- Department of Cardiac Vascular Surgery, The First Medical Center of the People's Liberation Army General Hospital, Beijing, China
Background: Depression is not uncommon among older adults with heart diseases and is related to poor prognosis at clinical setting. We aim to explore the association between plant-based diets and depression in older adults with heart disease and further investigate the mediating role of sleep disturbances in this relationship.
Methods: A cross-sectional sample of 2039 older adults with heart diseases were recruited from the 2018 Chinese Longitudinal Healthy Longevity Survey (CLHLS). Each individual completed assessments on dietary frequency, depression, sleep quality and duration. Plant-based diet index (PDI), healthy plant-based diet index (hPDI) and unhealthy plant-based diet index (uPDI) were calculated. Logistic regression models and restricted cubic spline curves (RCS) were employed to explore the relationship between plant-based diets and depression in older adults with heart disease. Meanwhile, mediation analysis was used to investigate the mediating roles of sleep quality and sleep duration.
Results: The higher the PDI (OR: 0.56, 95% CI: 0.36–0.88) and the hPDI (OR: 0.39, 95% CI: 0.24–0.62), the lower the risk of depression in older adults with heart disease. Conversely, the higher the uPDI, the higher the risk of depression (OR: 1.76, 95% CI: 1.07–2.92). RCS further confirmed a negative linear dose–response relationship between PDI, hPDI and depression in older adults with heart disease, and a positive trend was found between uPDI and depression. Notably, sleep quality (Indirect effect: −0.031, mediated proportion: 61%) partially mediated the relationship between PDI and depression. In the sex-based subgroup analysis, uPDI was only associated with a higher risk of depression in females.
Conclusion: This is the first study to suggest a significant negative relationship between plant-based diets and depression in older adults with heart disease. Sleep quality plays a mediating role in the association between plant-based diets and depression. Optimizing the dietary structure and improve sleep quality may help reduce the risk of depression in older adults with heart disease.
1 Introduction
With the aging of global population, the prevalence of cardiovascular diseases (CVD) among the elderly is showing a sustained upward trend (1). According to Global Burden of Cardiovascular Diseases 1999–2022, the proportion of deaths caused by CVD among the elderly accounts for as high as 66% of the total deaths (2). The prevalence of depression among older adults with CVD is two to three times higher than that in the general population (3, 4), especially among patients who have had myocardial infarction, heart failure, and coronary artery bypass grafting (5, 6). Among older adults with coronary artery disease (CAD), approximately 30% experience an exacerbation of depressive symptoms, and 15–20% are diagnosed with major depressive disorder (MDD). A large body of studies have shown a significant association between depression and CVD, and depression is positively correlated with the incidence and mortality of heart diseases, including increased mortality and readmission rates (6–8). After adjusted for traditional risk factors of heart disease, the impact of depression on the poor prognosis of CVD still remains significant (9). Risk factors associated with depression in older adults with CVD are multi-faceted, involving various fields such as psychological, social, and biological (10–13). Preventing the onset of depression is of significant importance in aspects such as improving the prognosis of older adults with heart disease, reducing medical costs, and enhancing the patients’ quality of life (14, 15).
Dietary patterns in older adults with heart disease may serve as a strategy for depression prevention, since dietary factors play a crucial role in the development of depression (16, 17). A plant-based diet may affect mood by altering the intake of neurotransmitters such as tryptophan (18). Some studies suggest that a healthy diet pattern can reduce the risk of depression, while an unhealthy one may increase it (19, 20). For older adults with heart disease, dietary factors may be of even greater importance since dietary factors are not only related to depression but also closely associated with the development of CVD (21–23). Plant-based diets refer to a dietary pattern that emphasizes plant-based foods as the main source of food (24). Satija et al. used a hierarchical approach to create three plant-based diet indices: the overall Plant-based Diet Index (PDI), the unhealthy Plant-based Diet Index (uPDI), and the healthy Plant-based Diet Index (hPDI) (25). This model takes into account the intake of various plant-based and animal-based foods. It assigns different scores according to their impacts on health to evaluate the dietary pattern. a large number of studies suggested that PDI is associated with a lower risk of stroke (26), diabetes (27) CVD, and overall mortality (28). A plant-based diet is typically rich in antioxidants, such as vitamin C, folic acid, and phytochemicals, which play a critical role in reducing neuro-oxidative damage and protecting neurons (29). A cross-sectional study of multi-center data indicated that no significant association between PDI, hPDI and depression or anxiety exists, while uPDI is associated with an increased risk of depression and anxiety (30). Other studies on different populations, including the healthy middle-aged and the elderly, adolescents, and patients with diabetes, found that adhering to hPDI dietary pattern is associated with a reduced risk of dementia and depression, whereas adhering to uPDI dietary pattern is associated with an increased risk (31–33). However, the relationship between the plant-based diets and depression in older adults with heart diseases has not been explored yet.
Sleep disturbances are prevalent among the elderly population, particularly among those with heart diseases (34). The relationship between sleep disturbances and depression has been reported by numerous studies (35, 36). Some regarded sleep abnormalities as common symptoms of depression, but a bidirectional relationship between sleep and depression has also been found (37, 38). A longitudinal study suggest that sleep problems often indicate the potential emergence of depression (39). Meanwhile, patients with depression also tend to have sleep issues (40). On the other hand, a healthy plant-based diet can improve sleep quality, while insufficient intake of plant-based diet may trigger sleep problems (41–43). However, the role of sleep disturbances in the relationship between PDI and depression among older adults with heart disease remains to be explored.
To fill the gaps in the aforementioned research, we aim to explore the relationship between plant-based diets and depression in older adults with heart disease using a large, nationally representative population sample. Meanwhile, the mediating role of disturbances in sleep quality and duration in the association between plant-based diets and depression. Our work has significant clinical implications as it may indicate an evidence-based approach for the prevention of depression in older adults with heart disease.
2 Materials and methods
2.1 Research subjects
The participants in our study are recruited from The Chinese Longitudinal Healthy Longevity Survey (CLHLS) (44). This project is a follow-up survey of the elderly organized by the Center for Healthy Aging and Development Studies/National School of Development at Peking University. It began in 1998 and were carried out periodically, with data collection conducted every 3 to 4 years for the same population. The survey covers 23 provinces, municipalities, and autonomous regions across the country. The questionnaires are divided into two types: the questionnaire for surviving interviewees and the questionnaire for family members of deceased elderly people. The survey subjects include the elderly aged 65 and above and adult children aged 35–64. A total of 15,874 elderly people over 65 were interviewed, and information on 2,226 elderly people who died during the period from 2014 to 2018 was collected. This survey has obtained formal authorization from the Biomedical Ethics Committee of Peking University, China (Approval No.: IRB00001052-13074), and every interviewee participating in the survey has signed an informed consent form as required. Studies using data from CLHLS datasets have been previously published (45–47).
We utilized the questionnaire data of surviving interviewees from the CLHLS 2018 (Total participants:15874). Participants aged below 65 years old and with missing values in assessment of depression, sleep, and dietary intake were excluded. Eventually, 2039 older adults with heart diseases were included in the analysis (see Supplementary Figure S1).
2.2 Outcome measures
In this study, the dependent variable is the presence of depression. A shortened version of Center for Epidemiological Studies Depression Scale (CES-D-9) to assess depression, by using 9 items excluding sleep assessment (48, 49). The CES-D-9 adopts a 4-point Likert scale. Responses to each question are “rarely,” “occasionally,” “often,” and “most of the time.” Scores for items with positive effects are reversed. The total score of CES-D-9 ranges from 0 to 27. We defined a CES-D-9 ≥ 9 as indicating the presence of depression. The Cronbach’sαof CES-D-9 is 0.77 in our study, demonstrating good internal consistency and reliability.
2.3 Measurement of PDI
Based on previous research (25, 43, 50), we evaluated plant-based diets by calculation of the PDI (Plant-based Diet Index), healthy plant-based diet index (hPDI) and unhealthy plant-based diet index (uPDI) based on participants’ dietary information using a simplified food frequency questionnaire, which was tested for reliability and validity in previous studies (51, 52). Taking into account the composition of various foods, 16 of the most commonly consumed foods were classified into three groups: animal-sourced foods, healthy plant-based foods, and unhealthy plant-based foods. For the 16 food groups, a score rating from 1–5 was assigned. Regarding PDI, the scores of plant-based foods increase from 1 to 5 as the consumption frequency rises, while the scores of animal-based foods show a reversed trend. hPDI assigns positive scores to healthy plant-based foods and negative scores to unhealthy plant-based foods as well as animal-based foods. In contrast, uPDI gives positive scores to unhealthy plant-based foods and negative scores to healthy plant-based foods and animal-based foods. Then, all the scores are summed up to obtain the final scores of PDI, hPDI, and uPDI for the 16 food groups. For more detailed information on the construction of PDI, hPDI, and uPDI, please refer to Supplementary Table S1. Theoretically, the score range of these indices varies from 16 to 80 points. A higher score of PDI and hPDI indicates a stronger compliance with plant-based diets, while a higher uPDI indicates the opposite. In addition, we divided the scores of PDI, hPDI, and uPDI into four quartiles, Q1, Q2, Q3, and Q4, for subsequent analysis. In our study, the Cronbach’sαof PDI, hPDI and uPDI were 0.79, 0.76 and 0.77, respectively.
2.4 Assessment of sleep health
The assessment of sleep health is defined by two components: sleep quality and sleep duration. We rely on two questions in the questionnaire for evaluation. One is “How is your current sleep quality?” and the other is “How many hours do you usually sleep per day currently?.” In terms of sleep quality, for the responses of “very good,” “good,” “fair,” “poor,” and “very poor” from the respondents, they are assigned scores from 1 to 5 in sequence. The higher the score, the worse the sleep quality. Regarding sleep duration, based on the sleep-time recommendations for cardiovascular disease patients in multiple studies (34, 53), the sleep duration is classified into three categories: less than 6 h, 6–8 h, and more than 8 h. Among these, a sleep duration of less than 6 h or more than 8 h is assigned a value of “1” during the assessment, indicating disturbance of sleep duration, while the normal sleep duration (6–8 h) is assigned a value of “0,” suggesting no disturbances in sleep duration.
2.5 Covariates
Based on previous relevant studies (54–58), the covariates involved in this study cover two aspects: the demographic and socioeconomic characteristics, including gender, age, and place of residence, marital status, educational status, occupation, annual family income, housing property, and regional factors (from south or north China); the life style and comorbidity: including factors like smoking, alcohol consumption, exercise, body mass index, diabetes, dyslipidemia, and cerebrovascular diseases. Additionally, we have created and included Directed Acyclic Graphs (DAG) diagrams to visually represent the relationships between the variables studied (see Supplementary Figure S2).
2.6 Statistical analysis
Categorical variables were described using frequencies and percentages. Since none of the numerical variables passed the normality test, continuous variables were described using the median (interquartile range). The Chi-square test and Mann–Whitney U test were used to compare the differences between depressed and non-depressed individuals for categorical variables and continuous variables, respectively. Three logistic regression models were used to systematically examine the relationship between plant-based diets and depression while controlling for potential confounders at different levels. Model A did not adjust for any covariates to identify the raw association and lays the groundwork for further analysis (Crude model). Model B was adjusted for key demographic and socioeconomic variables including gender, age, place of residence, geographical region, marital status, education level, occupation, annual family income, and housing property. Model C was further adjusted for lifestyle and comorbidity factors such as smoking, alcohol consumption, exercise, BMI, diabetes, cerebrovascular diseases, and dyslipidemia based on Model B. Restricted cubic spline (RCS) with four knots was used to explore the dose–response relationships between PDI, uPDI, hPDI and depression in older adults with heart disease. In addition, subgroup analyses by different genders were conducted. Subsequently, Spearman correlation analysis was used to explore the correlations among PDI, uPDI, hPDI, sleep quality, sleep duration, and depression scores. Then, the mediating effects of sleep quality and sleep duration disorders in the relationship between plant-based diets and depression were further tested separately. The Bootstrap method was used to evaluate their mediating effects and 95% CI. PDI, uPDI, and hPDI were, respectively, included as independent variables in three mediating models. All statistical analyses were performed using R (version 4.4.1). The R package “rms” was used for restricted cubic spline (RCS) analysis, and the “mediation” package was used for mediation analysis. A two-sided p-value<0.05 was defined as significant in all tests.
3 Results
3.1 Characteristics of study participants
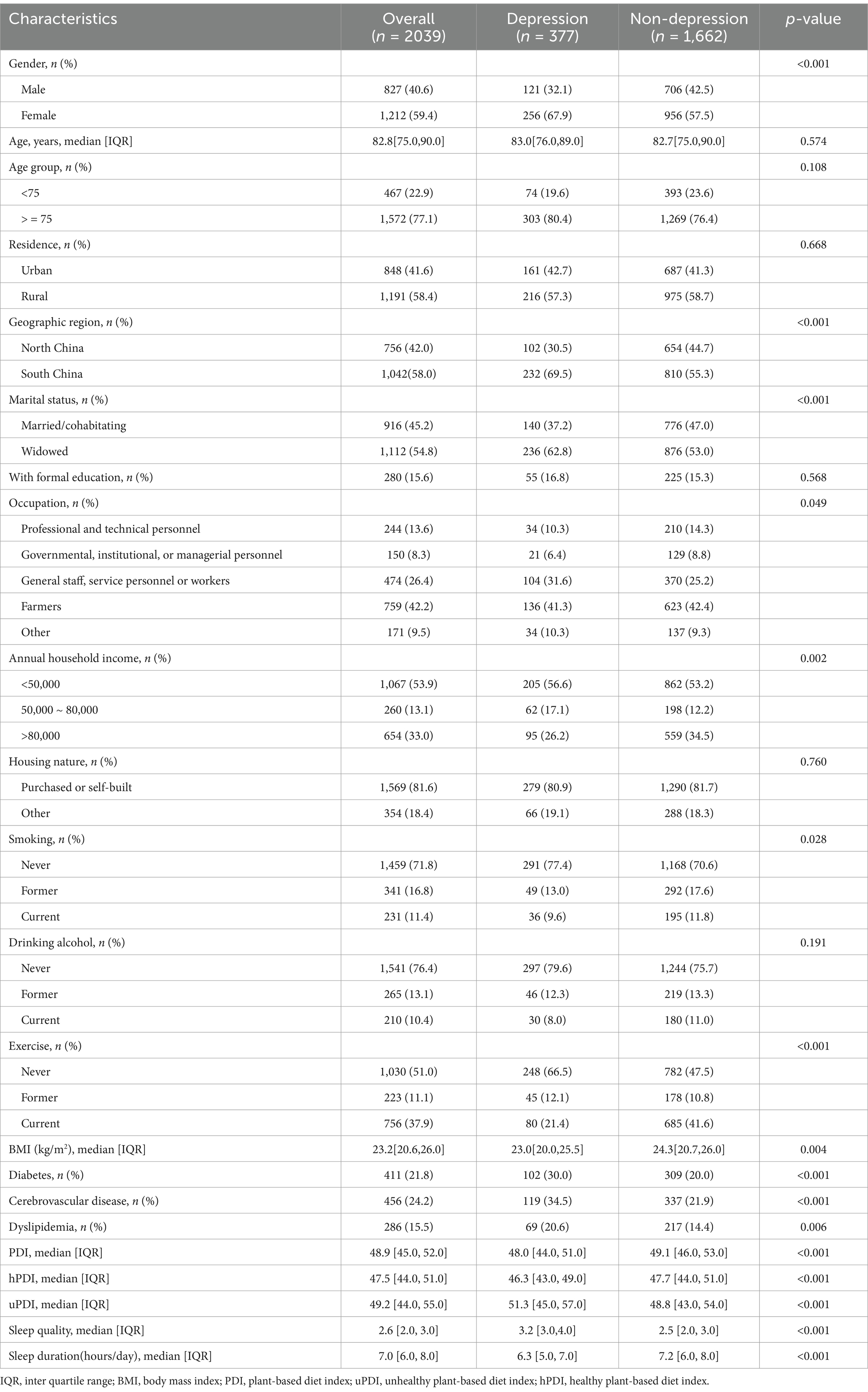
In this study, 2039 older adults with heart disease were included, 827 (40.6%) were male and 1,212 (59.4%) were female. The median age of these participants was 82.8 (IQR, 75.0–90.0) years old. There were 848 (41.6%) urban residents, 1,112 (54.8%) widowed individuals, and 1,042 (58.0%) participants living in the southern region of China. The specific baseline characteristics grouped by the presence or absence of depression are presented in Table 1.
3.2 Association between plant-based diets and depression
In Model A, PDI (OR: 0.52, 95% CI: 0.37–0.70) and hPDI (OR: 0.44, 95% CI: 0.31–0.62) were associated with lower risk of depression. However, uPDI was associated with higher prevalence of depression (OR: 2.05, 95% CI: 1.49–2.82).
In the partially adjusted model (Model B), PDI (OR: 0.52, 95% CI: 0.35–0.77) and hPDI (OR: 0.45, 95% CI: 0.30–0.67) were still associated with lower risk of depression, while uPDI showed a positive connection with depression (OR: 1.95, 95% CI: 1.27–3.01).
In the fully adjusted model (Model C), greater adherence to PDI (OR: 0.56, 95% CI: 0.36–0.88) and hPDI (OR: 0.39, 95% CI: 0.24–0.62) were associated with a lower prevalence of depression in older adults with heart disease, while uPDI still positively associated with risk of depression (OR: 1.76, 95% CI: 1.07–2.92) (see Table 2).
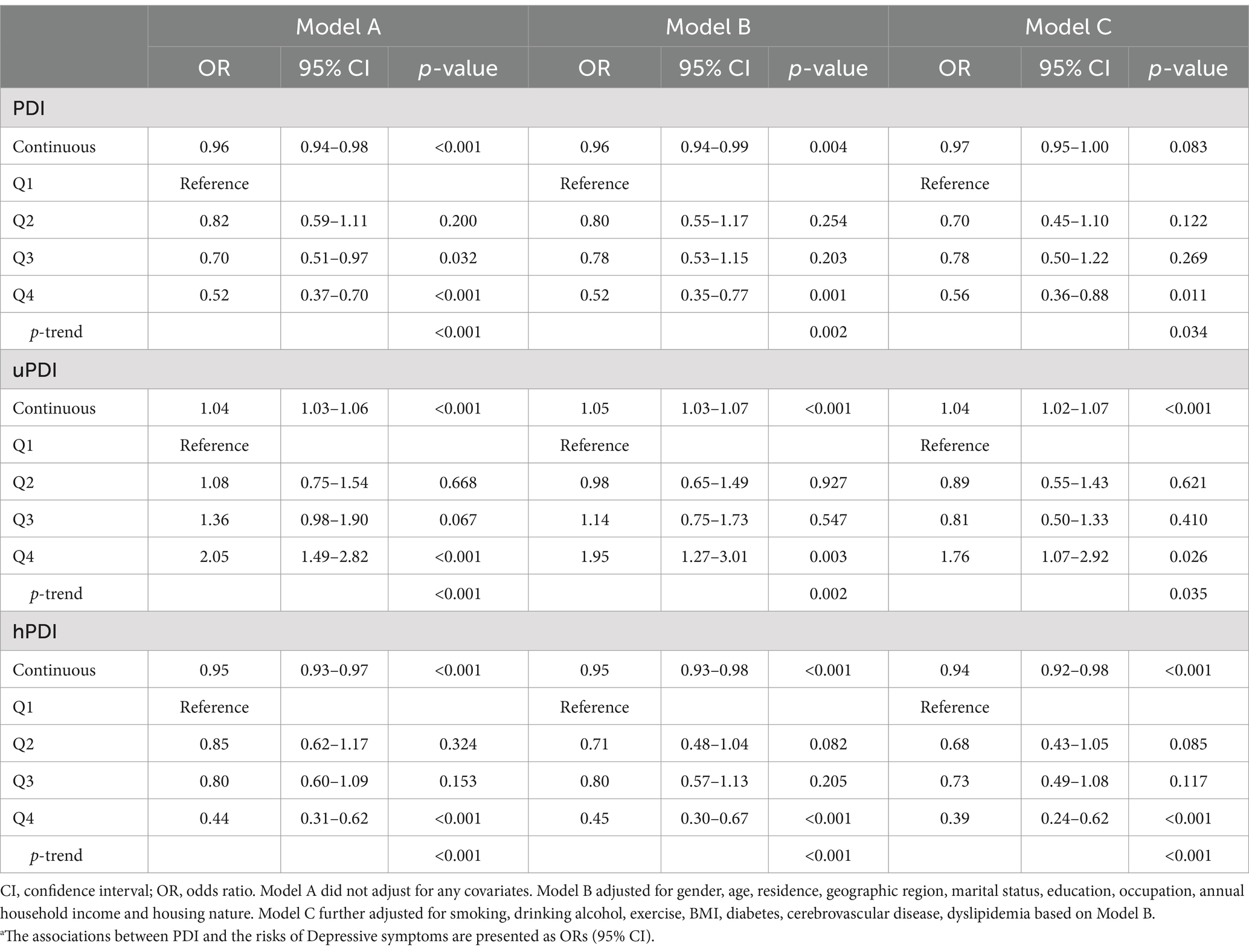
Table 2. Associations between PDI and risks of depressive symptoms among older adults with heart disease.a
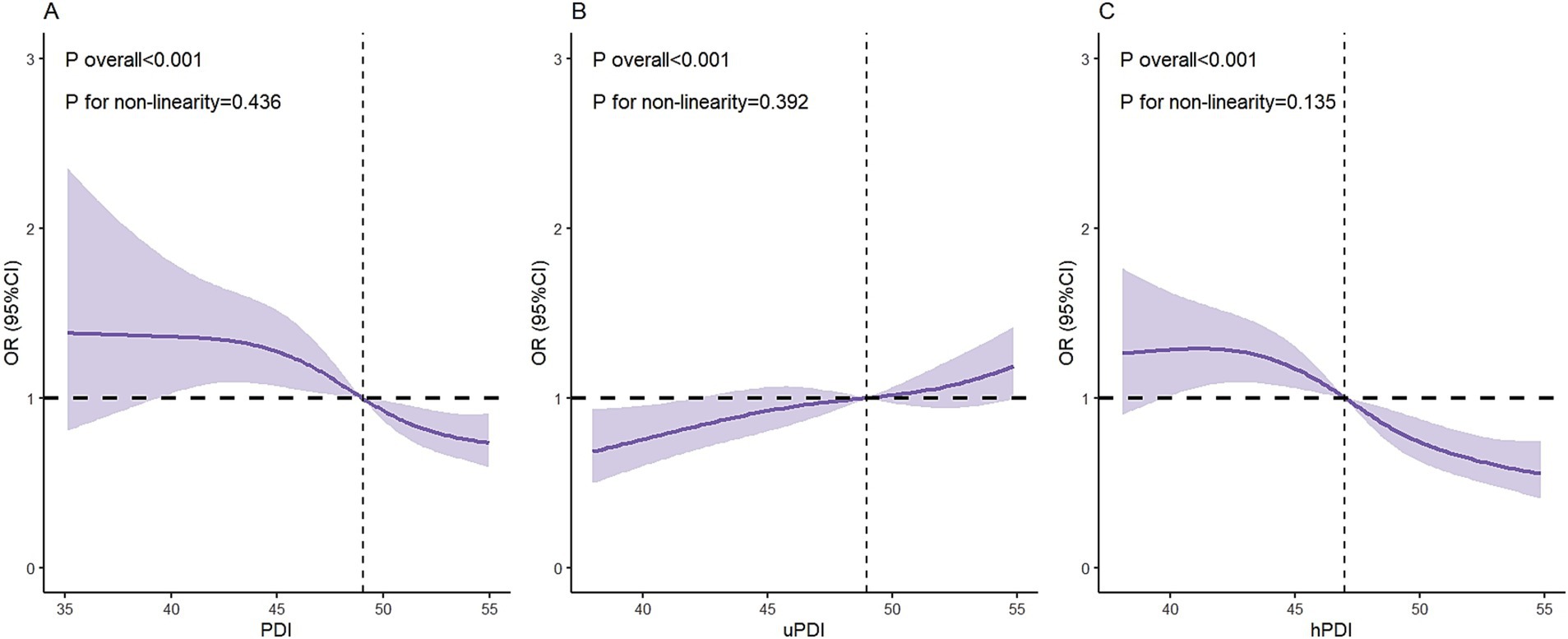
The results of the RCS curves indicated that both the PDI and hPDI diet showed a negative linear dose–response relationship with depression in older adults with heart disease, while the uPDI diet was positively correlated with depression in these patients (see Figure 1).
3.3 Subgroup analysis
The subgroup analysis showed that, for the uPDI, compared with the female patients in the lowest quartile (Q1), highest quartile (Q4) was associated with an increased risk of depression (OR: 1.97, 95% CI: 1.04–3.82). For the hPDI, compared with the lowest quartile, Q4 in both the male (OR: 0.26, 95% CI: 0.11–0.58) and female (OR: 0.49, 95% CI: 0.26–0.91) subgroups had a lower risk of depression (Table 3).
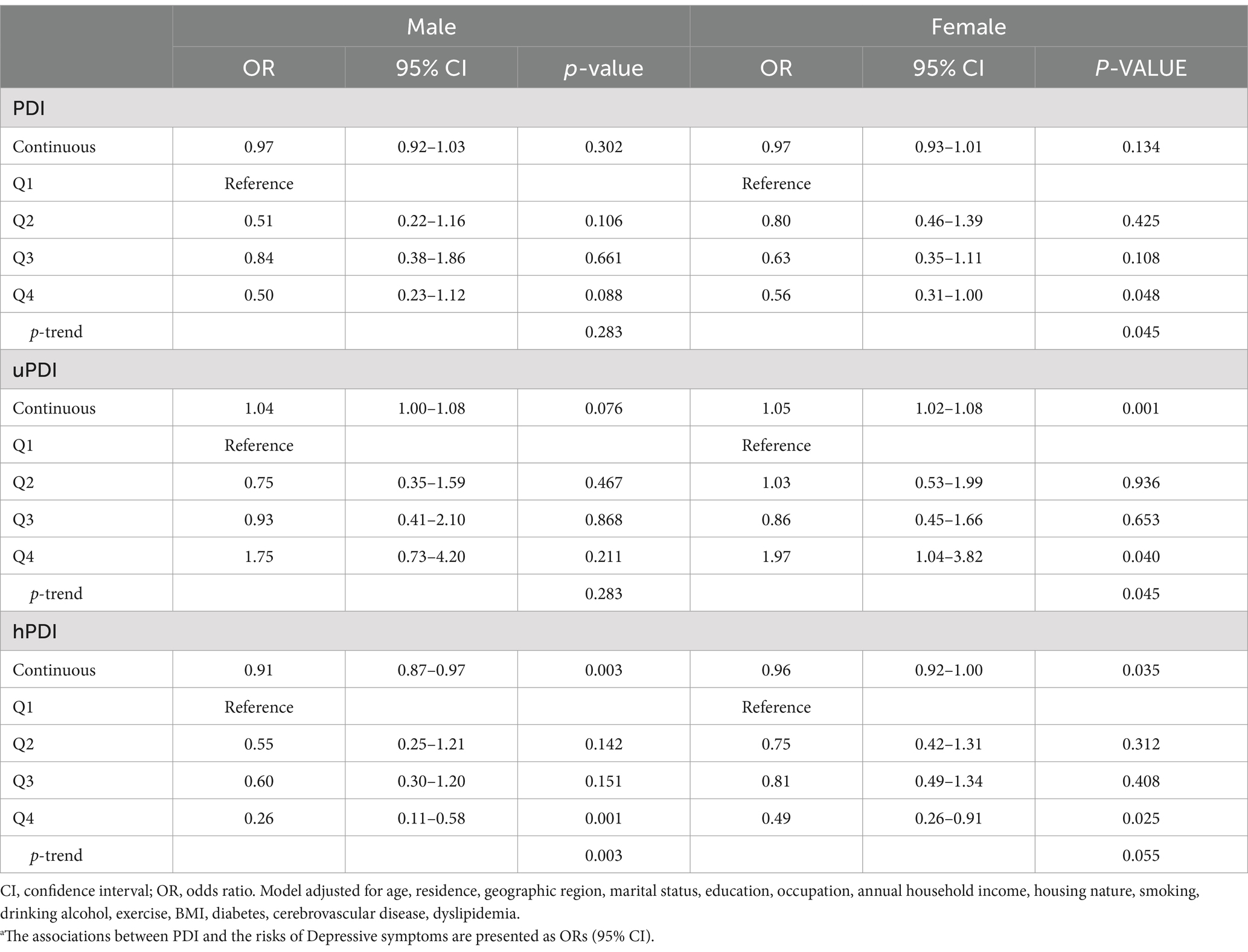
Table 3. Sex differences in the associations between PDI and Risks of Depressive Symptoms among older adults with heart disease.a
3.4 Spearman correlation analysis
Depressive symptoms in heart disease patients were positively correlated with poor sleep quality (r = 0.34) and sleep duration disturbances (r = 0.08). Depressive symptoms in older adults with heart disease showed a negative correlation with the PDI (r = −0.10) and the hPDI (r = −0.13), and a positive correlation with the uPDI (r = 0.17). Poor sleep quality was negatively correlated with the PDI (r = −0.13), and hPDI (r = −0.09) and positively correlated with the uPDI (r = 0.13), all p-values<0.001 (Figure 2).
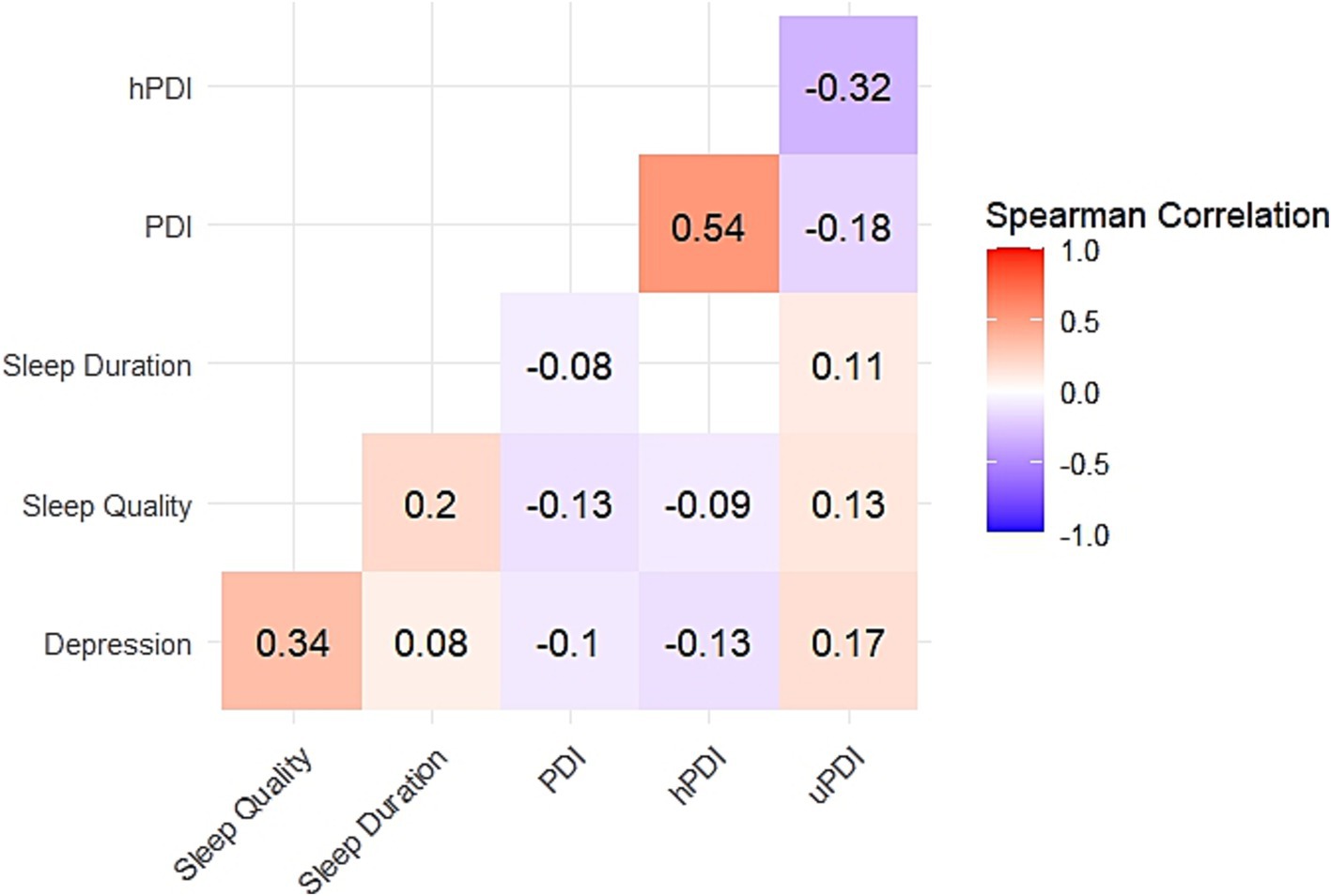
Figure 2. Results of Spearman correlation analysis. Red represents positive correlation, blue represents negative correlation, and the darker the color, the stronger the correlation. White indicates that there is no significant correlation between variables. All p < 0.001 for correlation with color.
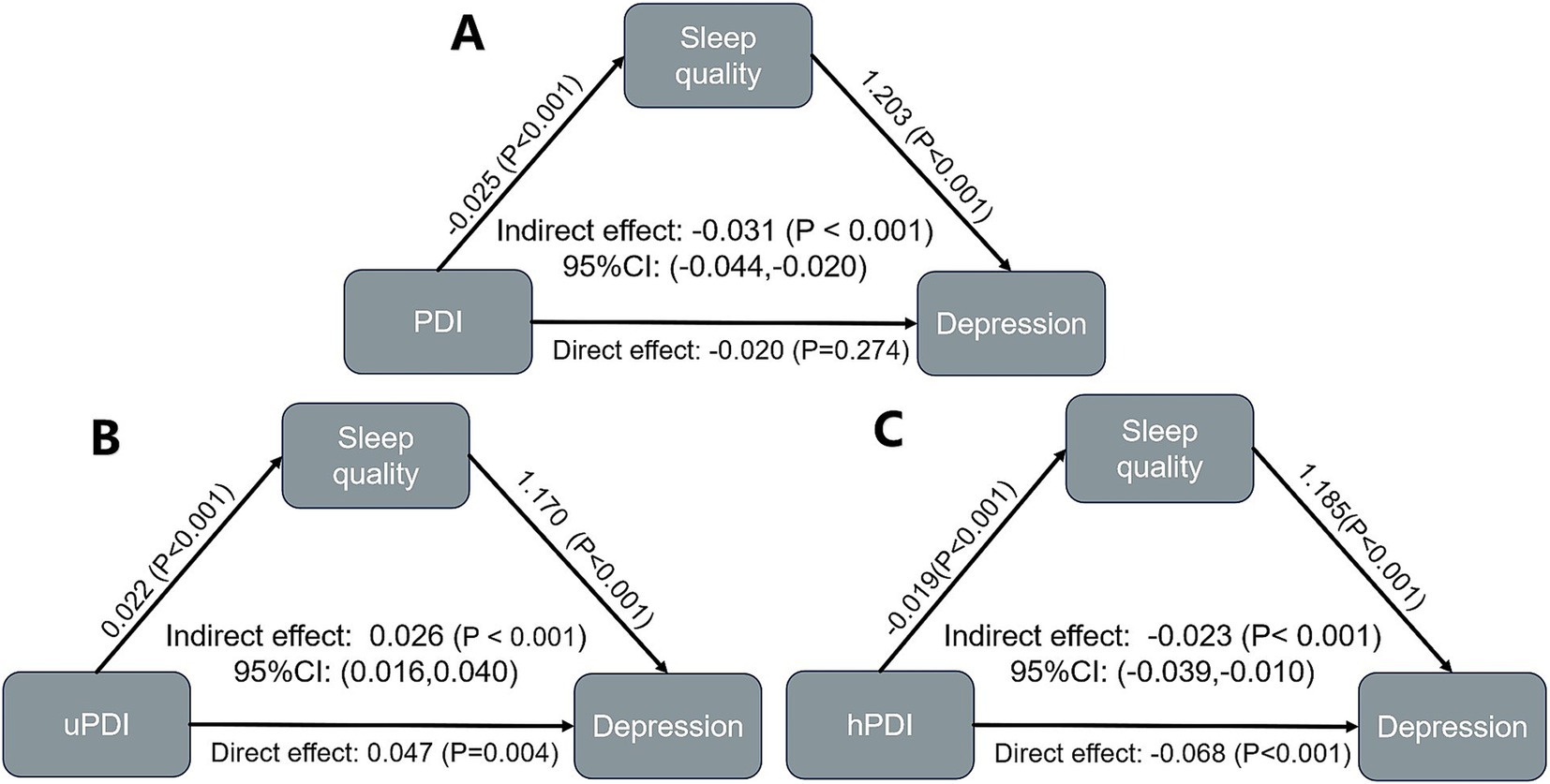
3.5 The mediating role of sleep quality and sleep duration
Sleep quality has a significant mediating effect in the relationship between PDI and depression in older adults with heart disease (Indirect effect: −0.031, 95% CI: −0.044 to −0.020). Sleep quality also has a significant mediating effect in the relationship between uPDI and depression (Indirect effect: 0.026, 95% CI: 0.016 to 0.040). Similarly, a mediating effect exists between hPDI and depression (Indirect effect: −0.023, 95% CI: −0.039 to −0.010) (Figure 3, Supplementary Table S2). The mediating effect of sleep duration in the relationship between plant-based diets and depression in older adults with heart disease was not significant (Supplementary Figure S3).
4 Discussion
For the first time, our study deeply explored the association between plant-based diets and depression in older adults with heart disease and further analyzed the mediating role played by sleep disturbances. We found a significant negative relationship between plant-based diets and depression. In addition, improved sleep quality showed a mediating effect in the association between healthy plant-based diets and depression. Sex difference was also examined and significant relationship between uPDI and the occurrence of depression was found in women, while there was no such relationship in men.
Participants with higher levels of PDI and hPDI had lower prevalence of depression, which may indicate that the higher the patients’ compliance with a healthy plant-based diet, the lower the risk of developing depressive symptoms. Multiple studies, such as those on young women (59) and the elderly (60), have shown that a high-quality plant-based diet is associated with a reduced risk of depressive symptoms. A cross-sectional study by Lee et al. found that lifestyle changes such as diet might have a positive impact on depression (61). Building on the above-mentioned studies, this research also confirmed the negative correlation between plant-based diets and depression among heart disease patients, further enriching the research in this field. Previous studies have shown that plant-based diets are rich in dietary fiber, which can improve the gut microbiota, and gut microbiota dysbiosis is associated with the occurrence of depression (62, 63). Moreover, healthy plant-based diets are abundant in unsaturated fatty acids and antioxidant components like flavonoids and vitamins. These substances have been found to possess anti-inflammatory properties (64, 65). Inflammation, on the other hand, is of great significance in the pathophysiology of both heart disease and depression (66–68).
Disturbances in sleep quality and sleep duration are another major risk factors for depression in older adults with heart disease. Of note, the correlation between sleep quality and depression seemed stronger, while the relationship between sleep duration and depression is relatively weaker. Some studies have shown that sleep disorders are important risk factors for depression and have a bidirectional association with depression (39, 69). Sleep disorders are associated with more severe depressive outcomes, including suicide risk, comorbidity with anxiety disorders, and others (70, 71). Some studies on the mechanisms of sleep and the onset of depression have found that sleep disturbances may disrupt the function of neural synaptic networks, including those in the hippocampus and prefrontal cortex, leading to impaired cognitive function. This process is associated with the development of depression (72, 73). In addition, patients with depression often exhibit excessive arousal. Depressive symptoms and sleep disturbances may interact with each other through common neurobiological pathways (74, 75).
Another significant finding of this study is that plant-based diets may improve the sleep quality and thus help lower the risk of depression in older adults with heart disease. Specifically, a healthy plant-based diet pattern helps optimize sleep quality, thus playing a role in reducing the risk of depression. In contrast, an unhealthy plant-based diet pattern may have a negative impact on sleep quality, thereby contributing to the occurrence or exacerbation of depression. Previous studies have found that adherence to a healthy plant-based diet is positively correlated with optimal sleep quality (42), and improved sleep can reduce the risk of depression (76, 77). From a biological perspective, phytoestrogens such as flavonoids, isoflavones, and lignans contained in plant-based diets can improve sleep quality. Moreover, a variety of plant-based foods such as fruits and vegetables can enhance sleep health by increasing the levels of melatonin and serotonin (78). Improved sleep can affect the regulatory mechanisms of the nervous system, including the circadian rhythm, neurotransmitter systems, and melatonin, thus alleviating symptoms of depression (79), the above-mentioned studies all support the findings of this research.
In addition, through sex-based subgroup analysis, this study further found that the uPDI diet was associated with the risk of depression in the female subgroup but not in males. As for the hPDI diet pattern, the protective effect of plant-based diets on depression in female older adults with heart disease was relatively weak. Such sex differences are not uncommon in research in the field of mental health. According to the theory of psychological gender differences, men and women differ in many aspects such as physiological structure, hormone levels, and social roles. These factors cause them to have different psychological and physiological responses to the same external stimuli (such as changes in diet patterns) (80). A large number of previous studies have found that women are more prone to be troubled by depression (81, 82), which is consistent with the conclusion of this study.
This study has several advantages. We used a large, nationally representative sample population, taking the lead in exploring the association between plant-based diets and depression in Chinese older adults with heart disease, and deeply analyzing the mediating role of sleep disorders in this relationship. When analyzing the relationship between PDI and depression in older adults with heart disease, this study excluded a variety of confounding factors to ensure the robustness of the results.
This study also has several limitations. Firstly, the cross-sectional design adopted in this study limit the ability to establish a causal relationship. The findings of this study need to be confirmed by future longitudinal intervention-based studies. Secondly, the data on diet, depression, and sleep status in this study were all derived from patients’ self-reports. Participants may have recall bias, leading to inaccurate assessments of some participants. Future research needs to adopt more objective assessment methods to explore this complex relationship more comprehensively, in-depth, and accurately, providing a more reliable basis for the health management of older adults with heart disease.
5 Conclusion
In conclusion, plant-based diets are associated with a lower risk depression in Chinese older adults with heart disease, and sleep quality disturbances can partially mediate this relationship. The results of this study provide a clear and evidence-based direction for dietary guidance practices for depression prevention in older adults with heart disease. By optimizing the diet structure and actively improving patients’ sleep quality, the risk of depression in older adults with heart disease could possibly reduce, as well as the prognosis of CVD.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: the data supporting the results of this study are publicly available in the China Longitudinal Healthy Longevity Survey (CLHLS) on the Peking University Open Data Platform: https://opendata.pku.edu.cn/dataverse/CHADS.
Ethics statement
The studies involving humans were approved by Medical Ethics Committee of Peking University, China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YY: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. YC: Formal analysis, Methodology, Writing – review & editing. NC: Funding acquisition, Resources, Writing – review & editing. JZ: Conceptualization, Project administration, Writing – review & editing. QX: Investigation, Resources, Writing – review & editing. YW: Formal analysis, Methodology, Writing – review & editing. WZ: Investigation, Project administration, Writing – review & editing. CY: Investigation, Methodology, Writing – review & editing. HL: Conceptualization, Methodology, Writing – review & editing. ZG: Conceptualization, Funding acquisition, Methodology, Resources, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by the China Rehabilitation Medical Association Science and Technology Development Project 2024 (Grant No.: KFKT-2024-003).
Acknowledgments
We sincerely thank all the effort made by the staff and the participants of the CLHLS study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1567436/full#supplementary-material
References
1. Ruan, Y, Guo, Y, Zheng, Y, Huang, Z, Sun, S, Kowal, P, et al. Cardiovascular disease (Cvd) and associated risk factors among older adults in six low-and middle-income countries: results from sage wave 1. BMC Public Health. (2018) 18:778. doi: 10.1186/s12889-018-5653-9
2. Mensah, GA, Fuster, V, Murray, CJL, and Roth, GA. Global burden of cardiovascular diseases and risks, 1990-2022. J Am Coll Cardiol. (2023) 82:2350–473. doi: 10.1016/j.jacc.2023.11.007
3. Rutledge, T, Reis, VA, Linke, SE, Greenberg, BH, and Mills, PJ. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. (2006) 48:1527–37. doi: 10.1016/j.jacc.2006.06.055
4. Li, H, Zheng, D, Li, Z, Wu, Z, Feng, W, Cao, X, et al. Association of Depressive Symptoms with incident cardiovascular diseases in middle-aged and older Chinese adults. JAMA Netw Open. (2019) 2:e1916591. doi: 10.1001/jamanetworkopen.2019.16591
5. Cooney, MT, Kotseva, K, Dudina, A, De Backer, G, Wood, D, and Graham, I. Determinants of risk factor control in subjects with coronary heart disease: a report from the Euroaspire iii investigators. Eur J Prev Cardiol. (2013) 20:686–91. doi: 10.1177/2047487312445562
6. Colquhoun, DM, Bunker, SJ, Clarke, DM, Glozier, N, Hare, DL, Hickie, IB, et al. Screening, referral and treatment for depression in patients with coronary heart disease. Med J Aust. (2013) 198:483–4. doi: 10.5694/mja13.10153
7. Jiang, W, Alexander, J, Christopher, E, Kuchibhatla, M, Gaulden, LH, Cuffe, MS, et al. Relationship of depression to increased risk of mortality and Rehospitalization in patients with congestive heart failure. Arch Intern Med. (2001) 161:1849–56. doi: 10.1001/archinte.161.15.1849
8. Nicholson, A, Kuper, H, and Hemingway, H. Depression as an Aetiologic and prognostic factor in coronary heart disease: a Meta-analysis of 6362 events among 146 538 participants in 54 observational studies. Eur Heart J. (2006) 27:2763–74. doi: 10.1093/eurheartj/ehl338
9. Ford, DE, Mead, LA, Chang, PP, Cooper-Patrick, L, Wang, NY, and Klag, MJ. Depression is a risk factor for coronary artery disease in men: the precursors study. Arch Intern Med. (1998) 158:1422–6. doi: 10.1001/archinte.158.13.1422
10. Kessler, RC, Berglund, P, Demler, O, Jin, R, Koretz, D, Merikangas, KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (Ncs-R). JAMA. (2003) 289:3095–105. doi: 10.1001/jama.289.23.3095
11. Shapiro, PA, Fedoronko, DA, Epstein, LA, Mirasol, EG, and Desai, CV. Psychiatric aspects of heart and lung disease in critical care. Crit Care Clin. (2008) 24:921–47. doi: 10.1016/j.ccc.2008.05.003
12. de Jonge, P, Mangano, D, and Whooley, MA. Differential Association of Cognitive and Somatic Depressive Symptoms with heart rate variability in patients with stable coronary heart disease: findings from the heart and soul study. Psychosom Med. (2007) 69:735–9. doi: 10.1097/PSY.0b013e31815743ca
13. Denollet, J, Strik, JJ, Lousberg, R, and Honig, A. Recognizing increased risk of depressive comorbidity after myocardial infarction: looking for 4 symptoms of anxiety-depression. Psychother Psychosom. (2006) 75:346–52. doi: 10.1159/000095440
14. Murray, CJ, and Lopez, AD. Measuring the global burden of disease. N Engl J Med. (2013) 369:448–57. doi: 10.1056/NEJMra1201534
15. Armstrong, NM, Meoni, LA, Carlson, MC, Xue, QL, Bandeen-Roche, K, Gallo, JJ, et al. Cardiovascular risk factors and risk of incident depression throughout adulthood among men: the Johns Hopkins precursors study. J Affect Disord. (2017) 214:60–6. doi: 10.1016/j.jad.2017.03.004
16. Gorbachev, D, Markina, E, Chigareva, O, Gradinar, A, Borisova, N, and Syunyakov, T. Dietary patterns as modifiable risk factors for depression: a narrative review. Psychiatr Danub. (2023) 35:423–31.
17. Swainson, J, Reeson, M, Malik, U, Stefanuk, I, Cummins, M, and Sivapalan, S. Diet and depression: a systematic review of whole dietary interventions as treatment in patients with depression. J Affect Disord. (2023) 327:270–8. doi: 10.1016/j.jad.2023.01.094
18. Medawar, E, Huhn, S, Villringer, A, and Veronica, WA. The effects of plant-based diets on the body and the brain: a systematic review. Transl Psychiatry. (2019) 9:226. doi: 10.1038/s41398-019-0552-0
19. Lai, JS, Hiles, S, Bisquera, A, Hure, AJ, McEvoy, M, and Attia, J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. (2014) 99:181–97. doi: 10.3945/ajcn.113.069880
20. O'Neil, A, Quirk, SE, Housden, S, Brennan, SL, Williams, LJ, Pasco, JA, et al. Relationship between diet and mental health in children and adolescents: a systematic review. Am J Public Health. (2014) 104:e31–42. doi: 10.2105/AJPH.2014.302110
21. Eagles, JM, and Robson, SJ. The role of diet and obesity in the association between depression and cardiovascular disease. Br J Psychiatry. (2021) 219:462. doi: 10.1192/bjp.2021.79
22. Zhang, S, Limei, E, Lu, Z, Yu, Y, Yang, X, Chen, Y, et al. The chain-mediating effect of obesity, depressive symptoms on the association between dietary quality and cardiovascular disease risk. Nutrients. (2023) 15:629. doi: 10.3390/nu15030629
23. Hu, EA, Steffen, LM, Coresh, J, Appel, LJ, and Rebholz, CM. Adherence to the healthy eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr. (2020) 150:312–21. doi: 10.1093/jn/nxz218
24. Shen, X, Tilves, C, Kim, H, Tanaka, T, Spira, AP, Chia, CW, et al. Plant-based diets and the gut microbiome: findings from the Baltimore longitudinal study of aging. Am J Clin Nutr. (2024) 119:628–38. doi: 10.1016/j.ajcnut.2024.01.006
25. Satija, A, Bhupathiraju, SN, Spiegelman, D, Chiuve, SE, Manson, JE, Willett, W, et al. Healthful and unhealthful plant-based diets and the risk of coronary heart disease in U.S. adults. J Am Coll Cardiol. (2017) 70:411–22. doi: 10.1016/j.jacc.2017.05.047
26. Baden, MY, Shan, Z, Wang, F, Li, Y, Manson, JE, Rimm, EB, et al. Quality of plant-based diet and risk of Total, ischemic, and hemorrhagic stroke. Neurology. (2021) 96:e1940–53. doi: 10.1212/WNL.0000000000011713
27. Satija, A, Bhupathiraju, SN, Rimm, EB, Spiegelman, D, Chiuve, SE, Borgi, L, et al. Plant-based dietary patterns and incidence of type 2 diabetes in us men and women: results from three prospective cohort studies. PLoS Med. (2016) 13:e1002039. doi: 10.1371/journal.pmed.1002039
28. Kim, H, Caulfield, LE, Garcia-Larsen, V, Steffen, LM, Coresh, J, and Rebholz, CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. (2019) 8:e012865. doi: 10.1161/JAHA.119.012865
29. Wu, PY, Chen, KM, and Belcastro, F. Dietary patterns and depression risk in older adults: systematic review and Meta-analysis. Nutr Rev. (2021) 79:976–87. doi: 10.1093/nutrit/nuaa118
30. Haghighatdoost, F, Mahdavi, A, Mohammadifard, N, Hassannejad, R, Najafi, F, Farshidi, H, et al. The relationship between a plant-based diet and mental health: evidence from a cross-sectional multicentric community trial (Lipokap study). PLoS One. (2023) 18:e0284446. doi: 10.1371/journal.pone.0284446
31. Wu, H, Gu, Y, Meng, G, Wu, H, Zhang, S, Wang, X, et al. Quality of plant-based diet and the risk of dementia and depression among middle-aged and older population. Age Ageing. (2023) 52:afad070. doi: 10.1093/ageing/afad070
32. Khayyatzadeh, SS, Mehramiz, M, Mirmousavi, SJ, Mazidi, M, Ziaee, A, Kazemi-Bajestani, SMR, et al. Adherence to a dash-style diet in relation to depression and aggression in adolescent girls. Psychiatry Res. (2018) 259:104–9. doi: 10.1016/j.psychres.2017.09.075
33. Daneshzad, E, Keshavarz, S-A, Qorbani, M, Larijani, B, Bellissimo, N, and Azadbakht, L. Association of dietary acid load and plant-based diet index with sleep, stress, anxiety and depression in diabetic women. Br J Nutr. (2020) 123:901–12. doi: 10.1017/S0007114519003179
34. Nambiema, A, Lisan, Q, Vaucher, J, Perier, MC, Boutouyrie, P, Danchin, N, et al. Healthy sleep score changes and incident cardiovascular disease in European prospective community-based cohorts. Eur Heart J. (2023) 44:4968–78. doi: 10.1093/eurheartj/ehad657
35. Tonon, AC, Constantino, DB, Amando, GR, Abreu, AC, Francisco, AP, de Oliveira, MAB, et al. Sleep disturbances, circadian activity, and nocturnal light exposure characterize high risk for and current depression in adolescence. Sleep. (2022) 45:zsac104. doi: 10.1093/sleep/zsac104
36. Mirchandaney, R, Asarnow, LD, and Kaplan, KA. Recent advances in sleep and depression. Curr Opin Psychiatry. (2023) 36:34–40. doi: 10.1097/YCO.0000000000000837
37. Du, Y, Wang, M, Wang, Y, Dou, Y, Yan, Y, Fan, H, et al. The association between dietary quality, sleep duration, and depression symptoms in the general population: findings from cross-sectional Nhanes study. BMC Public Health. (2024) 24:2588. doi: 10.1186/s12889-024-20093-9
38. Yasugaki, S, Okamura, H, Kaneko, A, and Hayashi, Y. Bidirectional relationship between sleep and depression. Neurosci Res. (2023) 211:57–64. doi: 10.1016/j.neures.2023.04.006
39. Franzen, PL, and Buysse, DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. (2008) 10:473–81. doi: 10.31887/DCNS.2008.10.4/plfranzen
40. Sukegawa, T, Itoga, M, Seno, H, Miura, S, Inagaki, T, Saito, W, et al. Sleep disturbances and depression in the elderly in Japan. Psychiatry Clin Neurosci. (2003) 57:265–70. doi: 10.1046/j.1440-1819.2003.01115.x
41. Duquenne, P, Capperella, J, Fezeu, LK, Srour, B, Benasi, G, Hercberg, S, et al. The association between ultra-processed food consumption and chronic insomnia in the Nutrinet-Santé study. J Acad Nutr Diet. (2024) 124:1109–17.e2. doi: 10.1016/j.jand.2024.02.015
42. Tang, S, Zhou, J, Liu, C, Wang, S, Cong, Y, Chen, L, et al. Association of Plant-Based Diet Index with sleep quality in middle-aged and older adults: the healthy dance study. Sleep Health. (2023) 9:698–703. doi: 10.1016/j.sleh.2023.04.003
43. Liu, J, Liu, Z, Zhou, Y, Wu, L, Wang, N, Liu, X, et al. The relationship between plant-based diet indices and sleep health in older adults: the mediating role of depressive symptoms and anxiety. Nutrients. (2024) 16:3386. doi: 10.3390/nu16193386
44. Data PUOR. (2024). Chinese longitudinal healthy longevity and happy family study (Clhls-Hf). Available online at: https://opendata.pku.edu.cn/dataset.xhtml?persistentId=doi:10.18170/DVN/WBO7LK (Accessed December 20, 2024).
45. Lv, Y, Zhang, Y, Li, X, Gao, X, Ren, Y, Deng, L, et al. Body mass index, waist circumference, and mortality in subjects older than 80 years: a Mendelian randomization study. Eur Heart J. (2024) 45:2145–54. doi: 10.1093/eurheartj/ehae206
46. Xi, D, Liu, L, Zhang, M, Huang, C, Burkart, KG, Ebi, K, et al. Risk factors associated with heatwave mortality in Chinese adults over 65 years. Nat Med. (2024) 30:1489–98. doi: 10.1038/s41591-024-02880-4
47. Gao, M, Kuang, W, Qiu, P, Wang, H, Lv, X, and Yang, M. The time trends of cognitive impairment incidence among older Chinese people in the community: based on the Clhls cohorts from 1998 to 2014. Age Ageing. (2017) 46:787–93. doi: 10.1093/ageing/afx038
48. Xiao, S, Shi, L, Zhang, J, Li, X, Lin, H, Xue, Y, et al. The role of anxiety and depressive symptoms in mediating the relationship between subjective sleep quality and cognitive function among older adults in China. J Affect Disord. (2023) 325:640–6. doi: 10.1016/j.jad.2023.01.048
49. Li, SH, Lloyd, AR, and Graham, BM. Subjective sleep quality and characteristics across the menstrual cycle in women with and without generalized anxiety disorder. J Psychosom Res. (2021) 148:110570. doi: 10.1016/j.jpsychores.2021.110570
50. Thompson, AS, Tresserra-Rimbau, A, Karavasiloglou, N, Jennings, A, Cantwell, M, Hill, C, et al. Association of Healthful Plant-Based Diet Adherence with risk of mortality and major chronic diseases among adults in the Uk. JAMA Netw Open. (2023) 6:e234714. doi: 10.1001/jamanetworkopen.2023.4714
51. Zhao, W, Hasegawa, K, and Chen, J. The use of food-frequency questionnaires for various purposes in China. Public Health Nutr. (2002) 5:829–33. doi: 10.1079/PHN2002374
52. Yin, Z, Fei, Z, Qiu, C, Brasher, MS, Kraus, VB, Zhao, W, et al. Dietary diversity and cognitive function among elderly people: a population-based study. J Nutr Health Aging. (2017) 21:1089–94. doi: 10.1007/s12603-017-0912-5
53. Chen, R, Chen, Q, Lu, G, Zhang, M, Zhang, M, Yang, H, et al. Sleep duration and depressive symptoms in Chinese middle-aged and older adults: the moderating effects of grip strength. J Affect Disord. (2023) 339:348–54. doi: 10.1016/j.jad.2023.07.059
54. Li, S, Jia, Z, Zhang, Z, Li, Y, Ding, Y, Qin, Z, et al. Effect of gender on the association between cumulative cardiovascular risk factors and depression: results from the us National Health and nutrition examination survey. Gen Psychiatr. (2023) 36:e101063. doi: 10.1136/gpsych-2023-101063
55. Wong, CW, Kwok, CS, Narain, A, Gulati, M, Mihalidou, AS, Wu, P, et al. Marital status and risk of cardiovascular diseases: a systematic review and Meta-analysis. Heart. (2018) 104:1937–48. doi: 10.1136/heartjnl-2018-313005
56. Effects of Education on Adult Mortality. A global systematic review and Meta-analysis. Lancet Public Health. (2024) 9:e155–65. doi: 10.1016/S2468-2667(23)00306-7
57. Bloomberg, M, Brocklebank, L, Hamer, M, and Steptoe, A. Joint associations of physical activity and sleep duration with cognitive ageing: longitudinal analysis of an English cohort study. Lancet Healthy Longev. (2023) 4:e345–53. doi: 10.1016/S2666-7568(23)00083-1
58. GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the global burden of disease study 2021. Lancet. (2024) 403:2100–32. doi: 10.1016/S0140-6736(24)00367-2
59. Vasmehjani, AA, Darabi, Z, Ghayour-Mobarhan, M, Ferns, GA, and Khayyatzadeh, SS. The associations between plant-based dietary indices with depression and quality of life and insomnia among Iranian adolescent girls in 2015. Sci Rep. (2024) 14:11683. doi: 10.1038/s41598-024-61952-0
60. Qi, R, Sheng, B, Zhou, L, Chen, Y, Sun, L, and Zhang, X. Association of Plant-Based Diet Indices and Abdominal Obesity with mental disorders among older Chinese adults. Nutrients. (2023) 15:2721. doi: 10.3390/nu15122721
61. Lee, MF, Eather, R, and Best, T. Plant-based dietary quality and depressive symptoms in Australian vegans and vegetarians: a cross-sectional study. BMJ Nutr Prev Health. (2021) 4:479–86. doi: 10.1136/bmjnph-2021-000332
62. Holscher, HD. Dietary Fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. (2017) 8:172–84. doi: 10.1080/19490976.2017.1290756
63. Cryan, JF, O'Riordan, KJ, Cowan, CSM, Sandhu, KV, Bastiaanssen, TFS, Boehme, M, et al. The microbiota-gut-brain Axis. Physiol Rev. (2019) 99:1877–2013. doi: 10.1152/physrev.00018.2018
64. Kalupahana, NS, Claycombe, KJ, and Moustaid-Moussa, N. (N-3) fatty acids alleviate adipose tissue inflammation and insulin resistance: mechanistic insights. Adv Nutr. (2011) 2:304–16. doi: 10.3945/an.111.000505
65. Maleki, SJ, Crespo, JF, and Cabanillas, B. Anti-inflammatory effects of flavonoids. Food Chem. (2019) 299:125124. doi: 10.1016/j.foodchem.2019.125124
66. Akiyama, H, Barger, S, Barnum, S, Bradt, B, Bauer, J, Cole, GM, et al. Inflammation and Alzheimer's disease. Neurobiol Aging. (2000) 21:383–421. doi: 10.1016/S0197-4580(00)00124-X
67. Wienecke, LM, Cohen, S, Bauersachs, J, Mebazaa, A, and Chousterman, BG. Immunity and inflammation: the neglected key players in congenital heart disease? Heart Fail Rev. (2022) 27:1957–71. doi: 10.1007/s10741-021-10187-6
68. Bartekova, M, Radosinska, J, Jelemensky, M, and Dhalla, NS. Role of cytokines and inflammation in heart function during health and disease. Heart Fail Rev. (2018) 23:733–58. doi: 10.1007/s10741-018-9716-x
69. Zhai, L, Zhang, H, and Zhang, D. Sleep duration and depression among adults: a Meta-analysis of prospective studies. Depress Anxiety. (2015) 32:664–70. doi: 10.1002/da.22386
70. Alvaro, PK, Roberts, RM, and Harris, JK. A systematic review assessing Bidirectionality between sleep disturbances, anxiety, and depression. Sleep. (2013) 36:1059–68. doi: 10.5665/sleep.2810
71. Bao, YP, Han, Y, Ma, J, Wang, RJ, Shi, L, Wang, TY, et al. Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neurosci Biobehav Rev. (2017) 75:257–73. doi: 10.1016/j.neubiorev.2017.01.032
72. Castrén, E. Neuronal network plasticity and recovery from depression. JAMA Psychiatry. (2013) 70:983–9. doi: 10.1001/jamapsychiatry.2013.1
73. Diekelmann, S, and Born, J. The memory function of sleep. Nat Rev Neurosci. (2010) 11:114–26. doi: 10.1038/nrn2762
74. Riemann, D, Spiegelhalder, K, Nissen, C, Hirscher, V, Baglioni, C, and Feige, B. Rem sleep instability--a new pathway for insomnia? Pharmacopsychiatry. (2012) 45:167–76. doi: 10.1055/s-0031-1299721
75. Feige, B, Al-Shajlawi, A, Nissen, C, Voderholzer, U, Hornyak, M, Spiegelhalder, K, et al. Does rem sleep contribute to subjective wake time in primary insomnia? A comparison of polysomnographic and subjective sleep in 100 patients. J Sleep Res. (2008) 17:180–90. doi: 10.1111/j.1365-2869.2008.00651.x
76. Sharma, V, Sharkey, KM, Palagini, L, Mazmanian, D, and Thomson, M. Preventing recurrence of postpartum depression by regulating sleep. Expert Rev Neurother. (2023) 23:1–9. doi: 10.1080/14737175.2023.2237194
77. Carney, CE, Edinger, JD, Kuchibhatla, M, Lachowski, AM, Bogouslavsky, O, Krystal, AD, et al. Cognitive behavioral insomnia therapy for those with insomnia and depression: a randomized controlled clinical trial. Sleep. (2017) 40:zsx019. doi: 10.1093/sleep/zsx019
78. Zuraikat, FM, Wood, RA, Barragán, R, and St-Onge, MP. Sleep and diet: mounting evidence of a cyclical relationship. Annu Rev Nutr. (2021) 41:309–32. doi: 10.1146/annurev-nutr-120420-021719
79. Pandi-Perumal, SR, Monti, JM, Burman, D, Karthikeyan, R, BaHammam, AS, Spence, DW, et al. Clarifying the role of sleep in depression: a narrative review. Psychiatry Res. (2020) 291:113239. doi: 10.1016/j.psychres.2020.113239
80. Hyde, JS. Gender Similarities and Differences. Annu Rev Psychol. (2014) 65:373–98. doi: 10.1146/annurev-psych-010213-115057
81. Weissman, MM, Bland, RC, Canino, GJ, Faravelli, C, Greenwald, S, Hwu, HG, et al. Cross-National Epidemiology of major depression and bipolar disorder. JAMA. (1996) 276:293–9. doi: 10.1001/jama.1996.03540040037030
Keywords: heart disease, depression, plant-based diets, cross-sectional study, sleep, older adults
Citation: Yu Y, Cheng Y, Cheng N, Zhang J, Xu Q, Wang Y, Zhou W, Yan C, Li H and Gong Z (2025) Association between plant-based diets and depression in older adults with heart disease: the mediating role of sleep disturbances. Front. Nutr. 12:1567436. doi: 10.3389/fnut.2025.1567436
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Raúl Sampieri-Cabrera, National Autonomous University of Mexico, MexicoShaojie Liu, Frist Affiliated Hospital of Xiamen University, China
Copyright © 2025 Yu, Cheng, Cheng, Zhang, Xu, Wang, Zhou, Yan, Li and Gong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiyun Gong, emhpeXVuZ29uZ2dAb3V0bG9vay5jb20=
 Yaqun Yu
Yaqun Yu Zhiyun Gong
Zhiyun Gong