional design of the study. Further clarification of these relationships requires studies using experimental or longitudinal designs. Second, a mismatch of the number of patients and the controls existed. Additional prospective research with larger clinical samples may be warranted. Third, this study lacks the representativeness of the clinical sample. It is difficult to apply the results to other clinical groups who typically undergo cosmetic surgery to alter specific facial features, such as “double-eyelids” and large eyes, a melon-shaped face, and small, proportionate, defined chin. Fourth, gender differences were found concerning shame regarding one’s body and shape/weight concerns, revealing that women experience more body dissatisfaction than do men (Else-Quest et al., 2012; Buchanan et al., 2013). Lastly, we did not collect the educational level of all the subjects, which may affect the differences in the psychological factors between the two groups.
Although this study found the predictive effect of interpersonal pressure on facial appearance dissatisfaction, most existing studies focused on the impact of the specific aspects of interpersonal pressure on body dissatisfaction and have found evidence concerning the impact of different forms of interpersonal pressure, such as peer pressure and parental pressure (Helfert and Warschburger, 2011; Vries et al., 2015; Girard et al., 2018). Future research is needed to examine the effects of interpersonal pressure from family members, friends, and romantic partners on facial appearance dissatisfaction, and to clarify how an individual who is dissatisfied with oneself appearance to interpret and internalize these experiences. Moreover, as mentioned above, the media pressure of self-report and the pressure caused by direct media exposure on facial appearance dissatisfaction may have a different role. Future research is required to further clarify the precise mechanisms of media message to facial appearance dissatisfaction.
First, there were differences between patients and the controls concerning facial appearance dissatisfaction, media pressure, interpersonal pressure, and fear of negative appearance evaluation. These differences between the two groups indicate that the psychosocial factors for orthognathic patients are needed to be paid attention to before the surgical treatment.
Second, we found that facial appearance dissatisfaction was predicted by interpersonal pressure and fear of negative appearance evaluation in both orthognathic patients and non-patients groups. Furthermore, interpersonal pressure and fear of negative appearance evaluation were more strongly associated with facial appearance dissatisfaction for the orthognathic patients. These findings further stress the importance of an interdisciplinary team in building the doctor team, including psychologists when working with people with dentofacial deformities. Psychologists should use measurement to assess the orthognathic patients’ psychological state, and use reasonable interventions to adjust the psychological problems caused by the disease. More specifically, given that the fear of negative appearance evaluation has the strongest influence for orthognathic patients in this study, the psychologists in the team should pay attention to the role of fear of negative appearance evaluations and work toward changing people’s attitudes concerning the negative appearance feedback to improve their facial appearance satisfaction. We believe that the research presented here is a step toward understanding negative appearance evaluation fears as an important risk factor for facial appearance dissatisfaction. Future research can further explore the psychological interventions used to change the fear of negative facial appearance in patients with dentofacial deformities.
In conclusion, the findings of this study expand upon previous work in the field by exploring the effects of risk factors of facial appearance dissatisfaction in both orthognathic patients and non-surgical controls. Generally, the patients and the controls showed the same pattern of results. The results suggest that interpersonal pressure and fear of negative appearance evaluation play a crucial role in facial appearance dissatisfaction for orthognathic patients as well as the non-surgical sample. More significantly, the findings point to the possibility that interventions promoting facial appearance satisfaction could change people’s attitudes toward appearance feedback from friends or family, especially for orthognathic patients. In building the doctor team, it is important to form an interdisciplinary team, including psychologists when working with people with dentofacial deformities. Although the focus of orthognathic surgery procedures is on correcting the morphological deformity, the assessment and treatment plan should also involve the psychosocial aspects of orthognathic patients.
The datasets generated for this study are available on request to the corresponding author.
The studies involving human participants were reviewed and approved by the Southwest University Human Ethics Committee. The patients/participants provided their written informed consent to participate in this study.
PS made substantial contributions to the interpretation of data. PS and YH designed the study and wrote the protocol. HK was responsible for data collection. TW revised the language. HC conducted literature searches and provided summaries of previous research studies. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
This research was supported by grants from the National Natural Science Foundation of China (31771237) and the Fundamental Research Funds for the Central Universities (SWU1709106).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Alanko, O. M. E., Svedströmoristo, A. L., Peltomäki, T., Kauko, T., and Tuomisto, M. T. (2014). Psychosocial well-being of prospective orthognathic-surgical patients. Acta Odontol. Scand. 72, 887–897. doi: 10.3109/00016357.2014.920107
Al-Asfour, A., Waheedi, M., and Koshy, S. (2018). Survey of patient experiences of orthognathic surgery: health-related quality of life and satisfaction. Int. J. Oral Maxillofac. Surg. 47, 726–731. doi: 10.1016/j.ijom.2017.12.010
Berger, Z. E., and Dalton, L. J. (2011). Coping with a cleft II: factors associated with psychosocial adjustment of adolescents with a cleft lip and palate and their parents. Cleft Palate Craniofac. J. 48, 82–90. doi: 10.1597/08-094
Buchanan, N. T., Bluestein, B. M., Nappa, A. C., Woods, K. C., and Depatie, M. M. (2013). Exploring gender differences in body image, eating pathology, and sexual harassment. Body Image 10, 352–360. doi: 10.1016/j.bodyim.2013.03.004
Cadogan, J., and Bennun, I. (2011). Face value: an exploration of the psychological impact of orthognathic surgery. Br. J. Oral Maxillofac. Surg. 49, 376–380. doi: 10.1016/j.bjoms.2010.07.006
Chen, H., and Jackson, T. (2007). Stability of body image concerns among Chinese adolescents: nine-month test-retest reliabilities of the negative physical self scale. Percept. Mot. Skills 105, 677–680. doi: 10.2466/PMS.105.6.677-680
Chen, H., and Jackson, T. (2012). Gender and age group differences in mass media and interpersonal influences on body dissatisfaction among Chinese adolescents. Sex Roles 66, 3–20. doi: 10.1007/s11199-011-0056-8
Chen, H., Jackson, T., and Huang, X. (2006). The negative physical self scale: initial development and validation in samples of Chinese adolescents and young adults. Body Image 3, 401–412. doi: 10.1016/j.bodyim.2006.07.005
Chng, S. C. W., and Fassnacht, D. B. (2016). Parental comments: relationship with gender, body dissatisfaction, and disordered eating in Asian young adults. Body Image 16, 93–99. doi: 10.1016/j.bodyim.2015.12.001
Claes, L., Hart, T. A., Smits, D., Van den Eynde, F., Mueller, A., and Mitchell, J. E. (2012). Validation of the social appearance anxiety scale in female eating disorder patients. Eur. Eat. Disord. Rev. 20, 406–409. doi: 10.1002/erv.1147
Else-Quest, N. M., Higgins, A., Allison, C., and Morton, L. C. (2012). Gender differences in self-conscious emotional experience: a meta-analysis. Psychol. Bull. 138, 947–981. doi: 10.1037/a0027930
Eslamipour, F., Najimi, A., Tadayonfard, A., and Azamian, Z. (2017). Impact of orthognathic surgery on quality of life in patients with dentofacial deformities. Int. J. Dent. 2017:4103905. doi: 10.1155/2017/4103905
Feragen, K. B., and Stock, N. M. (2016). A longitudinal study of 340 young people with or without a visible difference: the impact of teasing on self-perceptions of appearance and depressive symptoms. Body Image 16, 133–142. doi: 10.1016/j.bodyim.2016.01.003
Feragen, K. B., and Stock, N. M. (2017). Psychological adjustment to craniofacial conditions (excluding oral clefts): a review of the literature. Psychol. Health 32, 253–288. doi: 10.1080/08870446.2016.1247838
Frejman, M. W., Vargas, I. A., Rösing, C. K., and Closs, L. Q. (2013). Dentofacial deformities are associated with lower degrees of self-esteem and higher impact on oral health-related quality of life: results from an observational study involving adults. J. Oral Maxillofac. Surg. 71, 763–767. doi: 10.1016/j.joms.2012.08.011
Gignac, G. E., and Szodorai, E. T. (2016). Effect size guidelines for individual differences researchers. Personal. Individ. Differ. 102, 74–78. doi: 10.1016/j.paid.2016.06.069
Girard, M., Rodgers, R. F., and Chabrol, H. (2018). Prospective predictors of body dissatisfaction, drive for thinness, and muscularity concerns among young women in France: a sociocultural model. Body Image 26, 103–110. doi: 10.1016/j.bodyim.2018.07.001
Gomes, A. M. D., Garbin, C. A. S., Ferraz, F. W. D., Saliba, T. A., and Garbin, A. J. I. (2019). Dentofacial deformities and implications on quality of life: a presurgical multifactorial analysis in patients seeking orthognathic surgical treatment. J. Oral Maxillofac. Surg. 77:409.e1. doi: 10.1016/j.joms.2018.09.023
Griffiths, S., Murray, S. B., Bentley, C., Gratwick-Sarll, K., Harrison, C., and Mond, J. M. (2017). Sex differences in quality of life impairment associated with body dissatisfaction in adolescents. J. Adolesc. Health 61, 77–82. doi: 10.1016/j.jadohealth.2017.01.016
Hart, T. A., Flora, D. B., Palyo, S. A., Fresco, D. M., Holle, C., and Heimberg, R. G. (2008). Development and examination of the social appearance anxiety scale. Assessment 15, 48–59. doi: 10.1177/1073191107306673
Helfert, S., and Warschburger, P. (2011). A prospective study on the impact of peer and parental pressure on body dissatisfaction in adolescent girls and boys. Body Image 8, 101–109. doi: 10.1016/j.bodyim.2011.01.004
Jackson, T., and Chen, H. (2008). Sociocultural influences on body image concerns of adolescent girls and young women from China. Sex Roles 58, 402–411. doi: 10.1007/s11199-007-9342-x
Jackson, T., and Chen, H. (2010). Sociocultural experiences of bulimic and non-bulimic adolescents in a school-based Chinese sample. J. Abnorm. Child Psychol. 38, 69–76. doi: 10.1007/s10802-009-9350-0
Jackson, T., and Chen, H. (2011). Risk factors for disordered eating during early and middle adolescence: prospective evidence from mainland Chinese boys and girls. J. Abnorm. Psychol. 120, 454–464. doi: 10.1037/a0022122
Johnson, S. M., Edwards, K. M., and Gidycz, C. A. (2015). Interpersonal weight-related pressure and disordered eating in college women: a test of an expanded tripartite influence model. Sex Roles 72, 15–24. doi: 10.1007/s11199-014-0442-0
Lee, L., Chen, S. H., Yu, C. C., Lo, L. J., Lee, S. R., and Chen, Y. R. (2007). Stigma, body image, and quality of life in women seeking orthognathic surgery. Plast. Reconstr. Surg. 120, 225–231. doi: 10.1097/01.prs.0000264100.57630.c7
Leite, P. C. C., Camarini, E. T., Iwaki Filho, L., Pavan, A. J., Farah, G. J., and da Silva, M. B. (2004). Estudo epidemiológico das deformidades dentofaciais de Maringá/PR-1997/2003. Pesqui. Bras. Odontopediatr. Clin. Integr. 4, 217–220.
Levine, M. P., and Harrison, K. (2009). “Media effects on body image and eating disorders” in Media effects: Advances in theory and research. eds. Bryant, J., and Oliver, M. B.. 3rd edition (New York: Routledge), 490–516.
Levinson, C. A., and Rodebaugh, T. L. (2012). Social anxiety and eating disorder comorbidity: the role of negative social evaluation fears. Eat. Behav. 13, 27–35. doi: 10.1016/j.eatbeh.2011.11.006
Lundgren, J. D., Anderson, D. A., and Thompson, J. K. (2004). Fear of negative appearance evaluation: development and evaluation of a new construct for risk factor work in the field of eating disorders. Eat. Behav. 5, 75–84. doi: 10.1016/S1471-0153(03)00055-2
Menzel, J. E., Schaefer, L. M., Burke, N. L., Mayhew, L. L., Brannick, M. T., and Thompson, J. K. (2010). Appearance-related teasing, body dissatisfaction, and disordered eating: a meta-analysis. Body Image 7, 261–270. doi: 10.1016/j.bodyim.2010.05.004
Morgan, L. K., and Kisley, M. A. (2014). The effects of facial attractiveness and perceiver’s mate value on adaptive allocation of central processing resources. Evol. Hum. Behav. 35, 96–102. doi: 10.1016/j.evolhumbehav.2013.11.002
Newton, J. T., and Minhas, G. (2005). Exposure to ‘ideal’facial images reduces facial satisfaction: an experimental study. Community Dent. Oral Epidemiol. 33, 410–418. doi: 10.1111/j.1600-0528.2005.00239.x
Ong, M. A. H. (2004). Spectrum of dentofacial deformities: a retrospective survey. Ann. Acad. Med. Singap. 33, 239–242. doi: 10.1080/13506120410001682569
Qiu, W. L. (2008). Oral and maxillofacial surgery. Shanghai, China: Shanghai Scientific and Technical Publishers.
Rhodes, G. (2006). The evolutionary psychology of facial beauty. Annu. Rev. Psychol. 57, 199–226. doi: 10.1146/annurev.psych.57.102904.190208
Roberts, R. M., and Mathias, J. L. (2013). Predictors of mental health in adults with congenital craniofacial conditions attending the Australian craniofacial unit. Cleft Palate Craniofac. J. 50, 414–423. doi: 10.1597/11-105
Robinson, L., Prichard, I., Nikolaidis, A., Drummond, C., Drummond, M., and Tiggemann, M. (2017). Idealised media images: the effect of fitspiration imagery on body satisfaction and exercise behaviour. Body Image 22, 65–71. doi: 10.1016/j.bodyim.2017.06.001
Ryan, F. S., Barnard, M., and Cunningham, S. J. (2012). What are orthognathic patients’ expectations of treatment outcome-a qualitative study. J. Oral Maxillofac. Surg. 70, 2648–2655. doi: 10.1016/j.joms.2012.01.002
Sar, C., Soydan, S. S., Ozcirpici, A. A., and Uckan, S. (2015). Psychosocial and functional outcomes of orthognathic surgery: comparison with untreated controls. J. Oral Maxillofac. Surg. Med. Pathol. 27, 451–457. doi: 10.1016/j.ajoms.2014.03.001
Schaefer, M. K., and Salafia, E. H. B. (2014). The connection of teasing by parents, siblings, and peers with girls’ body dissatisfaction and boys’ drive for muscularity: the role of social comparison as a mediator. Eat. Behav. 15, 599–608. doi: 10.1016/j.eatbeh.2014.08.018
Searle, A., Neville, P., and Waylen, A. (2017). Psychological growth and well-being in individuals born with cleft: an application of self-determination theory. Psychol. Health 32, 459–482. doi: 10.1080/08870446.2016.1275630
Soh, C. L., and Narayanan, V. (2014). The impact of surgical correction on the quality of life in patients with dentofacial deformity—a prospective study. J. Oral Maxillofac. Surg. Med. Pathol. 27, 323–327. doi: 10.1016/j.ajoms.2014.03.003
Stice, E., and Agras, W. S. (1998). Predicting onset and cessation of bulimic behaviors during adolescence: a longitudinal grouping analysis. Behav. Ther. 29, 257–276. doi: 10.1016/S0005-7894(98)80006-3
Thogersen-Ntoumani, C., Ng, J. Y. Y., Ntoumanis, N., Chatzisarantis, N., Vlachopoulos, S., Katartzi, E. S., et al. (2016). ‘Mum’s the word’: predictors and outcomes of weight concerns in pre-adolescent and early adolescent girls. Body Image 16, 107–112. doi: 10.1016/j.bodyim.2015.12.004
Thompson, J. K., Heinberg, L. J., Altabe, M., and Tantleff-Dunn, S. (1999). Exacting beauty: Theory, assessment and treatment of body image disturbance. Washington, DC: American Psychological Association.
Thompson, J. K., and Smolak, L. (2001). Body image, eating disorders, and obesity in youth: Assessment, prevention, and treatment. Washington, DC: American Psychological Association.
Thompson, J. K., van den Berg, P., Roehrig, M., Guarda, A. S., and Heinberg, L. J. (2004). The sociocultural attitudes towards appearance scale-3 (SATAQ-3): development and validation. Int. J. Eat. Disord. 35, 293–304. doi: 10.1002/eat.10257
Versnel, S. L., Duivenvoorden, H. J., Passchier, J., and Mathijssen, I. M. J. (2010). Satisfaction with facial appearance and its determinants in adults with severe congenital facial disfigurement: a case-referent study. J. Plast. Reconstr. Aesthet. Surg. 63, 1642–1649. doi: 10.1016/j.bjps.2009.10.018
Vries, D. A. D., Peter, J., Graaf, H. D., and Nikken, P. (2015). Adolescents’ social network site use, peer appearance-related feedback, and body dissatisfaction: testing a mediation model. J. Youth Adolesc. 45, 211–224. doi: 10.1007/s10964-015-0266-4
Wang, Y., Fardouly, J., Vartanian, L. R., and Lei, L. (2019). Selfie-viewing and facial dissatisfaction among Chinese adolescents: a moderated mediation model of general attractiveness internalization and body appreciation. Body Image 30, 35–43. doi: 10.1016/j.bodyim.2019.05.001
Want, S. C., and Saiphoo, A. (2017). Social comparisons with media images are cognitively inefficient even for women who say they feel pressure from the media. Body Image 20, 1–6. doi: 10.1016/j.bodyim.2016.10.009
Watson, D., and Friend, R. (1969). Measurement of social-evaluative anxiety. J. Consult. Clin. Psychol. 33, 448–457. doi: 10.1037/h0027806
Keywords: facial appearance dissatisfaction, orthognathic patients, media pressure, interpersonal pressure, fear of negative appearance evaluation
Citation: Shi P, Huang Y, Kou H, Wang T and Chen H (2019) Risk Factors for Facial Appearance Dissatisfaction Among Orthognathic Patients: Comparing Patients to a Non-Surgical Sample. Front. Psychol. 10:2775. doi: 10.3389/fpsyg.2019.02775
Received: 26 July 2019; Accepted: 25 November 2019;
Published: 11 December 2019.
Edited by:
Ian Stephen, Macquarie University, AustraliaReviewed by:
Bárbara Nazaré, Universidade Lusófona, PortugalCopyright © 2019 Shi, Huang, Kou, Wang and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Wang, NTAwMDc3QGNxbXUuZWR1LmNu; Hong Chen, Y2hlbmhzd3VAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.