- 1College of Chinese Medicinal Materials, National and Local Joint Engineering Research Center for Ginseng Breeding and Development, Jilin Agricultural University, Changchun, China
- 2College of Life Sciences, Engineering Research Center of the Chinese Ministry of Education for Bioreactor and Pharmaceutical Development, Jilin Agricultural University, Changchun, China
- 3Liaoning Xifeng Pharmaceutical Group Co., Ltd., Huanren, China
Background: Hyperuricemia (HUA) is a metabolic disease caused by reduced excretion or increased production of uric acid. This research aims to study the practical components, active targets, and potential mechanism of the “Radix ginseng (RG)-Ziziphus jujube (ZJ)” herb pair through molecular docking, network pharmacology, and animal experiments.
Methods: The potential targets of “Radix ginseng (RG)-Ziziphus jujube (ZJ)” herb pair were obtained from the TCMSP database. The therapeutic targets of HUA were acquired from the GendCards, OMIM, PharmGkb, and TTD databases. Protein-protein interaction network (PPI) was constructed in the STRING 11.0 database. The David database was used for enrichment analysis. Molecular Docking was finished by the AutoDock Vina. And we employed Radix ginseng and Ziziphus jujube as raw materials, which would develop a new functional food fresh ginseng paste (FGP) after boiling. In addition, benzbromarone (Ben) (7.8 mg/kg) and allopurinol (All) (5 mg/kg) were used as positive drugs to evaluate the hyperuricemia induced by FGP (400 and 800 mg/kg) potassium oxazine (PO) (100 mg/kg) and hypoxanthine (HX) (500 mg/kg) on mice.
Results: The results showed that 25 targets in the “RG-ZJ” herb pair interacted with hyperuricemia. Then protein-protein interaction (PPI) analysis showed that TNF, IL-1β, and VEGFA were core genes. KEGG enrichment analysis showed that the Toll-like receptor signaling pathway and IL-17 signaling pathway were mainly involved. Meantime, animal experiments showed that FGP could improve the HUA status of mice by reducing serum UA BUN, XO, and liver XO levels (p < 0.05, p < 0.01). Furthermore, we analyzed the main ingredients of FGP by HPLC. We found that the main ingredients of FGP had solid binding activity to the core target of HUA by molecular docking.
Conclusion: This study explored the active ingredients and targets of the “RG-ZJ” herb pair on HUA through network pharmacology, molecular docking, and animal experiments. It revealed the improvement of FGP in mice with HUA.
Introduction
Hyperuricemia (HUA) is a disease caused by purine metabolic disorder or decreased uric acid (UA) excretion leading to increased serum UA levels (Wu et al., 2020). At present, people’s living standards continue to improve, and the diet structure has undergone unreasonable changes. People’s excessive intake of high protein and purine food leads to an increasing trend in the number of HUA patients, characterized by younger age (Simin et al., 2022). HUA can cause gout, also an inducing factor for hypertension, obesity, cardiovascular disease, renal failure, and other diseases (Ma et al., 2019; Bezerra et al., 2021; Yang et al., 2022). However, the current first-line drugs to treat HUA have specific side effects, such as Benzbromarone (Dalbeth et al., 2021) and Allopurinol (Khanna et al., 2012).
In the development process of traditional Chinese medicine (TCM), herb pairs (mixture of two herbs), as the basic composition units of Chinese herbal formulas, have special clinical significance in TCM and are much simpler than other complex formulas without altering their basic therapeutic features (Han et al., 2016). Radix ginseng (RG) contains various active ingredients such as ginsenosides and polysaccharides. It has various pharmacological activities, such as pharmacological activities of antibiosis, anti-tumor activities, antioxidation, anti-diabetes, and anti-cardiovascular diseases (Khanna et al., 2012; Li et al., 2015). Moreover, it has strong liver and kidney protection. In addition, many studies have shown that the secondary saponins in ginseng have better pharmacological activities, such as ginsenoside Rk3, Rh4, Rg3, Rg5, and Rh2 (Yu et al., 2012; Li et al., 2016; Zhang et al., 2018; Hu et al., 2019; Liu et al., 2020). Ziziphus jujube (ZJ) is a healthy food containing various biologically active substances, such as polysaccharides, polyphenols, alkaloids, and other nutrients (Hernández et al., 2016; Lu et al., 2021). These nutrients from ZJ have physiological functions, including antioxidant (Zhao et al., 2014), anti-inflammatory, hypoglycemia (Kawabata et al., 2017), and anti-hyperlipidemia (Jeong and Kim, 2019). Both RG and ZJ are typical medicinal and edible medicinal materials with good pharmacological activities. The “RG-ZJ” herb pair has greater medicinal value. In this study, we developed a potential functional food Fresh Ginseng Paste (FGP), which was prepared by cooking Radix ginseng (RG)and Ziziphus jujube (ZJ) in the best proportion. The preparation method of fresh ginseng paste is to select fresh ginseng and jujube (RG: ZJ = 1: 3). Firstly, the ginseng was purified, and the ginseng whiskers were separated from the main root. At the same time, the jujube was crushed into 200 mesh very fine powder, and then the ginseng whiskers were added to the purified water with a ratio of 1: 30 according to the mass. After the fire was boiled, the fire was boiled for 30 min. After repeating twice, it was crushed into a homogenate and mixed with the jujube very fine powder. At 45°C, the control pressure was 1.1 Mpa for 30 min, and it was boiled into a thick paste. FGP has been proved to have pharmacological activities such as promoting sleep (Su et al., 2021) and anti-fatigue and has great potential for development. Furthermore, FGP contains abundant saponins and flavonoids, which can be effectively improved.
Based on the above research, in the study, network pharmacology was employed to predict the mechanism of action of the “RG-ZJ” herb pair on HUA intervention, screen out the foremost practical components, and predict the targets that it acts on HUA. To verify the above results, the improvement effect of FGP on HUA in mice was preliminarily explored.
Materials and methods
Materials and equipment
Sixteen ginsenosides 20(S)-ginsengoside Rg2, 20 (S)-ginsengoside Rh1, 20 (R)-ginsenoside Rh1, F1, Rg6, F4, Rk3, Rh4, 20 (S)-sinsenoside Rg3, 20 (R)-ginsenoside Rg3, CK, Rk1, Rg5, 20 (S)-ginsenoside Rh2, 20 (R)-ginsenoside Rh2, and PPD standards were purchased from the Hongjiu Biotech Co., Ltd. (Jilin, China). The purity of all these standards was over 98% as indicated by the manufacturer. HPLC-grade acetonitrile was purchased from Merck Co. (Merck, Darmstadt, Germany). Wahaha purified water was purchased from Hangzhou Wahaha Group Co., LTD. Ultraviolet spectrophotometer (UV) was purchased from Shanghai Metash instruments Co., LTD. (UV-9000, Shanghai, China). Other chemicals were of reagent grade. Waters e 2695 HPLC system (Palo Alto, CA, United States).
Sample preparation
Fresh Ginseng Paste (FGP) was produced and provided by Liaoning XIFENG Pharmaceutical Group Co., Ltd. (License No. SC10721052200667). FGP based on “RG-ZJ”, selected natural growth was born of Panax ginseng C.A. Meyer cv. Silvatica, covered for 5 years with high quality, using the unique patented technology, scientific processing, transformation of rare active substances, enrichment of the represented by Rg3, Rk1, Rg5, of 16 kinds of rare saponins group based on maximum keep the effective active substances in the ginseng. 5 g FGP sample was extracted three times with 100 ml of analytical pure methanol at room temperature by ultrasonication (60 kHz, heat power 330 W; KQ-600KDB, Kun-shan, China) for 60 min. The residue was dissolved in 1 ml of solvent (MeOH: H2O = 1:1, v/v), and then filtered through a 0.45 µm polytetrafluoroethylene (PTFE) syringe filter (Waters, Milford, MA, United States) and it was ready for HPLC analysis.
Chromatographic conditions
Samples were analyzed on a Waters e2695 HPLC system (Waters Corporation, Milford, United States) equipped with a UV detector. Analytes were separated on a Waters C18 column (4.6 cm × 25 cm, 5 μm) at 30 °C and the detection wavelength was set at 203 nm. The mobile phase consisted of a mixture of acetonitrile (A) and water (B) and were set in a gradient elution program: 0–40 min, 18.0%–21.0% A; 40–42 min, 21.0–26.0% A; 42–46 min, 26.0%–32.0% A; 46–66 min, 32.0%–34.0% A; 66–71 min, 34.0%–38.0% A; 71–78 min, 38.0%–49.1% A; 78–82 min, 49.1% A. 82–83 min, 49.1%–50.6% A.83–88 min, 50.6%–59.6% A.88–90 min, 59.6%–65% A.90–97 min, 65.0% A. 97–102 min, 65.0%–75.0% A.102–110 min, 75.0%–85.0% with a flow rate of 1.0 ml/min. The injection volume was 20 μl.
Determination of ginsenosides in fresh ginseng paste
20(S)-ginsengoside Rg2, 20 (S)-ginsengoside Rh1, 20 (R)-ginsenoside Rh1, F1, Rg6, F4, Rk3, Rh4, 20 (S)-sinsenoside Rg3, 20 (R)-ginsenoside Rg3, CK, Rk1, Rg5, 20 (S)-ginsenoside Rh2, 20 (R)-ginsenoside Rh2, and PPD were prepared and diluted with 20% (v/v) methanol aqueous solution to appropriate concentration for the establishment of calibration curves (Table 1). The content of total saponins in FGP was calculated by UV detection method, and the type and content of ginsenosides were calculated by normalization method of standard curve above.
Chemicals and reagents
Hypoxanthine (CAS. 68-94-0, HX); Potassium oxazine (CAS. 2207-75-2, PO); Benzbromarone (CAS. 3562-84-3, Ben); Allopurinol (CAS. 315-30-0, All) (Solabor Bio Co., Ltd.); Commercial assay kits for uric acid (UA), xanthine oxidase (XO), blood urea nitrogen (BUN) and hematoxylin and eosin (H&E) dye kits were purchased from Nanjing Jiancheng Bioengineering Institute (Nanjing, China).
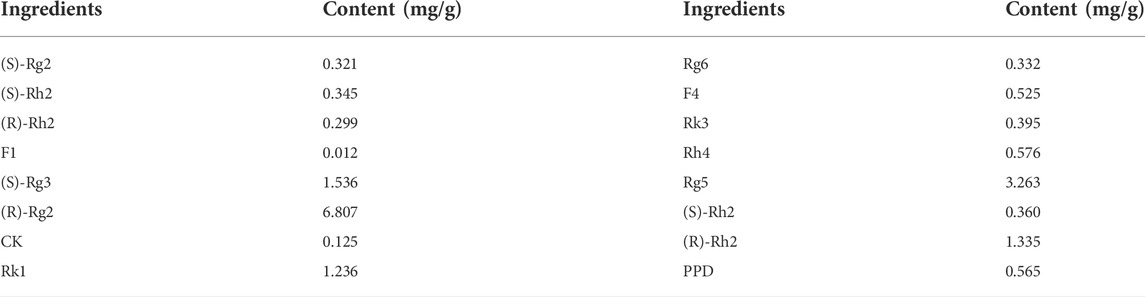
Ingredients from “ RG-ZJ ” and hyperuricemia target prediction
All the ingredient data of Radix ginseng (RG) and Ziziphus jujube (ZJ) were retrieved from TCMSP (https://tcmspw.com/tcmsp.php) and Swiss target, RG and ZJ as the search keywords, oral bioavailability (OB) ≥ 30%, drug-like properties (DL) ≥ 0.18 for screening, and then target prediction. Then, the target information of hyperuricemia (HUA) was predicted through the above four databases of GendCards, OMIM, PharmGkb, and TTD, and the repeats were removed and intersected with the drug targets. In addition, the Venn diagram is used for visualization.
Enrichment analysis and network construction
Common target proteins screened by the “RG-ZJ” herb pair and HUA were uploaded to String (https://string-db.org/, v11.0) online platform database (Chen et al., 2018; Lee et al., 2018), to construct a protein-protein interaction network model and obtain a PPI interaction network. Then the biological process (BP), molecular function (MF), cellular component (CC), and role of “RG-ZJ” in the potential targets of the HUA intervention pathway were explored. This study used the critical targets of proteins to submit the PPI network to the DAVID database (https://david.ncifcrf.gov/, v6.8) (Jiang et al., 2022), for GO (Gene Ontology) bioprocess enrichment analysis and KEGG pathway enrichment analysis.
Animals and experimental design
6-week-old male ICR mice (weighting 18–23 g) were obtained from Liaoning Changsheng Biotechnology Co., Ltd. (Certificate No. SCXK [Liao] 2020-0001). The mice underwent adaptive feeding for at least one week. All animal handling and experimental procedures are maintained in accordance with the Ethical Committee approval for Laboratory Animals of Jilin Agricultural University.
In this study, HUA was induced in mice according to the method in the previous study [24]. All experimental animals were randomly divided into six groups (n = 8): normal group, HUA group, positive groups (All: 5 mg/kg/day; Ben: 7.8 mg/kg/day), and FGP treatment (400 and 800 mg/kg) groups. All groups except the normal group received intraperitoneal injection of PO (100 mg/kg/day) and gavage administration of HX (500 mg/kg/day) for seven consecutive days to elevate UA levels. The same volume of saline was employed in the normal group. The FGP group was pre-administered with 400 and 800 mg/kg and prepared FGP into suspension with normal saline once a day for seven consecutive days. From the 14th day, all groups except the normal group were injected with PO (100 mg/kg) and administered intragastrically with HX (500 mg/kg) daily. The continuous molding and administration were performed for 7 days. To ensure efficacy, Ben (7.8 mg/kg) and All (5 mg/kg) were administered by intragastric administration one day before the model was established in the positive group. In addition, we fed the normal group with physiological saline. Twelve hours after injection, blood samples were gathered and allowed to clot for 45 min at room temperature. Then, the serum was centrifuged (3500 rpm, 10 min, and 4°C) and stored at −20°C for biochemical analysis, including UA, BUN, and XO detection. The remaining serum was stored in a −80°C refrigerator for subsequent indicators detection. After weighing the anatomical liver and kidney tissues, part of them were fixed in 10% neutral formalin buffer, and part of them was wrapped with tin paper, frozen in liquid nitrogen, and stored at −80°C.
Determination of biochemical parameters
The activities of uric acid (UA), Xanthine oxidase (XO), and blood urea nitrogen (BUN) in serum and the level of XO in liver tissues were quantified by those mentioned above in commercially available kits (Nanjing Jiancheng Bioengineering Institute, Nanjing, China) according to the manufacturer’s protocol. The absorbance was measured at the corresponding wavelength using an automatic microplate reader (Bio Tek Elx800, Berton Instruments, United States).
hematoxylin and eosin staining
Kidney tissues were collected and then washed with phosphate-buffered saline. The tissues were fixed with 4% paraformaldehyde for 24 h, embedded in paraffin, and cut into 5 μm thickness. The histopathological changes were mounted with neutral gum, and representative images were captured using a light microscope (Olympus BX-60, Tokyo, Japan).
Molecular docking
The binding ability of key compounds including (20R)-ginsenoside Rg3, ginsenoside Rg5, ginsenoside Rh4, oleanolic acid, and kaempferol to key targets in FGP was verified by molecular docking. The above compounds were determined in the PubChem database (https://pubchem.ncbi.nlm.nih.gov/), and the crystal structures of TNF-α-P01375, IL-1β-M4WG34, VEGFA-P15692 and XO-P80457 were obtained from the Protein Data Bank database (http://www.rcsb.org/) in PDB format. AutoDockTools-1.5.6 was used to save protein and ligand data in PDBQT format. Finally, AutoDockVina.exe was used for molecular docking, and the results were calculated. The docking results of the critical target proteins with the best binding ability to the compounds were shown by PyMOL software.
Statistical analysis
All data were expressed as the mean ± standard deviation (Mean ± S.D). Statistical graphs were performed using GraphPad Prism 8.0.2 software (San Diego, CA, United States). P < 0.001, p < 0.01 or p < 0.05 were considered being significant.
Results
Chemical constituents of fresh ginseng paste and acquisition of active constituents of “RG-ZJ” herb pair
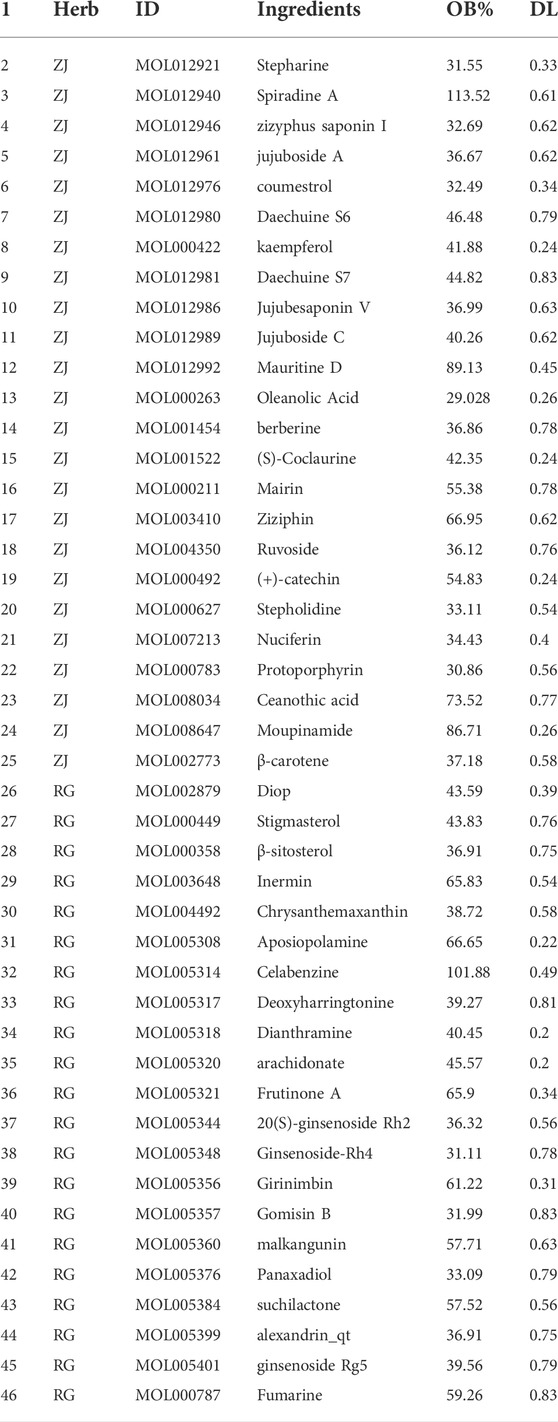
As shown in Table 2, the “RG-ZJ” active ingredients data were screened according to the TCMSP database and related literature. The results showed that 46 effective compounds and corresponding gene targets were obtained (Figure 1), and HPLC identified saponins in FGP. Quantitative analysis of saponins in FGP was determined as follows: 1. (S)-Rg2:1.76%; 2. (S)-Rh1:1.88%; 3. (R)-Rh1:1.59%; 4. F1:0.06%; 5. Rg6:1.76%; 6. F4:2.79%; 7. Rk3:2.09%; 8. Rh4:3.06%; 9. (S)-Rg3:8.16%; 10. (R)-Rg3:36.15%; 11. CK:0.66%; 12. Rk1:6.56%; 13. Rg5:17.33%; 14. (S)-Rh2:1.91%; 15. (R)-Rh2:7.09%; 16. PPD:3.00%. The total saponin content in FGP was 0.883 g/100 g FGP (Table 2).
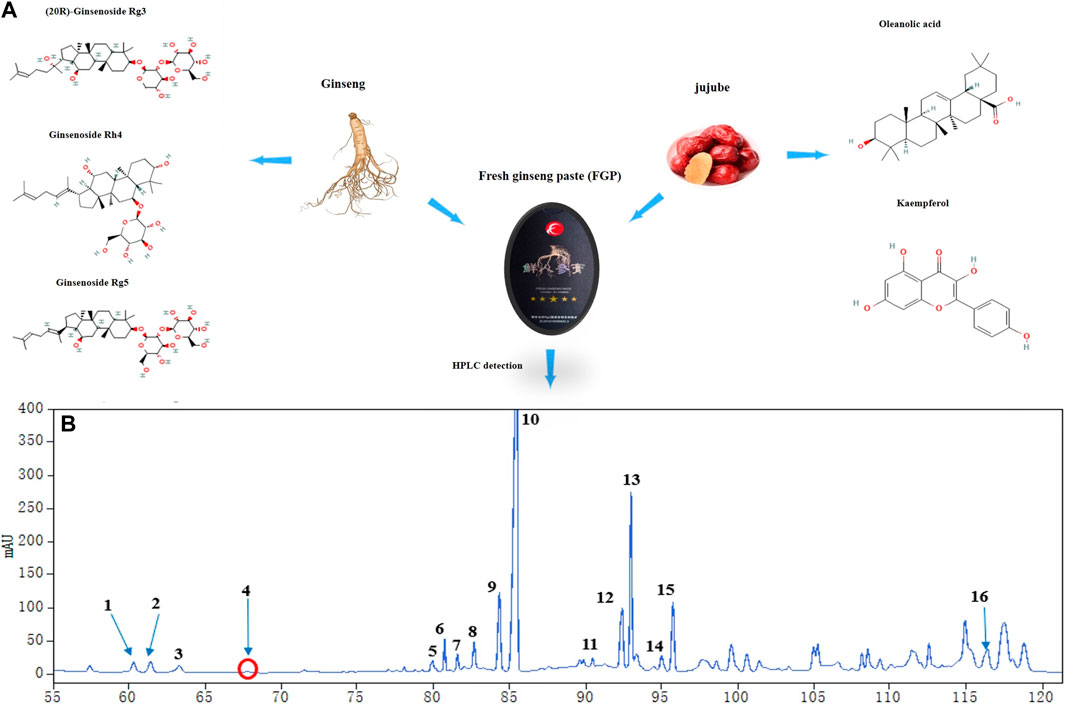
FIGURE 1. Analysis of principal components in FGP. Main components of Fresh ginseng paste (FGP) (A); Identification of the main components in FGP by HPLC analysis (B); 1. (S)-Rg2; 2. (S)-Rh1; 3. (R)-Rh1; 4. F1; 5. Rg6; 6. F4; 7. Rk3; 8. Rh4; 9. (S)-Rg3; 10. (R)-Rg3; 11. CK; 12. Rk1; 13. Rg5; 14. (S)-Rh2; 15. (R)-Rh2; 16. PPD.
Network construction and enrichment analysis of “RG-ZJ” herb pair and HUA-related targets
We associated drug targets with disease genes, obtained 25 targets of 12 active components in Figures 2B,C, and further constructed a regulatory network diagram of active ingredients and related targets in “RG- ZJ.” There were 49 nodes and 73 edges. As shown in Figure 3A, we obtained 1140 biological processes (BP), 147 cellular components (CC), and 69 molecular functions (MF) by GO enrichment analysis, involving responses to heterogeneous stimuli, regulation of leukocyte chemotaxis, osteoblast differentiation, regulation of leukocyte migration, and mitochondrial membrane gap, platelet alpha particle lumen, and membrane microregions. We obtained 64 related signaling pathways, including Toll-like receptors and IL-17, and MAPK signaling pathways through KEGG enrichment analysis (Figure 3B).
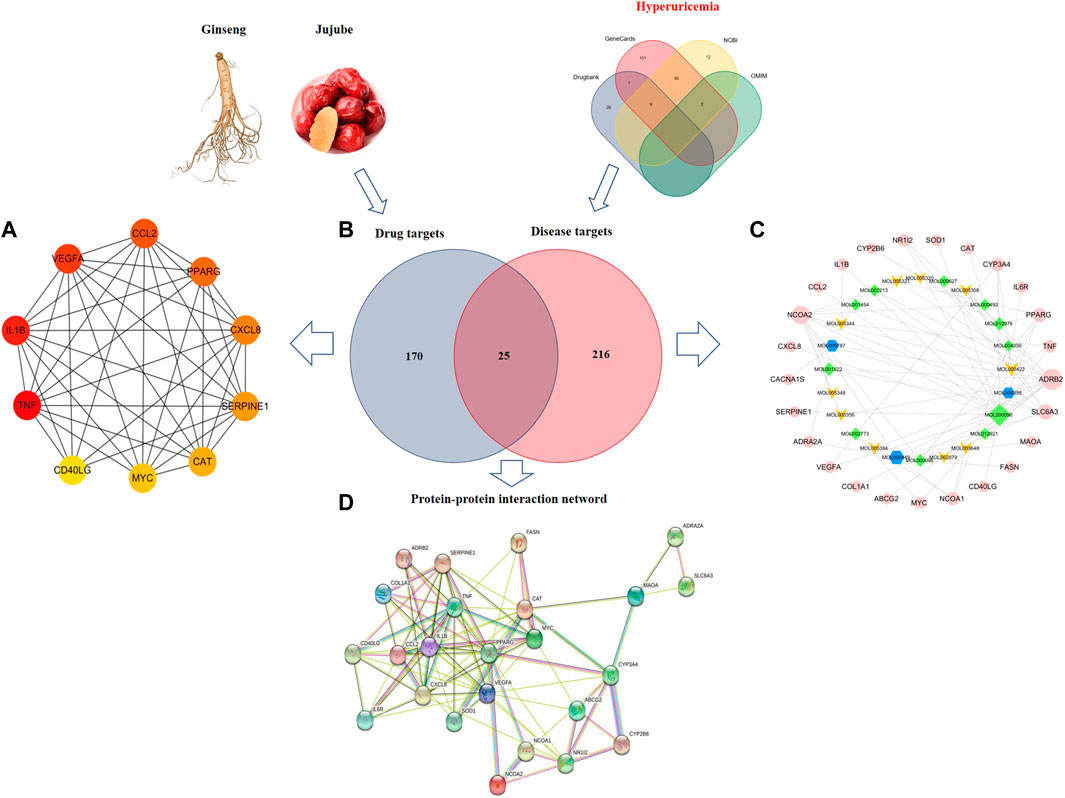
FIGURE 2. Visualization of the interaction targets between “RG-ZJ” components and the HUA disease diagram. Screened core targets (A); Venn diagram showing the numbers of the overlapped and specific targets among the RG- ZJ herb pair (blue circle) and HUA (red circle) (B); Compound-target-pathway network of the “RG- ZJ” herb pair against HUA. The light green and yellow nodes are active ingredients of ZJ and RG, respectively. The pink nodes is the potential targets (C); Construction of protein interaction network (D).
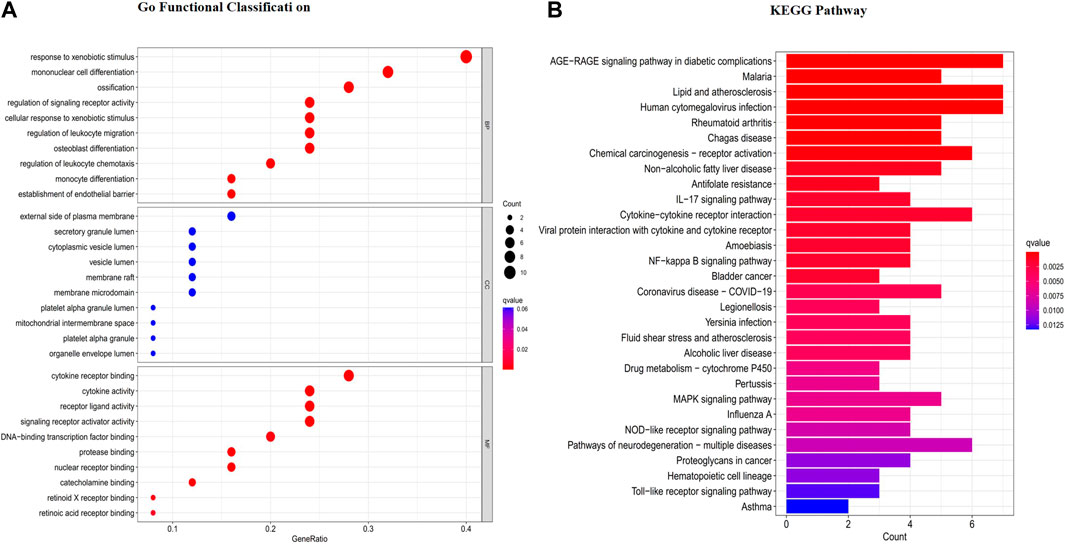
FIGURE 3. GO enrichment (A) and KEGG pathway analysis (B) of the HUA targets of the “RG-ZJ” herb pair.
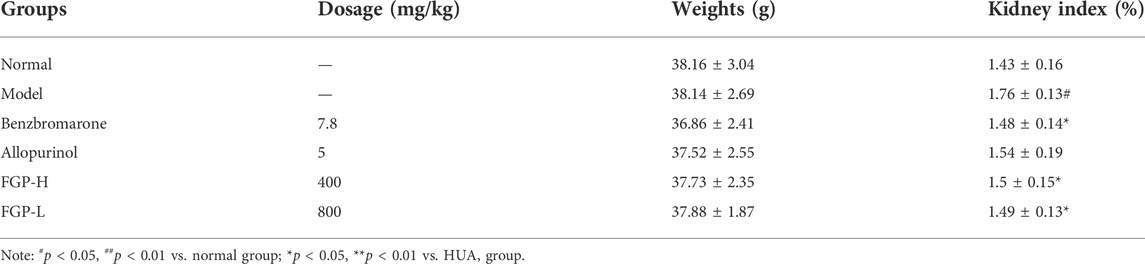
Effect of fresh ginseng paste on biochemical indicators in Hyperuricemia mice
As shown in Figure 4, compared with the normal group, the levels of UA, BUN and XO after PO (100 mg/kg) and HX (500 mg/kg) administration were significantly increased (p < 0.05) (p < 0.05). It is indicated that the HUA model was successfully established. After administration of Ben and All, the UA level in mice was significantly decreased (p < 0.05). In addition, the levels of UA, BUN, and XO in the 400 mg/kg and 800 mg/kg of FGP were significantly lower than this in the HUA group (p < 0.05). In particular, the level of UA in the serum of mice was significantly reduced (p < 0.01).
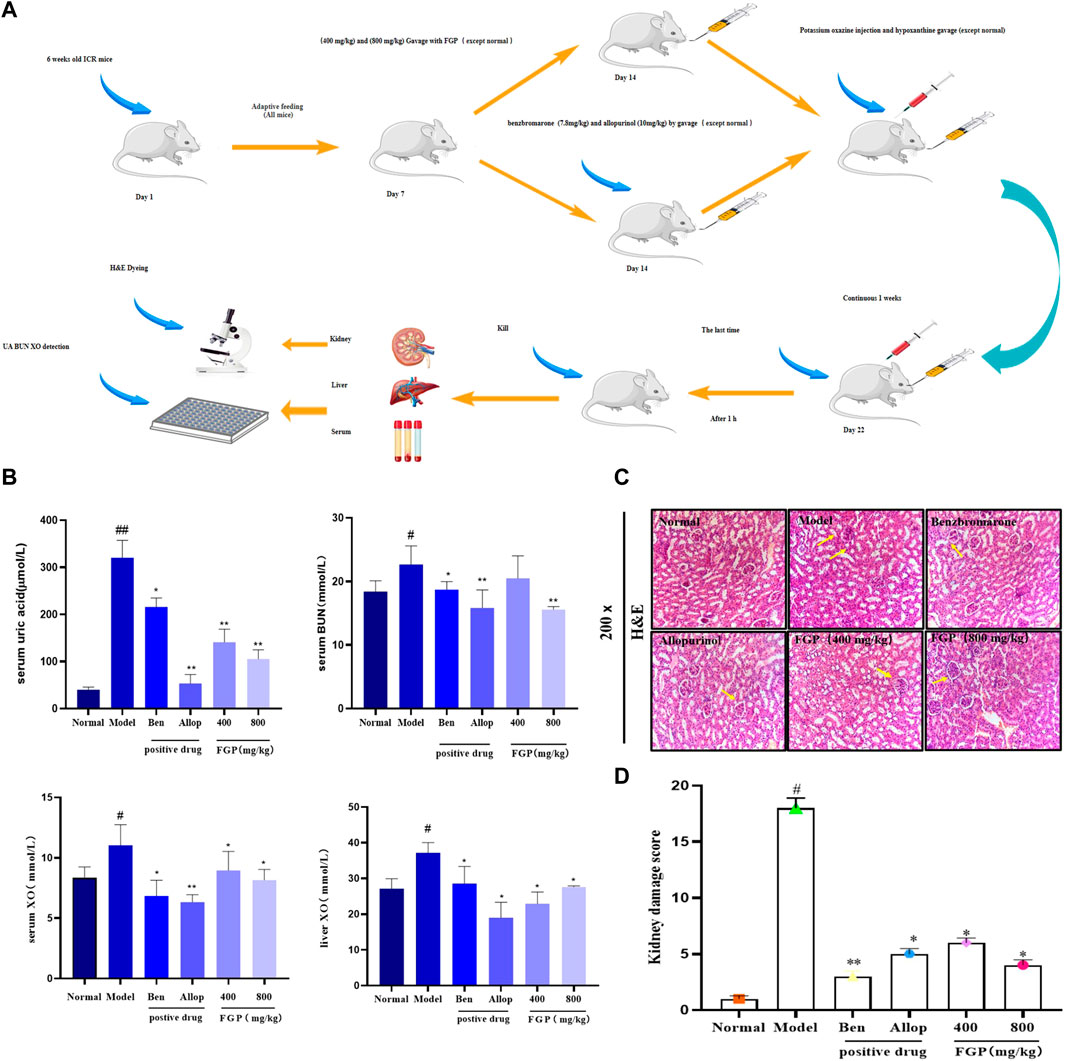
FIGURE 4. Effects on related indexes in HUA mice. Experimental animals and design process (A). Effects of FGP on UA, BUN levels in the serum in mice and effects of FGP on XO activities in the liver and serum in mice (B); Histological examination of the kidney (200 ×) (C); Pathological changes of kidney and Ridit analysis (D). Data are expressed as the mean ± SD (n = 8). #p < 0.05, ##p < 0.01 vs. normal group; *p < 0.05, **p < 0.01 or ***p < 0.001 vs. HUA group.
Effect of fresh ginseng paste on histopathological alterations in Hyperuricemia mice
The results showed that compared with the normal group, the renal coefficient of the model group was significantly increased (p < 0.05), which was related to renal edema caused by HUA (Table 3). However, both positive drugs and FGP treatment attenuated this change. In addition, the H&E staining results in Figures 4E,F showed that compared with the normal group, the number of glomeruli in the model group was significantly reduced (p < 0.05), and there were local edema, glomerular ablation, and unclear boundary. However, FGP effectively improved this pathological state, reduced glomerular ablation, and increased the number of glomeruli. The above results show that FGP could promote the excretion of UA and avoid renal edema.
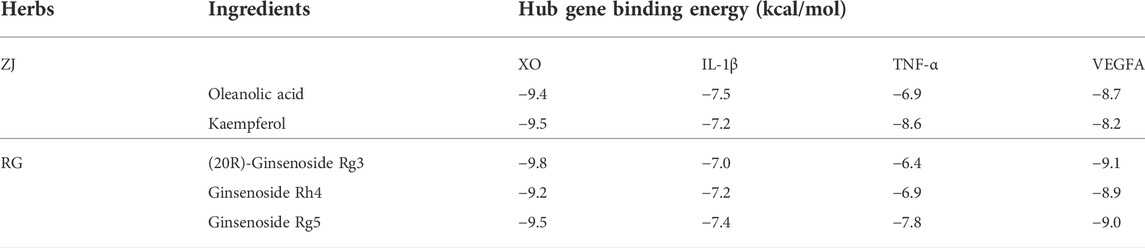
Molecular docking validation of core targets and active compounds
Molecular docking was applied to analyze the binding of the critical target TNF-α, IL-1β, VEGFA and XO with five main active compounds in FGP. The binding energy between the above compounds and the target was lower than −5.0 kJ/mol (Table 4). As shown in Figures 5, 6, the key targets TNF-α, IL-1β, VEGFA, and XO were stably combined with five compounds, including (20R)-ginsenoside Rg3, ginsenoside Rg5, ginsenoside Rh4, oleanolic acid, and kaempferol. The results showed that the above compounds of FGP could affect the critical targets of HUA. It is worth noting that XO has been studied as an inhibitory target for UA reduction in many natural products. Interestingly, the compounds in our FGP had excellent binding activity to XO (Binding energies were less than −7.0 kJ/mol).
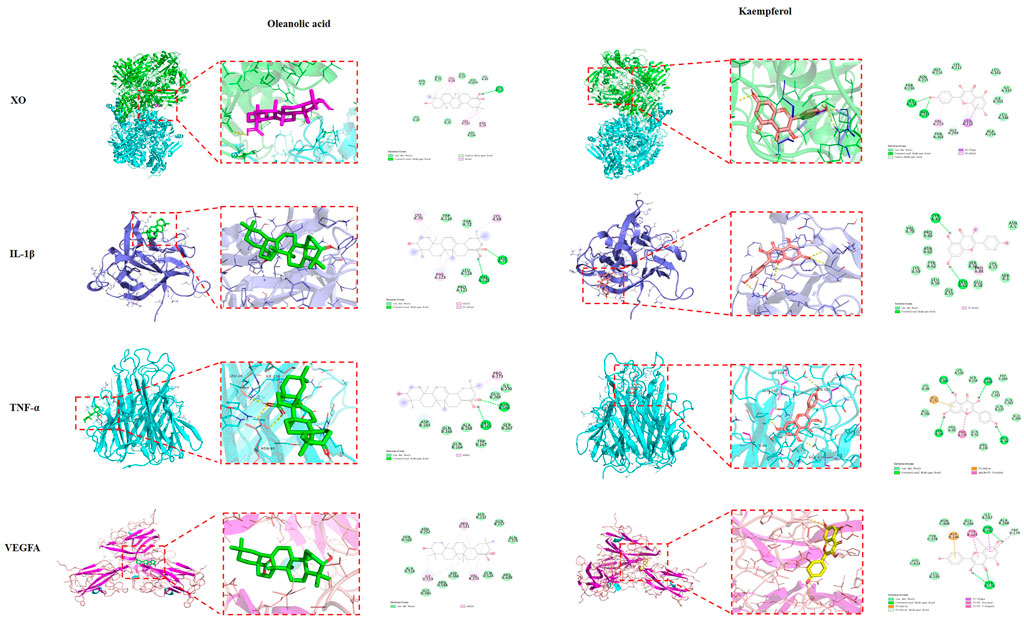
FIGURE 5. Molecular docking of oleanolic acid and kaempferol with TNF-α, IL-1B, VEGFA, and XO, respectively.
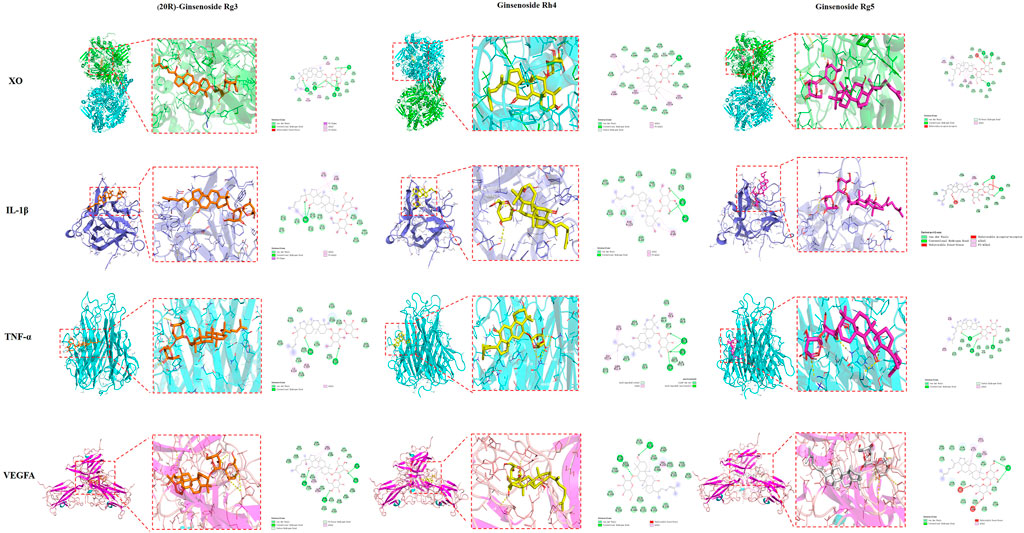
FIGURE 6. Molecular docking of 20(R)-ginsenoside Rg3, ginsenoside Rg5, and ginsenoside Rh4 with TNF-α, IL-1βVEGFA, and XO, respectively.
Discussion
Excessive UA level is considered the main cause of HUA (Zhang et al., 2018). Renal excretion accounts for 70% of total UA elimination, with the remaining 30% eliminated in the intestine. Renal UA underexcretion is the leading cause of HUA, found in approximately 90% of HUA patients (Lee et al., 2018). Both Radix ginseng (RG) and Ziziphus jujube (ZJ) have the effect of invigorating the kidney and enhancing metabolism (Rekha et al., 2021). Therefore, this study explored the potential mechanism of the “RG-ZJ” drug in the treatment of HUA through network pharmacology, molecular docking, and animal experiments.
At present, the research on the analysis of active compounds obtained from traditional Chinese medicine (TCM) and disease targets through network pharmacology is increasing, especially for herb pairs. The present study explored potential targets in the “RG-ZJ” herb pair for improving HUA through network pharmacology (Lu et al., 2020). The results showed that the “RG-ZJ” herb pair could improve HUA through CCL2, TNF-α, IL-1β, and VEGFA. Previous studies have analyzed the potential mechanism of Plantain in the treatment of HUA by network pharmacology and found that Plantain can affect HUA by interacting with MAPK1, TNF-α, and other targets (Pei et al., 2020). At the same time, some studies have predicted the targets of practical components in the “Gardenia-Poria” couplet on HUA, and the results show that the core targets of its role include IL-1β and IL-6 (Liu et al., 2021). In addition, previous studies found that baicalin and baicalein could improve HUA by down-regulating TLRs, NLRP3, and MAPK through network pharmacology analysis (Huilong et al., 2021). Combined with the above results, it can be found that the key pathways affecting HUA are mainly concentrated on the IL-17 signaling pathway and MAPK signaling pathway, which is consistent with the results of this study. Our prediction results were in line with previous reports and confirmed the reliability of the prediction on effective compounds of “RG-ZJ” against HUA. Besides, KEGG results also suggested that “RG-ZJ” might reduce the inflammatory response in HUA by affecting the TNF-α signaling pathway, IL-17 signaling pathway, and MAPK signaling pathway. The results are also consistent with previous studies.
The main role in the formation of UA is purines, and the accumulation of purines in the body is the main reason for the production of HUA. XO is the critical enzyme in the last step of UA synthesis, which catalyzes the oxidation of hypoxanthine to xanthine and then to UA, or directly to UA (Furuhashi et al., 2018; Kawachi et al., 2021). Several studies have shown that flavonoids (Scheepers et al., 2019) and saponins (Xu et al., 2022) isolated from TCM can reduce UA by reducing the content of XO in the liver while enhancing renal excretion of UA. Meanwhile, previous reports have shown that Urtica extracts can reduce serum UA levels by improving renal metabolism (Liu et al., 2020). Related research found that Hedyotis diffusa extract could improve HUA symptoms by reducing UA and BUN levels in serum (Zhang et al., 2021). In this study, animal experiments found that FGP can significantly reduce the levels of UA, BUN, and XO in HUA mice and improve the renal injury caused by HUA. These results are consistent with the above research results.
Due to the limitations of network pharmacology, the screening of drug components and disease targets is not comprehensive. Therefore, based on network pharmacology, this study screened five compounds that might play a role in FGP. Three core targets are related to HUA, TNF, IL-1β, VEGFA, and XO, through a large number of literature and previous research accumulation. Through molecular docking technology, the above compounds were docked with the target. The results showed that the above compounds had a strong binding ability with targets, which further proved the possibility of FGP improving HUA and preliminarily revealed the possible mechanism of action. However, there were still some shortcomings in this research. Since the pathological development of HUA involves complex pathological processes, the mechanism predicted above of “RG-ZJ” in treating HUA still needs to be supplemented by in vivo and in vitro experiments. In the future, we will continue to explore the mechanisms of “RG-ZJ” practical components in the treatment of HUA diseases in the hope of providing new insights for clinical drug development.
Conclusion
In summary, firstly we analyzed the target of interaction between “RG-ZJ” couplet medicines and HUA through network pharmacology. Then through molecular docking and animal experiments, the improvement effect of potential functional food FGP processed by “RG-ZJ” on HUA was revealed, and the possible effect mechanism was preliminarily explored, providing a theoretical basis for the further development of ginseng products.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The animal study was reviewed and approved by Animal Ethics Committee of Jilin Agricultural University.
Author contributions
WL, ZW, SR, and X-jL developed a major research plan. HZ and WL analyze data, draw charts and write manuscripts. S-MQ and QG helped collect data and references. J-FC and X-HL provided advice and data processing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the grants of the National Natural Science Foundation of China (No. 82104465), Jilin Science & Technology Development Plan (No. 20200301037RQ), and the Science and Technology Innovation Fund for College Students (No. 20220123482). This study was also supported by the grants of the National key research and development project (No. 2021YFD1600901).
Conflict of interest
Author X-HL was employed by the company Liaoning Xifeng Pharmaceutical Group Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CP, Cisplatin; ER, Endoplasmic reticulum; FGP, Fresh Ginseng Paste; HUA, Hyperuricemia; BUN, serum urea nitrogen; UA, uric acid; XO, xanthine oxidase; XOIs, XO inhibitors; PPI, Protein-protein interaction; GO, gene ontology; PO, potassium oxazine; HX, hypoxanthine; Ben, benzbromarone; All, allopurinol.
References
Bezerra, T. T. D., Bezerra, L. S., Santos-Veloso, M. A. O., Lordsleem, A., and Lima, S. G. (2021). Association between hyperuricemia and hypertension: A case-control study. Rev. Assoc. Med. Bras. 67 (6), 828–832. doi:10.1590/1806-9282.20210021
Chen, G., Huang, C., Liu, Y., Chen, T., Huang, R., Liang, M., et al. (2018). A network pharmacology approach to uncover the potential mechanism of yinchensini decoction. Evid. Based. Complement. Altern. Med. 2018, 2178610. doi:10.1155/2018/2178610
Dalbeth, N., Gosling, A. L., Gaffo, A., and Abhishek, A. (2021). Gout. Lancet 397 (10287), 1843–1855. doi:10.1016/s0140-6736(21)00569-9
Furuhashi, M., Matsumoto, M., Tanaka, M., Moniwa, N., Murase, T., Nakamura, T., et al. (2018). Plasma xanthine oxidoreductase activity as a novel biomarker of metabolic disorders in a general population. Circ. J. 82 (7), 1892–1899. doi:10.1253/circj.CJ-18-0082
Han, B., Huang, H., Li, Z., Gong, M., Shi, W., Zhu, C., et al. (2016). Therapeutic effects of Chinese medicine herb pair, huzhang and guizhi, on monosodium urate crystal-induced gouty arthritis in rats revealed by anti-inflammatory assessments and NMR-based metabonomics. Evid. Based. Complement. Altern. Med. 2016, 9398435. doi:10.1155/2016/9398435
Hernández, F., Noguera-Artiaga, L., Burló, F., Wojdyło, A., Carbonell-Barrachina Á, A., and Legua, P. (2016). Physico-chemical, nutritional, and volatile composition and sensory profile of Spanish jujube (Ziziphus jujuba Mill.) fruits. J. Sci. Food Agric. 96 (8), 2682–2691. doi:10.1002/jsfa.7386
Hu, J. N., Xu, X. Y., Li, W., Wang, Y. M., Liu, Y., Wang, Z., et al. (2019). Ginsenoside Rk1 ameliorates paracetamol-induced hepatotoxicity in mice through inhibition of inflammation, oxidative stress, nitrative stress and apoptosis. J. Ginseng Res. 43 (1), 10–19. doi:10.1016/j.jgr.2017.07.003
Huilong, X., Huan, L., Ziyuan, L., Yongjie, L., Yang, L., Yinsheng, Q., et al. (2021). Network pharmacology and molecular docking analysis on molecular targets: Mechanisms of baicalin and baicalein against hyperuricemic nephropathy %J Toxicology and Applied Pharmacology. (prepublish).
Jeong, O., and Kim, H. S. (2019). Dietary chokeberry and dried jujube fruit attenuates high-fat and high-fructose diet-induced dyslipidemia and insulin resistance via activation of the IRS-1/PI3K/Akt pathway in C57BL/6 J mice. Nutr. Metab. 16, 38. doi:10.1186/s12986-019-0364-5
Jiang, G., Sun, C., Wang, X., Mei, J., Li, C., Zhan, H., et al. (2022). Hepatoprotective mechanism of Silybum marianum on nonalcoholic fatty liver disease based on network pharmacology and experimental verification. Bioengineered 13 (3), 5216–5235. doi:10.1080/21655979.2022.2037374
Kawabata, K., Kitamura, K., Irie, K., Naruse, S., Matsuura, T., Uemae, T., et al. (2017). Triterpenoids isolated from Ziziphus jujuba enhance glucose uptake activity in skeletal muscle cells. J. Nutr. Sci. Vitaminol. 63 (3), 193–199. doi:10.3177/jnsv.63.193
Kawachi, Y., Fujishima, Y., Nishizawa, H., Nakamura, T., Akari, S., Murase, T., et al. (2021). Increased plasma XOR activity induced by NAFLD/NASH and its possible involvement in vascular neointimal proliferation. JCI Insight 6 (17), 144762. doi:10.1172/jci.insight.144762
Khanna, D., Fitzgerald, J. D., Khanna, P. P., Bae, S., Singh, M. K., Neogi, T., et al. (2012). 2012 American College of rheumatology guidelines for management of gout. Part 1: Systematic nonpharmacologic and pharmacologic therapeutic approaches to hyperuricemia. Arthritis Care Res. 64 (10), 1431–1446. doi:10.1002/acr.21772
Lee, A. Y., Park, W., Kang, T. W., Cha, M. H., and Chun, J. M. (2018). Network pharmacology-based prediction of active compounds and molecular targets in Yijin-Tang acting on hyperlipidaemia and atherosclerosis. J. Ethnopharmacol. 221, 151–159. doi:10.1016/j.jep.2018.04.027
Li, W., Wang, Z., Gu, J., Chen, L., Hou, W., Jin, Y., et al. (2015). Bioconversion of ginsenoside Rd to ginsenoside M1 by snailase hydrolysis and its enhancement effect on insulin secretion in vitro. Pharmazie 70 (5), 340
Li, W., Yan, M. H., Liu, Y., Liu, Z., Wang, Z., Chen, C., et al. (2016). Ginsenoside Rg5 ameliorates cisplatin-induced nephrotoxicity in mice through inhibition of inflammation, oxidative stress, and apoptosis. Nutrients 8 (9), E566. doi:10.3390/nu8090566
Liu, L., Jiang, S., Liu, X., Tang, Q., Chen, Y., Qu, J., et al. (2021). Inflammatory response and oxidative stress as mechanism of reducing hyperuricemia of gardenia jasminoides-poria cocos with network pharmacology. Oxid. Med. Cell. Longev. 2021, 8031319. doi:10.1155/2021/8031319
Liu, P., Xu, H., Shi, Y., Deng, L., and Chen, X. (2020a). Potential molecular mechanisms of Plantain in the treatment of gout and hyperuricemia based on network pharmacology. Evid. Based. Complement. Altern. Med. 2020, 3023127. doi:10.1155/2020/3023127
Liu, X., Mi, X., Wang, Z., Zhang, M., Hou, J., Jiang, S., et al. (2020b). Ginsenoside Rg3 promotes regression from hepatic fibrosis through reducing inflammation-mediated autophagy signaling pathway. Cell. Death Dis. 11 (6), 454. doi:10.1038/s41419-020-2597-7
Lu, C., Min, S., Lusha, Z., Chunxiao, L., Zhirui, F., Wake, C. J., et al. (2020). The protective effects of different compatibility proportions of the couplet medicines for Astragali Radix and Angelica sinensis Radix on myocardial infarction injury. Pharm. Biol. 58 (1), 165–175. doi:10.1080/13880209.2020.1725581
Lu, Y., Bao, T., Mo, J., Ni, J., and Chen, W. (2021). Research advances in bioactive components and health benefits of jujube (Ziziphus jujuba Mill.) fruit. J. Zhejiang Univ. Sci. B 22 (6), 431–449. doi:10.1631/jzus.B2000594
Ma, Z., Wang, Y., Xu, C., Ai, F., Huang, L., Wang, J., et al. (2019). Obesity-related genetic variants and hyperuricemia risk in Chinese men. Front. Endocrinol. 10, 230. doi:10.3389/fendo.2019.00230
Pei, L., Huachong, X., Yucong, S., Li, D., and Xiaoyin, C. (2020). Potential molecular mechanisms of Plantain in the treatment of gout and hyperuricemia based on network pharmacology. Evid Based Alternat. Med. 2020, 3023127. doi:10.1155/2020/3023127
Rekha, U. V., Bhuminathan, S., and Shankar, P. R. (2021). Anticancer activity of "Ziziphus jujuba" - a review. J. Pharm. Res. Int., 261–269. doi:10.9734/jpri/2021/v33i59b34377
Scheepers, L., Jacobsson, L. T. H., Kern, S., Johansson, L., Dehlin, M., and Skoog, I. (2019). Urate and risk of alzheimer's disease and vascular dementia: A population-based study. Alzheimers Dement. 15 (6), 754–763. doi:10.1016/j.jalz.2019.01.014
Simin, F., Sijie, W., Fei, X., and Ping, S. (2022). Natural compounds lower uric acid levels and hyperuricemia: Molecular mechanisms and prospective. Trends Food Sci. Technol. 123, 87–102. doi:10.1016/j.tifs.2022.03.002
Su, W.-Y., Wang, W. T., Lin, X.-H., Lin, X.-x., and Li, W. (2021). Using the synergistic pentobarbital sodium model to explore the sleep-promoting effect of fresh ginseng paste on mice. J. Jilin Agric. Univ. 43 (03), 349–354. doi:10.13327/j.jjlau.2020.5662
Wu, X., Jian, G., Tang, Y., Cheng, H., Wang, N., and Wu, J. (2020). Asymptomatic hyperuricemia and incident congestive heart failure in elderly patients without comorbidities. Nutr. Metab. Cardiovasc. Dis. 30 (4), 666–673. doi:10.1016/j.numecd.2019.12.008
Xu, J. F., Xia, J., Wan, Y., Yang, Y., Wu, J. J., Peng, C., et al. (2022). Vasorelaxant activities and its underlying mechanisms of magnolia volatile oil on rat thoracic aorta based on network pharmacology. Front. Pharmacol. 13, 812716. doi:10.3389/fphar.2022.812716
Yang, C., He, Q., Chen, Z., Qin, J. J., Lei, F., Liu, Y. M., et al. (2022). A bidirectional relationship between hyperuricemia and metabolic dysfunction-associated fatty liver disease. Front. Endocrinol. 13, 821689. doi:10.3389/fendo.2022.821689
Yu, L., Jiang, B. P., Luo, D., Shen, X. C., Guo, S., Duan, J. A., et al. (2012). Bioactive components in the fruits of ziziphus jujuba mill. against the inflammatory irritant action of Euphorbia plants. Phytomedicine 19 (3-4), 239–244. doi:10.1016/j.phymed.2011.09.071
Zhang, C. L., Zhang, J. J., Zhu, Q. F., Guan, H. Y., Yang, Y. X., He, X., et al. (2021). Antihyperuricemia and antigouty arthritis effects of Persicaria capitata herba in mice. Phytomedicine. 93, 153765. doi:10.1016/j.phymed.2021.153765
Zhang, R., Zhan, S., Li, S., Zhu, Z., He, J., Lorenzo, J. M., et al. (2018a). Anti-hyperuricemic and nephroprotective effects of extracts from Chaenomeles sinensis (Thouin) Koehne in hyperuricemic mice. Food Funct. 9 (11), 5778–5790. doi:10.1039/c8fo01480a
Zhang, Y., Jin, L., Liu, J., Wang, W., Yu, H., Li, J., et al. (2018b). Effect and mechanism of dioscin from Dioscorea spongiosa on uric acid excretion in animal model of hyperuricemia. J. Ethnopharmacol. 214, 29–36. doi:10.1016/j.jep.2017.12.004
Keywords: radix ginseng, ziziphus jujube, fresh ginseng paste, hyperuricemia, network pharmacology, molecular docking
Citation: Zhang H, Liu W, Qi S-M, Chi J-F, Gao Q, Lin X-H, Ren S, Wang Z, Lei X-j and Li W (2022) Improved effect of fresh ginseng paste (radix ginseng-ziziphus jujube) on hyperuricemia based on network pharmacology and molecular docking. Front. Pharmacol. 13:955219. doi: 10.3389/fphar.2022.955219
Received: 28 May 2022; Accepted: 10 October 2022;
Published: 25 October 2022.
Edited by:
Francesca Oliviero, University of Padua, ItalyReviewed by:
Javier Fernández-Torres, National Institute of Rehabilitation Luis Guillermo Ibarra Ibarra, MexicoJiangning Hu, Dalian Polytechnic University, China
Copyright © 2022 Zhang, Liu, Qi, Chi, Gao, Lin, Ren, Wang, Lei and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiu-juan Lei, eGl1anVhbmxAamxhdS5lZHUuY24=; Wei Li, bGl3ZWk3NzI3QDEyNi5jb20=
†These authors share first authorship
 Hao Zhang1,2
Hao Zhang1,2 Zi Wang
Zi Wang Wei Li
Wei Li