Plant-based diet and risk of all-cause mortality: a systematic review and meta-analysis
A Commentary on
Plant-based diet and risk of all-cause mortality: a systematic review and meta-analysis
by Tan, J., Zhang, S., Jiang, Y., Li, J., and Yang, C. (2024). Front. Nutr. 11:1481363. doi: 10.3389/fnut.2024.1481363
Introduction
The recent article on plant-based diets and risk of all-cause mortality by Tan et al. (1) provides the basis to examine the effect of underestimating the real associations of mortality rates (regression dilution) due to changes in the values of the dietary variables with time after their determination at baseline. Changes in variables were demonstrated in 1999 using data from the Framingham Study in the US (2). Figure 1 in that article shows paired mean values for blood pressure and cholesterol for quintiles defined at baseline and remeasured every two years. The range for the first and fifth quintile for systolic blood pressure changed from 51 mmHg at baseline to 35 mmHg at 6 years, 27 mmHg at 16 years, and 18 mmHg at 26 years. Thus, health outcomes at longer follow-up periods will be based on values that gradually depart from baseline values.
Regression dilution has been demonstrated for various health outcomes with respect to serum 25-hydroxyviamin D [25(OH)D] concentrations. The most recent review shows the effect for stroke and major cardiovascular (CVD) events with respect to baseline serum 25(OH)D concentrations for follow-up periods of one–to–ten and one–to-eight years, respectively (3). This review also references earlier reviews for all-cause mortality rate, cancer incidence, incidence of Alzheimer's disease and dementia. The analyses generally show that the value of regression fit to the shortest follow-up period is about twice the size of the standard meta-analysis that does not take follow-up period into account.
Analysis
For the analysis mean follow-up periods were obtained from the data in Table 1 in Tan et al. (1). Values for the effect of plant-based diets were obtained from Figures 2–4 in Tan et al. (1). Data were analyzed using SigmaStat 4.0 (Grafiti, Palo Alto, CA, USA). The RR values for diet in the four-year follow-up study were based on a comparison of the 90th percentile with the 10th percentile of PDI (4). The hazard ratio values were converted to those for quintiles to align with the 7.8-year follow-up period study, which was based on the extreme quintiles.
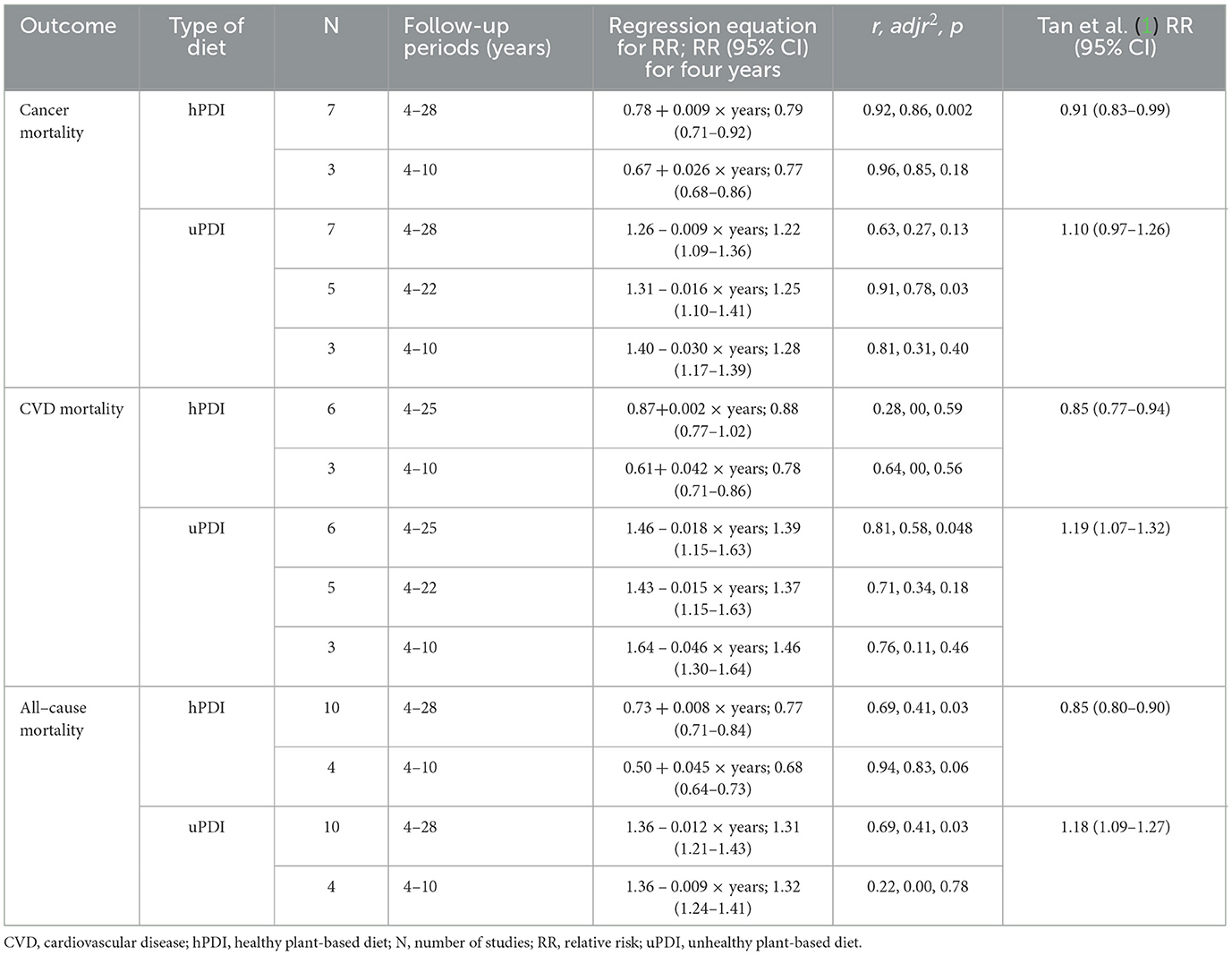
Table 1. Regression fits to the relative risks of healthy plant-based diets and unhealthy plant-based diets and cancer, CVD, and all-cause mortality rates based on data in Tan et al. (1).
Table 1 gives the equations for relative risk (RR), the statistical correlation results and p-values, and the RR values calculated by Tan et al. In the analyses, follow-up periods were used from four–to–ten to 28 years. Since follow-up periods longer than 10 years result in significant reductions in correlations between variables and health outcomes, different maximum follow-up periods were used in the analyses reported in Table 1.
The values of the regression fit for the shortest follow-up period, 4 years, is considered to be the most accurate correlation between the diet and the mortality rates. As can be seen, the difference from 1.00 for RRs for 4-year values for follow-up periods up to 25 years from 0.8 to 2.3 times as large as for Tan's RR; for 4-year values for follow-up periods <10 years from about 1.5 to 2.8 times as large as for Tan's RR. Also, that the regression fits to the data show that using the cutoff for the longest follow-up period at >20 years generally decreases the calculated RR for four years for hPDI. These findings are attributed to omitting studies where the “regression dilution” effect is greater. However, the p-value is mostly non-significant when fewer studies being used in the analysis.
The regression fits to the data for CVD are the least robust. This may be due to the fact that mortality from CVD often occurs after a number of years with CVD, resulting in various approaches to treatment.
Discussion
A recent Harvard analysis of diet and incidence of various diseases was published (5). The data for the analysis were obtained from 205,852 healthcare professionals from three US cohorts followed for up to 32 years. Participants completed food frequency questionnaires every 4 years. As shown in Table 2 of that article, the fully-adjusted associations between the 90th and 10th percentiles for the hPDI were 0.84 (95% CI, 0.82–0.87) for major chronic diseases; 0.85 (95% CI, 0.81–0.90) for major CVD; 0.78 (95% CI, 0.75–0.81) for type 2 diabetes mellitus; and 0.95 (95% CI, 0.91–0.99) for cancer. It is well known that vitamin D has a much larger effect on cancer mortality rates than on cancer incidence rates (6). Perhaps the same thing applies to diet as well.
Author contributions
WG: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The author has received grants for vitamin D research from Bio-Tech Pharmacal, Inc. (Fayetteville, AR, USA) for several years through the end of 2023.
Conflict of interest
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tan J, Zhang S, Jiang Y, Li J, Yang C. Plant-based diet and risk of all-cause mortality: a systematic review and meta-analysis. Front Nutr. (2024) 11:1481363. doi: 10.3389/fnut.2024.1481363
2. Clarke R, Shipley M, Lewington S, Youngman L, Collins R, Marmot M, et al. Underestimation of risk associations due to regression dilution in long-term follow-up of prospective studies. Am J Epidemiol. (1999) 150:341–53. doi: 10.1093/oxfordjournals.aje.a010013
3. Grant WB, Boucher BJ. How follow-up period in prospective cohort studies affects relationship between baseline serum 25(OH)D concentration and risk of stroke and major cardiovascular events. Nutrients. (2024) 16:3759. doi: 10.3390/nu16213759
4. Wang DD Li Y, Nguyen XT, Song RJ, Ho YL, Hu FB, et al. Degree of adherence to plant-based diet and total and cause-specific mortality: prospective cohort study in the Million Veteran Program. Public Health Nutr. (2023) 26:381–92. doi: 10.1017/S1368980022000659
5. Wang P, Song M, Eliassen AH, Wang M, Fung TT, Clinton SK, et al. Optimal dietary patterns for prevention of chronic disease. Nat Med. (2023) 29:719–28. doi: 10.1038/s41591-023-02235-5
Keywords: all-cause mortality, cancer mortality, cardiovascular mortality, cohort study, meta-analysis, follow-up period, healthy plant-based diet, unhealthy plant-based diet
Citation: Grant WB (2025) Commentary: Plant-based diet and risk of all-cause mortality: a systematic review and meta-analysis. Front. Nutr. 12:1529857. doi: 10.3389/fnut.2025.1529857
Received: 25 November 2024; Accepted: 17 January 2025;
Published: 31 January 2025.
Edited by:
Maria Rembiałkowska, Warsaw University of Life Sciences, PolandReviewed by:
Elli Polemiti, Charité University Medicine Berlin, GermanyCopyright © 2025 Grant. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: William B. Grant, d2JncmFudEBpbmZpb25saW5lLm5ldA==
†ORCID: William B. Grant orcid.org/0000-0002-1439-3285
 William B. Grant
William B. Grant