
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 15 November 2018
Sec. Psychology for Clinical Settings
Volume 9 - 2018 | https://doi.org/10.3389/fpsyg.2018.02226
This article is part of the Research Topic Coping with Life Stress View all 21 articles
Context: Families with high rates of childhood adversities (CAs) (multi problem families, MPF) have an increasing importance in public health-policy.
Objective: The present study addresses the relationship between risk- and protective factors and the severity and treatment-outcome of mental disorders.
Setting: Family-therapeutic home-based treatment for MPF. We examined a clinical sample (N = 1031) of children between the age of 4 to 17, and a non-clinical sample of 148 children. We hypothesized that of all children of the clinical group have a predominance of risk factors and a higher number of psychopathological symptoms. Furthermore, we hypothesized that children with a predominance of protective factors benefit stronger from psychotherapy.
Main Results: In the clinical sample, most children met the criteria of a psychopathological diagnosis (95.7%, as compared to 21.6% in the non-clinical sample) and showed significant higher rates of CAs and significant less protective factors as compared to the non-clinical sample. The clinical group showed a significant reduction of psychopathological symptoms and benefited equally well from treatment. The number of risk factors was a significant predictor for a child from the non-clinical sample to meet the criteria of a psychopathological diagnosis, while the number of protective factors significantly predicted the absence thereof.
Conclusion: Children and adolescents with high scores of CAs show significant associations with child psychiatric symptoms (d = 0.35; including all ICD-diagnosis such as, e.g., Asperger Syndrome, ADHD etc. with a higher rate of genetic etiology). Early life stressors, however, do not trigger an irreversible fate, as psychotherapy with young people with high numbers of risk factors does help to reduce psychopathological symptoms significantly (range of five outcome parameters: d = 0.31–0.72).
Epidemiological data show that up to 20% of children and adolescents show mental disorders (Belfer, 2008). The prevalence of neglect, maltreatment, deprivation in childhood in Germany is estimated with about 10–15% (Reichl et al., 2014), higher rates were found in multi problem families (MPF; Belfer, 2008), which leads to an increased risk of vulnerability for children (Egle et al., 2004; Bachler et al., 2014). High-risk families not only meet many criteria of family adversity indices, but also show low treatment compliance and low relational functioning of the families (Bachler et al., 2017). MPF exhibit structural, dynamic, and social characteristics that could lead to an increased risk of vulnerability and implement and test treatment procedures that help adults and children of such multi-problem or high-risk families. Typically, families in such problematic situations exhibit disorders in parental relationship behavior, have a lower socioeconomic status (SES), and are associated with conditions of deprivation (Woolfenden et al., 2001; Witkiewitz et al., 2013). Low SES has been shown to be linked to parental behavior as a moderating and mediating terms of being less engaged, less parental monitoring and a less enriched environment, thereby exerting negative attachment-related effects to child development (Bornstein and Bradley, 2003). There is an extensive research about mediating and moderating factors in the development of psychopathological symptoms (Luo and Waite, 2005; Lund et al., 2011; Cabaj et al., 2014; Rasmussen et al., 2014).
These problems sometimes run across many generations in the families, which eventually creates a lack of trust into governmental and municipalities’ services and a belief that the life’s problems are an inevitable fate. Therefore, MPF form a clientele that is sometimes referred to as “hard to reach,” even though it has been shown that psychotherapy is effectively possible (Curtis et al., 2004). Untreated, multi-generational psycho-social problems have an impact on and interaction with education, SES, general health, quality of life, number of children and more, and therefore have been shown to form a high economic burden to societies (Wittchen and Jacobi, 2005). Detection and treatment of MPF is thus ethically and financially of high importance to social policy and the general public, in order to not allow these networks of childhood adversities (CAs) forming it to an irreversible damage as measured by psychiatric diagnoses/symptoms.
Kessler et al. (2010) undertook the approach of relating 12 CAs – grouped into clusters of interpersonal loss, parental maladjustment, maltreatment and others – with the onset of 20 DSM IV disorders in a cross-national study. They found that in high-income as well as in low-income countries, there was an almost equal chance of 38.4% (and 39.1%) to report one or more of the CAs. The presence of one or more CAs accounted for 28.2% of all DSM-IV diagnoses over all countries, and were significantly correlated with an increased risk for DSM-IV disorder (Klasen et al., 2015). Slopen et al. (2014) examined the influence of high and chronic exposure to CAs at different developmental periods in childhood on internalizing and externalizing symptoms, as well as other health related parameters (weight, blood pressure) of adolescents or adults (Edwards and Hans, 2015). They showed that onset and continuance of cumulative childhood adversity are influencing mental and physical health risks in general. Similarly, it has been shown that children or adolescents with 4 or more CAs were 7.3 times more likely to display depression, anxiety, affect regulation problems, or substance abuse (Putnam et al., 2013). Besides forming general risk factors, CAs might also play a direct role in onset of specific disorders and specific symptoms (Bentall et al., 2014; Young and Widom, 2014), while it has also been found that severity of CAs plays a bigger role than their mere number (Schilling et al., 2008).
Research into the underlying mechanisms of cross-generational impact of CAs sketch a picture of interactions between nature and nurture. Cicchetti and Rogosch (2012) reported a different genotype between maltreated and non-maltreated children, which was associated to their individual level of resilience. The influence of bonding patterns has been demonstrated in several studies (Haushofer and Fehr, 2014; Reichl et al., 2014). The neuropathophysiology of psychosocial stress and stress responsivity has, e.g., been linked to the HPA axis, as well as neurogenesis and the development of functionality and morphology of the brain (Bick et al., 2012). Kim et al. (2013) revealed the influence of childhood poverty in low SES families and CAs on amygdala and prefrontal cortex dysregulation. This proven shift in the subcortical mode is a result of individually different susceptibility to qualities of environments through genetic factors as Bakermans-Kranenburg and van Ijzendoorn (2006) showed for the DRD4 dopaminergic system, behavior problems and parenting. Environments (e.g., parenting) are steering epigenetic processes and children’s behavior is forming parenting (Hartman and Belsky, 2016). Taken together, there is empirical evidence that CAs and also protective factors are integrated into the interacting levels of behavior, environment, and gene-expression, as it is conceptualized in the model of genetic differential sensitivity to social environment (GDSE, Hengartner et al., 2013; Mitchell et al., 2013; McDonald et al., 2016; Moore and Depue, 2016).
The existing literature and research is, however, thin on the interaction between protective factors and risk-factors and especially their influence on psychotherapy in form of increased number of symptoms and effectiveness of treatment (Andershed and Andershed, 2015). The present research therefore aimed at replicating earlier results, that children and adolescents from a non-clinical sample have lower risk factors and more protective factors as compared to a clinical sample for a German-Austrian setting. Furthermore, we tested the hypothesis that the number of risk- and protective factors (and their combination) predicts the presence and absence of psychopathological diagnosis in a non-clinical sample. In addition, we addressed the respective relationship between CAs and protective factors and symptomatic burden.
TAF-treatment in the clinical sample is initiated through the proposal of the regional youth services (Salzburg, Upper Austria and South East of Bavaria-Germany). The indication is done after a first diagnostic and selective-indicative clearing. All 1031 families for whom the treatment began in 2008 or later but only if the index child was older than 4 years were included in the study (consecutive sample). The data on the children and adolescents in the comparative sample (n = 148) were collected at a grammar school in southern Germany. The drop out quote of the clinical group was 17% (failed compliance). The treatment length 21.6 months (mean).
The clinical sample of the present study consisted of all patients/families, entering TAF in the years between 2008 and 2017. Diagnostic clearing cases cover patients that were placed in new families, entered outpatient psychotherapy or suffered of severe psychopathology.
An overview of socio-demographic data, ICD-10 diagnoses and symptom-score (pre-post) can be seen in Table 1.
TAF (therapeutic, outreach intervention) is a disorder-oriented, therapeutic, intervention for MPF. It constitutes an integrative form of family therapy (FT) for MPFs and integrates family-therapeutic interventions and elements of structural psychotherapy. TAF incorporates the various common principles for treatment of structural psychotherapy (for the improvement of ego-structural competencies) that were identified by the task force of the APA Division 12: strong working alliance, therapist’s ability to repair alliance-ruptures, collaboration on goals, and a high level of therapist activity (Critchfield and Benjamin, 2006).
All instruments of measurement used in this study are part of a standardized in-house manual (TAF-DOK). Some of the instruments of TAF-DOK are only applicable to children under the age of 4 years. A total of 118 cases were therefore not considered in the clinical group because we did not have access to a kindergarten.
The MPI (Esser et al., 1989) is a structural, standardized, clinical interview for therapists to assess the severity of the mental disorder of children, adolescents, and primary attachment figure. The interview is divided into three parts: the parents’ and child’s demographic and social statistics, child and adolescent psychiatric symptoms and socio-familial conditions/and important life events. The 37 questions regarding child and adolescent psychiatric symptoms are leading through clearly stipulated criteria and scores of severity to a cumulative child-psychiatric symptom-score and different ICD-10 diagnoses (non ICD-10 diagnose; ICD-10 F92-98 mood, anxiety, and attachment disorders; ICD-10 F 90 ADHD; ICD-10 60 personality disorders, ICD-10 F 91 externalizing symptoms and maladaptive behavior; and F84-89 special diagnoses ICD-10) and comorbidities. The interrater reliability is 0.71–1.0, i.e., the kappa coefficient of concurrence of the diagnoses was determined as r = 0.71 (percentage of concurrence 79% between the clinical, professional opinions).
The FAI was developed by Rutter and Quinton (1977). It measures five family-related CAs of chronic disharmony in the family, a low SES, small living quarters, parental criminality, and mental disorder of the mother. Reliability is given as 0.65, and validity in the range of 0.66 to 0.70 (Rutter and Quinton, 1977).
Egle et al. (2004) presented a meta-analytic overview of empirically found protective and adverse life events. The results of this meta-analysis were used to create a screening questionnaire, which includes 22 adverse live events. CAs were assessed dichotomously.
We generated five Clusters of CAs: Cluster 1a (SES-Resources): low SES, poor schooling of parents, unemployment, large family and very narrow living room, single parent, contacts with institutions of social control; Cluster 2a (violence): crime or antisocial behavior of parents, chronic disharmony in the family, authoritarian paternal behavior; Cluster 3a (attachment related CAs): maternal occupational activity in the first year of life, insecure attachment behavior after 12/18 months of age, loss of parent, divorce, separation of parents, frequently changing early reference person, improper contacts with peers, age distance to the nearest siblings younger than 18 months, prolonged separation from the parents during the first 7 years of life, male sex; Cluster 4a (physical or mental illness): mental disorder of the father or mother, severe physical illness of the father or the mother, chronically ill sibling; Cluster 5a (single or cumulative trauma): sexual abuse and physical maltreatment and emotional neglect. Similarly we recorded eight protective life events: Cluster 1p (social resources): good relationship with at least one primary caregiver, secure attachment behavior, extended family, compensatory parents relationship, good replacement milieu after an early mother loss, social promotion (e.g., school, church, reliable support reference person); Cluster 2p (individual resources): above average intelligence, robust active temperament, self-efficacy.
SSE-TAF (social self-sufficiency) is a validated (interrater reliability 0.73) part of the TAF documentation (TAF-DOK) and tries to document the social self-preservation ability of the family with one item (Bachler et al., 2014). The SSE TAF measures the ability to work and is a is based on a 5-tiered Likert scale.
Global Assessment of Psychosocial Functioning is used as measurement for scaling the individual competence-related and psychosocial functional level. It includes interpersonal and employment abilities and represents a one-dimensional depiction of a patient’s psychosocial functioning level (Soderberg et al., 2005). The rating ranges between 0 and 100. The interrater reliability has been reported with 0.74. A score of ≤50 indicates severe limitations.
The GARF scale was used to rate the psychosocial functioning level of the families (Stasch and Cierpka, 2006). The GARF detects three dimensions: (a) problem solving; (b) organization; and (c) emotional climate. The scaling occurs between 0 and 100. The interrater reliability is reported with 0.72, the Cronbach alpha with 0.91, and the generalizability coefficient (GC) with 0.93.
The data of the clinical sample was collected by the respective therapist of a family during the first 3 months of treatment. The non-clinical sample was drawn from two schools in Bavaria (Elementary School and High School), using the same methods as in the clinical sample. The non-clinical sample was matched (age and gender) according to the characteristics of the clinical group. For the statistical analyses (calculating mean, standard deviations, independent samples t-test, logistic binary regression, Pearson’s correlation coefficient, and linear regression analysis) IBM® SPSS® Statistics Premium GradPack 23 for Windows has been used.
There is no potential conflict of interest. This study was carried out in accordance with the recommendations of WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The investigation has been approved by the Ethics Committee of our Institutions (Institute for Psychoanalysis and Family Therapy Salzburg Austria).
In the clinical sample 95.7% of the cases met the ICD-10 criteria for at least one psychopathological diagnosis, compared to 21.6% in the non-clinical sample.
The mean number of CAs was 7.81 (SD = 3.18) for the clinical sample and 1.83 (SD = 2.08) for the non-clinical sample. Therefore, the clinical sample met on average 35.49% (SD = 14.48%) of 22 CAs, while the non-clinical sample did so for 8.35% (SD = 9.47%). Tested with an independent samples t-test, this constitutes a significant difference [t(1155) = 22.12, p < 0.001, d = 2.27], meaning that kids in the clinical sample had significant more CAs.
As can be seen on the left side of Figure 1, children in the clinical sample (solid line) were exposed to more risk factors as compared to the non-clinical sample (dashed line). In addition – as scan be seen on the right side of Figure 1 – persons in the clinical sample grew up with significantly less protective factors [clinical: M = 32.41%, SD = 18.1%; non-clinical: M = 69.53%, SD = 17.63%; independent samples t-test: t(1155) = -23.37, p < 0.001, d = -2.08].
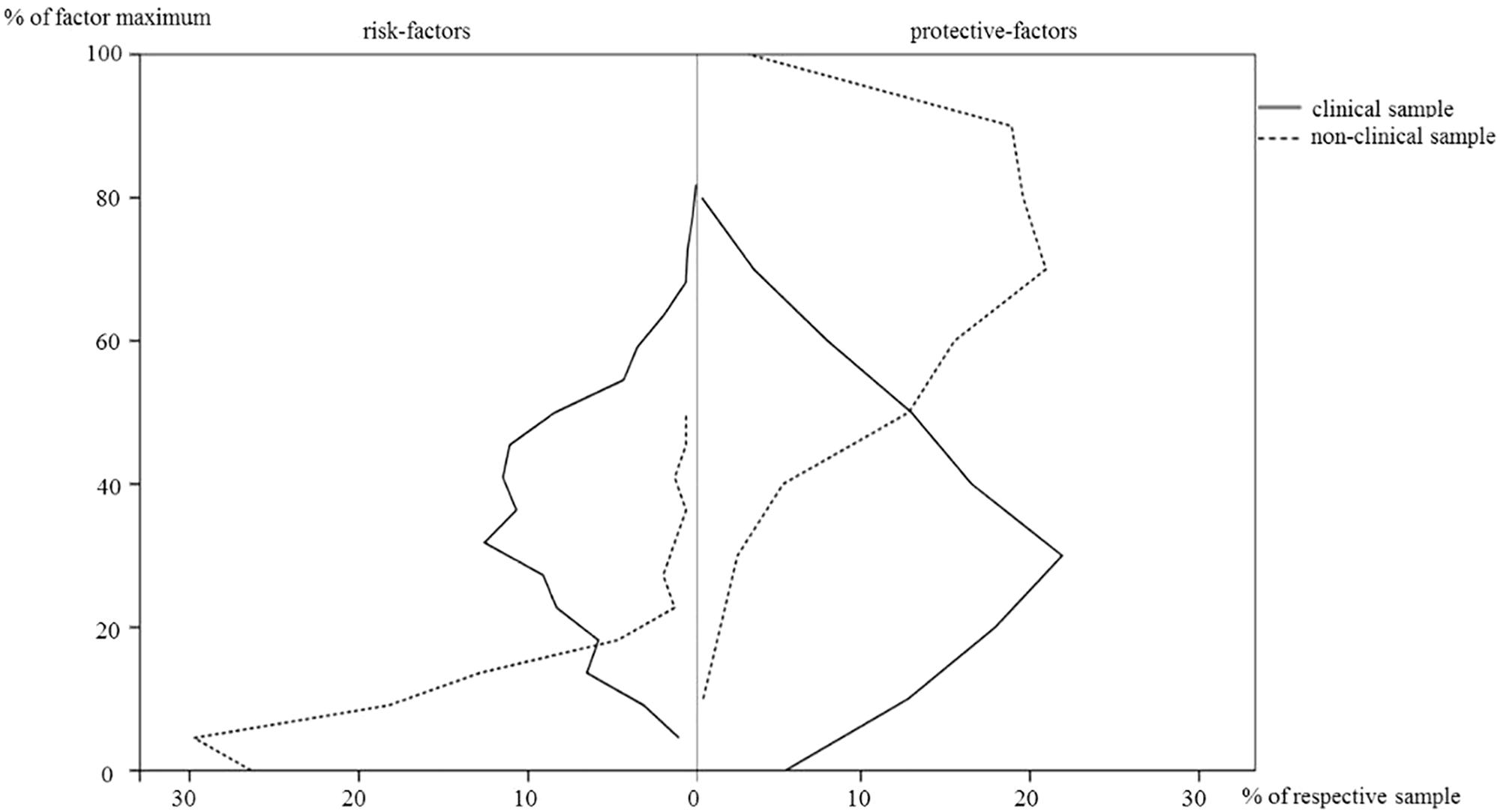
FIGURE 1. Percentages of corrected risk- and protective-factors in the clinical and non-clinical sample.
The three most prevalent CAs in the non-clinical sample were divorce or separation of parents (14.2%), employment of mother during first year after childbirth (21.2%) and a low SES (10.9%).
Cluster 5a (single or cumulative trauma): sexual abuse, physical maltreatment, and emotional neglect.
To test the relationship between the risk-/protective factors with the presence of a psychopathological diagnosis, we conducted a logistic binary regression. Both, CAs (B = 5.06, exp b = 158.01, p = 0.017) and protective factors (B = -0.34, exp b = 0.03, p = 0.006), turn out to be significant predictors for the existence/absence of a psychopathological diagnosis in the non-clinical sample [X2(1) = 18.0, p < 0.001; R2 = 0.177 (Nagelkerke, 1991), 0.112 (Cox and Snell, 1989)]. These results suggest that in a normal population of schoolchildren, protective factors make it significantly less likely to have a psychopathological diagnosis, while risk factors increase that chance significantly. In our non-clinical sample, children with a negative ratio of protective to risk factors had a 9.4% chance of meeting criteria for an ICD-10 diagnosis, while none (0%) of the kids with a positive ratio (more protective factors) did.
For the clinical sample, all psycho-social post treatment scores were significantly lower as compared to before treatment. The psychopathological symptoms as measured by Mannheim Parental Interview dropped from 12.57 (SD = 9.35) to 7.73 (SD = 7.69) after treatment, as can be seen in Figure 2. Tested with a paired samples t-test, that constitutes a significant reduction in psychopathologic symptoms [t(1000) = 18.94, p < 0.001; d = 0.61], even though the sample includes high rates of diagnoses like adolescent personality disorders and Asperger-syndrome with lower therapeutic variability. The family adversity index (FAI) significantly dropped from 2.33 (SD = 1.11) to 2.05 [SD = 1.12; t(1030) = 11.19, p < 0.001, d = 0.35]. The ability for social self-preservation (SSE-TAF) improved from 3.21 (SD = 1.24) to 2.94 [SD = 1.20; t(1029) = 10.05, p < 0.001, d = 0.31]. The three assessments of global functioning in terms of caregiver (GAF) [Mpre = 6.12, SD = 1.56, Mpost = 6.63, SD = 1.63; t(1030) = -14.52, p < 0.001, d = -0.45], index child caregiver (CGAF) [Mpre = 5.72, SD = 1.55, Mpost = 6.70, SD = 1.63; t(753) = -19.83, p < 0.001, d = -0.72] and relational functioning caregiver (GARF) [Mpre = 5.82, SD = 1.80, Mpost = 6.82, SD = 1.89; t(804) = -16.01, p < 0.001, d = -0.54] all also improved significantly.
The number of risk factors was significantly correlated to all measures related to psychological problems in the clinical sample (MPI: Pearson’s r = 0.17, p < 0.001; FAI: Pearson’s r = 0.46, p < 0.001; GAF: Pearson’s r = -0.3, p < 0.001; CGAF: Pearson’s r = -0.21, p < 0.001; GARF: Pearson’s r = -0.25, p < 0.001) and also in the non-clinical sample (MPI: Pearson’s r = 0.32, p < 0.001). The hypothesis that the higher the number of CAs – and therefore risk-factors – coincides with a higher number of psychopathological symptoms, was confirmed by a linear regression analysis [F(1,1007) = 30.29, p < 0.001]. The parameter of the risk-score significantly predicted the number of psychopathological symptoms [t(1007) = 11.24, p < 0.001]. With a R2 = 0.03 and the value b = 11.02, these results can be interpreted in a way, that for each two additional risk-factors, we can predict an increase of one point on the psychopathological symptom-score at the beginning of treatment, as measured by the MPI.
We did not find evidence for the hypothesis that higher risk-scores have a predictive value for the treatment effect [F(1,999) = 2.04, p = 0.154], suggesting that treatment is as effective for patients with high risk as it is for patients with only a few or no risk factors.
The protective-factors were significantly correlated to the number/severity of psychological problems, in the opposing direction of the risk-factors for the clinical sample (MPI: Pearson’s r = -0.26, p < 0.001; FAI: Pearson’s r = -0.18, p < 0.001; GAF: Pearson’s r = 0.23, p < 0.001; CGAF: Pearson’s r = 0.32, p < 0.001; GARF: Pearson’s r = 0.23, p < 0.001) and also in the non-clinical sample (MPI: Pearson’s r = -0.26, p < 0.001), constituting the exact complementary result of the risk factors. We tested the hypothesis that a higher number of protective factors predicts lower number of psychopathological symptoms. A linear regression analysis revealed that patients’ number of protective factors significantly predicted the pre-treatment scores of MPI [F(1,1007) = 73.31, p < 0.001]. The parameter of protective-factors with an R2 = 0.07 and b = -13.43 significantly predicted [t(1007) = -8.56, p < 0.001] that for each protective factor the psychopathological symptom-score can be expected to be 1.3 lower on average, constituting a buffering effect of protective-factors.
The hypothesis that the number of protective factors also predicts the number of symptoms after treatment was met in the opposite direction as previously hypothesized [F(1,999) = 10.94, p < 0.001]. With an R2 = 0.01 and a b = 4.63, the linear regression analysis significantly predicted [t(999) = 3.31, p = 0.001] that for each additional protective factor, the treatment will reduce 0.46 less symptoms. This might be interpreted in the light of the results that patients with more protective factors had less symptoms to start with at the beginning of treatment and therefore less chance to reduce these, as can be seen in Figure 2 and is reported in the next paragraph.
By subtracting the corrected risk-factors from the corrected protective factors, we separated the clinical sample into two groups of patients with predominance of risk-factors (risk-group, n = 556) and predominance of protective-factors (protective-group, n = 445), respectively.
As can be seen in Figure 2, the mean psychopathological symptoms of these two groups at beginning of treatment (risk-group: M = 14.58, SD = 9.53; protective-group: M = 10.07, SD = 8.48) differed significantly [t(1007) = 7.72, p < 0.001].
Even though both groups significantly reduce their psychopathology scores during treatment [risk-group: M = 9.16, SD = 8.23, t(555) = 14.53, p < 0.001; protective-group: M = 5.96, SD = 6.54, t(444) = 12.33, p < 0.001], there remains a significant difference between the two groups [t(999) = 6.69, p < 0.001] after treatment. The risk group – dotted line in Figure 2 – did show a trend for having a bigger total reduction of their symptoms [F(1,999) = 6.53, p = 0.011]. Taken together, patients with a higher number of CAs than protective factors showed more psychopathological symptoms before and after treatment, but had a tendency to reduce more of their symptoms, as compared to children that had more protective factors.
As can be seen in Table 2, the different clusters of protective- and risk factors correlated differently with psychopathological symptoms at beginning of the treatment. The cluster of attachment related risk-factors show the strongest relation to the symptoms (Pearson’s r = 0.24, p < 0.001), with the other clusters of violence (Pearson’s r = 0.12, p < 0.001) and trauma (Pearson’s r = 0.13, p < 0.001) to be also significantly correlated.
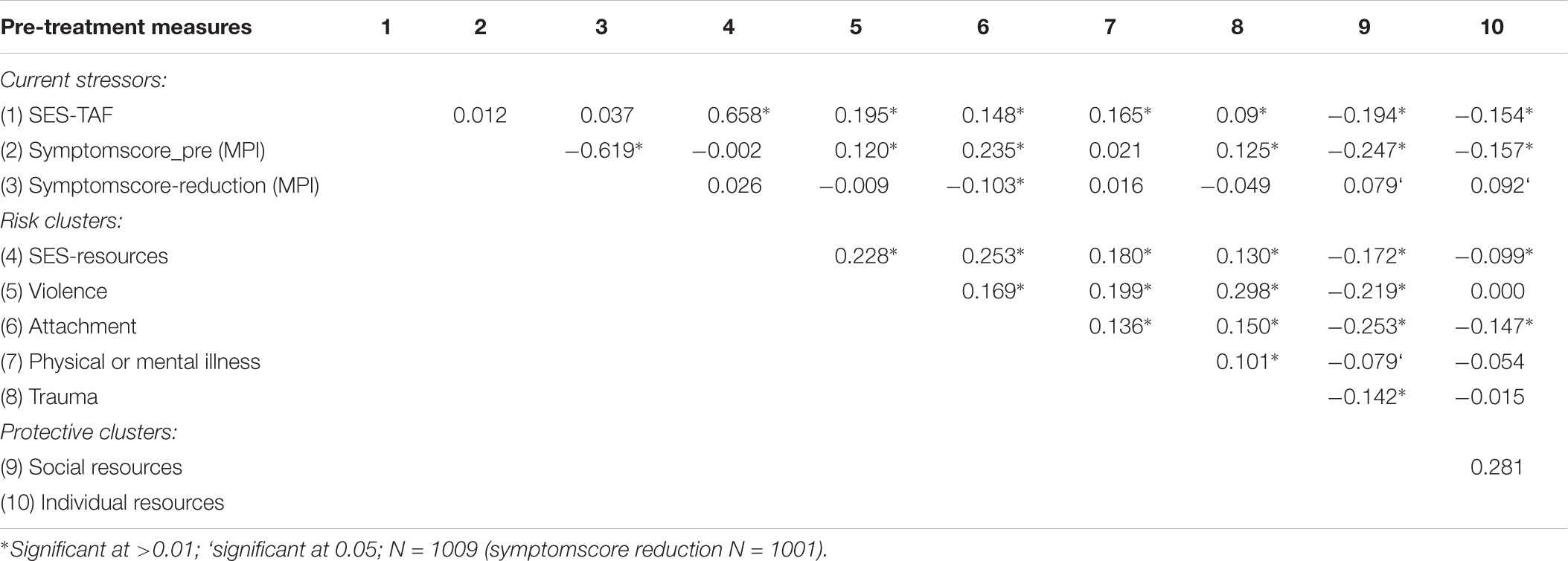
TABLE 2. Bivariate correlation matrix of current stressors (socio-economic status and psychopathology), childhood adversities (risk-clusters), and protective clusters.
Both clusters of the protective factors are significantly negative correlated with the symptom-score at beginning of treatment (social resources: Pearson’s r = -0.25, p < 0.001; individual resources: Pearson’s r = -0.16, p < 0.001).
Multi-problem families are often faced with a cross-generational, self-sustaining network of problems, where the social, educational, occupational, physical, and psychological maladaptation of one generation increase the risk of the family’s next generation. In our study, a representative sample of 148 children and adolescents from two schools were faced with an average of 1.84 (8.35% of 22) childhood-adversities, while a clinical sample of 1009 kids were exposed to a significant higher number of CAs (7.81; 35.49%). These children not only grow up under circumstances of heightened risk, they also have a significant lower number of positive, protective factors at their disposal (clinical sample: 32.41%; non-clinical: 69.53%). Children that meet the criteria of a psychopathological diagnosis will have encountered a smaller SES, more violence in the family, attachment-difficulties, more psychological and physical illness of their family members and are more likely to have gone through a traumatic experience, while they have less individual and social resources to cope with these adversities. In such an environment, psychopathology possibly has better chances to evolve and persist.
In addition, not only the presence of a diagnosis is more likely, but also the number of symptoms is significantly positive correlated with different clusters of CAs (and negatively correlated with the two protective clusters) in the clinical sample as well as in the non-clinical sample. For each two more CAs encountered in early life, the symptomatic score increases on average by one point when at the beginning of treatment. Each protective factor reduces that score by 1.3 points.
These results clearly support the notion that growing up in a family with multiple problems forms a thread to future psychological health of a child, but that fate is not irreversible. When undergoing psychotherapeutic treatment, as in the present clinical sample, the average patients – independently of their adverse or beneficial circumstances – benefit significantly from therapy. The treatment effect did not depend on the severity of disorders. To get a deeper understanding of the role, CAs and protective factors play in therapeutic processes, we divided the group of all patients into two groups that either had a predominance of adversities or protective factors. The group with more risk factors displayed a higher symptom-score before and after treatment. However, this group presented itself with an equally strong reduction of symptoms after therapy. In fact, the symptomatic drop was almost stronger for the risk-group, which, however, has to be interpreted in the light of having started out with more symptoms.
Combined, these results of therapeutic effectiveness shed a positive light on the question, whether the cross generational network of problems can be dismantled. Knowing that therapy even in severe circumstances is possible, not only demands public investment into therapy for the young person at hand, but is publicly even more beneficial, since it is likely to cut the cross-generational inheritance of adverse living conditions. That argument is supported by the comparison of a clinical sample with a non-clinical sample, where it could be shown that the chances for developing a psychopathology decreases with the decrease of CAs and increase of protective factors in early life.
The understanding of the etiology of psychological problems needs to take into account the framework of CAs and their interaction with protective factors. The individual risk of developing mental health problems is possibly caused by individual vulnerability, personal and family-related resources (PFs), as well as by the age, frequency, the duration and the accumulation of various risk factors. However, even when a kid grows up in bad circumstances and does develop psychopathological symptoms, therapy is possible and with high outcome values. Adaptive treatments can prevent disorder-related long-term effects and can decrease family related indices of CAs (FAI, d = 0.35). Our study showed that therapeutic home-based treatment with high structural and process quality can successfully treat groups with severe child-psychiatric disorders. But we need further research about treatment aptitude and “what works for whom” (Beutler et al., 2016).
Our data allow us to point out the importance of CAs × PFs interactions as a framework to explain individual differential susceptibility for environmental influences in G × E interaction. This will have relevance for preventive and curative interventions in child-protection, and health policy pay off, because the direct and indirect costs of CAs over the course of lifetime are very high (Masten, 2011). The costs of the developmental effects of serious child maltreatment exceeds 210.000$ per victim (Klika and Herrenkohl, 2013). Empirical research about these issues are important because the long-term effects of CAs are harmful and costly. We can summarize that the development of child psychiatric symptoms is determined by the complexity of a number of genetic, epigenetic, and different environmental influences (socio-familial, socioeconomic factors, and by CAs × PFs interactions) with non-additive influence at different stages of age.
Three important tasks can be derived from the presented results: First, families, neighbors, schools, social services and governments have to take action to prevent, screen and if necessary, act quickly on harsh conditions in and for families, for not allowing to have violence and rates of early life stressors dominate childrens’ life’s (Flouri et al., 2015; Bethell et al., 2016). Second, more empirical research has to be conducted, to better understand dysfunction specific resilience mechanisms and underlying gene–environment interactions. The regulating function of the HPA axis and in consequence long-term functionality of the brain is, e.g., just one mechanism, how early uninterrupted life-stressors might have a lasting influence (Bick et al., 2012). Third, generalizing research on groups has to be expanded by designs that allow a better understanding of which treatment might help whom and when the best. Therefore our empirical study is a contribution to treatment aptitude research (Beutler et al., 2016).
Even though we had three sources of data with high reliability to the assessment of the CAs (primary care giver, adolescents, and therapists), retrospective assessment has possible biases in terms of under-reporting (memory) or over-reporting (trying to please the interviewer). Furthermore, the study has a naturalistic design, the treatments were conducted as usual, with adherence check for the interventions. Therefore, causal interpretations, are, in a strict sense, not possible.
All authors designed the study and proofread the literature. BA was responsible for statistics. EB and AF collected the data. EB, HB, MN, and GS wrote the paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We are grateful to the European Union and to the Land Salzburg, Land Upper Austria the Government of Upper Bavaria, which provided financial support (EFRE funds J00111) on this empirical research about MPF.
Andershed, A. K., and Andershed, H. (2015). Risk and protective factors among preschool children: integrating research and practice. J. Evid. Inf. Soc. Work 12, 412–424. doi: 10.1080/15433714.2013.866062
Bachler, E., Fruehmann, A., Bachler, H., Aas, B., Nickel, M., and Schiepek, G. K. (2017). Patterns of change in collaboration are associated with baseline characteristics and predict outcome and dropout rates in treatment of multi-problem families. A validation study. Front. Psychol. 8:1221. doi: 10.3389/fpsyg.2017.01221
Bachler, E., Frühmann, A., Strunk, G., Aas, B., Bachler, H., and Nickel, M. (2014). Differential effects of the working alliance in family therapeutic home-based treatment of multi-problem families. J. Fam. Ther. 28, 120–148. doi: 10.1111/1467-6427.12063
Bakermans-Kranenburg, M. J., and van Ijzendoorn, M. H. (2006). Gene-environment interaction of the dopamine D4 receptor (DRD4) and observed maternal insensitivity predicting externalizing behavior in preschoolers. Dev. Psychobiol. 48, 406–409. doi: 10.1002/dev.20152
Belfer, M. L. (2008). Child and adolescent mental disorders: the magnitude of the problem across the globe. J. Child Psychol. Psychiatry 49, 226–236. doi: 10.1111/j.1469-7610.2007.01855.x
Bentall, R. P., de Sousa, P., Varese, F., Wickham, S., Sitko, K., Haarmans, M., et al. (2014). From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc. Psychiatry Psychiatr. Epidemiol. 49, 1011–1022. doi: 10.1007/s00127-014-0914-0
Bethell, C., Gombojav, N., Solloway, M., and Wissow, L. (2016). Adverse childhood experiences, resilience and mindfulness-based approaches: common denominator issues for children with emotional, mental, or behavioral problems. Child Adolesc. Psychiatr. Clin. N. Am. 25, 139–156. doi: 10.1016/j.chc.2015.12.001
Beutler, L. E., Someah, K., Kimpara, S., and Miller, K. (2016). Selecting the most appropriate treatment for each patient. Int. J. Clin. Health Psychol. 16, 99–108. doi: 10.1016/j.ijchp.2015.08.001
Bick, J., Naumova, O., Hunter, S., Barbot, B., Lee, M., Luthar, S. S., et al. (2012). Childhood adversity and DNA methylation of genes involved in the hypothalamus-pituitary-adrenal axis and immune system: whole-genome and candidate-gene associations. Dev. Psychopathol. 24, 1417–1425. doi: 10.1017/S0954579412000806
Bornstein, M., and Bradley, R. (2003). Socioeconomic Status, Parenting and Child Development. Monographs in Parenting. New York, NY: Psychology Press.
Cabaj, J. L., McDonald, S. W., and Tough, S. C. (2014). Early childhood risk and resilience factors for behavioural and emotional problems in middle childhood. BMC Pediatr. 14:166. doi: 10.1186/1471-2431-14-166
Cicchetti, D., and Rogosch, F. A. (2012). Gene x Environment interaction and resilience: effects of child maltreatment and serotonin, corticotropin releasing hormone, dopamine, and oxytocin genes. Dev. Psychopathol. 24, 411–427. doi: 10.1017/S0954579412000077
Critchfield, K. L., and Benjamin, L. S. (2006). “Integration of therapeutic factores in treating personality disorders,” in Priciples of Therapeutic Change that Work, eds L. G. Castonguay and L. E. Beutler (New York, NY: Oxford University Press), 253–271.
Curtis, N. M., Ronan, K. R., and Borduin, C. M. (2004). Multisystemic treatment: a meta-analysis of outcome studies. J. Fam. Psychol. 18, 411–419. doi: 10.1037/0893-3200.18.3.411
Edwards, R. C., and Hans, S. L. (2015). Infant risk factors associated with internalizing, externalizing, and co-occurring behavior problems in young children. Dev. Psychol. 51, 489–499. doi: 10.1037/a0038800
Egle, U., Hoffmann, S. O., and Joraschky, P. (2004). Sexueller Missbrauch, Misshandlung Vernachlässigung. Erkennung Therapie und Prävention der Frühen Stresserfahrung. [Sexual Abuse, Neglect, Deprivation. Recognition Treatment and Prevention of Early Stress Experience]. Stuttgart: Schattauer.
Esser, G., Blanz, B., Geisel, B., and Laucht, M. (1989). Mannheimer Eltern-Interview. Beltz: Hogrefe-Verlag.
Flouri, E., Midouhas, E., Joshi, H., and Tzavidis, N. (2015). Emotional and behavioural resilience to multiple risk exposure in early life: the role of parenting. Eur. Child Adolesc. Psychiatry 24, 745–755. doi: 10.1007/s00787-014-0619-7
Hartman, S., and Belsky, J. (2016). An evolutionary perspective on family studies: differential susceptibility to environmental influences. Fam. Process 55, 700–712. doi: 10.1111/famp.12161
Haushofer, J., and Fehr, E. (2014). On the psychology of poverty. Science 344, 862–867. doi: 10.1126/science.1232491
Hengartner, M. P., Muller, M., Rodgers, S., Rossler, W., and Ajdacic-Gross, V. (2013). Can protective factors moderate the detrimental effects of child maltreatment on personality functioning? J. Psychiatr. Res. 47, 1180–1186. doi: 10.1016/j.jpsychires.2013.05.005
Kessler, R. C., McLaughlin, K. A., Green, J. G., Gruber, M. J., Sampson, N. A., Zaslavsky, A. M., et al. (2010). Childhood adversities and adult psychopathology in the WHO world mental health surveys. Br. J. Psychiatry 197, 378–385. doi: 10.1192/bjp.bp.110.080499
Kim, P., Evans, G. W., Angstadt, M., Ho, S. S., Sripada, C. S., Swain, J. E., et al. (2013). Effects of childhood poverty and chronic stress on emotion regulatory brain function in adulthood. Proc. Natl. Acad. Sci. U.S.A. 110, 18442–18447. doi: 10.1073/pnas.1308240110
Klasen, F., Otto, C., Kriston, L., Patalay, P., Schlack, R., Ravens-Sieberer, U., et al. (2015). Risk and protective factors for the development of depressive symptoms in children and adolescents: results of the longitudinal BELLA study. Eur. Child Adolesc. Psychiatry 24, 695–703. doi: 10.1007/s00787-014-0637-5
Klika, J. B., and Herrenkohl, T. I. (2013). A review of developmental research on resilience in maltreated children. Trauma Violence Abuse 14, 222–234. doi: 10.1177/152483801348780
Lund, C., De Silva, M., Plagerson, S., Cooper, S., Chisholm, D., Das, J., et al. (2011). Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet 378, 1502–1514. doi: 10.1016/S0140-6736(11)60754-X
Luo, Y., and Waite, L. J. (2005). The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. J. Gerontol. B Psychol. Sci. Soc. Sci. 60, S93–S101. doi: 10.1093/geronb/60.2.S93
Masten, A. S. (2011). Resilience in children threatened by extreme adversity: frameworks for research, practice, and translational synergy. Dev. Psychopathol. 23, 493–506. doi: 10.1017/S0954579411000198
McDonald, S., Kehler, H., Bayrampour, H., Fraser-Lee, N., and Tough, S. (2016). Risk and protective factors in early child development: results from the all our babies (AOB) pregnancy cohort. Res. Dev. Disabil. 58, 20–30. doi: 10.1016/j.ridd.2016.08.010
Mitchell, C., McLanahan, S., Brooks-Gunn, J., Garfinkel, I., Hobcraft, J., and Notterman, D. (2013). Genetic differential sensitivity to social environments: implications for research. Am. J. Public Health 103(Suppl. 1), S102–S110. doi: 10.2105/AJPH.2013.301382
Moore, S. R., and Depue, R. A. (2016). Neurobehavioral foundation of environmental reactivity. Psychol. Bull. 142, 107–164. doi: 10.1037/bul0000028
Nagelkerke, N. (1991). A note on a general definition of the coefficient of determination. Biometrika 78, 691–692. doi: 10.1093/biomet/78.3.691
Putnam, K. T., Harris, W. W., and Putnam, F. W. (2013). Synergistic childhood adversities and complex adult psychopathology. J. Trauma. Stress 26, 435–442. doi: 10.1002/jts.21833
Rasmussen, C. S., Nielsen, L. G., Petersen, D. J., Christiansen, E., and Bilenberg, N. (2014). Adverse life events as risk factors for behavioural and emotional problems in a 7-year follow-up of a population-based child cohort. Nord. J. Psychiatry 68, 189–195. doi: 10.3109/08039488.2013.794473
Reichl, C., Kaess, M., Resch, F., and Brunner, R. (2014). [The role of genotype in the intergenerational transmission of experiences of childhood adversity]. Z. Kinder Jugendpsychiatr. Psychother. 42, 349–359. doi: 10.1024/1422-4917/a000310
Rutter, M., and Quinton, D. (1977). “Psychiatric disorder ecological factors and concepts of causation,” in Ecological Factors in Human Development, ed. M. McGurk (Amsterdam: North Holland), 173–187.
Schilling, E. A., Aseltine, R. H., and Gore, S. (2008). The impact of cumulative childhood adversity on young adult mental health: measures, models, and interpretations. Soc. Sci. Med. 66, 1140–1151. doi: 10.1016/j.socscimed.2007.11.023
Slopen, N., McLaughlin, K. A., and Shonkoff, J. P. (2014). Interventions to improve cortisol regulation in children: a systematic review. Pediatrics 133, 312–326. doi: 10.1542/peds.2013-1632
Soderberg, P., Tungstrom, S., and Armelius, B. A. (2005). Reliability of global assessment of functioning ratings made by clinical psychiatric staff. Psychiatr. Serv. 56, 434–438. doi: 10.1176/appi.ps.56.4.434
Stasch, M., and Cierpka, M. (2006). Beziehungsdiagnostik mit der GARF Skala. Psychotherapeut 11, 56–63.
Witkiewitz, K., King, K., McMahon, R. J., Wu, J., Luk, J., Bierman, K. L., et al. (2013). Evidence for a multi-dimensional latent structural model of externalizing disorders. J. Abnorm. Child Psychol. 41, 223–237. doi: 10.1007/s10802-012-9674-z
Wittchen, H. U., and Jacobi, F. (2005). Size and burden of mental disorders in Europe–a critical review and appraisal of 27 studies. Eur. Neuropsychopharmacol. 15, 357–376. doi: 10.1016/j.euroneuro.2005.04.012
Woolfenden, S. R., Williams, K., and Peat, J. (2001). Family and parenting interventions in children and adolescents with conduct disorder and delinquency aged 10-17. Cochrane Database Syst. Rev. 2:CD003015. doi: 10.1002/14651858.CD003015
Keywords: protective factors, multi problem family, childhood adversities, outcome research evaluation, family therapies
Citation: Bachler E, Frühmann A, Bachler H, Aas B, Nickel M and Schiepek GK (2018) The Effect of Childhood Adversities and Protective Factors on the Development of Child-Psychiatric Disorders and Their Treatment. Front. Psychol. 9:2226. doi: 10.3389/fpsyg.2018.02226
Received: 03 October 2017; Accepted: 26 October 2018;
Published: 15 November 2018.
Edited by:
Alexander Libin, MedStar Health Research Institute (MHRI), United StatesReviewed by:
Hans Menning, University of Zurich, SwitzerlandCopyright © 2018 Bachler, Frühmann, Bachler, Aas, Nickel and Schiepek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Egon Bachler, ZHIuZWdvbi5iYWNobGVyQHQtb25saW5lLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.