
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Pediatr. , 06 October 2022
Sec. Children and Health
Volume 10 - 2022 | https://doi.org/10.3389/fped.2022.947646
This article is part of the Research Topic Advances of Health Care Transition for Patients with Childhood-onset Chronic Diseases: International Perspectives, Volume II View all 17 articles
 Yuri Yoshimoto-Suzuki1,2
Yuri Yoshimoto-Suzuki1,2 Daisuke Hasegawa1
Daisuke Hasegawa1 Yosuke Hosoya1
Yosuke Hosoya1 Go Saito1
Go Saito1 Kyoko Nagase3
Kyoko Nagase3 Michiyo Gunji3
Michiyo Gunji3 Kyoko Kobayashi4
Kyoko Kobayashi4 Yasushi Ishida5
Yasushi Ishida5 Atsushi Manabe6
Atsushi Manabe6 Miwa Ozawa1*
Miwa Ozawa1*Background: Childhood cancer survivors (CCSs) have a lifelong increased risk of chronic health problems, most of which are associated with the curative therapies. Recent studies have suggested that prospective active screening using comprehensive assessments for CCSs is superior in identifying undiagnosed chronic health problems.
Methods: To assess the significance of active screening using comprehensive medical examinations for detecting chronic health problems in multiple organ systems in CCSs, we retrospectively compared the frequency and severity of health problems between two different cohorts of CCSs in a single institution: 110 CCSs who visited the outpatient clinic for regular follow-ups between December 2010 and December 2015 (regular follow-up group) vs. 58 CCSs who underwent comprehensive medical examinations between February 2016 and September 2019 (active screening group). CCSs were defined as patients aged ≥ 18 years who had been diagnosed as having childhood cancer ≥ 10 years before and had survived without cancer for ≥ 5 years.
Results: Patient characteristics were similar between the two groups except for primary diagnosis (more brain tumors and embryonal tumors in the active screening group) and treatment history (more alkylating agents used and surgical interventions performed in the active screening group). The prevalence and the median number of health problems were significantly higher in the active screening group than in the regular follow-up group: 93% vs. 67% and 1.0 [0.0–8.0] vs. 2.0 [0.0–7.0] respectively. In term of organ-specific health problems, pulmonary dysfunction, neurocognitive impairment, ocular abnormalities, and dental abnormalities were identified more in the active screening group, partly because these problems had not been assessed in the regular follow-up group. Nevertheless, the prevalence of grade 3–5 health problems was similar between the two groups, except for pulmonary dysfunction.
Conclusion: Active screening using comprehensive medical examinations was effective for identifying health problems in CCSs. Although the prevalence of severe problems identified by both approaches was similar, comprehensive medical examinations could detect overlooked problems such as severe pulmonary dysfunction, dental maldevelopment, and borderline intellectual functioning, which might have an impact on quality of life in CCSs.
Progress in the development of therapies for children with cancer has resulted in a >80% survival rate in developed countries, and children who overcome childhood cancer grow up as childhood cancer survivors (CCSs) (1). CCSs have a lifelong increased risk of chronic health problems, most of which are associated with the curative therapies. Chronic health problems in CCSs include cardiac dysfunction, pulmonary dysfunction, renal impairment, endocrine and reproductive disorders, growth impairment, neurocognitive impairment, and subsequent malignant neoplasms (2, 3). These health problems have previously been evaluated using self-report questionnaires or registry data. Recent studies have shown that prospective active screening using comprehensive systematic assessments for all CCSs was superior in identifying a substantial number of undiagnosed chronic health problems (4, 5). In fact, a large study of active screenings for adult CCSs revealed that the estimated cumulative prevalence of chronic health problems and serious/disabling or life-threatening problems at 45 years of age was 95.5 and 80.5%, respectively (6).
At St. Luke’s International Hospital, active screening for late-onset health problems among CCSs was started in February 2016. CCSs aged ≥ 18 years or older who were diagnosed as having childhood cancer at least 10 years before and remained in remission for ≥ 5 years underwent comprehensive medical examinations. Before the active screenings were initiated, patients treated for childhood cancer were evaluated for health problems during regular clinic visits at the discretion of the physician in accordance with the Children’s Oncology Group Long-term Follow-Up Guidelines (7) considering cancer type and treatment history.
In the present study, we compared the frequencies and severities of late-onset health problems between different approaches, namely, comprehensive medical examinations and regular clinic-based evaluations. The aim of this study was to assess the utility of active screening using comprehensive medical examinations in detecting chronic health problems of multiple organ systems in CCSs, which might be overlooked at regular clinic visits.
All data were obtained through the studies approved by the institutional review board of St. Luke’s International Hospital. In the present study, CCSs were defined as patients aged ≥ 18 years who were diagnosed with childhood cancer ≥ 10 years before and survived without cancer for ≥ 5 years. Data of 58 CCSs who underwent comprehensive medical examinations between February 2016 and September 2019 were prospectively collected (active screening group). We also reviewed the medical records of 147 CCSs who visited the outpatient clinic for regular follow-ups between December 2010 and December 2015, and their medical records were retrospectively analyzed. Of those 147 CCSs, 37 CCSs were excluded because they also underwent a comprehensive medical examination after February 2016, and were thus included in the active screening group in this analysis. Finally, 110 CCSs were assigned to the regular follow-up group. Written informed consent was obtained from all participants in the active screening group and opt-out consent involving provision of an information leaflet was obtained when the medical records of patients in the regular follow-up group were reviewed.
In the active screening group, participants underwent a comprehensive evaluation as follows: medical history, physical examination, resting blood pressure, complete blood cell count, comprehensive metabolic panel, fasting lipid profile, blood sugar, hemoglobin A1C level, endocrine–reproductive function (thyroid, gonadal, hypothalamic–pituitary axis function), urinalysis, fecal occult blood test, echocardiography, pulmonary function testing, audiological testing, ophthalmologic evaluation, dental evaluation, neurocognitive testing, bone mineral density testing, gynecological examination (female only), thyroid ultrasonography, abdominal ultrasonography, and brain MRI. These examinations were selected according to the comprehensive medical checkup system administered in healthy adults in Japan (8) and the St. Jude Lifetime Cohort (SJLIFE) study (6). In the regular follow-up group, medical records and the most recent examination results were reviewed, and information about health problems was extracted. Medical assessments for CCSs in the regular follow-up group were performed at the discretion of the pediatric oncologist in accordance with the guidelines (7) considering cancer type and treatment history. The cost of examinations for CCSs in the active screening group and the regular follow-up group was covered by the research grant and public health insurance, respectively. In both groups, cancer-related information, including type of cancer, cumulative doses of chemotherapy, information on hematopoietic cell transplantation, surgical interventions, and the dose and anatomical location of radiological therapy, was extracted from the medical chart for each patient.
The criteria for positive screening and the grading are shown in Table 1. Chronic health problems were classified according to the modified National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE) version 4.0, which was also utilized in the SJLIFE study (9). We made additional minor modifications to the SJLIFE-modified CTCAE as follows: obesity was defined as BMI ≥ 25 based on Asian criteria; HbA1c and cholesterol level was used in the evaluation of diabetes mellitus and hyperlipidemia, respectively, because the results of fasting tests were not always available in the regular follow-up group; hypothalamic–pituitary axis dysfunction was diagnosed using growth hormone provocation tests or ACTH (adrenocorticotropic hormone) stimulation tests in children in the regular follow-up group who were positive in screening for insulin-like growth factor-1 or morning cortisol level, respectively; hepatitis B or C virus infections were classified as grade 3 if they were serologically positive.
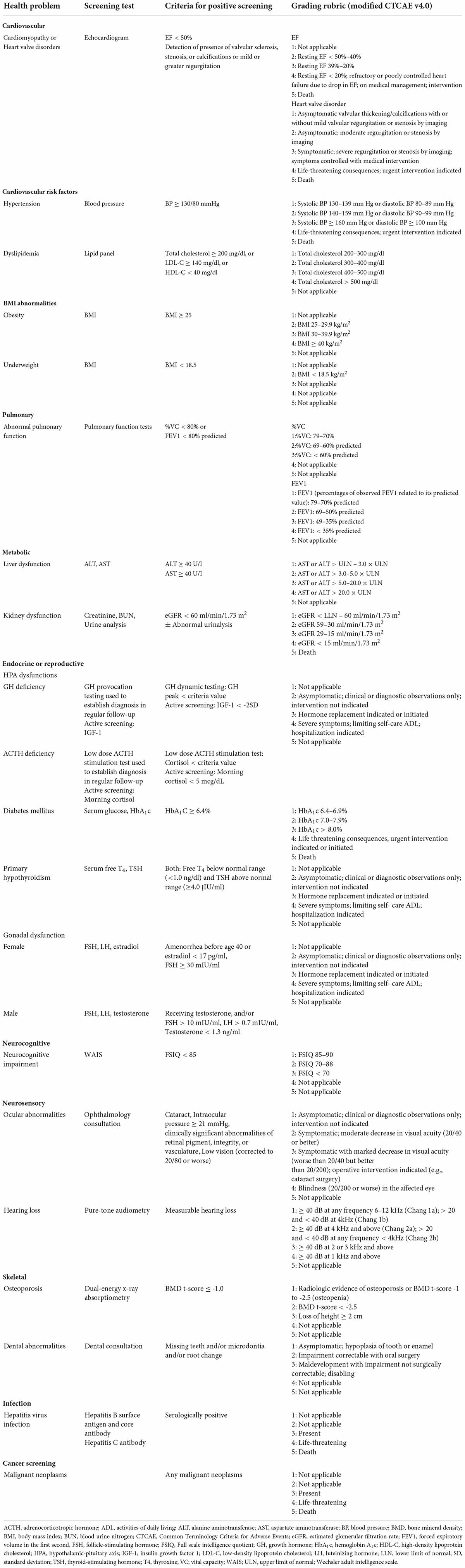
Table 1. Definition of health problems, screening tests, criteria for positive screening, and grading rubric.
Health problems were compared between the active screening group and the regular follow-up group. The significance of the presence and the number of health problems per CCS was tested by Fisher’s exact test, a non-parametric test, and one-way analysis of variance. Non-parametric variables were tested using the Mann–Whitney test and Kruskal–Wallis test. Data were analyzed using EZR (Saitama Medical Center, Jichi Medical University), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) (10); more precisely, it is a modified version of R commander, which is designed to perform statistical functions frequently used in biostatistics.
The demographic, treatment, and diagnostic characteristics of the 110 CCSs in the regular follow-up group and the 58 CCSs in the active screening group are shown in Table 2. The proportion of males (43.6% vs. 46.6%), median age at diagnosis (6 years vs. 6 years), median age at the last follow-up (27.5 years vs. 25.5 years), and median duration of follow-up from diagnosis (19.0 years vs. 18.0 years) were not statistically different between the regular follow-up group and the active screening group. Hematological malignancies were more prevalent in the regular follow-up group than in the active screening group (81.8% vs. 70.7%), whereas the proportion of CNS tumors and embryonal tumors was higher in the active screening group. All CCSs received chemotherapy, but the proportion of CCSs receiving alkylating agents was higher in the active screening group. Nearly half of the CCSs in both groups received radiotherapy, and the main target organ was the brain. The proportion of CCSs who underwent surgical intervention was higher in the active screening group.
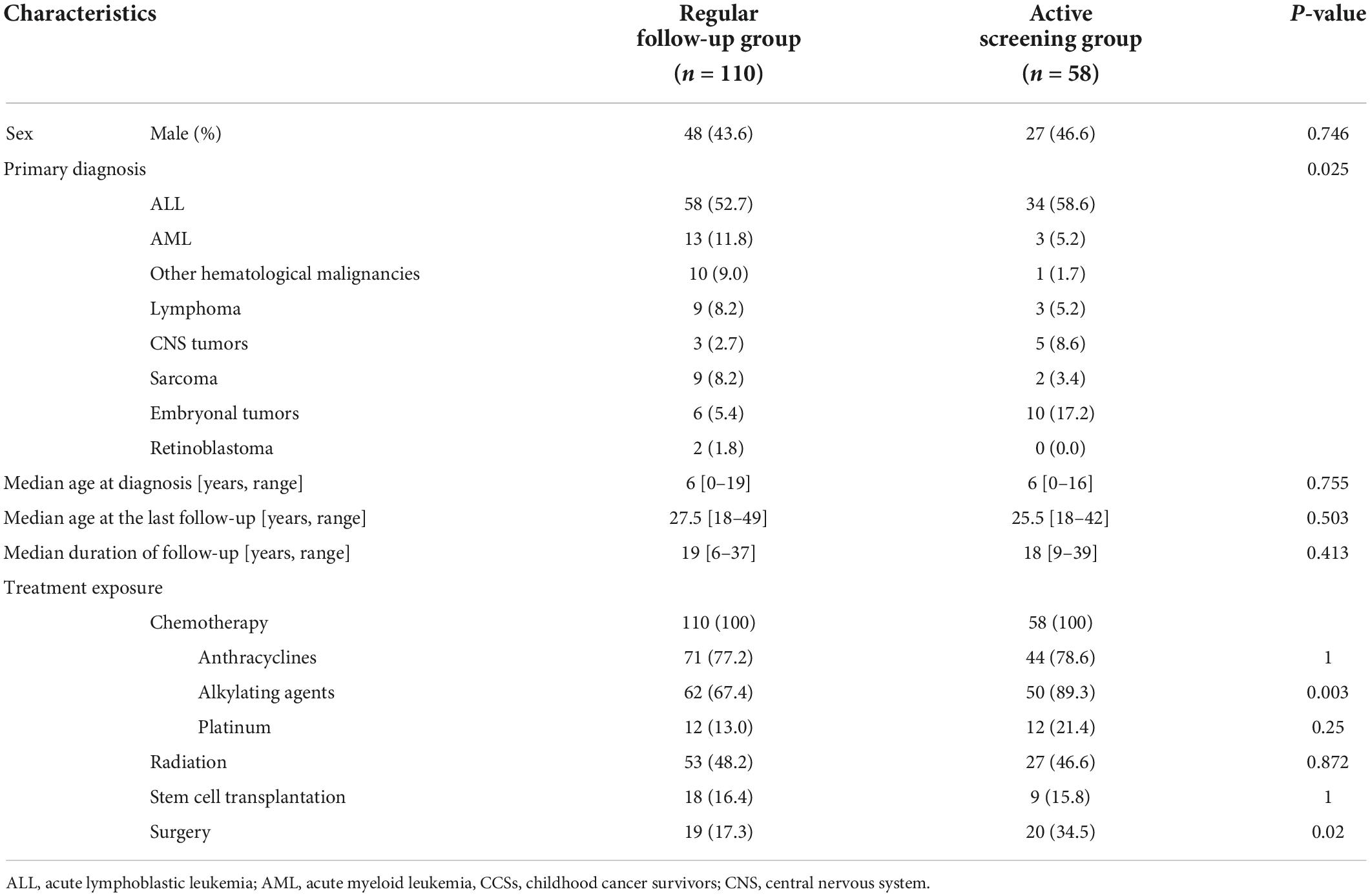
Table 2. Demographic, treatment, and diagnostic characteristics of CCSs in the regular follow-up group (n = 110) and the active screening group (n = 58).
The prevalence of any health problems was significantly higher in the active screening group than in the regular follow-up group (93.1% vs. 67.3%; Table 3). In addition, the median number of any health problems was also higher in the active screening group than in the regular follow-up group (1.0 [0.0–8.0] vs. 2.0 [0.0–7.0]), and a third of CCSs in the active screening group had 4 or more health problems. In contrast, the prevalence and median number of severe health problems (≥ grade 3) were not significantly different between the two groups. Similar results were obtained from intrapatient comparisons in 37 CCSs who underwent regular follow-up and then active screening (data is not shown).
The median number of health problems was high in CCSs with CNS tumors (4.5 [1.0–8.0]; Table 4). Radiotherapy (2.5 vs. 1.0), hematopoietic cell transplantation (3.0 vs. 1.0), and platinum agents (3.0 vs. 1.0) were also associated with a higher number of health problems. The prevalence of severe health problems (≥grade 3) was also high in these CCSs: 62.5% in CCSs with CNS tumors, 41.2% in CCSs receiving radiotherapy, 51.9% in transplanted CCSs, and 50% in CCSs receiving platinum agents. The age at diagnosis, age at the last follow-up, and duration of follow-up were not associated with the mean number or severity of health problems.
Table 5 summarizes the prevalence of organ-specific health problems and the proportion of CCSs who did not undergo the screening tests for each health problem. Almost all the health problems were systematically evaluated in the active screening group by comprehensive medical examinations, whereas regular clinic-based evaluations failed to assess several organ-specific health problems, for example echocardiograms (the proportion of “not-tested” CCSs was 79.1%), pulmonary function tests (94.5%), neurocognitive evaluations (88.2%), ophthalmologic examinations (80.9%), audiometry (90.9%), bone mineral density tests (93.6%), and dental examinations (100%). These discrepancies in the frequency of organ-specific evaluations resulted in differences in the prevalence of relevant health problems between the regular follow-up group and the active screening group: pulmonary dysfunction (2.7% vs. 20.7%), neurocognitive impairment (4.5% vs. 22.4%), ocular abnormalities (8.2% vs. 22.4%), and dental abnormalities (unknown vs. 37.9%). However, the prevalence of severe organ-specific health problems (≥grade 3) was the same between the two groups except for pulmonary dysfunction (1.7% vs. 6.9%; P = 0.049). In fact, most of the ocular abnormalities reported in the active screening group were trivial (e.g., optic disk cupping, n = 11), while cataract was found in 2 CCSs. No CCSs in the regular follow-up group had dental examinations, whereas 54 of 58 CCSs (93.1%) in the active screening group underwent dental examinations and dental problems were reported in 22 CCSs: missing teeth in 14, microdontia in 8, and root change in 8. These dental abnormalities detected in the active screening group were not disabling and could be surgically corrected and were thus classified as grade 1–2. Of 12 patients who showed abnormal pulmonary function in active screening group, 11 had restrictive impairment and 4 were classified as grade 3–4.
This report delineates the prevalence and severity of health problems across multiple organ systems in adult CCSs, as assessed by comprehensive medical examinations and regular clinic-based evaluations performed at a single center in Japan. Similar to previous reports, the incidence and severity of chronic health problems were associated with specific clinical factors such as CNS tumors, radiotherapy, hematopoietic cell transplantation, and platinum agents.
Active screening successfully identified more health problems compared with regular clinic-based evaluations (93.1% vs. 67.3%). This result might be attributable to efficient screening using comprehensive examinations to evaluate systemic health problems. In fact, several examinations were rarely performed in CCSs at regular follow-ups: echocardiograms, pulmonary function tests, neurocognitive evaluations, ophthalmologic examinations, audiometry, bone mineral density tests, and dental examination. Active screening revealed that pulmonary dysfunction, neurocognitive impairment, ocular abnormalities, and dental abnormalities were more prevalent than previously thought. In the SJLIFE study, prospective and risk-based systematic screening of health problems among CCSs revealed that the prevalence of newly diagnosed neurocognitive and neurosensory deficits, heart valve disorders, and pulmonary dysfunction was particularly increased, which was almost similar to our study. The examinations administered in the active screening group were selected according to the comprehensive medical checkup system administered in healthy adults in Japan (8) and the SJLIFE study (6). Comprehensive medical checkups allow for early detection of diseases in healthy adults and are widely used in Japan. Considering that this medical program is not covered by public health insurance, the cost-effectiveness of comprehensive medical examinations for CCSs needs to be further evaluated.
Most of the problems overlooked in the regular follow-up group were classified as grade 1–2; however, this may not mean that active screening resulted in overdiagnosis of clinically insignificant health problems in CCSs. For example, grade 1–2 dental anomalies were found in 40% of CCSs in the active screening group. Although these dental problems were not disabling and could be surgically corrected, they had potential impact on functional and aesthetic prognoses. Previous studies showed that the prevalence of root abnormalities ranged from 1.3 to 5.6%, and microdontia from 1 to 2% in a population of healthy children (11). The prevalence of hypodontia varies between 4 and 8% depending on the ethnic background (12). Pulmonary dysfunction and neurocognitive impairment were also more prevalent in the active screening group. Considering that the morbidity rate of pulmonary dysfunction was equivalent to that in the SJLIFE study (6) and that 4 of 12 pulmonary dysfunctions found in the active screening group were classified as ≥ grade 3, active screening successfully identified severe underlying pulmonary dysfunctions. Careful follow-up, education, and appropriate intervention such as pneumococcal vaccination should be implemented for CCSs with asymptomatic pulmonary dysfunction to prevent future worsening of pulmonary function. Identification of borderline intellectual functioning in a substantial number of CCSs in the active screening group is also important because of the potential impacts on quality of life. Further investigation is needed to clarify the significance of early interventions in CCSs with borderline intellectual functioning detected by active screening. The significance of ophthalmological abnormalities found in the present study may be controversial. Eleven of the 13 ophthalmological abnormalities in the active screening group were optic disk cupping, which were asymptomatic and concluded to be a non-specific finding by a more detailed follow-up. Because ocular abnormalities affect quality of life in CCSs, further investigation and analysis are needed to determine the importance of early detection of subtle changes in ophthalmological findings.
Because the prevalence of obesity, hypertension, and several laboratory abnormalities such as dyslipidemia and endocrinopathy did not increase by active screening, routine physical examinations and blood tests were adequate to identify these problems. Despite the low examination rate in the regular follow-up group, the similar prevalence of cardiac dysfunction and osteoporosis between the two groups was surprising. One plausible explanation may be that these problems were appropriately evaluated based on treatment history in the regular follow-up group. Another explanation may be that the follow-up duration of the present study was too short to detect subclinical cardiotoxicity among asymptomatic CCSs with normal ejection fractions. Cardiac dysfunction increases markedly with aging, and as many as 1 in 8 of CCSs treated with anthracyclines and chest radiation therapy will have a life-threatening cardiovascular event within 30 years after treatment (13). Further follow-up using parameters for early detection of subclinical diastolic dysfunction, including strain measurements by speckle tracking, may be required (14).
To our knowledge, this is the first study to prospectively explore systemic health problems in Asian CCSs using comprehensive screening for multiple organs (15). Most previous studies of CCSs in Asian countries have focused on epidemiological research or organ-specific toxicities (15). Health problems in CCSs are affected by a complex of multiple factors. Differences in genetic variations, socioeconomic status, health behaviors, lifestyle, treatment regimens, and clinical practice can be reflected in the prevalence of health problems in CCSs. The relatively low incidence of obesity in our cohort may exemplify the ethnic difference. Differences in genetic variations that influence the incidence of chronic health problems in CCSs between Asian and other populations should be explored in the future.
Several limitations should be considered when interpreting the results of this study. The major limitation is the small sample size. Second, the follow-up period was short, and the participants were relatively young. The health problems of CCSs are known to increase with age (16). Although the number and severity of health problems did not increase with age and from the time since diagnosis of pediatric cancer in this study, continuing active screening is expected to contribute to the prompt identification of health problems in CCSs. In addition, generalizability of our findings may be skeptical because most long-term follow-up clinics cannot afford to do the comprehensive medical testing. We believe that one of the significances of our study is that active screening could identify several overlooked problems, which was not regarded as severe based on CTCAE-based criteria but may affect quality of life in CCSs as described above. We are now planning detailed analyses on these subclinical but important health problems and will propose refined risk-based regular follow-up program including pulmonary function tests, neurocognitive evaluations, and dental examination.
Our study revealed that active screening using comprehensive medical examinations can identify health problems in CCSs efficiently. Although the prevalence of severe problems was the same between regular clinic-based evaluations based on follow-up guidelines and comprehensive medical examinations, the latter detected several overlooked problems such as pulmonary dysfunction, dental maldevelopment, and borderline intellectual functioning, which might have an impact on quality of life in CCSs. The cost-effectiveness of active screening should be further addressed in future studies.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from all participants in the Active screening group and opt-out consent involving provision of an information leaflet was obtained when the medical records of patients in the Regular follow-up group were reviewed. This study was approved by the Ethics board of St. Luke’s International Hospital.
YY-S, DH, YH, KK, YI, AM, and MO conceived and designed the study. GS, KN, and MG collected the clinical information and data. YY-S and DH analyzed the data, interpreted the results, and wrote the manuscript. YH, YI, AM, and MO contributed to the interpretation of the data and revised the manuscript. All the authors reviewed the manuscript and approved the final version of the manuscript.
This work was supported by Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (2014–2019: 26463429 and 2018-2021: 18H03098), Grant-in-Aid for Scientific Research from the Ministry of Health, Labor and Welfare of Japan (2020–2022: 20EA1022), a research grant from Children’s Cancer Association of Japan (2020–2021), a research grant from the Gold Ribbon Network (2017 and 2020), Relay For Life Japan: “Project Future” Research Grant (2016–2017), and Heart Link Working Project: Childhood Cancer Follow-up Research Grant (2014–2015).
The authors thank the patients and their parents for participating in this study. Sachiko Ohde (Graduate School of Public Health, St. Luke’s International University) and Seiju Sasaki (Center for Preventive Medicine, St. Luke’s International Hospital) for valuable advice regarding the conception and analysis; and all of our colleagues who were involved in the patients’ care and assisted with the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Armstrong GT, Chen Y, Yasui Y, Leisenring W, Gibson TM, Mertens AC, et al. Reduction in Late Mortality among 5-Year Survivors of Childhood Cancer. N Engl J Med. (2016) 374:833–42. doi: 10.1056/NEJMoa1510795
2. Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, et al. Childhood cancer survivor, chronic health conditions in adult survivors of childhood cancer. N Engl J Med. (2006) 355:1572–82. doi: 10.1056/NEJMsa060185
3. Landier W, Armenian S, Bhatia S. Late effects of childhood cancer and its treatment. Pediatr Clin North Am. (2015) 62:275–300. doi: 10.1016/j.pcl.2014.09.017
4. Geenen MM, Cardous-Ubbink MC, Kremer LC, van den Bos C, van der Pal HJ, Heinen RC, et al. Medical assessment of adverse health outcomes in long-term survivors of childhood cancer. JAMA. (2007) 297:2705–15. doi: 10.1001/jama.297.24.2705
5. Sieswerda E, Mulder RL, van Dijk IW, van Dalen EC, Kniinenburg SL, van der Pal HJH, et al. The EKZ/AMC childhood cancer survivor cohort: methodology, clinical characteristics, and data availability. J Cancer Surviv. (2013) 7:439–54. doi: 10.1007/s11764-013-0283-9
6. Hudson MM, Ness KK, Gurney JG, Mulrooney DA, Chemaitilly W, Krull KR, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. (2013) 309:2371–81. doi: 10.1001/jama.2013.6296
7. Children’s Oncology Group.Long-term follow-up guidelines for survivors of childhood, adolescent, and young adult cancers. Version 5.0. (2018). Available online at: http://www.survivorshipguidelines.org (accessed April 27, 2022).
8. Lu J. Ningen Dock: Japan’s unique comprehensive health checkup system for early detection of disease. Glob Health Med. (2022) 4:9–13. doi: 10.35772/ghm.2021.01109
9. Hudson MM, Ehrhardt MJ, Bhakta N, Baassiri M, Eissa H, Chemaitilly W, et al. Approach for classification and severity grading of long-term and late-onset health events among childhood cancer survivors in the St. Jude Lifetime Cohort. Cancer Epidemiol Biomarkers Prev. (2017) 26:666–74. doi: 10.1158/1055-9965
10. Kanda Y. Investigation of the freely available easy-touse software ‘EZR’ for medical statistics. Bone Marrow Transpl. (2013) 48:452–8. doi: 10.1038/bmt.2012.244
11. Immonen E, Nikkilä A, Peltomäki T, Aine L, Lohi O. Late adverse effects of childhood acute lymphoblastic leukemia treatment on developing dentition. Pediatric Blood Cancer. (2021) 68:e29200. doi: 10.1002/pbc.29200
12. Polder BJ, Van’t Hof MA, Van der Linden FPGM, Kuijpers-Jagtman AM. A meta-analysis of the prevalence of dental agenesis of permanent teeth. Commun Dent Oral Epidemiol. (2004) 32:217–26. doi: 10.1111/j.1600-0528.2004.00158.x
13. van der Pal HJ, van Dalen EC, Hauptmann M, Kok WE, Caron HN, van den Bos C, et al. Cardiac function in 5-year survivors of childhood cancer: a long-term follow-up study. Arch Intern Med. (2010) 170:1247–55. doi: 10.1001/archinternmed.2010.233
14. Armstrong GT, Joshi VM, Ness KK, Marwick TH, Zhang N, Srivastava D, et al. Comprehensive echocardiographic detection of treatment-related cardiac dysfunction in adult survivors of childhood cancer: results from the St. Jude Lifetime Cohort Study. J Am Coll Cardiol. (2015) 65:2511–22. doi: 10.1016/j.jacc.2015.04.013
15. Poon LHJ, Yu CP, Peng L, Ewig CL, Zhang H, Li CK, et al. Clinical ascertainment of health outcomes in Asian survivors of childhood cancer: a systematic review. J Cancer Surviv. (2019) 13:374–96. doi: 10.1007/s11764-019-00759-9
Keywords: childhood cancer survivor, health problem, late effects, long-term care, screening
Citation: Yoshimoto-Suzuki Y, Hasegawa D, Hosoya Y, Saito G, Nagase K, Gunji M, Kobayashi K, Ishida Y, Manabe A and Ozawa M (2022) Significance of active screening for detection of health problems in childhood cancer survivors. Front. Pediatr. 10:947646. doi: 10.3389/fped.2022.947646
Received: 19 May 2022; Accepted: 09 September 2022;
Published: 06 October 2022.
Edited by:
Yuko Ishizaki, Kansai Medical University, JapanReviewed by:
AnnaLynn Williams, University of Rochester Medical Center, United StatesCopyright © 2022 Yoshimoto-Suzuki, Hasegawa, Hosoya, Saito, Nagase, Gunji, Kobayashi, Ishida, Manabe and Ozawa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Miwa Ozawa, mochiwa@luke.ac.jp
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.