
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pharmacol. , 02 June 2022
Sec. Ethnopharmacology
Volume 13 - 2022 | https://doi.org/10.3389/fphar.2022.837907
This article is part of the Research Topic Treatment of Infectious Diseases with Bioactive Compounds from Medicinal Plants: Their Mechanisms and Applications View all 11 articles
The increasing and widespread application of antibacterial drugs makes antibiotic resistance a prominent and growing concern in clinical practice. The emergence of multidrug-resistant bacteria presents a global threat. However, the development and use of novel antibacterial agents involves time-consuming and costly challenges that may lead to yet further drug resistance. More recently, researchers have turned to traditional Chinese medicine to stem the rise of antibiotic resistance in pathogens. Many studies have shown traditional Chinese medicines to have significant bacteriostatic and bactericidal effects, with the advantage of low drug resistance. Some of which when combined with antibiotics, have also demonstrated antibacterial activity by synergistic effect. Traditional Chinese medicine has a variety of active components, including flavonoids, alkaloids, phenols, and quinones, which can inhibit the growth of drug-resistant bacteria and be used in combination with a variety of antibiotics to treat various drug-resistant bacterial infections. We reviewed the interaction between the active ingredients of traditional Chinese medicines and antibiotic-resistant bacteria. At present, flavonoids and alkaloids are the active ingredients that have been most widely studied, with significant synergistic activity demonstrated when used in combination with antibiotics against drug-resistant bacteria. The reviewed studies show that traditional Chinese medicine and its active ingredients have antimicrobial activity on antibiotic-resistant bacteria, which may enhance the susceptibility of antibiotic-resistant bacteria, potentially reduce the required dosage of antibacterial agents and the rate of drug resistance. Our results provide direction for finding and developing alternative methods to counteract drug-resistant bacteria, offering a new therapeutic strategy for tackling antibiotic resistance.
In the late 1950s, most Staphylococcus aureus strains became resistant to penicillin (Paul D Stapleton, 2002). Researchers then developed new drugs, such as methicillin and vancomycin, to treat penicillin-resistant bacteria. Unfortunately, the existence of methicillin-resistant S. aureus (MRSA) was first reported in 1961 (Barber, 1961). Antibiotic resistance is a global problem. Although it is a natural process for bacteria to develop antibiotic resistance, antibiotic resistance is accelerated by the misuse and abuse of antibiotics, which makes it more difficult to prevent and control bacterial infections (Piddock, 2012). Currently, more and more infections become complicated to treat or even untreatable, as overuse of antibiotics reduces their effectiveness. Thus far, there is no antibiotic capable of solving the problem of resistant strains, where it is predicted that antibiotic resistance will re-emerge even with the most vigorous research and development of new drugs (Barriere, 2014). Antibiotic resistance leads to higher hospital costs, delayed discharge times and higher mortality rates, where at least 700,000 people die worldwide each year as a result. The report on the review of Antimicrobial Resistance chaired by Jim O’Neill warns that if bacterial drug resistance remains to increase at the rate of today’s levels, 10 million people per year may die of antibiotic resistance by 2050.
In recent years, the exploration of methods to control drug-resistant strains has attracted extensive attention from scholars hoping to find a promising alternative solution. Traditional Chinese medicine (TCM) has attracted the greatest interest among all methods. TCM has a long history and rich experience in treating infectious diseases. The antibacterial action of TCM and its compounds has a complex multi-link, multi-target, and multi-site process. Compared with antibiotics, TCM is characterised with more resources, easier access, lower drug resistance, more active ingredients (Yang et al., 2010; Wu et al., 2019) fewer adverse reactions, and more targets (Messier and Grenier, 2011; Eumkeb et al., 2012a). Many studies have shown that TCM has significant bacteriostatic or bactericidal effects. These effects occur mainly through inhibition of biofilm formation of drug-resistant bacteria, efflux pump system, enzyme activity, and changes in the permeability of bacteria and other drug-resistant mechanisms (Su et al., 2020). Polygonum cuspidatum (Polygonum cuspidatum Sieb. et Zucc.) extracts can exert antibacterial and bactericidal effects by destroying bacterial cell membranes and walls (Su et al., 2015). Extracts from Hypericum perforatum (Hypericum perforatum L.) and Sophora moorcroftiana (Sophora moorcroftiana (Benth.Baker)) also have antibacterial effects, as the extracts can inhibit the growth of drug-resistant bacteria by suppressing the efflux pump system (Wang et al., 2014; Dogan et al., 2019). Resveratrol can inhibit biofilm formation of avian pathogenic Escherichia coli to achieve a bacteriostatic effect (Ruan et al., 2021).
Studies have demonstrated that some TCM can directly inhibit drug-resistant bacteria. However, for TCM with no individually attributed antibacterial activity, if combined with antibacterial drugs, the synergistic effect of TCM can make these TCM play an important role in bacterial infection treatment. The synergistic effect by TCM can also enhance the susceptibility of drug-resistant bacteria to antibiotics and even reverse drug resistance. Studies on the antibacterial effects of pterostilbene and gentamicin alone and in combination showed no significant difference in antibacterial effects. However, when they were combined they completely inhibited the growth of bacteria and had synergistic antibacterial effects (Lee et al., 2017). The synergistic application of TCM and antibiotics in drug-resistant bacteria has stronger antibacterial activity, which is a recognised antibacterial treatment measure (Wagner and Ulrich-Merzenich, 2009). Several alternative antibiotic treatments for bacteria, such as bacteriocins (Cotter et al., 2013), essential oils (Esmael et al., 2020; Puvaca et al., 2021), antibodies (Berghman et al., 2005), and phage therapy (Chang et al., 2018), have been evaluated in studies and confirmed in vitro and with the use of animal models. However, these still present with many issues to consider, including cost, side effects, and safety, where most of them are still far from clinical use. As TCM has already been used clinically with a long history, combining antibiotics and TCM is a promising alternative therapy to resolve antibiotic resistance. As extracts from TCM may contain hundreds of chemical components, the isolation of active compounds under the guidance of bioassays is crucial to study their synergistic effects in detail. This review summarises the effects of flavonoids, alkaloids, phenols, and quinones (chemical structures of key compounds in these classes are shown in Figure 1) combined with antibiotics on bacterial and drug-resistant bacterial infections. It provides the basis for an alternative approach, involving TCM to treat bacterial and drug-resistant bacterial infections in the future, by applying a relatively new and promising option in antibiotic resistant treatment.
Search strategy and research criteria: English articles published from September 2001 to May 2021 were searched in the PubMed database, and related keywords such as: “Traditional Chinese medicine,” “Chinese herbal medicine,” “antibiotics,” “drug-resistant bacteria,” “flavonoids,” “alkaloids,” “phenols,” and “quinones” were used to search the database. The study included published data but excluded TCM treatments for other diseases, such as cancer. 180 English language articles published mainly since 2011 were located which related to the use of components from TCM against drug-resistant bacteria. According to our criteria, we reviewed the abstract and content of the articles, with 115 studies included as references, among which 86 were identified. Most of these papers focus on the synergistic antibacterial activity of the active ingredients of TCM combined with antibiotics against drug-resistant bacteria, and how some active ingredients of TCM can reverse drug resistance.
Synergy judgment criteria: In order to assess if a TCM component in combination with an antibiotic demonstrated a synergistic activity, we used the published definition of the fractional inhibitory concentration index (FICI), which is the sum of the FICs of each of the drugs, which were defined as the minimal inhibition concentration (MIC) of each drug when used in combination divided by the MIC of each drug when used alone, i.e., FICI = (MIC of drug A in combination/MIC of drug A alone) + (MIC of drug B in combination/MIC of drug B alone). FICI were graded as: ≤ 0.5, synergy; > 0.5–≤ 1.0, additive; >1.0–≤ 2.0, indifference; and >2.0, antagonism (Kang et al., 2011).
Flavonoids are compounds of some widely distributed plants and are found in photosynthetic cells, which exist broadly within the plant kingdom and in almost all parts of the plant (Havsteen, 1983). Baicalein and baicalin in the root of Scutellaria baicalensis Georgi, luteolin in the root and stem of Reseda odorata L., and quercetin in the flower and leaf of Camellia sinensis (L.) Kuntze are all flavonoids. For centuries, preparations containing flavonoids as the key physiologically active ingredients have been used by clinicians to treat human diseases. It is reported that flavonoids have anti-inflammatory and antibacterial effects, whilst potentially having antiviral, antioxidant and free radical scavenging abilities (Kumar and Pandey, 2013). Researchers have also actively investigated the antibacterial effects of flavonoids in combination with antibiotics.
Mai Fujita et al. (2005) demonstrated that the combination of baicalein with tetracycline and β-lactam antibiotics significantly reduced the MIC of MRSA such that it played an antibacterial role. When baicalein and ciprofloxacin were combined to treat MRSA infection, 12 of the 20 drug-resistant strains had FICI≤0.5, which mainly inhibited the efflux of ciprofloxacin by suppressing the efflux pump, thereby exerting a synergistic anti-MRSA effect (Chan et al., 2011). The main mechanism of the combination of active ingredients of TCM and antibiotics is shown in Figure 2. Qian et al. (2015) also found that the combined application of baicalein and penicillin can resist penicillinase-producing MRSA or S. aureus infection. When the concentration of baicalein increased from 8 μg/ml to 32 μg/ml, the MIC of penicillin decreased from 64 μg/ml to 4 μg/ml, significantly improving the resistant bacteria’s susceptibility to penicillin. Recent studies have demonstrated that linezolid and baicalein can inhibit biofilm formation in vivo to play an anti-MRSA role (Liu T. et al., 2020). Baicalin has similar effects to baicalein, and if Baicalin is used in combination with oxytetracycline and tetracycline, it can resist S. aureus infection, while in combination with β-lactam antibiotics, it yields anti-MRSA activity (Iain and Liu, 2000; Novy et al., 2011).
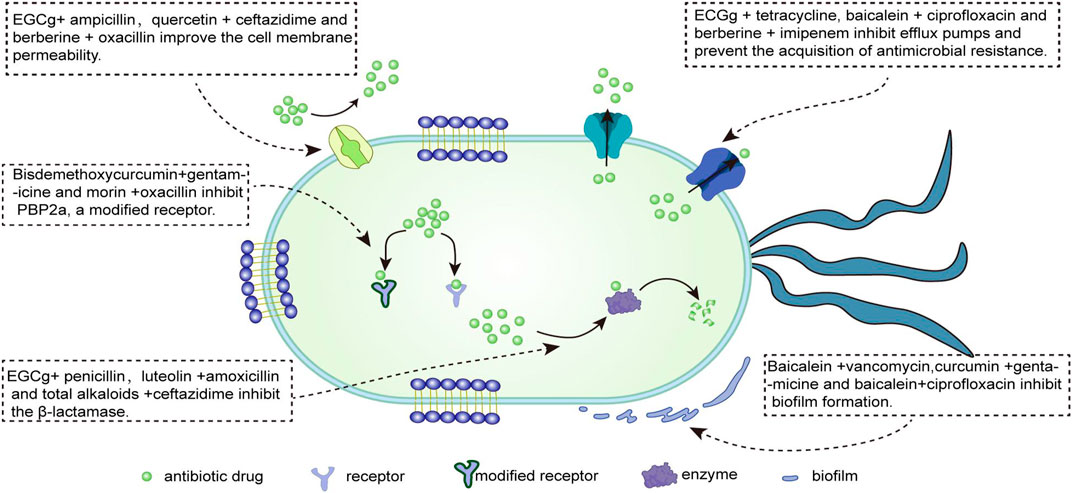
FIGURE 2. The major mechanism and target of the antibacterial effect of antibiotics combined with active ingredients of traditional Chinese medicine.
Usman Amin et al. (2016) demonstrated synergistic effects of luteolin and quercetin combined with ceftriaxone and imipenem against MRSA. In addition, luteolin combined with ampicillin, oxacillin, and gentamicin can synergically enhance the antibacterial action of aminoglycosides and β-lactam antibiotics against MRSA. The FICI of the combination of
It has been reported (Kang et al., 2011; Cai et al., 2018; Vivekanandan et al., 2018) that silibinin, an extract of Silybum marianum (L.) Gaertn., has anti-MRSA activity when combined with oxacillin or ampicillin. Another extract, silymarin, can improve the toxicity of linezolid and synergistic anti-MRSA infection, while a high concentration silibinin with kanamycin can inhibit the growth of S. aureus. Pimchan et al. (2017) demonstrated a synergistic effect between α-mangostin and ceftazidime in A. baumannii. The FICI of the combination of α-mangiferin and oxacillin against oxacillin-resistant Staphylococcus saprophyticus was 0.37. The number of bacterial colonies decreased by the combination of 2 μg/ml α-mangostin and 16 μg/ml oxacillin, and in the time-kill curves test ≥2 log10 cfu/ml also verified the synergy. When α-mangostin is combined with gentamicin and vancomycin hydrochloride, it can help inhibit vancomycin-resistant Enterococci (VRE) and MRSA infection, respectively (Sakagami et al., 2005; Phitaktim et al., 2016). Table 1 lists the antibacterial effects of flavonoids combined with antibiotics.
Alkaloids are components of botanical drugs and are widely distributed in nature. They are organic compounds with biological activity and are present within a wide range of plants, bacteria, and fungi (Qiu et al., 2014). Berberine is extracted from Berberis vulgaris L., total alkaloids from Sophora alopecuroides L., and tetrandrine from Stephania tetrandra S. Moore are common alkaloids. Several clinical studies have reported that alkaloids have anti-inflammatory (Souza et al., 2020), antibacterial activities (Liu Y. et al., 2020) and antiviral (Gorpenchenko et al., 2019) pharmacological effects. Studies have shown that these alkaloid compounds are important in enhancing antibiotic effects for treating infections (Cushnie et al., 2014). In recent years, researchers have explored cooperative applications of alkaloids and antibiotics to fight against bacterial resistance.
Hyeon-Hee et al. (2005) showed the anti-MRSA effect of berberine. The FICI of berberine combined with ampicillin (0.625) had an additive effect, whereas if it joined with oxacillin (0.5) it had a synergistic effect. Some scholars have found that berberine combined with azithromycin has a synergistic antibacterial effect on MRSA and P. aeruginosa, and if it paired with levofloxacin, it could resist MRSA infection. The combination of ¼ MIC berberine and
Khameneh et al. (2015) demonstrated that the co-application of piperine and gentamicin nanoliposomes on MRSA had a significant synergistic antibacterial effect. Some researchers have shown that low-dose total alkaloids of Sophora alopecuroides L. and ciprofloxacin have synergistic antibacterial activity against multidrug-resistant E. coli. Total alkalids can enhance bacterial susceptibility to ciprofloxacin and cooperate with cefotaxime and ceftazidime against extended-spectrum β-lactamase (ESBL)-producing E. coli infection (Zhou et al., 2013; Pourahmad Jaktaji and Mohammadi, 2018). In time-kill curve tests, Zhang et al. (2010) showed that the combined application of 30 μg/ml tetrandrine and ketoconazole on drug-resistant Candida had synergistic antibacterial effects in vitro and in vivo but had no bactericidal effect. Tetrandrine and cefazolin in bisbenzylisoquinoline alkaloids presented a considerable synergistic effects against 90% of 10 clinically isolated MRSA strains, with the FICI between 0.188 and 0.625, while demethyltetrandrine and cefazolin had respective additive activities against 50% and 90% of tested MRSA strains, with the FICI ranging from 1.5 to 2.0 (Zuo et al., 2011). Another compound from TCM, called sanguinarine, can restore antibacterial activity of ampicillin, oxacillin, norfloxacin, and ciprofloxacin to treat MRSA by inhibiting the growth of drug-resistant bacteria (Obiang-Obounou et al., 2011). Table 2 lists the antibacterial effects of the above alkaloids combined with antibiotics.
Phenolic compounds are some of the most diverse bioactive secondary metabolites in medicinal plants. They may also be a part of or the main component that contributes to a plants’ bioactivity, with high antibacterial potential (Pinheiro et al., 2018). Phenolic compounds include: epigallocatechin gallate (EGCg), magnolol and honokiol, and eugenol, extracted from Camellia sinensis (L.) Kuntze, Magnolia officinalis Rehder & E.H.Wilson, and Syzygium aromaticum (L.) Merr. & L.M.Perry, respectively. Studies have found that they have anti-inflammatory, antibacteria and antioxidant effects (Daglia, 2012). These compounds may also be used to inhibit or kill pathogenic microorganisms (Marino et al., 2001). Researchers have also investigated the application of phenolic compounds with antibacterial drugs in the treatment of bacterial infections.
Hu et al. (Hu et al., 2001; 2002) demonstrated in 2001 that epigallocatechin gallate (EGCg) could be used together with β-lactam antibiotics, such as ampicillin or sulbactam for the treatment of MRSA infection. EGCg can also be combined with carbapenem antibiotics such as imipenem or panipenem in the treatment of MRSA infection, and reverse MRSA resistance. When EGCg is paired with oxytetracycline it has antibacterial effects on MRSA. EGCg at 4 μg/ml showed synergistic and additive effects on six and two clinically tested MRSA strains, respectively, with the FICI from 0.288 to 0.527 (Novy et al., 2013). A study showed that EGCg can further inhibit penicillinase to protect the antibacterial activity of penicillin and ampicillin against penicillinase-producing S. aureus (Zhao et al., 2002). It has been reported (Sudano Roccaro et al., 2004) that 50 μg/ml EGCg (
Kim et al. (2015) demonstrated that 10 μg/ml magnolol and 25 μg/ml honokiol combined with oxacillin has synergistic effects on MRSA. This application can increase the susceptibility of β-lactam antibiotics to MRSA. In vivo and in vitro experiments have demonstrated that the survival rate for honokiol combined with fluconazole in the treatment of fluconazole-resistant C. albicans infection reached 100%, compared with 20% for honokiol-treated or control group of mice over a period of 5 days (Jin et al., 2010). Sousa Silveira et al. (2020) found that thymol and tetracycline had an anti-S. aureus effect. In this study, the results of a fumigation bioassay showed that thymol had an obvious toxic effect on Drosophila melanogaster within 48 h of exposure with an EC50 (concentration for 50% of maximal effect) value of 17.96 μg/ml. Another study, showed the combination of mupirocin and thymol can enhance the antibacterial activity of mupirocin against MRSA (Kifer et al., 2016). Hemaiswarya and Doble (2009) found that eugenol combined with β-lactam antibiotics such as vancomycin, ampicillin, or oxacillin, had a synergistic antibacterial effect on Gram-negative bacilli. Some scholars (Wang et al., 2018; Dhara and Tripathi, 2020) showed that eugenol combined with colistin enhanced the antibacterial activity of the antibiotics against colistin-resistant E. coli, while the combination of eugenol with cefotaxime and ciprofloxacin could resist ESBL-producing quinolone-resistant pathogenic Enterobacteria, with FICI ≤0.5. Khan et al. (2019) demonstrated a synergistic effect of low doses (100 μg/ml) of eugenol together with amphotericin B (0.05 μg/ml) against C. albicans, with a FICI of 0.27. However, methyl gallate of Galla Rhois (Rhus chinensis Mill.), or carvacrol and nalidixic acid combination had a synergistic or partial synergistic effect (FICI = 0.31–0.75) on pathogens resistant to nalidixic acid, whereas methyl gallate or carvacrol restored the antibacterial activity of nalidixic acid (Choi et al., 2009).
Bahari et al. (2017) showed that sub-MIC of curcumin combined with azithromycin and gentamicin had a synergistic effect on P. aeruginosa PAO1. Moreover, the combination of sub-MIC curcumin and ceftazidime had a synergistic effect on P. aeruginosa PAO1 with a FICI of 0.26, and its combination with ciprofloxacin had a FICI of an additive effect (Roudashti et al., 2017). Several studies (Kaur et al., 2018; Itzia Azucena et al., 2019; Sundaramoorthy et al., 2020) showed that curcumin itself did not affect bacterial growth, but when combined with ceftazidime could resist enterotoxin E. coli infection. When combined with salicylate and colistin, curcumin could reduce the biological load of colisin-resistant E. coli U3790 and K. pneumoniae BC936. In addition, curcumin has a synergistic antibacterial effect on A. baumannii when paired with colistin. In another study, Wang et al. (Wang et al., 2020) demonstrated that the combination of
Abu El-Wafa et al. (2020) showed that the combination of phenolic extracts of pomegranate (Punica granatum L.) and rosemary (Rosmarinus officinalis L.) with piperacillin, ceftazidime, imipenem, gentamicin, and levofloxacin was effective in treating against P. aeruginosa PS-1 and exhibited a synergistic effect (FICI ≤0.5), which radically reduced the MIC of P. aeruginosa. Liu et al. (2016) found that the combination of salvianolic acid salt in Salvia miltiorrhiza (Salvia miltiorrhiza Bge.) and ampicillin applied to MRSA had the best antibacterial effects, which could also reverse MRSA resistance. Table 3 lists the antibacterial effects of the above phenolic compounds combined with antibiotics.
Quinone compounds in TCM can be divided into four types: benzoquinone, naphthoquinone, phenanthrene quinone, and anthraquinone. Anthraquinone and naphthoquinone are widely used in antibacterial treatment. Anthraquinone compounds from various plants were reported to have antibacterial activity (Novais et al., 2018) and anti-inflammatory, antifungal and antiviral effects (Li and Jiang, 2018). Naphthoquinone and naphthoquinone derivatives (Janeczko et al., 2016) were also reported to have antibacterial activity. Rhein extracted from Rheum palmatum L., resveratrol from the rhizome of Polygonum cuspidatum Sieb. et Zucc., and cryptotanshinone from Salvia miltiorrhiza Bge. are quinones. Quinone compounds in combination with antibiotics have been developed as a new measure for treating antibiotic resistance.
Joung et al. (2012) demonstrated that the FICI of rhein combined with ampicillin or oxacillin for all MRSA strains was 0.28–1 and 0.18–1, respectively and showed a synergistic or partial synergistic effect. Cannatelli et al. (2018) reported that resveratrol had no obvious intrinsic antibacterial activity but displayed synergistic effects with colistin on colistin-resistant Gram-negative bacilli of different species. Resveratrol oxide combined with vancomycin and ciprofloxacin had a synergistic effect on MRSA. It was partially additive or synergistic for the combination of resveratrol oxide with ampicillin, oxacillin, and norfloxacin. These combinations completely inhibited the growth of bacteria after 24 h (Joung et al., 2015). Studies have found that hypericin and β-lactam antibiotics such as oxacillin have anti-MRSA ability (Wang et al., 2019). Cha et al. (2014) demonstrated that cryptotanshinone combined with ampicillin, oxacillin, or vancomycin had synergistic effects on methicillin-resistant and vancomycin-resistant S. aureus and greatly inhibited the growth of bacteria. In addition, cryptotanshinone, together with gentamicin and streptomycin at safe doses (gentamicin ≤12 μg/ml and streptomycin ≤20 μg/ml) had a synergistic antibacterial effect on S. aureus. It reduced the resistance of aminoglycoside antibiotics to drug-resistant S. aureus, while the combination of cryptotanshinone with fosfomycin showed synergistic effect on fosfomycin-sensitive and fosfomycin-resistant S. aureus (FICI, 0.3125–0.375) (Teng et al., 2018; Ruan et al., 2020). Table 4 lists the antibacterial effects of the above quinones in combination with antibiotics.
Lu et al. (2013) demonstrated that sodium new houttuyfonate could be synergistic with cephalosporin, meropenem, oxacillin, and netilmicin against MRSA infection. The median FIC of the checkerboard method was 0.38, 0.38, 0.25, and 0.38, respectively. Several studies (Jiang et al., 2011; Li et al., 2011; Wei et al., 2020) reported that artesunate combined with oxacillin and ampicillin had a synergistic antibacterial effect on MRSA. Combined with β-lactam antibiotics such as ampicillin, artesunate could also inhibit E. coli infection and enhance the antibacterial activity of fluoroquinolones against multidrug-resistant E. coli. The combination of 3-benzylchroman derivatives from the Chinese drug, Caesalpinia sappan L., with the aminoglycoside antibiotic can also be effective against MRSA. Morin, and trans-cinnamaldehyde combined with oxacillin has shown a synergistic effect against MRSA and potential for reversing the drug resistance of MRSA. Magnolia officinalis (Magnolia officinalis Rehder & E.H.Wilson) and Verbena (Verbena officinalis L.) extracts combined with oxacillin have otherwise showed a synergistic effect with partial efficacy against MRSA infection, where the colony number decreased by 3log10 cfu/mL (DPS-1 and DPS-3) after a treatment with a combination of
TCM has great antibacterial potential, with low toxicity, low drug resistance, and abundant resources. With further research on the mechanism of bacterial drug resistance and the continuous progress in the extraction technology of effective ingredients of TCM, the combined application of various active ingredients or compounds of TCM and antibiotics in the control of bacterial or drug-resistant bacteria infection has been widely studied. The active ingredients of TCM act as synergists by enhancing the antibacterial activity, improve the therapeutic effect and reduce the dosage of antibiotics and adverse reactions. At present, all studies on antibacterial or bacteriostatic effects from the combination of active ingredients of TCM and antibiotics have been conducted in vitro. There is insufficient evidence to prove the effectiveness, stability, selective toxicity, and targeted availability of these combinations in the human body. Therefore, further in vivo studies and animal models are needed. This paper summarises the interaction between different compounds of TCM, such as flavonoids, alkaloids, phenols and quinones, with antibiotics in the fight against drug-resistant bacteria. Using different active TCM ingredients with the same antibiotic, has a synergistic effect on drug-resistant bacteria. The same TCM ingredient can also have a synergistic antibacterial effect with different antibiotics. The above studies found that the combination of quercetin and berberine with antibiotics yielded good synergistic antibacterial effects and a broad antibacterial spectrum. Therefore, as the most researched active ingredients of TCM with strong antibacterial effects, flavonoids and alkaloids will be promising antibacterial choices when used in combination with antibiotics. This provides a new avenue to solve the problem of bacterial resistance through TCM and an important theoretical basis for finding alternative methods to counteract resistant bacteria. The combined use of TCM and antibiotics has become a new and alternative trend for antibacterial treatment. In the face of the current drug resistance crisis and the dilemma of new drug research and development, finding a more effective and safer alternative for the treatment of drug-resistant bacterial infection is crucial. The in-depth study of the synergistic antibacterial effect and synergistic mechanism of the combination of active components of TCM and antibiotics in vivo, may become an important research direction in the future.
JG, SD, and JL conceived and designed the work; XJ and FQ coordinated technical support and funding; JL wrote the manuscript and created the tables and figures; SF offered advice and explanation; XL checked the language of the article. All authors contributed to the article and approved the submitted version.
This work was funded by the National Natural Science Foundation of China (Grant Nos. 32170119 and 31870135).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abreu, A. C., Saavedra, M. J., Simões, L. C., and Simões, M. (2016). Combinatorial Approaches with Selected Phytochemicals to Increase Antibiotic Efficacy against Staphylococcus aureus Biofilms. Biofouling 32, 1103–1114. doi:10.1080/08927014.2016.1232402
Abu El-Wafa, W. M., Ahmed, R. H., and Ramadan, M. A. (2020). Synergistic Effects of Pomegranate and Rosemary Extracts in Combination with Antibiotics against Antibiotic Resistance and Biofilm Formation of Pseudomonas aeruginosa. Braz J. Microbiol. 51, 1079–1092. doi:10.1007/s42770-020-00284-3
Bahari, S., Zeighami, H., Mirshahabi, H., Roudashti, S., and Haghi, F. (2017). Inhibition of Pseudomonas aeruginosa Quorum Sensing by Subinhibitory Concentrations of Curcumin with Gentamicin and Azithromycin. J. Glob. Antimicrob. Resist 10, 21–28. doi:10.1016/j.jgar.2017.03.006
Barber, M. (1961). Methicillin-resistant Staphylococci. J. Clin. Pathol. 14, 385–393. doi:10.1136/jcp.14.4.385
Barriere, S. L. (2014). Clinical, Economic and Societal Impact of Antibiotic Resistance. Expert Opin. Pharmacother. doi:10.1517/14656566.2015.983077
Berghman, L. R., Abi-Ghanem, D., and Ricke, S. C. (2005). Antibodies: An Alternative for Antibiotics? Poult. Sci.
Buommino, E., Vollaro, A., Nocera, F. P., Lembo, F., Dellagreca, M., De Martino, L., et al. (2021). Synergistic Effect of Abietic Acid with Oxacillin against Methicillin-Resistant Staphylococcus Pseudintermedius. Antibiot. (Basel) 10. doi:10.3390/antibiotics10010080
Cai, J. Y., Li, J., Hou, Y. N., Ma, K., Yao, G. D., Liu, W. W., et al. (2018). Concentration-dependent Dual Effects of Silibinin on Kanamycin-Induced Cells Death in Staphylococcus aureus. Biomed. Pharmacother. 102, 782–791. doi:10.1016/j.biopha.2018.03.133
Cannatelli, A., Principato, S., Colavecchio, O. L., Pallecchi, L., and Rossolini, G. M. (2018). Synergistic Activity of Colistin in Combination with Resveratrol against Colistin-Resistant Gram-Negative Pathogens. Front. Microbiol. 9, 1808. doi:10.3389/fmicb.2018.01808
Cha, J. D., Lee, J. H., Choi, K. M., Choi, S. M., and Park, J. H. (2014). Synergistic Effect between Cryptotanshinone and Antibiotics against Clinic Methicillin and Vancomycin-Resistant Staphylococcus aureus. Evid. Based Complement. Altern. Med. 2014, 450572. doi:10.1155/2014/450572
Chan, B. C., Ip, M., Lau, C. B., Lui, S. L., Jolivalt, C., Ganem-Elbaz, C., et al. (2011). Synergistic Effects of Baicalein with Ciprofloxacin against NorA Over-expressed Methicillin-Resistant Staphylococcus aureus (MRSA) and Inhibition of MRSA Pyruvate Kinase. J. Ethnopharmacol. 137, 767–773. doi:10.1016/j.jep.2011.06.039
Chang, R. Y. K., Wallin, M., Lin, Y., Leung, S. S. Y., Wang, H., Morales, S., et al. (2018). Phage Therapy for Respiratory Infections. Adv. Drug Deliv. Rev. 133, 76–86. doi:10.1016/j.addr.2018.08.001
Choi, J. G., Kang, O. H., Lee, Y. S., Oh, Y. C., Chae, H. S., Jang, H. J., et al. (2009). Antibacterial Activity of Methyl Gallate Isolated from Galla Rhois or Carvacrol Combined with Nalidixic Acid against Nalidixic Acid Resistant Bacteria. Molecules 14, 1773–1780. doi:10.3390/molecules14051773
Cotter, P. D., Ross, R. P., and Hill, C. (2013). Bacteriocins - a Viable Alternative to Antibiotics? Nat. Rev. Microbiol. 11, 95–105. doi:10.1038/nrmicro2937
Cushnie, T. P., Cushnie, B., and Lamb, A. J. (2014). Alkaloids: an Overview of Their Antibacterial, Antibiotic-Enhancing and Antivirulence Activities. Int. J. Antimicrob. Agents 44, 377–386. doi:10.1016/j.ijantimicag.2014.06.001
da Costa Júnior, S. D., Da Silva, W. R. C., Da Silva, A. M. C. M., Maciel, M. A. V., and Cavalcanti, I. M. F. (2020). Synergistic Effect between Usnic Acid and Polymyxin B against Resistant Clinical Isolates of Pseudomonas aeruginosa. Evid. Based Complement. Altern. Med. 2020, 9852145. doi:10.1155/2020/9852145
Daglia, M. (2012). Polyphenols as Antimicrobial Agents. Curr. Opin. Biotechnol. 23, 174–181. doi:10.1016/j.copbio.2011.08.007
Dhara, L., and Tripathi, A. (2020). The Use of Eugenol in Combination with Cefotaxime and Ciprofloxacin to Combat ESBL-Producing Quinolone-Resistant Pathogenic Enterobacteriaceae. J. Appl. Microbiol. 129, 1566–1576. doi:10.1111/jam.14737
Dogan, S., Gokalsin, B., Senkardes, I., Dogan, A., and Sesal, N. C. (2019). Anti-Quorum Sensing and Anti-biofilm Activities of Hypericum perforatum Extracts against Pseudomonas aeruginosa. J. Ethnopharmacol. 235, 293–300.
Dziedzic, A., Wojtyczka, R. D., and Kubina, R. (2015). Inhibition of Oral Streptococci Growth Induced by the Complementary Action of Berberine Chloride and Antibacterial Compounds. Molecules 20, 13705–13724. doi:10.3390/molecules200813705
Esmael, A., Hassan, M. G., Amer, M. M., Abdelrahman, S., Hamed, A. M., Abd-Raboh, H. A., et al. (2020). Antimicrobial Activity of Certain Natural-Based Plant Oils against the Antibiotic-Resistant Acne Bacteria. Saudi J. Biol. Sci. 27, 448–455. doi:10.1016/j.sjbs.2019.11.006
Eumkeb, G., Siriwong, S., Phitaktim, S., Rojtinnakorn, N., and Sakdarat, S. (2012a). Synergistic Activity and Mode of Action of Flavonoids Isolated from Smaller Galangal and Amoxicillin Combinations against Amoxicillin-Resistant Escherichia coli. J. Appl. Microbiol. 112, 55–64. doi:10.1111/j.1365-2672.2011.05190.x
Eumkeb, G., Siriwong, S., and Thumanu, K. (2012b). Synergistic Activity of Luteolin and Amoxicillin Combination against Amoxicillin-Resistant Escherichia coli and Mode of Action. J. Photochem Photobiol. B 117, 247–253. doi:10.1016/j.jphotobiol.2012.10.006
Fatemi, N., Sharifmoghadam, M. R., Bahreini, M., Khameneh, B., and Shadifar, H. (2020). Antibacterial and Synergistic Effects of Herbal Extracts in Combination with Amikacin and Imipenem against Multidrug-Resistant Isolates of Acinetobacter. Curr. Microbiol. 77, 1959–1967. doi:10.1007/s00284-020-02105-0
Fujita, M., Shiota, S., Hatano, T., Kuroda, T., Hatano, T., Mizushima, T. T., et al. (2005). Remarkable Synergies between Baicalein and Tetracycline, and Baicalein and Beta-Lactams against Methicillin-Resistant Staphylococcus aureus. Microbiol. Immunol. 49, 391–396. doi:10.1111/j.1348-0421.2005.tb03732.x
Gorpenchenko, T. Y., Grigorchuk, V. P., Bulgakov, D. V., Tchernoded, G. K., and Bulgakov, V. P. (2019). Tempo-Spatial Pattern of Stepharine Accumulation in Stephania Glabra Morphogenic Tissues. Int. J. Mol. Sci. 20. doi:10.3390/ijms20040808
Havsteen, B. (1983). Flavonoids, a Class of Natural Products of High Pharmacological Potency. Biochem. Pharmacol. 32, 1141–1148. doi:10.1016/0006-2952(83)90262-9
Hemaiswarya, S., and Doble, M. (2009). Synergistic Interaction of Eugenol with Antibiotics against Gram Negative Bacteria. Phytomedicine 16, 997–1005. doi:10.1016/j.phymed.2009.04.006
Hu, Z. Q., Zhao, W. H., Asano, N., Yoda, Y., Hara, Y., and Shimamura, T. (2002). Epigallocatechin Gallate Synergistically Enhances the Activity of Carbapenems against Methicillin-Resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 46, 558–560. doi:10.1128/aac.46.2.558-560.2002
Hu, Z. Q., Zhao, W. H., Hara, Y., Shimamura, T., Hara, Y., and Shimamura, T. (2001). Epigallocatechin Gallate Synergy with Ampicillin/sulbactam against 28 Clinical Isolates of Methicillin-Resistant Staphylococcus aureus. J. Antimicrob. Chemother. 48, 361–364. doi:10.1093/jac/48.3.361
Iain, X., and Liu, D. G. D. a. R. M. E. R. (2000). Baicalin Synergy with B-Lactam Antibiotics against Methicillinresistant Staphylococcus aureus and Other B-Lactam-Resistant Strains of S. aureus. J. Pharm. Pharmacol. 52, 361±366.
Itzia Azucena, R. C., José Roberto, C. L., Martin, Z. R., Rafael, C. Z., Leonardo, H. H., Gabriela, T. P., et al. (2019). Drug Susceptibility Testing and Synergistic Antibacterial Activity of Curcumin with Antibiotics against Enterotoxigenic Escherichia coli. Antibiot. (Basel) 8. doi:10.3390/antibiotics8020043
Janeczko, M., Demchuk, O. M., Strzelecka, D., Kubiński, K., and Masłyk, M. (2016). New Family of Antimicrobial Agents Derived from 1,4-naphthoquinone. Eur. J. Med. Chem. 124, 1019–1025. doi:10.1016/j.ejmech.2016.10.034
Jiang, W., Li, B., Zheng, X., Liu, X., Cen, Y., Li, J., et al. (2011). Artesunate in Combination with Oxacillin Protect Sepsis Model Mice Challenged with Lethal Live Methicillin-Resistant Staphylococcus aureus (MRSA) via its Inhibition on Proinflammatory Cytokines Release and Enhancement on Antibacterial Activity of Oxacillin. Int. Immunopharmacol. 11, 1065–1073. doi:10.1016/j.intimp.2011.02.028
Jin, J., Guo, N., Zhang, J., Ding, Y., Tang, X., Liang, J., et al. (2010). The Synergy of Honokiol and Fluconazole against Clinical Isolates of Azole-Resistant Candida Albicans. Lett. Appl. Microbiol. 51, 351–357. doi:10.1111/j.1472-765X.2010.02900.x
Joung, D. K., Choi, S. H., Kang, O. H., Kim, S. B., Mun, S. H., Seo, Y. S., et al. (2015). Synergistic Effects of Oxyresveratrol in Conjunction with Antibiotics against Methicillin-Resistant Staphylococcus aureus. Mol. Med. Rep. 12, 663–667. doi:10.3892/mmr.2015.3345
Joung, D. K., Joung, H., Yang, D. W., Kwon, D. Y., Choi, J. G., Woo, S., et al. (2012). Synergistic Effect of Rhein in Combination with Ampicillin or Oxacillin against Methicillin-Resistant Staphylococcus aureus. Exp. Ther. Med. 3, 608–612. doi:10.3892/etm.2012.459
Joung, D. K., Kang, O. H., Seo, Y. S., Zhou, T., Lee, Y. S., Han, S. H., et al. (2016). Luteolin Potentiates the Effects of Aminoglycoside and β-lactam Antibiotics against Methicillin-Resistant Staphylococcus aureus In Vitro. Exp. Ther. Med. 11, 2597–2601. doi:10.3892/etm.2016.3212
Kang, H. K., Kim, H. Y., and Cha, J. D. (2011). Synergistic Effects between Silibinin and Antibiotics on Methicillin-Resistant Staphylococcus aureus Isolated from Clinical Specimens. Biotechnol. J. 6, 1397–1408. doi:10.1002/biot.201000422
Kaur, A., Sharma, P., and Capalash, N. (2018). Curcumin Alleviates Persistence of Acinetobacter Baumannii against Colistin. Sci. Rep. 8, 11029. doi:10.1038/s41598-018-29291-z
Khameneh, B., Iranshahy, M., Ghandadi, M., Ghoochi Atashbeyk, D., Fazly Bazzaz, B. S., and Iranshahi, M. (2015). Investigation of the Antibacterial Activity and Efflux Pump Inhibitory Effect of Co-loaded Piperine and Gentamicin Nanoliposomes in Methicillin-Resistant Staphylococcus aureus. Drug Dev. Ind. Pharm. 41, 989–994. doi:10.3109/03639045.2014.920025
Khan, S. N., Khan, S., Misba, L., Sharief, M., Hashmi, A., and Khan, A. U. (2019). Synergistic Fungicidal Activity with Low Doses of Eugenol and Amphotericin B against Candida Albicans. Biochem. Biophys. Res. Commun. 518, 459–464. doi:10.1016/j.bbrc.2019.08.053
Kifer, D., Mužinić, V., and Klarić, M. Š. (2016). Antimicrobial Potency of Single and Combined Mupirocin and Monoterpenes, Thymol, Menthol and 1,8-cineole against Staphylococcus aureus Planktonic and Biofilm Growth. J. Antibiot. (Tokyo) 69, 689–696. doi:10.1038/ja.2016.10
Kim, S. Y., Kim, J., Jeong, S. I., Jahng, K. Y., and Yu, K. Y. (2015). Antimicrobial Effects and Resistant Regulation of Magnolol and Honokiol on Methicillin-Resistant Staphylococcus aureus. Biomed. Res. Int. 2015, 283630. doi:10.1155/2015/283630
Kumar, L., Chhibber, S., and Harjai, K. (2013). Zingerone Inhibit Biofilm Formation and Improve Antibiofilm Efficacy of Ciprofloxacin against Pseudomonas aeruginosa PAO1. Fitoterapia 90, 73–78. doi:10.1016/j.fitote.2013.06.017
Kumar, S., and Pandey, A. K. (20132013). Chemistry and Biological Activities of Flavonoids: an Overview. ScientificWorldJournal 2013, 162750. doi:10.1155/2013/162750
Kuok, C. F., Hoi, S. O., Hoi, C. F., Chan, C. H., Fong, I. H., Ngok, C. K., et al. (2017). Synergistic Antibacterial Effects of Herbal Extracts and Antibiotics on Methicillin-Resistant Staphylococcus aureus: A Computational and Experimental Study. Exp. Biol. Med. (Maywood) 242, 731–743. doi:10.1177/1535370216689828
Lee, W. X., Basri, D. F., and Ghazali, A. R. (2017). Bactericidal Effect of Pterostilbene Alone and in Combination with Gentamicin against Human Pathogenic Bacteria. Molecules 22. doi:10.3390/molecules22030463
Li, B., Yao, Q., Pan, X. C., Wang, N., Zhang, R., Li, J., et al. (2011). Artesunate Enhances the Antibacterial Effect of {beta}-Lactam Antibiotics against Escherichia coli by Increasing Antibiotic Accumulation via Inhibition of the Multidrug Efflux Pump System AcrAB-TolC. J. Antimicrob. Chemother. 66, 769–777. doi:10.1093/jac/dkr017
Li, X., Song, Y., Wang, L., Kang, G., Wang, P., Yin, H., et al. (2021). A Potential Combination Therapy of Berberine Hydrochloride with Antibiotics against Multidrug-Resistant Acinetobacter Baumannii. Front. Cell. Infect. Microbiol. 11, 660431. doi:10.3389/fcimb.2021.660431
Li, Y., Huang, J., Li, L., and Liu, L. (2017). Synergistic Activity of Berberine with Azithromycin against Pseudomonas Aeruginosa Isolated from Patients with Cystic Fibrosis of Lung In Vitro and In Vivo. Cell. Physiol. Biochem. 42, 1657–1669. doi:10.1159/000479411
Li, Y., and Jiang, J. G. (2018). Health Functions and Structure-Activity Relationships of Natural Anthraquinones from Plants. Food Funct. 9, 6063–6080. doi:10.1039/c8fo01569d
Liang, R. M., Yong, X. L., Duan, Y. Q., Tan, Y. H., Zeng, P., Zhou, Z. Y., et al. (2014). Potent In Vitro Synergism of Fusidic Acid (FA) and Berberine Chloride (BBR) against Clinical Isolates of Methicillin-Resistant Staphylococcus aureus (MRSA). World J. Microbiol. Biotechnol. 30, 2861–2869. doi:10.1007/s11274-014-1712-2
Liu, Q. Q., Han, J., Zuo, G. Y., Wang, G. C., and Tang, H. S. (2016). Potentiation Activity of Multiple Antibacterial Agents by Salvianolate from the Chinese Medicine Danshen against Methicillin-Resistant Staphylococcus aureus (MRSA). J. Pharmacol. Sci. 131, 13–17. doi:10.1016/j.jphs.2015.10.009
Liu, T., Luo, J., Bi, G., Du, Z., Kong, J., and Chen, Y. (2020a). Antibacterial Synergy between Linezolid and Baicalein against Methicillin-Resistant Staphylococcus aureus Biofilm In Vivo. Microb. Pathog. 147, 104411. doi:10.1016/j.micpath.2020.104411
Liu, Y., Cui, Y., Lu, L., Gong, Y., Han, W., and Piao, G. (2020b). Natural Indole-Containing Alkaloids and Their Antibacterial Activities. Arch. Pharm. Weinh. 353, e2000120. doi:10.1002/ardp.202000120
Lu, X., Yang, X., Li, X., Lu, Y., Ren, Z., Zhao, L., et al. (2013). In Vitro activity of Sodium New Houttuyfonate Alone and in Combination with Oxacillin or Netilmicin against Methicillin-Resistant Staphylococcus aureus. PLoS One 8, e68053. doi:10.1371/journal.pone.0068053
Marino, M., Bersani, C., and Comi, G. (2001). Impedance Measurements to Study the Antimicrobial Activity of Essential Oils from Lamiaceae and Compositae. Int. J. Food Microbiol. 67, 187–195. doi:10.1016/s0168-1605(01)00447-0
Messier, C., and Grenier, D. (2011). Effect of Licorice Compounds Licochalcone A, Glabridin and Glycyrrhizic Acid on Growth and Virulence Properties of Candida Albicans. Mycoses 54, e801–6. doi:10.1111/j.1439-0507.2011.02028.x
Morita, Y., Nakashima, K., Nishino, K., Kotani, K., Tomida, J., Inoue, M., et al. (2016). Berberine Is a Novel Type Efflux Inhibitor Which Attenuates the MexXY-Mediated Aminoglycoside Resistance in Pseudomonas aeruginosa. Front. Microbiol. 7, 1223. doi:10.3389/fmicb.2016.01223
Mun, S. H., Lee, Y. S., Han, S. H., Lee, S. W., Cha, S. W., Kim, S. B., et al. (2015). In Vitro Potential Effect of Morin in the Combination with β-Lactam Antibiotics against Methicillin-Resistant Staphylococcus aureus. Foodborne Pathog. Dis. 12, 545–550. doi:10.1089/fpd.2014.1923
Novais, J. S., Moreira, C. S., Silva, A. C. J. A., Loureiro, R. S., Sá Figueiredo, A. M., Ferreira, V. F., et al. (2018). Antibacterial Naphthoquinone Derivatives Targeting Resistant Strain Gram-Negative Bacteria in Biofilms. Microb. Pathog. 118, 105–114. doi:10.1016/j.micpath.2018.03.024
Novy, P., Rondevaldova, J., Kourimska, L., and Kokoska, L. (2013). Synergistic Interactions of Epigallocatechin Gallate and Oxytetracycline against Various Drug Resistant Staphylococcus aureus Strains In Vitro. Phytomedicine 20, 432–435. doi:10.1016/j.phymed.2012.12.010
Novy, P., Urban, J., Leuner, O., Vadlejch, J., and Kokoska, L. (2011). In Vitro synergistic Effects of Baicalin with Oxytetracycline and Tetracycline against Staphylococcus aureus. J. Antimicrob. Chemother. 66, 1298–1300. doi:10.1093/jac/dkr108
Obiang-Obounou, B. W., Kang, O. H., Choi, J. G., Keum, J. H., Kim, S. B., Mun, S. H., et al. (2011). In Vitro potentiation of Ampicillin, Oxacillin, Norfloxacin, Ciprofloxacin, and Vancomycin by Sanguinarine against Methicillin-Resistant Staphylococcus aureus. Foodborne Pathog. Dis. 8, 869–874. doi:10.1089/fpd.2010.0759
Pal, A., and Tripathi, A. (2020). Demonstration of Bactericidal and Synergistic Activity of Quercetin with Meropenem Among Pathogenic Carbapenem Resistant Escherichia coli and Klebsiella pneumoniae. Microb. Pathog. 143, 104120. doi:10.1016/j.micpath.2020.104120
Pal, A., and Tripathi, A. (2019). Quercetin Potentiates Meropenem Activity Among Pathogenic Carbapenem-Resistant Pseudomonas aeruginosa and Acinetobacter Baumannii. J. Appl. Microbiol. 127, 1038–1047. doi:10.1111/jam.14388
Phitaktim, S., Chomnawang, M., Sirichaiwetchakoon, K., Dunkhunthod, B., Hobbs, G., and Eumkeb, G. (2016). Synergism and the Mechanism of Action of the Combination of α-mangostin Isolated from Garcinia Mangostana L. And Oxacillin against an Oxacillin-Resistant Staphylococcus Saprophyticus. BMC Microbiol. 16, 195. doi:10.1186/s12866-016-0814-4
Piddock, L. J. (2012). The Crisis of No New Antibiotics-Wwhat Is the Way Forward? Lancet Infect. Dis. 12, 249–253. doi:10.1016/S1473-3099(11)70316-4
Pimchan, T., Maensiri, D., and Eumkeb, G. (2017). Synergy and Mechanism of Action of α-mangostin and Ceftazidime against Ceftazidime-Resistant Acinetobacter Baumannii. Lett. Appl. Microbiol. 65, 285–291. doi:10.1111/lam.12789
Pinheiro, P. F., Menini, L. A. P., Bernardes, P. C., Saraiva, S. H., Carneiro, J. W. M., Costa, A. V., et al. (2018). Semisynthetic Phenol Derivatives Obtained from Natural Phenols: Antimicrobial Activity and Molecular Properties. J. Agric. Food Chem. 66, 323–330. doi:10.1021/acs.jafc.7b04418
Pourahmad Jaktaji, R., and Mohammadi, P. (2018). Effect of Total Alkaloid Extract of Local Sophora Alopecuroides on Minimum Inhibitory Concentration and Intracellular Accumulation of Ciprofloxacin, and acrA Expression in Highly Resistant Escherichia coli Clones. J. Glob. Antimicrob. Resist 12, 55–60. doi:10.1016/j.jgar.2017.09.005
Puvaca, N., Milenkovic, J., Galonja Coghill, T., Bursic, V., Petrovic, A., Tanaskovic, S., et al. (2021). Antimicrobial Activity of Selected Essential Oils against Selected Pathogenic Bacteria: In Vitro Study. Antibiot. (Basel) 10.
Qian, M., Tang, S., Wu, C., Wang, Y., He, T., Chen, T., et al. (2015). Synergy between Baicalein and Penicillins against Penicillinase-Producing Staphylococcus aureus. Int. J. Med. Microbiol. 305, 501–504. doi:10.1016/j.ijmm.2015.05.001
Qiu, S., Sun, H., Zhang, A. H., Xu, H. Y., Yan, G. L., Han, Y., et al. (2014). Natural Alkaloids: Basic Aspects, Biological Roles, and Future Perspectives. Chin. J. Nat. Med. 12, 401–406. doi:10.1016/S1875-5364(14)60063-7
Qu, S., Dai, C., Shen, Z., Tang, Q., Wang, H., Zhai, B., et al. (2019). Mechanism of Synergy between Tetracycline and Quercetin against Antibiotic Resistant Escherichia coli. Front. Microbiol. 10, 2536. doi:10.3389/fmicb.2019.02536
Roudashti, S., Zeighami, H., Mirshahabi, H., Bahari, S., Soltani, A., and Haghi, F. (2017). Synergistic Activity of Sub-inhibitory Concentrations of Curcumin with Ceftazidime and Ciprofloxacin against Pseudomonas aeruginosa Quorum Sensing Related Genes and Virulence Traits. World J. Microbiol. Biotechnol. 33, 50. doi:10.1007/s11274-016-2195-0
Ruan, X., Deng, X., Tan, M., Yu, C., Zhang, M., Sun, Y., et al. (2021). In Vitro antibiofilm Activity of Resveratrol against Avian Pathogenic Escherichia coli. BMC Vet. Res. 17, 249. doi:10.1186/s12917-021-02961-3
Ruan, Z., Cui, J., He, Z., Guo, Y., Jia, X., and Huang, X. (2020). Synergistic Effects from Combination of Cryptotanshinone and Fosfomycin against Fosfomycin-Susceptible and Fosfomycin-Resistant Staphylococcus aureus. Infect. Drug Resist 13, 2837–2844. doi:10.2147/IDR.S255296
Sakagami, Y., Iinuma, M., Piyasena, K. G., and Dharmaratne, H. R. (2005). Antibacterial Activity of Alpha-Mangostin against Vancomycin Resistant Enterococci (VRE) and Synergism with Antibiotics. Phytomedicine 12, 203–208. doi:10.1016/j.phymed.2003.09.012
Shi, C., Li, M., Muhammad, I., Ma, X., Chang, Y., Li, R., et al. (2018). Combination of Berberine and Ciprofloxacin Reduces Multi-Resistant Salmonella Strain Biofilm Formation by Depressing mRNA Expressions of luxS, rpoE, and ompR. J. Vet. Sci. 19, 808–816. doi:10.4142/jvs.2018.19.6.808
Shi, G., Shao, J., Wang, T., Wu, D., and Wang, C. (2017). Mechanism of Berberine-Mediated Fluconazole-Susceptibility Enhancement in Clinical Fluconazole-Resistant Candida tropicalis Isolates. Biomed. Pharmacother. 93, 709–712. doi:10.1016/j.biopha.2017.06.106
Siriwong, S., Teethaisong, Y., Thumanu, K., Dunkhunthod, B., and Eumkeb, G. (2016). The Synergy and Mode of Action of Quercetin Plus Amoxicillin against Amoxicillin-Resistant Staphylococcus Epidermidis. BMC Pharmacol. Toxicol. 17, 39. doi:10.1186/s40360-016-0083-8
Siriwong, S., Thumanu, K., Hengpratom, T., and Eumkeb, G. (2015). Synergy and Mode of Action of Ceftazidime Plus Quercetin or Luteolin on Streptococcus Pyogenes. Evid. Based Complement. Altern. Med. 2015, 759459. doi:10.1155/2015/759459
Sousa Silveira, Z., Macêdo, N. S., Sampaio Dos Santos, J. F., Sampaio De Freitas, T., Rodrigues Dos Santos Barbosa, C., Júnior, D. L. S., et al. (2020). Evaluation of the Antibacterial Activity and Efflux Pump Reversal of Thymol and Carvacrol against Staphylococcus aureus and Their Toxicity in Drosophila melanogaster. Molecules 25. doi:10.3390/molecules25092103
Souza, C. R. M., Bezerra, W. P., and Souto, J. T. (2020). Marine Alkaloids with Anti-inflammatory Activity: Current Knowledge and Future Perspectives. Mar. Drugs 18. doi:10.3390/md18030147
Stapleton, P. D., and Taylor, P. W. (2002). Methicillin Resistance in Staphylococcus aureus: Mechanisms and Modulation. Sci. Prog. 85, 57–72. doi:10.3184/003685002783238870
Su, F., and Wang, J. (2018). Berberine Inhibits the MexXY-OprM Efflux Pump to Reverse Imipenem Resistance in a Clinical Carbapenem-Resistant Pseudomonas aeruginosa Isolate in a Planktonic State. Exp. Ther. Med. 15, 467–472. doi:10.3892/etm.2017.5431
Su, P. W., Yang, C. H., Yang, J. F., Su, P. Y., and Chuang, L. Y. (2015). Antibacterial Activities and Antibacterial Mechanism of Polygonum Cuspidatum Extracts against Nosocomial Drug-Resistant Pathogens. Molecules 20, 11119–11130. doi:10.3390/molecules200611119
Su, T., Qiu, Y., Hua, X., Ye, B., Luo, H., Liu, D., et al. (2020). Novel Opportunity to Reverse Antibiotic Resistance: To Explore Traditional Chinese Medicine with Potential Activity against Antibiotics-Resistance Bacteria. Front. Microbiol. 11, 610070. doi:10.3389/fmicb.2020.610070
Sudano Roccaro, A., Blanco, A. R., Giuliano, F., Rusciano, D., and Enea, V. (2004). Epigallocatechin-gallate Enhances the Activity of Tetracycline in Staphylococci by Inhibiting its Efflux from Bacterial Cells. Antimicrob. Agents Chemother. 48, 1968–1973. doi:10.1128/AAC.48.6.1968-1973.2004
Sundaramoorthy, N. S., Sivasubramanian, A., and Nagarajan, S. (2020). Simultaneous Inhibition of MarR by Salicylate and Efflux Pumps by Curcumin Sensitizes Colistin Resistant Clinical Isolates of Enterobacteriaceae. Microb. Pathog. 148, 104445. doi:10.1016/j.micpath.2020.104445
Teethaisong, Y., Sirichaiwetchakoon, N. K., Kupittayanant, P. S., Eumkeb, G., and Eumkeb, G. (2014). Synergistic Activity and Mechanism of Action of Stephania Suberosa Forman Extract and Ampicillin Combination against Ampicillin-Resistant Staphylococcus aureus. J. Biomed. Sci. 21, 90. doi:10.1186/s12929-014-0090-2
Teng, Z., Li, M., Shi, D., Deng, X., and Wang, J. (2018). Synergistic Interactions of Cryptotanshinone and Aminoglycoside Antibiotics against Staphylococcus aureus In Vitro. J. Glob. Antimicrob. Resist 13, 264–265. doi:10.1016/j.jgar.2018.05.013
Usman Amin, M., Khurram, M., Khan, T. A., Faidah, H. S., Ullah Shah, Z., Ur Rahman, S., et al. (2016). Effects of Luteolin and Quercetin in Combination with Some Conventional Antibiotics against Methicillin-Resistant Staphylococcus aureus. Int. J. Mol. Sci. 17. doi:10.3390/ijms17111947
Vázquez, N. M., Fiorilli, G., Cáceres Guido, P. A., and Moreno, S. (2016). Carnosic Acid Acts Synergistically with Gentamicin in Killing Methicillin-Resistant Staphylococcus aureus Clinical Isolates. Phytomedicine 23, 1337–1343. doi:10.1016/j.phymed.2016.07.010
Vipin, C., Saptami, K., Fida, F., Mujeeburahiman, M., Rao, S. S., AthmikaArun, A. B., et al. (2020). Potential Synergistic Activity of Quercetin with Antibiotics against Multidrug-Resistant Clinical Strains of Pseudomonas aeruginosa. PLoS One 15, e0241304. doi:10.1371/journal.pone.0241304
Vivekanandan, L., Sheik, H., Singaravel, S., and Thangavel, S. (2018). Ameliorative Effect of Silymarin against Linezolid-Induced Hepatotoxicity in Methicillin-Resistant Staphylococcus aureus (MRSA) Infected Wistar Rats. Biomed. Pharmacother. 108, 1303–1312. doi:10.1016/j.biopha.2018.09.133
Wagner, H., and Ulrich-Merzenich, G. (2009). Synergy Research: Approaching a New Generation of Phytopharmaceuticals. Phytomedicine 16, 97–110. doi:10.1016/j.phymed.2008.12.018
Wang, G., Li, L., Wang, X., Li, X., Zhang, Y., Yu, J., et al. (2019). Hypericin Enhances β-lactam Antibiotics Activity by Inhibiting sarA Expression in Methicillin-Resistant Staphylococcus aureus. Acta Pharm. Sin. B 9, 1174–1182. doi:10.1016/j.apsb.2019.05.002
Wang, S., Kim, M. C., Kang, O. H., and Kwon, D. Y. (2020). The Mechanism of Bisdemethoxycurcumin Enhances Conventional Antibiotics against Methicillin-Resistant Staphylococcus aureus. Int. J. Mol. Sci. 21. doi:10.3390/ijms21217945
Wang, S., Kang, O. H., and Kwon, D. Y. (2021). Trans-Cinnamaldehyde Exhibits Synergy with Conventional Antibiotic against Methicillin-Resistant Staphylococcus aureus. Int. J. Mol. Sci. 22. doi:10.3390/ijms22052752
Wang, S. Y., Sun, Z. L., Liu, T., Gibbons, S., Zhang, W. J., and Qing, M. (2014). Flavonoids from Sophora Moorcroftiana and Their Synergistic Antibacterial Effects on MRSA. Phytother. Res. 28, 1071–1076. doi:10.1002/ptr.5098
Wang, Y. M., Kong, L. C., Liu, J., and Ma, H. X. (2018). Synergistic Effect of Eugenol with Colistin against Clinical Isolated Colistin-Resistant Escherichia coli Strains. Antimicrob. Resist Infect. Control 7, 17. doi:10.1186/s13756-018-0303-7
Wei, S., Yang, Y., Tian, W., Liu, M., Yin, S., and Li, J. (2020). Synergistic Activity of Fluoroquinolones Combining with Artesunate against Multidrug-Resistant Escherichia coli. Microb. Drug Resist 26, 81–88. doi:10.1089/mdr.2018.0463
Wojtyczka, R. D., Dziedzic, A., Kępa, M., Kubina, R., Kabała-Dzik, A., Mularz, T., et al. (2014). Berberine Enhances the Antibacterial Activity of Selected Antibiotics against Coagulase-Negative Staphylococcus Strains In Vitro. Molecules 19, 6583–6596. doi:10.3390/molecules19056583
Wu, S. C., Yang, Z. Q., Liu, F., Peng, W. J., Qu, S. Q., Li, Q., et al. (2019). Antibacterial Effect and Mode of Action of Flavonoids from Licorice against Methicillin-Resistant Staphylococcus aureus. Front. Microbiol. 10, 2489. doi:10.3389/fmicb.2019.02489
Wultanska, D., Piotrowski, M., and Pituch, H. (2020). The Effect of Berberine Chloride And/or its Combination with Vancomycin on the Growth, Biofilm Formation, and Motility of Clostridioides Difficile. Eur. J. Clin. Microbiol. Infect. Dis. 39, 1391–1399.
Xu, Y., Quan, H., Wang, Y., Zhong, H., Sun, J., Xu, J., et al. (2017). Requirement for Ergosterol in Berberine Tolerance Underlies Synergism of Fluconazole and Berberine against Fluconazole-Resistant Candida Albicans Isolates. Front. Cell. Infect. Microbiol. 7, 491. doi:10.3389/fcimb.2017.00491
Yang, J. F., Yang, C. H., Chang, H. W., Yang, C. S., Wang, S. M., Hsieh, M. C., et al. (2010). Chemical Composition and Antibacterial Activities of Illicium Verum against Antibiotic-Resistant Pathogens. J. Med. Food 13, 1254–1262. doi:10.1089/jmf.2010.1086
Yong, J., Zu, R., Huang, X., Ge, Y., and Li, Y. (2020). Synergistic Effect of Berberine Hydrochloride and Fluconazole against Candida Albicans Resistant Isolates. Front. Microbiol. 11, 1498. doi:10.3389/fmicb.2020.01498
Yu, H. H., Kim, K. J., Cha, J. D., Kim, H. K., Lee, Y. E., and You, N. Y. Y. O. (2005). Antimicrobial Activity of Berberine Alone and in Combination with Ampicillin or Oxacillin against Methicillin-Resistant Staphylococcus aureus. J. Med. Food 8, 454–461. doi:10.1089/jmf.2005.8.454
Zhang, H., Wang, K., Zhang, G., Ho, H. I., and Gao, A. (2010). Synergistic Anti-candidal Activity of Tetrandrine on Ketoconazole: an Experimental Study. Planta Med. 76, 53–61. doi:10.1055/s-0029-1185973
Zhao, W. H., Hu, Z. Q., Hara, Y., and Shimamura, T. (2002). Inhibition of Penicillinase by Epigallocatechin Gallate Resulting in Restoration of Antibacterial Activity of Penicillin against Penicillinase-Producing Staphylococcus aureus. Antimicrob. Agents Chemother. 46, 2266–2268. doi:10.1128/aac.46.7.2266-2268.2002
Zhou, X. Y., Ye, X. G., He, L. T., Zhang, S. R., Wang, R. L., Zhou, J., et al. (2016). In Vitro characterization and Inhibition of the Interaction between Ciprofloxacin and Berberine against Multidrug-Resistant Klebsiella pneumoniae. J. Antibiot. (Tokyo) 69, 741–746. doi:10.1038/ja.2016.15
Zhou, X. Z., Jia, F., Liu, X. M., Yang, C., Zhao, L., and Wang, Y. J. (2013). Total Alkaloids from Sophora Alopecuroides L. Increase Susceptibility of Extended-Spectrum β-lactamases Producing Escherichia coli Isolates to Cefotaxime and Ceftazidime. Chin. J. Integr. Med. 19, 945–952. doi:10.1007/s11655-011-0899-4
Zuo, G. Y., Han, Z. Q., Hao, X. Y., Han, J., Li, Z. S., and Wang, G. C. (2014). Synergy of Aminoglycoside Antibiotics by 3-Benzylchroman Derivatives from the Chinese Drug Caesalpinia Sappan against Clinical Methicillin-Resistant Staphylococcus aureus (MRSA). Phytomedicine 21, 936–941. doi:10.1016/j.phymed.2014.03.004
Zuo, G. Y., Li, Y., Han, J., Wang, G. C., Zhang, Y. L., and Bian, Z. Q. (2012). Antibacterial and Synergy of Berberines with Antibacterial Agents against Clinical Multi-Drug Resistant Isolates of Methicillin-Resistant Staphylococcus aureus (MRSA). Molecules 17, 10322–10330. doi:10.3390/molecules170910322
Keywords: traditional Chinese medicine, active ingredient, combined, antibiotic, drug-resistant bacterial
Citation: Li J, Feng S, Liu X, Jia X, Qiao F, Guo J and Deng S (2022) Effects of Traditional Chinese Medicine and its Active Ingredients on Drug-Resistant Bacteria. Front. Pharmacol. 13:837907. doi: 10.3389/fphar.2022.837907
Received: 17 December 2021; Accepted: 25 April 2022;
Published: 02 June 2022.
Edited by:
Joan Villena García, Universidad de Valparaíso, ChileReviewed by:
Susan Semple, University of South Australia, AustraliaCopyright © 2022 Li, Feng, Liu, Jia, Qiao, Guo and Deng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fengling Qiao, cWlhb3poYW95aUBjZHV0Y20uZWR1LmNu; Jinlin Guo, Z3VvNTk2QGNkdXRjbS5lZHUuY24=; Shanshan Deng, anpseGRkc3NAMTYzLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.