- 1Student Research Committee, Tabriz University of Medical Sciences, Tabriz, Iran
- 2Nutrition Research Center, Department of Clinical Nutrition, School of Nutrition and Food Sciences, Tabriz University of Medical Sciences, Tabriz, Iran
Background: Exercise and nutritional support are effective strategies in hemodialysis patients who often face health issues like protein-energy wasting (PEW). Therefore, this study aimed to evaluate whether combining exercise with nutritional support offers additional benefits for anthropometry, body composition, and biochemical markers of nutrition in hemodialysis patients.
Methods: This systematic review searched databases, including PubMed, Scopus, and Web of Science, until 14 February 2024 to identify relevant randomized controlled trials. Following screening and data extraction, quality assessment was conducted using the revised Cochrane Risk of Bias tool (ROB2). The study was reported following PRISMA guidelines.
Results: Six studies comprising 199 male and female hemodialysis patients were included. These studies did not report any significant differences in anthropometry, body composition, and nutritional status between individuals who received an exercise program along with nutritional support and those who received only nutritional support.
Conclusion: This systematic review suggests that the combination of exercise with nutritional support may not improve the positive effects of nutritional support on anthropometry, body composition, and nutritional status in hemodialysis patients. However, due to the low quality and significant heterogeneity among the existing studies, further research is required to draw definitive conclusions.
Systematic review registration: PROSPERO (www.crd.york.ac.uk/prospero; registration no: CRD42024542613).
1 Introduction
End-stage renal disease (ESRD) is the final and permanent stage of chronic kidney disease, which occurs when the kidneys are no longer able to function well enough to support long-term survival without renal replacement therapy (1). Globally, its prevalence is projected to increase from 2.6 million in 2010 to 5.4 million in 2030 (2). Renal replacement therapy has different approaches, with hemodialysis being the most common choice for ESRD patients (3–5). However, it often causes protein-energy wasting (PEW), a syndrome defined by adverse nutrition and body composition changes leading to fat and muscle depletion (6). Hormonal imbalances, systemic inflammation, increased catabolism, the release of myocytokines, and the retention of toxins due to uremic syndrome are some factors contributing to decreased functionality and PEW (7). Various nutritional and body composition markers are used to identify PEW, such as hypoalbuminemia, a key biomarker and a strong predictor of mortality in this population (8–10). Unintentional weight loss or a decrease in BMI can also be important indicators of PEW (8). Chronic kidney disease (CKD), particularly in those undergoing dialysis, often leads to impaired physical function and physical inactivity (11). However, regular exercise has been shown to be beneficial in preventing and treating uremic muscle wasting, improving cardiac function, reducing cardiovascular risk factors, increasing muscular strength, and enhancing exercise capacity (12–14). The Kidney Disease Improving Global Outcomes (KDIGO) 2024 Guideline even recommends that CKD patients undertake moderate-intensity physical activity for at least 150 min a week, or to a level suited to their cardiovascular and physical tolerance (15). Olvera-Soto et al. (16) found that three-month resistance exercise significantly increased arm muscle area, arm muscle circumference, handgrip strength, and body fat percentage. In addition, Torres et al. (17) demonstrated that a combination of resistance training and flexibility exercise for 3 months improved body composition parameters (BMI and lean tissue index) and lipid profiles (total cholesterol, LDL, and triglycerides). In another study, Liao et al. (18) indicated that three-month cycling exercise significantly increased albumin levels and BMI and reduced inflammatory cytokines such as hs-CRP and IL-6. Similarly, optimal nutritional support has shown the potential to improve lean body mass or albumin levels (19, 20). Some studies also explored the effects of nutritional support in these patients. Qin et al. (21) observed that two-month oral nutritional supplementation significantly increased serum albumin, hemoglobin, and dietary energy intake among hemodialysis patients (21). Furthermore, a recent consensus statement suggests that the combination of adequate nutrition and exercise may be more effective than either intervention alone in preventing muscle loss among dialysis patients. However, this study also indicated that further investigation in clinical trials is necessary (22). Therefore, our study aims to systematically summarize randomized controlled trials that concentrated solely on hemodialysis patients to evaluate if the addition of exercise to nutritional support demonstrates any extra benefits on biochemical markers of nutrition, anthropometry, and body composition in this population.
2 Materials and methods
2.1 Study design
This systematic review was reported following the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines (23), with the protocol registered on PROSPERO (d3d3LmNyZC55b3JrLmFjLnVrL3Byb3NwZXJv; registration no: CRD42024542613).
2.2 Search strategy
We systematically searched PubMed, Web of Science, and Scopus databases until 14 February 2024, using the following search strategy: (“Exercise” OR “Physical fitness” OR “Sports” OR “Exercise therapy” OR “Physical Activity” OR “Exercise training” OR “Physical exercise”) AND (“Nutritional support” OR “Nutritional supplementation” OR “Oral nutritional supplementation” OR “Nutritional intervention” OR “Nutritional therapy” OR “Enteral nutrition” OR “Parenteral nutrition”) AND (“Biomarkers of nutritional status” OR “Nutritional status indicators” OR “Nutritional status” OR “Nutritional assessment” OR “Nutritional biomarkers” OR “Malnutrition” OR “Biochemical indicators” OR “Biochemical parameters”) OR (“Body composition” OR “Body fat distribution” OR “Body fat percentage” OR “Lean body mass” OR LBM OR “Body weights and measures” OR “Body mass index” OR BMI OR “Anthropometry” OR “Skinfold thickness” OR “Waist-Hip ratio”; Supplementary Tables 1, 2). Moreover, the references of the retrieved articles and existing reviews were manually checked for additional resources.
2.3 Inclusion and exclusion criteria
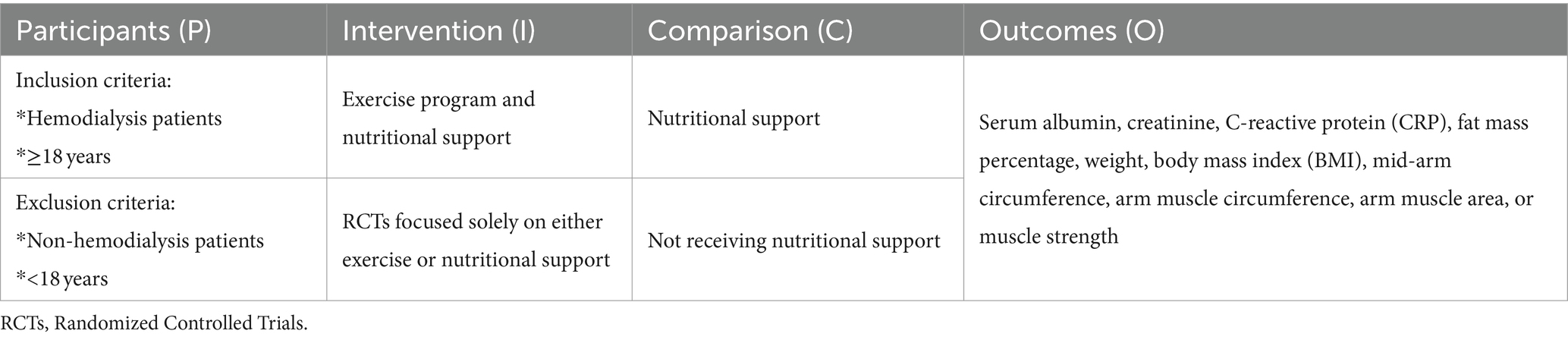
We only included randomized controlled trials (RCTs) evaluating the effects of combining an exercise program with nutritional support on nutritional biochemical markers, anthropometric indices, and body composition in male and female hemodialysis patients undergoing dialysis at least twice a week. Only English-language articles, with no restrictions on publication date, were included. Moreover, we excluded studies other than RCTs, those lacking relevant data, and studies that involved individuals under the age of 18. In addition, we excluded RCTs investigating the sole effect of either exercise or nutritional support. We also excluded studies with a control group not receiving nutritional support. The PICO (Population, Intervention, Comparison, and Outcomes) framework is shown in Table 1.
2.4 Study screening
Two independent reviewers (RKY, NR) carefully reviewed all retrieved articles by reading their titles and abstracts. If there was any uncertainty about excluding a study, it was reviewed in full to reduce the risk of accidental exclusion. Two reviewers then independently analyzed the full texts of potentially relevant papers. Any disagreements were resolved by a third party (AO). We used a PRISMA flowchart to summarize this process.
2.5 Data extraction
The studies included in the analysis underwent a standardized data extraction process using a spreadsheet prepared by one of the authors (RKY). A second reviewer (NR) verified the extracted data to minimize errors and bias. If any data was missing from the reports, we made efforts to contact study authors to obtain necessary information. In cases where a study had more than two comparisons, only the ones meeting the eligibility criteria were considered. The following details were extracted: first author, publication year, study location, health status, age, gender, study design, sample size, type and protocol of exercise program, amount of nutritional support received, method of nutritional support administration in both intervention and control groups, duration of interventions, and the means and standard deviations or median (first and third quartiles) of the outcomes at baseline and post-intervention.
2.6 Quality assessment
Two reviewers (RKY, NR) independently assessed the quality of the articles using the Cochrane tool for assessing the risk of bias in randomized controlled trials (RoB 2) (24). This tool consists of seven domains: (I) random sequence generation; (II) allocation concealment; (III) blinding of participants and personnel; (IV) blinding of outcome assessment; (V) incomplete outcome data; (VI) selective reporting; and (VII) other sources of bias. Any disagreements were reconciled by a third party (AO). The risk of bias is presented in Table 2.
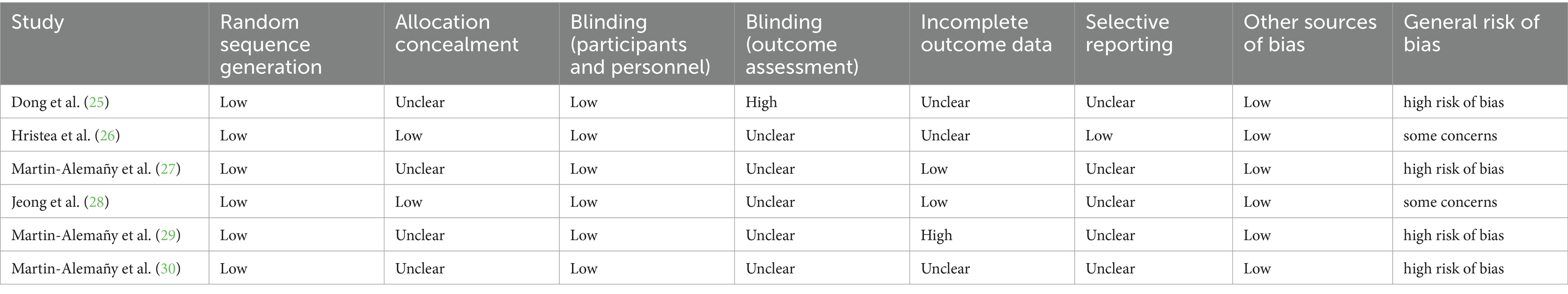
Table 2. Risk of bias assessed according to the revised cochrane risk-of-bias tool for randomized trials (RoB 2).
2.7 Data synthesis
We extracted data from the included studies and presented it in table format. The study outcomes are outlined in the results section. Due to the limited number of studies and the high heterogeneity, we could not conduct a meta-analysis.
3 Results
3.1 Study selection and characteristics
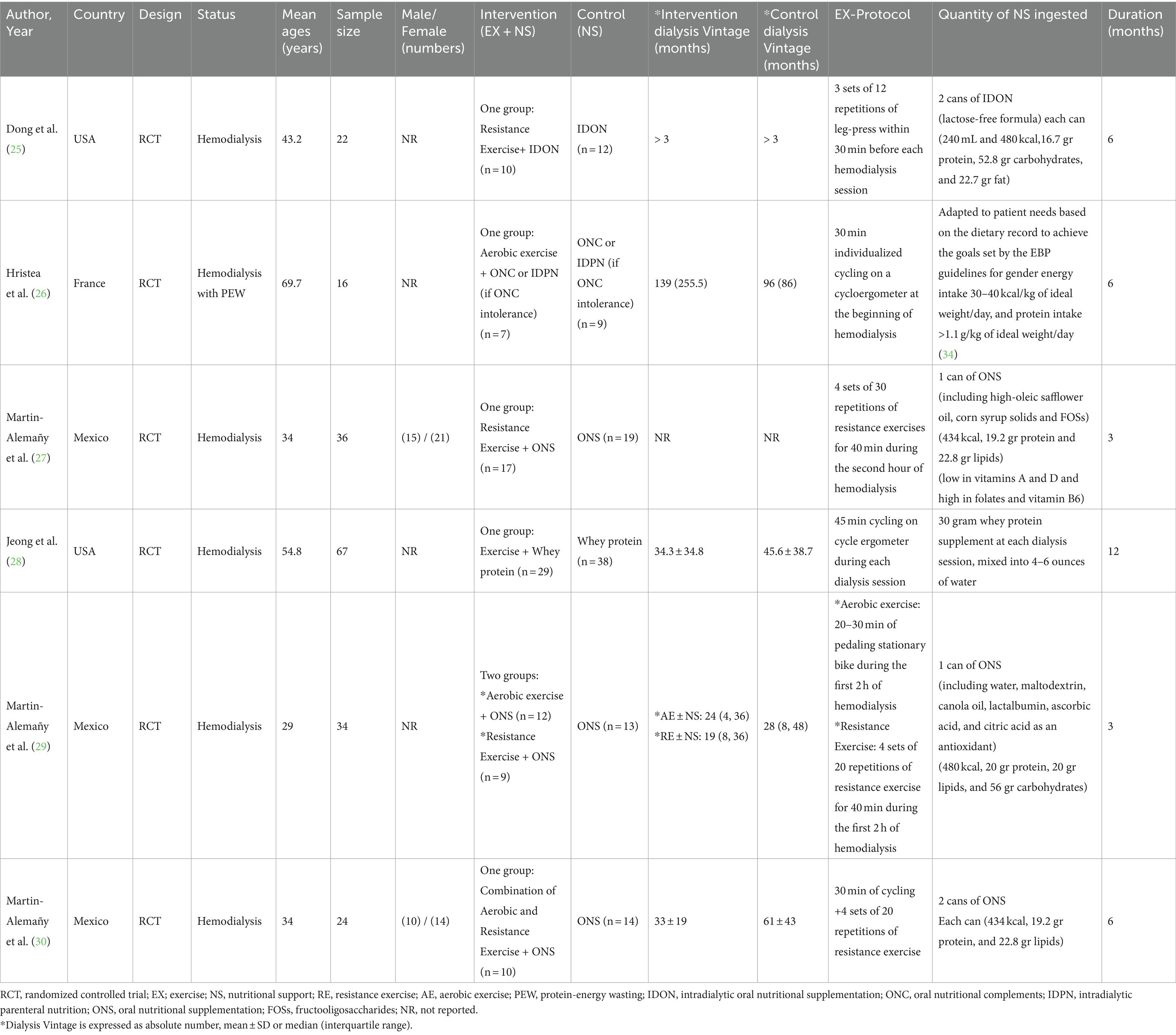
A total of 928 articles were discovered through a comprehensive search, and four more were found from reference lists. After removing duplicates, 629 papers were screened for eligibility by reviewing their titles and abstracts. Thirty articles were then assessed in full-text form, and 24 studies were excluded for the following reasons: (a) studies with non-hemodialysis population, (b) review and observational studies, (c) studies with insufficient data on baseline or endpoint of outcome variables, (d) non-English articles, (e) studies solely focused on either exercise or nutritional support, and (f) studies with a control group not receiving nutritional support. Ultimately, six articles, including two pilot studies, were included in the current review (25–30). The flow chart for the process of the study selection is displayed in Figure 1. A total of 199 male and female hemodialysis patients were included in the study. There were 94 individuals in the intervention group (exercise program and nutritional support) and 105 participants in the control group (nutritional support). All subjects received oral nutritional supplements (ONS) or intradialytic parenteral nutrition (IDPN) for nutritional support. The protein content of each can of ONS was between 16.7 and 20 grams. Those in the intervention groups also participated in resistance, aerobic, or a combination of both exercise programs. In addition, one study implemented the exercise program 30 min before hemodialysis (25), and other studies conducted it during dialysis (26–30). The duration of the studies varied from 3 to 12 months, and the mean age of the patients ranged from 29 to 70 years. All studies were published between 2011 and 2022. Three trials [Martin-Alemañy et al. (27); Martin-Alemañy et al. (29); and Martin-Alemañy et al. (30)] were conducted in Mexico, one trial [Hristea et al. (26)] was performed in France, and two trials [Dong et al. (25); and Jeong et al. (28)] were conducted in the USA. Studies by Hristea et al. (26) and Martin-Alemañy et al. (30) were pilot studies. The characteristics of the studies are presented in Table 3.
3.2 Exercise plus nutritional support versus nutritional support
Eligible studies, including two pilot studies, compared the effects of exercise combined with nutritional support to nutritional support alone on biochemical markers of nutrition (albumin, C-reactive protein (CRP), and creatinine levels), weight, BMI, fat mass percentage (FM%), muscle mass and muscle strength in hemodialysis patients (25–30). The intervention group underwent both exercise and nutritional support, while the control group received only nutritional support.
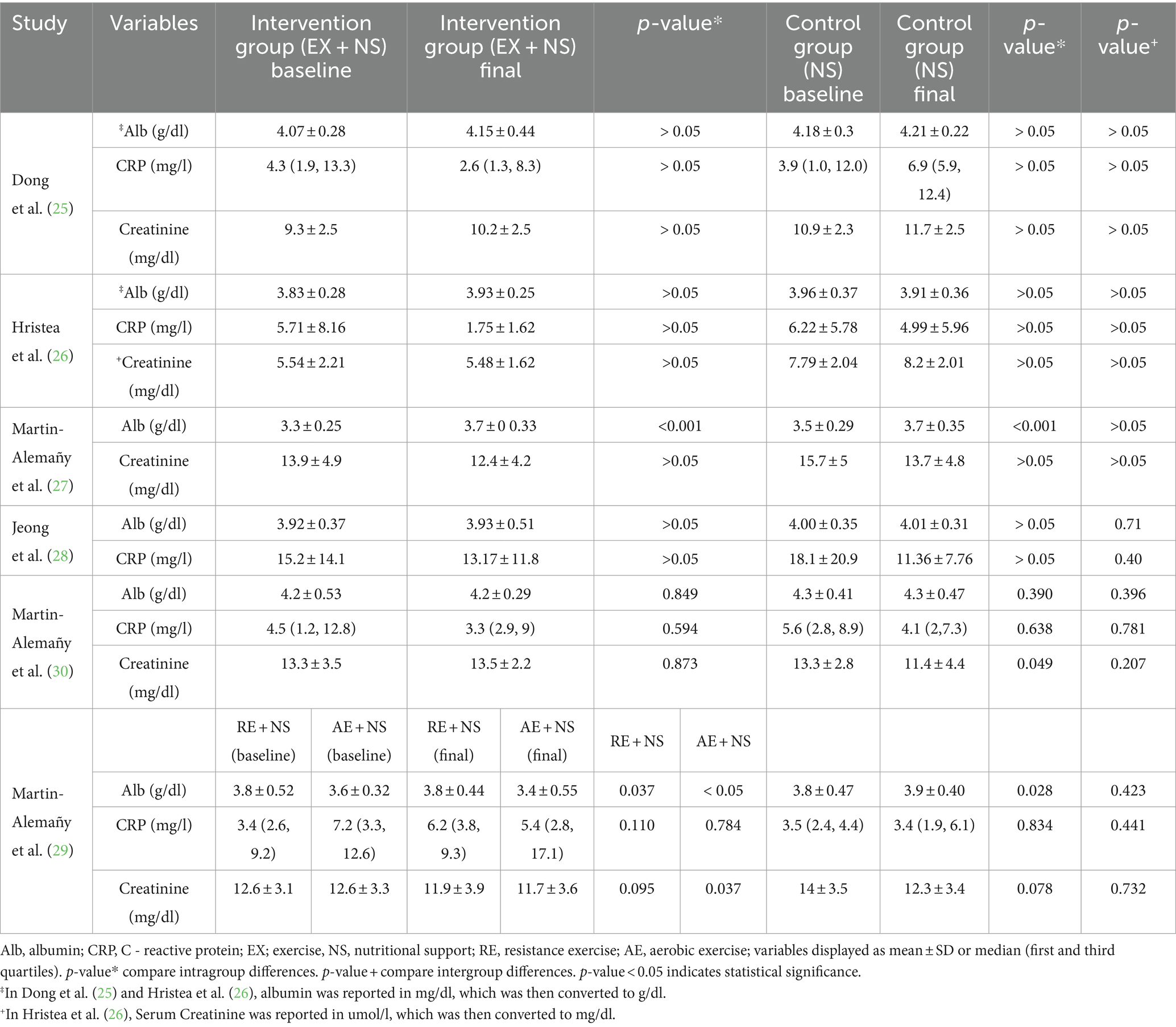
3.2.1 Biochemical markers of nutrition
Four studies [Dong et al. (25); Martin-Alemañy et al. (27); Jeong et al. (28); and Martin-Alemañy et al. (29)] found no statistically significant differences in albumin levels between the intervention and control groups. Similarly, three studies [Dong et al. (25); Jeong et al. (28); and Martin-Alemañy et al. (29)] observed no statistically significant intergroup differences in CRP levels. Likewise, three studies [Dong et al. (25); Martin-Alemañy et al. (27); and Martin-Alemañy et al. (29)] also revealed no statistically significant differences in creatinine levels between the groups. These results were supported by pilot studies conducted by Hristea et al. (26) and Martin-Alemañy et al. (30), which reported no significant intergroup differences in albumin, CRP, and creatinine levels. The changes in biochemical markers of nutrition are detailed in Table 4.
3.2.2 Anthropometry and body composition
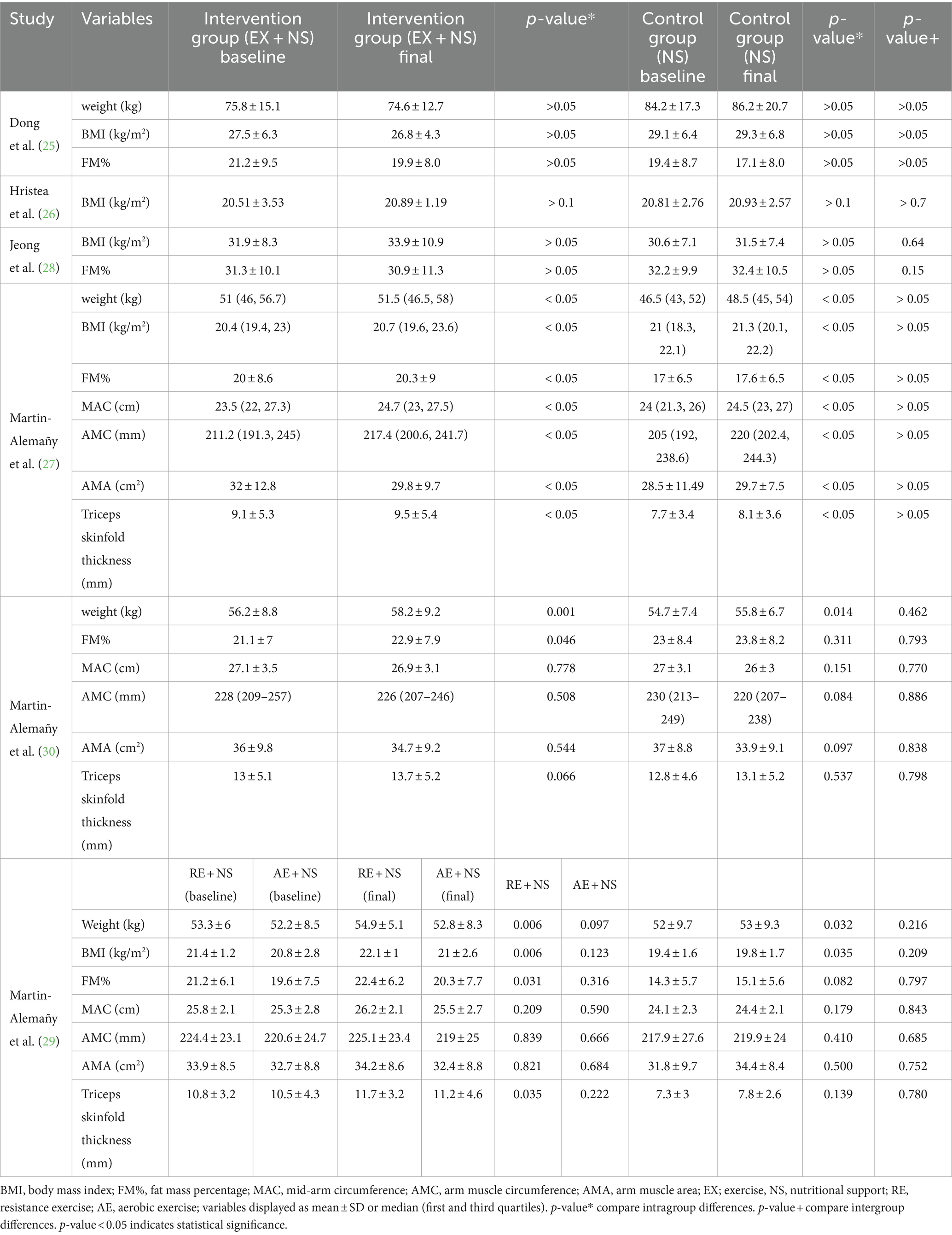
3.2.2.1 Body weight
Three studies [Dong et al. (25); Martin-Alemañy et al. (27); and Martin-Alemañy et al. (29)] indicated no statistically significant differences in body weight between the intervention and control groups. Similarly, a pilot study by Martin-Alemañy et al. (30) also revealed no significant intergroup differences in body weight. The changes in body weight are displayed in Table 5.
3.2.2.2 BMI and FM %
Four studies [Dong et al. (25); Martin-Alemañy et al. (27); Jeong et al. (28); and Martin-Alemañy et al. (29)] reported no statistically significant differences in BMI and FM % between the groups. Two pilot studies also confirmed these findings, which Hristea et al. (26) found no significant intergroup differences in BMI and Martin-Alemañy et al. (30) found no significant intergroup differences in FM%. The changes in BMI and FM% are reported in Table 5.
3.2.2.3 Muscle mass
Two studies [Martin-Alemañy et al. (27); and Martin-Alemañy et al. (29)] assessed muscle mass using mid-arm circumference (MAC), arm muscle circumference (AMC), arm muscle area (AMA), and triceps skinfold thickness. They both reported no statistically significant differences in muscle mass between the intervention and control groups. Likewise, a pilot study by Martin-Alemañy et al. (30) observed no significant intergroup differences in muscle mass. The detailed results regarding muscle mass are available in Table 5.
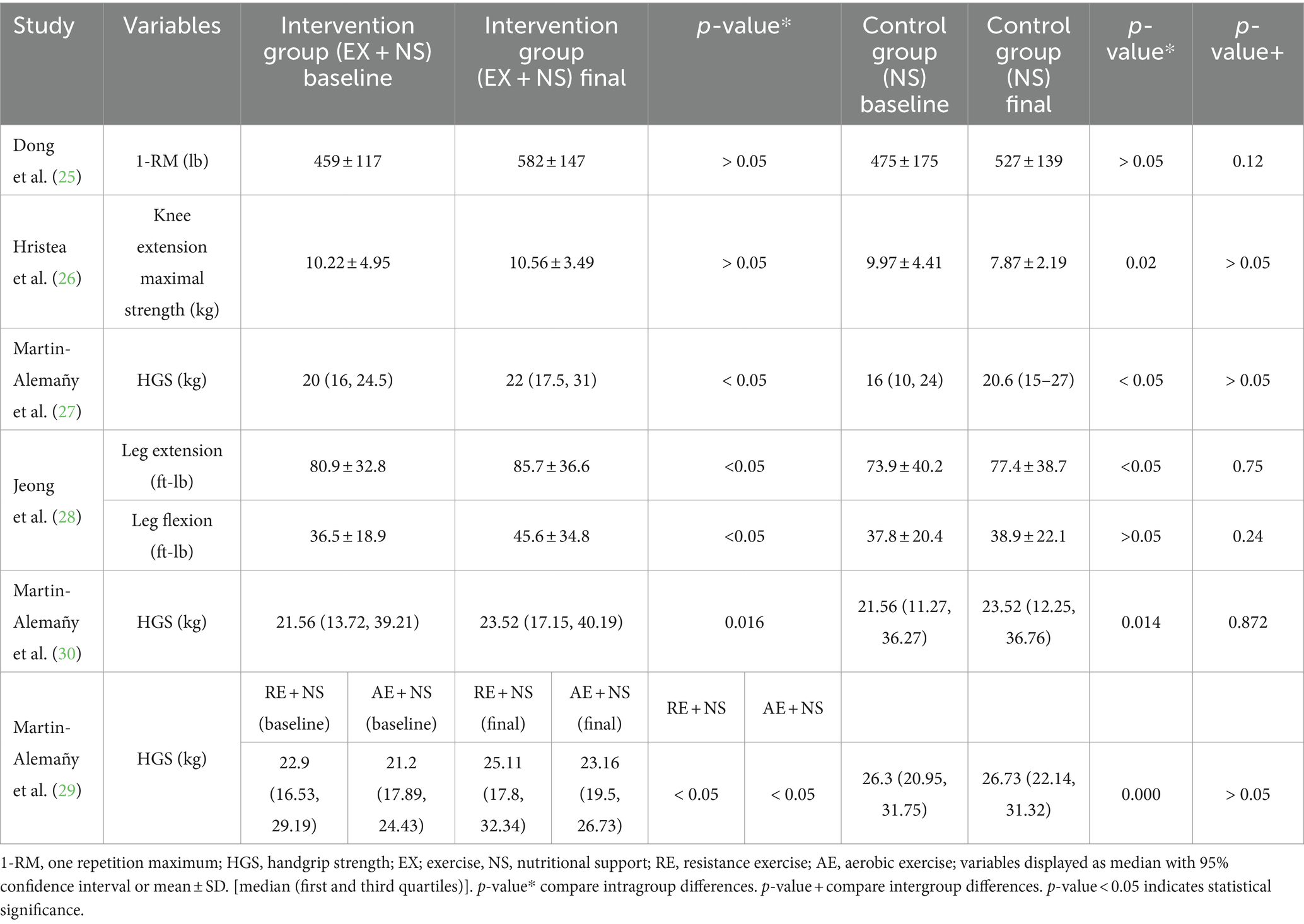
3.2.2.4 Muscle strength
Four studies [Dong et al. (25); Martin-Alemañy et al. (27); Jeong et al. (28); and Martin-Alemañy et al. (29)] used handgrip strength (HGS), one Repetition Maximum (1-RM), knee extension maximal strength, and leg maximal flexion force as the measures of muscle strength for comparison. They all indicated no statistically significant differences in muscle strength between the intervention and control groups. Additionally, pilot studies by Hristea et al. (26) and Martin-Alemañy et al. (30) also reported no significant intergroup differences in muscle strength (26, 30). The detailed results for muscle strength assessment are provided in Table 6.
4 Discussion
We conducted this systematic review to investigate whether the addition of exercise to nutritional support provides further benefits for biochemical indicators of nutritional status and body composition in hemodialysis patients. Given the potential advantages of exercise and nutritional care in this population, exploring the combined effects of these approaches might contribute to improving the overall well-being of patients.
4.1 Main findings
This review revealed that combining an exercise program with nutritional support does not produce synergistic effects on biochemical markers of nutrition, anthropometry, and body composition in hemodialysis patients. However, when these two interventions are examined separately, studies suggest that both exercise and nutritional support may induce anabolic effects. For instance, adequate nutritional support can enhance nutritional markers and improve protein homeostasis (31). Protein intake—especially essential amino acids (EAAs)—activates the mTORC1 pathway in skeletal muscle cells. This activation results in phosphorylating two key downstream targets: eukaryotic translation initiation factor 4E-binding protein 1 (4E-BP1) and ribosomal protein S6 kinase beta-1 (S6K1). This process promotes protein synthesis by facilitating the assembly of the translation initiation complex and recruiting ribosomes to mRNA (32). Additionally, exercise alone may help prevent muscle atrophy by inhibiting apoptotic processes and protein degradation (33). Exercise also stimulates muscle protein synthesis by activating mTORC1 through the Akt/PKB pathway. Akt/PKB further phosphorylates and inhibits glycogen synthase kinase three beta (GSK-3β), a negative regulator of mTORC1 (32). Given the ability of exercise to enhance the sensitivity of muscle cells to amino acids (32), we hypothesized that a combination of protein ingestion and physical exercise may offer additional benefits for hemodialysis patients. However, comparing changes between groups receiving both interventions and those receiving only nutritional support did not confirm our hypothesis. Although this systematic review was conducted rigorously and considered all available data, the findings should be interpreted cautiously due to concerns about the quality of the included studies.
4.2 Overview of the studies reviewed
This systematic review included six randomized controlled trials that examined the effects of adding exercise to nutritional support compared to receiving nutritional support alone (25–30). The interventions spanned from 3 to 12 months and involved supervised exercise programs (such as resistance, aerobic, or a combination) along with oral nutritional supplements (ONS) or intradialytic parenteral nutrition (IDPN). In our review of the included trials, we observed that some studies, emphasizing a resistance training program, demonstrated significant improvements in albumin and some body composition indices across all participants (27, 29). This may suggest the potential of resistance exercise to ameliorate muscle wasting; however, the findings also indicated no statistically significant differences in nutritional status and body composition between the groups receiving both interventions and those receiving only nutritional support. Several factors may explain the lack of significant impact of combining exercise with nutritional support. For instance, the studies provided data on the caloric or protein content of the nutritional support, but the adequacy of these values in relation to the patients’ overall dietary intake remains uncertain, making it difficult to understand the effectiveness of the exercise programs in improving body composition (25–30). Some studies did not also report sample size calculations, leaving the power to detect differences unclear (26–28). Additionally, high dropout rates may have influenced the results (26, 28), and there were issues with adherence reporting (25, 26, 28, 30) and the short duration of some interventions (27, 29). Furthermore, the inclusion of younger patients with good nutritional status or physical performance may have restricted the ability to detect clear benefits (25, 29, 30). Overall, due to the insufficient power, we could not conclusively determine the effects of combined nutritional and exercise interventions in hemodialysis patients.
4.3 Strengths and limitations
The present literature review consists of some strengths and limitations. This is the first systematic review which evaluates the potential effects of adding exercise to nutritional support in hemodialysis patients. We included studies with a control group receiving nutritional support to observe the effects of exercise clearly. Our literature search was also comprehensive, and the included articles were relatively new and well-designed. However, most studies had a small number of patients and a short duration of follow-up. High heterogeneity, failure to find the source of the heterogeneity, and the risk of bias in some factors should be considered limitations. Additionally, two of the included studies were pilot studies, so their findings may not be conclusive due to the low power. Moreover, we did not assess the risk of publication bias due to the inability of performing a meta-analysis, which is considered a methodological limitation of this review.
5 Conclusion
In conclusion, our findings suggest that adding exercise may not enhance the anabolic effects of nutritional support on anthropometry, body composition, and nutritional status in hemodialysis patients. However, these conclusions are not definitive due to the limited statistical power and heterogeneous nature of the existing studies. The low quality of these studies warrants cautious interpretation of the results. Therefore, further high-quality clinical trials with larger sample sizes, longer durations, and more robust designs are recommended to provide more accurate and comprehensive insights into the potential benefits of combining exercise with nutritional support in hemodialysis patients.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
RK: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. NR: Data curation, Investigation, Writing – review & editing. AO: Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1471455/full#supplementary-material
References
1. Agarwal, R . Defining end-stage renal disease in clinical trials: a framework for adjudication. Nephrol Dial Transplant. (2016) 31:864–7. doi: 10.1093/ndt/gfv289
2. Liyanage, T, Ninomiya, T, Jha, V, Neal, B, Patrice, HM, Okpechi, I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. (2015) 385:1975–82. doi: 10.1016/S0140-6736(14)61601-9
3. Pecoits-Filho, R, Okpechi, IG, Donner, J-A, Harris, DC, Aljubori, HM, Bello, AK, et al. Capturing and monitoring global differences in untreated and treated end-stage kidney disease, kidney replacement therapy modality, and outcomes. Kidney Int Suppl. (2020) 10:e3–9. doi: 10.1016/j.kisu.2019.11.001
4. Bello, AK, Levin, A, Tonelli, M, Okpechi, IG, Feehally, J, Harris, D, et al. Assessment of global kidney health care status. JAMA. (2017) 317:1864–81. doi: 10.1001/jama.2017.4046
5. Bello, AK, Levin, A, Lunney, M, Osman, MA, Ye, F, Ashuntantang, GE, et al. Status of Care for end Stage Kidney Disease in countries and regions worldwide: international cross sectional survey. BMJ. (2019) 367:l5873. doi: 10.1136/bmj.l5873
6. Oliveira, EA, Zheng, R, Carter, CE, and Mak, RH. Cachexia/protein energy wasting syndrome in CKD: causation and treatment. Semin Dial. (2019) 32:493–9. doi: 10.1111/sdi.12832
7. Lodebo, BT, Shah, A, and Kopple, JD. Is it important to prevent and treat protein-energy wasting in chronic kidney disease and chronic Dialysis patients? J Ren Nutr. (2018) 28:369–79. doi: 10.1053/j.jrn.2018.04.002
8. Fouque, D, Kalantar-Zadeh, K, Kopple, J, Cano, N, Chauveau, P, Cuppari, L, et al. A proposed nomenclature and diagnostic criteria for protein–energy wasting in acute and chronic kidney disease. Kidney Int. (2008) 73:391–8. doi: 10.1038/sj.ki.5002585
9. Kalantar-Zadeh, K, Kilpatrick, RD, Kuwae, N, McAllister, CJ, Alcorn, H Jr, Kopple, JD, et al. Revisiting mortality predictability of serum albumin in the Dialysis population: time dependency, longitudinal changes and population-attributable fraction. Nephrol Dial Transplant. (2005) 20:1880–8. doi: 10.1093/ndt/gfh941
10. Ikizler, TA, Wingard, RL, Harvell, J, Shyr, Y, and Hakim, RM. Association of Morbidity with markers of nutrition and inflammation in chronic hemodialysis patients: a prospective study. Kidney Int. (1999) 55:1945–51. doi: 10.1046/j.1523-1755.1999.00410.x
11. Clyne, N, Jogestrand, T, Lins, LE, Pehrsson, SK, and Ekelund, LG. Factors limiting physical working capacity in Predialytic Uraemic patients. Acta Med Scand. (1987) 222:183–90. doi: 10.1111/j.0954-6820.1987.tb10657.x
12. Cheema, BSB, and Fiatarone Singh, MA. Exercise training in patients receiving maintenance hemodialysis: a systematic review of clinical trials. Am J Nephrol. (2005) 25:352–64. doi: 10.1159/000087184
13. Clapp, EL, Bevington, A, and Smith, AC. Exercise for children with chronic kidney disease and end-stage renal disease. Pediatr Nephrol. (2012) 27:165–72. doi: 10.1007/s00467-010-1753-1
14. Kosmadakis, GC, John, SG, Clapp, EL, Viana, JL, Smith, AC, Bishop, NC, et al. Benefits of regular walking exercise in advanced pre-Dialysis chronic kidney disease. Nephrol Dial Transplant. (2012) 27:997–1004. doi: 10.1093/ndt/gfr364
15. Levin, A, Ahmed, SB, Carrero, JJ, Foster, B, Francis, A, Hall, RK, et al. Executive summary of the Kdigo 2024 clinical practice guideline for the evaluation and Management of Chronic Kidney Disease: known knowns and known unknowns. Kidney Int. (2024) 105:684–701. doi: 10.1016/j.kint.2023.10.016
16. Olvera-Soto, MG, Valdez-Ortiz, R, Alvarenga, JCL, and de los Ángeles Espinosa-Cuevas, M. Effect of resistance exercises on the indicators of muscle reserves and handgrip strength in adult patients on hemodialysis. J Ren Nutr. (2016) 26:53–60. doi: 10.1053/j.jrn.2015.06.006
17. Torres, E, Aragoncillo, I, Moreno, J, Vega, A, Abad, S, García-Prieto, A, et al. Exercise training during hemodialysis sessions: physical and biochemical benefits. Ther Apher Dial. (2020) 24:648–54. doi: 10.1111/1744-9987.13469
18. Liao, M-T, Liu, W-C, Lin, F-H, Huang, C-F, Chen, S-Y, Liu, C-C, et al. Intradialytic aerobic cycling exercise alleviates inflammation and improves endothelial progenitor cell count and bone density in hemodialysis patients. Medicine. (2016) 95:e4134. doi: 10.1097/MD.0000000000004134
19. Rattanasompattikul, M, Molnar, MZ, Lee, ML, Dukkipati, R, Bross, R, Jing, J, et al. Anti-inflammatory and anti-oxidative nutrition in Hypoalbuminemic Dialysis patients (Aionid) study: results of the pilot-feasibility, double-blind, randomized, placebo-controlled trial. J Cachexia Sarcopenia Muscle. (2013) 4:247–57. doi: 10.1007/s13539-013-0115-9
20. Stratton, RJ, Bircher, G, Fouque, D, Stenvinkel, P, De Mutsert, R, Engfer, M, et al. Multinutrient Oral supplements and tube feeding in maintenance Dialysis: a systematic review and Meta-analysis. Am J Kidney Dis. (2005) 46:387–405. doi: 10.1053/j.ajkd.2005.04.036
21. Qin, A, Tan, J, Hu, W, Liu, Y, Chen, L, Tang, Y, et al. Oral energy supplementation improves nutritional status in hemodialysis patients with protein–energy wasting: a pilot study. Front Pharmacol. (2022) 13:839803. doi: 10.3389/fphar.2022.839803
22. Battaglia, Y, Baciga, F, Bulighin, F, Amicone, M, Mosconi, G, Storari, A, et al. Physical activity and exercise in chronic kidney disease: consensus statements from the physical exercise working Group of the Italian Society of nephrology. J Nephrol. (2024) 37:–1765. doi: 10.1007/s40620-024-02049-9
23. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The Prisma 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
24. Sterne, JAC, Savović, J, Page, MJ, Elbers, RG, Blencowe, NS, Boutron, I, et al. Rob 2: a revised tool for assessing risk of Bias in randomised trials. BMJ. (2019) 366:l4898. doi: 10.1136/bmj.l4898
25. Dong, J, Sundell, MB, Pupim, LB, Wu, P, Shintani, A, and Ikizler, TA. The effect of resistance exercise to augment long-term benefits of intradialytic Oral nutritional supplementation in chronic hemodialysis patients. J Ren Nutr. (2011) 21:149–59. doi: 10.1053/j.jrn.2010.03.004
26. Hristea, D, Deschamps, T, Paris, A, Lefrançois, G, Collet, V, Savoiu, C, et al. Combining intra-dialytic exercise and nutritional supplementation in malnourished older Haemodialysis patients: towards better quality of life and autonomy. Nephrology (Carlton). (2016) 21:785–90. doi: 10.1111/nep.12752
27. Martin-Alemañy, G, Valdez-Ortiz, R, Olvera-Soto, G, Gomez-Guerrero, I, Aguire-Esquivel, G, Cantu-Quintanilla, G, et al. The effects of resistance exercise and Oral nutritional supplementation during hemodialysis on indicators of nutritional status and quality of life. Nephrol Dial Transplant. (2016) 31:1712–20. doi: 10.1093/ndt/gfw297
28. Jeong, JH, Biruete, A, Tomayko, EJ, Wu, PT, Fitschen, P, Chung, HR, et al. Results from the randomized controlled Ihope trial suggest no effects of Oral protein supplementation and exercise training on physical function in hemodialysis patients. Kidney Int. (2019) 96:777–86. doi: 10.1016/j.kint.2019.03.018
29. Martin-Alemañy, G, Espinosa-Cuevas, M, Pérez-Navarro, M, Wilund, KR, Miranda-Alatriste, P, Cortés-Pérez, M, et al. Effect of Oral nutritional supplementation with and without exercise on nutritional status and physical function of adult hemodialysis patients: a parallel controlled clinical trial (Avante-Hemo study). J Ren Nutr. (2020) 30:126–36. doi: 10.1053/j.jrn.2019.06.010
30. Martin-Alemañy, G, Perez-Navarro, M, Wilund, KR, García-Villalobos, G, Gómez-Guerrero, I, Cantú-Quintanilla, G, et al. Effect of intradialytic Oral nutritional supplementation with or without exercise improves muscle mass quality and physical function in hemodialysis patients: a pilot study. Nutrients. (2022) 14:2946. doi: 10.3390/nu14142946
31. Dong, J, and Ikizler, TA. New insights into the role of anabolic interventions in Dialysis patients with protein energy wasting. Curr Opin Nephrol Hypertens. (2009) 18:469–75. doi: 10.1097/MNH.0b013e328331489d
32. Garibotto, G, Saio, M, Aimasso, F, Russo, E, Picciotto, D, Viazzi, F, et al. How to overcome anabolic resistance in Dialysis-treated patients? Front Nutr. (2021) 8:701386. doi: 10.3389/fnut.2021.701386
33. Deligiannis, A, D'Alessandro, C, and Cupisti, A. Exercise training in Dialysis patients: impact on cardiovascular and skeletal muscle health. Clin Kidney J. (2021) 14:ii25–33. doi: 10.1093/ckj/sfaa273
34. Magnard, J, Deschamps, T, Cornu, C, Paris, A, and Hristea, D. Effects of a six-month intradialytic physical activity program and adequate nutritional support on protein-energy wasting, physical functioning and quality of life in chronic hemodialysis patients: Actinut study protocol for a randomised controlled trial. BMC Nephrol. (2013) 14:259. doi: 10.1186/1471-2369-14-259
Keywords: exercise, nutritional support, biochemical markers of nutrition, anthropometry, body composition, hemodialysis, protein-energy wasting
Citation: Kamalzadeh Yazdi R, Radkhah N and Ostadrahimi A (2024) Does exercise enhance the benefits of nutritional support on the biochemical markers of nutrition, anthropometry, and body composition in hemodialysis patients? A systematic review. Front. Nutr. 11:1471455. doi: 10.3389/fnut.2024.1471455
Edited by:
Steven E. Riechman, Texas A&M University, United StatesReviewed by:
Aaron Riviere, Texas A&M University, United StatesYuri Battaglia, University of Verona, Italy
Copyright © 2024 Kamalzadeh Yazdi, Radkhah and Ostadrahimi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alireza Ostadrahimi, b3N0YWRyYWhpbWlAdGJ6bWVkLmFjLmly
 Raheleh Kamalzadeh Yazdi
Raheleh Kamalzadeh Yazdi Nima Radkhah
Nima Radkhah Alireza Ostadrahimi
Alireza Ostadrahimi