- 1Department of Health Promotion and Behavioral Sciences, University of Texas Health Science Center at Houston, School of Public Health, Houston, TX, United States
- 2Michael and Susan Dell Center for Healthy Living, Department of Health Promotion and Behavioral Sciences, University of Texas Health Science Center at Houston, School of Public Health in Austin, Austin, TX, United States
- 3Center for Health Equity, Department of Epidemiology, University of Texas Health Science Center at Houston, School of Public Health, Houston, TX, United States
- 4Brighter Bites, Houston, TX, United States
Objective: Several studies suggest that during the early pandemic, amidst socioeconomic instability, children from underserved families were more likely to resort to consuming cheaper, lower-quality foods with longer shelf lives. This study investigated the change in unhealthy food consumption across different phases (pre, early, mid) of the COVID-19 pandemic, and whether the strength of association between unhealthy food consumption and household socioeconomic disadvantage (HSED) varied across phases of the pandemic.
Methods: This study utilized serial cross-sectional data collected from low-income families enrolled in a school-based food co-op, Brighter Bites. Secondary data analysis included 5,384 surveys from families who had complete data: 3422 pre-pandemic, 944 from the early pandemic, and 1,018 mid-pandemic. Outcome measures included sugary food intake and convenience/fast food intake, each of which was operationalized as a scale using pre-validated items from the surveys. HSED was operationalized as a composite of parent employment, parent education, food insecurity, and participation in government programs; responses were categorized into low, medium, and high HSED groups for analysis. We examined the interaction between HSED and time period to explore how HSED and its association with dietary measures changed over the course of the pandemic.
Results: A significant linear negative trend, i.e., a decrease in consumption from pre-to-mid-pandemic period was seen in sugary food intake (p < 0.001), but not in convenience food intake. In data pooled across time-periods, both sugary food and convenience/fast food consumption were inversely associated with HSED, and low unhealthy food consumption was observed among high-disadvantage groups. No significant interaction between time period and HSED was observed on either scale. However, the post-regression estimates from the adjusted interaction model showed a significant association between convenience/fast food consumption and HSED in pre- and mid-pandemic periods.
Conclusion: The study highlights the nuances of socioeconomic dynamics on the diet behaviors of children from low-income families during a natural disaster.
Introduction
Unhealthy food consumption contributes to a plethora of chronic diseases in the United States (U.S.) (1, 2); nearly half the elementary-aged children (6–11 years) consume inferior quality diets and excess junk food compared to their peers in other age groups (3–5). During the early phase of the COVID-19 pandemic, social measures like lockdowns/school closures implemented to curb transmission of the SARS-COV2 virus, worsened diet quality among families with children (6, 7). Longitudinal studies conducted on diverse U.S. populations reported the highest increase in eating disorders and BMI in this age group (8). As the elementary school age is considered a critical period in the development of chronic diseases that track into adulthood, it is vital to identify any detrimental diet changes that may have occurred during the pandemic, among this population (9).
Socioeconomic status (SES) has emerged as a crucial determinant of diet and nutrition quality, and their downstream health consequences; as families with lower SES often face barriers such as limited financial resources, reduced access to healthy foods, and greater reliance on cheaper, calorie-dense options, which can lead to poorer diet quality and subsequent health issues (10). Particularly during times of crises, families experiencing poverty are more vulnerable to macroeconomic fluctuations (11, 12). Along with the ongoing challenges that low-income families face, the added burden of food insecurity further exacerbates their situation, creating a cumulative socioeconomic disadvantage (13). During the pandemic, millions of Americans experienced pandemic-related job losses and financial setbacks, resulting in a three-fold increase in the prevalence of food insecurity in the U.S. (14). Low-income families with children, especially those belonging to racial minority groups, were disproportionately affected by interruptions in food supply chain, government assistance programs, and nutritious school meals. Overburdened with financial insecurity and loss of access to reliable food sources, these families were forced to choose affordability over quality of food (15–19). Studies conducted during the early pandemic reported an increase in the purchase and consumption of sugary drinks, chips, ready-to-eat meals, and a decrease in fresh produce, among children belonging to such vulnerable families (19, 20). However, a majority of these studies did not include objective control data from pre-pandemic time for comparison. Furthermore, as schools reopened for hybrid learning in 2021, USDA introduced new waivers in school meal programs, such as meal-time and meal pattern flexibility to ensure continued access to school meals (21–23). There is little information on how elementary-aged children’s diet changed with the re-opening of schools and economic instability experienced in the U.S. at that time, with objective comparative data (24, 25). It is of particular interest to understand how children’s dietary behaviors were impacted by rapidly evolving government mandates and employment situations, especially since this knowledge provides critical insights into the immediate health impacts of the pandemic and serves as a foundation for evidence-based disaster preparedness strategies.
Therefore, this study aims to investigate changes in unhealthy food consumption across different phases (pre, early, mid) of the COVID-19 pandemic. The second objective is to examine the strength of associations between unhealthy food consumption and household socioeconomic disadvantage, and determine whether the magnitude of these associations varied across phases of the pandemic.
Materials and methods
Research design and study participants
This study utilized serial survey-based cross-sectional data collected between 2018 and 2022 from Brighter Bites, a theory-grounded school-based food co-op health intervention serving low-income families across the U.S. (26). Brighter Bites is a 501c3 non-profit organization that implements school-based health promotion programs in Texas (Houston, Austin, Dallas, San Antonio); Florida (Southwest Florida); New York (New York City); Washington, D.C.; California (Salinas, Los Angeles, Bakersfield); and Arizona (Phoenix). The organization provides free fresh produce and implementation support of nutrition education at schools that predominately serve children from low-income families for 3 years in a row, to mitigate food insecurity and improve dietary habits (16, 27–29). Each school year, at the beginning of the fall semester, before the Brighter Bites program began, informed consent was obtained, and electronic surveys were sent to parents to obtain data. Survey completion and participation in the study was voluntary, and all participants provided informed consent. The University of Texas Health Science Center at Houston (UTHealth Houston) is the evaluation partner for Brighter Bites. As a part of a data sharing agreement, deidentified data were shared with UTHealth for analysis. The UTHealth Committee for Protection of Human Subjects approved the parent study (HSC-SPH-15-0752).
The current analysis is based on four of these annual baseline parent surveys (2018–2019, 2019–2020, 2020–2021, 2021–2022) from seven areas (Houston, Dallas, Austin, Southwest Florida, Washington, D.C., Salinas, and Bakersfield). The response rate for each year is as follows: 2018–28.1%, 2019–27.9%, 2020–33%, 2021–16.8%. Parent and child data from 5,384 surveys (self-reported data from the parents); 3,422 during the pre-pandemic period (fall 2018, 2019), 944 from the early pandemic period (fall 2020), and 1,018 from the mid-pandemic period (fall 2021) were included in the analysis.
Measures
Children’s unhealthy food consumption
Nine pre-validated items (30) were identified from the parent survey that captured the frequency of consumption of the following unhealthy items in the week prior to survey completion – sugar-sweetened beverages (SSB) (3 items), sugary cereals, frozen desserts, fried potatoes, chips, heat-and-serve meals, and meals from the restaurant. The responses for all the items were captured on a Likert scale (never in a week – every day in a week). For this study, dietary items were broadly classified into two main categories based on the Family Life, Activity, Sun, Health, and Eating (FLASHE) study data guide (30). (1) Sugary foods including Sugar-Sweetened Beverages (SSB), sugary cereals, and frozen desserts, and (2) Convenience/Fast-food including fried potatoes, chips, heat-and-serve meals, and meals from restaurants. These categories represented the two most consumed unhealthy food groups during the pandemic period (31–34). The possible score for sugary foods ranges between 0 to 20, and the possible score for the convenience/fast-food category ranges between 0 and 16. In both cases, higher scores represented a higher frequency in the consumption of that food group.
Assessment of household socioeconomic disadvantage
Socioeconomic disadvantage is a multidimensional construct that cannot be captured by single item scales (10). Especially in low income populations, where income sources are irregular and not reliably reported, alternative measures need to be utilized to capture variation of socioeconomic status. We utilized a composite household socioeconomic disadvantage measure from literature, which encompassed indicators both stable and those that were relatively exacerbated by the pandemic (35). Based on literature (10, 35), we utilized four variables: parent employment, parent education, food insecurity, and participation in government assistance programs to create the composite measure – household socioeconomic disadvantage.
In our dataset (pooled over time period), when analyzed independently, we noticed that almost all components of HSED were significantly associated with both sugary food (p < 0.05) and convenience/fast food (p < 0.05), except for food insecurity with convenience/fast food scale (p = 0.643); the strongest association was observed for food insecurity with sugary food scale (Coeff: 0.22; p = 0.004), and for parent education with convenience/fast food scale (Coeff: 0.36; p = <0.001). Although food insecurity was not a significant predictor, we included it in our composite HSED measure due to its empirical association with diet behavior, and its relevance to the COVID-19 pandemic.
Information regarding each component of household socio-economic status was captured using appropriate single-item scales (10, 36). Information regarding parent education was categorized into 0: never – attended middle school; 1: attended/graduate high school; and 2: attended/graduated college; employment status of the parent was categorized as 0: involuntarily unemployed; 2: voluntarily unemployed; and 2: employed. Food insecurity was measured using the Hunger Vital Sign questionnaires, and individuals who selected “sometimes true” or “often true” for either question were classified as food insecure (37). Participation in any government assistance programs (WIC, SNAP, Double Dollars, Medicaid, Medicare, CHIP, free/reduced meals at school) were categorized as not participating or participating. Using the above information, we created a composite measure of household socio-economic disadvantage, guided by similar work in prior literature (10, 35). The summative composite score ranged from 0 to 8 representing decreasing order of household socioeconomic disadvantage (HSED). The scores were grouped into high (score 0–2), medium (score 3–5), and low (score 6–8) disadvantage groups for analysis. Additionally, each HSED component was examined independently in relation to the outcomes, to provide insight into their role as individual predictors of unhealthy food consumption.
Effect modifier
We examined whether the phase of the pandemic modified the relationship between socioeconomic disadvantage and dietary measures. Three phases were identified: pre-pandemic (fall 2018 to fall 2019), early pandemic (fall 2020), and mid pandemic (fall 2021). This categorization of corresponded to macro-socioeconomic changes that occurred in the U.S. during this time. Macroeconomic changes in the early pandemic phase (March 2020 – March 2021) included increases in unemployment, the introduction of government fiscal response (Families First Act; CARES act; SNAP and WIC waivers) while macrosocial changes include school closures, and halting of school lunch programs. The macroeconomic environment of the mid pandemic phase (March 2021 – May 2022) was characterized by high inflation, decline in unemployment, extension of benefits, and macrosocial changes such as school reopening, adapted school nutrition programs (e.g., waivers in NSLP) (21, 23–25, 38).
Covariates
Data on child’s grade (K-5), gender (male, female/), race (Black/African American, Hispanic/Latino/Mexican American, White/Caucasian, Asian, Native Hawaiian/Pacific Islander, American Indian/Alaskan Native, Other), number of children at home, and number of people at home were collected in the surveys. Beneficial food consumed in the week before the survey was captured in the following items – 100% fruit juice, water, fresh fruits, vegetables, and other non-fried vegetables. These variables were combined to form a beneficial food scale (30).
Statistical analysis
Schools that were only in the first year of the Brighter Bites program, (i.e., those who had not received any component of the intervention at the time of the baseline survey), were included in the analysis. Means and standard deviations were reported for continuous measures while proportions were reported for. Categorical variables. The changes in unhealthy food consumption over time (time period 0 = pre-pandemic; 1 = early pandemic; 2 = mid pandemic) were reported using p for linear trend. Mixed effects regression models were built using pooled data from 2018 to 2021 and were used to examine the strength of the association of unhealthy food consumption with household socioeconomic disadvantage. Covariates were selected for analysis using Wald tests. Univariable analysis was conducted to determine the unadjusted associations between the outcome and each covariate. Next, based on statistically significant bivariate associations with the outcome, and modification of regression coefficients by 10%, we identified that child’s race and beneficial food scale served as potential confounders and adjusted for them in our analysis. We also ran initial models including location fixed effects, but none of these effects was significant, hence they were discarded. The overall fit of the models was determined using likelihood ratio tests. Additional tests for multicollinearity included checking the variance inflation factor (VIF). No multicollinearity was detected.
To assess changes in this association over time, an interaction term between household socioeconomic disadvantage and time period was added to the model. Post-regression estimates including predicted means and pairwise comparison of effects were examined to quantify the independent and joint effects of household socioeconomic disadvantage and time period. Mixed models accounted for school-level clustering. Statistical significance was set at p < 0.05. All analyses were performed using STATA Version 17.0 (College Station, TX: Stata Press. StataCorp. 2019).
Results
Overall, 5,384 participants were included in the final analysis; this includes complete data from 3,422 surveys during the pre-pandemic period (fall 2018, 2019), 944 surveys from the early pandemic period (fall 2020), and 1,018 surveys from the mid-pandemic period (fall 2021). The sociodemographic data of the participants included in the analysis are presented in Table 1. Mothers (92.4%) completed the majority of the surveys. In all three time periods, a majority of the children studied in grades 3–5 (pre: 39.7%; early: 47.9%; mid: 45.4%), and belonged to Mexican American/Hispanic/Latino race/ethnicity (pre: 83.7%; early: 82.4%; mid: 81.5%). According to parent demographic data, a majority of the parents either attended or completed high school (pre: 53.5%; early: 57.9%; mid: 52.1%), and were voluntarily unemployed (pre: 50%; early: 48.2%; mid: 55.6%). More than three-quarters of the parents reported participating in government assistance programs (pre: 87.9%; early: 93.6%; mid: 92.3%), and approximately quarter of them reported food insecurity (pre: 26.7%; early: 15.3%; mid: 25.4%). A majority of the participants were at greatest disadvantage; more than one-third belonged to high socioeconomic disadvantage groups during all the time periods (pre: 38.6%; early: 42.6%; mid: 44.1%).
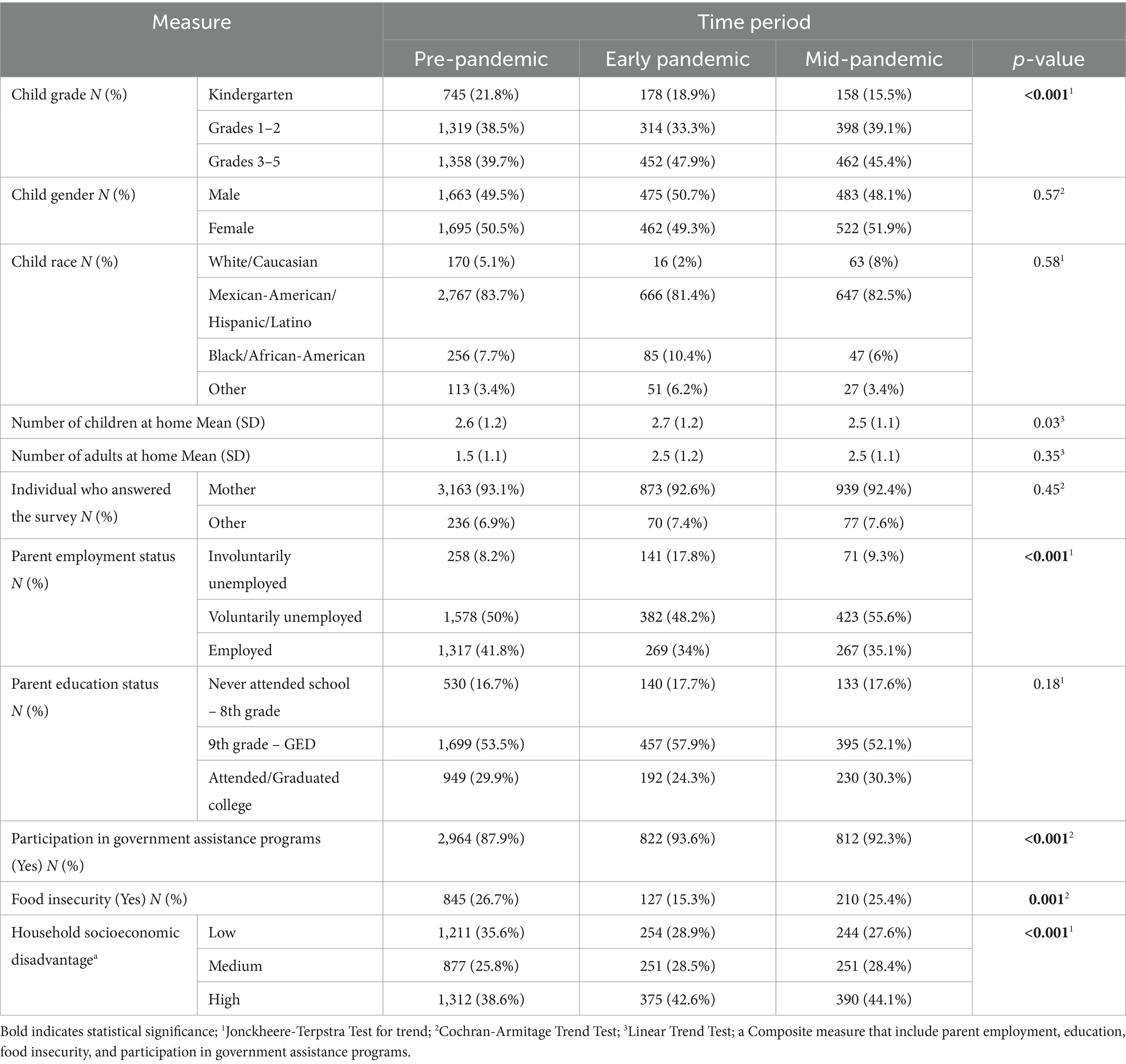
Table 1. Sociodemographic summary of the families included in the analysis (Brighter Bites pre-fall parent surveys 2018–2022).
Changes in unhealthy food consumption over the course of the pandemic
A significant negative trend was observed in the sugary foods scale, indicating a decrease in the consumption of sugary food from the pre- to mid-pandemic period (p < 0.001). For the convenience/fast food scale, we noticed a slight increase in consumption from the pre- to early pandemic, followed by a decrease to the mid-pandemic. No significant linear trend was observed (p = 0.57; Table 2).
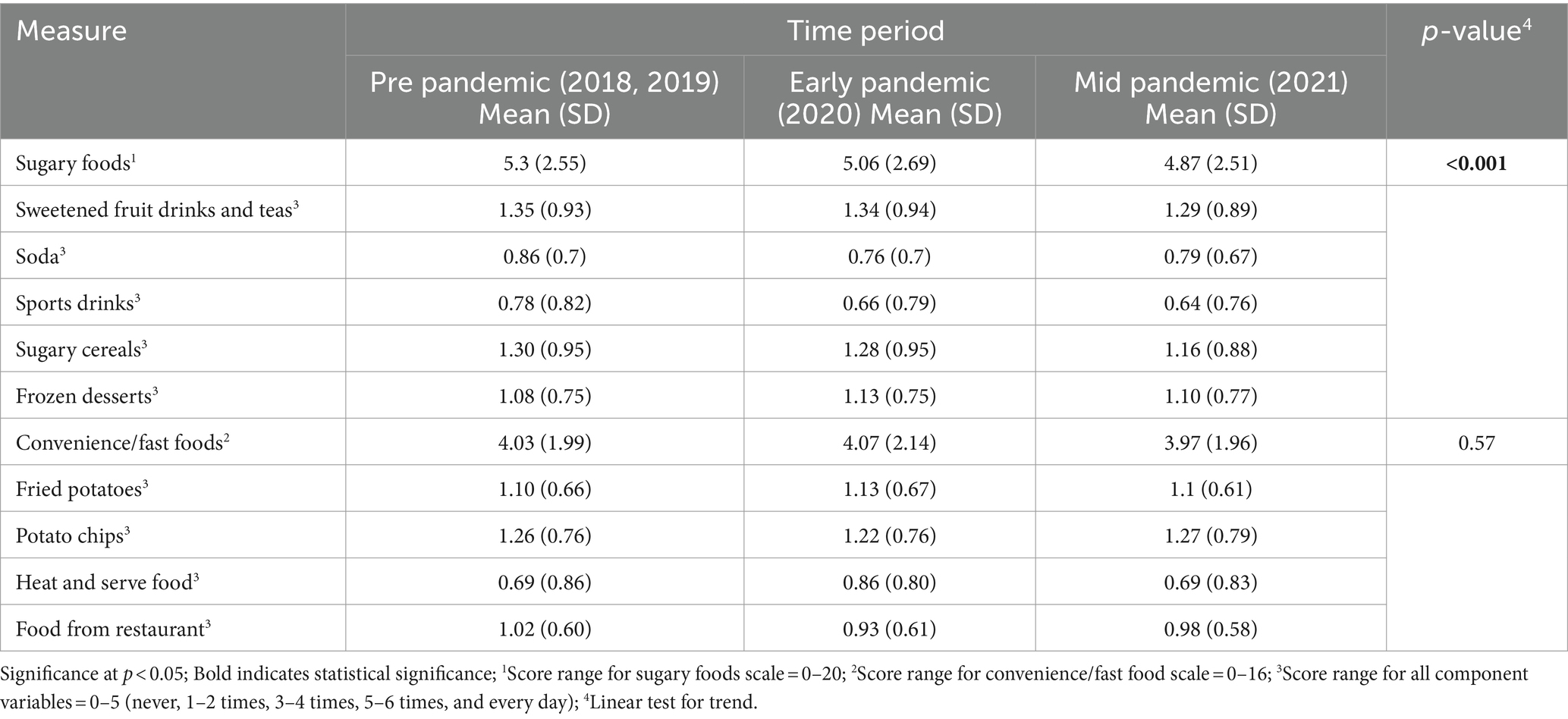
Table 2. Serial cross-sectional changes in child unhealthy food consumption through the course of the pandemic (Brighter Bites 2018–2022).
Mixed effect models were used to estimate the magnitude of change in sugary foods and convenience/fast foods scale during the pandemic as compared to pre-pandemic period. As compared to the pre-pandemic period, sugary food consumption decreased in the early pandemic period (β = −0.29; 95% CI: −0.56, −0.02; p = 0.032), and in the mid-pandemic period (β = −0.51; 95% CI: −0.76, −0.25; p = <0.001), after adjusting for confounders. Convenience/fast food consumption showed only slight and non-significant decreases in the early pandemic period (β = −0.04; 95% CI: −0.24, 0.15; p = 0.654), and in the mid-pandemic (β = −0.12; 95% CI: −0.03, 0.07; p = 0.216), as compared to pre-pandemic time period (Table 3).
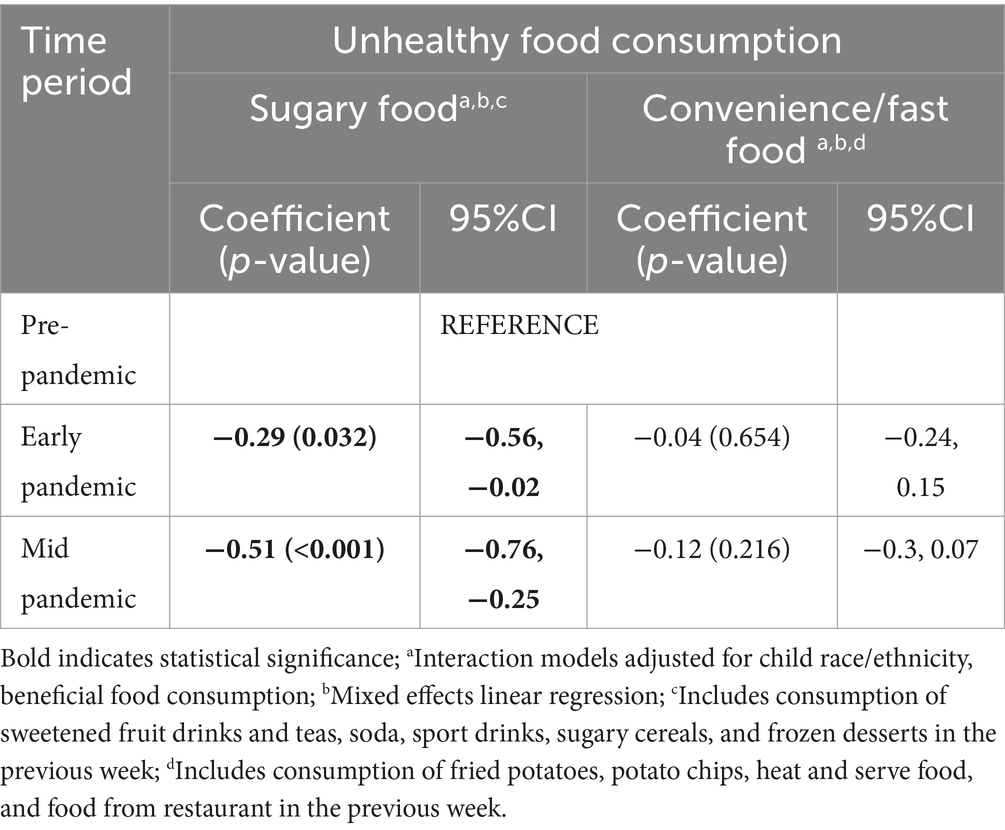
Table 3. Magnitude of change in unhealthy food consumption during the pandemic as compared to pre-pandemic period.
Association between unhealthy food consumption and household socioeconomic disadvantage
Table 4 examines differences in unhealthy food consumption across household socioeconomic disadvantage categories using data pooled across the pandemic, i.e., without reference to time period. Overall, we noticed that lower unhealthy food consumption among those who were more disadvantaged. Pooled across study periods, sugary food and convenience/fast food consumption appears to be highest in the low socioeconomic disadvantage group (reference group, Table 4). As compared to the low socioeconomic disadvantage group, sugary food consumption was significantly lower in the medium disadvantage group (β = −0.2; p = 0.036, 95% CI: −0.38, −0.013), and in the high socioeconomic disadvantage group (β = −0.16; p = 0.06, 95% CI: −0.33, −0.006), after adjusting for confounders. As compared to the low socioeconomic disadvantage group, convenience/fast food consumption was lower in the medium disadvantage group (β = −0.28; p = <0.001, 95% CI: −0.48, −0.20) and in the high disadvantage group (β = −0.34; p = <0.001, 95% CI: −0.41, −0.15), after adjusting for confounders.
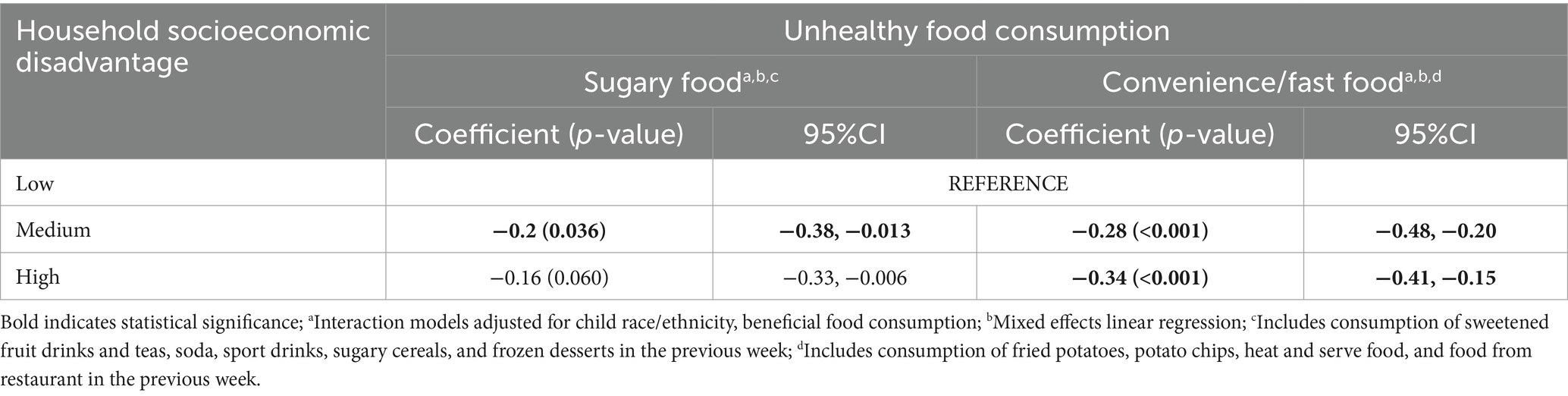
Table 4. Cross-sectional associations of unhealthy food consumption with household socioeconomic disadvantage (pooled data from 2018 to 2022).
Interaction effect of household socioeconomic disadvantage and time period on unhealthy food consumption
The post-regression estimates from the adjusted interaction model show that the socioeconomic differences in convenience/fast food consumption disappeared during the mid-pandemic phase (Table 5).The significant association between convenience/fast food consumption and household socioeconomic disadvantage was seen in pre-pandemic (pairwise estimate low vs. high socioeconomic disadvantage group: contrast = 0.33, p ≤ 0.001; low vs. medium socioeconomic disadvantage group: contrast = 0.31, p ≤ 0.001); and mid-pandemic period (pairwise estimate low vs. high socioeconomic disadvantage group: contrast = 0.27, p ≤ 0.001; low vs. medium socioeconomic disadvantage group: contrast = 0.22, p ≤ 0.001) time periods.
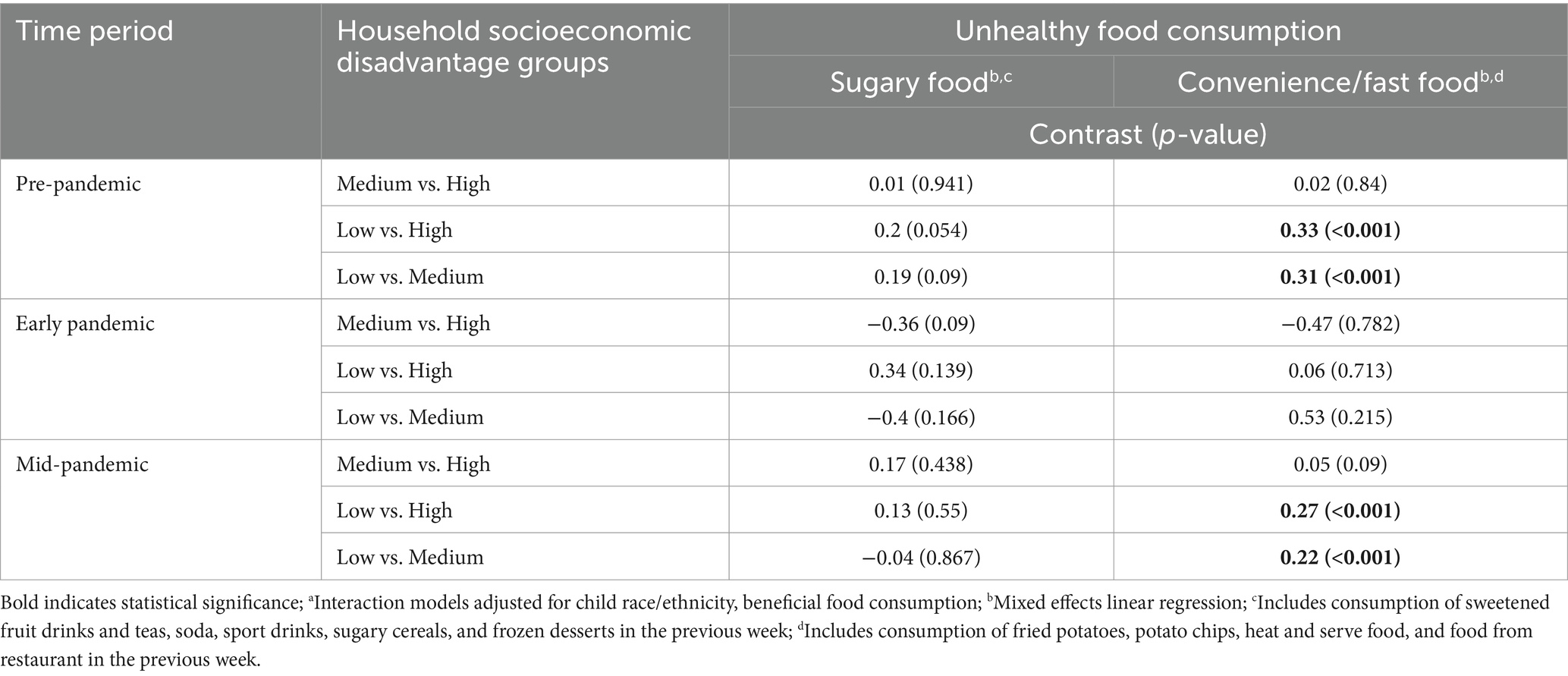
Table 5. Post regression estimates (pairwise comparison of effects) from the adjusteda interaction model.
Discussion
Periods of instability can cause significant changes in dietary behaviors. Although evidence of the short-term impacts of the COVID-19 pandemic has been explored by studies across the globe, there is little evidence of the long-term effects in the years following the pandemic. Our study investigated serial cross-sectional changes in unhealthy food consumption over the course of the pandemic. We observed a significant minor decrease in sugary food consumption during the early and mid-pandemic phases. In regard to convenience/fast food consumption, we observed a slight increase in consumption from the pre- to early pandemic, followed by a decrease to the mid-pandemic.
These results only partially align with the results from other national (33, 39–41) and international studies (9, 18, 42, 43); a majority of other studies that collected data in the first months of the pandemic (March–April 2020) report contradictory results (15–18). A cross-sectional study conducted by Adams et al. (20) reported a decrease in sweets and dessert consumption among approximately one-third of food-insecure families (20). A study conducted in Greece among secondary school students also reported a decrease in sweets and sugary drinks (42). We hypothesize that this may be partly attributed to the time of data collection. In a longitudinal study that examined changes in home food availability, it was noted that although about one-third of the sample reported an increase in desserts at home in May 2020, a decrease in the same was noticed in 30% of the families in September 2020 (33). As the data for our study was collected in the fall of each year, it is possible that “panic-buying” and “comfort food” purchases had subsided, and that the children had already adapted to their new lifestyle (33, 44). Another reason could also be the pandemic-related waivers in the implementation of government nutrition programs. For instance, state agencies reported that utilization of the COVID-19 Child Nutrition nationwide waivers improved the implementation of the National School Lunch Program (NSLP), Summer Food Service Program, and Child and Adult Care Food Program (45). Similarly, Adams et al. (46) noted that in 2021, parents who participated in child tax credit expansion reported a significant decrease in children’s consumption of added sugar and sugar-sweetened beverages (46). In addition to this, innovative implementation of health promotion programs such as non-profit–for-profit partnerships (47) and direct to consumer models (48), have been proven effective to improve access to fresh food in times of crises (49). It is important to evaluate the public health impact of pandemic-related policies and novel solutions, introduced during a disaster, on the behaviors of individuals in different economic strata.
We also observed heterogeneity in unhealthy food consumption among children, by socioeconomic disadvantage levels. There were significantly lower levels of convenience/fast food and sugary food consumption among those who were most disadvantaged. Of note, this sample was homogenously lower income given that one of the eligibility criteria for participating in Brighter Bites is that the school composition is >75% of the children receive free/reduced lunch program. However, even within our lower income sample, we saw differences by SES disadvantage. Previous studies have reported discrepancies in the association between socioeconomic status and eating behaviors. A study that examined family-affluence-related inequities in adolescent food consumption among 41 countries reported that in some countries, adolescents from the lowest family affluence consumed fewer fruits, vegetables, sweets, and chocolates (50). The low budget constraint and limited ability to buy food of any kind may explain this result (18, 50). Notably, the socioeconomic disadvantage measure in our study included multiple components. Previous studies report that children’s reduced consumption of healthy food was associated with mothers’ higher education and/or a full-time employment status (51). Parents who work full-time or multiple jobs may face time constraints in meal planning, preparation, and consequently in providing healthier food for their children (52, 53). However, we noticed a lack of socioeconomic heterogeneity in convenience/fast food consumption during early pandemic period. This may be attributed to the relatively uniform impact of the early pandemic period experiences across the disadvantaged groups of the low-income sample (54). Food supply chain disruptions and restaurant closures might have minimized differences in fast-food consumption since fewer families, regardless of their specific level of disadvantage, could easily obtain these foods. These findings underscore the critical need to develop sustainable and resilient food systems that ensure reliable access to healthy food options for all socioeconomic groups, particularly in times of crisis. It is imperative to examine multiple barriers to healthy food access that arise during and after a disaster, using comprehensive and nuanced measures (49). Moving beyond physical access to food, studies have also recorded the urgency of investigating other factors such as social accessibility, cultural acceptability, and food agency during a crisis and addressing these factors through community cross-sectoral collaboration (49, 55).
Our study was novel in examining the changes in unhealthy food consumption and its association with household socioeconomic disadvantage through the course of a public health crisis. Using multi-site data, the external validity of the study is strengthened. The serial cross-sectional nature of our data, along with access to pre-pandemic data helped us investigate changes over time, which is an added strength to this study. However, the validity of the study results may have been compromised due to multiple reasons. The results may have limited generalizability to other populations across the country, a. since those who participated in our study may have been in extreme need of help during the COVID-19 pandemic, b. a majority of our participants belonged to the Mexican/Hispanic/Latino race ethnicity. As this ethnic group exhibits a collectivist cultural lifestyle, the home environment findings reported may not be generalizable to individualistic group. The study may also be subjected to selection bias since study surveys were available only to those with digital access. The data may also be subjected to social desirability bias due to the self-reporting nature of the surveys. Finally, low response rate could have led to non-random loss of data.
Conclusion
Our findings provide valuable insights into the varied impact of an unprecedented crisis on unhealthy food consumption of children from low-income families at different levels of socioeconomic disadvantage. The results can serve as a benchmark for community or government organizations to design tailored policies/intervention strategies that address the specific challenges faced by underserved communities. Careful investigation is required in qualifying a community as economically vulnerable to disasters or economic shutdowns. Further research needs to be conducted to understand the nuances of socioeconomic dynamics on the diet behaviors of families-in-need in the post-pandemic setting.
Data availability statement
The data analyzed in this study are not publicly available. Data may be made available upon reasonable request to the corresponding author. Requests to access these datasets should be directed to Tml2ZWRoaXRoYS5wcEBnbWFpbC5jb20=.
Ethics statement
The studies involving humans were approved by the University of Texas Health Science Center at Houston (UTHealth Houston) School of Public Health Office of Student Research. The parent study was approved by the UTHealth Houston Committee for Protection of Human Subjects (IRB# HSC-383 SPH-15-0752). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NP: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. NR: Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation. R-JC: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. CM: Writing – original draft, Writing – review & editing, Conceptualization, Supervision, Validation. MP: Writing – original draft, Writing – review & editing, Data curation, Methodology, Resources. JN: Methodology, Resources, Writing – original draft, Writing – review & editing, Data curation. DE: Writing – original draft, Writing – review & editing. SS: Methodology, Resources, Writing – original draft, Writing – review & editing, Conceptualization, Formal analysis, Funding acquisition, Investigation, Visualization.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study is funded by UTHealth Houston – Cancer Prevention Research Institute of Texas Innovation for Cancer Prevention Research Pre-Doctoral Fellowship (Grant #RP210042). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Cancer Prevention Research Institute of Texas.
Acknowledgments
The authors would like to thank Brighter Bites, participating schools, and families.
Conflict of interest
Shreela Sharma serves on the board of directors of Brighter Bites 501c3 nonprofit organization. This is an unpaid board position.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Willett, WC, Koplan, JP, Nugent, R, Dusenbury, C, Puska, P, and Gaziano, TA. Prevention of chronic disease by means of diet and lifestyle changes In: DT Jamison, JG Breman, AR Measham, G Alleyne, M Claeson, and DB Evans, editors. Disease Control Priorities in Developing Countries. 2nd ed. Washington, DC: The International Bank for Reconstruction and Development (2006)
2. World Health Organization . Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation. World Health Organization. (2003).
3. Liu, J, Micha, R, Li, Y, and Mozaffarian, D. Trends in food sources and diet quality among US children and adults, 2003-2018. JAMA Netw Open. (2021) 4:e215262. doi: 10.1001/jamanetworkopen.2021.5262
4. Liu, J, Lee, Y, Micha, R, Li, Y, and Mozaffarian, D. Trends in junk food consumption among US children and adults, 2001–2018. Am J Clin Nutr. (2021) 114:1039–48. doi: 10.1093/ajcn/nqab129
5. Liu, J, Rehm, CD, Onopa, J, and Mozaffarian, D. Trends in diet quality among youth in the United States, 1999-2016. JAMA. (2020) 323:1161–74. doi: 10.1001/jama.2020.0878
6. Chang, T, Chen, Y, Chen, W, Chen, CY, Hsu, WY, Chou, Y, et al. Weight gain associated with COVID-19 lockdown in children and adolescents: a systematic review and meta-analysis. Nutrients. (2021) 13:3668. doi: 10.3390/nu13103668
7. Keith-Jennings, B, Nchako, C, and Llobrera, J. Number of families struggling to afford food rose steeply in pandemic and remains high, especially among children and households of color. Center on Budget and Policy Priorities (2021).
8. Lange, SJ, Kompaniyets, L, Freedman, DS, Kraus, EM, and Porter, RDNP3, et al. Longitudinal trends in body mass index before and during the COVID-19 pandemic among persons aged 2-19 years - United States, 2018-2020. MMWR Morb Mortal Wkly Rep. (2021) 70:1278–83. doi: 10.15585/mmwr.mm7037a3
9. Perrar, I, Alexy, U, and Jankovic, N. Changes in total energy, nutrients and food group intake among children and adolescents during the COVID-19 pandemic-results of the DONALD study. Nutrients. (2022) 14:297. doi: 10.3390/nu14020297
10. Braveman, PA, Cubbin, C, Egerter, S, Chideya, S, Marchi, KS, Metzler, M, et al. Socioeconomic status in health research: one size does not fit all. JAMA. (2005) 294:2879–88. doi: 10.1001/jama.294.22.2879
11. Wolf, S, Gennetian, LA, Morris, PA, and Hill, HD. Patterns of income instability among low-and middle-income households with children. Fam Relat. (2014) 63:397–410. doi: 10.1111/fare.12067
12. Han, W, and Hart, J. Job precarity and economic prospects during the COVID-19 public health crisis. Soc Sci Q. (2021) 102:2394–411. doi: 10.1111/ssqu.13031
13. Seabrook, JA, and Avison, WR. Socioeconomic status and cumulative disadvantage processes across the life course: implications for health outcomes. Can Rev Sociol. (2012) 49:50–68. doi: 10.1111/j.1755-618X.2011.01280.x
14. Abrams, EM, Greenhawt, M, Shaker, M, Pinto, AD, Sinha, I, and Singer, A. The COVID-19 pandemic: adverse effects on the social determinants of health in children and families. Ann Allergy Asthma Immunol. (2022) 128:19–25. doi: 10.1016/j.anai.2021.10.022
15. Schanzenbach, D, and Pitts, A. How much has food insecurity risen? Evidence from the census household pulse survey. Institute for Policy Research Rapid Research. Report. (2020) 1:1–10. Available at: https://www.ipr.northwestern.edu/documents/reports/ipr-rapid-research-reports-pulse-hh-data-10-june-2020.pdf
16. Sharma, SV, Upadhyaya, M, Bounds, G, and Markham, C. A public health opportunity found in food waste. Prev Chronic Dis. (2017) 14:14. doi: 10.5888/pcd14.160596
17. Hecht, AA, Dunn, CG, Kinsey, EW, Read, MA, Levi, R, Richardson, AS, et al. Estimates of the nutritional impact of non-participation in the national school lunch program during COVID-19 school closures. Nutrients. (2022) 14:1387. doi: 10.3390/nu14071387
18. Gedeon, R, Hallit, S, and Wakim, LH. Food insecurity and eating habits of lebanese children aged 5-11 years during the COVID-19 pandemic and the socioeconomic crisis: a national study. BMC Public Health. (2022) 22:1982. doi: 10.1186/s12889-022-14387-z
19. O'Meara, L, Turner, C, Coitinho, DC, and Oenema, S. Consumer experiences of food environments during the covid-19 pandemic: global insights from a rapid online survey of individuals from 119 countries. Glob Food Sec. (2022) 32:100594. doi: 10.1016/j.gfs.2021.100594
20. Adams, EL, Caccavale, LJ, Smith, D, and Bean, MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity. (2020) 28:2056–63. doi: 10.1002/oby.22996
21. Food and Nutrition Service United States Department of Agriculture . SY 2021–22 waivers and flexibilities. Food and Nutrition Service U.S. Department of Agriculture. Available at: https://www.fns.usda.gov/disaster/pandemic/cn-2021-22-waivers-and-flexibilities (Accessed Feb 8, 2023).
22. Center on Budget and Policy Priorities . States are using much-needed temporary flexibility in SNAP to respond to COVID-19 challenges. (2020).
23. Balasuriya, L, Berkowitz, SA, and Seligman, HK. Federal nutrition programs after the pandemic: learning from P-EBT and SNAP to create the next generation of food safety net programs. Inquiry. (2021) 58:5190. doi: 10.1177/00469580211005190
24. OECD . Organisation for economic co-operation and development. Job retention schemes during the COVID-19 lockdown and beyond. Paris, France: OECD Publishing (2020).
26. Sharma, SV, Markham, C, Chow, J, Ranjit, N, Pomeroy, M, and Raber, M. Evaluating a school-based fruit and vegetable co-op in low-income children: a quasi-experimental study. Prev Med. (2016) 91:8–17. doi: 10.1016/j.ypmed.2016.07.022
27. Sharma, SV, Chow, J, Pomeroy, M, Raber, M, Salako, D, and Markham, C. Lessons learned from the implementation of brighter bites: a food co-op to increase access to fruits and vegetables and nutrition education among low-income children and their families. J Sch Health. (2017) 87:286–95. doi: 10.1111/josh.12497
28. Sharma, SV, Chuang, R, Rushing, M, Naylor, B, Ranjit, N, Pomeroy, M, et al. Social determinants of health–related needs during COVID-19 among low-income households with children. Prev Chronic Dis. (2020) 17:E119. doi: 10.5888/pcd17.200322
29. Marshall, AN, Markham, C, Ranjit, N, Bounds, G, Chow, J, and Sharma, SV. Long-term impact of a school-based nutrition intervention on home nutrition environment and family fruit and vegetable intake: a two-year follow-up study. Prev Med Rep. (2020) 20:101247. doi: 10.1016/j.pmedr.2020.101247
30. National Cancer Institute . Family life, activity, sun, health and eating (FLASHE) survey data. National Cancer Institute, (2017).
31. Bennett, G, Young, E, Butler, I, and Coe, S. The impact of lockdown during the COVID-19 outbreak on dietary habits in various population groups: a scoping review. Front Nutr. (2021) 8:626432. doi: 10.3389/fnut.2021.626432
32. Pourghazi, F, Eslami, M, Ehsani, A, Ejtahed, H, and Qorbani, M. Eating habits of children and adolescents during the COVID-19 era: a systematic review. Front Nutr. (2022) 9:1004953. doi: 10.3389/fnut.2022.1004953
33. Adams, EL, Caccavale, LJ, Smith, D, and Bean, MK. Longitudinal patterns of food insecurity, the home food environment, and parent feeding practices during COVID-19. Obes Sci Pract. (2021) 7:415–24. doi: 10.1002/osp4.499
34. Neshteruk, CD, Zizzi, A, Suarez, L, Erickson, E, Kraus, WE, Li, JS, et al. Weight-related behaviors of children with obesity during the COVID-19 pandemic. Child Obes. (2021) 17:371–8. doi: 10.1089/chi.2021.0038
35. Smith, KR, Jansen, E, Thapaliya, G, Aghababian, AH, Chen, L, Sadler, JR, et al. The influence of COVID-19-related stress on food motivation. Appetite. (2021) 163:105233. doi: 10.1016/j.appet.2021.105233
37. Hager, ER, Quigg, AM, Black, MM, Coleman, SM, Heeren, T, Rose-Jacobs, R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. (2010) 126:e26–32. doi: 10.1542/peds.2009-3146
38. Bauer, L, Broady, K, Edelberg, W, and O’Donnell, J. Ten facts about COVID-19 and the US economy. Brookings Institution, No. 17. (2020).
39. Sylvetsky, AC, Kaidbey, JH, Ferguson, K, Visek, AJ, and Sacheck, J. Impacts of the COVID-19 pandemic on children's sugary drink consumption: a qualitative study. Front Nutr. (2022) 9:860259. doi: 10.3389/fnut.2022.860259
40. Adams, EL, Caccavale, LJ, Smith, DI, and Bean, MK. Food insecurity, federal nutrition support, and parent feeding practices during COVID-19: a 1-year follow-up study. Public Health Rep. (2023) 138:323–32. doi: 10.1177/00333549221132532
41. Bekelman, TA, Knapp, EA, Dong, Y, Dabelea, D, Bastain, TM, Breton, CV, et al. Sociodemographic variation in children's health behaviors during the COVID-19 pandemic. Child Obes. (2023) 19:226–38. doi: 10.1089/chi.2022.0085
42. Aguilar-Martinez, A, Bosque-Prous, M, Gonzalez-Casals, H, Colillas-Malet, E, Puigcorbé, S, Esquius, L, et al. Social inequalities in changes in diet in adolescents during confinement due to COVID-19 in Spain: the DESKcohort project. Nutrients. (2021) 13:1577. doi: 10.3390/nu13051577
43. Androutsos, O, Perperidi, M, Georgiou, C, and Chouliaras, G. Lifestyle changes and determinants of children's and adolescents' body weight increase during the first COVID-19 lockdown in Greece: the COV-EAT study. Nutrients. (2021) 13:930. doi: 10.3390/nu13030930
44. Okrent, A, and Zeballos, E. COVID-19 working paper: Consumer food spending changes during the COVID-19 pandemic. (2022).
45. Severn, V, Washburn, L, Frisk, R, and Conway, K. Child nutrition program operations during the COVID-19 pandemic, march through september 2020: school meals operations study (SMO) year 1 report. US Department of Agriculture, Food and Nutrition Service, Office of Policy Support: Alexandria, VA (2023).
46. Adams, E, Brickhouse, T, Dugger, R, and Bean, M. Patterns of food security and dietary intake during the first half of the child tax credit expansion. Health Aff. (2022) 41:680–8. doi: 10.1377/hlthaff.2021.01864
47. Haidar, A, Markham, C, Marshall, A, Chuang, RJ, Spence, M, Boone, J, et al. Innovative partnerships to address food insecurity during the COVID-19 pandemic: the brighter bites produce voucher program. Int J Environ Res Public Health. (2021) 18:9175. doi: 10.3390/ijerph18179175
48. Durant, JL, Asprooth, L, Galt, RE, Schmulevich, SP, Manser, GM, and Pinzón, N. Farm resilience during the COVID-19 pandemic: the case of California direct market farmers. Agric Syst. (2023) 204:103532. doi: 10.1016/j.agsy.2022.103532
49. Clay, L . Post-disaster food & nutrition security: the disaster food security framework (DFSF). UMBC Faculty Collection (2023).
50. Zaborskis, A, Grincaitė, M, Kavaliauskienė, A, and Tesler, R. Family structure and affluence in adolescent eating behaviour: a cross-national study in forty-one countries. Public Health Nutr. (2021) 24:2521–32. doi: 10.1017/S1368980020003584
51. Alsharairi, NA, and Somerset, S. Parental work status and children's dietary consumption: Australian evidence. Int J Consum Stud. (2018) 42:522–32. doi: 10.1111/ijcs.12463
52. Li, J, O'Sullivan, T, Johnson, S, Stanley, F, and Oddy, W. Maternal work hours in early to middle childhood link to later adolescent diet quality. Public Health Nutr. (2012) 15:1861–70. doi: 10.1017/S1368980011003053
53. Sweeting, H, and West, P. Dietary habits and children's family lives. J Hum Nutr Diet. (2005) 18:93–7. doi: 10.1111/j.1365-277X.2005.00592.x
54. Poole, MK, Fleischhacker, SE, and Bleich, SN. Addressing child hunger when school is closed—considerations during the pandemic and beyond. N Engl J Med. (2021) 384:e35. doi: 10.1056/NEJMp2033629
Keywords: diet, unhealthy food, children, COVID-19 pandemic, public health nutrition
Citation: Parthasarathy N, Ranjit N, Chuang R-J, Markham C, Pomeroy M, Noyola J, Ernest DK and Sharma SV (2024) Changes in unhealthy food consumption among vulnerable elementary-aged children in the United States during the COVID-19 pandemic: a serial cross-sectional analysis. Front. Nutr. 11:1468767. doi: 10.3389/fnut.2024.1468767
Edited by:
Gordana Kenđel Jovanović, Teaching Institute of Public Health of Primorsko Goranska County, CroatiaReviewed by:
Eliana Zeballos, Economic Research Service — USDA, United StatesNasreen Moursi, Uniformed Services University of the Health Sciences, United States
Copyright © 2024 Parthasarathy, Ranjit, Chuang, Markham, Pomeroy, Noyola, Ernest and Sharma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nivedhitha Parthasarathy, Tml2ZWRoaXRoYS5wcEBnbWFpbC5jb20=
 Nivedhitha Parthasarathy
Nivedhitha Parthasarathy Nalini Ranjit
Nalini Ranjit Ru-Jye Chuang
Ru-Jye Chuang Christine Markham
Christine Markham Mike Pomeroy4
Mike Pomeroy4 Jacqueline Noyola
Jacqueline Noyola Deepali K. Ernest
Deepali K. Ernest Shreela V. Sharma
Shreela V. Sharma