
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 04 February 2025
Sec. Nutritional Epidemiology
Volume 12 - 2025 | https://doi.org/10.3389/fnut.2025.1493253
Background: Oxidative stress plays a crucial role in the female reproductive system. The oxidative balance score (OBS) is a new measure for assessing the balance between antioxidant and pro-oxidative factors in diet and lifestyle. However, limited studies have explored the relationship between OBS and infertility.
Methods: We performed a cross-sectional study including 2,664 women aged 20–45 years, based on data from the 2013–2020 National Health and Nutrition Examination Survey (NHANES). The OBS was derived from 16 dietary components and 4 lifestyle factors. We used multivariate logistic regression analysis to examine the association between OBS and infertility.
Results: The analysis revealed a significant negative association between higher OBS and infertility risk, with an odds ratio (OR) of 0.98 (95% CI, 0.95–1.00) after full adjustment. Compared to the first quartile of OBS, the second, third, and fourth quartiles showed ORs of 0.71 (95% CI, 0.45–1.11), 0.79 (95% CI, 0.51–1.22), and 0.57 (95% CI, 0.35–0.92), respectively. Similarly, women in the highest dietary OBS and lifestyle OBS quartiles had a lower infertility risk compared to those in the lowest quartiles, with ORs of 0.60 (95% CI, 0.39–0.94) and 0.54 (95% CI, 0.32–0.93), respectively. Furthermore, subgroup analysis indicated that the association between the fourth quartile of OBS and infertility remained consistent, except among women with other ethnicities—including multi-racial, and college graduate or higher.
Conclusion: These findings suggest that high dietary OBS and lifestyle OBS are associated with a lower risk of infertility.

Graphical Abstract. This study included a total of 2,664 women aged 20–45 years from National Health and Nutrition Examination Survey (NHANES) 2013–2020. Oxidative balance score (OBS), derived from 16 dietary and 4 lifestyle components, was analyzed to assess its association with self-reported infertility using multivariate logistic regression. The results indicate a significant inverse relationship between OBS and infertility risk. Higher dietary and lifestyle OBS also correlated with reduced infertility risk. NHANES, National Health and Nutrition Examination Survey; OBS, Oxidative balance score.
The World Health Organization (WHO) defines infertility as the failure to achieve pregnancy after 1 year or more of regular, unprotected sexual intercourse (1). Recent studies report that approximately 15% of couples of reproductive age have infertility, with rates reaching up to 30% in certain regions, including sub-Saharan Africa and South Asia, North Africa, the Middle East, Central and Eastern Europe, and Central Asia (2, 3). The causes of infertility are complex and involve various prevalent conditions. Several common diseases may affect female infertility, including premature ovarian insufficiency (4), polycystic ovary syndrome (5), endometriosis (6, 7), tubal obstruction (8), and chronic inflammatory diseases (4). Apart from these common diseases, lifestyle factors can also significantly influence female fertility, either positively or negatively (9). Adverse lifestyle choices, such as malnutrition, excessive alcohol consumption, smoking, excessive exercise, stress, inadequate sleep, environmental pollution, and unhealthy sexual practices, have been shown to negatively impact women's reproductive health and fertility (10). Due to the multiple factors influencing female fertility and the unclear underlying mechanisms, approximately 15% of infertile couples are diagnosed with “unexplained infertility” (11). Numerous studies have indicated that reactive oxygen species (ROS) production might contribute to infertility. ROS may play a role in multiple infertility-related pathological processes, such as peritoneal issues, tubal dysfunction, endometriosis, and unexplained infertility (12).
Oxidative stress describes a state of imbalance between the generation of ROS and the body's antioxidant defense mechanisms (13). It plays a crucial role in reproductive systems, affecting oocyte maturation in females, embryonic development, and implantation (14). Various factors influence the oxidative stress state, including the consumption of oxidative or antioxidant-rich foods (15–17) and lifestyle factors such as alcohol consumption, smoking, obesity, and physical activity (18, 19). Therefore, to comprehensively investigate the impact of dietary and lifestyle changes on oxidative stress status, it is particularly important to propose a method capable of integrating and quantifying the balance between antioxidant and pro-oxidant components.
The oxidative balance score (OBS) is a novel measure to assess the balance between antioxidant and pro-oxidative components in dietary and lifestyle factors (20). In general, a higher OBS indicates a preference for antioxidants over pro-oxidants (21). Multiple epidemiological investigations have shown a negative relationship between OBS and the likelihood of various common diseases, including hypertension, diabetes, and erectile dysfunction (22–24). However, the relationship between OBS and female infertility has been directly examined in only a limited number of studies.
Therefore, our study aims to explore the relationship between OBS and female infertility through a cross-sectional analysis of data from the National Health and Nutrition Examination Survey (NHANES) collected between 2013 and 2020. The OBS incorporated both lifestyle and dietary components. We hypothesized that higher OBS is associated with lower risk of female infertility, with the goal of providing new insights into the role of nutrition and lifestyle in female infertility and contributing to a broader understanding of how dietary and lifestyle factors influence reproductive health.
Participants were selected from the NHANES, a stratified, multi-stage cluster probability sampling survey conducted during 2013–2020. The NHANES program provides a sample that represents the national population, and the data can be freely accessed on their official website (https://www.cdc.gov/nchs/nhanes/index.htm). NHANES studies are conducted every 2 years to assess the health and nutritional status of participants. All NHANES studies involving human participants are approved by the National Center for Health Statistics Ethics Review Board, and informed consent is obtained from all participants.
Ultimately, 12,403 participants aged 12 years and above qualified to participate in the reproductive health questionnaire. However, our study exclusively included those between 20 and 45 years (n = 4,413) (25, 26). Participants were excluded from the final analysis based on the following criteria: (1) missing data in infertility information and OBS components (N = 1,174); (2) missing data in covariates (N = 441): including poverty income ratio (PIR), educational level, hypertension, diabetes, age at first menstrual period, and pelvic inflammatory disease (PID) and (3) participants who had tumors and implausible energy intakes (below 800 kcal/d or over 4,200 kcal/d) (N = 152). Ultimately, we selected 2,664 female participants in the final analysis (Figure 1).
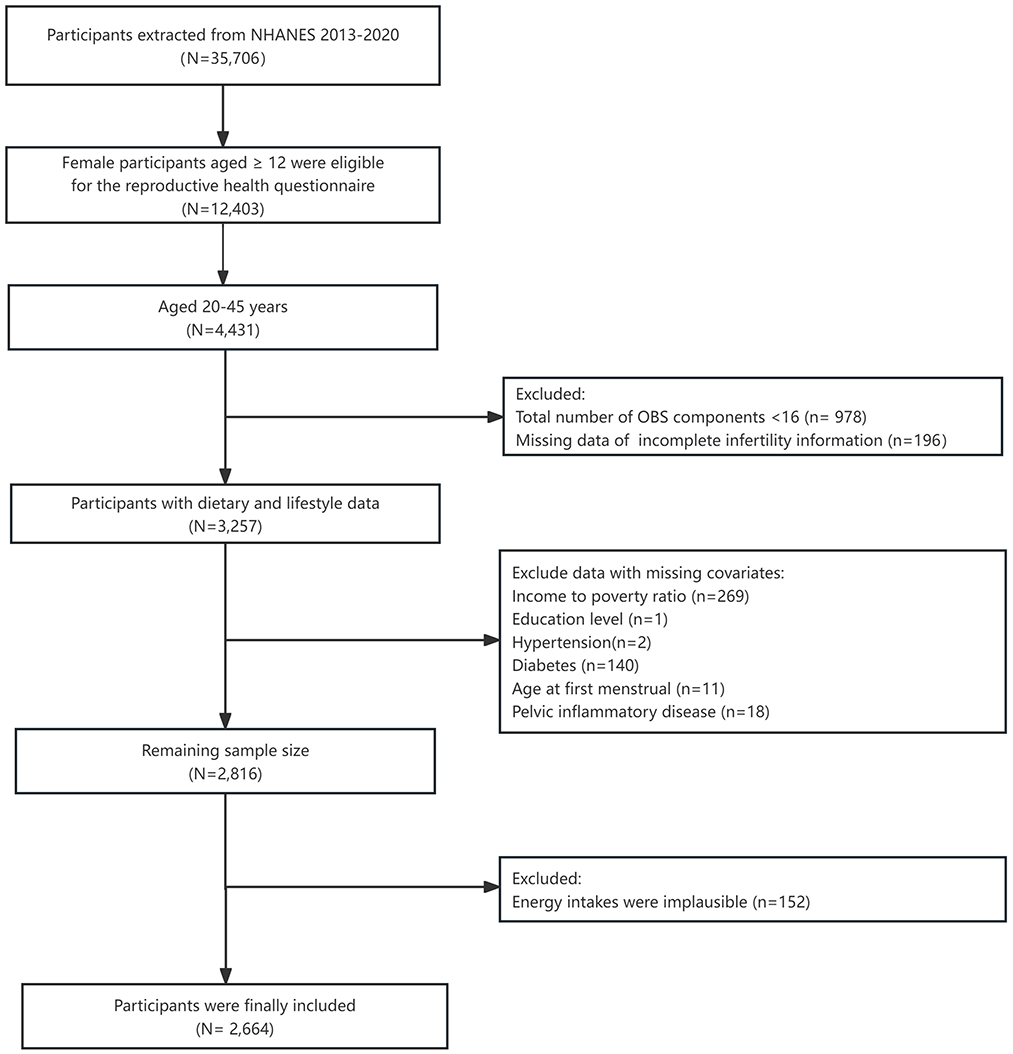
Figure 1. Flow chart of the study participants. NHANES, National Health and Nutrition Examination Survey.
The OBS was calculated by integrating 16 dietary components and 4 lifestyle factors, including 5 pro-oxidants and 15 antioxidants factors (27). Dietary OBS, including total folate, carotene, vitamins B6, B12, C, and E, niacin, riboflavin, dietary fiber, calcium, magnesium, zinc, copper, selenium, iron, and total fat, was obtained from two 24-hour dietary interviews. Antioxidants (such as vitamins and minerals) were scored based on tertiles 1 to 3, with scores of 0, 1, and 2, respectively. Conversely, pro-oxidants (iron and total fat) were scored in reverse order, with higher values receiving lower scores (28) (Supplementary Table S1). The lifestyle OBS incorporated four components: body mass index (BMI), cotinine, physical activity, and alcohol intake. Serum cotinine concentrations were measured to assess smoking exposure, covering both active smoking and second-hand smoke exposure (29). Physical activity in total was measured by applying the metabolic equivalent of task (MET) (30), derived from the total weekly duration of transportation, moderate, and intense activities. BMI, cotinine, and physical activity were scored based on tertiles 1 to 3, with scores of 0, 1, and 2 assigned, respectively. Alcohol intake is scored as 2, 1, and 0 points for non-drinkers (0 to 15 g/d), moderate drinkers, and heavy drinkers (≥15 g/d), respectively (28) (Supplementary Table S1). The total OBS is calculated by summing the scores of all components. An elevated OBS reflects a stronger antioxidant effect. Participants in this study were required to have a minimum of 16 out of the 20 OBS components (31).
Infertility was evaluated using two questions from the self-reported health survey (32): (1) RHQ074: “Have you ever attempted to conceive for a period of at least 1 year without success?” and (2) RHQ076: “Have you ever sought medical advice or consulted a healthcare professional because you were unable to conceive?” Women who answered “yes” to either of these questions were classified as having a history of infertility.
According to clinical practice and previous studies (32–34), our study used age (< 35, ≥35), race (including Mexican–American, other Hispanic, Non-Hispanic Black, Non-Hispanic White, and other Race—including Multi-Racial), marital status (Never married, Divorced/Separated/Widowed, and Married/Living with partner), education level (High school/GED/ < 11th grade, Some college or AA degree, and College graduate or above), income-to-poverty ratio (PIR), hypertension, diabetes, hyperlipidemia, pelvic inflammatory disease (PID), and age of menarche as covariates. The family PIR scale, ranging from 0 to 5, is divided into three categories. PID was determined through self-reported responses to questions from the reproductive health questionnaire, specifically: “Have you ever been treated for pelvic inflammatory disease/PID?” Age of menarche was divided into two categories: under 15 years and 15 years or older.
All analyses were conducted based on the principle of complex multi-stage stratified sampling. Individual sample weight was computed by dividing the number of survey cycle years by the total number of survey cycle years and multiplying by the 2-day dietary sample weight (WTDR2D), following the recommended weight method in NHANES guidelines. Categorical variables were expressed as frequencies and percentages, while continuous variables were represented by means and standard deviations (SD). The Pearson chi-square test was used to analyze the differences in categorical variables between infertile and non-infertile female. Multivariate logistic regression was performed with different models to explore the association between OBS and infertility. Model 1 was a crude model. Model 2 was adjusted for age, race, education level, and marital status, and income-to-poverty ratio (PIR). To further exclude the effects of diabetes, hypertension, and hyperlipidemia, Model 3 was adjusted for Model 2 + diabetes, hypertension, and hyperlipidemia. Model 4 was adjusted for Model 3 + PID, and age of menarche. The OBS was also converted to a categorical variable, as well as being analyzed as a continuous variable.
Finally, sensitivity analyses were conducted to (1) explore the independent relationships between dietary OBS, lifestyle OBS, and infertility and (2) perform subgroup analyses stratified by factors such as race, pelvic inflammatory disease, and the diagnoses of hypertension, hyperlipidemia, and diabetes. The results of the interaction are presented as P-values. Data management and analyses were conducted using R version 4.1.2 (http://www.R-project.org). A two-tailed P-value of < 0.05 was regarded as statistically significant.
A total of 2664 women aged 20–45 years were included in this study, of whom 13.96% (372/2,664) had infertility. Table 1 lists the baseline characteristics of the study participants. The average mean (SD) BMI of infertile and non-infertile women was 31.98 (0.73) and 28.92(0.32) kg/m2, respectively, and the mean (SD) age was 34.96 (0.56) and 32.24 (0.24) years, respectively. Women with infertility were generally older and showed a greater prevalence of obesity compared to non-infertile women (P < 0.05). Women without infertility had a lower proportion of being married or living with a partner compared to those with infertility (57.36% vs. 72.86%, P < 0.001). Infertile women exhibited a higher prevalence of PID history compared to non-infertile women (P < 0.05). There were no significant differences between the two groups in terms of race, PIR, education level, and age at first menstrual period.
Table 2 demonstrates a negative association between OBS and infertility, and this relationship remains stable across various models. The OR of OBS for infertility was 0.98 (95% CI, 0.95–1.00) in the crude model. The results were robust in Model 2 (adjusting for age, race, marital status, education level, and PIR), Model 3 (adjusting for age, race, marital status, education level, PIR, hypertension, hyperlipidemia, and diabetes), and fully adjusted Model 4 (adjusting for age, race, marital status, PIR, hypertension, hyperlipidemia, diabetes, PID, and age of menarche), with ORs of 0.97 (95% CI, 0.95–1.00), 0.98 (95% CI, 0.95–1.00), and 0.98 (95% CI, 0.95–1.00), respectively. Then, we categorized OBS into quartiles to examine the possible relationship between OBS and infertility. Following full adjustment, the ORs for OBS levels in quartiles two, three, and four were 0.71 (95% CI, 0.45–1.11), 0.79 (95% CI, 0.51–1.22), and 0.57 (95% CI, 0.35–0.92), respectively, compared to the first quartile as the reference (p for trend = 0.04).
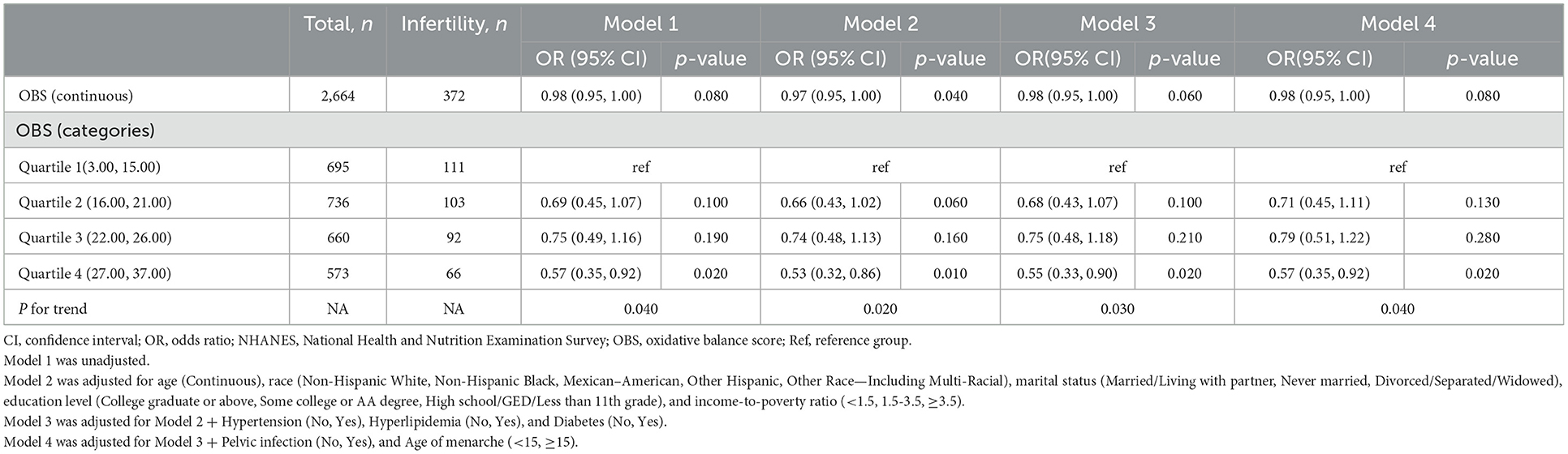
Table 2. Association between OBS and the risk of infertility in U.S. women aged 20–45 years from 2013 to 2020 NHANES, weighted.
An inverse association between dietary and lifestyle OBS and infertility is indicated in Table 3, and this relationship remains consistent across different models. In the crude model (Model 1), continuous lifestyle OBS demonstrated a significant negative association with female infertility, with an OR of 0.86 (95% CI: 0.78–0.94). In Models 3 and 4, the results were stable, with an OR of 0.88 (95% CI: 0.88–0.96) and 0.89 (95% CI: 0.81–0.97). Moreover, when dietary OBS and lifestyle OBS were categorized based on quartiles, the negative association with female infertility was found to be stronger for the highest quartile (Q4) of dietary OBS and lifestyle OBS compared to the lowest quartile (Q1). In dietary OBS Model 4, the OR for Q4 was 0.60 (95% CI: 0.39–0.94), while the ORs for infertility in Q2 and Q3 were 0.62 (95% CI: 0.40–1.95) and 0.97 (95% CI: 0.65–1.45), respectively (p for trend = 0.119). In lifestyle OBS Model 4, Q4 had an OR of 0.54 (95% CI: 0.32–0.93), while Q2 and Q3 had an OR of 1.05 (95% CI: 0.70–1.59) and 0.69 (95% CI: 0.44–1.09), respectively (p for trend = 0.009).
To confirm the stability of the association between OBS and infertility across different subgroups, we conducted subgroup analyses and interaction tests (Table 4). The findings indicated that the association between the fourth quartile of OBS and infertility remained generally stable across different subgroups, including age, race, marital status, education level, PIR, hyperlipidemia, diabetes, hypertension, PID, and age of menarche. In addition, the association between OBS and infertility was not influenced by the interactions across various subgroups (P-values for interaction > 0.05).
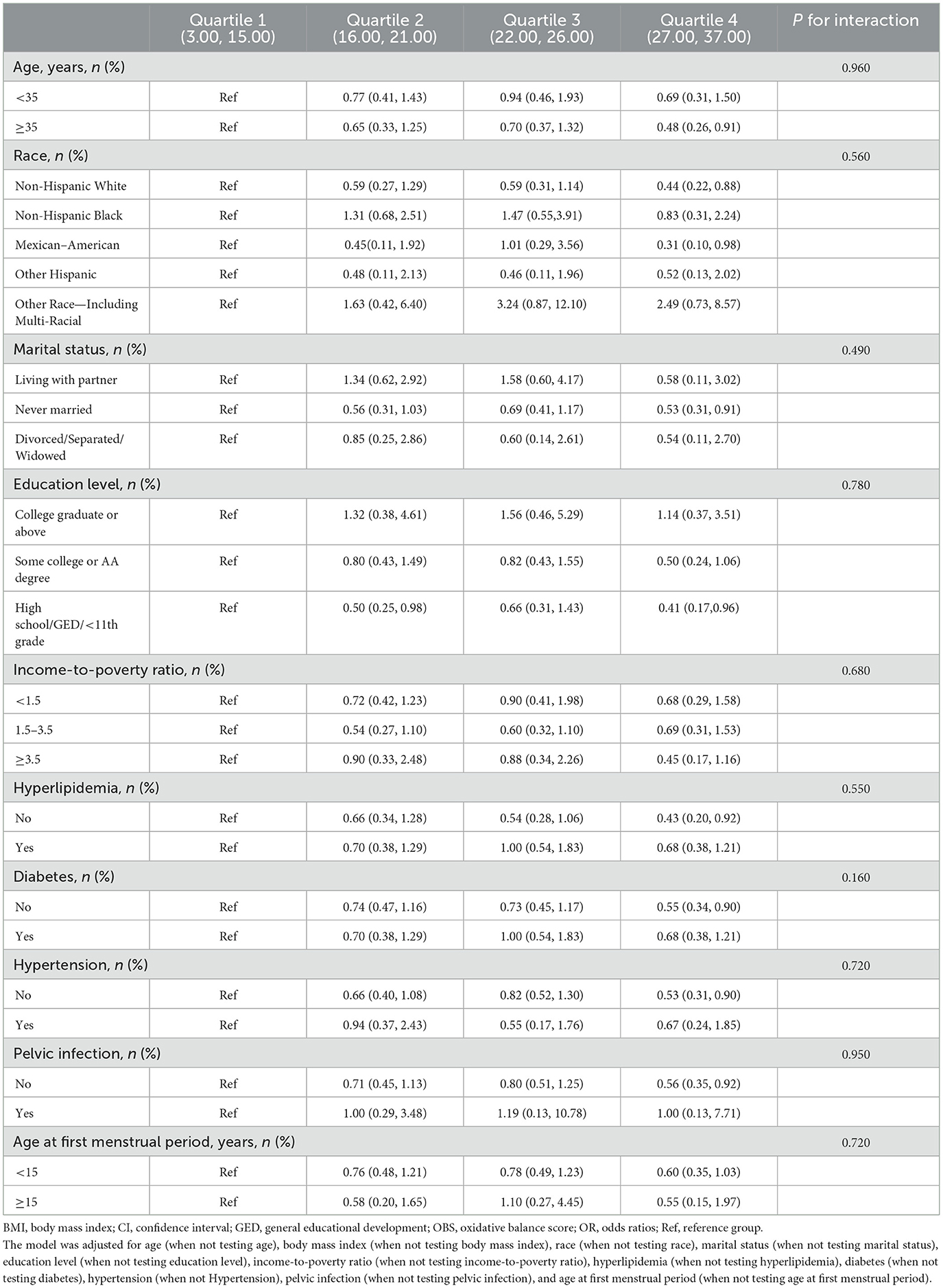
Table 4. Subgroup analyses of the association between OBS and infertility from 2013 to 2020 NHANES according to quartile of OBS.
In this nationally representative cross-sectional survey based on NHANES, a notable negative correlation was observed between OBS and female infertility. The higher total OBS was associated with a lower incidence of female infertility, with substantial trends across OBS quartiles. This negative association persisted even after adjusting for various covariates, indicating a 43% decrease in the odds of infertility from the first to the fourth quartile of OBS. Furthermore, in comparison with the lowest quartile, the highest quartiles of dietary OBS and lifestyle OBS were significantly associated with a lower risk of infertility. For dietary OBS, every single-unit increase was associated with an 11% reduction in infertility rates after full adjustment. Notably, lifestyle OBS demonstrated a more pronounced effect; every single-unit increase in lifestyle OBS corresponded to a 46% reduction in infertility rates after full adjustment.
OBS consists of 20 components, namely, total folate, carotene, vitamins (B6, B12, C, and E), niacin, riboflavin, dietary fiber, calcium, magnesium, iron, zinc, copper, selenium, total fat, BMI, smoking, alcohol intake, and physical activity, many of which have been shown to be closely associated with female infertility in previous studies. A cohort study of 2,370 women in the US population revealed a significant negative correlation between dietary fiber intake and female infertility (OR: 0.643, 95% CI: 0.480–0.861) (35). A randomized controlled trial called The Fast Track and Standard Treatment (FASTT) showed that higher intakes of antioxidants, including β-carotene, vitamin C, and vitamin E, were associated with a shorter time to conception among a cohort of couples being treated for unexplained infertility (36). Similarly based on a cohort of 18,555 married women, the Nurses' Health Study (37) included total intakes of each nutrient such as folic acid, various vitamins, iron, zinc, niacin, pantothenate, and retinol in the multivariable adjustment model to examine whether the inclusion of individual nutrients would attenuate the relationship between multivitamin use and infertility. The results showed that, after multivariable adjustment, the RR and 95% CI for infertility among women consuming more than six nutrients per week were 0.59 (95% CI: 0.46–0.75; P < 0.001), and the relationship between multivitamin use and infertility remained robust even after adjusting for individual nutrients such as iron, vitamin D, and folic acid. Furthermore, Dimitrios (38) indicated that calcium and vitamin D intake suppresses parathyroid hormone production, potentially improving hyperandrogenemia and anovulation associated with polycystic ovary syndrome (PCOS), thereby enhancing the chances of conception. In addition, a study conducted in a gynecology hospital in Nigeria involving 90 participants also found significantly lower levels of zinc (Zn) and magnesium (Mg) (P < 0.05) and significantly higher selenium (Se) levels (P < 0.05) in women with infertility compared to controls (39). Based on our findings, the quartile analysis of dietary OBS shows that higher quartiles of dietary OBS are significantly associated with a reduced risk of infertility compared to the lowest quartile (e.g., the OR for the fourth quartile is 0.60, 95% CI: 0.39–0.94, P = 0.030), further supporting the potential link between diet and reproductive health. These results suggest that improving diet quality, such as increasing the intake of antioxidants, dietary fiber, and key micronutrients, could guide public health interventions to reduce the incidence of infertility.
In addition to dietary factors, lifestyle is also associated with infertility. A descriptive cross-sectional study (40) involving 216 couples found significant differences in physical activity levels between infertile and fertile women (73.1% vs. 86.1%, respectively; p = 0.03). A systematic review of 98,657 women reported a combined relative risk (RR) of 0.87 (95% CI: 0.78–0.95) for fecundability among alcohol consumers compared to non-drinkers (41). Similarly, Goldman (42) found an increase in infertility, due to ovulatory factor or endometriosis, with alcohol use. Specifically, compared to non-drinkers, the OR for ovulatory infertility was 1.3 (95% CI: 1.0–1.7) in moderate drinkers and 1.6 (95% CI: 1.1–2.3) in heavy drinkers. BMI has also been shown to influence infertility. Grodstein (43) reported that, compared to women with lower BMI (20–24.9), obese women (BMI ≥27) had a relative risk (RR) of 3.1 (95% CI: 2.2–4.4) for ovulatory infertility. Moreover, the risk of ovulatory infertility was slightly elevated in moderately overweight women (BMI 25–26.9) and underweight women (BMI < 17), with RRs of 1.2 (95% CI: 0.8–1.9) and 1.6 (95% CI: 0.7–3.9), respectively. In addition, a controlled clinical study identified a significant correlation between smoking and female fertility, demonstrating markedly higher cotinine levels in follicular fluid among active smokers (710.4 ± 128.2 ng/mL) compared to passive smokers (76.3 ± 56.5 ng/mL) and non-smokers (4.2 ± 2.0 ng/mL), highlighting the detrimental impact of smoking on female fertility (44). Based on our findings, the quartile analysis of lifestyle OBS shows that higher quartiles of lifestyle OBS are significantly associated with a reduced risk of infertility compared to the lowest quartile (e.g., the OR for the fourth quartile is 0.54, 95% CI: 0.32–0.93, P = 0.030). This result further supports the importance of lifestyle factors, such as physical activity, BMI control, limiting alcohol consumption, and smoking cessation, in reproductive health. These findings suggest that improving lifestyle factors could provide effective public health interventions to reduce the incidence of infertility, particularly among high-risk populations.
Our findings suggest that infertility risk is associated with the combined oxidative and antioxidant profiles of multiple components. Compared to individual factors, OBS, as a composite index that includes both pro-oxidants and antioxidants, gives a more comprehensive reflection of the combined impact of diet and lifestyle on oxidative stress (45, 46). Therefore, the OBS is used as a comprehensive measure of exposure related to oxidative stress. Previous studies have shown that high OBS is associated with many other reproductive-related diseases. For example, a cross-sectional survey of the U.S. population indicated that elevated OBS was linked to a reduced prevalence of endometriosis, especially in women with irregular menstrual cycles and those taking female hormone supplements (47). Therefore, it is important to assess the relationship between oxidative balance and female infertility with composite indicators. These findings highlight the potential for using OBS as a framework for developing public health interventions or policies aimed at reducing infertility risk by promoting dietary and lifestyle improvements to maintain optimal oxidative balance.
Our study has several advantages. To the best of our knowledge, compared to previous studies that only focused on the effect of single dietary nutrient intake on female infertility, this study uses a more comprehensive dietary antioxidant capacity measurement method to evaluate the contribution of multiple dietary antioxidants to female infertility (31, 48). Moreover, compared to other dietary antioxidant composite indicators, this indicator includes a greater number of comprehensive factors and reasonably incorporates lifestyle factors (49, 50). Subgroup analysis and interaction tests were further performed on potential confounders such as age, race, marital status, education level, PIR, hypertension, diabetes, hyperlipidemia, PID, and age at menarche to confirm the robustness of the study results. This study included a nationally representative large sample that is reflective of the national population. The results can be extrapolated to the female infertility population nationwide, providing evidence-based dietary and lifestyle recommendations for female infertility management.
This study has several limitations. First, infertility has multifactorial causes, and we were unable to identify which specific type of infertility is most affected by the OBS. Future research should focus more on exploring the relationship between OBS and different types of infertility. Second, the cross-sectional design of the data limits the ability to establish a causal relationship between OBS and infertility, and only a correlation can be obtained. Third, the role of endogenous factors within the oxidative stress pathway requires further investigation. The absence of direct oxidative stress biomarkers in this study restricts the ability to validate the effectiveness of OBS and limits our understanding of the mechanisms underlying these observations. Fourth, the diagnosis of infertility was solely based on questionnaire data, without incorporating more specific clinical symptoms, which may lead to potential biases in the inclusion of study participants. Finally, our study primarily focused on European and American populations, which could limit the applicability of our results to other ethnic groups. Therefore, future research with larger and more ethnically diverse samples is essential to confirm our findings across various populations. Despite these limitations, our study preliminarily confirms the significant role of OBS in infertility, highlighting the importance of the synergistic effects of multiple factors. These findings offer valuable insights and serve as a foundation for guiding future research directions.
Our findings suggest that high dietary OBS and lifestyle OBS are associated with a lower risk of infertility. These findings support the idea that improving diet and lifestyle factors in a comprehensive manner can reduce the risk of female infertility, particularly through increased dietary antioxidant intake and optimizing lifestyle factors such as smoking cessation, weight management, and regular physical activity to enhance reproductive health.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: https://www.cdc.gov/nchs/nhanes/index.htm.
The studies involving humans were approved by National Center for Health Statistics Research Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
MM: Writing – original draft, Data curation, Formal analysis, Writing – review & editing. HX: Conceptualization, Data curation, Writing – original draft. KW: Methodology, Writing – original draft. YC: Conceptualization, Software, Writing – original draft. TP: Data curation, Writing – review & editing. QZ: Formal analysis, Funding acquisition, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by Scientific Research Project of Guangdong Provincial Bureau of Traditional Chinese Medicine (No. 20241308), Guangdong Basic and Applied Basic Research Foundation (No. 2022A1515220178), Guangdong TCM Antiaging Engineering Technology Research Center (No. 2022E040), Guangdong Famous Traditional Chinese Medicine Inheritance Studio Construction Program, Foshan Antiaging Engineering Technology Research Center, and Foshan Traditional Chinese Medicine Clinical Science and Technology Innovation Base Construction Program. The funders of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
We extend our gratitude to NHANES for making the data publicly accessible.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1493253/full#supplementary-material
1. World Health Organization. Infertility Prevalence Estimates: 1990–2021. Available at: https://www.who.int/publications/i/item/978920068315 (accessed April 3, 2023).
2. Van Der Kelen A, Okutman Ö, Javey E, Serdarogullari M, Janssens C, Ghosh MS, et al. A systematic review and evidence assessment of monogenic gene-disease relationships in human female infertility and differences in sex development. Hum Reprod Update. (2023) 29:218–32. doi: 10.1093/humupd/dmac044
3. Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. (2012) 9:e1001356. doi: 10.1371/journal.pmed.1001356
4. Hart RJ. Physiological aspects of female fertility: role of the environment, modern lifestyle, and genetics. Physiol Rev. (2016) 96:873–909. doi: 10.1152/physrev.00023.2015
5. Stener-Victorin E, Teede H, Norman RJ, Legro R, Goodarzi MO, Dokras A, et al. Polycystic ovary syndrome. Nature reviews Disease primers. (2024) 10:27. doi: 10.1038/s41572-024-00511-3
6. Tanbo T, Fedorcsak P. Endometriosis-associated infertility: aspects of pathophysiological mechanisms and treatment options. Acta Obstet Gynecol Scand. (2017) 96:659–67. doi: 10.1111/aogs.13082
7. Barnhart K, Dunsmoor-Su R, Coutifaris C. Effect of endometriosis on in vitro fertilization. Fertil Steril. (2002) 77:1148–55. doi: 10.1016/S0015-0282(02)03112-6
8. El-Kharoubi AF, Szasz F. Tubal blockage surgery: a retrospective cohort study on clinical characteristics and reproductive outcomes within six years. Cureus. (2023) 15:e39879. doi: 10.7759/cureus.39879
9. Skoracka K, Eder P, Łykowska-Szuber L, Dobrowolska A, Krela-Kazmierczak I. Diet and nutritional factors in male (in)fertility-underestimated factors. J Clini Med. (2020) 9:1400. doi: 10.3390/jcm9051400
10. Ferramosca A, Zara V. Diet and male fertility: the impact of nutrients and antioxidants on sperm energetic metabolism. Int J Mol Sci. (2022) 23:2542. doi: 10.3390/ijms23052542
11. Carson SA, Kallen AN. Diagnosis and management of infertility: a review. JAMA. (2021) 326:65–76. doi: 10.1001/jama.2021.4788
12. Anton C, Ciobica A, Doroftei B, Maftei R, Ilea C, Darii Plopa N, et al. A review of the complex relationship between irritable bowel syndrome and infertility. Medicina. (2020) 56:592. doi: 10.3390/medicina56110592
13. Palomba S, Daolio J, Romeo S, Battaglia FA, Marci R, La Sala GB. Lifestyle and fertility: the influence of stress and quality of life on female fertility. Reprod Biol Endocrinol. (2018) 16:113. doi: 10.1186/s12958-018-0434-y
14. Qi L, Li Y, Zhang L, Li S, Zhang X, Li W, et al. Immune and oxidative stress disorder in ovulation-dysfunction women revealed by single-cell transcriptome. Front Immunol. (2023) 14:1297484. doi: 10.3389/fimmu.2023.1297484
15. Agarwal A, Gupta S, Sharma RK. Role of oxidative stress in female reproduction. Reprod Biol Endocrinol. (2005) 3:28. doi: 10.1186/1477-7827-3-28
16. Fang YZ, Yang S, Wu G. Free radicals, antioxidants, and nutrition. Nutrition. (2002) 18:872–9. doi: 10.1016/S0899-9007(02)00916-4
17. Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. (2006) 160:1–40. doi: 10.1016/j.cbi.2005.12.009
18. Albano E. Alcohol, oxidative stress and free radical damage. Proc Nutr Soc. (2006) 65:278–90. doi: 10.1079/PNS2006496
19. Barreiro E, Peinado VI, Galdiz JB, Ferrer E, Marin-Corral J, Sánchez F, et al. Cigarette smoke-induced oxidative stress: a role in chronic obstructive pulmonary disease skeletal muscle dysfunction. Am J Respir Crit Care Med. (2010) 182:477–88. doi: 10.1164/rccm.200908-1220OC
20. Jakubiak GK, Osadnik K, Lejawa M, Kasperczyk S, Osadnik T, Pawlas N. Oxidative stress in association with metabolic health and obesity in young adults. Oxid Med Cell Longev. (2021) 2021:9987352. doi: 10.1155/2021/9987352
21. Xu Z, Xue Y, Wen H, Chen C. Association of oxidative balance score and lung health from the national health and nutrition examination survey 2007-2012. Front Nutrit. (2022) 9:961950. doi: 10.3389/fnut.2022.961950
22. Hernández-Ruiz Á, García-Villanova B, Guerra-Hernández EJ, Carrión-García CJ, Amiano P, Sánchez MJ, et al. Oxidative balance scores (Obss) integrating nutrient, food and lifestyle dimensions: development of the nutrientl-Obs and foodl-Obs. Antioxidants. (2022) 11:300. doi: 10.3390/antiox11020300
23. Lee JH, Son DH, Kwon YJ. Association between oxidative balance score and new-onset hypertension in adults: a community-based prospective cohort study. Front Nutr. (2022) 9:1066159. doi: 10.3389/fnut.2022.1066159
24. Demirer B, Yardimci H, Erem Basmaz S. Inflammation level in type 2 diabetes is associated with dietary advanced glycation end products, mediterranean diet adherence and oxidative balance score: a pathway analysis. J Diabetes Complicat. (2023) 37:108354. doi: 10.1016/j.jdiacomp.2022.108354
25. Dong M, Xu X, Li Y, Wang Y, Jin Z, Tan J. Impact of infertility duration on female sexual health. Reprod Biol Endocrinol. (2021) 19:157. doi: 10.1186/s12958-021-00837-7
26. Tang J, Xu Y, Wang Z, Ji X, Qiu Q, Mai Z, et al. Association between metabolic healthy obesity and female infertility: the national health and nutrition examination survey, 2013-2020. BMC Public Health. (2023) 23:1524. doi: 10.1186/s12889-023-16397-x
27. Wang L, Huang S, Feng Z, Xiao J, Luo G, Zhang Y. Assessing the role of antioxidant and pro-oxidant balance in mediating the relationship between vitamin K intake and depressive symptoms in adults. Front Nutr. (2024) 11:1384489. doi: 10.3389/fnut.2024.1384489
28. Zhang W, Peng SF, Chen L, Chen HM, Cheng XE, Tang YH. Association between the oxidative balance score and telomere length from the national health and nutrition examination survey 1999-2002. Oxid Med Cell Longev. (2022) 2022:1345071. doi: 10.1155/2022/1345071
29. Tsai J, Homa DM, Neff LJ, Sosnoff CS, Wang L, Blount BC, et al. Trends in secondhand smoke exposure, 2011-2018: impact and implications of expanding serum cotinine range. Am J Prev Med. (2021) 61:e109–e17. doi: 10.1016/j.amepre.2021.04.004
30. Wang Y, Li J, Sun W, Tong Y, Han L, Jiang Z, et al. Associations between the oxidative balance score and constipation: a cross-sectional study of the NHANES, 2005-2010. BMC Public Health. (2024) 24:1908. doi: 10.1186/s12889-024-19428-3
31. Liu F, You F, Yang L, Du X, Li C, Chen G, et al. Nonlinear relationship between oxidative balance score and hyperuricemia: analyses of NHANES 2007-2018. Nutr J. (2024) 23:48. doi: 10.1186/s12937-024-00953-1
32. Xu H, Wen Q, Xing X, Chen Y, Zhu Q, Tan M, et al. High dietary inflammatory index increases the risk of female infertility: an analysis of NHANES 2013-2018. Nutrition research (New York, NY). (2024) 125:50–60. doi: 10.1016/j.nutres.2024.02.006
33. Lyra P, Botelho J, Machado V, Rota S, Walker R, Staunton J, et al. Self-reported periodontitis and C-reactive protein in parkinson's disease: a cross-sectional study of two american cohorts. NPJ Parkinson's Dis. (2022) 8:40. doi: 10.1038/s41531-022-00302-1
34. Chen Z, Wu Z, Zhang Y. Association between dietary magnesium intake and pelvic inflammatory disease in US women: a cross-sectional study of NHANES. Front Nutr. (2024) 11:1430730. doi: 10.3389/fnut.2024.1430730
35. Cai Q, Chen T. Association between dietary fiber and female fertility: a NHANES-based study. Reprod Sci. (2023) 30:1555–64. doi: 10.1007/s43032-022-01103-w
36. Ruder EH, Hartman TJ, Reindollar RH, Goldman MB. Female dietary antioxidant intake and time to pregnancy among couples treated for unexplained infertility. Fertil Steril. (2014) 101:759–66. doi: 10.1016/j.fertnstert.2013.11.008
37. Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Use of multivitamins, intake of B vitamins, and risk of ovulatory infertility. Fertil Steril. (2008) 89:668–76. doi: 10.1016/j.fertnstert.2007.03.089
38. Farmakiotis D, Katsikis I, Panidis D. Calcium homeostasis and anovulatory infertility. Hum Reprod. (2007) 22:3264. doi: 10.1093/humrep/dem330
39. Oluboyo A. Evaluation of selected trace elements and glutathione peroxidase levels in female infertility. J Obstet Gynecol Cancer Res. (2022) 7:374–81. doi: 10.30699/jogcr.7.5.374
40. Khosrorad T, Dolatian M, Riazi H, Mahmoodi Z, Alavimajd H, Shahsavari S, et al. Comparison of lifestyle in fertile and infertile couples in kermanshah during 2013. Iranian J Reprod Med. (2015) 13:549–56.
41. Fan D, Liu L, Xia Q, Wang W, Wu S, Tian G, et al. Female alcohol consumption and fecundability: a systematic review and dose-response meta-analysis. Sci Rep. (2017) 7:13815. doi: 10.1038/s41598-017-14261-8
42. Grodstein F, Goldman MB, Cramer DW. Infertility in women and moderate alcohol use. Am J Public Health. (1994) 84:1429–32. doi: 10.2105/AJPH.84.9.1429
43. Grodstein F, Goldman MB, Cramer DW. Body mass index and ovulatory infertility. Epidemiology. (1994) 5:247–50. doi: 10.1097/00001648-199403000-00016
44. Phipps WR, Cramer DW, Schiff I, Belisle S, Stillman R, Albrecht B, et al. The association between smoking and female infertility as influenced by cause of the infertility. Fertil Steril. (1987) 48:377–82. doi: 10.1016/S0015-0282(16)59402-3
45. Lakkur S, Judd S, Bostick RM, McClellan W, Flanders WD, Stevens VL, et al. Oxidative stress, inflammation, and markers of cardiovascular health. Atherosclerosis. (2015) 243:38–43. doi: 10.1016/j.atherosclerosis.2015.08.032
46. Wen H, Li X, Chen J, Li Y, Yang N, Tan N. Association of oxidative balance score with chronic kidney disease: NHANES 1999-2018. Front Endocrinol. (2024) 15:1396465. doi: 10.3389/fendo.2024.1396465
47. Zhou X, Shen W, Zhu J, Chen Y, Zhang J. Association between the Oxidative Balance Score and Endometriosis: A Population-Based Study. Int J Women's Health. (2024) 16:1293–301. doi: 10.2147/IJWH.S466189
48. Chen Q, Bao W, Kong X, Zhu J, Hou S, Zhang Y, et al. Association between the oxidative balance score and kidney stones in adults. World J Urol. (2024) 42:425. doi: 10.1007/s00345-024-05144-5
49. Jia Z, Chen K. Association between the composite dietary antioxidant index and periodontitis in US adults: a cross-sectional analysis. Quint. Int. (2024) 55:734–42. doi: 10.3290/j.qi.b5714863
Keywords: oxidative balance score, female infertility, dietary antioxidants, oxidative stress, NHANES
Citation: Ma M, Xu H, Wang K, Chen Y, Pan T and Zhu Q (2025) Higher oxidative balance score is associated with a decreased risk of infertility: an analysis of NHANES 2013–2020. Front. Nutr. 12:1493253. doi: 10.3389/fnut.2025.1493253
Received: 08 September 2024; Accepted: 13 January 2025;
Published: 04 February 2025.
Edited by:
Hamid Reza Nouri, National Jewish Health, United StatesReviewed by:
Pengpeng Wang, Zhengzhou University, ChinaCopyright © 2025 Ma, Xu, Wang, Chen, Pan and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiaoling Zhu, MTA1NjA3MzA0NkBxcS5jb20=
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.