- 1Department of Emergency, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 2Department of Pulmonary and Critical Care Medicine, The First Affiliated Hospital of Wenzhou Medical University, Wenzhou, China
- 3Department of Gastroenterology, Minhang District Central Hospital of Shanghai, Fudan University, Shanghai, China
Background: An imbalance of the pro-oxidant and antioxidant profiles in the body contributes to the development of diseases, including female infertility.
Methods: In this study, we performed a secondary analysis of the National Health and Nutrition Examination Survey and calculated the values of oxidative balance score (OBS). A weighted logistic regression model was used to explore the potential relationship between OBS (continuous factor and quartile set) and female infertility, and the P for trend was calculated. Subgroup analyses were also carried out further to explore the association between OBS and female infertility, and the P for interactions were obtained.
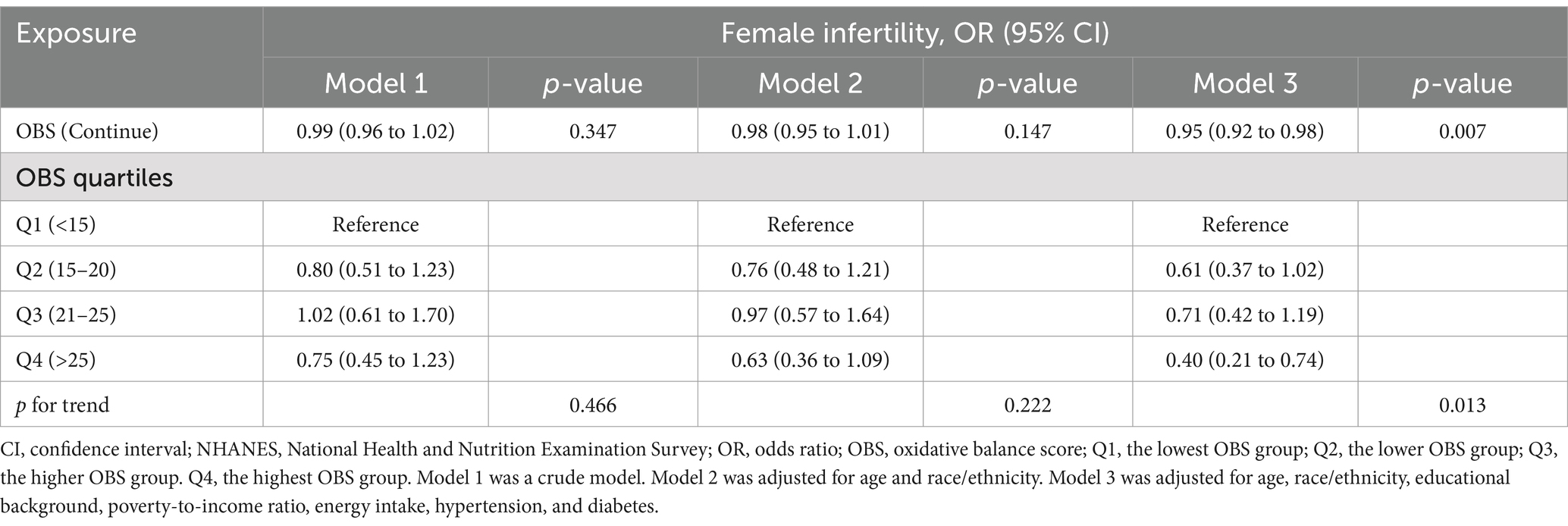
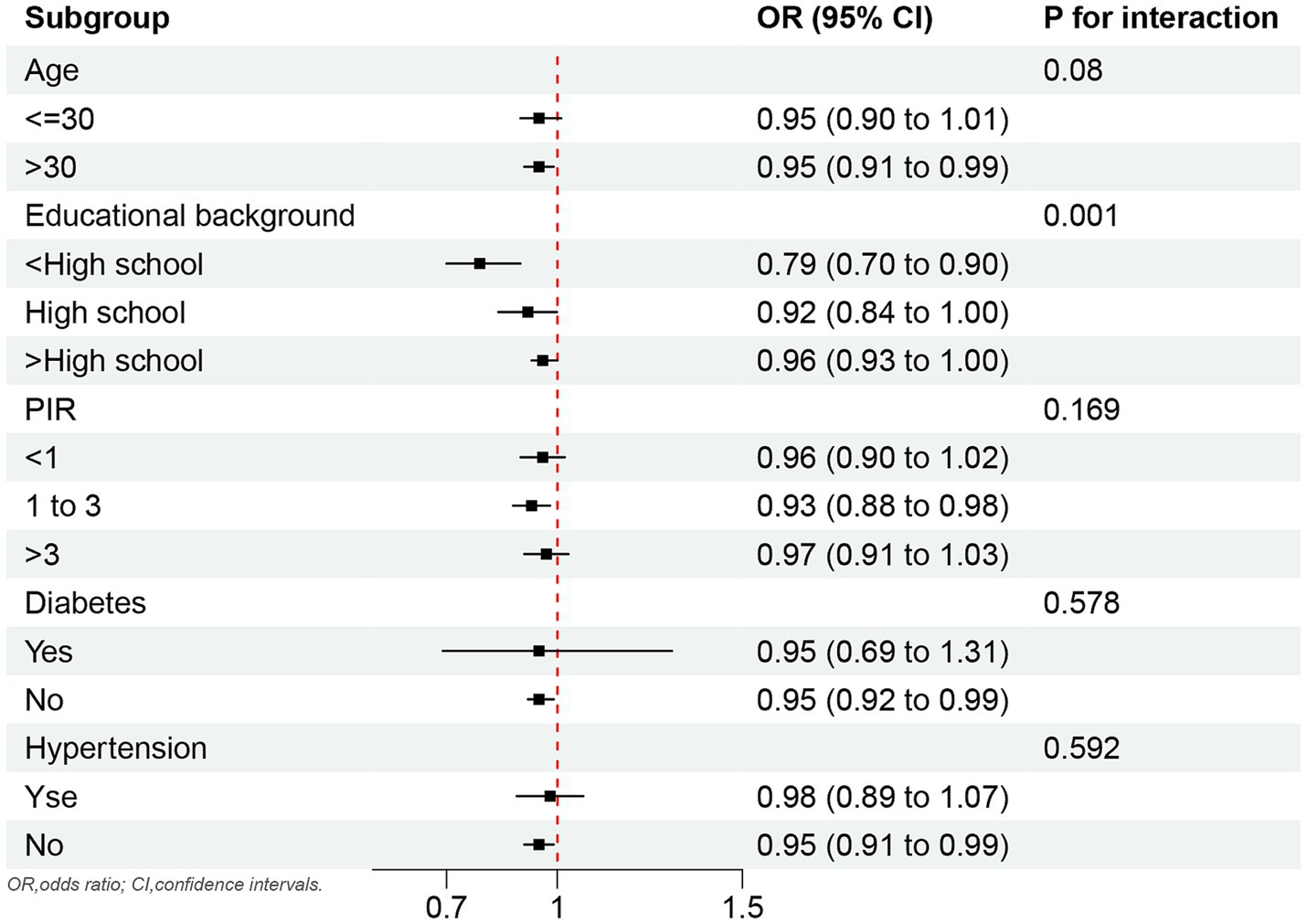
Results: There were 1,626 females (aged 18 to 45) included in the study, including 198 with infertility and a prevalence of approximately 13.28%. Multifactorial logistic regression showed a 5% decrease in infertility for each unit increased in OBS (OR, 0.95; 95% CI, 0.92 to 0.98). When OBS was used as a categorical variable, female infertility decreased by 60% in the highest OBS group compared with the lowest OBS group (OR, 0.40; 95% CI, 0.21 to 0.74). In addition, subgroup analyses showed that the negative association between OBS and infertility was significant in the non-chronic disease (hypertension and diabetes) population, those with less than a high school educational background, poverty-to-income ratio (1 to 3), and those with more than 30 years of age.
Conclusion: Higher OBS was negatively associated with female infertility. Further prospective studies are needed to determine causality and to provide new perspectives on female infertility in the context of diet and lifestyle.
Introduction
Infertility is in the spotlight once again with the global decline in fertility (1). It is a public health problem, the odds of infertility are trending upward to 8.1% from 2017 to 2019 in the United States (2). Although assisted reproductive technologies and advanced medications continue to develop (3, 4), they cannot address the root cause of the problem. Reproductive health should be emphasized in life and included in daily health management. In addition, there are many secondary conditions caused by infertility, such as depression (5). Many factors cause infertility, external factors include heavy metal pollution and air pollution (6, 7), and internal factors such as inflammation levels, oxidative and antioxidant imbalances (8, 9). Infertile females not only lead to marital crises but also suffer more (10). Therefore, it is important to prevent female infertility based on so many adverse effects.
The properties of diet and drugs are very closely associated with female infertility. Toxic mediators in the environment are reproductively toxic and also increase the risk of infertility by altering oxidation levels in the body (11). Therefore, some drugs are used to combat oxidative stress to improve pregnancy outcomes in in vitro fertilization (12). Recently, astaxanthin, as an antioxidant, helps reduce levels of oxidative stress in infertile females with polycystic ovary syndrome (13). In addition, some natural antioxidant supplementation (vitamins and flavonoids) improves female fertility (14). In addition to diet and medication, lifestyle has an irreplaceable role to play in female infertility. Both smoking and physical activity potentially affect female fertility (15, 16). However, these studies only focused on the effect of a single oxidative factor on female infertility. Regulating the level of oxidative stress in the body may offer new promise for female infertility. For example, physiologically, polycystic ovary syndrome leads to increased levels of oxidative stress thus leading to infertility (17). The concept of a relationship between overall oxidation levels and female infertility has not been proposed.
Oxidative balance score (OBS) as an overall pro-oxidant and antioxidant properties level is a highly important measure, higher OBS means greater antioxidant capacity of the body. It has steadily developed into an epidemiological indicator over the years. It also has been shown to correlate with various health problems such as sleep and lung disease (18, 19). Given the inextricable relationship between diet/lifestyle properties and female infertility, there is lacking comprehensive research on the unique role of antioxidant levels in female infertility. Therefore, the potential research between overall levels of oxidative and antioxidant properties and female infertility is enormous and promising. We hypothesized that there was a negative relationship between OBS and the risk of female infertility. Weighted logistic regression was used to explore the potential relationship between OBS (continuous factor and quartile set) and female infertility. By exploring the relationship between infertility and OBS, it may provide new ideas for infertility prevention.
Materials and methods
Population selection
We performed a secondary analysis of the National Health and Nutrition Examination Survey (NHANES) data. NHANES is a health prevention program that covers a wide range of people and has laboratory tests, questionnaires, and other information that can be used to investigate risk factors for disease and provide prevention strategies to prevent disease.
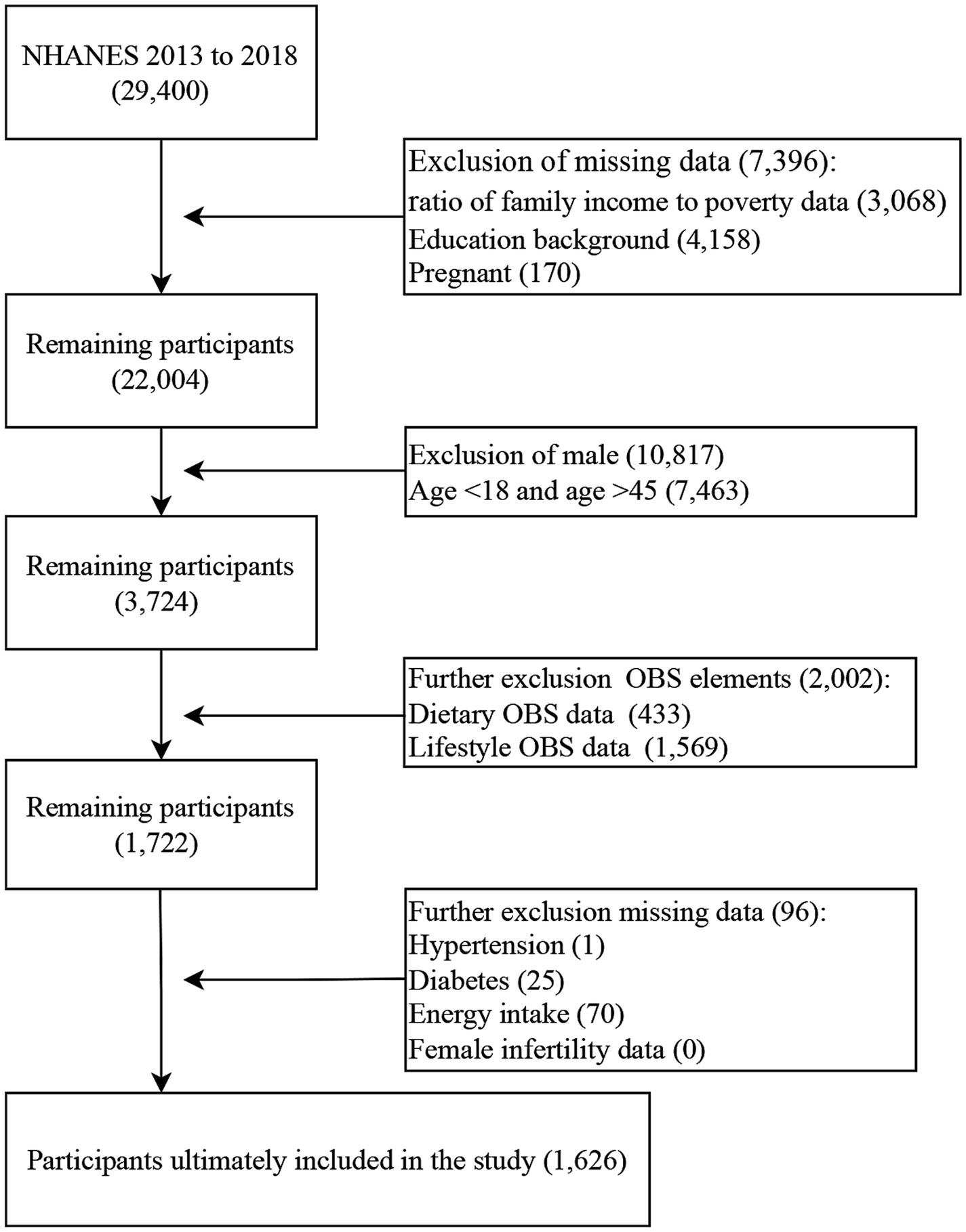
A total of 29,400 participants were in NHANES from 2013 to 2018 (three survey cycles). First, we excluded missing poverty-to-income ratio (PIR) data (3,068), education background data (4,158), and pregnancy (170). Second, we exclude males (10,817) and females aged under 18 or age older than 45 (7,463). Then, participants missing OBS elements data were excluded (2,002). Next, we further excluded missing data on hypertension, diabetes, energy intake, and female infertility data (96). Finally, the sample included in the study was 1,626 participants (Figure 1).
Exposure definition
OBS calculations are constantly being innovated. Based on the most recent studies of OBS calculations, the study incorporated 5 pro-oxidants and 15 antioxidants. Five pro-oxidant components included total fat, iron, serum cotinine, alcohol consumption, and body mass index (BMI). Fifteen antioxidants included dietary fiber, carotene, riboflavin, niacin, vitamin B6, total folate, vitamin B1, vitamin C, vitamin E, calcium, magnesium, zinc, copper, selenium, and physical activity. Higher OBS means higher antioxidant levels. Dietary OBS information was obtained from participants. To ensure the accuracy of dietary intake, participants underwent two 24-h dietary recall interviews. The first dietary recall interview was collected in person at a mobile screening center, and the second interview was collected by telephone 3 to 10 days later. The final intake obtained was the average of the two interviews. Alcohol consumption, serum cotinine, BMI, and physical activities were used to define lifestyle OBS. Alcohol consumption was defined as alcoholic beverages on average in the past 12 months. Serum cotinine levels were used as a measure of smoking. The physical activity definition was referred to in this study (20) and the formula was as follows: metabolic equivalent score * frequency of each physical activity per week * duration of each physical activity.
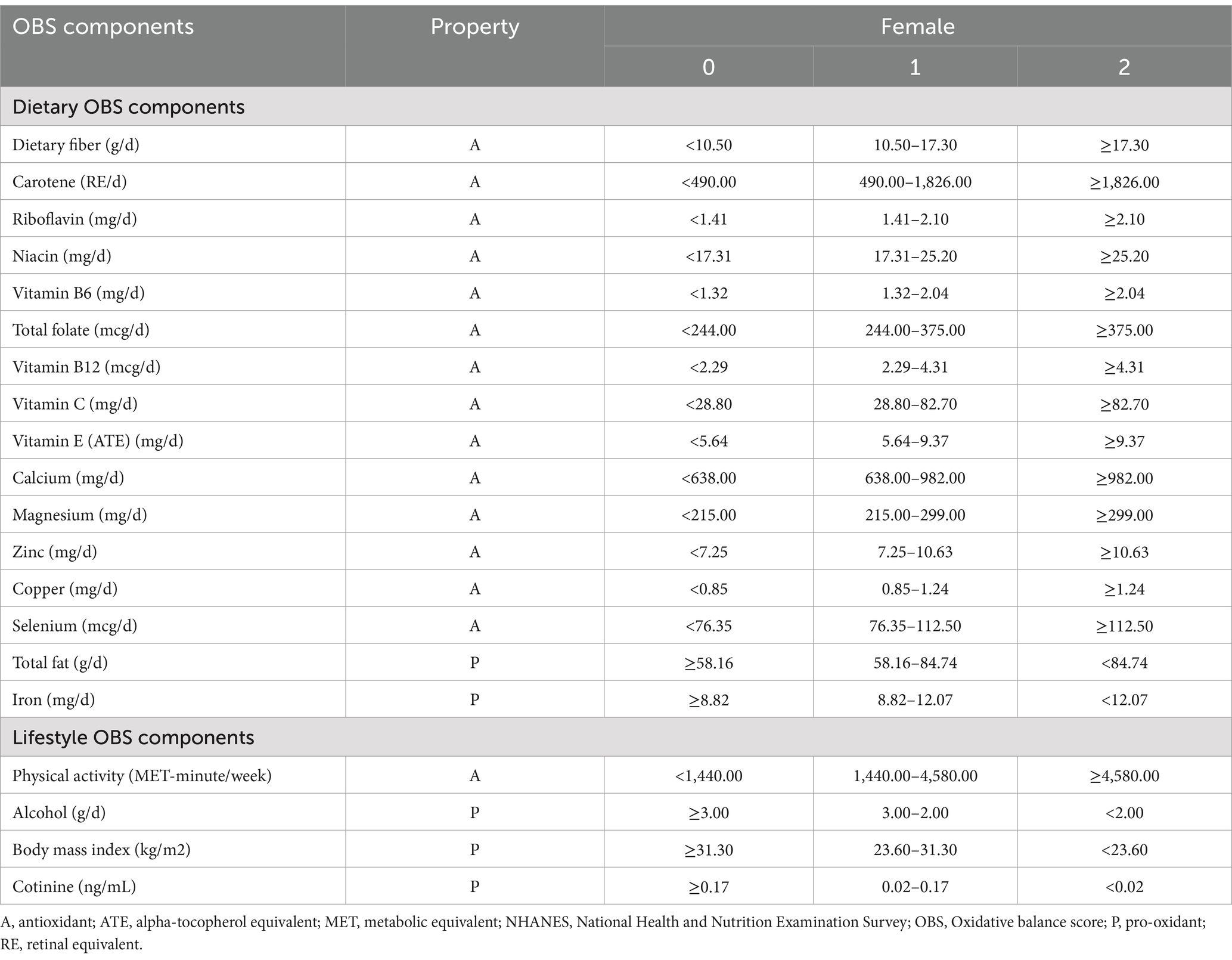
In the female population, each OBS component was divided according to tertiles. Antioxidant components were assigned a score of 2, 1, and 0 from high to low, while pro-oxidant components were assigned a score of 0, 1, and 2. The total OBS was the sum of the antioxidant and pro-oxidant components (Table 1). The maximum score could reach 40. Furthermore, the total OBS was divided into dietary OBS and lifestyle OBS.
Outcome definitions
Female infertility as the outcome of the study was derived from the Reproductive Health Questionnaire. The female population aged 18 to 45 years was selected for this study. Participants were asked “Have you ever attempted to become pregnant over a period of at least a year without becoming pregnant?” and “Have you ever been to a doctor or other medical provider because you have been unable to become pregnant?,” female infertility was defined when any of them answered “Yes.”
Covariates definitions
First, age, race/ethnicities (Non-Hispanic White, Non-Hispanic Black, other Hispanic, Mexican-American, and other races/ethnicities), educational background (below high school, high school, and above high school), and PIR as demographic factors were included. Second, uncontrolled hypertension is associated with female infertility (21). The molecular mechanisms by which diabetes affects female infertility have been revealed (22). Therefore, hypertension and diabetes were included as covariates. Hypertension was defined using the following questionnaire: “Have you ever been told by a doctor or other health professional that you had hypertension, also called high blood pressure?,” and diabetes was defined by the questionnaire: “Have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes?.” Concerning previous studies on the association of OBS with disease, total energy intake should be included as a covariate and extreme energy intake needs to be excluded (<500 or >3,500 kcal day−1 for females) (23, 24). Energy intake was 24 h before the interview and was averaged from two 24-h dietary recall interviews (days 1 and 3 to 10 days later).
Statistical analysis
We downloaded the three survey cycle data (2013 to 2018) from the NHANES website. A normality test was performed on the continuous variables, we expressed the non-normal continuous variables in terms of the median and the categorical variables expressed as unweighted frequencies (weighted percentages).
The Rao–Scott chi-squared test and the Kruskal–Wallis test were used for categorical and non-normal continuous variables, respectively, to correctly test for the baseline characteristics of the OBS quartiles. The weighted logistic regression was used to explore the relationship between OBS and female infertility. The model 1 was not adjusted. The model 2 was adjusted by age and race/ethnicity. The model 3 was adjusted all the covariates.
In addition, the study also investigated the association between dietary OBS and lifestyle OBS and female infertility. Subgroup analyses were also performed by age, educational background, PIR, hypertension, and diabetes. To test the stability of the model, sensitivity analyses were conducted by excluding the OBS components one by one.
R software (4.2.2) was used to perform the analyses. The statistical significance threshold was set at 0.05.
Results
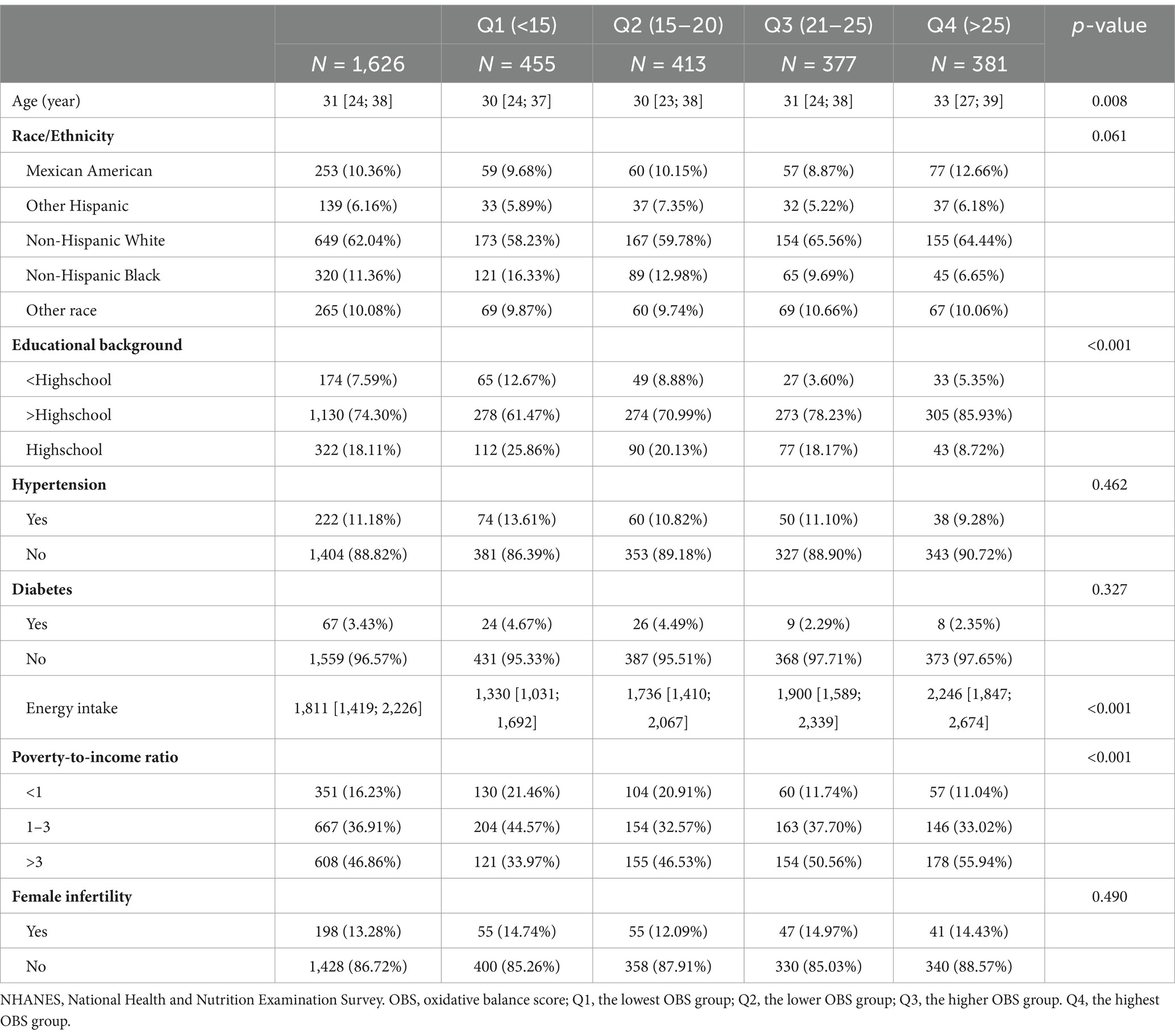
Baseline characteristics of participants by OBS’ quartiles
A total of 1,626 female participants who met the inclusion criteria made up the final sample. The female infertility rate was approximately 13.28%. Non-Hispanic White individuals (62.04%) make up the majority of them and 56% of participants had above high school educational background. The rate of female infertility among participants was 13.28% (Table 2).
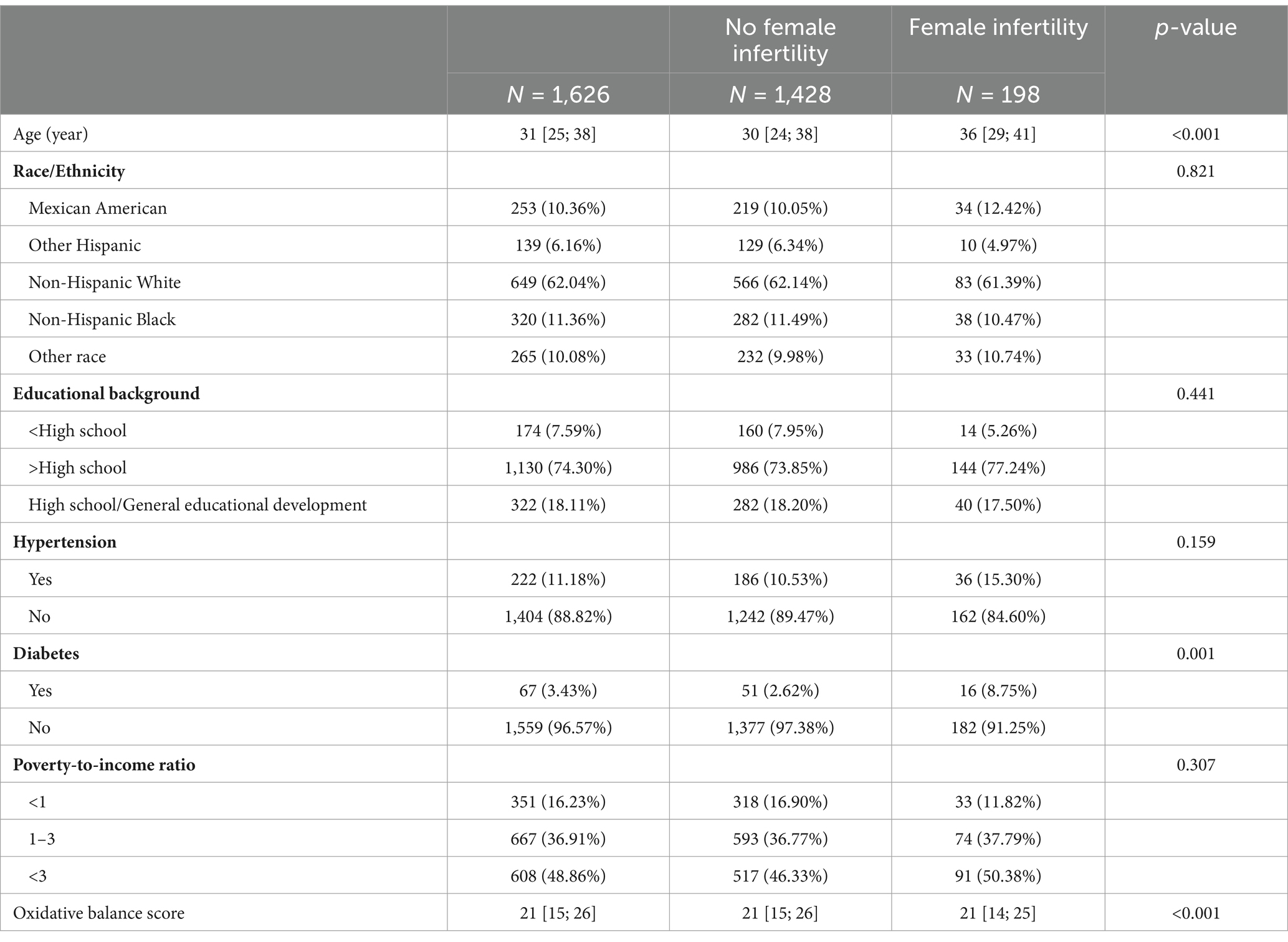
Baseline characteristics of with or without female infertility
As shown in Table 3, participants with infertility had older age, diabetes, and lower OBS compared to no infertility participants (p-value less than 0.05).
Association between OBS and female infertility
As shown in Table 4, OBS was a significantly negative association with female fertility after adjusting all covariates in model 3 (OR, 0.95; 95%CI, 0.92 to 0.98). In addition, female infertility was decreased by 60% from the lowest OBS group to the highest OBS group (OR, 0.40; 95%CI, 0.921 to 0.74).
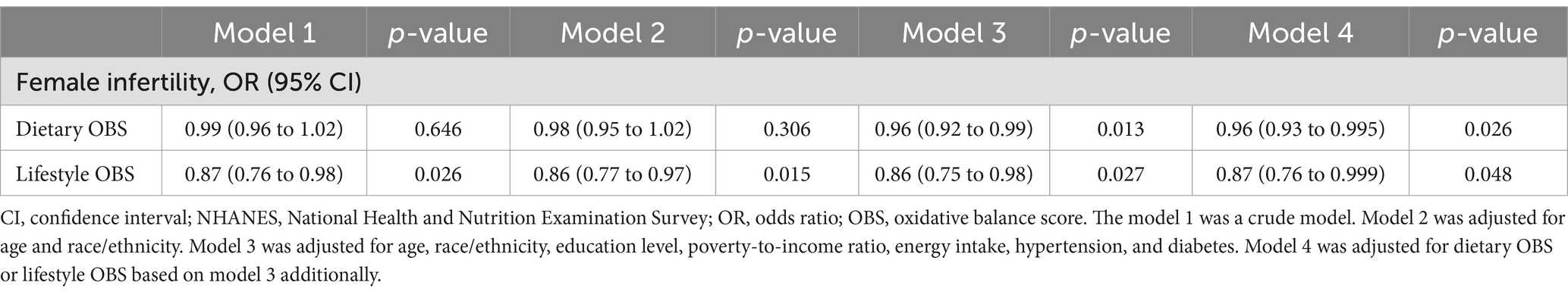
Association between the dietary OBS/lifestyle OBS and female infertility
As shown in Table 5, dietary OBS and lifestyle OBS were negatively associated with female infertility, and ORs (95%CI) were 0.96 (0.93 to 0.995) and 0.87 (0.76 to 0.999) in model 4, respectively.
Subgroup analyses
The negative correlation between OBS and female infertility was marked present in females older than 30 years (OR, 0.95; 95%CI, 0.91 to 0.99) and PIR in 1 to 3 (OR, 0.93; 95%CI, 0.88 to 0.98). In addition, this relationship also existed for those with less than a high school educational background and the p for interaction was 0.001. Furthermore, the negative correlation between OBS and female infertility also remained in females without chronic diseases (hypertension and diabetes; Figure 2).
In addition, with the removal of any individual OBS component, the relationship between OBS and female infertility was still robustly present (Supplementary S1).
Discussion
Our study revealed a negative correlation between OBS and female infertility. As OBS increased, female infertility decreased, as evidenced by a 60% reduction in infertility in the highest OBS group compared to the lowest OBS group. In addition, dietary OBS and lifestyle OBS were both negatively associated with OBS. Subgroup analyses suggested that this relationship was significant in those aged older than 30 years and with a PIR of 1 to 2, but not in educational background above high school, hypertensive, and diabetic patients.
Increasing attention is being paid to the role of diet in infertility. Previous studies have shown that dietary fiber content is negatively associated with infertility in obese females (25). Polycystic ovary syndrome, a major factor in infertility, is associated with a lower intake of carotenoids, lutein, riboflavin, niacin, and fiber in this population (26). In addition, altering oxidative stress in the female reproductive tract through vitamin C supplementation decreases infertility in diabetic females (27). Vitamin C as an antioxidant also alleviates symptoms of endometriosis (28). The amount of zinc in the diet also leads to differences in the risk of infertility (29). However, some studies have also indicated that differences in iron in the blood of infertile patients may be the result of differences in iron absorption caused by various flora in the intestines (30). Copper and zinc levels were higher in infertile women with endometrial disease (31). Some studies have recommended the inclusion of screening for ferritin levels in unexplained infertility (32). However, previous studies have examined the relationship with infertility for one micronutrient and have not evaluated overall levels for a relatively large number of elements. Our study is based on the sum of antioxidant and pro-oxidant components in the body, which is more indicative of a relationship with infertility than the individual components.
Environmental exposure to tobacco smoke is an important contributor to infertility, especially as blood cotinine concentrations increase the risk of infertility (33). In addition, secondhand smoke exposure further reduces conception rates in women with polycystic ovary syndrome (PCOS) (34). However, it has also been shown that malondialdehyde and total antioxidant capacity are not associated with cotinine in infertile females (35). Physical activity has a lot of benefits, not only can it enhance the reproductive function of women with polycystic ovary syndrome to reduce infertility, but it can also alleviate women’s stress from social and psychological sources (36). Physical activity and infertility risk show a non-linearity and appropriate physical activity is beneficial for reproductive health (37). In males, diminishing oxidative stress through high-intensity exercise improved reproductive function (38). Obesity increases the risk of female infertility and miscarriages (39). A Korean survey showed that alcohol consumption can increase infertility and that the odds of infertility increased among those with a BMI ≥ 25 (40). However, it has also been shown that alcohol use does not correlate with follicular fluid-soluble receptors of advanced glycation end-products causing oxidative damage to ovarian follicles (41). In contrast, however, women with PCOS drank less alcohol than women without PCOS (42). In the U.S. population, obesity has led to increased rates of infertility, mostly due to anovulation (43). Obesity contributes to increased infertility through several mechanisms, and the accumulation of fat leads to systemic oxidative stress (44). Increased BMI is negatively correlated with follicle-stimulating hormone and luteinizing hormone (45). Obesity also has a significant impact on metabolism, nursing interventions for women of childbearing age at different times of pregnancy have also been proposed (46). In our results, lifestyle OBS was found to be negatively associated with infertility, suggesting that the level of infertility can be altered through lifestyle modification.
Similarly, social factors can have an impact on infertility. Some studies have shown a negative correlation between the level of education and the stress associated with female infertility (47). Second, women with fewer years of education and lower incomes in the United States have higher rates of infertility (2). Our study showed that the negative association of OBS with infertility was reflected in the population with PIR < 1. However, a study revealed PIR is positively associated with the risk of infertility (48). In recent decades, females have become more focused on advancing in their education as well as their careers, and there is a clear trend to delay fertility (49). In addition, as our results demonstrate, the relationship between OBS and female infertility was negative in the low-education population. The results reflected the importance of implementing infertility prevention measures in this population.
In addition, although the study did a lot of correlation analyses between OBS and female infertility, there were a few points that need to be noted. For example, we diagnose female infertility using a questionnaire form to understand a specific group. Questionnaires were often susceptible to personal perceptions, values, social expectations, and peer pressures. The consistency and reliability of the data were compromised. This was especially true when sensitive topics were involved. Although the questionnaire form of the survey could illustrate the science to a certain extent, having objective laboratory test results seemed to be able to study the problem more accurately. Therefore, scientific research through biomarkers as well as clinical assessment were necessary.
It was worth noting that OBS was an indicator that continues to improve as research progresses. The OBS in the study only represented 5 pro-oxidants and 15 antioxidant components in the human body. It was undeniable that the levels of chemical elements in the human body and the environment in which an individual lives were complex. The OBS for this study only represents the levels of oxidation and antioxidants calculated as best as possible from this database. As the study continues, the OBS will be improved and made representative. It has already been found that obesity-derived hormones have a moderating role in infertility (50). For example, an important possible reason for this was the specific role of adiponectin and visfatin in oxidative stress (51, 52). Therefore, including obesity-derived hormones in analyses may be a promising direction as obesity rates increase.
This study also had strengths and limitations. First, participants in the secondary analyses were taken from the representative NHANES database, and the results have broad applicability in the United States. Second, the study weighted the data to make the results more reliable and stable. Third, multivariate weighted regression models as well as sensitivity analysis were included in the study to investigate the potential relationship between OBS and female infertility further. However, the study also has limitations. First, the biggest limitation was the study was designed as a cohort study and could not conclude causality. Female infertility diagnosed using a questionnaire format was subjective. Participants might provide inaccurate information due to vague memories or emotional overtones. A proportion of participants might have cognitive biases, such as self-denial and overconfidence, which could affect the veracity of the questionnaire. However, the design of the questionnaire in NHANES was rigorous and every step was strictly controlled from the selection of the sample, interview setting and mode of administration, quality assurance and quality control, data processing, and editing. In the data analysis stage, we also weighted the data according to the official tutorial to try our best to reduce bias. However, prospective studies are necessary in the future.
Conclusion
The study highlighted the importance of intervening in the degree of oxidation and antioxidation in bodies. It seemed that higher OBS was negatively associated with female infertility, especially among some key populations. The potential molecular mechanisms and temporal sequencing between OBS and female infertility need to be further verified. In the future, combining diet and lifestyle may deepen the understanding of female infertility, particularly early intervention, and health management for specific populations. Furthermore, the study provided public health policy recommendations for low fertility in some countries.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the National Center for Health Statistics institutional review board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XLe: Data curation, Software, Visualization, Writing – original draft. XLi: Data curation, Software, Writing – original draft. CYu: Data curation, Validation, Writing – original draft. LX: Data curation, Software, Writing – original draft. LZ: Software, Visualization, Writing – original draft. CYa: Supervision, Writing – review & editing. ZX: Project administration, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1484756/full#supplementary-material
References
1. Aitken, RJ. The global decline in human fertility: the post-transition trap hypothesis. Life. (2024) 14:369. doi: 10.3390/life14030369
2. Snow, M, Vranich, TM, Perin, J, and Trent, M. Estimates of infertility in the United States: 1995-2019. Fertil Steril. (2022) 118:560–7. doi: 10.1016/j.fertnstert.2022.05.018
3. Malik, S, Saeed, S, Saleem, A, Khan, MI, Khan, A, and Akhtar, MF. Alternative treatment of polycystic ovary syndrome: pre-clinical and clinical basis for using plant-based drugs. Front Endocrinol (Lausanne). (2023) 14:1294406. doi: 10.3389/fendo.2023.1294406
4. Vaidakis, D, Papapanou, M, and Siristatidis, CS. Autologous platelet-rich plasma for assisted reproduction. Cochrane Database Syst Rev. (2024) 4:Cd013875. doi: 10.1002/14651858.CD013875.pub2
5. Sun, F, Liu, M, Hu, S, Xie, R, Chen, H, Sun, Z, et al. Associations of weight-adjusted-waist index and depression with secondary infertility. Front Endocrinol (Lausanne). (2024) 15:1330206. doi: 10.3389/fendo.2024.1330206
6. LaPointe, S, Lee, JC, Nagy, ZP, Shapiro, DB, Chang, HH, Wang, Y, et al. Ambient traffic related air pollution in relation to ovarian reserve and oocyte quality in young, healthy oocyte donors. Environ Int. (2024) 183:108382. doi: 10.1016/j.envint.2023.108382
7. Miglietta, S, Cristiano, L, Battaglione, E, Macchiarelli, G, Nottola, SA, De Marco, MP, et al. Heavy metals in follicular fluid affect the ultrastructure of the human mature cumulus-oocyte complex. Cells. (2023) 12:2577. doi: 10.3390/cells12212577
8. Khan, MZ, Khan, A, Chen, W, Chai, W, and Wang, C. Advancements in genetic biomarkers and exogenous antioxidant supplementation for safeguarding mammalian cells against heat-induced oxidative stress and apoptosis. Antioxidants. (2024) 13:258. doi: 10.3390/antiox13030258
9. Qi, J, Su, Y, Zhang, H, and Ren, Y. Association between dietary inflammation index and female Infertility from National Health and nutrition examination survey: 2013-2018. Front Endocrinol (Lausanne). (2024) 15:1309492. doi: 10.3389/fendo.2024.1309492
10. Khalesi, ZB, and Kenarsari, FJ. Anxiety, depression, and stress: a comparative study between couples with male and female infertility. BMC Womens Health. (2024) 24:228. doi: 10.1186/s12905-024-03072-5
11. Shi, W, Zhang, Z, Li, M, Dong, H, and Li, J. Reproductive toxicity of Pfoa, Pfos and their substitutes: a review based on epidemiological and toxicological evidence. Environ Res. (2024) 250:118485. doi: 10.1016/j.envres.2024.118485
12. Fan, J, Chen, C, and Zhong, Y. A cohort study on Ivf outcomes in infertile endometriosis patients: the effects of rapamycin treatment. Reprod Biomed Online. (2024) 48:103319. doi: 10.1016/j.rbmo.2023.103319
13. Jabarpour, M, Aleyasin, A, Shabani Nashtaei, M, and Amidi, F. Astaxanthin supplementation impact on insulin resistance, lipid profile, blood pressure, and oxidative stress in polycystic ovary syndrome patients: a triple-blind randomized clinical trial. Phytother Res. (2024) 38:321–30. doi: 10.1002/ptr.8037
14. Vašková, J, Klepcová, Z, Špaková, I, Urdzík, P, Štofilová, J, Bertková, I, et al. The importance of natural antioxidants in female reproduction. Reproduction. (2023) 12:907. doi: 10.3390/antiox12040907
15. Huang, J, Okuka, M, McLean, M, Keefe, DL, and Liu, L. Effects of cigarette smoke on fertilization and embryo development in vivo. Fertil Steril. (2009) 92:1456–65. doi: 10.1016/j.fertnstert.2008.07.1781
16. Xie, F, You, Y, Guan, C, Gu, Y, Yao, F, and Xu, J. Association between physical activity and infertility: a comprehensive systematic review and Meta-analysis. J Transl Med. (2022) 20:237. doi: 10.1186/s12967-022-03426-3
17. Zeng, Z, Shan, H, Lin, M, Bao, S, Mo, D, Deng, F, et al. Sirt3 protects endometrial receptivity in patients with polycystic ovary syndrome. Chin Med J (2024). doi: 10.1097/CM9.0000000000003127 [Epub ahead of print].
18. Lei, X, Xu, Z, and Chen, W. Association of oxidative balance score with sleep quality: Nhanes 2007-2014. J Affect Disord. (2023) 339:435–42. doi: 10.1016/j.jad.2023.07.040
19. Xu, Z, Xue, Y, Wen, H, and Chen, C. Association of Oxidative Balance Score and Lung Health from the National Health and nutrition examination survey 2007-2012. Front Nutr. (2022) 9:961950. doi: 10.3389/fnut.2022.961950
20. Tian, X, Xue, B, Wang, B, Lei, R, Shan, X, Niu, J, et al. Physical activity reduces the role of blood cadmium on depression: a cross-sectional analysis with Nhanes data. Environ Pollut. (2022) 304:119211. doi: 10.1016/j.envpol.2022.119211
21. Xiong, W, Han, L, Tang, X, Li, R, Chen, W, Liu, X, et al. Maternal hypertension and Fecundability: a population-based cohort study. Hypertension. (2024) 81:e173–84. doi: 10.1161/HYPERTENSIONAHA.124.23562
22. Andlib, N, Prabha, S, and Thakur, SC. Unraveling the molecular pathogenesis of type 2 diabetes and its impact on female infertility: a bioinformatics and systems biology approach. Comput Biol Med. (2024) 180:108987. doi: 10.1016/j.compbiomed.2024.108987
23. Xu, Z, Lei, X, Chu, W, Weng, L, Chen, C, and Ye, R. Oxidative balance score was negatively associated with the risk of metabolic syndrome, metabolic syndrome severity, and all-cause mortality of patients with metabolic syndrome. Front Endocrinol (Lausanne). (2023) 14:1233145. doi: 10.3389/fendo.2023.1233145
24. Zhang, W, Peng, SF, Chen, L, Chen, HM, Cheng, XE, and Tang, YH. Association between the oxidative balance score and telomere length from the National Health and Nutrition Examination Survey 1999-2002. Oxidative Med Cell Longev. (2022) 2022:1345071–11. doi: 10.1155/2022/1345071
25. Cai, Q, and Chen, T. Association between dietary fiber and female fertility: a Nhanes-based study. Reprod Sci. (2023) 30:1555–64. doi: 10.1007/s43032-022-01103-w
26. Badri-Fariman, M, Naeini, AA, Mirzaei, K, Moeini, A, Hosseini, M, Bagheri, SE, et al. Association between the food security status and dietary patterns with polycystic ovary syndrome (Pcos) in overweight and obese Iranian women: a case-control study. J Ovarian Res. (2021) 14:134. doi: 10.1186/s13048-021-00890-1
27. Gupta, HP, Pandey, R, and Ravi, RK. Altered sperm fate in the reproductive tract milieu due to oxidative stress leads to sub-fertility in type 1 diabetes females: a Drosophila-based study. Life Sci. (2023) 313:121306. doi: 10.1016/j.lfs.2022.121306
28. Amini, L, Chekini, R, Nateghi, MR, Haghani, H, Jamialahmadi, T, Sathyapalan, T, et al. The effect of combined vitamin C and vitamin E supplementation on oxidative stress markers in women with endometriosis: a randomized, triple-blind placebo-controlled clinical trial. Pain Res Manag. (2021) 2021:5529741–6. doi: 10.1155/2021/5529741
29. Huang, J, Hu, L, and Yang, J. Dietary zinc intake and body mass index as modifiers of the association between household pesticide exposure and infertility among us women: a population-level study. Environ Sci Pollut Res Int. (2023) 30:20327–36. doi: 10.1007/s11356-022-23629-x
30. Yao, X, Zuo, N, Guan, W, Fu, L, Jiang, S, Jiao, J, et al. Association of gut microbiota enterotypes with blood trace elements in women with infertility. Nutrients. (2022) 14:3195. doi: 10.3390/nu14153195
31. Li, D, Jiang, T, Wang, X, Yin, T, Shen, L, Zhang, Z, et al. Serum essential trace element status in women and the risk of endometrial diseases: a case-control study: serum essential trace element status in women and the risk of endometrial diseases: a case-control study. Biol Trace Elem Res. (2023) 201:2151–61. doi: 10.1007/s12011-022-03328-x
32. Holzer, I, Ott, J, Beitl, K, Mayrhofer, D, Heinzl, F, Ebenbauer, J, et al. Iron status in women with infertility and controls: a case-control study. Front Endocrinol (Lausanne). (2023) 14:1173100. doi: 10.3389/fendo.2023.1173100
33. Peng, L, Luo, X, Cao, B, and Wang, X. Unraveling the link: environmental tobacco smoke exposure and its impact on infertility among American women (18-50 years). Front Public Health. (2024) 12:1358290. doi: 10.3389/fpubh.2024.1358290
34. Li, J, Wu, Q, Wu, XK, Zhou, ZM, Fu, P, Chen, XH, et al. Effect of exposure to second-hand smoke from husbands on biochemical Hyperandrogenism, metabolic syndrome and conception rates in women with polycystic ovary syndrome undergoing ovulation induction. Hum Reprod. (2018) 33:617–25. doi: 10.1093/humrep/dey027
35. Kazemi, A, Ramezanzadeh, F, Esfahani, MH, Saboor-Yaraghi, AA, Nejat, S, and Rahimi-Foroshani, A. Impact of environmental tobacco smoke exposure in women on oxidative stress in the antral follicle and assisted reproduction outcomes. J Res Med Sci. (2013) 18:688–94.
36. Butt, MS, Saleem, J, Zakar, R, Aiman, S, Khan, MZ, and Fischer, F. Benefits of physical activity on reproductive health functions among polycystic ovarian syndrome women: a systematic review. BMC Public Health. (2023) 23:882. doi: 10.1186/s12889-023-15730-8
37. Zhang, H, Hua, L, Liu, D, Su, X, Chen, J, and Chen, J. Effects of physical activity on infertility in reproductive females. Reprod Biol Endocrinol. (2024) 22:62. doi: 10.1186/s12958-024-01234-6
38. Maleki, BH, and Tartibian, B. High-intensity exercise training for improving reproductive function in infertile patients: a randomized controlled trial. J Obstet Gynaecol Can. (2017) 39:545–58. doi: 10.1016/j.jogc.2017.03.097
39. Metwally, M, Ong, KJ, Ledger, WL, and Li, TC. Does high body mass index increase the risk of miscarriage after spontaneous and assisted conception? A meta-analysis of the evidence. Fertil Steril. (2008) 90:714–26. doi: 10.1016/j.fertnstert.2007.07.1290
40. Lee, J, Choo, CW, Moon, KY, Lyu, SW, Kim, H, Lee, JY, et al. Risk factors for infertility in Korean women. J Korean Med Sci. (2024) 39:e85. doi: 10.3346/jkms.2024.39.e85
41. Sopasi, F, Spyropoulou, I, Kourti, M, Vasileiadis, S, Tripsianis, G, Galazios, G, et al. Oxidative stress and female infertility: the role of follicular fluid soluble receptor of advanced glycation end-products (Srage) in women with endometriosis. Hum Fertil (Camb). (2023) 26:1400–7. doi: 10.1080/14647273.2023.2230360
42. Kazemi, M, Kim, JY, Wan, C, Xiong, JD, Michalak, J, Xavier, IB, et al. Comparison of dietary and physical activity behaviors in women with and without polycystic ovary syndrome: a systematic review and Meta-analysis of 39471 women. Hum Reprod Update. (2022) 28:910–55. doi: 10.1093/humupd/dmac023
43. Boots, CE, Gloff, M, Lustik, SJ, and Vitek, W. Addressing weight Bias in reproductive medicine: a call to revisit Bmi restrictions for in vitro fertilization. Fertil Steril. (2024) 122:204–10. doi: 10.1016/j.fertnstert.2024.05.140
44. Mele, VG, Chioccarelli, T, Finamore, R, D'Agostino, A, d'Agostino, M, Cimini, D, et al. Antioxidants positively regulate obesity dependent Circrnas - sperm quality - functional axis. Front Endocrinol (Lausanne). (2023) 14:1290971. doi: 10.3389/fendo.2023.1290971
45. Vedelek, V, Bicskei, P, Tábi, M, Lajkó, N, Ékes, C, Bereczki, K, et al. Endometrium development patterns and Bmi groups among in vitro fertilization patients; prognostic aspects. Front Endocrinol (Lausanne). (2024) 15:1379109. doi: 10.3389/fendo.2024.1379109
46. Schon, SB, Cabre, HE, and Redman, LM. The impact of obesity on reproductive health and metabolism in reproductive-age females. Fertil Steril. (2024) 122:194–203. doi: 10.1016/j.fertnstert.2024.04.036
47. Lei, A, You, H, Luo, B, and Ren, J. The associations between infertility-related stress, family adaptability and family cohesion in infertile couples. Sci Rep. (2021) 11:24220. doi: 10.1038/s41598-021-03715-9
48. Chen, X, Liang, J, Yang, Q, Huang, J, Li, L, and Deng, K. Age affects the association between socioeconomic status and infertility: a cross-sectional study. BMC Womens Health. (2023) 23:675. doi: 10.1186/s12905-023-02680-x
49. Datta, J, Palmer, MJ, Tanton, C, Gibson, LJ, Jones, KG, Macdowall, W, et al. Prevalence of infertility and help seeking among 15 000 women and men. Hum Reprod. (2016) 31:2108–18. Epub 2016/07/02. doi: 10.1093/humrep/dew123
50. Singh, A, Choubey, M, Bora, P, and Krishna, A. Adiponectin and Chemerin: contrary Adipokines in regulating reproduction and metabolic disorders. Reprod Sci. (2018) 25:1462–73. doi: 10.1177/1933719118770547
51. Alam, F, Shahid, M, Riffat, S, Zulkipli, IN, Syed, F, Ashraf, M, et al. Sirt1 and antioxidants in infertile females: exploration of the role of vitamin D. PLoS One. (2023) 18:e0287727. doi: 10.1371/journal.pone.0287727
Keywords: female infertility, oxidative balance score, NHANES, dietary, lifestyle
Citation: Lei X, Liu X, Yu C, Xia L, Zhou L, Yao C and Xu Z (2024) Higher oxidative balance score is associated with lower female infertility: a cross-sectional study. Front. Nutr. 11:1484756. doi: 10.3389/fnut.2024.1484756
Edited by:
Rosaria Meccariello, University of Naples Parthenope, ItalyReviewed by:
Małgorzata Natalia Słoma-Krześlak, Śląskiego Uniwersytetu Medycznego, PolandMayank Choubey, NYU Grossman Long Island School of Medicine, United States
Hamid Reza Nouri, National Jewish Health, United States
Copyright © 2024 Lei, Liu, Yu, Xia, Zhou, Yao and Xu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Can Yao, eWFvY2FuMTIzMEAxNjMuY29t; Zhixiao Xu, eHV6aGl4aWFvQHdtdS5lZHUuY24=
 Xiong Lei
Xiong Lei Xiling Liu2
Xiling Liu2 Zhixiao Xu
Zhixiao Xu