
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 26 July 2024
Sec. Nutrition Methodology
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1382078
This article is part of the Research TopicSustainable Diets with Sociocultural and Economic ConsiderationsView all 18 articles
 Anna Worthington1*
Anna Worthington1* Eva Liu1
Eva Liu1 Meika Foster2,3
Meika Foster2,3 Summer Rangimaarie Wright2
Summer Rangimaarie Wright2 Fiona E. Lithander3,4
Fiona E. Lithander3,4 Clare Wall1,4
Clare Wall1,4 Rajshri Roy1
Rajshri Roy1 Amber Parry-Strong3,5
Amber Parry-Strong3,5 Jeremy Krebs5,6
Jeremy Krebs5,6 Andrea Braakhuis1 on behalf of He Rourou Whai Painga Consortium
Andrea Braakhuis1 on behalf of He Rourou Whai Painga ConsortiumBackground: Following a Mediterranean diet (MedDiet) is associated with a lower risk of cardiovascular disease. He Rourou Whai Painga is a dietary intervention trial with behaviour change support that seeks to determine whether a MedDiet pattern can provide equivalent benefits in Aotearoa New Zealand (NZ), a country where cardiovascular disease is a leading cause of death. To do this, the MedDiet needs to be adapted in an acceptable way for NZ, with consideration of the Māori (indigenous) population.
Methods: The MedDiet was defined using existing MedDiet scoring tools and adapted to the NZ context using local guidelines. The resulting NZ MedDiet pattern was used to develop a kai/food basket, including products from industry partners, for participants in He Rourou Whai Painga. Criteria set for the kai/food basket included providing up to 75% of energy requirements and falling within the Australia/NZ Acceptable Macronutrient Distribution Range to reduce risk of chronic disease. Māori researchers on the team provided support to ensure Mātauranga Māori (Māori knowledge and values) was upheld through this process.
Results: The NZ MedDiet pattern criteria was similar to the identified MedDiet scoring tools, with differences in recommendations for dairy, red meat, alcohol and olive oil. The resulting kai/food baskets were estimated to provide on average 73.5% of energy requirements for households, with 36% from fat, 8.6% from saturated fat, 17% protein, and 42% carbohydrate. Forty-two industry partners, including 3 Māori businesses, agreed to provide 22 types of food products towards the total.
Conclusion: Small, feasible changes to the MedDiet can be made to align with the NZ guidelines and food environment. However, this eating pattern still differs from what the population, particularly Māori, are currently consuming. Continued partnership with Māori and additional behavioural support is important to facilitate adherence to this dietary pattern within He Rourou Whai Painga.
Trial registration: https://www.anzctr.org.au/Default.aspx, identifier ACTRN12622000906752 and https://www.isrctn.com/, identifier ISRCTN89011056.
Over the past two decades, the prevalence of many metabolic diseases has increased, presenting a significant global health burden (1, 2). In Aotearoa New Zealand (NZ), cardiovascular disease (CVD) is the leading cause of death, accounting for a third of all deaths annually (3), and approximately 5–6% of the population have type 2 diabetes mellitus (T2DM) (4). Over the past seven decades, mortality rates have been consistently higher for Māori (indigenous people of NZ), than non-Māori. Māori are 2.5 times more likely to have T2DM than non-Māori, and the prevalence of T2DM is the highest for Pacific people in NZ (5). Differences in prevalence and mortality signify the disproportionate and increased burden of cardiometabolic disease on Māori and Pacific peoples (4, 6). Metabolic syndrome (MetS) is a combination of multiple risk factors that increases the risk of CVD and T2DM (1). It is characterised by interconnected factors including hypertension, dyslipidaemia, disordered glucose metabolism, and obesity (2).
Unhealthy dietary habits and physical inactivity are important modifiable contributors to cardiometabolic disease risk worldwide (7, 8). The Mediterranean diet (MedDiet) is a well-studied dietary pattern characterised by an abundance of plant-based foods, olive oil, seafood, wholegrains and poultry, and low to moderate intake of red and processed meats, dairy products, and processed food (9, 10). Meta-analyses of the effects of the MedDiet on the MetS have demonstrated an overall positive impact of the MedDiet in decreasing MetS and its component factors in adults, including decreased blood glucose levels, blood pressure, and improved lipid profile (11), as well as decreasing the risk of overall mortality, CVD, and T2DM (12).
Considering the promise of the MedDiet in addressing MetS, it is of interest to investigate its potential in the New Zealand population. Indeed, the Eating and Activity Guidelines for NZ Adults (13) include the same food groups as the MedDiet, with only slight variations in the recommended proportions of different components (14). Additionally, aspects of the MedDiet align with traditional kai/food types and practices for Māori, such as a diet high in seafood (15), and valuing local, seasonal food, how it is prepared and the social context in which it is consumed (16). However, the 2008 NZ Adult Nutrition Survey reported that the average NZ diet differs significantly from the Eating and Activity Guidelines, and, in turn, a MedDiet. In particular, there was a higher intake of dairy and meat. This likely reflects food choices influenced by NZ’s history as an agricultural nation (17, 18). More recent cross-sectional studies of 908 (14) and 350 (19) NZ adults have demonstrated poor alignment with the MedDiet, indicating a significant shift in food choices will be required if the MedDiet is to be adopted in the NZ population (14, 19). Indeed, challenges exist with the transferability and adoption of the MedDiet to non-Mediterranean populations (20, 21); these include accessing and purchasing MedDiet foods such as olive oil (22), differences in habitual intake (14) and therefore adherence to a different dietary pattern (21), culture, religion, traditional cooking practices, and economic burden (23). Despite this, the MedDiet has been adapted and successfully implemented in different populations, such as in Northern Ireland and Australia, with concomitant improvements in MetS components and markers of cardiovascular risk (20, 24), demonstrating its potential for translation to other non-Mediterranean populations, such as New Zealand (25).
As there are substantial potential health benefits of the MedDiet, adaptation of the MedDiet to the NZ context should be explored, with consideration of the needs of Māori given the health disparities they experience. The He Rourou Whai Painga randomised controlled trial (RCT) aims to evaluate if a MedDiet pattern incorporating high quality NZ foods (“NZMedDiet”) improves a composite assessment of cardiometabolic health, the metabolic syndrome severity score (MetSSS) (26) for individuals identified as being at risk of cardiometabolic disease, in a study sample enriched for Māori. The planned intervention for this RCT is delivery in a household/whānau setting, underpinned by behavioural science. To support adherence to the NZMedDiet, participants will be provided kai/food baskets with high quality NZ foods that align with the NZMedDiet. Transparent documentation of the adaption or interpretation of a dietary pattern within nutrition trials is essential for providing context to observed results. However, the process of designing or adapting dietary patterns, such as the MedDiet, for free-living individuals who participate within trials is seldom reported (25). Consequently, the objective of the study reported here is to document the development of the NZMedDiet and composition of the kai/food baskets used in He Rourou Whai Painga; doing so provides a tangible process for adapting the MedDiet to other non-Mediterranean populations.
The present study aims to:
1. Adapt and define a MedDiet in the NZ context (“NZMedDiet”) for He Rourou Whai Painga.
2. Develop kai/food baskets that provide whānau/households with up to 75% of their estimated energy requirements with foods that align with the NZMedDiet in He Rourou Whai Painga.
He Rourou Whai Painga is a multi-centre trial consisting of two RCT phases and a longitudinal cohort study. The recruitment target is 200 participants with a MetSSS greater than 0.35 (26). Additionally, aligned both to the NZ Government’s Vision Mātauranga policy to support research of relevance to Māori and a collective worldview, a whānau-led approach will be taken where up to five members of a household in addition to the index participant will be invited to participate in the intervention. Full details on the trial have been published elsewhere (27). In brief, the first RCT compares the NZMedDiet to usual dietary intake with a primary outcome of the MetSSS 12 weeks after randomisation. For the 12-week intervention, participants will receive kai/food baskets containing ingredients and recipes for main meals and snacks, providing up to 75% of the energy requirements of the household/whānau, as per the protocol (27). Participants will also receive access to web-based nutrition education and opt-in online social support to help them adhere to the NZMedDiet. The second RCT compares the ongoing opt-in online social support, to no online social support with an outcome assessment 12-weeks after the second randomisation. From beginning the dietary intervention, the cohort will be followed for a total of 52 weeks.
A key foundation of this trial, therefore, was the development of the NZMedDiet and composition of the kai/food baskets to be received by all 200 participants and their participating whanau members. The process of developing this dietary pattern and kai/food baskets for He Rourou Whai Painga is outlined in Figure 1. This was overseen by a subgroup (the “NZMedDiet subgroup”) of study researchers consisting of eight NZ registered dietitians, two members of the consumer insights team, and another NZ registered dietitian from a commercial meal kit company. Importantly, Māori researchers were partnered with from the conception of this trial to support Pākehā/non-indigenous researchers with the design and implementation of this trial; this included advice while designing the dietary pattern to ensure its acceptability by Māori.
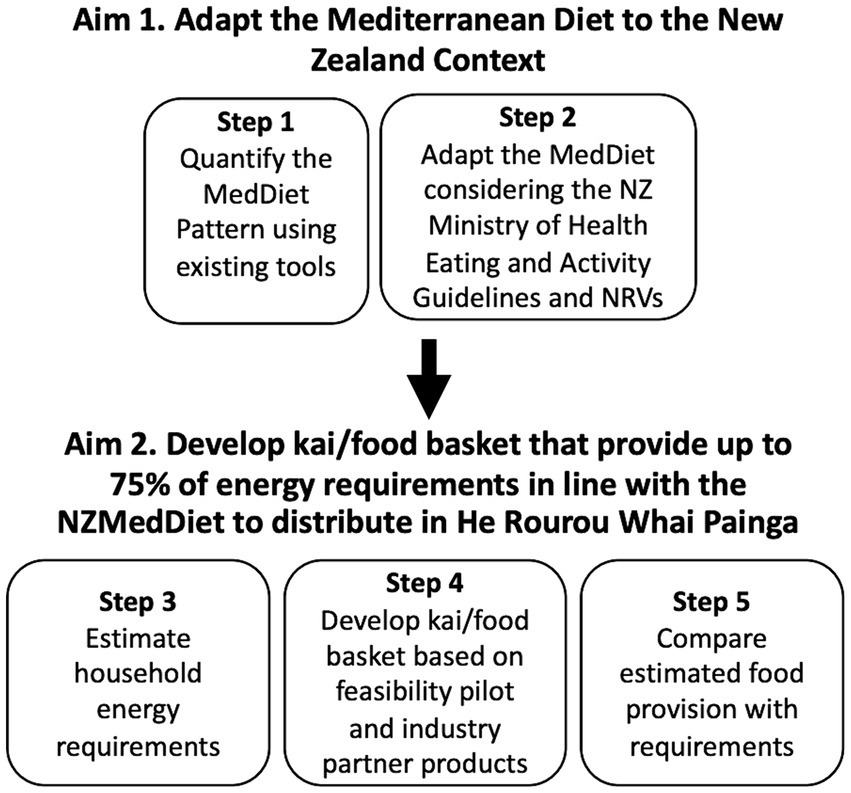
Figure 1. Process of developing kai/food baskets for He Rourou Whai Painga that align with a Mediterranean Diet (MedDiet) in the New Zealand (NZ) context. NRVs, Nutrient Reference Values for Australia and NZ (including the Acceptable Macronutrient Distribution Range to reduce risk of chronic disease); NZMedDiet, New Zealand Mediterranean Diet pattern.
The recommended number and size of food group servings within a MedDiet varies throughout the literature (9, 28, 29). For the study reported here, the literature-based adherence score (LAS) to the Mediterranean diet (29) and the widely used Mediterranean Diet Adherence Screener (MEDAS) scoring tool (30) were used to determine the MedDiet composition, including the serve number and sizes for each food group. The LAS was developed by Sofi and colleagues using data from a meta-analysis of cohort studies investigating the association between adherence to the MedDiet and health outcomes (29). It comprises nine food categories, with a maximum score of 18 points indicating the highest adherence relative to the average of the general population (28). The MEDAS, developed by the Prevención con Dieta Mediterránea investigators (30), is a 14-item yes/no questionnaire and includes additional questions related to criteria characteristic of a MedDiet that the LAS does not contain. Adherence to the MedDiet measured using both tools has been associated with positive health outcomes (31, 32).
Two NZ registered dietitians from the NZMedDiet subgroup compared the recommended number of serves and portion sizes from the LAS and MEDAS tools to the NZ Ministry of Health Eating and Activity Guidelines (“the NZ guidelines”) (13), for the following foods and food groups: olive oil, vegetables, fruits, breads and cereals, legumes, nuts, fish/seafood, eggs, poultry, dairy foods, alcohol, and sweets. The NZ Heart Foundation guidelines were used to guide the recommendations for red meat (33). Portion sizes from the identified tools were adapted to match the NZ guidelines. Where a discrepancy existed between the number of serves recommended in the MedDiet versus the NZ guidelines, a consensus and justification were reached by the dietitians for adapting the NZMedDiet criteria to be feasible in the NZ setting, while still aligning with the principles underpinning the MedDiet; this was relevant for dairy foods, olive oil and alcohol. The output of this exercise was an objectively defined NZMedDiet. Additionally, for the purpose of He Rourou Whai Painga, it was determined that the NZMedDiet should closely align with the Acceptable Macronutrient Distribution Range (AMDR) for the reduction of chronic disease risk outlined in the Nutrient Reference Values for Australia and NZ (34).
In the RCT, food is provided to supply up to 75% of a whānau/household’s energy requirement through provision of kai/food baskets. Energy requirements for adults were based on the Australia NZ Food Standards Code 1.2.8, as derived from average intakes of adult males and females surveyed in Australia and NZ (35, 36), while the Nutrient Reference Values for Australia and NZ were used to estimate the energy needs of children aged 11–17 years and 5–10 years (34, 37). To ensure food provision to participating whānau/households of up to six people is consistent and workable, three versions of the kai/food baskets were designed for whānau/household sizes of two, four, and six members; energy estimates were calculated based on pragmatically assigned whānau/household makeups of two adults, three adults and one child (5-10 yr), and four adults and two children (5-10 yr), respectively. Of note, older children aged 11–17 years had the same energy requirements as adults, and consequently any ‘adult’ in the household makeup could also be a child aged 11–17 years.
The kai/food baskets for the trial are based on the following criteria: they must provide as close as possible to 75% of total energy; align with the NZMedDiet criteria (Table 1); be consistent with the AMDR for the reduction of chronic disease risk; include products from NZ food and beverage companies (industry partners), including Māori companies; and be feasible to assemble and deliver to whānau/households in three NZ regions both in the North and South Island of NZ. A feasibility trial of He Rourou Whai Painga was conducted at the Centre for Endocrine, Diabetes and Obesity Research (CEDOR) in Wellington and at Tū Kotahi Māori Asthma and Research Trust at Kōkiri Marae (a community-based traditional Māori meeting place) in Lower Hutt, Wellington. This involved providing participants with up to 75% of their energy needs from foods aligning with a MedDiet. The feasibility trial confirmed that the use of commercial companies for the distribution of kai/food baskets was feasible and acceptable to participants (38). Consequently, two commercial companies were selected for the provision of kai/food baskets in the main trial, one of which is a meal kit home delivery service, and the other is an online grocery provider.
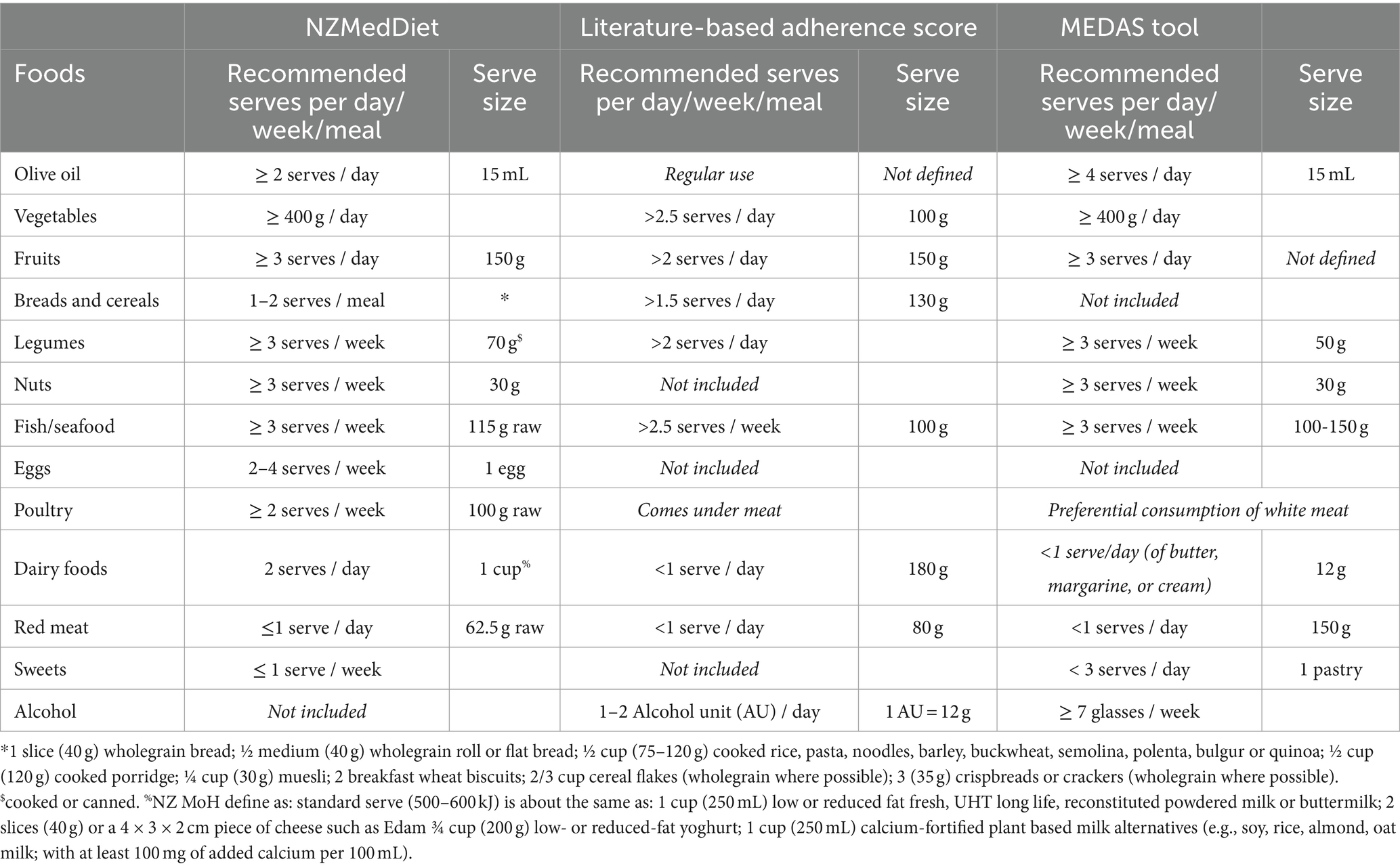
Table 1. Foods and their recommended serves per participant for the New Zealand Mediterranean Diet Pattern (NZMedDiet) compared to the literature-based adherence score, and Mediterranean Diet Adherence Screener (MEDAS) scoring tool.
The meal kit home delivery service is responsible for providing a weekly dinner box and fruit box. Dinner boxes are delivered to participants’ homes with recipe cards and all components of those meals appropriate to the household size; to serve either two, four, or six people. Researchers are responsible for selecting dinner meals in advance for participants from those offered each week by the meal kit home delivery service; the NZMedDiet subgroup established selection criteria to ensure meals chosen aligned with the NZMedDiet. The online grocery provider is responsible for the distribution of a weekly grocery box, which contains foods for breakfasts, lunches, and snacks. Additionally, a one-off starter box of food products provided by industry partners is distributed by the grocery provider in the first week of participants beginning in the intervention.
Participant feedback from the feasibility trial was used to make decisions regarding the kai/food baskets for the main trial; of note, the feasibility trial provided a strong voice for populations facing higher disparities of CVD, with 55 and 13.8% of participants identifying as Māori and Pacific, respectively (38). Feedback highlighted a need for variety in breakfasts and lunch options, hence three variations of the grocery box were developed for the whānau/household sizes of two, four and six members, resulting in nine versions of the grocery box. Additionally, food items that were not liked were swapped for items favoured by the feasibility trial participants, or the quantity provided was reduced. Feasibility trial participants identified food items that differed from what they traditionally use, and the need for instruction on how to prepare them; hence ingredient lists, recipes and meal plans for the grocery boxes were developed by the NZMedDiet subgroup and made available on a participant-facing website.
Food provided in the kai/food baskets comes from two sources; food provided in-kind to the study by industry partners and food purchased by the research team. A list of potential industry partners, including Māori food businesses, was generated using information provided by the Directorate of the High Value Nutrition National Science Challenge and commercial knowledge of the research team. Each potential partner was contacted with details of the study and invited to attend online and in-person information sessions, before being invited to complete a business case template for in-kind provision of a product to the study. Offered products were then screened by the NZMedDiet subgroup and wider research team, and those that aligned with the study values and prespecified criteria were accepted and incorporated into the kai/food baskets. Diet-specific criteria that products were required to meet before being accepted into the trial included alignment with a MedDiet pattern, alignment with healthy food guidelines when consumed in the prescribed quantities (for example carbonated beverages were generally excluded even when low in sugar content) and were not dietary supplements.
A nutrition database containing foods available in NZ, FoodWorks (version 10, Xyris Pty Ltd), was used to analyse the nutrition content of the grocery, fruit, and starter boxes. An average estimate of the energy content of dinner meals was provided by the meal kit home delivery service dietitian. The total amount of energy predicted to be provided over the 12 weeks was compared by two NZMedDiet subgroup dietitians (independently, with any differences resolved by consensus) to the estimated energy requirements per whānau/household to ensure it was close to but did not exceed 75%.
An estimate of energy intended to be provided by the kai/food baskets was compared to the amount of food required to meet the NZMedDiet criteria and total energy over 12 weeks. The number of serves of each food group per person provided over the 12 weeks was estimated based on the expected ingredients in the grocery, fruit and starter boxes, and as well as an average of 3 weeks of dinner recipes from the meal kit home delivery service. Of note, the dinner meals will differ every night across the 12 weeks in the actual study. The predicted nutrition content of the food provided was also compared to the AMDR for the reduction of chronic disease risk. Where possible, quantities of food intended to be provided were adjusted to more closely align with the AMDRs while still aligning with the NZMedDiet.
Table 1 depicts the recommended number and size of serves for the NZMedDiet compared to the ideal serve number and size in the LAS and MEDAS tool. Differences are apparent between the recommended number and size of food group serves in the LAS, MEDAS and NZ Guidelines for alcohol, red meat, dairy, and olive oil and were reconciled, as described below (13, 29, 30).
Portion sizes on the original LAS are derived from the calculation of mean value of weighted medians (or means) from the included cohort studies (29). Most of these aligned with the recommended serve sizes and numbers from the NZ guidelines, except for dairy and red meat. The NZ guidelines recommend 2.5–4 serves of dairy per day, depending on age and gender, where a serve is 250 mL of milk, 40 g cheese, or 200 g yoghurt (13). The LAS recommends less than one serve of dairy per day, where a serve is 180 g regardless of the source of dairy. Consensus was reached by the dietitians within the NZMedDiet subgroup to recommend two serves of dairy per day, which is at the conservative end of the NZ guidelines, to acknowledge the low to moderate consumption of dairy encouraged by the MedDiet. Additionally, the daily serve size of red meat was lowered from 80 g (LAS tool) and 150 g (MEDAS tool) to align with the NZ Heart Foundation guidelines of 62.5 g (Table 1), as per the evidence for reducing the occurrence of heart disease (33).
The NZ Guidelines do not provide specific recommendations on olive oil consumption (13). Additionally, quantifiable definitions were not provided for the use of olive oil in the LAS. Only one reference within the LAS included high olive oil intake as a component of the adherence score (39), and consequently these tertiles were used to define regular use (≥2 serves/day), frequent use (1–1.9 serves/day), and occasional use (<1 serve/day), where a serve is 15 mL (1 Tbsp). Although 1 point is awarded in the MEDAS tool for consuming ≥4 tbsp of olive oil per day, the LAS aligns more closely with the NZ context and was thought to be more acceptable and achievable given the primary sources of total and saturated fat, poly- and mono-unsaturated fatty acids in the NZ diet are butter and margarine (17), as well as considering the AMDRs where no more than 35 and 10% of energy from fat and saturated fat, respectively, is recommended.
Contrary to the MedDiet, the NZ Ministry of Health recommends limiting alcohol consumption to no more than two and three standard drinks per day for women and men, respectively, and including two alcohol-free days a week (40). Given the context of the study was to reduce risk of cardiovascular disease, the subgroup decided that explicit guidance about alcohol intake would not be given in He Rourou Whai Painga unless requested. If asked, participants would be referred to the NZ guidelines surrounding alcohol consumption.
Energy requirements of the average adult and children aged 11–17 years were based on the recommended total energy intake of 8,700 kJ per day (34, 37). The mean energy requirement of boys and girls aged 5–10 years was estimated to be 6,900 kJ per day (34). Therefore, over a 12-week period it was estimated that a whānau/household of two, four and six members would be provided 1,096 MJ, 2097 MJ and 3,062 MJ to reach 75% of energy requirements, respectively (Table 2).
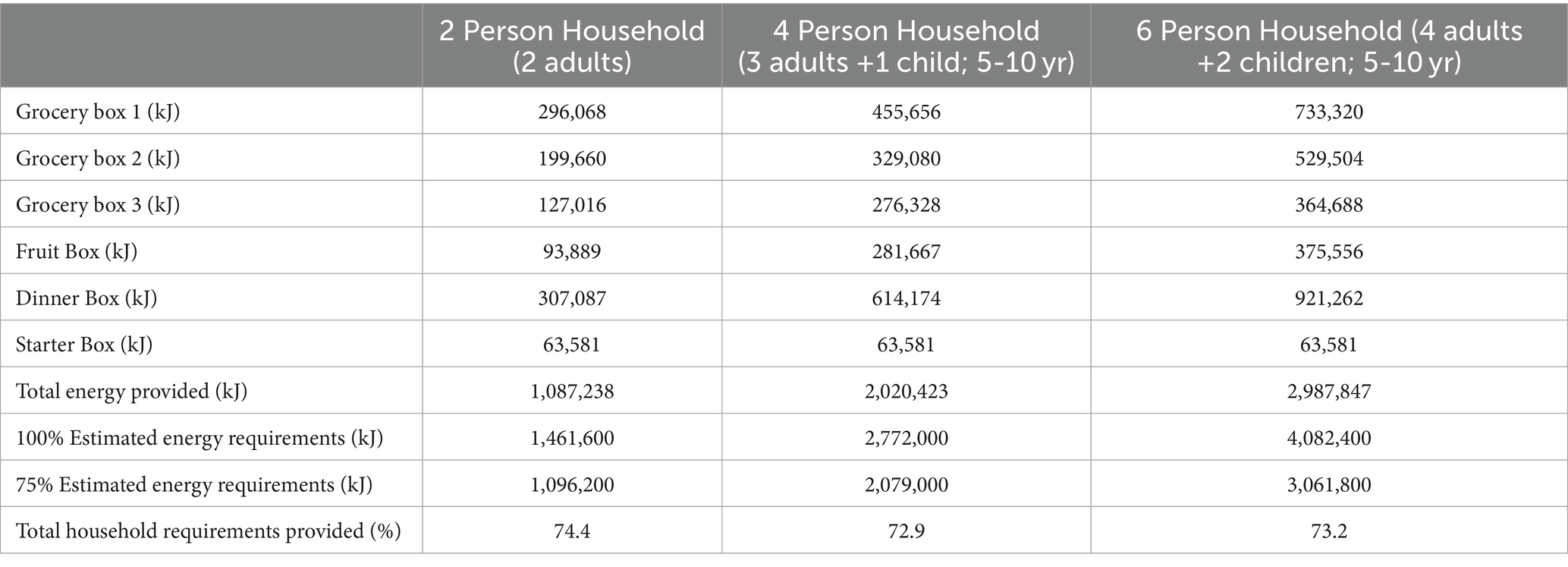
Table 2. Energy provided by kai/food baskets over 12 weeks compared to estimated whānau/household energy needs.
Figure 2 gives an overview of the kai/food basket that was developed. Identical to the feasibility trial, the meal kit home delivery service provides five dinner meals each week per participant in the main study, with each meal on average providing 2,559 kJ (example meals provided in Supplementary file 1). To ensure these dinner meals align with the NZMedDiet, the research team will use the following selection criteria each week: select as many fish-based meals as are available; as many vegetarian or chicken meals as are available; after that, choose a red meat-based meal that contains at least two serves of vegetables and uses wholegrains/legumes. Approximately 22 pieces of fruit are supplied per fruit box, with one, three and four boxes provided for whānau/households of two, four and six people, respectively. The kai/food baskets can be tailored to dietary preferences, such as vegetarian. The grocery box provides ingredients for approximately five breakfasts and five lunches per week; ingredient quantities and sample menus for each box can be found in Supplementary file 1. The quantity of additional snacks is based on providing up to 75% of total energy per whānau/household. The dinner, grocery, fruit and starter boxes are estimated to provide an average of 73.5% of a whānau/household’s total energy requirements for the specific whānau/household (Table 2).
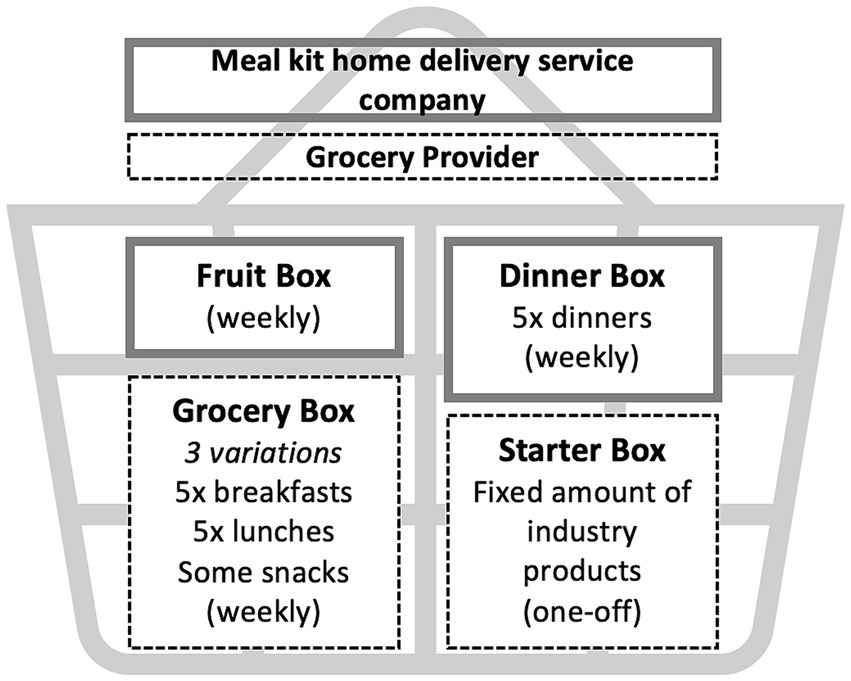
Figure 2. Kai/food baskets that whānau/households will be delivered by two providers in the phase one RCT intervention arm of He Rourou Whai Painga.
In total, 42 industry partners, three of which are Māori food businesses, will provide 22 different products, such as macadamias, kiwifruit, and seafood (Supplementary file 2). Of these partners, 18 will provide olive oil, and 9 will provide lean red meat products.
Compared to the NZMedDiet, the kai/food baskets are estimated to provide 100% or more of requirements for fruit, legumes, nuts, poultry and eggs, between 50 and 75% of vegetables, red meat, and breads and cereals, while less than 50% of olive oil, fish and dairy foods would be provided (Table 3).
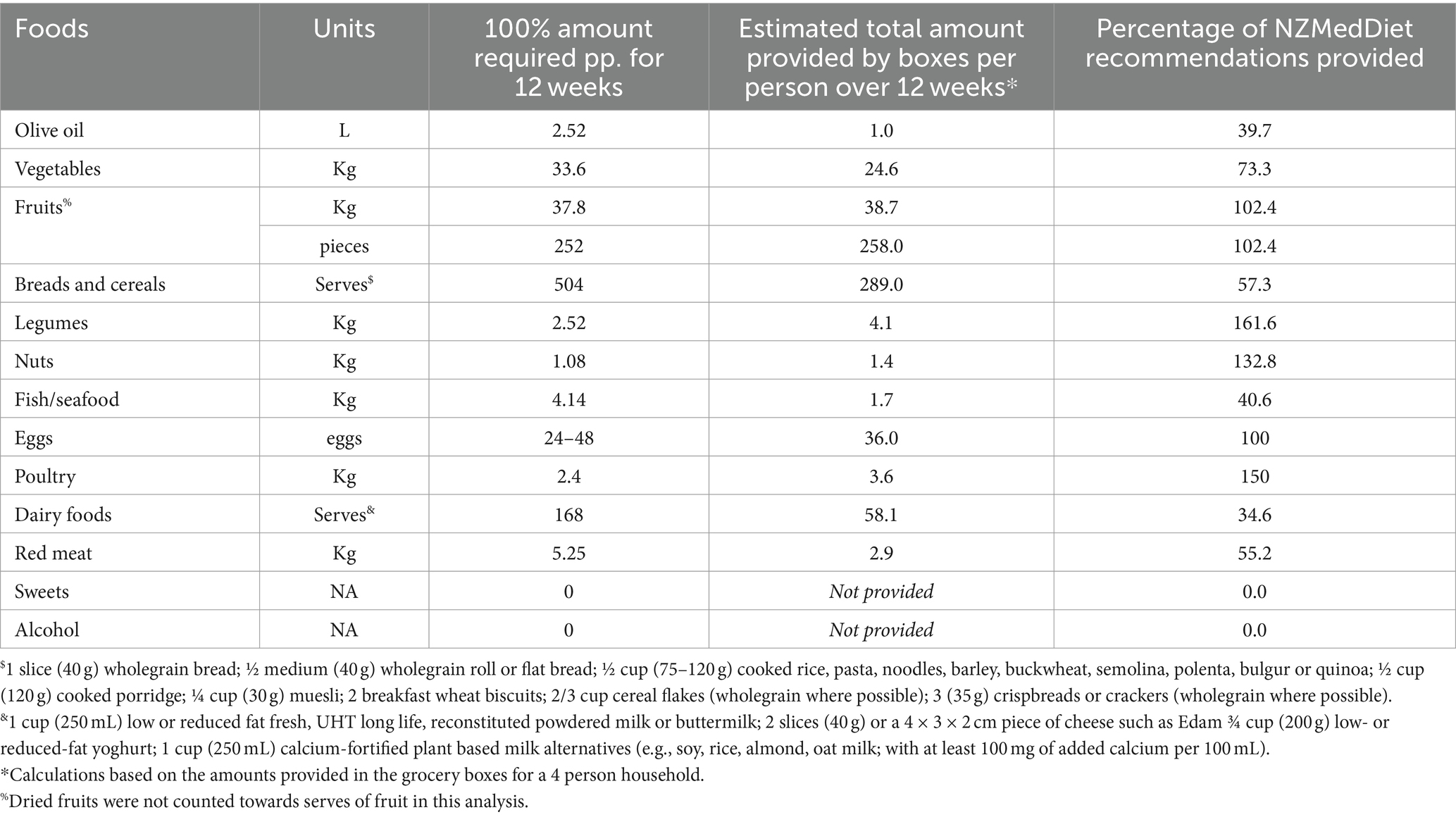
Table 3. Amount of food required to meet the NZMedDiet criteria over 12 weeks compared to an estimate of what will be provided by the He Rourou Whai Painga kai/food baskets.
The kai/food baskets that provide 75% of total energy are predicted to be slightly lower for carbohydrate and higher for fat than the macronutrient distribution to reduce chronic disease risk, while meeting the recommendations for protein and saturated fat (Table 4).
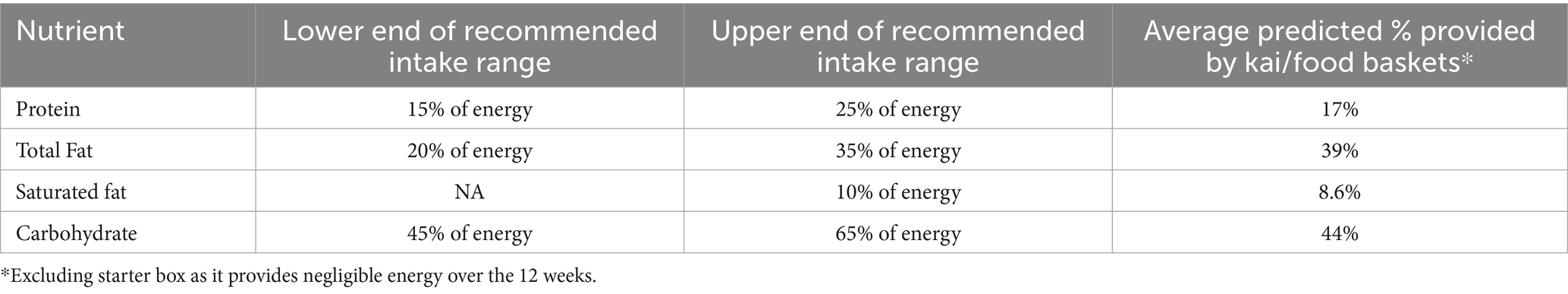
Table 4. Acceptable macronutrient distribution ranges to reduce chronic disease risk and predicted provision by He Rourou Whai Painga kai/food baskets.
This study reports the process by which the investigators of He Rourou Whai Painga created the NZ version of the MedDiet, and produced a method to deliver foods to participants and their whānau/households aligning with this dietary pattern to meet 75% of their energy needs. The NZMedDiet was developed by adapting the MedDiet, as defined by the LAS and MEDAS tools, to the NZ context and guidelines. The NZMedDiet criteria were used to guide the development of kai/food baskets, providing participants and household members in He Rourou Whai Painga with an estimated average of 73.5% of energy for 12 weeks. Kai/food baskets include NZMedDiet ingredients for breakfasts, lunches, dinners, and snacks, including 22 products from 42 industry partners.
The premise of promoting consumption of the MedDiet is that it will confer health benefits, such as reduction in CVD risk factors (11, 12). Consequently, the degree of difference between the NZMedDiet and the traditional MedDiet needs to be considered. Although the NZMedDiet does not exactly match any previously defined MedDiet scoring tool, when compared to the eight MedDiet questionnaires reviewed by Chiriacò et al. (28), all food items in the NZMedDiet fall within the identified ranges of existing recommended intakes. This indicates that the NZMedDiet is within the scope of how the MedDiet can plausibly be defined. However, when compared to the PyrMDS, considered the most accurate and reliable tool to estimate MedDiet adherence (28), the NZMedDiet falls just under the recommendations for vegetables (≥400 g/day NZMedDiet versus ≥480 g/day PyrMDS), legumes (210 g/week versus 300 g/week), and nuts (90 g/week versus 30-60 g/day), while recommending more red meat (≤437.5 g/week versus ≤200 g/week), and fewer sweets (≤1 serve/week versus ≤2/week) (28, 41). Additionally, the lifestyle habits of Mediterranean populations, such as physical activity, pattern of meals, and context in which meals are consumed, may act as confounding factors to the observed health benefits (22). However, a particular strength of He Rourou Whai Painga is its whānau/household collective wellbeing approach in recognition that food is largely consumed in a shared environment and it is common for cardiometabolic risk to cluster within a family (42); therefore, dietary interventions that target the wider family may be more likely to be successful compared to those which focus solely on improving the health of an individual. These differences in the NZMedDiet criteria compared to the traditional MedDiet and additional lifestyle considerations will be important to consider when analysing the effect of the NZMedDiet in He Rourou Whai Painga.
Trying to fit a MedDiet-style pattern to the AMDRs proved challenging with the provided kai/food baskets predicted to exceed the desired AMDR for fat (39%) and fall short of that for carbohydrates (44%). This is not surprising given the usual amount of fat in the MedDiet is 30–45% (9, 43). However, the type of fat may be of more importance in this case; the MedDiet typically has a higher ratio of mono- and poly-unsaturated fatty acids to saturated fatty acids which can improve LDL cholesterol levels, contributing to the reduction in CVD risk (44). The NZMedDiet is likely to have a similar ratio, as demonstrated by saturated fat predicted to provide less than 10% of total energy. The AMDR estimates do not account for the extra 25% of energy that participants are responsible for purchasing. Consequently, dietary assessment during the trial will be important to establish the actual macronutrient intake compared to the AMDR. Methods of measuring dietary intake will include the Otago Short Form Food Frequency Questionnaire and 24-h recalls (27).
To establish whether the NZMedDiet confers health benefits similar to the MedDiet it is key that participants are supported to adhere to it and that adherence is measured, as the level of adherence to a dietary pattern impacts the effect size on health outcomes (45, 46). For example, to achieve the desired NZMedDiet participants would ideally supplement the kai/food baskets with more olive oil, fish, vegetables and some bread and cereals, red meat, and dairy products. Given the current dietary pattern of NZ adults, particularly those of Māori and Pacific ethnicity, differs greatly from the MedDiet (14, 47) behavioural support to encourage purchase and consumption of these foods is important. Implementing a Mediterranean diet pattern in a non-Mediterranean country has its challenges, with previous research stating the following barriers to adopting such a diet; stress and work pressure; difficulties purchasing food items; increase in food costs and country-specific culture and climate being non-conducive (48). It will be important to identify specific barriers and effective support strategies relevant to the NZ context, including accounting for food practices (21, 49). To do this, the Behaviour Change Wheel (50) will be used in He Rourou Whai Painga, along with continued partnership with Māori as implemented in the feasibility trial (38). This behaviour change framework has been previously used to successfully develop a peer-support intervention to encourage dietary behaviour change towards a MedDiet in non-Mediterranean adults at high CVD risk (20, 51).
Strengths of this study include that we have clearly defined the recommended number of serves and portion sizes for each food group, enabling adherence to the dietary behaviours required within the NZMedDiet to be assessed, a factor frequently overlooked in dietary intervention trials (52, 53). Additionally, the involvement of Tū Kotahi Māori Asthma and Research Trust enabled the target audience to have a voice in what the kai/food baskets contained, demonstrating how these types of projects can be run in partnership with Māori in the community. Limitations of the design of the kai/food baskets include that they are designed based on fixed whānau/household makeups; three-person and five-person households will receive two-person and four-person kai/food baskets, meaning they are supplied less energy relative to other households of two-, four- and six-persons, to not exceed 75% of energy requirements. Additionally, restricting to six whānau/household members may exclude larger whānau/households from participating. The estimations of energy intake in this article are also limited by using 15 meals from the meal kit home delivery service over the 12 weeks; a greater variety of meals will be provided in the actual study. This estimation cannot be directly extrapolated to a two- or six-person whānau/household as, given the different energy requirements within the described whānau/households, the quantity of products received are not always factors of each other. For instance, a four-person whānau/household does not receive exactly double that of the two-person whānau/household, as its energy requirements are not double considering it factors in a child with lower energy requirements as a member. Again, this reinforces the importance of capturing dietary intake during the trial.
In summary, the MedDiet was able to be adapted to the NZ context for the purpose of He Rourou Whai Painga, along with the development of kai/food baskets containing locally sourced produce. He Rourou Whai Painga will provide valuable insight into the acceptability and effectiveness of this dietary pattern in the NZ population, particularly for Māori who experience a disproportionate and increased burden of CVD. Given the current NZ diet differs largely from the MedDiet, behavioural support and continued partnership with Māori will be important in facilitating adherence to the NZMedDiet.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval was granted by the New Zealand Health and Disability Ethics Committee—Northern B branch—reference 2022 FULL 12045 for He Rourou Whai Painga. Consent is not applicable for this aspect of the trial.
Jeremy D. Krebs, Department of Medicine, University of Otago Wellington, Wellington, New Zealand, Centre for Endocrine, Diabetes and Obesity Research (CEDOR), Wellington Regional Hospital –Te Whatu Ora, Wellington New Zealand, Principal investigator; Richard Gearry, Department of Medicine, University of Otago Christchurch, Christchurch, New Zealand; Troy L. Merry, Discipline of Nutrition, School of Medical Sciences, The University of Auckland, Auckland, New Zealand, Maurice Wilkins Centre for Molecular Biodiscovery, The University of Auckland, Auckland, New Zealand; Andrea Braakhuis, Discipline of Nutrition, School of Medical Sciences, The University of Auckland, Auckland, New Zealand; Fiona Lithander, Discipline of Nutrition, School of Medical Sciences, The University of Auckland, Auckland, New Zealand, Liggins Institute, The University of Auckland, Auckland, New Zealand; Meika Foster, Liggins Institute, The University of Auckland, Auckland, New Zealand, Edible Research Ltd, Ohoka, New Zealand; Anna Rolleston, Manawaora Integrated Health and Research Ltd, Tauranga, New Zealand; Amber Parry-Strong, Centre for Endocrine, Diabetes and Obesity Research (CEDOR), Wellington Regional Hospital–Te Whatu Ora, Wellington New Zealand; Cecilia Ross, Centre for Endocrine, Diabetes and Obesity Research (CEDOR), Wellington Regional Hospital –Te Whatu Ora, Wellington New Zealand; Mark Weatherall, Department of Medicine, University of Otago Wellington, Wellington, New Zealand; Denise Conroy, Plant and Food Research, Auckland, New Zealand; Cheryl Davies, Tū Kotahi Māori Asthma and Research Trust, Kōkiri Marae, Lower Hutt, New Zealand; Anna Worthington, 4 Discipline of Nutrition, School of Medical Sciences, The University of Auckland, Auckland, New Zealand.
AW: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. EL: Writing – original draft, Writing – review & editing. MF: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Supervision, Writing – review & editing. SW: Data curation, Formal analysis, Methodology, Validation, Writing – review & editing. FL: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Writing – review & editing. CW: Formal analysis, Supervision, Writing – review & editing. RR: Data curation, Formal analysis, Writing – review & editing. AP-S: Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Writing – review & editing. JK: Conceptualization, Funding acquisition, Supervision, Writing – original draft, Writing – review & editing. AB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. Research is supported by the High-Value Nutrition National Science Challenge and the Ministry for Business, Innovation and Employment.
We would like to acknowledge Catherine Wall. Additionally, the following food and beverage companies provided food in kind to the study: Chalmers Organics Ltd.; Comvita New Zealand Limited; Firstlight Foods Limited; Goodman Fielder New Zealand Limited; Little Beauties Ltd.; Meadow Mushrooms; Meat Industry Association; AFFCO Limited; Alliance Group Limited; Silver Fern Farms; Greenlea Premier Meats; Auckland Meat Processors Limited; Taylor Preston Limited; Prime Range Meats Limited; Moana New Zealand; Olives New Zealand; Leafyridge Olives; Dali; Noble Estate; Kapiti Olives; Loopline; Rata Olives; Blue Earth; Lot Eight; Olea Estate; The Village Press; Telegraph Hill; Kakariki Olives; Olivo; Old French Road; Mystery Valley Produce; Koru Olives; Fantail Grove; Malmac Trading Limited (trading as Pacific Harvest); Seadragon Marine Oils Limited; Superb Herb; Torere Macadamias; Waikokopu Grove and Orchard; and Zespri International Limited.
MF and SW were employed by the company Edible Research Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2024.1382078/full#supplementary-material
1. Chew, NWS, Ng, CH, Tan, DJH, Kong, G, Lin, C, Chin, YH, et al. The global burden of metabolic disease: data from 2000 to 2019. Cell Metab. (2023) 35:414–428.e3. doi: 10.1016/j.cmet.2023.02.003
2. Noubiap, JJ, Nansseu, JR, Lontchi-Yimagou, E, Nkeck, JR, Nyaga, UF, Ngouo, AT, et al. Geographic distribution of metabolic syndrome and its components in the general adult population: a meta-analysis of global data from 28 million individuals. Diabetes Res Clin Pract. (2022) 188:109924. doi: 10.1016/j.diabres.2022.109924
3. Hauora, Manatū. Custom requested mortality dataset provided to Heart Foundation from the NZ mortality collection. New Zealand: Te Whatu Ora. (2021).
4. Holder-Pearson, L, and Chase, JG. Socio-economic inequity: diabetes in New Zealand. Front Med (Lausanne). (2022) 9:9. doi: 10.3389/fmed.2022.756223
5. Shepard-Wipiiti, T, and Brennan, L. The economic and social cost of type 2 diabetes. (2021) [cited 2023 Aug 31]. Available from: https://healthierlives.co.nz/report-on-the-economic-and-social-cost-of-type-2-diabetes/
6. Chan, W, Wright, C, Riddell, T, Wells, S, Kerr, A, Gala, G, et al. Ethnic and socioeconomic disparities in the prevalence of cardiovascular disease in New Zealand. N Z Med J. (2008) 121:11–20.
7. Afshin, A, Sur, PJ, Fay, KA, Cornaby, L, Ferrara, G, Salama, JS, et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
8. Qiao, J, Lin, X, Wu, Y, Huang, X, Pan, X, Xu, J, et al. Global burden of non-communicable diseases attributable to dietary risks in 1990–2019. J Hum Nutr Diet. (2022) 35:202–13. doi: 10.1111/jhn.12904
9. Davis, C, Bryan, J, Hodgson, J, and Murphy, K. Definition of the Mediterranean diet. Literature Rev Nutris. (2015) 7:9139–53. doi: 10.3390/nu7115459
10. Papadaki, A, Nolen-Doerr, E, and Mantzoros, CS. The effect of the Mediterranean diet on metabolic health: a systematic review and Meta-analysis of controlled trials in adults. Nutrients. (2020) 12:3342. doi: 10.3390/nu12113342
11. Garcia, M, Bihuniak, J, Shook, J, Kenny, A, Kerstetter, J, and Huedo-Medina, T. The effect of the traditional Mediterranean-style diet on metabolic risk factors: a Meta-analysis. Nutrients. (2016) 8:168. doi: 10.3390/nu8030168
12. Dinu, M, Pagliai, G, Casini, A, and Sofi, F. Mediterranean diet and multiple health outcomes: an umbrella review of meta-analyses of observational studies and randomised trials. Eur J Clin Nutr. (2018) 72:30–43. doi: 10.1038/ejcn.2017.58
13. Hauora, M. Eating and activity guidelines for New Zealand adults: Updated 2020. Manatū Hauora. New Zealand: The Ministry of Health(2020).
14. Lovell, AL, Roy, R, Klein, A, Cavadino, A, Foster, M, Krebs, JD, et al. Habitual dietary patterns, nutrient intakes, and adherence to the Mediterranean diet among New Zealand adults: the NZ MED cross-sectional study. Nutrients. (2023) 15:2663. doi: 10.3390/nu15122663
15. McKerchar, C, Bowers, S, Heta, C, Signal, L, and Matoe, L. Enhancing Māori food security using traditional Kai. Glob Health Promot. (2015) 22:15–24. doi: 10.1177/1757975914543573
16. Burgess, H, and Koroi, H. Intergenerational intimacies: a whakapapa conceptualisation of Kai. Tamaki Makaurau. (2024) 9–57.
17. Manatū Hauora, University of Otago. A focus on nutrition: key findings of the 2008/09 New Zealand adult nutrition survey. Ministry of Health. (2011):333.
18. Tucker, C. Using environmental imperatives to reduce meat consumption: perspectives from New Zealand. Kōtuitui: New Zealand J Soc Sci. (2018) 13:99–110. doi: 10.1080/1177083X.2018.1452763
19. Mumme, KD, Conlon, C, von Hurst, PR, Jones, B, de Seymour, JV, Stonehouse, W, et al. Associations between dietary patterns and the metabolic syndrome in older adults in New Zealand: the REACH study. Br J Nutr. (2022) 128:1806–16. doi: 10.1017/S0007114521004682
20. McEvoy, CT, Moore, S, Erwin, C, Kontogianni, M, Wallace, SM, Appleton, KM, et al. Trial to encourage adoption and maintenance of a MEditerranean diet (TEAM-MED): a randomised pilot trial of a peer support intervention for dietary behaviour change in adults from a northern European population at high CVD risk. Br J Nutr. (2022) 128:1322–34. doi: 10.1017/S0007114521003986
21. Woodside, J, Young, IS, and McKinley, MC. Culturally adapting the Mediterranean diet pattern – a way of promoting more ‘sustainable’ dietary change? Br J Nutr. (2022) 128:693–703. doi: 10.1017/S0007114522001945
22. Hoffman, R, and Gerber, M. Evaluating and adapting the Mediterranean diet for non-Mediterranean populations: a critical appraisal. Nutr Rev. (2013) 71:573–84. doi: 10.1111/nure.12040
23. Martínez-González, MA, Salas-Salvadó, J, Estruch, R, Corella, D, Fitó, M, and Ros, E. Benefits of the Mediterranean diet: insights from the PREDIMED study. Prog Cardiovasc Dis. (2015) 58:50–60. doi: 10.1016/j.pcad.2015.04.003
24. Wade, AT, Davis, CR, Dyer, KA, Hodgson, JM, Woodman, RJ, and Murphy, KJ. A Mediterranean diet supplemented with dairy foods improves markers of cardiovascular risk: results from the MedDairy randomized controlled trial. Am J Clin Nutr. (2018) 108:1166–82. doi: 10.1093/ajcn/nqy207
25. Gibson, AA, Seimon, RV, Franklin, J, Markovic, TP, Byrne, NM, Manson, E, et al. Fast versus slow weight loss: development process and rationale behind the dietary interventions for the TEMPO diet trial. Obes Sci Pract. (2016) 2:162–73. doi: 10.1002/osp4.48
26. DeBoer, MD, Filipp, SL, and Gurka, MJ. Use of a metabolic syndrome severity score to track risk during treatment of prediabetes: an analysis of the diabetes prevention program. Diabetes Care. (2018) 41:2421–30. doi: 10.2337/dc18-1079
27. Lithander, FE, Parry-strong, A, Braakhuis, A, Worthington, A, Foster, M, Rolleston, A, et al. He Rourou Whai Painga, an Aotearoa New Zealand dietary pattern for metabolic health and Whānau wellbeing: protocol for a randomised controlled trial. Front Nutrition. (2023) 10:1298743. doi: 10.3389/fnut.2023.1298743
28. Chiriacò, M, Tubili, C, Bo, S, Parillo, M, Vetrani, C, Mazzotti, A, et al. Critical evaluation of the questionnaires assessing adherence to the Mediterranean diet that are based on servings. Nutr Metab Cardiovasc Dis. (2023) 33:724–36. doi: 10.1016/j.numecd.2023.01.024
29. Sofi, F, Macchi, C, Abbate, R, Gensini, GF, and Casini, A. Mediterranean diet and health status: an updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr. (2013) 17:2769–82. doi: 10.1017/S1368980013003169
30. Martínez-González, MA, García-Arellano, A, Toledo, E, Salas-Salvadó, J, Buil-Cosiales, P, Corella, D, et al. A 14-item Mediterranean diet assessment tool and obesity indexes among high-risk subjects: the PREDIMED trial. PLoS One. (2012) 7:e43134. doi: 10.1371/journal.pone.0043134
31. Konieczna, J, Yañez, A, Moñino, M, Babio, N, Toledo, E, Martínez-González, MA, et al. Longitudinal changes in Mediterranean diet and transition between different obesity phenotypes. Clin Nutr. (2020) 39:966–75. doi: 10.1016/j.clnu.2019.04.002
32. Trébuchet, A, Julia, C, Fézeu, L, Touvier, M, Chaltiel, D, Hercberg, S, et al. Prospective association between several dietary scores and risk of cardiovascular diseases: is the Mediterranean diet equally associated to cardiovascular diseases compared to National Nutritional Scores? Am Heart J. (2019) 217:1–12. doi: 10.1016/j.ahj.2019.07.009
33. NZ Heart Foundation. Red meat and poultry position statement. (2020) [cited 2023 Sep 22]. Available from: https://www.heartfoundation.org.nz/resources/red-meat-poultry-and-the-heart-position-statement
34. National Health and Medical Research Council, Australian Government Department of Health and ageing, New Zealand Manatū Hauora. Nutrient Reference Values for Australia and New Zealand. Canberra: National Health and Medical Research Council. (2006).
35. Horwath, C, Parnell, W, Birkbeck, J, Wilson, N, Russell, P, and Herbison, P. Life in New Zealand commission report. Wellington, N.Z: Hillary Commission for Recreation and Sport, c1991. (1991).
36. Winger, R. Australia New Zealand food standards code. Food Control. (2003) 14:355. doi: 10.1016/S0956-7135(03)00044-6
37. Food Standards Australia New Zealand. Standard 1.2.8 nutrition information requirements. Department of Health and Aged Care, Australian Government. (2016).
38. Parry-strong, A, Gearry, R, Merry, T, Weatherall, M, Davies, C, Worthington, A, et al. A high quality Aotearoa New Zealand diet for metabolic health and Whānau wellbeing: a feasibility study. BMC Nutrition. (2023) 9:146.
39. Agnoli, C, Grioni, S, Sieri, S, Palli, D, Masala, G, Sacerdote, C, et al. Italian mediterranean index and risk of colorectal cancer in the Italian section of the EPIC cohort. Int J Cancer. (2013) 132:1404–11. doi: 10.1002/ijc.27740
40. Hauora, Manatū. Alcohol. (2022) [cited 2023 Aug 24]. Available from: https://www.health.govt.nz/your-health/healthy-living/addictions/alcohol-and-drug-abuse/alcohol
41. Tong, TYN, Wareham, NJ, Khaw, KT, Imamura, F, and Forouhi, NG. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk study. BMC Med. (2016) 14:135. doi: 10.1186/s12916-016-0677-4
42. Triatin, RD, Chen, Z, Ani, A, Wang, R, Hartman, CA, Nolte, IM, et al. Familial co-aggregation and shared genetics of cardiometabolic disorders and traits: data from the multi-generational lifelines cohort study. Cardiovasc Diabetol. (2023) 22:282. doi: 10.1186/s12933-023-02017-w
43. Martínez-González, M, Hershey, M, Zazpe, I, and Trichopoulou, A. Transferability of the Mediterranean diet to non-Mediterranean countries. What is and what is not the Mediterranean diet. Nutrients. (2017) 9:1226. doi: 10.3390/nu9111226
44. Schwingshackl, L, Morze, J, and Hoffmann, G. Mediterranean diet and health status: active ingredients and pharmacological mechanisms. Br J Pharmacol. (2020) 177:1241–57. doi: 10.1111/bph.14778
45. Dansinger, ML, Gleason, JA, Griffith, JL, Selker, HP, and Schaefer, EJ. Comparison of the Atkins, Ornish, weight watchers, and zone diets for weight loss and heart disease risk reduction. JAMA. (2005) 293:43–53. doi: 10.1001/jama.293.1.43
46. Gibson, A, and Sainsbury, A. Strategies to improve adherence to dietary weight loss interventions in research and real-world settings. Behav Sci. (2017) 7:44. doi: 10.3390/bs7030044
47. Hauora, M. Adults’ dietary habits – Findings from the 2018/19 and 2019/20 New Zealand health survey. New Zealand: Ministry of Health. (2022).
48. Middleton, G, Keegan, R, Smith, MF, Alkhatib, A, and Klonizakis, M. Implementing a Mediterranean diet intervention into a RCT: lessons learned from a non-Mediterranean based country. J Nutr Health Aging. (2015) 19:1019–22. doi: 10.1007/s12603-015-0663-0
49. Murphy, KJ, and Parletta, N. Implementing a Mediterranean-style diet outside the Mediterranean region. Curr Atheroscler Rep. (2018) 20:28. doi: 10.1007/s11883-018-0732-z
50. Michie, S, Atkins, L, and West, R. The behaviour change wheel. 1st ed. London: Silverback Publishing (2014). 1003–1010 p.
51. McEvoy, CT, Moore, SE, Appleton, KM, Cupples, ME, Erwin, C, Kee, F, et al. Development of a peer support intervention to encourage dietary behaviour change towards a Mediterranean diet in adults at high cardiovascular risk. BMC Public Health. (2018) 18:1194. doi: 10.1186/s12889-018-6108-z
52. Hollænder, PL, Ross, AB, and Kristensen, M. Whole-grain and blood lipid changes in apparently healthy adults: a systematic review and meta-analysis of randomized controlled studies. Am J Clin Nutr. (2015) 102:556–72. doi: 10.3945/ajcn.115.109165
53. Marsh, A, Eslick, EM, and Eslick, GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. (2016) 55:897–906. doi: 10.1007/s00394-015-0922-1
Keywords: Mediterranean diet, metabolic syndrome, cardiovascular diseases, Aotearoa, New Zealand, dietary pattern, dietary behaviour change
Citation: Worthington A, Liu E, Foster M, Wright SR, Lithander FE, Wall C, Roy R, Parry-Strong A, Krebs J and Braakhuis A (2024) Development of an Aotearoa New Zealand adapted Mediterranean dietary pattern and Kai/food basket for the He Rourou Whai Painga randomised controlled trial. Front. Nutr. 11:1382078. doi: 10.3389/fnut.2024.1382078
Received: 19 February 2024; Accepted: 12 July 2024;
Published: 26 July 2024.
Edited by:
Li Chai, China Agricultural University, ChinaReviewed by:
Maud Rizk, University of Balamand, LebanonCopyright © 2024 Worthington, Liu, Foster, Wright, Lithander, Wall, Roy, Parry-Strong, Krebs and Braakhuis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anna Worthington, YW5uYS53b3J0aGluZ3RvbkBhdWNrbGFuZC5hYy5ueg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.