- 1Internal Medicine, The University of Texas Southwestern Medical Center, Dallas, TX, United States
- 2Psychiatry, The University of Texas Southwestern Medical Center, Dallas, TX, United States
- 3Parkland Health and Hospital System Dallas, TX, United States
- 4Psychiatry, Children’s Medical Center Dallas, Dallas, TX, United States
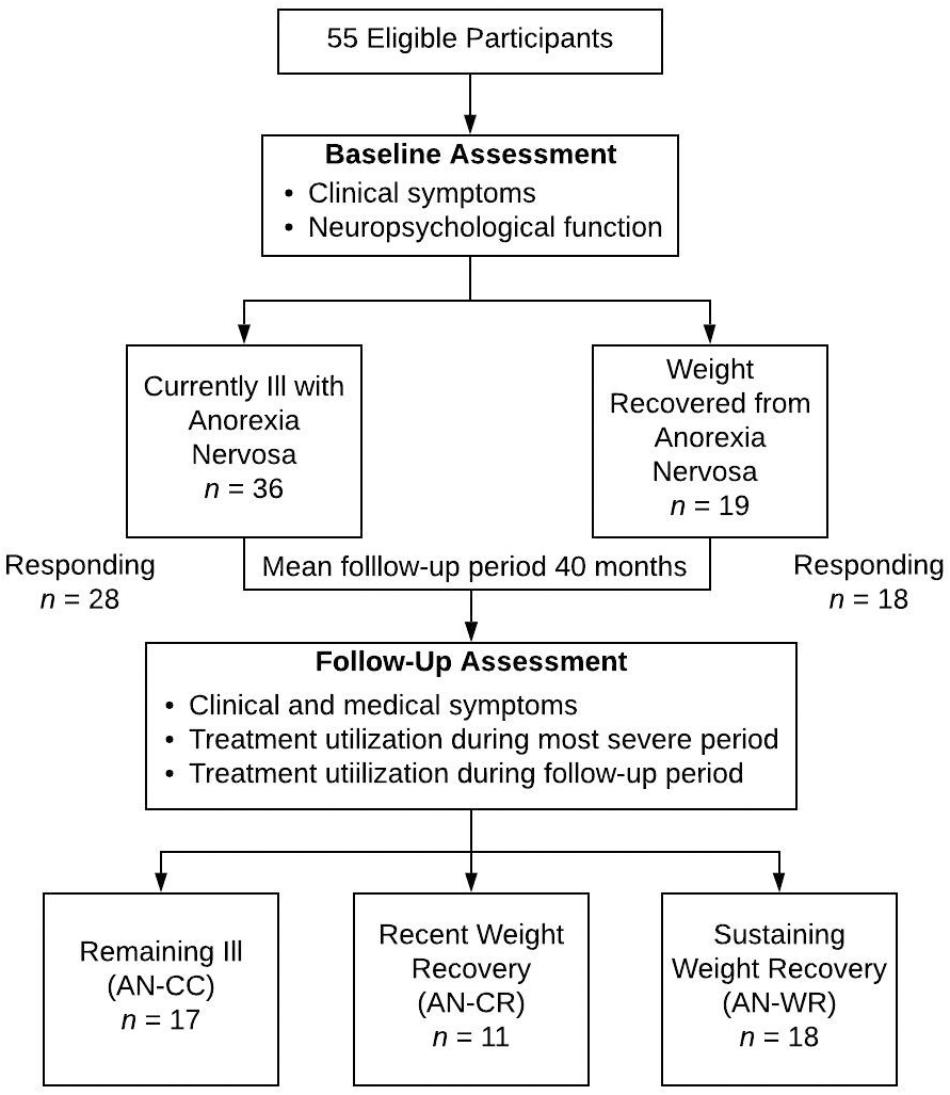
Anorexia nervosa (AN) has a prolonged course of illness, making both defining recovery and determining optimal outpatient treatments difficult. Here, we report the types of treatments utilized in a naturalistic sample of adult women with AN in Texas. Participants were recruited from earlier studies of women with AN (n = 28) and in weight recovery following AN (n = 18). Participants provided information about both their illness and treatments during their most severe period as well as during the 2–6 years following original assessments. Based upon their baseline and follow-up clinical status participants were classified as remaining ill (AN-CC, n = 17), newly in recovery (AN-CR, n = 11), and sustained weight-recovery (AN-WR, n = 18). Utilization of health care institutions and providers were compared across groups. There were no differences in groups related to symptoms or treatments utilized during the severe-period. During the follow-up period, intensive outpatient programs were utilized significantly more by the AN-CC group than the other groups, and dietitians were seen significantly less by the AN-WR group. Medical complications related to the ED were significantly more common in the AN-CC group. All groups maintained similar levels of contact with outpatient psychiatrists, therapists, and primary care physicians. Current treatments remain ineffective for a subset of AN participants. Future prospective studies assessing medical health and comorbidities in AN may provide additional insights into disease severity and predictors of clinical outcome.
Introduction
Anorexia nervosa (AN) is a serious mental illness characterized by difficulties consuming sufficient calories to maintain body weight in conjunction with disturbances in self-perception. Although this disease often begins in adolescence and young adulthood, the course of disease is prolonged and outcomes are poor (Eddy et al., 2017). In examination of treatment outcomes in partial hospitalization and intensive outpatient settings, individuals with AN had worse outcomes for global eating disorder severity and quality of life than individuals with bulimia nervosa, binge eating disorder, and other specified feeding or eating disorder (Hayes et al., 2018). Additionally, a recent meta-analysis showed that treatment changed only short-term weight outcomes but did not significantly impact either short-term or long-term psychosocial outcomes or long-term recovery (Murray et al., 2018).
Anorexia nervosa has a relapse rate of approximately 31%, with the highest risk in the 1–2 years post-treatment (Berends et al., 2018). The dropout rate from outpatient treatment for AN is estimated to range from 20 to 40% (Dejong et al., 2012). Qualitative research on recovered women highlights the importance of psychosocial support as part of recovery (Stockford et al., 2018). Most longitudinal work in adults has focused on assessment of changes in clinical symptoms (Eddy et al., 2017; Harper et al., 2017) or follow-up of patients after specific types of interventions (Schmidt et al., 2016; Makhzoumi et al., 2017). However, there is little evidence that defines what is optimal outpatient treatment for adults with AN, and minimal data describing even the types of treatment utilized in the community in the United States.
Here, we evaluated the symptoms, medical complications and types of treatments utilized by women with AN in Texas. All participants were originally recruited to participate in studies comparing women with AN currently and those in long-term weight recovery following AN. Previously, we reported on the re-assessed clinical status of these participants 2–6 years after original measures were collected (Harper et al., 2017). Neuropsychological function and clinical symptoms were compared across groups based on clinical outcome. We found that women with continued eating disorder had poorer neuropsychological function and self-competence at baseline than those recently recovered. Additionally, recently recovered women showed changes in depression and externalizing bias, a measure of self-related attributions. Here, we report and compare the types of treatment obtained by these subjects at the most severe stage of their eating disorder and during the time period since participating in the study as well as the medical symptoms. We hypothesized that there would be less utilization of outpatient treatment providers amongst the women that relapsed and persisted with disease relative to those that recovered.
Materials and Methods
Participants
Forty-six women ages 20–61 participated (Figure 1). All subjects had completed baseline measures as part of one or more of three previous studies (enrollment period was 2011–2014) including both currently ill and weight-recovered women with AN (Acevedo et al., 2015; Mcadams et al., 2015, McAdams et al., 2016). Weight recovery was defined as having maintained a body mass index (BMI) of greater than 19 for at least 12 months. In addition, the weight-recovered participants could not have met DSM-IV criteria for bulimia nervosa in the last 12 months. Participants provided written informed consent approved by the UT Southwestern Institutional Review Board. The Structured Clinical Interview for DSM-IV (First et al., 2002) was conducted upon initial enrollment to confirm current or past AN and comorbid diagnoses; all interviews were conducted by trained assessors at the masters or doctoral level. BMI was measured at that time. Follow up self-reports were collected and managed using REDCap electronic data capture tools hosted at UT Southwestern (Harris et al., 2009), where participants also provided digital consent upon beginning their follow-up surveys.
Outcome Criteria
For this study participants were classified at follow-up into one of 3 groups based upon baseline and follow-up clinical symptoms: remaining ill (AN-CC), in recovery from baseline ill status (AN-CR), and sustaining weight recovery (AN-WR). The primary outcome criterion was based on maintaining a BMI > 19 for at least 12 months without meeting criteria for bulimia nervosa; this matched the enrollment criteria utilized for weight-recovery in the original studies. BMI was obtained from medical records or clinician report. Participants in recovery could not have participated in intensive outpatient, partial hospital, residential, or inpatient treatment for at least 12 months.
Measurements of Treatment
Using a guided, semi-structured interview, each participant provided information about their eating disorder, focusing on characterization of their symptoms and interactions with clinical treatment providers. With regard to their eating disorder, each subject self-reported their age of onset, their age of first treatment, and their age during their worst period with the eating disorder. BMI, all care utilized immediately following the worst period (inpatient/residential, partial hospital, intensive outpatient, or outpatient), and the symptoms (restriction, binging, purging, depression, anxiety, alcohol, and other substance use) during the worst period were detailed. The duration and intensity of outpatient treatment following this period was queried, including interactions with five different types of clinical care (primary care physician, psychiatrist, therapist, dietitian, and group therapy). If answered affirmatively the type of clinical care was sought, then the frequency (annually, quarterly, monthly, biweekly, and weekly) and duration of that clinical interaction was inquired.
Separately, treatment utilization following the individuals’ participation in the research study was assessed. Two tables were completed for every subsequent 6 month period to present. The first table assessed a need for a higher level of care for the eating disorder (or a related comorbid condition such as suicidality or substance abuse) including both medical and psychiatric hospitalizations (further classified as inpatient, residential, partial hospital, and intensive outpatient), and ER visits. The second table assessed the participant’s interaction with five different types of outpatient clinical care, including frequency and duration, for each 6 month period.
Statistical Analysis
Statistical analyses were conducted using the IBM Statistical Package for Social Sciences (SPSS; v.23). To determine differences between groups, separate one-way analysis of variance (ANOVAs) were conducted on continuous data. Post hoc pairwise comparisons were conducted using a Bonferroni correction for multiple comparisons. Categorical and dichotomous (yes/no) data were analyzed by Chi-square analyses.
Results
Participants
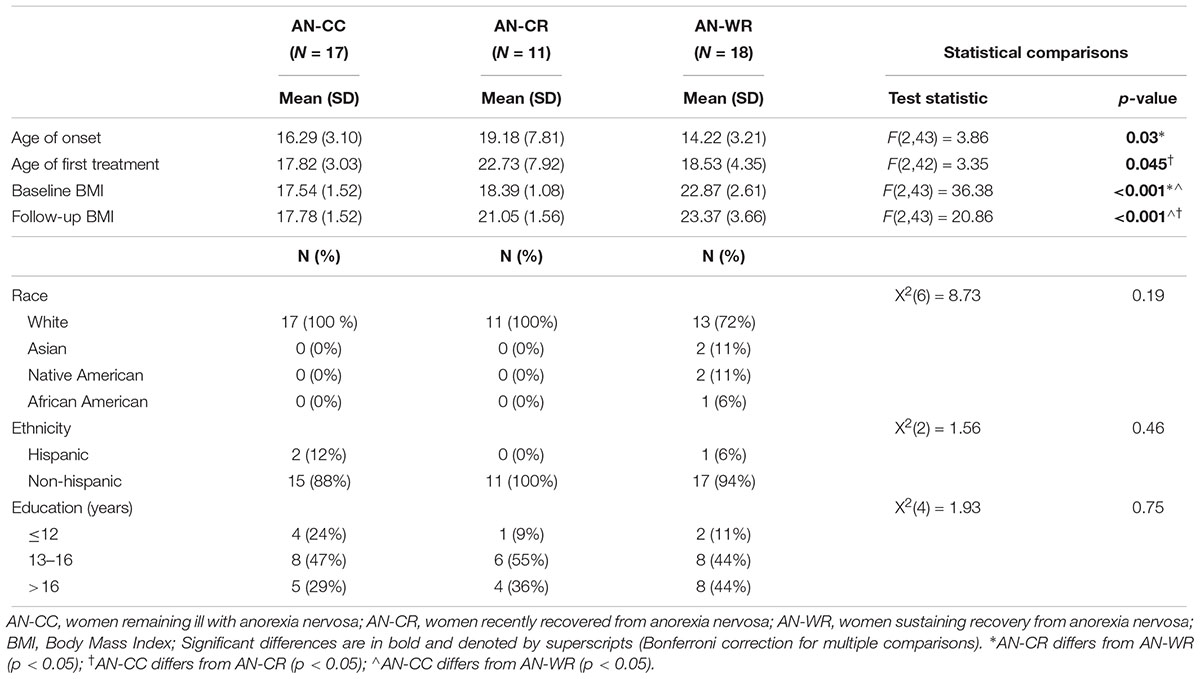
As previously reported, amongst the AN-C group, 17 participants remained ill (AN-CC) and 11 achieved recovery from a baseline ill status (AN-CR), a recovery rate of 39% (Table 1). In addition, all 18 of weight-recovered group remained weight-recovered at follow up (AN-WR). There were no differences in the distributions of subtypes of AN by group [AN binge-purge/restricting, AN-CC 9/8, AN-CR 5/6, AN-WR 11/7; X2(2) = 0.67, p = 0.71, V = 0.12].
The AN-CR group had a later age of onset than the AN-WR [age of onset in years, AN-CC, 16.3, AN-CR 19.2, AN-WR 14.2, F(2, 43) = 3.86, p = 0.03; post hoc AN-WR < AN-CR, p = 0.02]. The AN-CC group had an earlier age of first treatment than the AN-CR group [age of first treatment, AN-CC 17.8, AN-CR 22.7, AN-WR 18.5, F(2, 42) = 3.35, p = 0.045; post hoc AN-CC < AN-CR, p = 0.05]. The AN-CC and AN-CR groups both had a lower BMI at baseline than the AN-WR group [BMI at baseline, AN-CC 17.5, AN-CR 18.4, AN-WR 22.8, F(2, 43) = 36.4, p =< 0.001; post hoc AN-CC < AN-WR, p = 0.05 and AN-CR < AN-WR, p = 0.05] but did not differ from each other.
Severe-Period Symptoms and Treatments
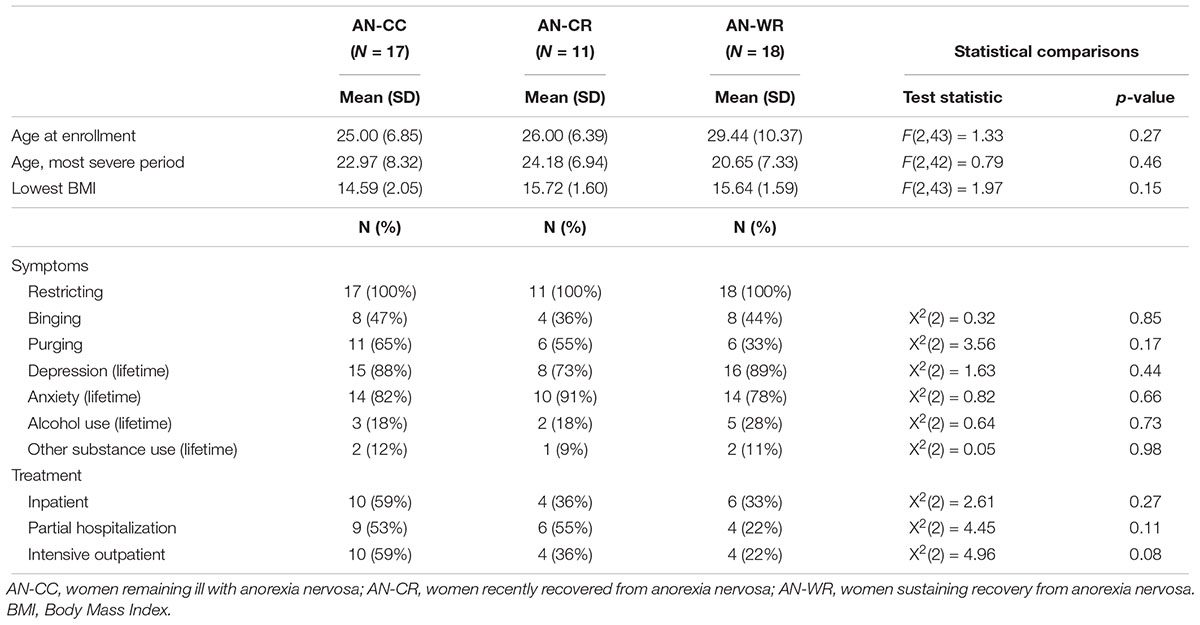
There were no differences in the clinical symptoms or treatments utilized in the worst period of the disease for any of the groups (Table 2). Eating disorder symptoms were considered most severe for all subjects on average at 22.6 years, and the lowest BMI was similar across all subjects (mean lowest BMI 15.32). Across all groups, 43.6% of subjects reported binge-eating behaviors, and 50% reported purging symptoms in the severe period. 84.8% of the subjects had comorbid depression and 82.6% had comorbid anxiety. Problems with alcohol and substance abuse were less prevalent across the sample, with 21.7% of subjects reporting an alcohol use disorder and 10.9% reporting substance abuse. No differences in the types of intensive treatment utilized following that severe-period were observed across the 3 groups, with 43.5% utilizing inpatient or residential treatments, 41.3% in partial hospital programs, 39.1% in intensive outpatient.
Follow-Up Period Symptoms and Treatments
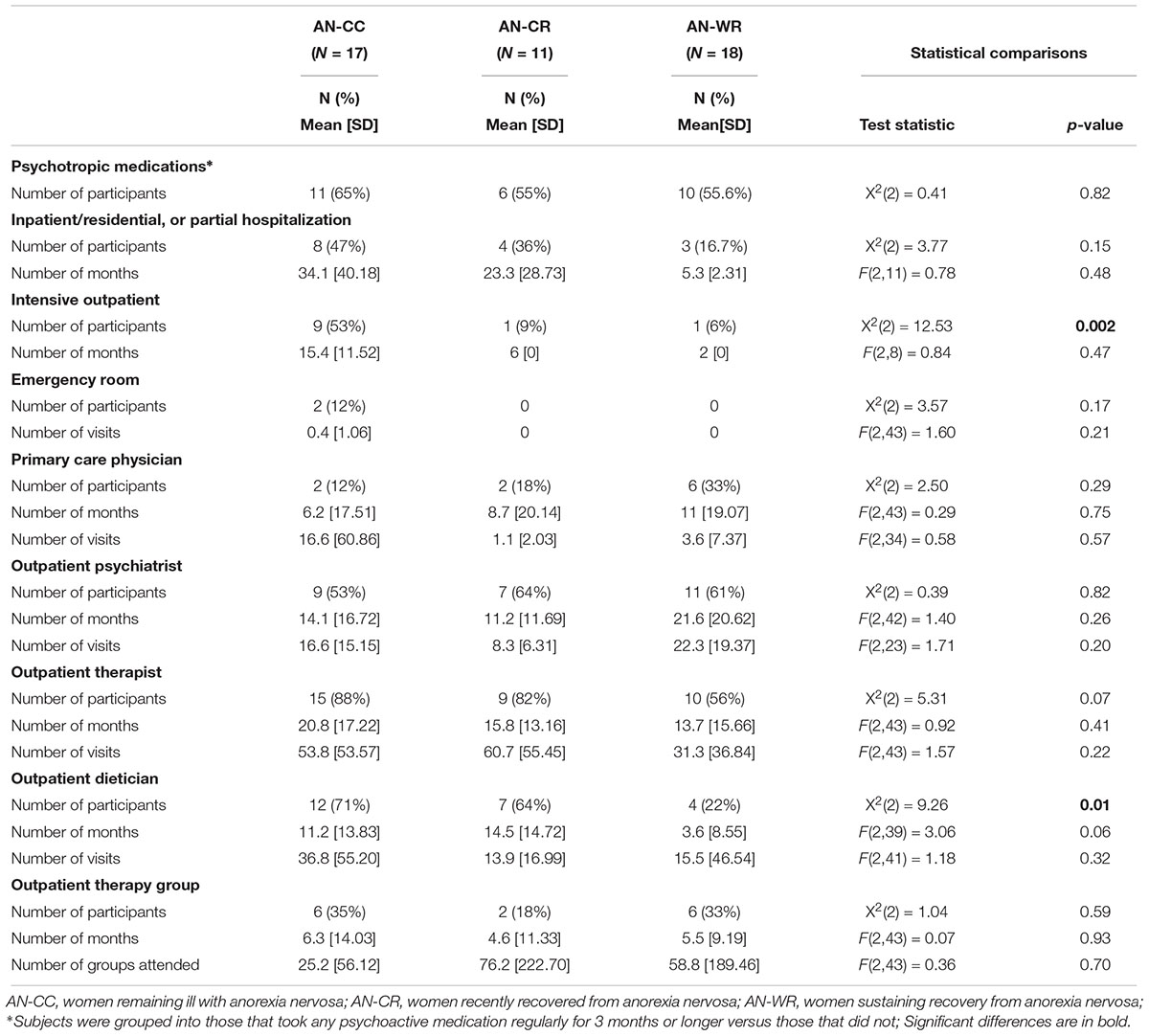
Participants were followed up on average 40 months after initial assessment [follow-up period, AN-CC 41.1, AN-CR 40.9, AN-WR 38.1, F(2, 43) = 0.07, p = 0.93]. Few differences were observed in the types and amount of care obtained from clinical providers in the follow-up period between initial participation in the study and returning for the follow-up measures (Table 3). Some members in all groups attended inpatient, residential or partial hospital eating disorder programs (AN-CC, 47%, AN-CR, 36%, and AN-WR, 17%). The three subjects in the AN-WR group that required a higher level of care did so for escalating ED symptoms consistent with having developed and then recovered from bulimia nervosa during the follow-up period. The only significant difference was related to intensive outpatient treatment programs, which were most heavily utilized by those currently ill with AN [AN-CC, 53%, AN-CR, 9%, AN-WR, 6%, X2(2) = 12.53, p = 0.002].
In terms of outpatient treatment, similar engagement in outpatient care was observed across all groups. No differences were observed in terms of contact with type of provider across groups with 58.7% in treatment with an outpatient psychiatrist, 73.9% reporting treatment with an outpatient therapist, and 30.4% engaging in group therapy. The more recently ill participants saw dieticians significantly more than those in sustained weight-recovery [AN-CC, 70%, AN-CR 64%, AN-WR 22%, X2(2) = 9.26, p = 0.01].
Medications and Medical Complications
In this retrospective study, virtually no participants were able to recall either the duration or names of all psychoactive medications taken. Many reported using medications while in inpatient/residential treatment programs but stopping them days or weeks after discharge for a wide variety of reasons (forgot to pick up, did not have a refill, did not think it was helpful). Because of this limited recall, subjects were grouped into those that took any psychoactive medication regularly for 3 months or longer versus those that did not. All participants that took a medication for more than 3 months appeared confident about their behavior. With these limits, no differences in medication use were seen across the three groups (Table 3).
Participants were also queried about the presence any medical illnesses derived from the eating disorder (low bone mineral density, anemia, electrolyte disturbances, and cardiovascular problems) or likely to impact their eating disorder symptoms (gastrointestinal disorders) as well as any non-ED associated medical problems. The AN-CC group reported significantly more ED-associated medical issues [low bone mineral density (Dejong et al., 2012), hypoglycemia, anemia (Hayes et al., 2018), hypophosphatemia] than the AN-CR (inflammatory bowel disease) and AN-WR (low bone mineral density, functional gastrointestinal disorders) groups [ED associated medical problems, AN-CC, 52.9%, AN-CR, 9.1%, AN-WR, 16.7%, χ2(2) = 8.29, p = 0.02]. There were not significant differences by groups for other medical problems [non-ED associated medical problems, AN-CC, 0%, AN-CR, 18.2%, AN-WR, 27.8%, χ2(2) = 5.33, p = 0.07]. The non-ED associated medical problems reported included migraines (Hayes et al., 2018), fibromyalgia, thyroid disorder (Hayes et al., 2018), rheumatoid arthritis, osteoarthritis, pelvic pain, and asthma. There were no differences in engagement with a primary care provider across the groups [percent with primary care provider, AN-CC, 11.8%, AN-CR, 18.2%, AN-WR, 33.3%, χ2(2) = 2.50, p = 0.29].
Discussion
In this study, we characterized both the medical and psychiatric symptoms and types of care accessed by a community sample of women living with and recovered from AN in the United States. This is a first and necessary step toward improving clinical outcomes for AN as it enables us to consider whether the impediments to recovery from AN are related primarily to access to care or the effectiveness of the care that is delivered. Most importantly, we found little evidence that the type of treatments utilized, either at the most severe stage of disease or in outpatient care, were related to longer-term clinical outcomes. Further, we found that most participants were engaged in regular outpatient treatment with therapists, dietitians, and psychiatrists. Another key finding is that the utilization of therapists and psychiatrists did not differ even for the women with years of recovery from AN relative to those more recently ill, suggesting that continued engagement with mental health professionals may be important for all patients with a history of AN.
Failure in treatment of AN is commonly ascribed to the egosyntonic nature of the disorder, with the resulting perception that women with the illness are deliberately choosing not to recover and are at fault (Gregertsen et al., 2017). However, the reality of the prolonged disease is that it gradually becomes ego-dystonic, as the patients recognize that they have actually lost the ability to eat sufficient food for their mental and physical health (Marzola et al., 2016), and express ambivalence toward the disease (Williams and Reid, 2010). Nevertheless, there remains a perspective that patients with AN choose to maintain their illness and could recover if able to utilize already-existing interventions (Crisp et al., 2000; Stewart et al., 2006; McAdams, 2017). This longitudinal data, albeit from a small sample, suggests otherwise. Somewhat surprisingly, all three groups of subjects – defined by their long-term clinical outcomes – engaged in the same types of treatments, with the only exception being more intensive outpatient treatment for those that continued with disease and increased treatment with outpatient dietitians in those more recently ill. Thus, ED treatment utilization was not correlated positively with sustained weight-recovery from AN. Different approaches to treating this disease are desperately needed in the United States. The medical profession should recognize that current treatments for AN are ineffective for many patients, and this should not be viewed as the patients’ choosing to stay sick any more than a lack of response of one’s cancer to chemotherapy is a choice that those patients make.
Clinical symptoms commonly tracked in eating disorders such as severity of disease based on BMI, presence of binging or purging behaviors, and comorbid anxiety or depressive disorders were also unrelated to long-term course of illness. Most subjects experienced depression and anxiety during their eating disorder. Binge-eating behaviors and purging symptoms were observed in about half of the participants, irrespective of group. These data are consistent with recent literature that suggests severity-specifiers for AN may not be clinically relevant (Gianini et al., 2017; Nakai et al., 2017). In a recent meta-analysis of treatments for AN, Murray et al. (2018) found that although weight improved amongst AN participants between beginning and end of treatment, weight was not improved at follow-up, and psychological changes were not observed at either time point. We previously reported that this cohort had no changes longitudinally in body shape questionnaire, anxiety, or self-esteem, although depression and externalizing bias did change over time across groups (Harper et al., 2017). Another novel finding is that all groups of patients reported that the most severe time-period for eating disorder symptomatology was in their early twenties, potentially identifying a specific high-risk time period of emerging adulthood that could be targeted by increased psychosocial supports or clinical monitoring for eating disorder symptoms.
Another potential gap in the treatment of AN identified here is in the recognition and treatment of the many medical complications and problems related to development or progression of the disorder. More of the AN-CC group reported significant medical complications from their disease than those in both the AN-CR and AN-WR groups. These medical complications included gastrointestinal disturbances (gastroesophageal reflux disorder, irritable bowel syndrome, and gastroparesis) as well as problems from chronic malnutrition (low bone mineral density and anemia) and purging behaviors (orthostatic hypotension and electrolyte abnormalities). The presence of medical complications of AN may provide a better severity specifier more closely related to course of illness than psychiatric symptoms or BMI alone, but few researchers examining the progress of eating disorder patients include assessments of medical health and comorbidities. Individuals with medical complications of the disease might also be less responsive to existing treatments for AN and related psychiatric comorbidities. It is particularly concerning that despite the increased presence of medical complications, the AN-CC group was no more likely to have a primary care provider than the other two groups. This may be related to the growing difficulty in securing a primary care provider in the United States (Bodenheimer and Pham, 2010). A multidisciplinary team that includes a primary care provider cognizant of the medical complications may be of particular benefit as medical information can be used psychotherapeutically to form an alliance with the patient and diminish his or her denial of the seriousness of the illness.
This study has many limitations. This was a small sample of individuals with AN, and treatment utilization was based on retrospective report of the patient. Because attending treatment programs often results in substantial disruptions of one’s life, recall related to the higher levels of care may be more accurate than the duration one worked with an outpatient therapist, psychiatrist or dietitian. External documentation, exam, or lab work to assess the presence or absence of medical complications for all participants was not possible. The study was based on DSM-IV criteria for AN rather than DSM-5 as the studies began before DSM-5 was published; given that the stringency for AN was actually reduced in DSM-5, all subjects meet those criteria as well. Clinical, cognitive, neural and genetic data from these subjects has been previously published, but information about their severe periods of illness and clinical utilization has not been reported previously.
Conclusion
In conclusion, we found little evidence to suggest the type of treatments utilized by AN participants were related to longer-term clinical outcomes. Participants who remained ill reported more medical complications related to their illness suggesting this may represent a more severe phenotype. Importantly, current treatments for AN are ineffective for a subset of eating disorder patients and larger studies that prospectively monitor AN including measurement of medical health and comorbidities in concert with clinical outcome are needed.
Ethics Statement
This study was carried out in accordance with the recommendations of UTSW IRB with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the UTSW IRB.
Author Contributions
BB and CM designed the study. BB, JH, and CM collected the data and contributed to writing and editing the manuscript. All authors processed and analyzed the data.
Funding
The funding for this study was provided by the Hogg Foundation for Mental Health, NIMH K23 MH093684 and R01 MH112927A, and Klarman Family Foundation Eating Disorder Research Grants Program 3887. Data collection was supported by Academic Information Systems grant support, CTSA NIH Grant UL1-RR024982. The research presented in this publication is solely the responsibility of the authors and does not necessarily represent the official views of any of the funding agencies.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Acevedo, S. F., Valencia, C., Lutter, M., and McAdams, C. J. (2015). Severity of eating disorder symptoms related to oxytocin receptor polymorphisms in anorexia nervosa. Psychiatry Res. 228, 641–648. doi: 10.1016/j.psychres.2015.05.040
Berends, T., Boonstra, N., and van Elburg, A. (2018). Relapse in anorexia nervosa: a systematic review and meta-analysis. Curr. Opin. Psychiatry 31, 445–455. doi: 10.1097/YCO.0000000000000453
Bodenheimer, T., and Pham, H. H. (2010). Primary care: current problems and proposed solutions. Health Aff. 29, 799–805. doi: 10.1377/hlthaff.2010.0026
Crisp, A. H., Gelder, M. G., Rix, S., Meltzer, H. I., and Rowlands, O. J. (2000). Stigmatisation of people with mental illnesses. Br. J. Psychiatry 177, 4–7. doi: 10.1192/bjp.177.1.4
Dejong, H., Broadbent, H., and Schmidt, U. (2012). A systematic review of dropout from treatment in outpatients with anorexia nervosa. Int. J. Eat Disord. 45, 635–647. doi: 10.1002/eat.20956
Eddy, K. T., Tabri, N., Thomas, J. J., Murray, H. B., Keshaviah, A., Hastings, E., et al. (2017). Recovery from anorexia nervosa and bulimia nervosa at 22-Year follow-up. J. Clin. Psychiatry 78, 184–189. doi: 10.4088/JCP.15m10393
First, M. B., Spitzer, R. L., Miriam, G., and Williams, J. B. W. (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition with Psychotic Screen (SCID-I/P W/PSY SCREEN). New York, NY: Biometrics Research, New York State Psychiatric Institute.
Gianini, L., Roberto, C. A., Attia, E., Walsh, B. T., Thomas, J. J., Eddy, K. T., et al. (2017). Mild, moderate, meaningful? Examining the psychological and functioning correlates of DSM-5 eating disorder severity specifiers. Int. J. Eat Disord. 50, 906–916. doi: 10.1002/eat.22728
Gregertsen, E. C., Mandy, W., and Serpell, L. (2017). The egosyntonic nature of anorexia: an impediment to recovery in anorexia nervosa treatment. Front. Psychol. 8:2273. doi: 10.3389/fpsyg.2017.02273
Harper, J. A., Brodrick, B., Van Enkevort, E., and McAdams, C. J. (2017). Neuropsychological and cognitive correlates of recovery in anorexia nervosa. Eur. Eat. Disord. Rev. 25, 491–500. doi: 10.1002/erv.2539
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., and Conde, J. G. (2009). Research electronic data capture (RED-Cap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381.
Hayes, N. A., Welty, L. J., Slesinger, N., and Washburn, J. J. (2018). Moderators of treatment outcomes in a partial hospitalization and intensive outpatient program for eating disorders. Eat. Disord. doi: 10.1080/10640266.2018.1512302.
Makhzoumi, S. H., Coughlin, J. W., Schreyer, C. C., Redgrave, G. W., Pitts, S. C., and Guarda, A. S. (2017). Weight gain trajectories in hospital-based treatment of anorexia nervosa. Int. J. Eat. Disord. 50, 266–274. doi: 10.1002/eat.22679
Marzola, E., Panepinto, C., Delsedime, N., Amianto, F., Fassino, S., and Abbate-Daga, G. (2016). A factor analysis of the meanings of anorexia nervosa: intrapsychic, relational, and avoidant dimensions and their clinical correlates. BMC Psychiatry 16:190. doi: 10.1186/s12888-016-0894-6
McAdams, C. J. (2017). Changing the brain to treat anorexia nervosa. Lancet Psychiatry 4, 262–263. doi: 10.1016/S2215-0366(17)30074-3
McAdams, C. J., Jeon-Slaughter, H., Evans, S., Lohrenz, T., Read Montague, P., and Krawczyk, D. C. (2016). Neural differences in self-perception during illness and after weight-recovery in anorexia nervosa. Soc. Cogn. Affect. Neurosci. 11, 1823–1831. doi: 10.1093/scan/nsw092
Mcadams, C. J., Lohrenz, T., and Montague, P. R. (2015). Neural responses to kindness and malevolence differ in illness and recovery in women with anorexia nervosa. Hum. Brain Mapp. 36, 5207–5219. doi: 10.1002/hbm.23005
Murray, S. B., Quintana, D. S., Loeb, K. L., Griffiths, S., and Le Grange, D. (2018). Treatment outcomes for anorexia nervosa: a systematic review and meta-analysis of randomized controlled trials. Psychol. Med. 49, 535–544. doi: 10.1017/S0033291718002088
Nakai, Y., Nin, K., Noma, S., Teramukai, S., Fujikawa, K., and Wonderlich, S. A. (2017). The impact of DSM-5 on the diagnosis and severity indicator of eating disorders in a treatment-seeking sample. Int. J. Eat. Disord. 50, 1247–1254. doi: 10.1002/eat.22777
Schmidt, U., Ryan, E. G., Bartholdy, S., Renwick, B., Keyes, A., O’Hara, C., et al. (2016). Two-year follow-up of the MOSAIC trial: a multicenter randomized controlled trial comparing two psychological treatments in adult outpatients with broadly defined anorexia nervosa. Int. J. Eat. Disord. 49, 793–800. doi: 10.1002/eat.22523
Stewart, M. C., Keel, P. K., and Schiavo, R. S. (2006). Stigmatization of anorexia nervosa. Int. J. Eat. Disord. 39, 320–325. doi: 10.1002/eat.20262
Stockford, C., Stenfert Kroese, B., Beesley, A., and Leung, N. (2018). Women’s recovery from anorexia nervosa: a systematic review and meta-synthesis of qualitative research. Eat. Disord. doi: 10.1080/10640266.2018.1512301 .
Keywords: eating disorders, bulimia nervosa, recovery, longitudinal, cohort, treatment
Citation: Brodrick B, Harper JA, Van Enkevort E and McAdams CJ (2019) Treatment Utilization and Medical Problems in a Community Sample of Adult Women With Anorexia Nervosa. Front. Psychol. 10:981. doi: 10.3389/fpsyg.2019.00981
Received: 10 January 2019; Accepted: 12 April 2019;
Published: 03 May 2019.
Edited by:
Emilio Gutierrez, Universidade de Santiago de Compostela, SpainReviewed by:
Rachel Miller Radin, University of California, San Francisco, United StatesTherese Fostervold Mathisen, Norwegian School of Sport Sciences, Norway
Copyright © 2019 Brodrick, Harper, Van Enkevort and McAdams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Brooks Brodrick, QnJvb2tzLkJyb2RyaWNrQFVUU291dGh3ZXN0ZXJuLmVkdQ==
 Brooks Brodrick
Brooks Brodrick Jessica A. Harper
Jessica A. Harper Erin Van Enkevort
Erin Van Enkevort Carrie J. McAdams2,4
Carrie J. McAdams2,4