
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 20 November 2024
Sec. Nutrition and Metabolism
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1473851
This article is part of the Research Topic Exploring the Obesity-Cancer Nexus: Dietary Influences and Biological Mechanisms View all 3 articles
Background: The association between high body-mass index (BMI) and colorectal cancer (CRC) has been confirmed and gained attention. However, a detailed understanding of the disease burden of high BMI and CRC remains lacking.
Objective: This study aimed to assess the temporal and geographical trends of CRC deaths and disability-adjusted life years (DALYs) caused by high BMI globally from 1990 to 2021, providing effective guidance for developing prevention and treatment strategies.
Methods: We used data from the 2021 Global Burden of Disease study to assess the global, regional, and national Deaths, DALYs, age-standardized mortality rate (ASMR), and age-standardized DALY rates (ASDR) caused by CRC related to high BMI, and further calculated the estimated annual percentage change (EAPC). We also considered factors such as gender, age, and sociodemographic index (SDI). We explore the relationship between EAPC and ASMR/ASDR (1990) and between EAPC and SDI (2021). Further, the autoregressive integrated moving average (ARIMA) model was applied to predict the disease burden from 2022 to 2035. The risk factors were calculated by Population Attributable Fraction (PAF).
Results: In 2021, CRC caused by high BMI resulted in 99,268 deaths (95% Uncertainty Interval (UI): 42,956–157,949) and 2,364,664 DALYs (95% UI: 1,021,594–3,752,340) globally, with ASMR and ASDR being 1.17 per 100,000 population (95% UI: 0.51–1.87) and 27.33 per 100,000 population (95% UI: 11.8–43.37), respectively. The disease burden was higher in males and the elderly, with significant differences between regions and sociodemographic groups. From 1990 to 2021, the ASMR for CRC associated with high BMI revealed little change globally, while the ASDR revealed an upward trend. The burden of CRC caused by high BMI has shifted from high SDI regions to low and low-middle SDI regions. Additionally, from 2022 to 2035, ASMR and ASDR are expected to increase in males, while ASMR and ASDR in females are expected to remain relatively stable.
Conclusion: From 1990 to 2021, the number of deaths and DALYs related to high BMI-associated CRC globally, as well as ASMR and ASDR, continue to rise. We predict that ASMR and ASDR may further increase by 2035, making it crucial to take timely and targeted interventions.
Colorectal cancer (CRC) is a malignant tumor with high incidence and mortality rates worldwide and poses a significant threat to public health. As the most common malignancy of the digestive system, CRC ranks third in cancer incidence and second in mortality worldwide (1, 2). Recently, with population aging, Westernized dietary patterns, and the prevalence of sedentary lifestyles, the incidence of CRC has exhibited a continuous upward trend, specifically in developing countries. The number of CRC cases and deaths worldwide has increased in recent years. Additionally, differences in CRC incidence and mortality rates are associated with varying levels of human development and regional disparities (3). Over the past 30 years, the trend in CRC incidence has remained stable or even declined in high sociodemographic index (SDI) countries, while it has been on the rise in low-income and transitioning economies. This indicates an unequal distribution of the CRC burden worldwide. Over time, this inequality seems to worsen, leading to a growing global gap in the CRC burden. Low- and middle-income countries are bearing an increasing CRC burden (3, 4).
Based on the Global Burden of Disease (GBD) 2021, there are over 20 risk factors contributing to CRC, among which dietary risk factors are the most significant, followed by metabolic risk factors (1, 5). Among the metabolic risk factors, a high body mass index is the most prominent. Numerous research conclusions have already been established regarding CRC attributed to dietary risk factors, which we will not elaborate on here (5). Next, we will primarily explore the epidemiological trends of CRC attributed to high BMI among metabolic risk factors and describe risk factors using PAF.
Body-mass index (BMI) is obtained by dividing a person’s weight (kg) by the square of their height (m). It is a direct indicator used to classify adults into three categories: underweight, BMI below 18.5; overweight, BMI 25.0–29.9; obese, BMI 30.0 and above (6). Numerous studies have demonstrated that a high BMI increases cancer risk, with an elevated BMI being considered an established risk factor for CRC and 12 other cancers. A meta-analysis by the World Cancer Research Fund indicates that for every 5 kg/m2 increase in BMI, the risk of CRC increases by 5% (7, 8). According to GBD 2021, 9.51% of the mortality burden and 9.69% of the disability-adjusted life years (DALYs) burden is attributable to high BMI (1, 9).
The mechanisms by which a high BMI affects CRC risk are complex and diverse. First, individuals with high BMI, hyperlipidemia, and insulin resistance have low-grade systemic inflammation, promoting tumor cell proliferation and angiogenesis while reducing apoptosis (10). Insulin resistance and hyperinsulinemia may promote tumorigenesis through the IGF-1 signaling pathway, and adipokines, such as leptin and adiponectin, secreted by adipose tissue may also be involved in the development and progression of CRC (11). Additionally, the mechanisms contributing to CRC may include physical activity levels, dietary patterns, genetic background, and the gut microbiome (12). Despite the extensive evidence provided by existing studies, limitations remain, such as reliance on cross-sectional or retrospective studies, making it difficult to determine causality. BMI, as a measure of obesity, also has some limitations. Future research may need to incorporate other metrics, such as waist circumference and body fat percentage, to comprehensively assess the relationship between body fat and CRC risk (13, 14).
By analyzing data from 204 countries and regions between 1990 and 2021, this study provides a comprehensive assessment of the impact of high BMI on the CRC burden, which is crucial for developing effective public health policies and personalized prevention strategies. Furthermore, we developed a model to forecast the global disease burden of high BMI-related CRC from 2022 to 2035. Future research should further elucidate the molecular mechanisms involved and explore effective interventions to reduce the risk of high BMI-related CRC.
GBD 2021 provides a comprehensive overview of disabilities and deaths caused by high BMI leading to CRC from 1990 to 2021 across different countries, ages, and genders. It estimated the incidence, prevalence, mortality, years of life lost (YLLs), years lived with disability (YLDs), and DALYs due to 369 diseases and injuries in 204 countries and regions. DALYs are a measure that combines years of YLLs and YLDs (15). We obtained the number of deaths and DALY data caused by high BMI leading to CRC in 204 countries and regions from the Global Health Data Exchange (GHDx) website,1 age-standardized mortality rates (ASMR), and age-standardized DALY rates (ASDR) (16, 17). The 204 countries and regions were further divided into 21 regions based on their geographical location. Moreover, data analysis adopted a stratified approach, dividing age into 16 different groups, with 15 being 5-year age intervals (20–94 years, in 5-year intervals) and one being individuals aged 95 years and above.
We separately obtained SDI data for 1990–2021 from the GHDx. SDI is a good indicator of socioeconomic development related to health. It is a composite indicator of lag-distributed income per capita, the average educational attainment of the population aged 15 years and above, and the total fertility rate under the age of 25, ranging from 0 to 1. According to the SDI quintiles, 204 countries or regions were divided into five quintiles: low SDI (< 0.45), low-middle SDI (≥ 0.45 and < 0.61), middle SDI (≥ 0.61 and < 0.69), high-middle SDI (≥ 0.69 and < 0.80), and high SDI (≥ 0.80) (18, 19).
In this study, we analyzed the global, national burden of CRC caused by high BMI using the ASMR and ASDR (per 100,000 population) to reflect the actual situation of deaths and DALYs (20). To assess trends, we used the linear regression equation (y = α + βx + ε), where y represents the age-standardized rate (ASR), which refers to ASIR, ASMR, or ASDR and x represents the calendar year. The estimated annual percentage change (EAPC) was calculated as 100 × (exp(β) − 1), with its 95% confidence interval (CI) determined using the linear regression model. If the EAPC value and its 95% CI lower limit are both greater than 0, the ASR is considered to exhibit an increasing trend annually. If the EAPC value and its 95% CI upper limit are both less than 0, the ASR is considered to exhibit a decreasing trend annually. If the EAPC is close to 0, the ASR is considered stable (21). This method is widely used to quantify and summarize temporal changes in ASR (22, 23). Statistical analyses were performed using R software (version 4.4.1), with p-values <0.05 considered statistically significant.
To analyze the factors influencing the EAPC of the CRC burden related to high BMI, we used Pearson correlation analysis to examine the relationship between EAPC and ASR in 1990 and the relationship between EAPC and SDI scores in 2021, with data analysis performed using R software (version 4.4.1), two-tailed p < 0.05 was considered statistically significant.
To forecast the global disease burden of high BMI-related CRC from 2022 to 2035, we used an autoregressive integrated moving average (ARIMA) model. It forecasts future values based on past properties (limitations and prediction errors). The ARIMA model is defined by three parameters: p, d, and q, where p is the order of autoregression, q is the order of moving average, and d is the degree of difference. The ARIMA equation is
where ϕ and θ are the autoregressive and moving average parameters, respectively. Yt represents the differenced time series, and εt is the value of the random shock at time t. α is a constant (24, 25). After multiple tests, we identified the optimal model using the ARIMA (1,1,2) model to predict ASMR and ASDR for males and the ARIMA (2,0,0) model to predict ASMR and ASDR for females.
From 1990 to 2021, globally, the incidence of CRC revealed an increasing trend, with the number of cases increasing from 916,584 (95% UI 866,238–951,895) in 1990 to 2,194,143 (95% UI: 2,001,272–2,359,390) in 2021, with an EAPC of 0.15 (95% CI: 0.12–0.19) (Table 1). In 2021, among the quintiles of SDI, areas with high SDI had the highest ASIR, but its annual growth rate decreased (EAPC = −0.25; 95% CI: −0.35 to −0.16), while the region with the highest annual growth rate was the middle SDI (EAPC = 1.38; 95% CI: 1.3–1.46) (Table 1). At the regional level of GBD, the region with the fastest growth in ASIR was Central Latin America (EAPC = 2.05; 95% CI: 1.99–2.11), and the region with the largest annual decline in ASIR was High-income North America (EAPC = −0.8; 95% CI: −0.92 to −0.67) (Table 1).
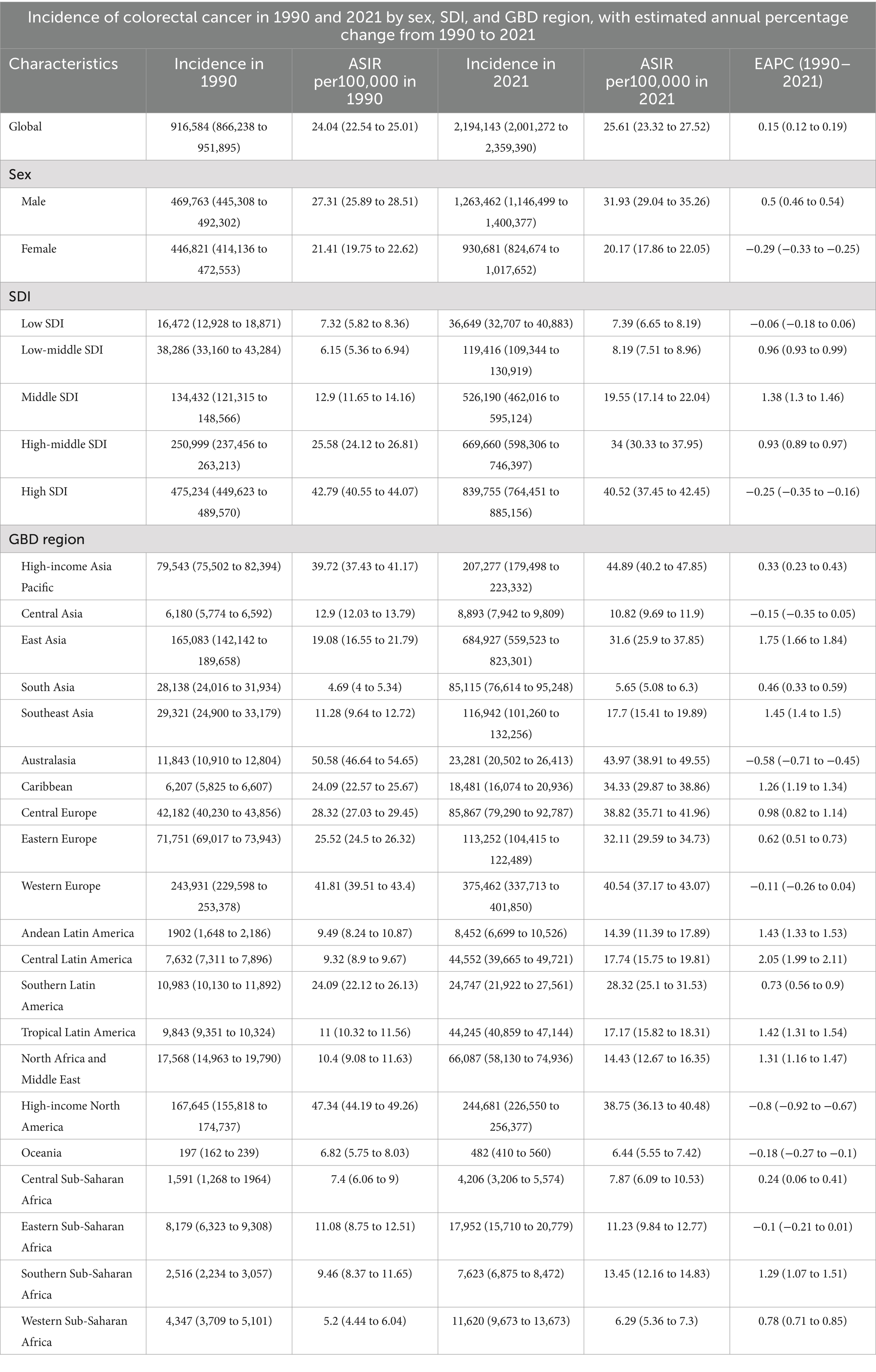
Table 1. Incidence of colorectal cancer in 1990 and 2021 by sex, SDI, and GBD region, with estimated annual percentage change from 1990 to 2021.
Metabolic risk factors accounted for 16.6% of the global CRC deaths burden in 2021, of which high BMI and high fasting glucose were the main contributors, accounting for 9.5 and 7.9%, respectively. This represents a significant increase compared to 1990, indicating that metabolic risk factors, specifically high BMI, have become important contributors to CRC risk (Supplementary Figure S1A). The CRC DALYs burden attributable to metabolic risk factors mirrored the same pattern of the burden of deaths (Supplementary Figure S1B). In 2021, the CRC burden of deaths and DALYs attributable to metabolic risk factors was higher in high SDI, at 18.9 and 19.1%, with the most prominent contribution from high BMI, at 10.9 and 11.6% (Supplementary Figures S1A,B). Within the GBD region, high-income North America had the highest burden, with high BMI also playing a significant role (Supplementary Figures S1A,B). These findings clearly indicate that high BMI is the most important risk factor among the metabolic risks associated with CRC.
Over the past 32 years, the number of deaths due to CRC associated with high BMI has rapidly increased from 41,536 (95% UI: 17,666–67,379) in 1990 to 99,268 (95% UI: 42,956–157,949) in 2021, an increase of 139%. Meanwhile, ASMR has also increased, but the change is non-significant, rising from 1.14 per 100,000 population (95% UI: 0.48–1.86) in 1990 to 1.17 per 100,000 population (95% UI: 0.51–1.87) in 2021. The EAPC of ASMR was 0 (95% UI: −0.04 to 0.04), revealing a relatively stable trend (Table 2). From 1990 to 2021, the number of deaths from high BMI-related CRC increased significantly in men and women. The number of deaths among women was higher than that of men from 1990 to 2008; however, after 2008, the number of deaths among men surpassed that of women. Moreover, the ASMR in men has always been higher than that in women (Figure 1C). Although the number of deaths for men and women increased over the past 32 years, the ASMR for women revealed a significant downward trend (EAPC = −0.37, 95% CI: −0.42 to −0.31), while the ASMR for men depicted an upward trend (EAPC = 0.39, 95% CI: 0.36–0.42) (Table 2; Figure 1C).
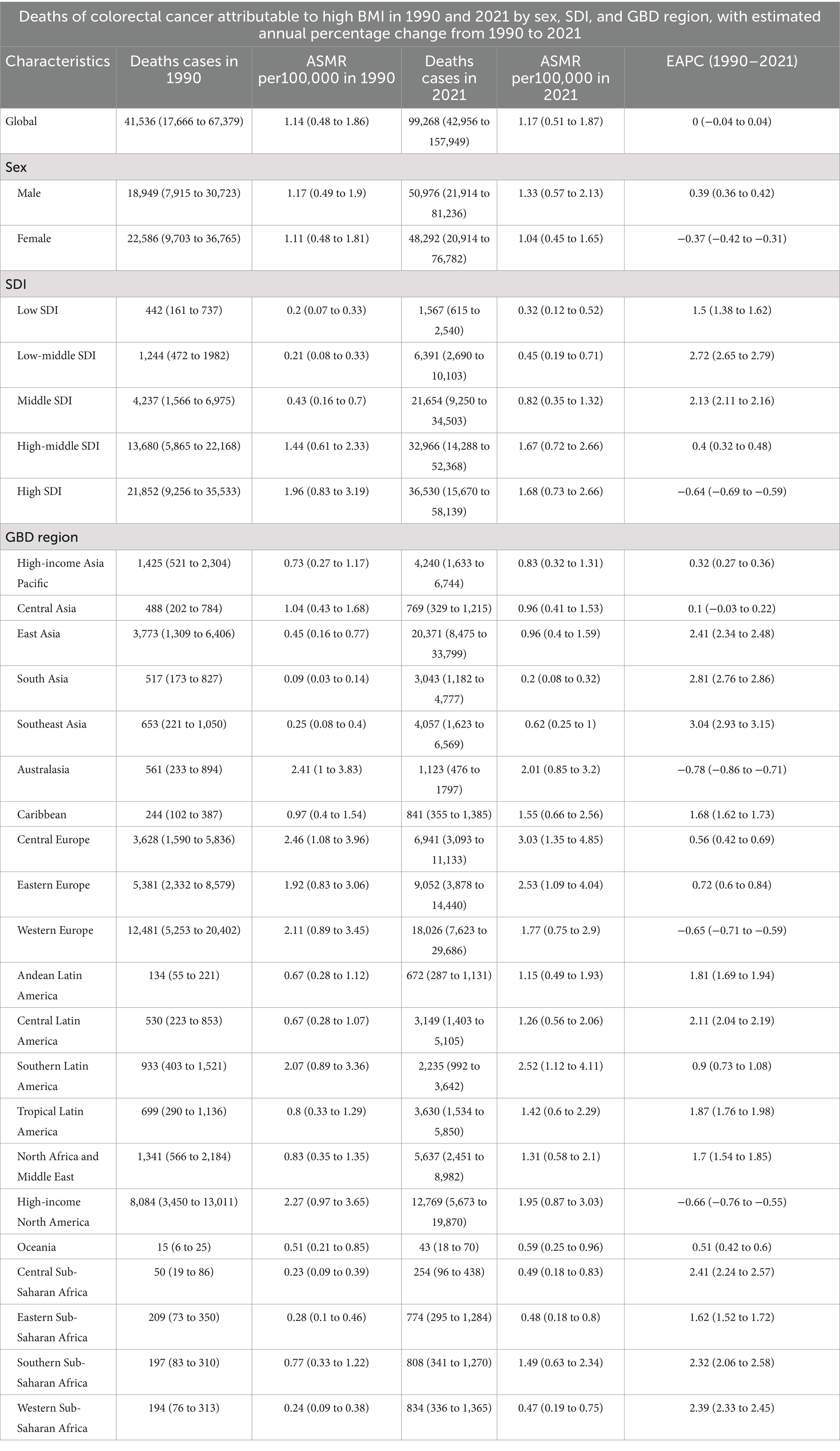
Table 2. Deaths of colorectal cancer attributable to high BMI in 1990 and 2021 by sex, SDI, and GBD region, with estimated annual percentage change from 1990 to 2021.

Figure 1. ASMR (A) and ASDR (B) for colorectal cancer attributable to high BMI by 5 SDI regions; the global number of deaths and ASMR for colorectal cancer attributable to high BMI by sex (C). The global number of DALYs and ASDR for colorectal cancer attributable to high BMI by sex (D); ASMR, age-standardized mortality rate; DALYs, disability-adjusted life-years; ASDR, age-standardized DALYs rate; SDI, sociodemographic index; BMI, body-mass index.
Significant differences in the burden of CRC were caused by high BMI in regions with different SDI levels. In 2021, the high SDI regions had the highest number of deaths from high BMI-related CRC, with 36,530 (95% UI: 15,670–58,139), accounting for more than 35% of global cases (Table 2). Although the ASMR in high SDI regions decreased from 1.96 per 100,000 population (95% UI: 0.83–3.19) in 1990 to 1.68 per 100,000 population (95% UI: 0.73–2.66) in 2021, it was still significantly higher than that in other SDI regions. Over the past 32 years, the ASMR in low, low-middle, middle, and high-middle SDI regions revealed an upward trend, with the most significant increase in low-middle SDI regions (EAPC = 2.72, 95% CI: 2.65–2.79). Conversely, the ASMR in the high SDI regions significantly decreased (EAPC = −0.64, 95% CI: −0.69 to −0.59) (Table 2; Figure 1A).
At the GBD regional level, in 2021, East Asia had the highest number of deaths from high BMI-related CRC, with 20,371 (95% UI: 8,475–33,799), followed by Western Europe, with 18,026 (95% UI: 7,623–29,686). Central Europe had the highest ASMR, at 3.03 per 100,000 population (95% UI: 1.35–4.85). From 1990 to 2021, Southeast Asia had the most significant increase in ASMR (EAPC = 3.04, 95% CI: 2.93–3.15). Furthermore, Australasia experienced the largest decrease in ASMR (EAPC = −0.78, 95% CI: −0.86 to −0.71) (Table 2).
At the national level, in 2021, China had the highest number of deaths from CRC due to high BMI, with 19,418 (95% UI: 8,053–32,452), followed by the United States, with 11,402 (95% UI: 5,070–17,661). Kuwait had the largest increase in the number of deaths, with a 974.3% rise over 32 years. Among the 204 countries, only Austria saw a decrease in the number of deaths (Supplementary Table S1; Figure 2C). Hungary had the highest ASMR, at 3.79 per 100,000 population (95% UI: 1.72–6.19), followed by Slovakia and Uruguay, with ASMRs of 3.53 per 100,000 population (95% UI: 1.61–5.66) and 3.45 per 100,000 population (95% UI: 1.54–5.72), respectively (Supplementary Table S1; Figure 2A). Moreover, since 1990, Vietnam has experienced the most significant increase in ASMR (EAPC = 4.65, 95% CI: 4.49–4.81). Meanwhile, 30 countries revealed a downward trend in ASMR, with Austria experiencing the most significant decrease (EAPC = −1.86, 95% CI: −1.92 to −1.8) (Supplementary Table S1; Figure 2E).
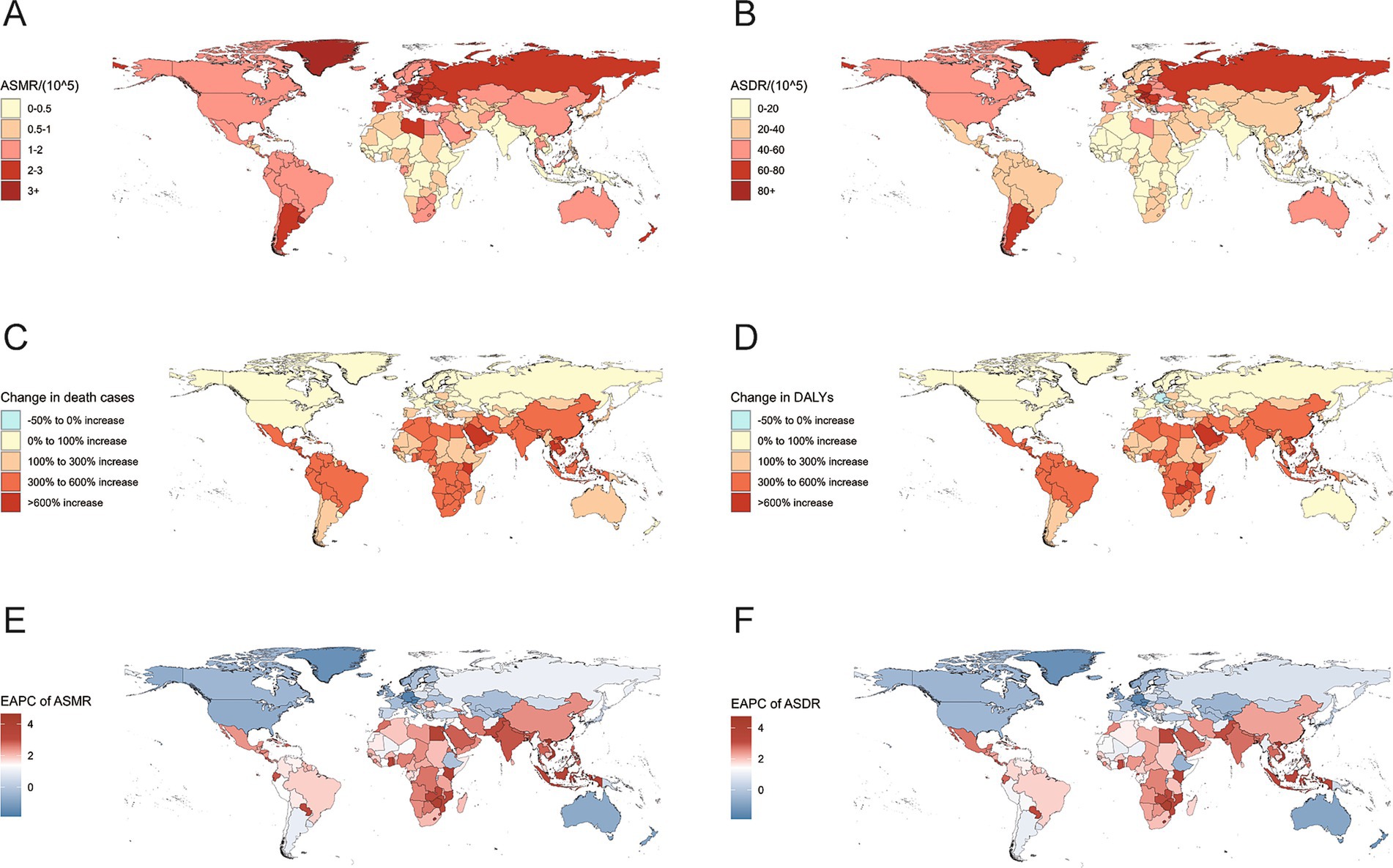
Figure 2. ASMR (A) and ASDR (B) for colorectal cancer attributable to high BMI in 204 countries in 2021; the percentage change in the number of deaths (C) and DALYs (D) for colorectal cancer attributable to high BMI from 1990 to 2021. The EAPC of the ASMR (E) and ASDR (F) for colorectal cancer attributable to high BMI from 1990 to 2021; ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; DALYs, disability-adjusted life-years; BMI, body-mass index; EAPC, estimated annual percentage change.
From 1990 to 2021, the number of DALYs due to high BMI-related CRC increased from 1,015,042 (95% UI: 429,787–1,631,974) in 1990 to 2,364,664 (95% UI: 1,021,594–3,752,340) in 2021 globally, an increase of 133%. The ASDR also rose from 25.54 per 100,000 population (95% UI: 10.83–41.2) in 1990 to 27.33 per 100,000 population (95% UI: 11.8–43.37) in 2021, with an EAPC of 0.12 (95% CI: 0.08–0.16) (Table 3). The trend of DALYs due to high BMI-related CRC in both men and women was similar to the trend in mortality. In 1990, the number of DALYs in women was higher than in men, but by 1999, the number of DALYs in men surpassed that in women, and the gap continued to widen (Figure 1D). Additionally, the ASDR for men increased from 26.42 per 100,000 population (95% UI: 10.97–42.88) in 1990 to 31.09 per 100,000 population (95% UI: 13.36–49.47) in 2021, revealing a significant upward trend (EAPC = 0.48, 95% CI: 0.45–0.51). In contrast, the ASDR for women decreased from 24.73 per 100,000 population (95% UI: 10.59–39.99) in 1990 to 23.96 per 100,000 population (95% UI: 10.36–37.75) in 2021, exhibiting a significant downward trend (EAPC = −0.26, 95% CI: −0.31 to −0.2) (Table 3; Figure 1D).

Table 3. DALYs of colorectal cancer attributable to high BMI in 1990 and 2021 by sex, SDI, and GBD region, with estimated annual percentage change from 1990 to 2021.
In terms of SDI, from 1990 to 2021, the number of DALYs and ASDR due to high BMI-related CRC in high SDI regions has always been the highest. However, the ASDR in high SDI regions decreased from 44.94 per 100,000 population (95% UI: 19.27–72.19) in 1990 to 40 per 100,000 population (95% UI: 17.48–62.93) in 2021, with an EAPC of −0.48 (95% CI: −0.52 to −0.43). This is the only SDI region where the ASDR exhibited a downward trend. The ASDR in other SDI regions revealed an upward trend, with the most significant increase in low-middle SDI regions (EAPC = 2.69, 95% CI: 2.63–2.76) (Table 3; Figure 1B).
For the GBD regions, in 2021, East Asia recorded the largest number of DALYs owing to high BMI-related CRC, with 529,352 cases (95% UI: 219,133–886,681). Central Europe had the most significant ASDR at 68.94 per 100,000 population (95% UI: 30.82–110.6). Over the past 32 years, 17 out of 21 GBD regions revealed an upward trend in ASDR, with Southeast Asia experiencing the most notable increase (EAPC = 2.84, 95% UI: 2.72–2.97). Conversely, Western Europe, high-income North America, Central Asia, and Australasia exhibited a downward trend in ASDR, with Australasia having the most pronounced decrease (EAPC = −0.94, 95% CI: −1.02 to −0.85) (Table 3).
From a national perspective, in 2021, China had the highest number of DALYs due to high BMI-related CRC, with 507,316 (95% UI: 209,264–853,770). From 1990 to 2021, among 204 countries, the number of DALYs increased rapidly in most countries, while only Austria, Germany, and the Czech Republic observed a decrease in DALYs, with reductions of 13.9, 5.6 and 4.8%, respectively (Supplementary Table S2; Figure 2D). Hungary exhibited the highest ASDR, at 92.03 per 100,000 population (95% UI: 41.88–149.98), followed by Slovakia, at 82.15 per 100,000 population (95% UI: 37.4–131.78) (Supplementary Table S2; Figure 2B). Notably, more than half of the countries have seen an increase in the ASDR EAPC. Vietnam (EAPC = 4.74, 95% CI: 4.54–4.94), Lesotho (EAPC = 4.7, 95% CI: 4.15–5.25), and Zimbabwe (EAPC = 4.11, 95% CI: 3.45–4.78) had the largest increases, which may indicate severe health challenges in these countries. Conversely, the ASDR in a few countries, such as the Czech Republic (EAPC = −1.81, 95% CI: −1.99 to −1.63) and Germany (EAPC = −1.65, 95% CI: −1.77 to −1.54), exhibited the most significant decrease (Supplementary Table S2; Figure 2F).
In 2021, the total number of deaths due to high BMI-related CRC increased for both men and women, with male deaths reaching 50,976 and female deaths reaching 48,292 (Table 2). The number of deaths for men and women exhibited a synchronous pattern, first increasing and then decreasing with age, peaking at 70–74 years. However, male deaths were not always higher than female deaths. Before the age of 80–84 years, male deaths were significantly higher than female deaths, but this trend reversed after the age of 80–84 years (Figure 3A). The trend in mortality rates was similar, with age-specific mortality rates in men and women increasing with age. Female mortality rates significantly exceeded male rates at ages 95+, whereas male mortality rates were higher than female rates before this age range (Figure 4A). The age-specific trend for DALYs was similar to that for mortality, but the peak number of DALYs occurred in the 65–69 age group (Table 3; Figure 3B). The age-specific DALY rates for men and women increased significantly with age, but the DALY rate for men began to decline after 90–94 years of age (Figure 4B). Globally, from 1990 to 2021, age-specific mortality rates for men and women in the 20–49 and 95+ age groups increased, with the 25–29 age group experiencing the fastest growth in mortality rates. Among men, from 1990 to 2021, mortality rates increased across almost all age groups, with the 25–29 age group exhibiting the most significant increase. In contrast, among women, mortality rates decreased in the 50–94 years age group, with the 65–69 years age group revealing the most significant decrease (Figure 4C).
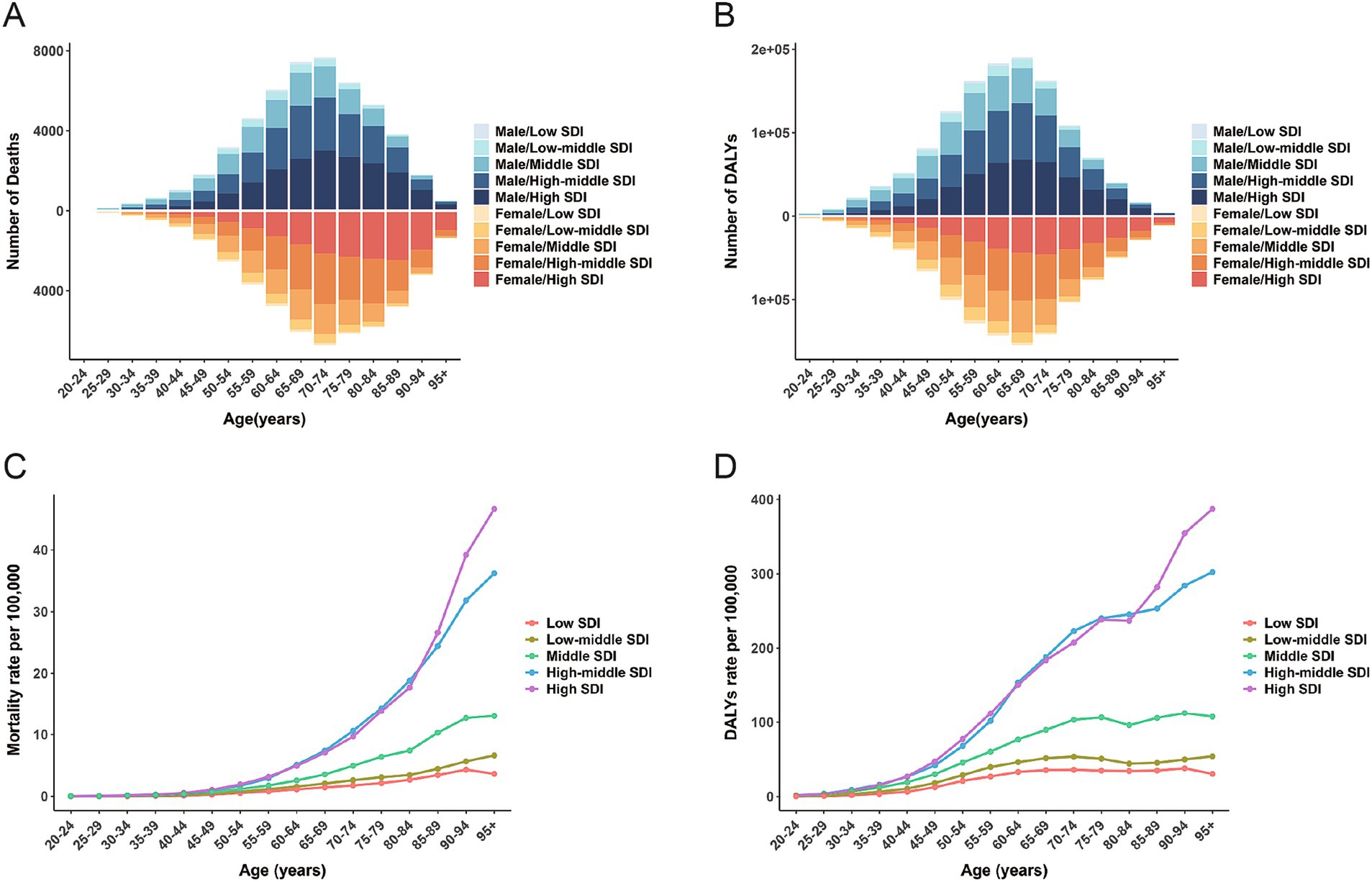
Figure 3. The global number of deaths (A) and DALYs (B) for colorectal cancer attributable to high BMI across age groups by sex and 5 SDI regions in 2021; The mortality rate (C) and DALYs rate (D) for colorectal cancer attributable to high BMI across age groups by 5 SDI regions in 2021; DALYs, disability-adjusted life-years; SDI, sociodemographic index; BMI, body-mass index.
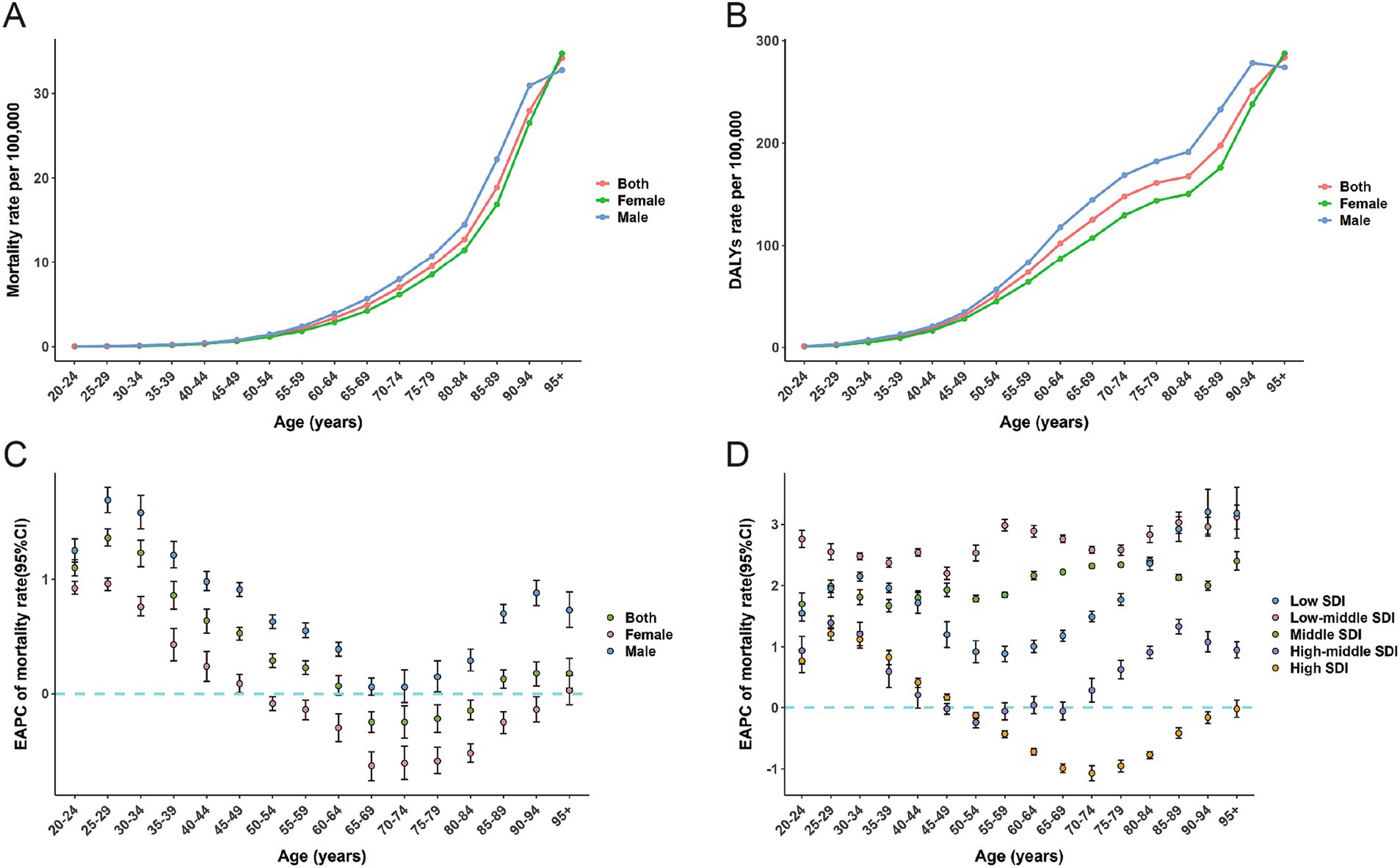
Figure 4. The mortality rate (A) and DALYs rate (B) for colorectal cancer attributable to high BMI across age groups by sex in 2021; EAPC of the mortality rate for colorectal cancer attributable to high BMI across age groups by sex from 1990-2021 (C); EAPC of the mortality rate for colorectal cancer attributable to high BMI across age groups by 5 SDI from 1990-2021 (D); DALYs, disability-adjusted life-years; SDI, sociodemographic index; BMI, body-mass index; EAPC, estimated annual percentage change.
In 2021, across the five SDI regions, age-specific mortality rates due to high BMI-related CRC generally increased with age. Age-specific mortality rates in high and middle-high SDI regions were significantly higher than in other regions (Figure 3C)The age-specific DALYs rate was similar to the mortality rate, with the difference that the DALYs rates in the high, middle, low-middle, and low SDI regions depicted a declining trend at ages 80–84 (Figure 3D). The peak age-specific mortality and DALY rates in most regions occurred after the age of 90. Similarly, from 1990 to 2021, the age-specific mortality rates in the low, low-middle, and middle SDI regions increased significantly across all age groups. Among the five SDI regions, the low-middle SDI regions had the largest increase in mortality rates, followed by the middle SDI regions (Figure 4D). In high SDI regions, age-specific mortality rates in the 50–94 age group decreased annually, with the 70–74 age group experiencing the largest decline. In high-middle SDI regions, only the 50–54 age group’s age-specific mortality rate decreased, while mortality rates in relatively younger and older age groups increased (Figure 4D).
Across the 21 GBD regions globally, from 1990 to 2021, the ASMR of high BMI-related CRC exhibited an inverted V-shaped nonlinear relationship with the SDI (ρ = 0.739, p < 0.001), peaking at an SDI of approximately 0.75. When SDI < 0.75, the ASMR increased gradually, whereas when SDI > 0.75, the ASMR declined rapidly (Figure 5A). A comparable relationship was also observed between the ASDR and SDI (Figure 5B). Among 204 countries worldwide, the ASMR of high BMI-related CRC in 1990 was significantly negatively correlated with EAPC from 1990 to 2021 (ρ = −0.693, p < 0.001) (Figure 6A), The ASDR in 1990 exhibited the same trend as the EAPC from 1990 to 2021 (ρ = −0.672, p < 0.001) (Figure 6B). The relationship between the EAPC of high BMI-related CRC and the SDI in 2021 exhibited an inverted “U” shape. When the SDI was below 0.5, a positive correlation was observed. When the SDI ≥ 0.5, both the EAPC of ASMR (ρ = −0.487, p < 0.001) and the EAPC of ASDR (ρ = −0.485, p < 0.001) were negatively correlated with the SDI (Figures 7A,B). The SDI for 204 countries from 1990 to 2021 are listed in Supplementary Table S3.
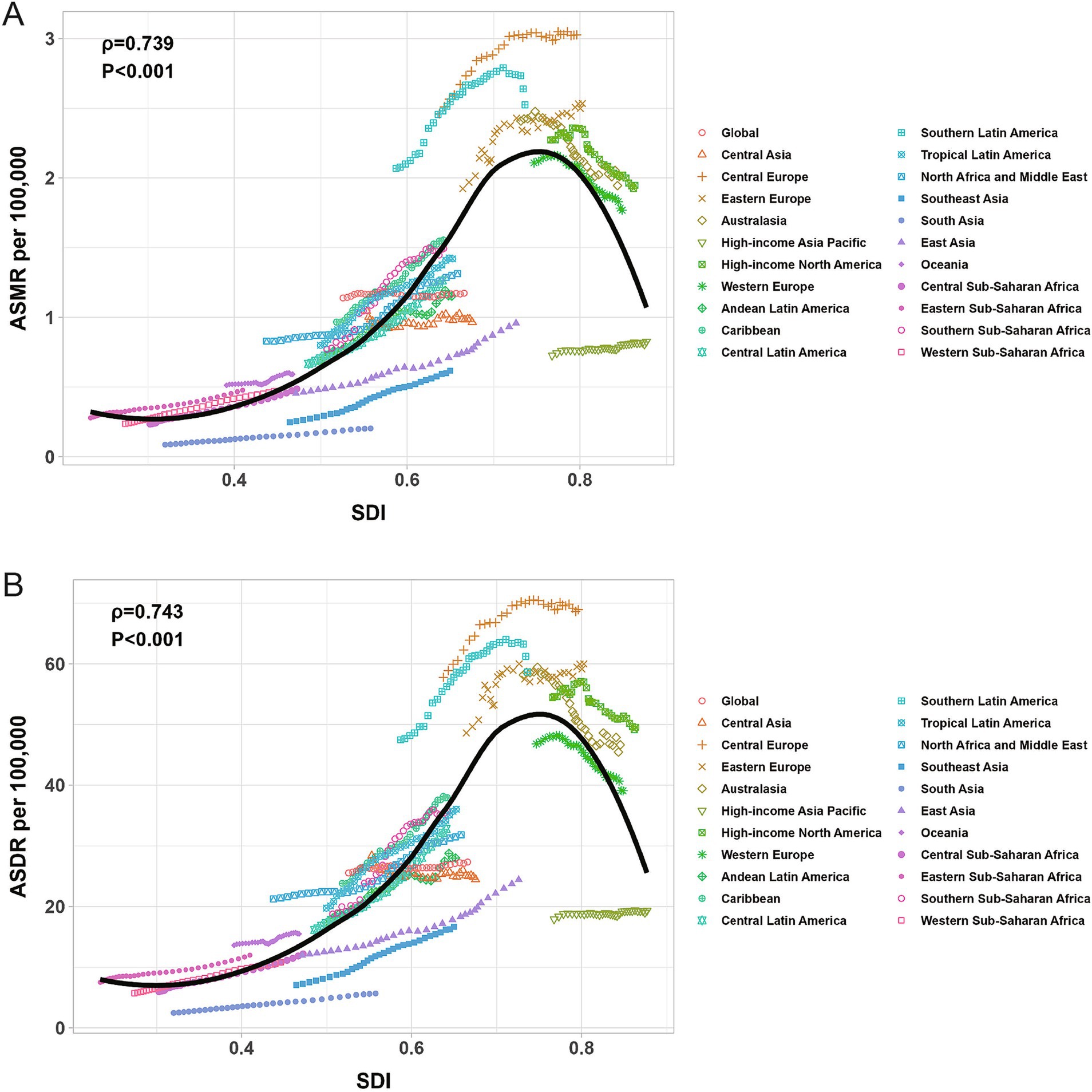
Figure 5. The correlation between ASMR for colorectal cancer attributable to high BMI and SDI (A); The correlation between ASDR for colorectal cancer attributable to high BMI and SDI (B); ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; SDI, sociodemographic index; BMI, body-mass index.
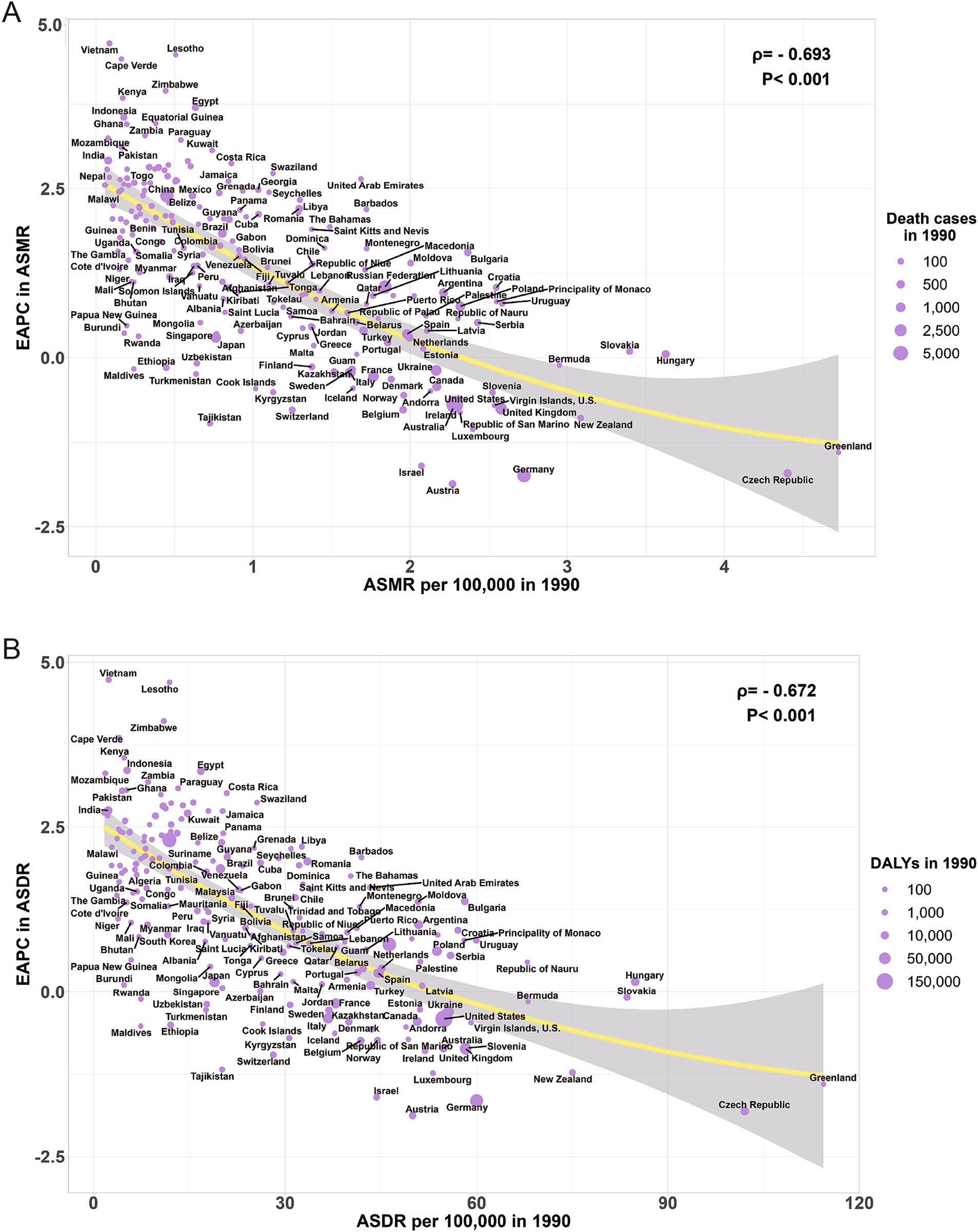
Figure 6. The correlation between ASMR for colorectal cancer attributable to high BMI in 1990 and EAPC of ASMR (A); The correlation between ASDR for colorectal cancer attributable to high BMI in 1990 and EAPC of ASDR (B); ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; BMI, body-mass index; EAPC, estimated annual percentage change.
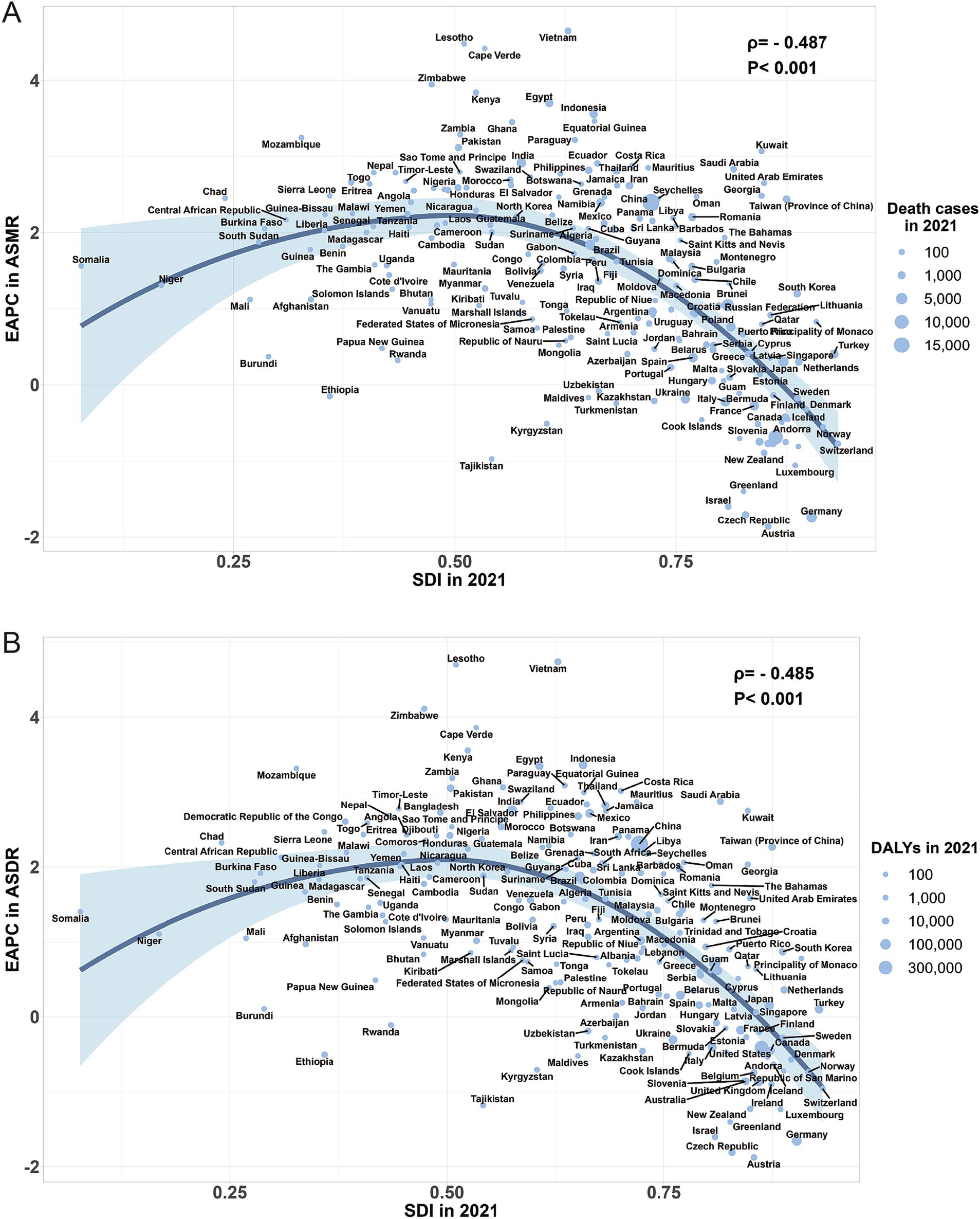
Figure 7. The correlation between the EAPC of ASMR for colorectal cancer attributable to high BMI and SDI in 2021 (A); The correlation between the EAPC of ASDR for colorectal cancer attributable to high BMI and SDI in 2021 (B); ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; SDI, sociodemographic index; BMI, body-mass index; EAPC, estimated annual percentage change.
According to the ARIMA model, from 2022 to 2035, the burden of high BMI-related CRC in males will continue to rise, with the ASMR increasing from 1.33 per 100,000 population (95% UI: 0.57–2.13) in 2021 to 1.4 per 100,000 population (95% UI: 1.33–1.47) in 2035, and the ASDR increasing from 31.09 per 100,000 population (95% UI: 13.36–49.47) in 2021 to 33.07 per 100,000 population (95% UI: 31.35–34.79) in 2035 (Table 4; Figures 8A,B). In females, both the ASMR and ASDR of high BMI-related CRC exhibited a slightly increasing trend and gradually stabilized (Table 4; Figures 8C,D).
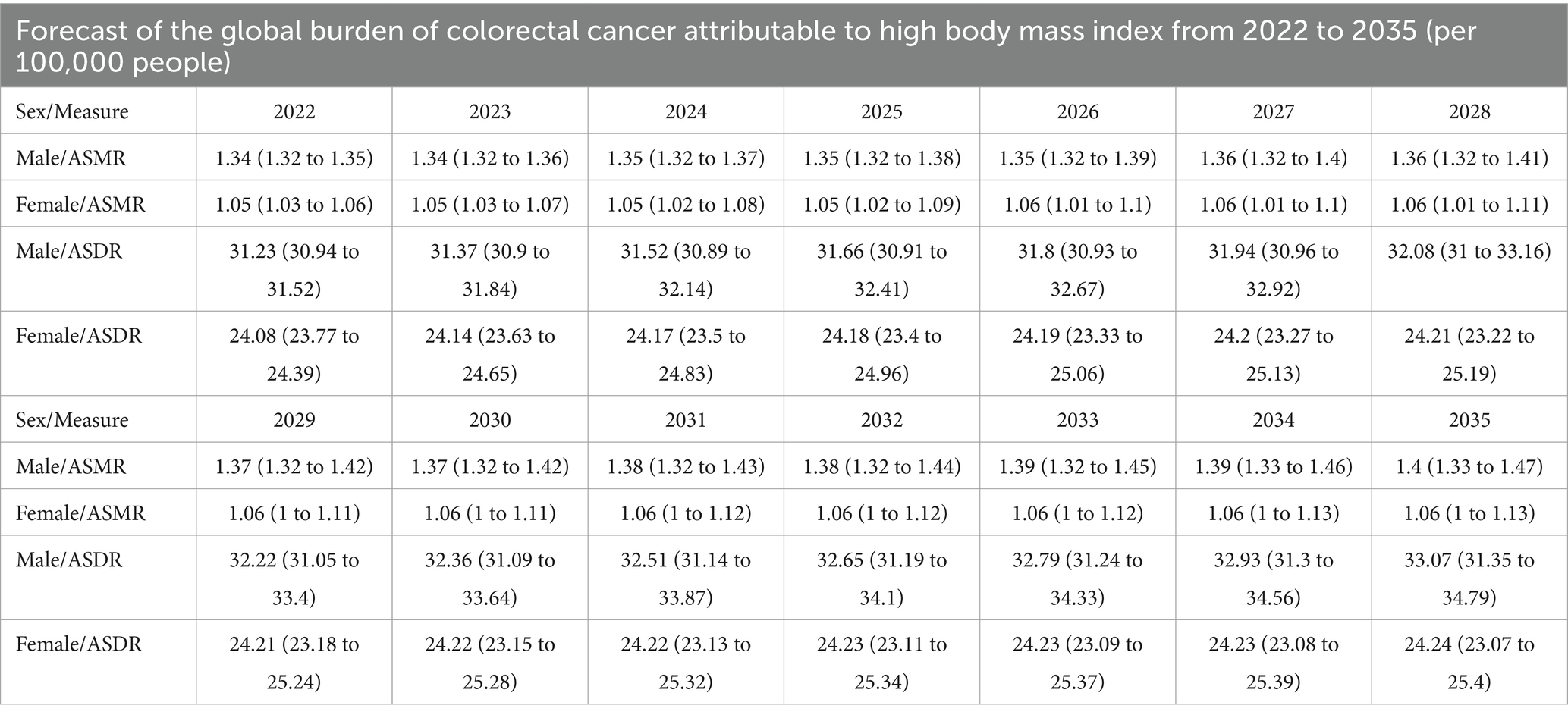
Table 4. Forecast of the global burden of colorectal cancer attributable to high body-mass index from 2022 to 2035 (per 100,000 people).
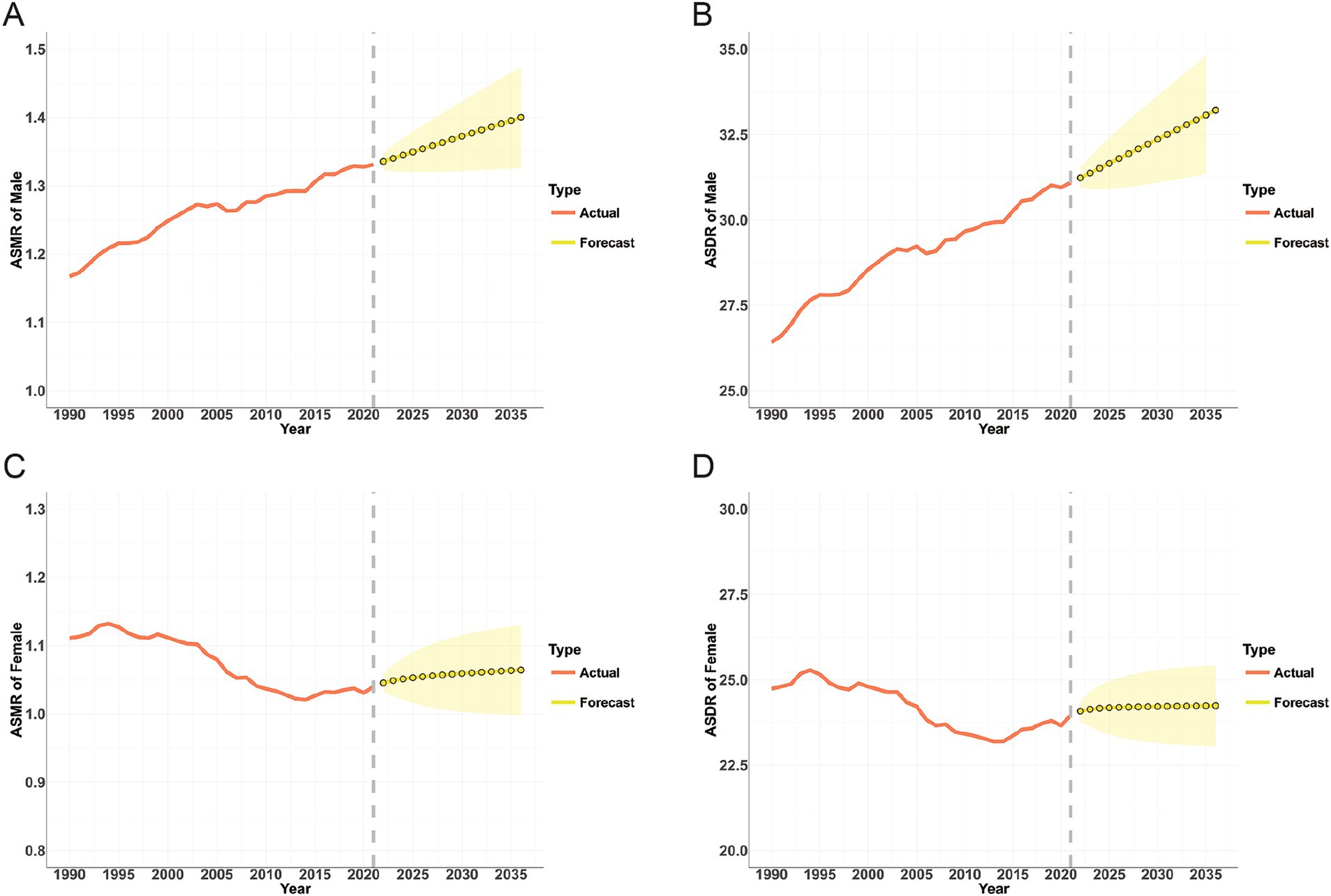
Figure 8. Projections of ASMR (A,C) and ASDR (B,D) for colorectal cancer attributable to high BMI in males and females from 2022 to 2035; The red line represents the actual value, and the fan represents the predicted distribution between the 2.5 and 97.5% quantiles. The forecast average is shown as a yellow dot. The vertical dotted line indicates where the prediction begins; ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; BMI, body-mass index.
In recent years, due to dietary and metabolic factors, as well as unhealthy habits such as smoking and drinking, the global incidence, mortality, and DALYs rates of CRC have been increasing annually and are expected to exceed 2,200,000 new and 1,100,000 deaths by 2030 (1, 4, 26). Interestingly, a high BMI has now surpassed smoking as a major risk factor for CRC, which cannot be ignored. In this study, we systematically analyzed the global burden of CRC caused by a high BMI from 1990 to 2021, stratified by age, gender, region, and SDI. Our results revealed that there are significant differences in the burden of CRC caused by high BMI across different regions and countries, as well as among different genders and age groups. However, it is worth noting that although the number of deaths and DALYs for men and women more than doubled in 2021, after age standardization, the ASMR and ASDR for men have increased significantly over the past 32 years, while for women, they have decreased significantly. The burden of high BMI-related CRC is significantly higher in men than in women, and this gap is widening annually. This may be because women’s lifestyles are healthier compared to men, and women have much higher levels of estrogen than men. Studies have demonstrated that the expression of estrogen receptor β (ERβ/ESR2) is negatively correlated with the presence of colorectal polyps and tumor staging, which can reduce the risk of death in women (27, 28).
Furthermore, compared to men of the same age, women aged ≥80 years had higher mortality and DALYs related to high BMI-associated CRC. Several perspectives have supported this phenomenon. First, women tend to live longer than men do, leading to a higher proportion of elderly women in the population. Second, differences in body composition also play a role; as age increases, men tend to have a higher proportion of lean muscle mass and strength, while women have more body fat and experience faster muscle function decline compared to elderly men. These factors contribute to an increased risk of BMI-related CRC in elderly women (29, 30).
In 2021, according to the GBD 2021, there were 99,268 deaths worldwide, of which 86,308 were elderly people aged 55 years and above, accounting for nearly 87%, indicating that the burden of high BMI-related CRC is mainly concentrated in the elderly. Population growth and aging are likely to be the main causes of this phenomenon. Elderly individuals may be more susceptible to the adverse effects of high BMI, including altered glucose metabolism and insulin resistance, which increases the risk of chronic diseases (31). Furthermore, this burden is closely related to socioeconomic development and unequal distribution. While the burden of CRC caused by high BMI is higher in regions with higher SDI levels, with more than two-thirds of the deaths occurring in high SDI and high-middle SDI regions, the growth rates of ASMR and ASDR in these regions have slowed or even declined in recent years. For instance, the ASMR and ASDR in Australasia and High-income North America have significantly decreased. Contrarily, in low, low-middle, and middle SDI regions, such as South Asia and Central Sub-Saharan Africa, although the baseline burden of CRC caused by high BMI is relatively low, the number and rate of deaths and DALYs have increased significantly and may not stop growing for some time. One possible explanation is that countries with a high SDI are more likely to implement routine and early CRC screening, a mature intervention measure to reduce CRC mortality risk (32, 33). Moreover, regions with higher SDI are often more accessible to health education and awareness programs. People in these regions may be more aware of the risks of obesity and adopt healthier lifestyles and behaviors (34). In contrast, people in lower economic regions may experience greater stress due to economic difficulties and limited access to healthcare, which can lead to increased BMI and unhealthy eating habits, including high intake of energy-dense and low-nutrient foods, while reducing physical activity levels, ultimately leading to obesity (35), Consequently, countries worldwide should recognize that high BMI will eventually result in higher health burdens and take timely targeted measures, such as strengthening health education, promoting healthy weight maintenance, and encouraging active participation in physical exercise to mitigate the burden of CRC caused by high BMI.
Our research found that from 1990 to 2021, among the 21 GBD regions, although Central Europe had the highest ASMR and ASDR of high BMI-related CRC, its EAPC was much lower than that of South Asia, Southeast Asia, and East Asia. Several explanations exist for this phenomenon. First, urbanization has brought about significant lifestyle changes, with reduced physical activity, more sedentary work, and reliance on motor vehicles for transportation, leading to decreased daily activity levels. These changes increase the risk of obesity (36, 37). Second, East Asian and Southeast Asian countries are undergoing a “nutrition transition”; the deeper the transition, the higher the incidence of overweight. Traditional low-fat diets typically feature complex carbohydrates, fresh fish, meat, and leafy vegetables, which can reduce the prevalence of metabolic syndrome and increase high-density lipoprotein cholesterol levels. These have gradually shifted to modern low-nutrition, high-calorie diets, including refined starches, oils, sugars, and processed meat. This significant dietary shift has greatly increased the burden of high BMI-related CRC in these regions (38, 39).
We also found that in 1990, the higher the baseline burden of ASMR and ASDR, the lower the EAPC, exhibiting a significant negative correlation. Most countries with high baseline burdens in 1990 were developed countries, such as the United States, the United Kingdom, and Australia. They could adopt various methods, such as health education, early screening, and early intervention, to reduce the disease burden of high BMI-related CRC. Conversely, countries with low baseline burdens, such as China and India, are mostly developing countries that have experienced rapid economic development and increasingly Westernized lifestyles over the past 30 years. The increase in obesity and decrease in physical activity owing to Westernized lifestyles are important reasons for the rapid increase in CRC incidence and mortality caused by high BMI in these countries (40). In countries with a higher SDI (> 0.5) in 2021, the decline rates of ASMR and ASDR were also faster, and the EAPC revealed an inverted U-shaped relationship with SDI. In countries with a lower SDI (< 0.5), ASMR and ASDR continued to rise. The burden of BMI-related CRC varies significantly across regions and countries, and prevention and treatment strategies should be formulated based on the specific conditions in each region and country. Developing countries can take measures to help residents establish healthy lifestyles, such as actively promoting healthy diets and physical activity to avoid the increased burden of CRC caused by Westernized lifestyles. Developed countries need to take more targeted measures to reduce the prevalence of obesity and low physical activity while continuing early screening and diagnosis.
Our study has some advantages. First, our study discusses in detail the geographical and temporal trends in the global CRC burden caused by high BMI and its influencing factors, which may serve as a reference for establishing interventions to address this challenge and monitor their effectiveness. Second, our study proposes practical strategies aimed at reducing the burden on particularly affected age groups, genders, regions, and countries. Finally, our study uses the ARIMA model (a powerful time-series forecasting tool) to predict the global CRC burden related to high BMI from 2020 to 2035, enhancing our insights into future trends. However, this study has some limitations. First, the accuracy and robustness of the GBD study estimates depend on the quality and quantity of source data. Although GBD 2021 uses many strategies to improve data quality and comparability, bias is inevitable, which may affect the completeness and accuracy of the analyzed data (41). Second, BMI is an imperfect measure of obesity because individuals with high muscle mass may exhibit elevated BMI without associated health risks. An ideal measure of obesity should include waist circumference, body fat composition, and other factors, such as the muscle-to-fat ratio and metabolic health markers (34). Therefore, using BMI classification cut-off values may misestimate the impact of high BMI on CRC in specific populations. Finally, differences in the quality and quantity of data sources, etiological assessments, and diagnostic accuracy of CRC across regions may lead to heterogeneity (42).
In summary, current research indicates that the global burden of CRC caused by high BMI has persisted over the past 30 years and may increase in the future, particularly in countries with a lower SDI. These increasing challenges compel us to formulate targeted public health interventions and policies. Besides, according to our predictions, global ASMR and ASDR may exhibit an upward trend between 2022 and 2035. We hope that our study can provide policymakers with insights into formulating disease control and prevention strategies tailored to the specific conditions of different countries, particularly those with relatively low SDI, according to their socioeconomic conditions.
Publicly available datasets were analyzed in this study. This data can be found at: http://ghdx.healthdata.org/gbd-results-tool.
XJ: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. DD: Conceptualization, Project administration, Supervision, Writing – original draft, Writing – review & editing. ZX: Investigation, Supervision, Writing – review & editing. MS: Investigation, Methodology, Visualization, Writing – original draft.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China project (82170536).
We appreciate the works by the Global Burden of Disease study 2021 collaborators. We would like to thank Weixue Huo (UmlkZ2V3YXlfSHVvQDEyNi5jb20=) for his outstanding work.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1473851/full#supplementary-material
SUPPLEMENTARY FIGURE S1 | Population attributable fraction of colorectal cancer deaths attributable to high BMI by 5 SDI areas and 21 GBD regions in 1990 and 2021 (A); Population attributable fraction of colorectal cancer DALYs attributable to high BMI by 5 SDI areas and 21 GBD regions in 1990 and 2021 (B); BMI, body-mass index; SDI, sociodemographic index; DALYs, disability-adjusted life-years.
1. Liu, Y, Zhang, CA-O, Wang, Q, Wu, K, Sun, Z, Tang, Z, et al. Temporal trends in the disease burden of colorectal cancer with its risk factors at the global and national level from 1990 to 2019, and projections until 2044. Clin Epidemiol. (2023) 15:55–71. doi: 10.2147/CLEP.S388323
2. Sung, HA-O, Ferlay, J, Siegel, RA-O, Laversanne, M, Soerjomataram, I, Jemal, A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71:209–49. doi: 10.3322/caac.21660
3. GBD 2019 Colorectal Cancer Collaborators . Global, regional, and national burden of colorectal cancer and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. (2022) 7:627–47. doi: 10.1016/S2468-1253(22)00044-9
4. Arnold, M, Sierra, MS, Laversanne, M, Soerjomataram, I, Jemal, A, and Bray, F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. (2017) 66:683–91. doi: 10.1136/gutjnl-2015-310912
5. Liang, Y, Zhang, NA-O, Wang, M, Liu, Y, Ma, L, Wang, Q, et al. Distributions and Trends of the Global Burden of Colorectal Cancer Attributable to Dietary Risk Factors over the Past 30 Years. Nutrients. (2023) 16:132. doi: 10.3390/nu16010132
6. WHO Expert Consultation . Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. (2004) 363:157–63. doi: 10.1016/S0140-6736(03)15268-3
7. Bouras, EA-O, Gill, DA-O, Zuber, VA-O, Murphy, NA-O, Dimou, N, Aleksandrova, KA-O, et al. Identification of potential mediators of the relationship between body mass index and colorectal cancer: a Mendelian randomization analysis. Int J Epidemiol. (2024) 53:dyae067. doi: 10.1093/ije/dyae067
8. Tan, DJH, Ng, CH, Muthiah, M, Yong, JN, Chee, D, Teng, M, et al. Rising global burden of cancer attributable to high BMI from 2010 to 2019. Metabolism. (2024) 152:155744. doi: 10.1016/j.metabol.2023.155744
9. Xing, QQ, Li, JM, Chen, ZJ, Lin, XY, You, YY, Hong, MZ, et al. Global burden of common cancers attributable to metabolic risks from 1990 to 2019. Med. (2023) 4:168–181.e3. doi: 10.1016/j.medj.2023.02.002
10. Alemán, JO, Eusebi, LH, Ricciardiello, L, Patidar, K, Sanyal, AJ, and Holt, PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. (2014) 146:357–73. doi: 10.1053/j.gastro.2013.11.051
11. Taguri, MA-O, Kuchiba, AA-O, Yamaji, TA-O, Sawada, NA-O, Goto, AA-OX, Iwasaki, MA-O, et al. Importance of circulating leptin and adiponectin in the causal pathways between obesity and the development of colorectal cancer in Japanese men. J Epidemiol. (2024). doi: 10.2188/jea.JE20230148
12. Huang, Y, Huang, X, Wang, Z, He, F, Huang, Z, Chen, C, et al. Analysis of differences in intestinal flora associated with different BMI status in colorectal cancer patients. J Transl Med. (2024) 22:142. doi: 10.1186/s12967-024-04903-7
13. Wang, SY, Zhang, WS, Jiang, CQ, Jin, YL, Zhu, T, Zhu, F, et al. Association of novel and conventional obesity indices with colorectal cancer risk in older Chinese: a 14-year follow-up of the Guangzhou Biobank Cohort Study. BMC Cancer. (2023) 23:286. doi: 10.1186/s12885-023-10762-0
14. Abar, L, Vieira, AR, Aune, D, Sobiecki, JG, Vingeliene, S, Polemiti, E, et al. Height and body fatness and colorectal cancer risk: an update of the WCRF-AICR systematic review of published prospective studies. Eur J Nutr. (2018) 57:1701–20. doi: 10.1007/s00394-017-1557-1
15. Kim, YE, Jung, YS, Ock, M, and Yoon, SJ. DALY estimation approaches: understanding and using the incidence-based approach and the prevalence-based approach. J Prev Med Public Health. (2022) 55:10–8. doi: 10.3961/jpmph.21.597
16. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
17. Murray, CA-O. The Global Burden of Disease Study at 30 years. Nat Med. (2022) 28:2019–26. doi: 10.1038/s41591-022-01990-1
18. GBD 2019 Demographics Collaborators . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1160–203. doi: 10.1016/S0140-6736(20)30977-6
19. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1223–49. doi: 10.1016/S0140-6736(20)30752-2
20. Hankey, BF, Ries, LA, Kosary, CL, Feuer, EJ, Merrill, RM, Clegg, LX, et al. Partitioning linear trends in age-adjusted rates. Cancer Causes Control. (2000) 11:31–5. doi: 10.1023/A:1008953201688
21. Zhou, L, Deng, Y, Li, N, Zheng, Y, Tian, T, Zhai, Z, et al. Global, regional, and national burden of Hodgkin lymphoma from 1990 to 2017: estimates from the 2017 Global Burden of Disease study. J Hematol Oncol. (2019) 12:107. doi: 10.1186/s13045-019-0799-1
22. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
23. GBD 2017 Causes of Death Collaborators . Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
24. Wei, J, Chen, L, Huang, S, Li, Y, Zheng, J, Cheng, Z, et al. Time Trends in the Incidence of Spinal Pain in China, 1990 to 2019 and Its Prediction to 2030: The Global Burden of Disease Study 2019. Pain Ther. (2022) 11:1245–66. doi: 10.1007/s40122-022-00422-9
25. Chaurasia, V, and Pal, SA-O. COVID-19 pandemic: ARIMA and regression model-based worldwide death cases predictions. SN Comput Sci. (2020) 1:288. doi: 10.1007/s42979-020-00298-6
27. Conti, L, Del Cornò, M, and Gessani, S. Revisiting the impact of lifestyle on colorectal cancer risk in a gender perspective. Crit Rev Oncol Hematol. (2020) 145:102834. doi: 10.1016/j.critrevonc.2019.102834
28. Williams, C, DiLeo, A, Niv, Y, and Gustafsson, J. Estrogen receptor beta as target for colorectal cancer prevention. Cancer Lett. (2016) 372:48–56. doi: 10.1016/j.canlet.2015.12.009
29. Kim, S, and Won, CW. Sex-different changes of body composition in aging: a systemic review. Arch Gerontol Geriatr. (2022) 102:104711. doi: 10.1016/j.archger.2022.104711
30. Bouchard, DR, Héroux, M, and Janssen, I. Association between muscle mass, leg strength, and fat mass with physical function in older adults: influence of age and sex. J Aging Health. (2011) 23:313–28. doi: 10.1177/0898264310388562
31. Chia, CW, Egan, JM, and Ferrucci, L. Age-related changes in glucose metabolism, hyperglycemia, and cardiovascular risk. Circ Res. (2018) 123:886–904. doi: 10.1161/CIRCRESAHA.118.312806
32. Meester, RG, Doubeni, CA, Lansdorp-Vogelaar, I, Goede, SL, Levin, TR, Quinn, VP, et al. Colorectal cancer deaths attributable to nonuse of screening in the United States. Ann Epidemiol. (2015) 25:208–213.e1. doi: 10.1016/j.annepidem.2014.11.011
33. Doubeni, CA, Fedewa, SA, Levin, TR, Jensen, CD, Saia, C, Zebrowski, AM, et al. Modifiable failures in the colorectal cancer screening process and their association with risk of death. Gastroenterology. (2019) 156:63–74.e6. doi: 10.1053/j.gastro.2018.09.040
34. Chen, Y, Ma, L, Han, Z, and Xiong, PA-O. The global burden of disease attributable to high body mass index in 204 countries and territories: Findings from 1990 to 2019 and predictions to 2035. Diabetes Obes Metab. (2024) 26:3998–4010. doi: 10.1111/dom.15748
35. Cotter, EW, and Kelly, NR. Stress-related eating, mindfulness, and obesity. Health Psychol. (2018) 37:516–25. doi: 10.1037/hea0000614
36. Lee, SA, Wen, W, Xu, WH, Zheng, W, Li, H, Yang, G, et al. Prevalence of obesity and correlations with lifestyle and dietary factors in Chinese men. Obesity (Silver Spring). (2008) 16:1440–7. doi: 10.1038/oby.2008.58
37. Tham, KW, Abdul Ghani, R, Cua, SC, Deerochanawong, C, Fojas, M, Hocking, S, et al. Obesity in South and Southeast Asia-A new consensus on care and management. Obes Rev. (2023) 24:e13520. doi: 10.1111/obr.13520
38. DiBello, JR, McGarvey, ST, Kraft, P, Goldberg, R, Campos, H, Quested, C, et al. Dietary patterns are associated with metabolic syndrome in adult Samoans. J Nutr. (2009) 139:1933–43. doi: 10.3945/jn.109.107888
39. Lin, TK, Teymourian, Y, and Tursini, MS. The effect of sugar and processed food imports on the prevalence of overweight and obesity in 172 countries. Glob Health. (2018) 14:35. doi: 10.1186/s12992-018-0344-y
40. Araghi, M, Soerjomataram, I, Bardot, A, Ferlay, J, Cabasag, CJ, Morrison, DS, et al. Changes in colorectal cancer incidence in seven high-income countries: a population-based study. Lancet Gastroenterol Hepatol. (2019) 4:511–8. doi: 10.1016/S2468-1253(19)30147-5
41. Zhi, X, Kuang, XH, Liu, K, and Li, J. The global burden and temporal trend of cancer attributable to high body mass index: Estimates from the Global Burden of Disease Study 2019. Front Nutr. (2022) 9:918330. doi: 10.3389/fnut.2022.918330
42. GBD 2017 Colorectal Cancer Collaborators . The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. (2019) 4:913–33. doi: 10.1016/S2468-1253(19)30345-0
Keywords: colorectal cancer, high body-mass index, mortality, disability adjusted life years, global burden, sociodemographic index
Citation: Jin X, Dong D, Xu Z and Sun M (2024) The global burden of colorectal cancer attributable to high body-mass index in 204 countries and territories: findings from 1990 to 2021 and predictions to 2035. Front. Nutr. 11:1473851. doi: 10.3389/fnut.2024.1473851
Received: 31 July 2024; Accepted: 04 November 2024;
Published: 20 November 2024.
Edited by:
Falak Zeb, University of Sharjah, United Arab EmiratesReviewed by:
Pugazhendhi Srinivasan, University of Kansas Medical Center, United StatesCopyright © 2024 Jin, Dong, Xu and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingming Sun, TWluZ3NvbmcwMjI2QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.