Abstract
The field of Clinical Research, like many other scientific disciplines, has struggled to recruit and retain talented researchers from diverse communities. While there is a strong history of documenting the problem, having a diverse and inclusive workforce is hindered by the lack of data-driven approaches, cross-institutional partnerships, access to mentors, and positive immersive experiences for people from underrepresented groups. Here, we describe a novel initiative for North Carolina Central University Clinical Research Sciences Program (NCCU-CRSP) student interns to partner with Duke University to have immersive clinical and pre-clinical research training in a 15-week internship as the culminating experience towards their degree for a Bachelor of Science in Clinical Research. The goals of the internship are: 1) to give hands-on training to enhance the impact of classroom-based learning, 2) broaden their understanding of the wide swath of positions available to them, 3) promote their sense of self-efficacy, confidence, science identity, research identity, and connections to the pre-clinical and clinical community, and 4) prepare them to be workforce ready upon graduating. The students dedicate 75% of their time to clinical research with Duke University at Pickett Road and 25% to pre-clinical research in the Collective for Psychiatric Neuroengineering in the Duke Psychiatry Department of the School of Medicine. They will also receive eight 1-h professional development training sessions from the Duke-NCCU Clinical and Translational Science Initiative’s Workforce Development Team and five 1-h sessions based on the Entering Research Curriculum developed by the Center for the Improvement of Mentored Experiences in Research (CIMER). Finally, they will be brought in as a cohort and coached on peer mentoring and mutual support frameworks to enhance their sense of community. These student-interns will perform pre- and post-internship self-assessment surveys to quantify their self-efficacy, feelings of belonging, access to research opportunities and mentors, and to give details of their future education and career goals. We will evaluate the impact of the internship using validated tools and apply these findings for future optimization of program design and tactical advice for other programs with shared missions. Furthermore, we will email them on an annual basis with follow-up surveys to assess the longitudinal impact of this internship program, their educational experiences at NCCU, what job titles they hold, how prepared they feel for their roles, and what they hope their future career trajectory will be. Collectively, these approaches will apply theoretical frameworks developed by social and cognitive psychology, vocational theory, and educational research to clinical research training with the goals of recruiting and training talented and diverse leaders within clinical research. We hope that by evaluating our successes, failures, strengths, and liabilities through empirically derived evidence we will also inspire future studies that use data-driven approaches to elevate our approaches as we work together to train and recruit talented researchers from diverse communities into our scientific enterprise and to launch them with more in-depth experiential learning that will empower them to succeed.
Introduction
The field of clinical research has identified an immense need to develop a more diverse and inclusive workforce (Locklear et al.; NSF, 2022). While Black, African American, Latino/a, Hispanic, Indigenous, and Native individuals comprise more than 30% of the US population, they comprise less than 19% of bachelor’s degrees and 15% of PhDs in biological sciences, thereby designating them as Historically Underrepresented (HU) groups (Statistics, 1994; NSF, 2022). Furthermore, the significant lack of diverse representation amongst clinical trial participants can drive a slew of problems, including compromising the generalizability of clinical research findings, undermining trust in the medical establishment and research community, and compounding health disparities (Improving Representation, 2022). There are ample emerging data illuminating how important physician-patient race concordance is, particularly in the context of boosting health service utilization and reducing infant mortality rates (LaVeist et al., 2003; Alsan et al., 2018; Greenwood et al., 2020). Similarly, studies have shown that more diverse personnel at clinical trial workplaces correlates to increased diversity in patients recruited to studies and African American women report to be more motivated to join studies if there is race concordance with the practitioners of the study (Frierson et al., 2019; Tufts Center for the Study of Drug Development, 2021). While many have identified the issues of a lack of diversity in the clinical research workforce and have measured its scope, novel and innovative tactics are required if we want to make real change (Byars-Winston et al., 2011; Valantine and Collins, 2015; Byars-Winston et al., 2016; Hitchcock et al., 2017; Winn Ariel et al., 2019). The number of clinical trials and the scope of clinical research are rapidly expanding, which requires an influx of workforce-ready individuals into our field if we aim to keep up with demand (US National Library of Medicine). We need education, training, and workforce development approaches paired with high-quality assessments to quantify the impact of interventions on 1) diversifying our field and 2) increasing the number of workforce-ready applicants to meet the ever-expanding needs of the field. Our methods must overcome the long-standing legacies of systemic inequality and structural racism to improve access to the education, training, and mentoring required for a robust career in clinical research. The time has come for large-scale investments to build sustainable, multifaceted, and empowered training programs that will equip the next-generation of diverse leaders in clinical science to achieve their goals and contribute to transformative breakthroughs.
We are fortunate to live in a time where there is tremendous innovation around how to evaluate the impact of educational interventions to improve diversity, equity, and inclusion outcomes. Specifically, six key domains have been empirically shown to improve retaining diverse individuals in the research enterprise: 1) development of scientific identity, 2) development of research identity, 3) increased self-efficacy, 4) improved sense of belonging, 5) expanding expected outcomes, and 6) good mentorship (Bakken et al., 2006; Graham et al., 2013; Byars-Winston et al., 2016; Winn Ariel et al., 2019). In this perspective article, we detail a pioneering internship program at the interface of Duke University clinical and pre-clinical research and North Carolina Central University (NCCU), a predominantly Black university located five miles away from Duke. 95% of NCCU students come from underrepresented racial and ethnic backgrounds and 61% of students were awarded Pell Grants last year, thus this group of students is a significantly more diverse population of individuals than the current population of clinical research professionals. Furthermore, we describe the implementation of validated tools to assess the impact of the internship on the six key domains described above that have been previously shown to promote recruitment and retention into any field. Through this pilot project, we hope to build long-term sustainability for our student interns and to contribute to a moonshot goal of diversifying the clinical research workforce to reflect the US population demographics by 2030 through data-driven approaches that promote equity and inclusion of talented, diverse leaders within the field of clinical research (Envisioning a TransformedBoard on Health Sciences PolicyHealth and Medicine DivisionNational Academies of Sciences et al., 2021).
Program design and methodology
This perspective article presents a novel approach for a capstone internship experience for seniors graduating with a Bachelor of Science in Clinical Research from NCCU. We apply adapted tools to assess the impact this experience has on the six key domains that have been shown to improve recruitment and retention in communities and vocational tracks for other fields. The intern participants will gain multifaceted, cross-institutional experiences in which they dedicate 75% of their time to clinical research with Duke University at Pickett Road paired with a Clinical Research Coordinator doing an NIH funded study. The other 25% of their time will be devoted to conducting pre-clinical research in the Collective for Psychiatric Neuroengineering focused on genetic engineering and gene therapy principles. In both settings, they will conduct rigorous analyses of the literature, develop technical skills, and work collaboratively to achieve progress in their respective studies. They will also receive eight 1-h sessions of professional development training from the Duke-NCCU Clinical and Translational Science Initiative’s Workforce Development Team and five 1-h sessions based on the Entering Research Curriculum developed by the Center for the Improvement of Mentored Experiences (Balster et al., 2010). The student interns will be brought in as a cohort and coached on peer mentoring and mutual support frameworks to enhance their sense of community. There will also be a network of formal and informal mentors who are specifically dedicated to improving their technical and interpersonal skills for success in the clinical research workforce.
Traditionally, there are no required educational backgrounds or specific competencies to become a clinical research professional. However, there are still stark diversity and equity issues in the field. There is mounting pressure to grow the clinical research workforce as the number of registered trials increases. However, strictly adding more people won’t solve all the field’s issues. If we aim to promote equity to reduce health disparities, we must maintain a steadfast focus on the goals: 1) growing this workforce, 2) recruiting talent from diverse communities, and 3) enhancing feelings of belonging and inclusion to retain individuals from diverse backgrounds throughout the process. The NCCU Clinical Research Science Program aims to create a robust curriculum that trains students from diverse backgrounds to develop core competencies that will empower them to be leaders in clinical research. In addition to their classroom training in pursuit of a Bachelor of Science, this internship program aims to facilitate them gaining professional skills, confidence, self-efficacy, sense of belonging, and to promote their identity as top-tier researchers and scientists. We hope to empower a well-qualified cohort of students to obtain roles as clinical research professionals with strong skills in core competency domains that the Joint Task Force for Clinical Trial Competency and Clinical Research Professional Workforce Development has recently developed (Sonstein and Jones, 2018).
While we have trained to the competencies outlined in the article above, the learning objectives for the internship are to test the “workability” of our cohort, specifically as follows.
1) Be able to follow Good Clinical Practices in the conduct of clinical research
2) Understand and describe the roles of various clinical research professionals within the clinical research team
3) Apply professionalism and interpersonal skills to ensure success in clinical and scientific workplaces
4) Build skillsets in quantitative research
5) Apply literature review skills to develop and share new knowledge in clinical and scientific research workplace
6) Execute well-researched presentations with confidence
7) Incorporate professional and research experiences into resumes and increase marketability of the scholars
Importantly, we will administer in-depth pre- and post-evaluations that rely on validated tools to determine the impact of our intervention on promoting recruitment and inclusion in a field (Gloria and Kurpius, 2001; Hurtado et al., 2007; Byars-Winston et al., 2011; Trujillo and Tanner, 2014; Byars-Winston et al., 2016). From these self-assessment surveys, we will quantify their changes in self-efficacy, feelings of belonging, access to research opportunities, access to research mentors, detail their future career goals, and use qualitative and quantitative measures to assess their confidence, comfort, and expectations of success within the clinical research field (Table 1). By doing so before and after the internship experiences of multiple cohorts, we will develop a robust understanding of the impact of this internship experience on our student interns with depth and nuance based on empirical evidence. Additionally, we will query the internship preceptors for each student to evaluate the interns’ skills, growth, and readiness to enter the workforce. Finally, we will do an annual survey following up with each intern to determine their career trajectory longitudinally and to ask how ready they felt to take on their new positions, to climb the career ladder in Clinical Research, and to determine if they were retained long-term in the field.
TABLE 1
| Self-efficacy |
|---|
| Confidence in conducting high quality clinical research |
| Confidence in understanding how a biology laboratory operates |
| Confidence in molecular biology techniques in the laboratory |
| Confidence in understanding and describing the roles of various clinical research professionals within a clinical research team |
| Confidence with applying good clinical practices to clinical research |
| Confidence in your capacity to succeed in clinical or pre-clinical research |
| Confidence in yourself professionally, in general |
| Confidence in talking about clinical research with other professionals |
| Confidence in talking about pre-clinical research with other professionals |
| Confidence in applying statistics to a research question |
| Confidence conducting quantitative research |
| Confidence conducting a literature review |
| Confidence applying a literature review to share knowledge with others in the workplace |
| Confidence in executing a well-researched presentation |
| Confidence in applying to your first job after you graduate |
| Confidence in having a strong career in clinical research that supports your goals in life |
| Sense of belonging |
|---|
| Comfort level in a scientific lab |
| Comfort level in a clinical research setting |
| Comfort level in any professional work setting |
| Satisfaction with access to clinical research opportunities |
| Satisfaction with access to clinical research mentors |
| Access to opportunities and mentors in clinical research. |
| Expected outcomes |
|---|
| A clinical research career would allow me to work that makes a difference in people's lives or society. |
| A clinical research career would allow me to work that I find satisfying |
| A clinical research career would allow me to go into a field with high employment demand |
| A clinical research career would allow me to get respect from other people |
| A clinical research career would allow me to earn an attractive salary. |
| How important do you think it is to have clinical research mentors? |
| How important do you think internships are to your Confidence in yourself? |
| How important do you think it is to have access to role models? |
| How important do you think it is to have peer colleagues in your STEMM career? |
| Clinical research Identity |
|---|
| Current Major |
| Future plans for higher education |
| Future plans for job titles to hold |
| I can picture myself being successful as a clinical science researcher |
| I am already successful as a clinical science researcher |
| Access to mentors and experiences |
|---|
| Clinical research scientist mentor numbers and frequency of contact |
| Hands-on research experience in clinical research opportunities |
| Pre-clinical research scientists mentor numbers and frequency of contact |
| Clinical research or pre-clinical research workplace access |
| Pre-clinical research science mentor numbers and frequency of contact |
| Clinical or pre-clinical research internship access |
Variables to be evaluated through pre- and post-assessments of student interns in the NCCU Clinical Research Science Program.
Many of these key focus areas overlap with the goals of the Joint Task Force for Clinical Competencies Domains (Figure 1) (Sonstein and Jones, 2018). We will develop their skills for Competency 1: Scientific Concepts and Research Design in both the Clinical Research at Pickett Road and the Pre-Clinical Molecular Neuroscience Research with the Collective for Psychiatric Neuroengineering by giving hands-on research experiences, helping interns to design experiences, analyze the literature, develop technical and interpersonal expertise to accomplish the goals of their research, and to take pieces of the studies from conception to execution and analysis. They will have thorough Ethical Training which aligns with Domain 2, including engaging in the Entering Research Curriculum (focusing on case studies of responsible conduct in research, setting expectations, and ethics discussions), attending an IRB meeting, and online learning with Clinical Research Coordinators and Experimental Scientists daily. We are giving them hands-on training to apply what they’ve learned in the classroom regarding Competency 4: Good Clinical Practice and Operations in the Clinical Research Setting. By promoting self-efficacy, a sense of belonging, and scientific identity in our students, we empower them to develop Competency 7: Leadership and Professionalism and Competency 8: Communication and Teamwork. We are further supporting Competency 8 through immersive experiences where they must work as a team to solve problems, give presentations, and develop their collaboration skills to accomplish the assigned tasks as an internship cohort. Taken together, we aim to integrate the advice and direction from Clinical Research and Research Mentorship experts to provide a holistic internship experience that will empower our students to be workforce-ready by up-skilling them in the key domains identified by this highly respected council.
FIGURE 1
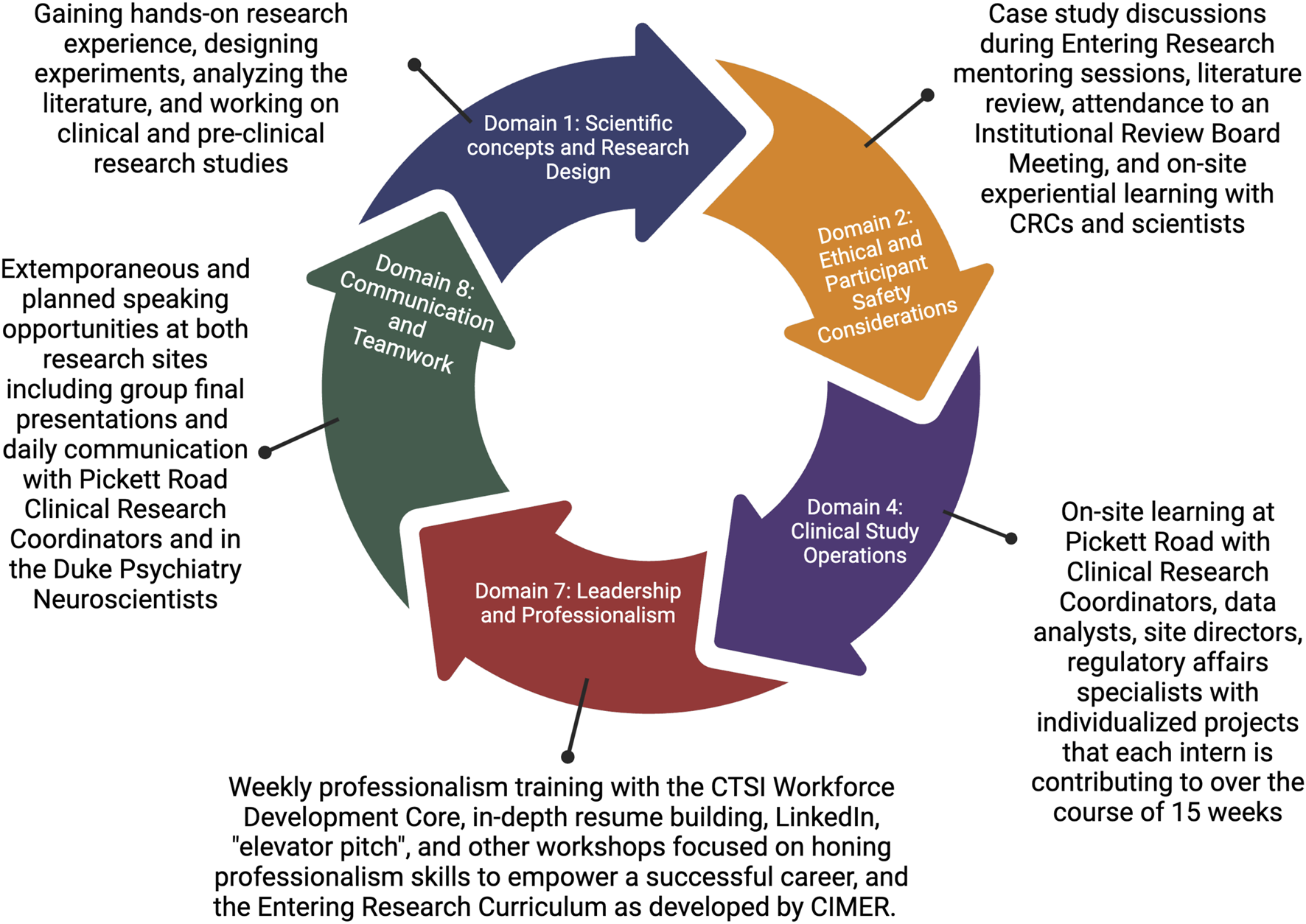
Joint Task Force key competency domains for clinical research and their alignment with internship activities.
Discussion and future remarks
Our mission is to develop a clinical research training program that diversifies the field through a robust understanding of the strengths and liabilities of our approach over multiple cohorts. This depth of understanding will be mission-critical to maximize our capacity to empower our student interns to become leaders in clinical research. We aim to apply the powerful tools and foundational theoretical frameworks that leaders in vocational psychology have developed in response to the critical need to increase the number of workforce-ready clinical researchers while concurrently diversifying the workforce. Analyzing our impact along the way will allow for iterative design to optimize our program in the future. We will use the gained knowledge to generate tactical advice for other programs with shared missions for the mutual edification of our programs.
Additionally, we will follow our interns longitudinally throughout their career trajectories to allow us to develop systems to assess the long-term impact interventions have on retention. In the near future, we also aim to query future employers as to how “job-ready” the graduates from our program were compared to other competitive applicants and what their primary foci are in the hiring process into their field. Finally, we will continue to document this journey and raise funds for this training program to bring about awareness and promote sustainability that will allow for a larger and more meaningful impact on future cohorts and larger participant pools.
While these strategies may only provide a partial solution to the long-standing systems of inequality that we must overcome, they provide three key improvements: 1) a framework that can be utilized and repurposed as we collectively work to recruit, train, and retain diverse researchers in clinical research (or other fields), 2) the application of vocational psychology theoretical frameworks to clinical research training opportunities as a novel synergistic integration of the fields, and 3) an opportunity to continue to revise our training models based on data-driven insights. If successful, we will contribute to the intentional deconstruction of systemic barriers that have historically driven health, economic, and educational inequalities that have held us back as a society and as a clinical research field.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
JD: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review and editing. KD: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing–review and editing. TL: Conceptualization, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This project is funded in part by CTSA grant UL1TR002553 for the Workforce Development Core and Howard Hughes Medical Investigators.
Acknowledgments
The authors would like to thank Amanda McMillan, Taryn Cavanaugh Faulk, Debra Freedman, Dr. Gentzon Hall, Johnathan Williford, and all other members of the Duke Clinical and Translational Research Workforce Development Core, Duke Pickett Road Clinical Research Site, North Carolina Central University Institutional Review Board, and members of the Collective for Psychiatric Neuroengineering that contributed invaluable support of the internship program. We would also like to thank Dr. Faye Calhoun, Dr. Lisa Davis, Dr. Jonathan Livingston, and Mr. William Smith for their invaluable support of our students and promoting equity and accessibility within this program and their leadership on the insurance and data accessibility at Duke. We would like to acknowledge Dr. Andy Li, and Ms. Roslyn Lewis, co-developers of the CRSP program, for their contributions to the curriculum, course development, and student training.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1
AlsanM.GarrickO.GrazianiG. C. (2018). Does diversity matter for health? Experimental evidence from Oakland (Working Paper 24787). Natl. Bureau Econ. Res. 10.3386/w24787
2
BakkenL. L.Byars-WinstonA.WangM.-F. (2006). Viewing clinical research career development through the lens of social cognitive career theory. Adv. Health Sci. Educ. Theory Pract.11, 91–110. 10.1007/s10459-005-3138-y
3
BalsterN.PfundC.RediskeR.BranchawJ. (2010). Entering research: a course that creates community and structure for beginning undergraduate researchers in the STEM disciplines. CBE Life Sci. Educ.9, 108–118. 10.1187/cbe.09-10-0073
4
Byars-WinstonA.GutierrezB.ToppS.CarnesM. (2011). Integrating theory and Practice to increase scientific workforce diversity: a framework for career development in graduate research training. CBE—Life Sci. Educ.10, 357–367. 10.1187/cbe.10-12-0145
5
Byars-WinstonA.RogersJ.BranchawJ.PribbenowC.HankeR.PfundC. (2016). New measures assessing predictors of academic persistence for historically underrepresented racial/ethnic undergraduates in science. CBE Life Sci. Educ.15, ar32. 10.1187/cbe.16-01-0030
6
Envisioning a TransformedBoard on Health Sciences PolicyHealth and Medicine DivisionNational Academies of Sciences, Engineering, and Medicine (2021). Envisioning a transformed clinical trials enterprise for 2030. Proc. a Workshop. 10.17226/26349
7
FriersonG. M.PintoB. M.DenmanD. C.LeonP. A.JaffeA. D. (2019). Bridging the Gap: racial concordance as a strategy to increase African American participation in breast cancer research. J. Health Psychol.24, 1548–1561. 10.1177/1359105317740736
8
GloriaA. M.KurpiusS. E. (2001). Influences of self-beliefs, social support, and comfort in the university environment on the academic nonpersistence decisions of American Indian undergraduates. Cultur. Divers. Ethn. Minor. Psychol.7, 88–102. 10.1037/1099-9809.7.1.88
9
GrahamM. J.FrederickJ.Byars-WinstonA.HunterA.-B.HandelsmanJ. (2013). Science education. Increasing persistence of college students in STEM. Science341, 1455–1456. 10.1126/science.1240487
10
GreenwoodB. N.HardemanR. R.HuangL.SojournerA. (2020). Physician-patient racial concordance and disparities in birthing mortality for newborns. Proc. Natl. Acad. Sci. U. S. A.117, 21194–21200. 10.1073/pnas.1913405117
11
HitchcockP.MathurA.BennettJ.CameronP.ChowC.CliffordP.et al (2017). The future of graduate and postdoctoral training in the biosciences. eLife6, e32715. 10.7554/eLife.32715
12
HurtadoS.HanJ. C.SáenzV. B.EspinosaL. L.CabreraN. L.CernaO. S. (2007). Predicting transition and adjustment to college: biomedical and behavioral science aspirants’ and minority students’ first year of college. Res. High. Educ.48, 841–887. 10.1007/s11162-007-9051-x
13
Improving Representation, Improving representation in clinical trials and research: building research equity for women and underrepresented groups. (2022). 10.17226/26479
14
LaVeistT. A.Nuru-JeterA.JonesK. E. (2003). The association of doctor-patient race concordance with health services utilization. J. Public Health Policy24, 312–323. 10.2307/3343378
15
LocklearT.DickersonK. C.DzirasaK.A more diverse biomedical and healthcare workforce is within our reach. Mod. Healthc.2, 20223.
16
NSF (2022). Women, minorities, and persons with disabilities in science and engineering. Available at: https://ncses.nsf.gov/pubs/nsf21321.
17
SonsteinS. A.JonesC. T. (2018). Joint task Force for clinical trial competency and clinical research professional workforce development. Front. Pharmacol.9, 1148. 10.3389/fphar.2018.01148
18
StatisticsN.Women, minorities, and persons with disabilities in science and engineering. Var. pagings (National Cent. Sci. Eng. Statistics, Natl. Sci. Found., 1994). Available at: https://www.nsf.gov/statistics/women/.
19
TrujilloG.TannerK. D. (2014). Considering the role of affect in learning: monitoring students’ self-efficacy, sense of belonging, and science identity. CBE Life Sci. Educ.13, 6–15. 10.1187/cbe.13-12-0241
20
Tufts Center for the Study of Drug Development (2021). Tufts University Impact Report, New Study finds site personnel race and ethnicity highly correlated with diversity of patients enrolled. Available at; https://f.hubspotusercontent10.net/hubfs/9468915/Impact%20Report%20Preview.png.
21
US National Library of MedicineClinicalTrials.gov trends, charts, and maps.
22
ValantineH. A.CollinsF. S. (2015). National Institutes of Health addresses the science of diversity. Proc. Natl. Acad. Sci. U. S. A.112, 12240–12242. 10.1073/pnas.1515612112
23
Winn ArielS.DelSignoreL.MarcusC.ChielL.FreimanE.StaffordD.et al (2019). Applying cognitive learning strategies to enhance learning and retention in clinical teaching settings. MedEdPORTAL15, 10850. 10.15766/mep_2374-8265.10850
Summary
Keywords
clinical research, internships, cross-institution collaboration, diversity equity and inclusion, key competence in science and technology
Citation
Derk J, Dzirasa K and Locklear T (2023) A novel cross-institutional college internship program to train future diverse leaders in clinical research with data-driven approaches to assess impact. Front. Pharmacol. 14:1294535. doi: 10.3389/fphar.2023.1294535
Received
14 September 2023
Accepted
17 November 2023
Published
06 December 2023
Volume
14 - 2023
Edited by
Barbara E. Bierer, Harvard Medical School, United States
Reviewed by
Kimberly McCall, University of Alabama at Birmingham, United States
Updates
Copyright
© 2023 Derk, Dzirasa and Locklear.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Julia Derk, julia.derk@duke.edu; Tracie Locklear, tlockl12@nccu.edu
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.