- 1Center of Excellence in Preventive and Integrative Medicine and Department of Preventive and Social Medicine, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand
- 2Dhurakij Pundit University, Bangkok, Thailand
- 3Department of International Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, United States
- 4Bumrungrad International Hospital, Bangkok, Thailand
- 5Department of Infection Biology & Microbiomes, Faculty of Health and Life Sciences, University of Liverpool, Liverpool, United Kingdom
Background: Thai desserts, celebrated for their exquisite sweetness, are widely enjoyed for personal indulgence and as cherished souvenirs. However, their high sugar content raises concerns regarding health impacts. This study aimed to quantify the glycemic index (GI) and glycemic load (GL) in healthy volunteers following consumption of various Thai desserts, out of 10 renowned desserts from across Thailand, identified by the Tourism Authority of Thailand, characterized by differing sugar levels.
Method: Eight were selected based on the absence of preservatives and microbial or chemical contaminations. Each participant consumed a 50-g serving of available carbohydrate (50avCHO) from these desserts. Ninety-six healthy volunteers, with a mean age of 31.8 ± 5.7 years, a mean body weight of 57.2 ± 7.3 kg, and 63.5% women, were randomized into eight groups, with each group comprising 12 participants. Blood samples were collected pre-and post-consumption to assess GI and GL values following established protocols.
Results: The findings revealed that Phetchaburi’s Custard Cake exhibited the lowest GI and GL values (53.4 and 26.7, respectively), with progressively higher values observed in Saraburi’s Curry Puff (61.8 and 30.9), Nakhon Sawan’s Mochi (68.9 and 34.4), Suphan Buri’s Sponge Cake (75.9 and 38.0), Ayutthaya’s Cotton Candy (81.4 and 40.7), Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit (87.4 and 43.7), Chon Buri’s Bamboo Sticky Rice (109.3 and 54.7), and Lampang’s Crispy Rice Cracker (149.3 and 74.7), respectively.
Conclusion: The study demonstrates that while Thai desserts exhibit a range of GI values, their GL values are uniformly high. It underscores the importance of disseminating GI and GL information to consumers, enabling them to make informed dietary choices and moderate their intake of these sugary delicacies.
Introduction
The dietary glycemic index (GI), a concept introduced in 1981, is a critical measure indicating the impact of digested food on blood glucose levels (1). The glycemic load (GL) complements this by quantifying the change in blood glucose in relation to the carbohydrate amount consumed (2). Both indices are crucial for managing dietary impacts on blood sugar, especially for individuals needing sugar control or managing diabetes (3, 4).
Research on the GI and GL across the globe has been extensive. Studies have highlighted the role of GI in food choice, demonstrating how high-GI foods can rapidly increase blood glucose levels, impacting pancreatic function and escalating the risk of diseases like NCDs, metabolic syndrome, and cardiovascular disease (5–11).
In the United Kingdom, research on commercially available products revealed that most ready-to-eat meals had low-GI values, except for those with high mashed potato content (12). The Middle East, particularly the UAE, has seen studies reporting GI and GL values of traditional foods, providing dietary guidance for the local population (13). In Asia, investigations include the impact of processing on the GI of wheat flour in India (14) and the GI and GL values of traditional Chinese foods (15, 16).
In Thailand, research has primarily focused on rice and fruits. Studies have reported low GI in varieties of rice, including brown and germinated brown rice (17), and explored the relationship between sugar content and GI in Thai fruits (18–20). However, the GI and GL values of Thai desserts, often high in carbohydrates and sugar, remain understudied (21).
Thai desserts are renowned for their taste, vibrant colors, and cultural significance, representing the diverse heritage of Thailand’s provinces (22, 23). These desserts, popular among tourists, highlight regional culinary differences and include unique local ingredients (24). Their high simple carbohydrate sugar content may significantly impact gut microflora (25).
This study aimed to fill this gap by quantifying the GI and GL of popular Thai desserts, thus contributing to the international database. This information will help consumers make informed dietary choices, potentially reducing disease risk and aiding in weight management and insulin regulation. Additionally, the study will provide dietary recommendations based on the glycemic response of the desserts, ensuring safety through chemical and microbiological analysis before trials (21).
Participants and methods
Food identification
The selection of desserts for this study was based on a comprehensive survey conducted by the Tourism Authority of Thailand (TAT) across 76 Thai provinces (24). This survey identified a range of popular foods and desserts, from which 44 foods and 10 desserts were selected for further study based on their popular ratings.
For each of the 10 desserts, representing 10 distinct provinces from four major regions of Thailand, three brands (labeled as a, b, and c) were randomly selected. This selection process ensured a diverse representation of regional culinary traditions. The provinces and their respective desserts included the following:
• Northern region: Lampang’s Crispy Rice Cracker/Khao-Tan (P04), Kamphaengphet’s Grass Jelly/Chao-Guay (P03), and Nakhon Sawan’s Mochi/Mo-Ji (P05).
• Central region: Suphan Buri’s Sponge Cake/Sa-Lee (P10), Ayutthaya’s Cotton Candy/Roti-Sai-Mai (P01), and Saraburi’s Curry Puff/Ka-Ree-Puff (P09).
• Western region: Phetchaburi’s Custard Cake/Khanom-Mo-Kaeng (P07), and Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit/Pai-Sap-Pa-Ros (P08).
• Eastern region: Chonburi’s Bamboo Sticky Rice/Khao-Lam (P02).
• Southern region: Phatthalung’s Caramel/Ka-La-Mae (P06).
These desserts were sourced from a variety of shops across Thailand and chosen through a random selection process. The selection criteria for these shops were rigorously defined to ensure quality and authenticity. The criteria included the following:
1. Local production: Shops must exclusively produce and distribute dessert products within their province, ensuring the authenticity and regional specificity of the desserts.
2. Food Safety Certification: Shops must hold at least one food safety certificate from a recognized official agency. This could include a food quality assurance certificate from the Food and Drug Administration (FDA) within the Ministry of Public Health (Division of Consumer Protection) or a food safety certificate from the Public Health Pharmacy Group Provincial Public Health Office.
3. Product Labeling: The name and manufacturer of each dessert product must be clearly stamped on the product label, providing traceability and transparency.
From each selected shop, three different products of the same dessert type were obtained, amounting to a total of 30 brands. This approach aimed to capture the variety within each dessert category while maintaining a controlled and systematic sampling.
Food contamination and nutrition value analysis
This stage of the study focused on a comprehensive analysis of ten products, each representing one from the three brands of the top 10 renowned Thai desserts, to evaluate food safety and nutritional value.
Preservative analysis
To detect benzoic acid and sorbic acid, the selected dessert samples were subjected to the high-performance liquid chromatography method (HPLC). The samples were prepared by cutting them into small pieces, drying, and powdering; 10 g of each powdered sample was dissolved in a methanol and 0.01 M ammonium acetate water buffer (2:3 v/v), sonicated for 10 min for complete extraction, and centrifuged at 3,000 rpm for 5 min. The resulting supernatant was filtered through a 0.45-μm cellulose membrane syringe filter before being analyzed using on an Agilent 1,100 HPLC column. Concentrated samples were diluted further with the mobile phase for precision.
Microbial contamination analysis
The microbial quality assessment involved checking for total aerobic plate count (APC), yeast, and mold (26). The methods used adhered to the FDA guidelines and were carried out by the Food Quality Assurance Service Center (FQA), a division of the Institute of Food Research and Product Development (IFRPD). Detected microorganisms in the dessert products were then identified at the FQA laboratory, which is accredited in food testing. This analysis ensures comprehensive safety evaluation in terms of microbiological content.
Nutritional value analysis
Using an HPLC, the nutritional content of the desserts was analyzed to understand their health implications. This included quantifying key nutritional components to offer insights into the nutritional profile of these traditional Thai desserts.
Ethical considerations
The research protocol for this study was meticulously reviewed and approved by the Ethics Committee for Human Research, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (COA No. 1414/2021, IRB No.696/63). Prior to randomization, all subjects were thoroughly informed about the purpose, procedures, potential risks, and benefits of the study. To ensure informed decision-making, each participant provided written and signed informed consent, reflecting their voluntary agreement to participate after understanding all aspects of the study. This process was in strict compliance with the ethical guidelines stipulated in the Declaration of Helsinki of the World Medical Association and the International Conference on Harmonization Guidelines for Good Clinical Practice. Furthermore, to maintain transparency and accountability, the study protocol was registered with the Thai Clinical Trials Registry (TCTR20201008003) before enrolling the first participant.
Study design, subjects, and blood sample collection
This investigation was structured as an open-label, randomized clinical trial designed to adhere to robust scientific standards and ensure the reliability of the results. The trial followed a systematic approach for participant eligibility determination, encompassing a comprehensive history taking, health check-up, and physical examination, assessment of waist circumference and body mass index (BMI), and blood laboratory tests.
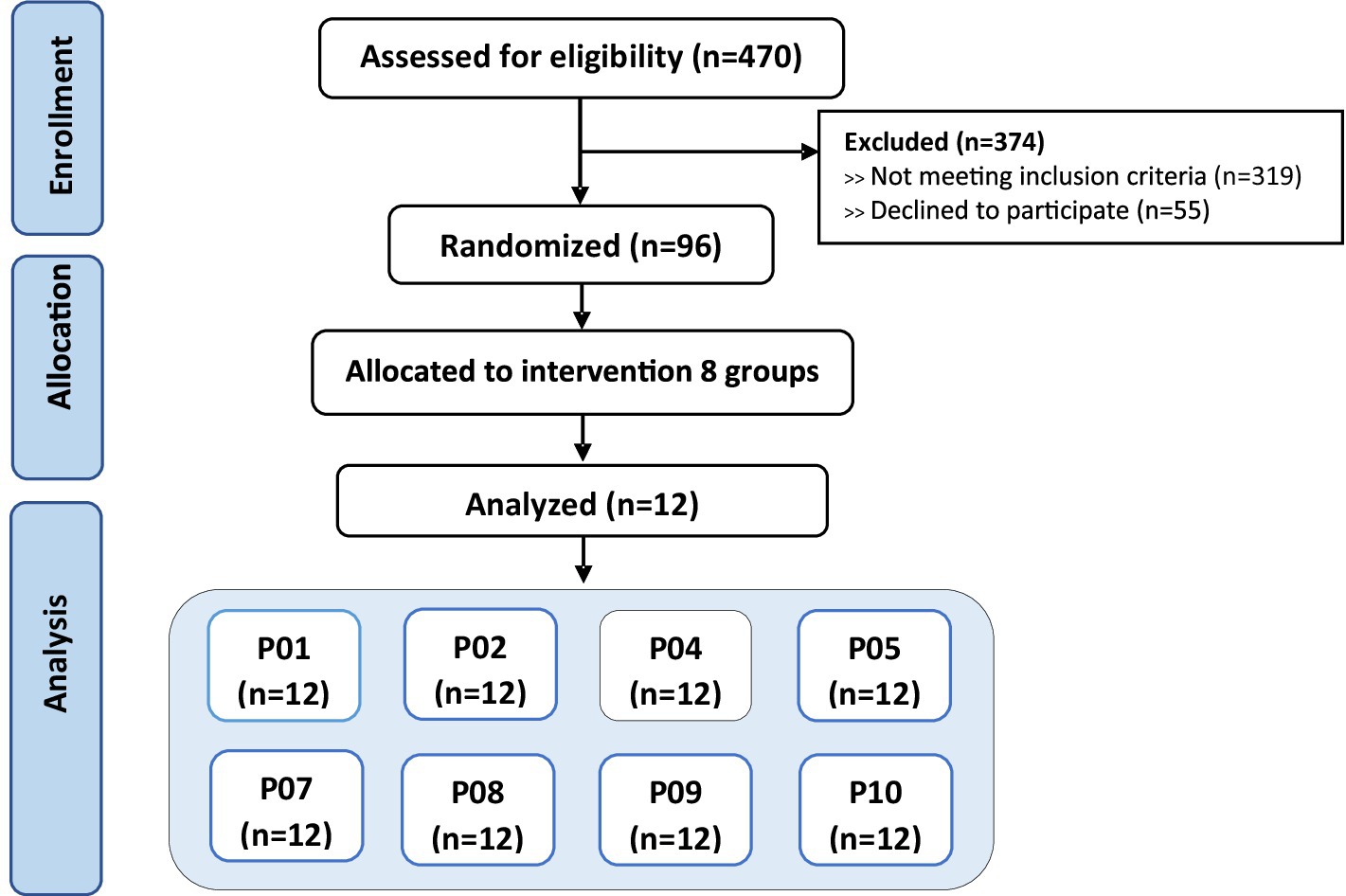
A total of 96 healthy Thai volunteers were enrolled in the study. Participants were Thai men and women aged between 18 and 45 years, in good general health with no chronic medical conditions. They had no history of metabolic disorders, such as diabetes mellitus, impaired glucose tolerance, metabolic syndrome, cardiovascular disease, kidney disease, or gastrointestinal diseases. Additionally, participants were not taking any regular medications that could affect glucose metabolism. Laboratory assessments confirmed that all participants had normal values for fasting blood sugar, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, and HbA1c. Physical examinations showed normal findings, including appropriate waist circumference and BMI within the normal range according to Asian standards (18.5–22.9 kg/m2). Participants were excluded if they had any underlying medical conditions known to influence glucose tolerance or metabolism, a first-degree family history of diabetes mellitus, or abnormal laboratory values outside the normal reference ranges. Those who were taking medications impacting glucose levels, engaged in heavy smoking (more than 10 cigarettes per day), or excessive alcohol consumption were also excluded. Pregnant or breastfeeding women were not eligible to participate (Figure 1).
Participants were randomly assigned to one of eight dessert groups, with each group comprising 12 subjects (n = 12). Each participant received only one type of dessert to test. This random assignment ensured that each dessert was evaluated by 12 different participants. There were no dropouts during the study duration; all participants completed the trial as per the protocol.
Baseline characteristics of all subjects included normal fasting blood glucose levels. The protocol of the study drew inspiration from the methodologies described by Brouns et al. (27, 28) and incorporated methods suggested by the FAO/WHO for glycemic response studies (21). According to the FAO/WHO guidelines, for reliable GI determination, a test should be conducted on six or more subjects, while testing on ten subjects is recommended for greater statistical power and precision (27). Venous blood samples from each subject were collected and processed. Within 30 min of collection, the samples were centrifuged to separate plasma, which was then promptly delivered for blood glucose level analysis.
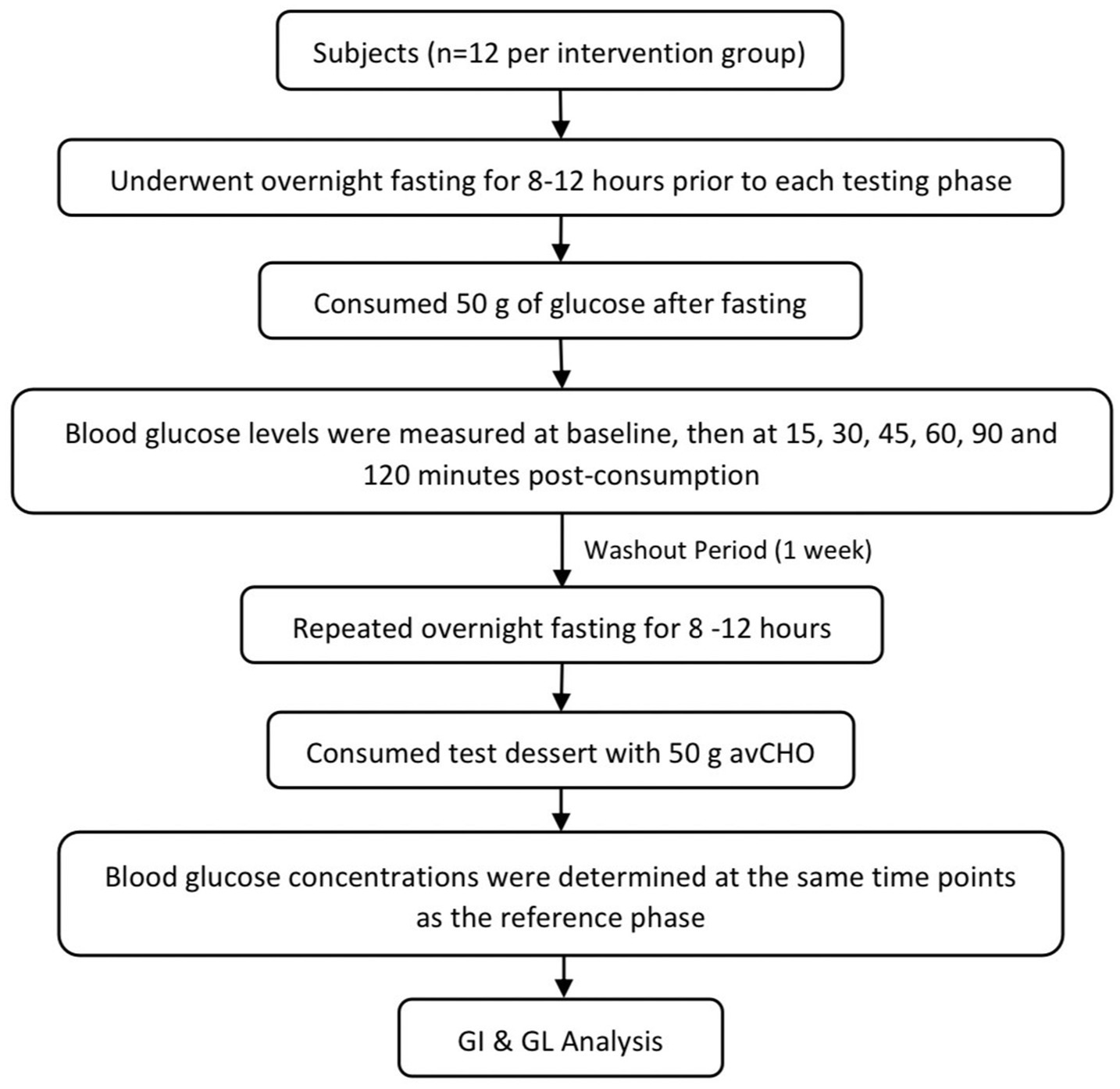
Determination of glycemic index and glycemic load
Participants fasted overnight for 8–12 h before each test. Initially, a reference glucose solution (50 g) was administered, and venous blood samples were collected at intervals of 15, 30, 45, 60, 90, and 120 min post-consumption. Following a 1-week washout period, this procedure was repeated with the test desserts, each providing 50 g of available carbohydrates (avCHO). Blood samples were then drawn by registered nurses using sterile techniques. A volume of 1.5 mL of blood was collected at each time point and immediately sent for glucose analysis. Participants were divided into eight groups, each assigned a different dessert. Blood glucose levels post-dessert consumption were compared with the baseline glucose solution. The glycemic index was calculated by plotting the blood glucose response (area under the curve) against the baseline. This streamlined approach provided a direct comparison of the glycemic response to different Thai desserts, enabling the accurate calculation of their glycemic index and load (Figure 2).
Calculations and statistical analysis
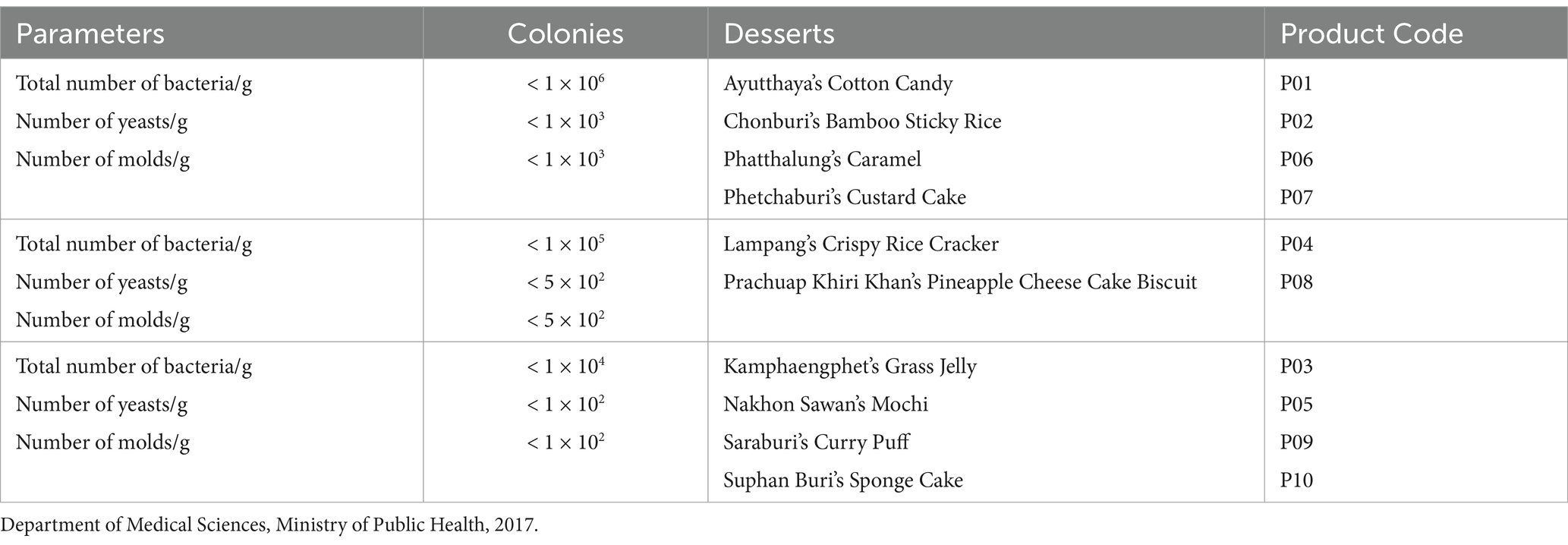
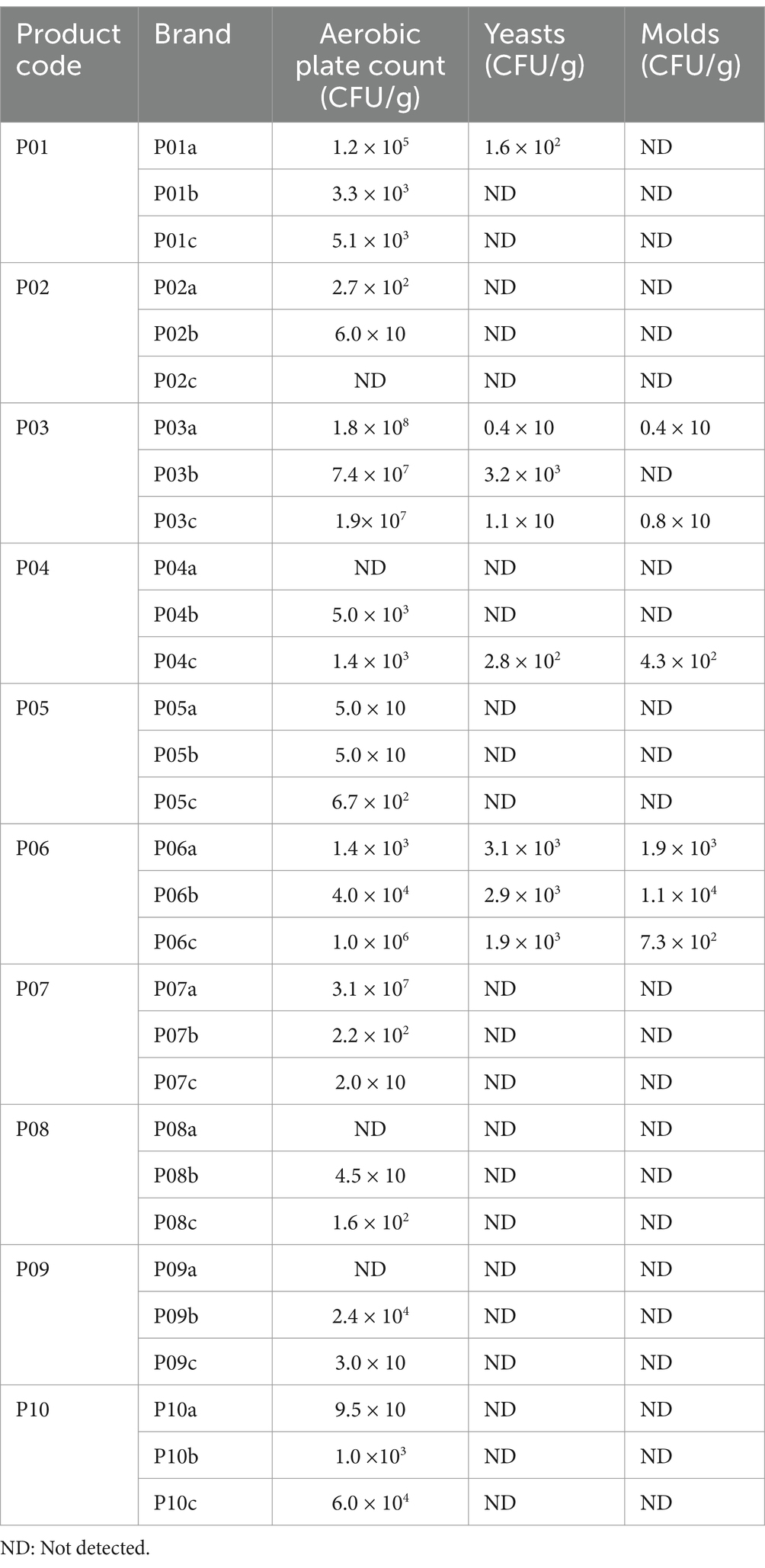
Descriptive statistics were employed to calculate the uptake of preservatives in desserts. The focus was on ensuring that preservative levels remained within the safe limit of <1,000 mg/kg as per regulatory guidelines. Microbial analysis involved total colony count data, expressed in colony-forming units (CFU) per gram of food. This analysis adhered to the quality criteria set by the Department of Medical Sciences, Ministry of Health (29). Results were presented as percentages relative to established standards (Table 1).
The glycemic index (GI) was calculated using the incremental area under the curve (IAUC) method (30). This method involves plotting the blood glucose response over time and applying the trapezoid rule to calculate the area. The GI of each dessert was defined as the IAUC for that dessert, expressed as a percentage of the IAUC for 50 g of glucose, with all areas below baseline excluded. The final GI value for each dessert was derived from the average of results obtained from 12 participants and reported as mean ± SE. The formula used was as follows: GI = (IAUC dessert/IAUC reference glucose) × 100 (27).
The glycemic load (GL) of each dessert was calculated by considering both the GI value and the carbohydrate content per serving. Specifically, the GL was determined by multiplying the GI of the dessert by the amount of available carbohydrates in a 50 g serving (avCHO). The formula used for this calculation is as follows: GL = (GI of the dessert x avCHO in a serving (g))/100 (31).
For statistical analysis, the data were processed using IBM SPSS Statistics version 28. Prior to analysis, the normality of quantitative variables was assessed using the Kolmogorov–Smirnov test, which confirmed that the data were normally distributed (p > 0.05). Results were expressed as percentages, frequencies, and means with standard errors (mean ± SE). Statistical significance was established at a 95% confidence level (p < 0.05). To test the mean differences in baseline data of the subjects, a one-way ANOVA statistical test was applied (32).
Results
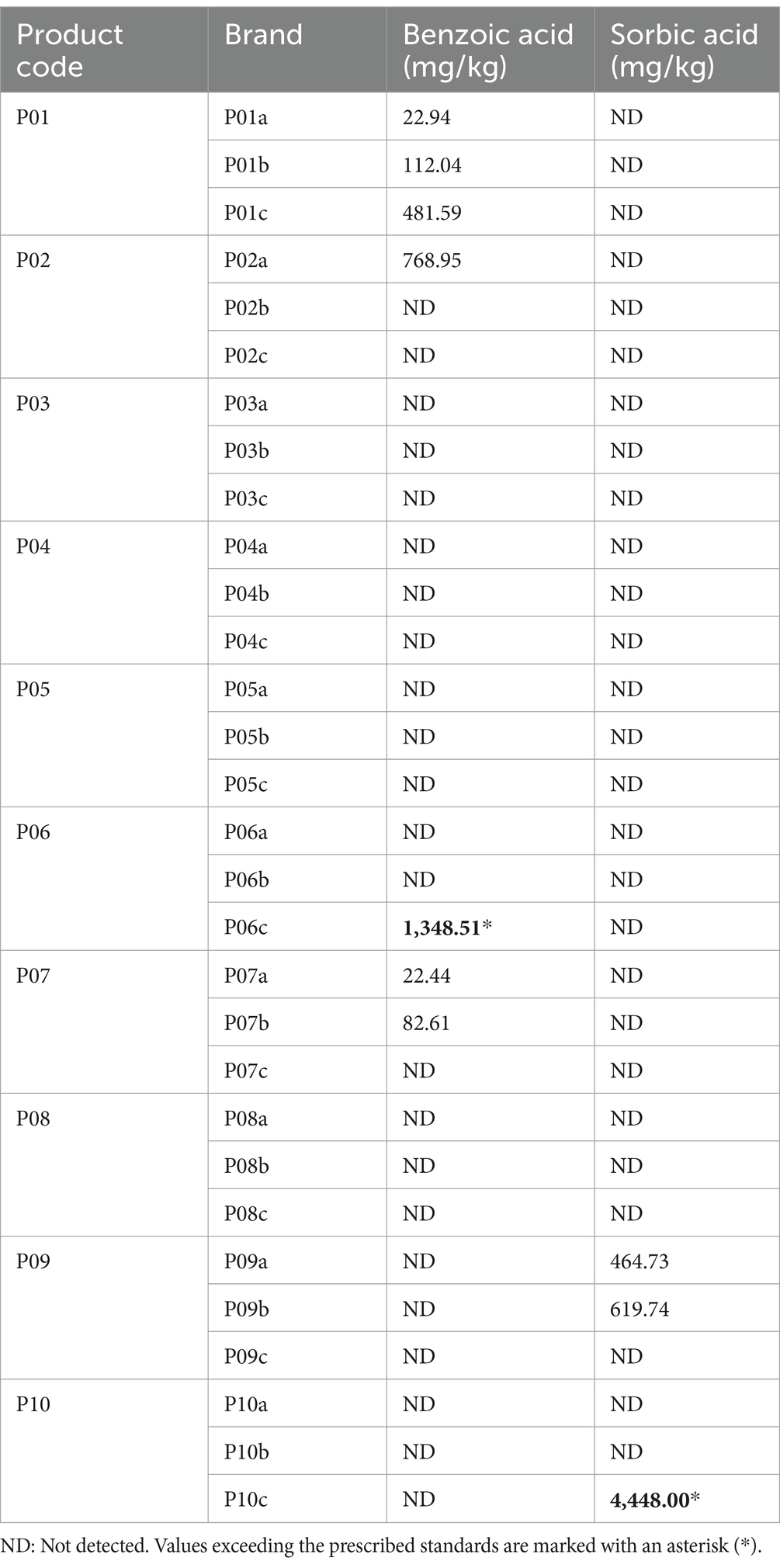
Chemical contamination
Among the 30 brands analyzed for chemical contamination due to preservative use, two brands, constituting 6.7% of the total, were found exceeding the permissible levels of preservatives (Table 2). Specifically, the levels of benzoic acid in brand P06c and sorbic acid in brand P10c surpassed the regulatory limit of 1,000 mg/kg, indicating a significant deviation from accepted food safety standards.
Microbial contamination
Microbial contamination was detected in 12 of the 30 brands tested, accounting for 40% of the total. Specific concerns were identified with certain products. Six brands (P03a, P03b, P03c, P07a, P09b, and P10c) showed bacterial presence beyond acceptable levels. Yeast contamination was observed in four brands (P06a, P06b, P06c, and P03b). Two brands (P06a and P06b) were found to contain mold. Particularly, products P03 and P06 across all brands were deemed unsafe due to the presence of both bacteria and yeast, indicating significant hygiene issues. In addition to microbial concerns, excessive levels of preservatives were found in two brands (P06c and P10c), with benzoic acid and sorbic acid surpassing the safety threshold of 1,000 mg/kg. These findings highlight critical lapses in food safety and hygiene practices for certain brands of Thai desserts (Table 3).
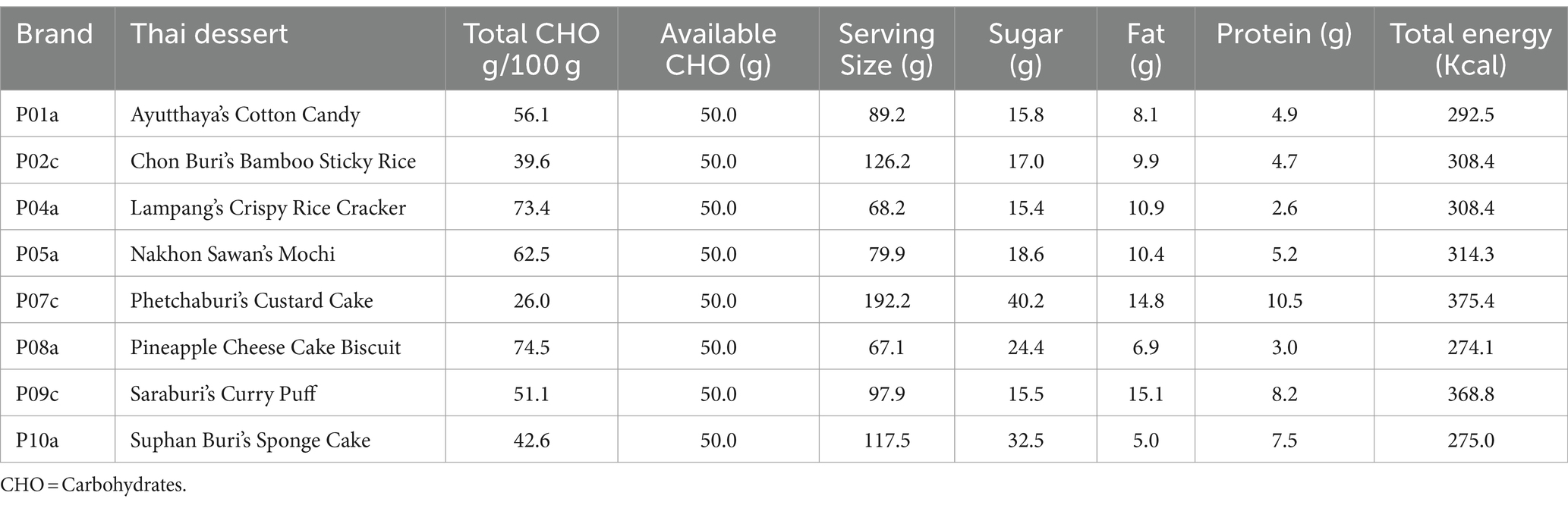
The evaluation identified eight Thai desserts that satisfied the set quality and food safety standards: Ayutthaya’s Cotton Candy (P01), Chon Buri’s Bamboo Sticky Rice (P02), Lampang’s Crispy Rice Cracker (P04), Nakhon Sawan’s Mochi (P05), Phetchaburi’s Custard Cake (P07), Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit (P08), Saraburi’s Curry Puff (P09), and Suphan Buri’s Sponge Cake (P10). The nutritional values of these selected desserts were meticulously analyzed to calculate their GI and GL, essential for assessing the amount consumed by the subjects (Table 4). This nutritional analysis covered total and available carbohydrates, serving sizes, sugar, fat, protein content, and total energy for each dessert. The gathered data facilitated the precise calculation of the GI and GL, which is crucial for evaluating the effects of these desserts on blood glucose levels. Such evaluations are particularly relevant for dietary recommendations aimed at individuals managing their blood sugar levels.
GI and GL of desserts
The study involved 96 healthy subjects divided into eight groups, with a balanced distribution of male and female participants. The subjects had an average age of 31.8 ± 5.7 years, with women comprising 63.5% of the group, and an average weight of 57.2 ± 7.3 kg. The mean Body Mass Index (BMI) across participants was 20.9 kg/m2. Analysis of biochemical baseline data indicated no significant variance between groups (ANOVA; p > 0.05), suggesting homogeneity in baseline characteristics among the groups (Table 5).
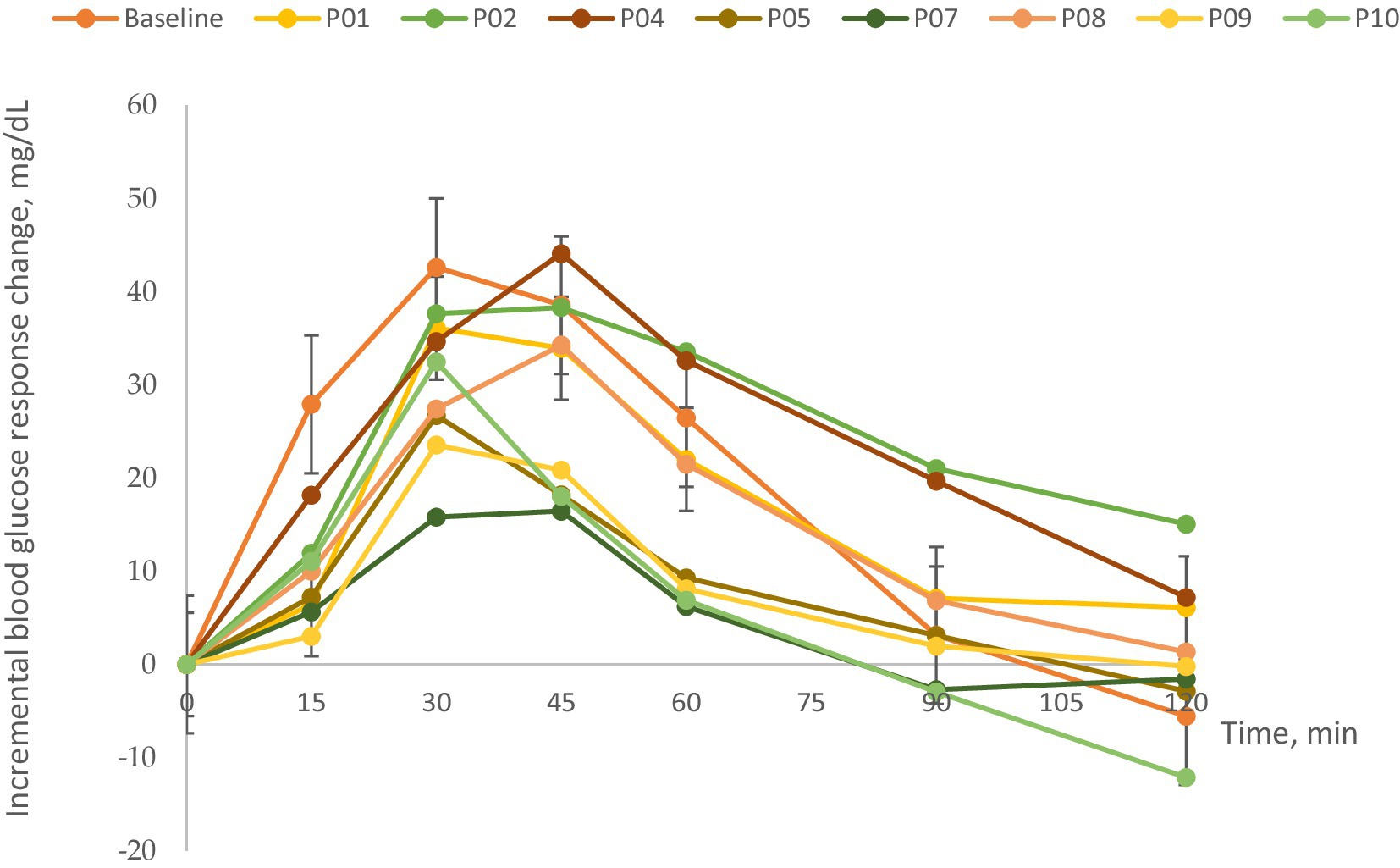
Figure 3 illustrates the mean changes in blood glucose concentrations from fasting baseline levels across the eight test desserts. It was observed that blood glucose levels in subjects peaked between 30 and 45 min following consumption of the selected Thai desserts and normalized by 120 min. This pattern underscores the glycemic response to the desserts, providing insights into their GI and GL values.
The GI and GL values determined for the selected Thai desserts are presented in Table 6. The calculated GI values for the eight desserts varied significantly, ranging from a low of 53.4 to a high of 149.3. According to the classification by Brand-Miller et al. (34), GI values are categorized as low (≤ 55), medium (56–69), and high (≥ 70). Based on this system, Phetchaburi’s Custard Cake had a low GI (53.4), Saraburi’s Curry Puff, and Nakhon Sawan’s Mochi were categorized as medium (61.8 and 68.9, respectively), while the remaining desserts, including Suphan Buri’s Sponge Cake (75.9), Ayutthaya’s Cotton Candy (81.4), Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit (87.4), Chon Buri’s Bamboo Sticky Rice (109.3), and Lampang’s Crispy Rice Cracker (149.3), were classified high. When examining the GL values based on a 50-g available carbohydrate serving, all desserts were classified as high according to the GL classification system by Venn et al. (33) with GL values exceeding 20.
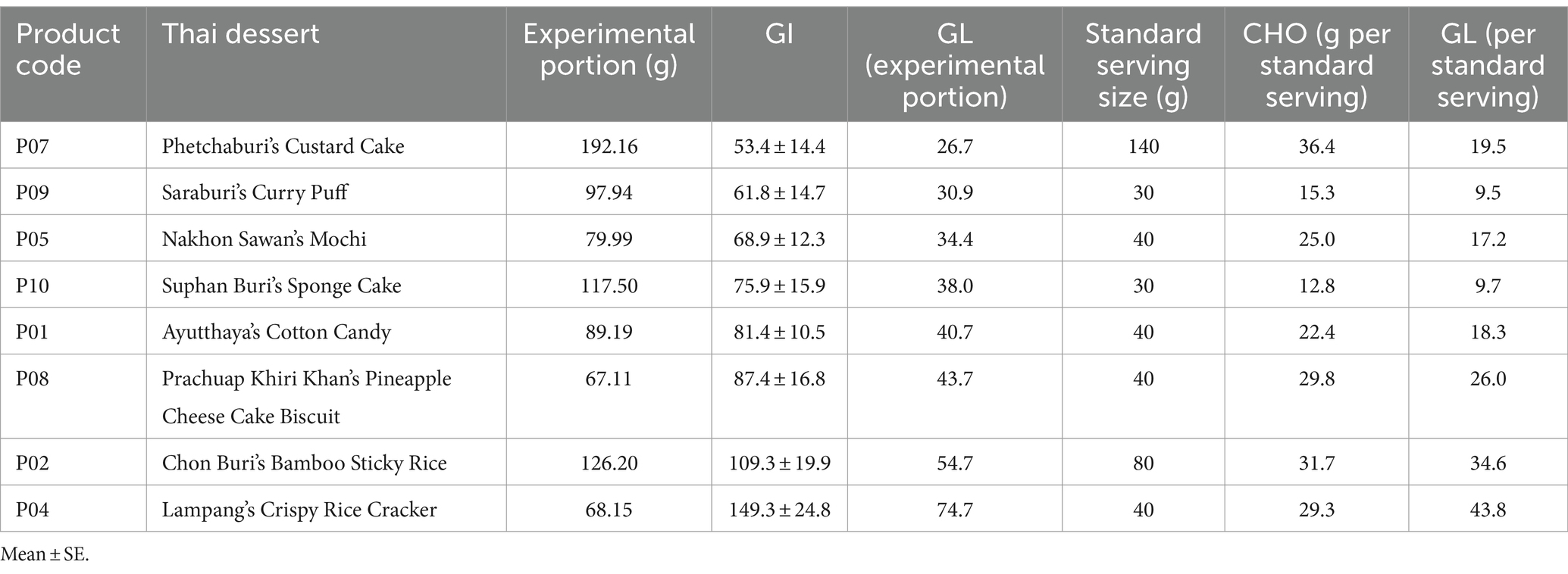
Table 6. Sorted glycemic index and load of Thai desserts based on experimental and standard serving sizes.
Discussion
The determination of reliable GI and GL values for iconic Thai desserts such as Phetchaburi’s Custard Cake, Saraburi’s Curry Puff, and others is vital not only for researchers but also for the general populace. In our study, the groups of subjects tested exhibited no significant statistical differences in baseline characteristics, ensuring the validity of the GI measurements. Our results indicated that most of the Thai desserts evaluated had medium-to high-GI values. Suphan Buri’s Sponge Cake had a GI of 75.9, which is comparable to that of white bread (GI > 70). In fact, five of the desserts studied—Suphan Buri’s Sponge Cake, Ayutthaya’s Cotton Candy, Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit, Chon Buri’s Bamboo Sticky Rice, and Lampang’s Crispy Rice Cracker—were classified as high-GI food (GI > 70). Desserts with medium GI values (GI 55–69) included Saraburi’s Curry Puff and Nakhon Sawan’s Mochi. The only low-GI dessert (GI < 55) identified in our study was Phetchaburi’s Custard Cake.
The observed GI differences are likely due to the diverse ingredients and their ratios, particularly the types and amounts of carbohydrates and sugars used in the desserts (35). Despite its higher sugar content, Phetchaburi’s Custard Cake exhibited a lower GI, suggesting lower glucose absorption possibly due to the presence of fats and proteins that delay digestion. Conversely, Lampang’s Crispy Rice Cracker, despite a lower sugar content, showed a higher GI. This can be attributed to its composition—primarily sticky rice, topped with cane sugar and fried, which may alter the starch structure, making the glucose more rapidly absorbable. These findings underline the importance of considering the whole food matrix, including types and amounts of carbohydrates, cooking methods, and additional ingredients, in understanding the GI values of foods (36).
Further analysis of the GL values for standard servings reveals a crucial aspect of dietary impact. The standard servings of Thai desserts, significantly smaller than the experimental portions, still present high GL values, underscoring the importance of portion control in dietary planning. Given the elevated GL values observed even in smaller, more realistic servings, this information is essential for consumers, particularly those managing glycemic responses. Moderation in the consumption of these desserts, guided by an understanding of both GI and GL values, is advisable to mitigate potential health risks associated with elevated blood glucose levels.
From a public health perspective, the high-GI and GL values observed in several Thai desserts highlight a significant concern. Regular consumption of high-GI foods can lead to rapid spikes in blood glucose levels, increasing the risk of developing type 2 diabetes, obesity, and cardiovascular diseases. Therefore, implementing strategies that inform and educate consumers about the glycemic impacts of the foods they consume is imperative.
Introducing GI and GL information on food labels can empower consumers to make informed dietary choices. By understanding the glycemic effects of desserts, individuals can moderate their intake of high-GI foods and opt for alternatives with lower glycemic responses. Educational campaigns are essential to raise awareness about the importance of GI and GL in managing blood glucose levels and overall health. Such initiatives can guide consumers in interpreting GI and GL values and incorporating this knowledge into their dietary habits.
Policymakers could consider regulations that mandate the disclosure of GI and GL information on packaged foods, especially for products with high carbohydrate content. Setting guidelines for maximum allowable sugar content in desserts could contribute to reducing the glycemic load of population. Encouraging food manufacturers to reformulate products to achieve lower GI values by modifying ingredients or preparation methods can also be beneficial.
Collaborating with food producers and culinary experts to modify traditional dessert recipes by reducing sugar content or incorporating ingredients with a lower glycemic impact can help decrease the GI and GL of these foods without compromising cultural heritage. For example, incorporating whole grains or fiber-rich ingredients may lower the glycemic response.
Regarding food safety, microbial contamination was found in 12 of the 30 dessert brands, with bacteria, yeast, or mold detected in products across various brands. Alarmingly, all brands of certain desserts such as grass jelly and caramel were found to be contaminated, indicating a systemic issue that transcends brand variations. Additionally, two brands, including caramel and sponge cake, were found to have chemical contamination due to excessive levels of preservatives, exceeding the threshold of 1,000 mg/kg. The prevalence of contamination highlights the critical need for comprehensive safety practices. As demonstrated in prior studies, sources of contamination can include production processes, packaging, and environmental factors (37). Compliance with established microbiological quality guidelines such as the FAO/WHO Codex (CAC/GL21-1997) is essential to safeguard consumer health (38).
A GI database for particular Thai desserts will be instrumental in guiding dietary choices, particularly for individuals with diabetes or those managing their glycemic response. Desserts high in carbohydrates, such as Ayutthaya’s Cotton Candy and Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit, significantly influence blood glucose levels, which can strain pancreatic function due to the rapid insulin production needed to process the influx of sugar. Understanding the GL in the context of portion sizes is crucial; our findings suggest that consuming these desserts in moderation is advisable to prevent adverse health outcomes.
Our findings underscore the need for a multifaceted approach to address the public health challenges posed by high-GI desserts. Mandating the inclusion of GI and GL information on packaging can help consumers make healthier choices by providing clear nutritional information. Public health campaigns should educate the population about the impacts of high-GI foods and how to manage glycemic responses through diet, enhancing consumer awareness and encouraging healthier eating habits. Governments can implement regulations to limit sugar content in desserts and promote the availability of lower GI options, thereby supporting public health initiatives. Additionally, collaborating with food manufacturers to reformulate products can reduce the glycemic impact without sacrificing cultural significance, fostering industry cooperation for healthier food options.
By combining these strategies, it is possible to reduce the risks associated with excessive consumption of high-glycemic foods and promote healthier dietary patterns among the Thai population. Integrating GI and GL information into dietary guidelines and nutrition education programs will empower individuals to make informed choices, ultimately contributing to better health outcomes.
A comparison of glycemic responses (GI and GL) between male and female participants was not conducted in this study. Each dessert group consisted of 12 participants with unequal numbers of men and women, with male participants ranging from 4 to 6 per group. The small and uneven sample sizes limited the statistical power to detect potential sex differences in glycemic responses. Consequently, our results reflect the combined responses of all participants regardless of sex. Future studies with larger and more balanced samples are recommended to explore whether sex differences influence the glycemic impact of these desserts.
Conclusion
The Thai desserts analyzed in this study, including Phetchaburi’s Custard Cake, Saraburi’s Curry Puff, Nakhon Sawan’s Mochi, Suphan Buri’s Sponge Cake, Ayutthaya’s Cotton Candy, Prachuap Khiri Khan’s Pineapple Cheese Cake Biscuit, Chon Buri’s Bamboo Sticky Rice, and Lampang’s Crispy Rice Cracker, were found to have a range of GI values from low to high, and uniformly high GL values. Given these findings, it is advisable for consumers to be mindful of the portions they consume, particularly in terms of proteins, fats, and carbohydrates, to prevent adverse health effects related to diabetes, obesity, or cardiovascular diseases. For individuals aiming to maintain health by managing blood glucose levels, selecting desserts with lower GI may be beneficial. The data on GI and GL values from this study can serve as a valuable resource for consumers, researchers, and dietitians making informed choices about Thai desserts. Furthermore, this information could influence positive changes in dessert consumption habits, enhancing public health and product quality. Additionally, these insights may guide the refinement and development of local Thai desserts, bolstering their role in promoting Thailand’s culinary tourism.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee for Human Research, Faculty of Medicine, Chulalongkorn University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
NN: Conceptualization, Data curation, Formal analysis, Investigation, Visualization, Writing – original draft, Writing – review & editing. SS: Data curation, Visualization, Writing – review & editing. TO: Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. AB: Conceptualization, Data curation, Supervision, Validation, Writing – review & editing. JH: Validation, Writing – review & editing. KP: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The 90th Anniversary of Chulalongkorn University Fund (Ratchadaphiseksomphot Endowment Fund GCUGR1125641036D); Ratchadapiseksompotch Fund, Graduate Affairs, Faculty of Medicine Chulalongkorn University (GA64/02); Chulalongkorn University Fundamental Fund 2565 (CUFRB65_food(1)_020_30_01); as well as Thailand Science Research and Innovation Fund Chulalongkorn University (FOODF67300006). TO, SS, and KP were funded by the Second Century Fund (C2F), Chulalongkorn University. The study was supported by Maha Chakri Sirindhorn Clinical Research Center under the Royal Patronage, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand, and HIV Netherlands Australia Thailand Research Collaboration (HIV-NAT) Laboratory is affiliated with The Thai Red Cross AIDS Research Centre in Bangkok, Thailand, to provide locations, equipment, and facilities throughout the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1452602/full#supplementary-material
References
1. Jenkins, DJ, Wolever, TM, Taylor, RH, Barker, H, Fielden, H, Baldwin, JM, et al. Glycemic index of foods: a physiological basis for carbohydrate exchange. Am J Clin Nutr. (1981) 34:362–6. doi: 10.1093/ajcn/34.3.362
2. Salmerón, J, Manson, JE, Stampfer, MJ, Colditz, GA, Wing, AL, and Willett, WC. Dietary fiber, glycemic load, and risk of non-insulin-dependent diabetes mellitus in women. JAMA. (1997) 277:472–7. doi: 10.1001/jama.1997.03540300040031
3. Schulze, MB, Liu, S, Rimm, EB, Manson, JE, Willett, WC, and Hu, FB. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women. Am J Clin Nutr. (2004) 80:348–56. doi: 10.1093/ajcn/80.2.348
4. Brand-Miller, J, and Buyken, AE. The relationship between glycemic index and health. Nutrients. (2020) 12:536. doi: 10.3390/nu12020536
5. Jenkins, DJ, Kendall, CW, Augustin, LS, Franceschi, S, Hamidi, M, Marchie, A, et al. Glycemic index: overview of implications in health and disease. Am J Clin Nutr. (2002) 76:266s–73s. doi: 10.1093/ajcn/76/1.266S
6. Azizi, F, Ghanbarian, A, Momenan, AA, Hadaegh, F, Mirmiran, P, Hedayati, M, et al. Prevention of non-communicable disease in a population in nutrition transition: Tehran lipid and glucose study phase II. Trials. (2009) 10:5. doi: 10.1186/1745-6215-10-5
7. McKeown, NM, Meigs, JB, Liu, S, Saltzman, E, Wilson, PW, and Jacques, PF. Carbohydrate nutrition, insulin resistance, and the prevalence of the metabolic syndrome in the Framingham offspring cohort. Diabetes Care. (2004) 27:538–46. doi: 10.2337/diacare.27.2.538
8. Liu, S, Willett, WC, Stampfer, MJ, Hu, FB, Franz, M, Sampson, L, et al. A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr. (2000) 71:1455–61. doi: 10.1093/ajcn/71.6.1455
9. Vega-López, S, Venn, BJ, and Slavin, JL. Relevance of the glycemic index and glycemic load for body weight, diabetes, and cardiovascular disease. Nutrients. (2018) 10:1361. doi: 10.3390/nu10101361
10. Jenkins, DJA, Dehghan, M, Mente, A, Bangdiwala, SI, Rangarajan, S, Srichaikul, K, et al. Glycemic index, glycemic load, and cardiovascular disease and mortality. N Engl J Med. (2021) 384:1312–22. doi: 10.1056/NEJMoa2007123
11. Hosseinpour-Niazi, S, Sohrab, G, Asghari, G, Mirmiran, P, Moslehi, N, and Azizi, F. Dietary glycemic index, glycemic load, and cardiovascular disease risk factors: Tehran lipid and glucose study. Arch Iran Med. (2013) 16:401–7.
12. Henry, CJ, Lightowler, HJ, Strik, CM, Renton, H, and Hails, S. Glycaemic index and glycaemic load values of commercially available products in the UK. Br J Nutr. (2005) 94:922–30. doi: 10.1079/BJN20051594
13. Al Dhaheri, AS, Henry, CJK, Mohamad, MN, Ohuma, EO, Ismail, LC, Al Meqbaali, FT, et al. Glycaemic index and glycaemic load values of commonly consumed foods in the United Arab Emirates. Br J Nutr. (2017) 117:1110–7. doi: 10.1017/S0007114517001027
14. Candal, C, and Erbas, M. The effects of different processes on enzyme resistant starch content and glycemic index value of wheat flour and using this flour in biscuit production. J Food Sci Technol. (2019) 56:4110–20. doi: 10.1007/s13197-019-03880-w
15. Chen, YJ, Sun, FH, Wong, SH, and Huang, YJ. Glycemic index and glycemic load of selected Chinese traditional foods. World J Gastroenterol. (2010) 16:1512–7. doi: 10.3748/wjg.v16.i12.1512
16. Lok, KY, Chan, R, Chan, D, Li, L, Leung, G, Woo, J, et al. Glycaemic index and glycaemic load values of a selection of popular foods consumed in Hong Kong. Br J Nutr. (2010) 103:556–60. doi: 10.1017/S0007114509992042
17. Wongpiyachon, S, Songchitsomboon, S, Wasusun, A, Sukviwat, W, Maneenin, P, and Cheaupan, K. Glycemic index of 8 Thai Rice varieties Rice Department, Rice Research and Development Division Suphanburi Rice Research Center (2015). 8:54–69.
18. Sripathumrak, P. Relationship between sugar content and glycemic index of Thai fruits. Bangkok: Chulalongkorn University (2004).
19. Visuthranukul, C, Sampatanukul, P, Aroonparkmongkol, S, Sirimongkol, P, and Chomtho, S. Glycemic index and glycemic load of common fruit juices in Thailand. J Health Popul Nutr. (2022) 41:5. doi: 10.1186/s41043-022-00284-z
20. Kamchansuppasin, A, Sirichakwal, P, Bunprakong, L, Yamborisut, U, Kongkachuichai, R, Kriengsinyos, W, et al. Glycaemic index and glycaemic load of commonly consumed Thai fruits. Int Food Res J. (2021) 28:788–94. doi: 10.47836/ifrj.28.4.15
21. Food and Agriculture Organization/World Health Organization . Carbohydrates in human nutrition. Report of a joint FAO/WHO expert consultation. FAO Food Nutr Pap. (1998) 66:1–140.
22. Sommart, K. Consumer perceptions towards marketing mixed innovation of Thai dessert, Phetchaburi province. The 13th RSU National Graduate Research Conference (2018). Vol 13. 835–840.
23. Tangtenglam, S. The influence of social media on the decision making for gastronomic tourism in Thailand. Journal of Research and Development Institute, Chaiyaphum Rajabhat University. (2021) 3:51–62.
24. The official website of Tourism Authority of Thailand . Available at: https://www.tourismthailand.org/ (Accessed November 1, 2021).
25. Jang, C, Hui, S, Lu, W, Cowan, AJ, Morscher, RJ, Lee, G, et al. The small intestine converts dietary fructose into glucose and organic acids. Cell Metab. (2018) 27:351–61.e3. doi: 10.1016/j.cmet.2017.12.016
26. Green, S. Research activities in toxicology and toxicological requirements of the FDA for food and color additives. Biomed Environ Sci. (1988) 1:424–30.
27. Brouns, F, Bjorck, I, Frayn, KN, Gibbs, AL, Lang, V, Slama, G, et al. Glycaemic index methodology. Nutr Res Rev. (2005) 18:145–71. doi: 10.1079/NRR2005100
28. The International Organization for Standardization . Food products -- Determination of the glycemic index (GI) and recommendation for food classification. ISO 26642. ISO 26642 (2010).
29. Bureau of Quality and Safety of Food, Department of Medical Sciences, Ministry of Public Health . Microbiological quality criteria of cooked food (desserts and pastries). (2017). Available at: http://bqsf.dmsc.moph.go.th/bqsfWeb/index.php/bio/ (Accessed November 1, 2021).
30. Allison, DB, Paultre, F, Maggio, C, Mezzitis, N, and Pi-Sunyer, FX. The use of areas under curves in diabetes research. Diabetes Care. (1995) 18:245–50. doi: 10.2337/diacare.18.2.245
31. Sun, L, Lee, DE, Tan, WJ, Ranawana, DV, Quek, YC, Goh, HJ, et al. Glycaemic index and glycaemic load of selected popular foods consumed in Southeast Asia. Br J Nutr. (2015) 113:843–8. doi: 10.1017/S0007114514004425
33. Brand-Miller, J, Wolever, MST, Foster-Powell, K, and Colagiuri, S. The new glucose revolution: The authoritative guide to the glycemic index—the dietary solution for lifelong health. New York: Marlowe & Company (2003).
34. Venn, BJ, Wallace, AJ, Monro, JA, Perry, T, Brown, R, Frampton, C, et al. The glycemic load estimated from the glycemic index does not differ greatly from that measured using a standard curve in healthy volunteers. J Nutr. (2006) 136:1377–81. doi: 10.1093/jn/136.5.1377
36. Phromphichai, R. Khao Tan. In: Phromphichai R, ed. The Encyclopedia of Northern Thai Culture, vol 2. Bangkok: Princess Maha Chakri Sirindhorn Anthropology Centre (Public Organization) (1999). 812.
37. Trongjit, K, and Pattarasanphet, J. Fungal contamibation in Kalamae dessert and its preservation. Koch Cha Sarn J Sci. (2016) 38:14–26.
Keywords: glycemic index, glycemic load, Thai desserts, sugar consumption, nutritional analysis, carbohydrate content, food safety
Citation: Namjud N, Senaprom S, Ondee T, Bumrungpert A, Heath J and Pongpirul K (2024) Glycemic index and glycemic load of brief sugary sweets: randomized controlled trials of eight Thai desserts. Front. Nutr. 11:1452602. doi: 10.3389/fnut.2024.1452602
Edited by:
Rani Polak, Spaulding Rehabilitation Hospital, United StatesReviewed by:
Lubia Velázquez López, Instituto Mexicano del Seguro Social, MexicoDavid J. A. Jenkins, Unity Health Toronto, Canada
Copyright © 2024 Namjud, Senaprom, Ondee, Bumrungpert, Heath and Pongpirul. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Krit Pongpirul, ZG9jdG9ya3JpdEBnbWFpbC5jb20=
 Nuttaphat Namjud1
Nuttaphat Namjud1 Thunnicha Ondee
Thunnicha Ondee Julia Heath
Julia Heath Krit Pongpirul
Krit Pongpirul