
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 14 March 2024
Sec. Nutrition, Psychology and Brain Health
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1371170
This article is part of the Research TopicNutrition and NeurobehaviorsView all 18 articles
Objective: There have been proposals that vitamin D may be associated with a reduction in the incidence of anxiety disorders. However, the findings thus far have been inconsistent, warranting further investigation. The purpose of this paper is to explore the link between serum vitamin D and anxiety.
Methods: Data are from the National Health and Nutrition Examination Survey (NHANES) in the United States from 2007 to 2012. Study included a total of 12,232 participants, and through the multivariate logistic regression to study the relationship between serum vitamin D and anxiety, smooth curve fitting is used to study the nonlinear relationship between serum vitamin D levels and anxiety.
Results: Serum vitamin D levels demonstrated a negative correlation with anxiety (p < 0.001). Vitamin D exhibited a significant impact on anxiety (Q4:OR = 0.774, 95% CI: 0.663–0.903, p < 0.01), and this effect remained significant even after adjusting for confounding variables (Q4:OR = 0.781, 95% CI: 0.669–0.912, p < 0.01). Smoothed curve fitting revealed a negative association between serum vitamin D levels and the risk of anxiety, and these findings persisted after accounting for confounding variables.
Conclusion: Serum vitamin D levels were inversely associated with anxiety risk in US adults. In the future, more accurate prospective studies are needed to confirm this result.
Anxiety is a common mental illness, mental health in the patient’s quality of life and had a profound influence on overall health (1). Anxiety disorders are a devastating and very common clinical condition that is one of the major causes of global disability (2). These disorders are often accompanied by emotional instability, cognitive dysfunction, and social problems, placing a heavy burden on the patient and the family (3, 4). In order to better understand and treat these mental disorders, researchers have been searching for factors that may be related to the onset of mental impairment and the severity of symptoms.
Vitamin D is a fat-soluble vitamin that is critical not only for bone health, but also for immune system and nervous system function (5–7). In one study, 5.9% of Americans were considered to be vitamin D deficient (serum vitamin D concentration less than 30 mmol or 12 ng/mL), and 24% of Americans were considered to be vitamin D insufficient (serum vitamin D concentration less than 50 mmol or less than 20 ng/mL) (8). Recent studies have shown that vitamin D deficiency is associated with a variety of health problems, including cardiovascular disease, autoimmune disease, and neuropsychiatric disorders (9–11). Vitamin D is therefore not only an essential factor in the maintenance of physical health, but may also have a significant role to play in the onset and progression of mental health problems.
However, there is still some degree of uncertainty about the association of vitamin D with anxiety disorders. A cohort study from the National FondaMental Expertise Centre (FACE-SZ) found that vitamin D supplementation reduces symptoms of depression and anxiety, but treatment of patients with vitamin D deficiency remains inadequate (12), other studies did not find a significant association, for example, in a related study evaluating the relationship between serum vitamin D and anxiety in adult cancer patients before and after chemotherapy, no correlation was found between anxiety scores and serum vitamin D levels in either group (p > 0.05). In another study on vitamin D and mental health in pregnant adolescents in Iran, there was no statistically significant association between vitamin D and anxiety (p > 0.05) (13, 14).
Therefore, this study was to explore the relationship between serum vitamin D levels and anxiety and its internal mechanism. By gaining insight into these associations, we can better understand these common mental disorders and provide more information and possibilities for their prevention and treatment. These findings are expected to have a positive impact on clinical practice and public health policies in the field of mental health.
The National Health and Nutrition Examination Survey (NHANES) is a research program designed to assess the health and nutritional status of adults and children in the United States. It conducts a series of surveys on different populations or health topics. The survey is unique in that it combines interviews and physical examinations. In 1999, the survey became an ongoing program covering a wide range of health and nutrition measures. The project samples about 5,000 people in counties across the country, with 15 counties visited each year. Random selection is made through a statistical process using the United States Census information. Three cycles of data from 2007–2012 were used for this cross-sectional study. Participants with incomplete information on anxiety, missing serum vitamin D data and basic information, and age < 20 years were excluded. In addition, subjects with missing serum vitamin D information and subjects with mean ± standard deviation more than three times the mean were also excluded. Finally, a total of 12,232 individuals were included in the final analysis (Figure 1).
The principle of the assay is the quantitative determination of 25-hydroxyvitamin D3 (25OHD3), epi-25-hydroxyvitamin D3 (epi-25OHD3) and 25-hydroxyvitamin D2 (25OHD2) in human serum using ultra-high performance liquid chromatography–tandem mass spectrometry (UHPLC–MS/MS). To process serum samples, an ethanol solution containing the three internal standards and 69–72% methanol solution is added first, followed by hexane. Analytes from the water phase extraction to n-hexane layer (liquid–liquid extraction), and then drying under vacuum. Extract with 69–72% of methanol to dissolve. To extract uniform fluid injection PFP column,25OHD3, epi-25OHD3, 25OHD2 and internal standard (is) 26,27-hexadeuterium-25-hydroxyvitamin D3, 6,19,19-trideuterium-3-epi-25-hydroxyvitamin were isolated D3 and 6,19, 19-Trideuterium-25-hydroxyvitamin D2. Use MS–ms in Thermo TSQ Vantage system, using positive ion mode of atmospheric pressure chemical ionization. Quantitative is by comparing the unknown peak area of analytes and calibrator known quantity in the solution of the analyte peak area. According to the internal standard peak area of objects with unknown calibration fluid matching of internal standard peak area in comparison, the calculation results are correct.
In this study, “serum vitamin D” refers to the concentration of 25OHD2 + 25OHD3 in the blood (nmol/L). Measurement of serum levels of 25OHD2 and 25OHD3 can provide insight into whether an individual has enough of the precursor form in their body for further metabolism to the active form in response to vitamin D intake and sun exposure. This provides an assessment of an individual’s overall vitamin D status and can help guide vitamin D supplementation or adjustments to diet and sun exposure.
In NHANES 2007–2012, information on anxiety status was collected by questionnaire using a computer assisted personal interview (interviewer administration) system during physical examination at a mobile examination center (MEC). Anxiety was evaluated during the individual interview by the following question, “During the past 30 days, about how many days did you feel worried, nervous, or anxious?” This evaluation is based on the 14-item Healthy Days measure developed by the United States Centers for Disease Control and Prevention (CDC), which has been incorporated into the Health-Related Quality of Life (HRQoL) assessment. The reliability of HRQoL monitoring questions is moderate to excellent (15). Anxiety states were categorized as “no” (feeling anxious 0 to 6 days per month) and “yes” (feeling anxious 7 to 30 days per month) (16).
Demographic information was collected using a standardized questionnaire, including gender (male or female), age, race (Mexican American, other Hispanic, non-Hispanic white, non-Hispanic black, or other race), marital status (not living alone, living alone), education (< high school, high school, > high school), and poverty income ratio. Other confounding variables include smoking (defined as smoking at least 100 cigarettes in a lifetime) and alcohol consumption (defined as drinking at least 12 drinks in a year) (17). Hypertension and diabetes were derived from self-reported physician diagnosis (yes/no). Body mass index is calculated weight (kg) divided by the square of height (m2).
The baseline information was expressed as mean ± standard deviation (SD) for continuous variables and as frequency (composition ratio) [n(%)] for categorical variables. For continuous variables, Kruskal Wallis rank sum tests were performed and Fisher’s exact probability tests were performed for count variables with theoretical counts less than 10. Multivariate logistic regression used appropriate weights. Smoothed curve fitting was employed to explore the non-linear association of serum vitamin D with anxiety symptoms. Model 1 was unadjusted, model 2 was adjusted for gender, age, and race, and model 3 was adjusted for all variables including gender, age, race, education, marital status, body mass index, poverty income ratio, drinking status, smoking status, diabetes, and hypertension. In the regression model, each quantile median serum vitamin D levels are used for continuous variables, to calculate the p for trend. p values <0.05 on both sides were considered statistically significant. We merged and transformed the data using SPSS 27.0, followed by weighted analyses and smoothed curve fitting using EmpowerStats software.1
The object of study for a total of 12,232 people. Table 1 shows the characteristics of a stratified study population based on serum vitamin D quartiles from the National Health and Nutrition Examination Survey (NHANES) 2007–2012. The analyses revealed significant differences among serum vitamin D levels and various factors. In demographic characteristics, was significantly associated with age and serum vitamin D levels (p < 0.001). Significant differences (p < 0.001) were found between other variables such as gender, race, education, marital status, smoking status, drinking status, hypertension, body mass index, poverty income ratio, and serum vitamin D.
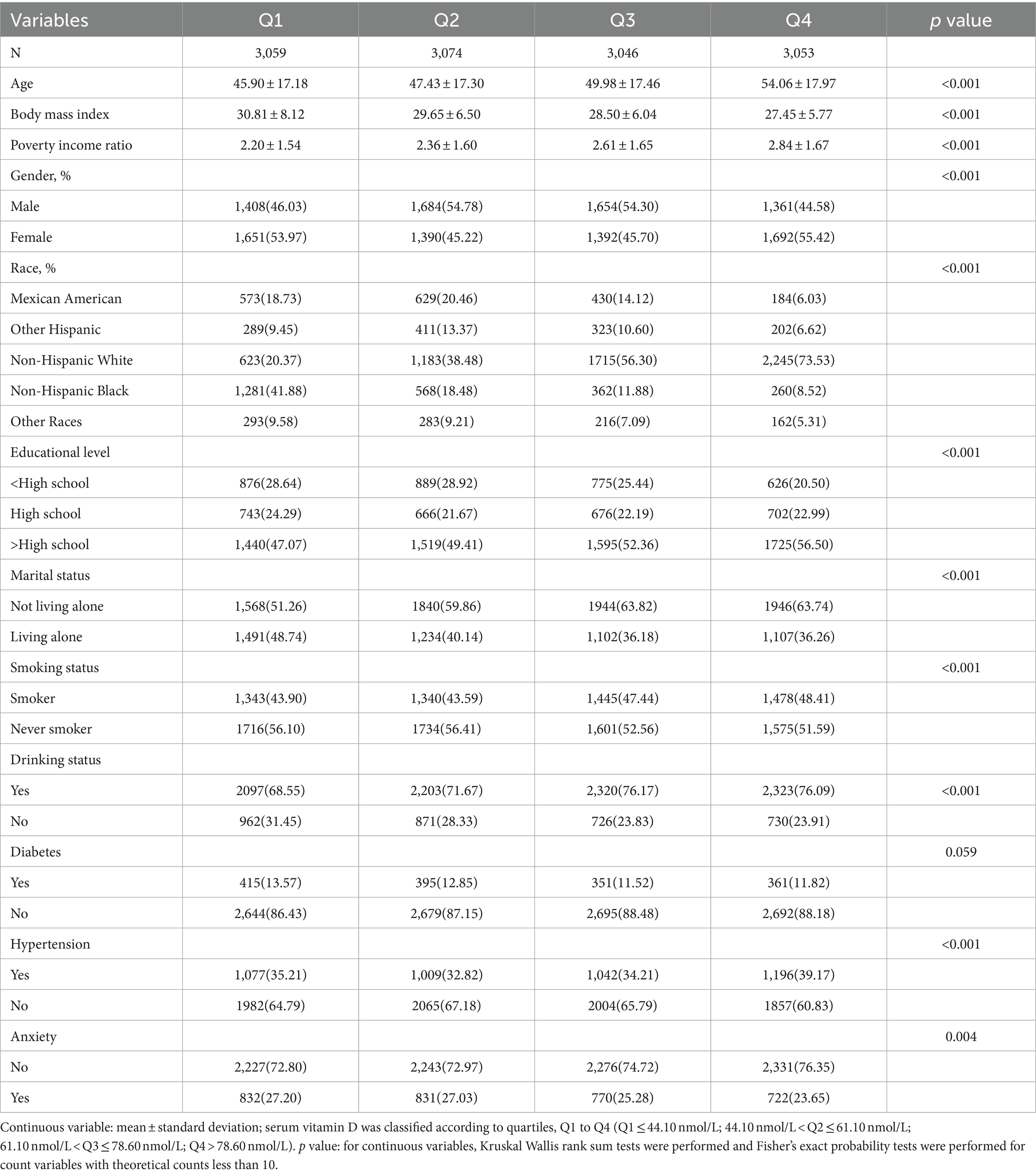
Table 1. Study population characteristics based on the serum vitamin D group in NHANES, 2007–2012 (N = 12,232).
Table 2 shows the characteristics of the participants according to the number of days of anxiety. A total of 3,155 participants engaged in anxious behavior for 7 or more days in a 30-day period. The mean age of anxious subjects was 46.70 ± 16.22 years, which was significantly lower than the age of non-anxious subjects (50.25 ± 18.16 years, p < 0.001). It was also found that anxious subjects had higher body mass index levels than non-anxious subjects and lower serum vitamin D levels than non-anxious subjects (60.89 ± 24.14 nmol/L, p < 0.001). Females were more prone to anxiety (59.46%). Significant differences were found between the two groups in gender, age, body mass index, poverty income ratio, serum vitamin D, race, education, marital status, smoking status, drinking status, hypertension, and diabetes (p < 0.05).
In Table 3, logistic regression analyses were performed between each variable and anxiety. We found that females had a higher risk of anxiety compared to males (OR = 1.506, 95% CI: 1.349–1.681, p < 0.001), older people aged 60 years and above had a lower risk of anxiety compared to younger people aged 20–39 years, and those with high educational qualifications had a lower risk of anxiety compared to those with low educational qualifications. People who were living alone had a higher risk of developing an anxiety disorder, while non-smokers had a lower risk of developing an anxiety disorder.
Table 4 shows the relationship between serum vitamin D levels and anxiety. Participants were grouped according to the interquartile range (IQR) of serum vitamin D (Q 1: 0–25%; Q 2: >25–50%; Q 3: >50–75%; Q 4: >75%) and analyzed using Q 1 as the reference group. In Model 1, no adjustment was made for any of the variables. Serum vitamin D was significantly associated with anxiety in Q 4 compared to Q 1, with an OR and 95% CI of 0.774 (0.663, 0.903). The results of Model 2, adjusted for gender, age and race, showed that serum vitamin D levels were negatively associated with anxiety with an OR and 95% CI of 0.730 (0.621, 0.857). Model 3 was adjusted for all covariates. Serum vitamin D in Q4 was significantly associated with anxiety, with an OR and 95% CI of 0.781(0.669,0.912), respectively. In all three models, p for trend was less than 0.001.
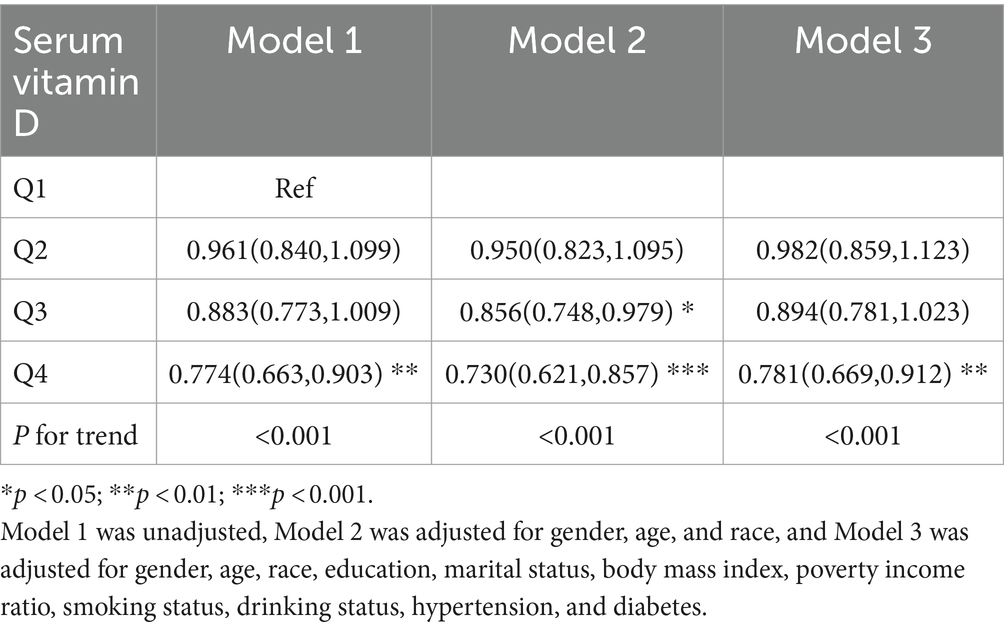
Table 4. Results of multivariate logistic analysis of the relationship between serum vitamin D and anxiety, weighted.
We performed a smoothed curve fit as shown in Figure 2. Figure 2A is unadjusted for variables, showing that as serum vitamin D levels increase, anxiety risk decreases. In Figure 2B, when all variables were adjusted, anxiety risk decreased as vitamin D levels increased. In Figure 3, the results of the smoothed curve fit showed an overall decreasing trend in anxiety risk with increasing serum vitamin D levels after stratifying by gender, age, race, education, marital status, smoking status, drinking status, hypertension, and diabetes, respectively.
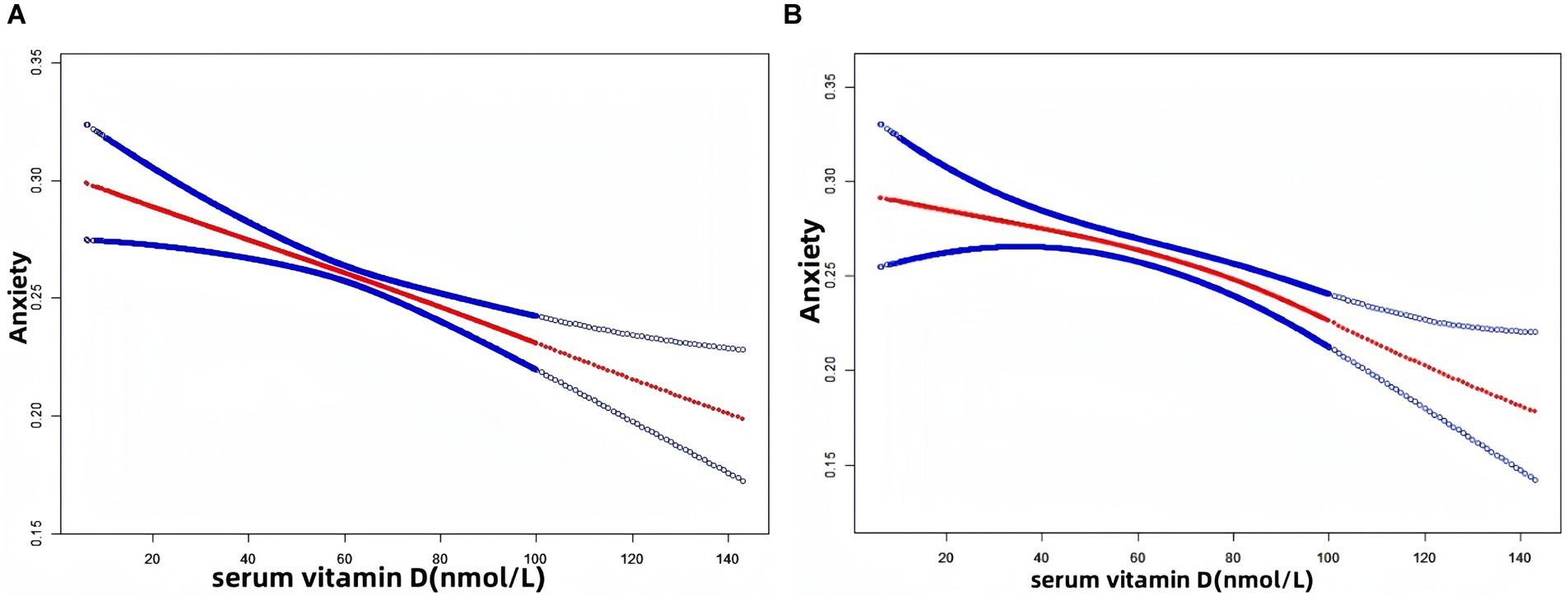
Figure 2. Results of smoothed curve fitting between serum vitamin D and anxiety. (A) Unadjusted for variables; (B) Adjusted for gender, age, race, education, marital status, body mass index, poverty income ratio, smoking status, drinking status, hypertension, and diabetes. The red solid arcs indicate the smoothed curve fitting between the variables. The area between the two blue dashed lines represents the 95% CI.
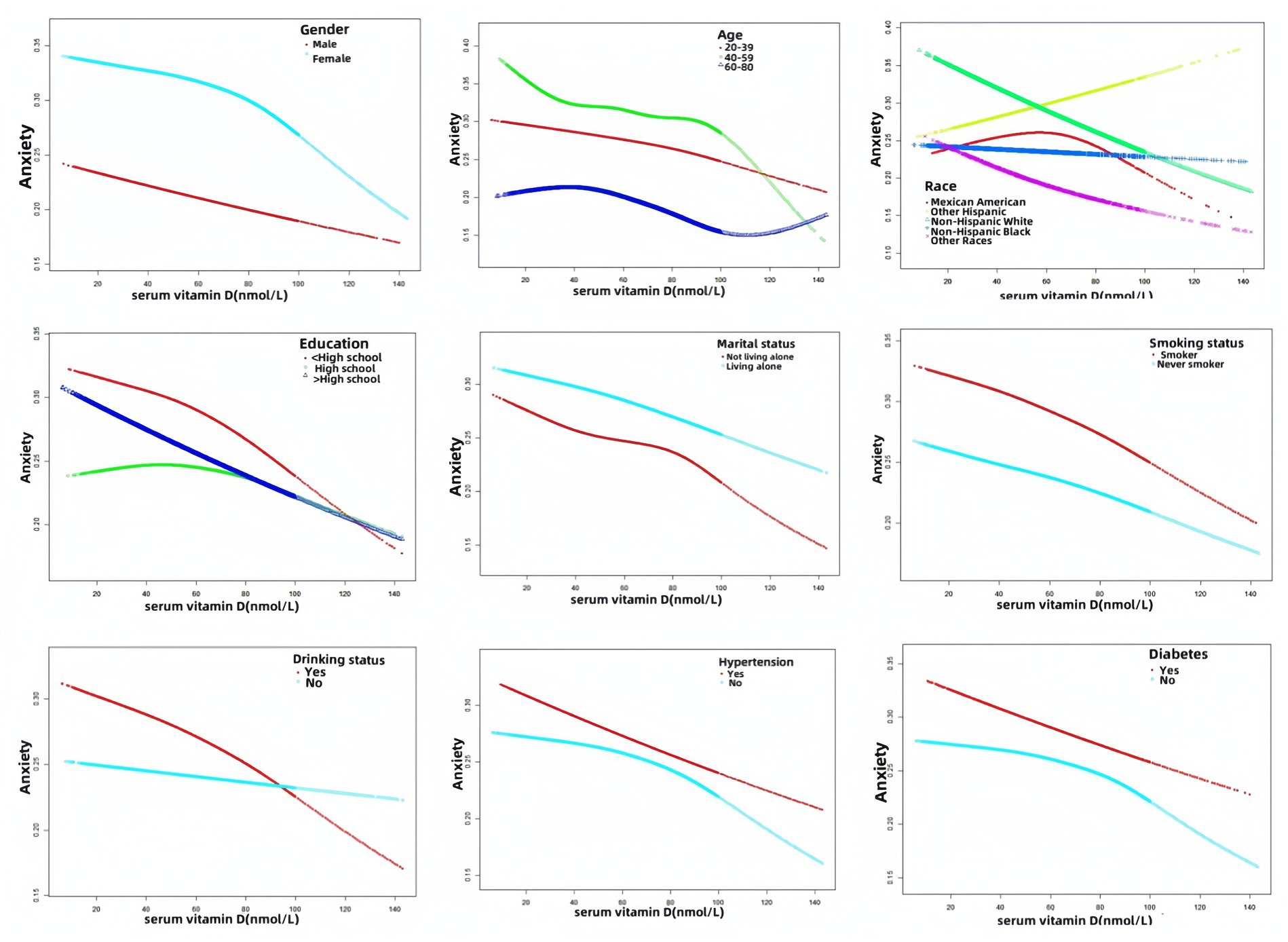
Figure 3. Results of smoothed curve fitting between serum vitamin D and anxiety stratified by gender, age, race, education, marital status, smoking status, drinking status, hypertension, and diabetes.
To our knowledge, this is the first article to use NHANES data to study the serum vitamin D-anxiety relationship. We use NHANES data of 2007–2012, and use weighted logistic regression and smoothing curve fitting analysis of serum vitamin D concentrations and the relationship between the risk of anxiety symptoms. The results showed that serum vitamin D was inversely associated with the risk of anxiety symptoms in adults.
Many studies have confirmed the beneficial effects of vitamin D on the development of anxiety disorders. A study has found that vitamin D supplements can effectively reduce the severity of generalized anxiety symptoms (18). Low vitamin D levels were linked to increased depression and anxiety symptoms in a study on the role of vitamin D in anxiety (19). In a about vitamin D supplement for older people with pre-diabetes the influence of anxiety and depression state of randomized controlled study, found that once a week for vitamin D supplement plan can effectively alleviate the high risk population of anxiety and depression symptoms (20). In addition, in a relatively young endurance athletes increase the intake of vitamin D may reduce mental anxiety (21). Finally, in a biological experiment, it was observed that mice exhibited increased anxiety-like behavior on behavioral tests after vitamin D deficiency (22).
Of course, some studies have reported results contrary to ours. There was no correlation found between depression and anxiety scores and serum vitamin D levels in a study assessing the relationship between serum vitamin D and B12 levels, nutritional levels, depression and anxiety in adult cancer patients before and after chemotherapy (13). In a study examining the relationship between vitamin D and anxiety and depression in pregnant adolescents, no relationship was found between serum vitamin D and anxiety or depression (14). In one of Australia’s young women 25—hydroxy serum vitamin D and the study of mental health, vitamin D status also proved to have nothing to do with depression or anxiety diagnosis report (23). Overall, there are inconsistent findings regarding the association between vitamin D and anxiety, which may be due to differences in demographic characteristics of the study samples, study design, environmental factors, seasonal variations, co-morbidities, and dietary habits.
The relationship between serum vitamin D and anxiety varies across demographic and lifestyle factors. Gender differences may be due to differential effects of sex hormones on vitamin D metabolism and the nervous system, whereas age differences may be related to age-related declines in the ability to synthesize vitamin D and more chronic health problems in older people. In terms of race differences, there may be genetic differences as well as social, cultural, and economic differences. Education level may reflect socioeconomic status and access to resources, while marital status may be associated with social support, family stress, and life stability. Smoking and drinking differences may relate to the effects of these habits on vitamin D metabolism and the immune system, as well as their relationship to ways of coping with stress and social activities. Finally, hypertension and diabetes differences may be due to the fact that chronic diseases indirectly affect anxiety levels by affecting the inflammatory responses (24, 25). Further research is needed in the future to confirm these findings and determine the reasons for this discrepancy.
A unique neurosteroid hormone, vitamin D’s receptors are found in neurons and glial cells in different parts of the brain, including the cingulate gyrus and hippocampus (26). Vitamin D with antioxidant and anti-inflammatory properties, promote neurogenesis and neural regulation, and adjust the gut microbiota (27). It in regulating neurotrophic factor, nerve protection, neural plasticity, brain development and neural immune adjustment plays an important role in the process of brain (28). Vitamin D deficiency may contribute to anxiety and depression (29).
Mechanisms of action between vitamin D and anxiety have been studied. Neurons and glial cells in different areas of the prefrontal cortex and hippocampus system expression of VDR and vitamin D metabolism enzymes, suggesting that vitamin D may play a role in anxiety (30). Positive regulation of antioxidant enzymes by osteotriol (a form of vitamin D) contributes to redox homeostasis and thus attenuates neuroinflammatory processes (31, 32). Vitamin D in the immune and nervous regulation part through its interaction with gut microbiota (33). Vitamin D deficiency, VDR, or CYP27B1 depletion has been shown to cause an increase in Mycobacterium anisopliae and Mycobacterium avium, triggering epithelial barrier dysfunction and intestinal inflammation. The positive regulation of antioxidant enzymes such as HO-1, CAT, and SOD by calcitriol contributes to the REDOX balance, thereby reducing the neuroinflammatory process (34, 35).
There are several benefits of our study as follows. To ensure the validity of our results, we used appropriate weighting and confounding adjustments in our analyses. Second, our sample size was large enough to effectively reveal the relationship between serum vitamin D and anxiety. Finally, we focused specifically on the relationship between serum vitamin D levels and anxiety. Compared to depression, relatively few studies have been conducted on the relationship between serum vitamin D and anxiety. There are also several flaws in our study. Firstly, because this was a cross-sectional study, it was not possible to determine a causal relationship between serum vitamin D and anxiety. Second, the measure of anxiety was a self-reported outcome by the subjects and may have been influenced by subjective factors. In addition, it was not possible to adjust for all covariates, and only those included were adjusted. Potential uncontrolled variables may still influence our conclusions. Finally, these data are from the American population and caution should be exercised when extrapolating to the population as a whole.
Serum vitamin D was inversely associated with anxiety. The future more prospective studies are needed to confirm this.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found at: https://www.cdc.gov/nchs/nhanes.
The studies involving humans were approved by National Center for Health Statistics Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
ZW: Conceptualization, Writing – original draft. LB: Conceptualization, Investigation, Software, Writing – original draft, Writing – review & editing. SW: Writing – review & editing. JC: Writing – review & editing. HJ: Writing – review & editing. JS: Writing – review & editing.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Ministry of Humanities and Social Science Education Project (No. 19YJC630182) and Scientific Research Foundation for Excellent Talents of Xuzhou Medical University (No. D2019004).
The authors sincerely appreciate the researchers who shared the original dataset for this study. For additional requirements for specific article types and further information please refer to “Article types” on every Frontiers journal page.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kimball, SM, Mirhosseini, N, and Rucklidge, J. Database analysis of depression and anxiety in a community Sampleresponse to a micronutrient intervention. Nutrients. (2018) 10:152. doi: 10.3390/nu10020152
2. Pennington, A . Anxiety Disorders. Prim Care. (1997) 24:103–11. doi: 10.1016/S0095-4543(22)00088-4
3. Gao, YN, Coombes, B, Ryu, E, Pazdernik, V, Jenkins, G, Pendegraft, R, et al. Phenotypic distinctions in depression and anxiety: a comparative analysis of comorbid and isolated cases. Psychol Med. (2023) 53:7766–74. doi: 10.1017/S0033291723001745
4. An, JH, Jeon, HJ, Cho, S-J, Chang, SM, Kim, B-S, Hahm, B-J, et al. Subthreshold lifetime depression and anxiety are associated with increased lifetime suicide attempts: a Korean Nationwide study. J Affect Disord. (2022) 302:170–6. doi: 10.1016/j.jad.2022.01.046
5. Charoenngam, N, Shirvani, A, and Holick, MF. Vitamin D for skeletal and non-skeletal health: what we should know. J Clin Orthop Trauma. (2019) 10:1082–93. doi: 10.1016/j.jcot.2019.07.004
6. Eder, K, and Grundmann, SM. Vitamin D in dairy cows: metabolism, status and functions in the immune system. Arch Anim Nutr. (2022) 76:1–33. doi: 10.1080/1745039X.2021.2017747
7. Norlin, M . Effects of vitamin D in the nervous system: special focus on interaction with steroid hormone Signalling and a possible role in the treatment of brain Cancer. J Neuroendocrinol. (2020) 32:e12799. doi: 10.1111/jne.12799
8. Schleicher, RL, Sternberg, MR, Looker, AC, Yetley, EA, Lacher, DA, Sempos, CT, et al. National Estimates of serum Total 25-Hydroxyvitamin D and metabolite concentrations measured by liquid chromatography-tandem mass spectrometry in the us population during 2007-2010. J Nutr. (2016) 146:1051–61. doi: 10.3945/jn.115.227728
9. Oberoi, D, Mehrotra, V, and Rawat, A. "vitamin D" as a profile marker for cardiovascular diseases. Ann Card Anaesth. (2019) 22:47–50. doi: 10.4103/aca.ACA_66_18
10. Wisniewska, A, and Szypowska, A. The role of vitamin D in selected autoimmune diseases. Rocz Panstw Zakl Hig. (2021) 72:111–21. doi: 10.32394/rpzh.2021.0156
11. Rihal, V, Khan, H, Kaur, A, Singh, TG, and Abdel-Daim, MM. Therapeutic and mechanistic intervention of vitamin D in neuropsychiatric disorders. Psychiatry Res. (2022) 317:114782. doi: 10.1016/j.psychres.2022.114782
12. Fond, G, Godin, O, Schurhoff, F, Berna, F, Bulzacka, E, Andrianarisoa, M, et al. Hypovitaminosis D is associated with depression and anxiety in schizophrenia: results from the national Face-Sz cohort. Psychiatry Res. (2018) 270:104–10. doi: 10.1016/j.psychres.2018.09.024
13. Kacar, M, and Erzurum, AN. The dietary risk factors on Cancer patients receiving chemotherapy and correlation between serum vitamin D and B12 levels, Depression and Anxiety Status. Nutr Hosp. (2023) 41:112–21. doi: 10.20960/nh.04530
14. Bahramy, P, Mohammad-Alizadeh-Charandabi, S, Ramezani-Nardin, F, and Mirghafourvand, MSerum Levels of Vitamin D, Calcium. Magnesium, and copper, and their relations with mental health and sexual function in pregnant Iranian adolescents. Biol Trace Elem Res. (2020) 198:440–8. doi: 10.1007/s12011-020-02109-8
15. Andresen, EM, Catlin, TK, Wyrwich, KW, and Jackson-Thompson, J. Retest reliability of surveillance questions on health related quality of life. J Epidemiol Community Health. (2003) 57:339–43. doi: 10.1136/jech.57.5.339
16. Dantzer, JA, and Keet, CA. Anxiety associated with food allergy in adults and adolescents: an analysis of data from the National Health and nutrition examination survey (Nhanes) 2007-2010. J Allergy Clin Immunol Pract. (2020) 8:1743–1746.e5. doi: 10.1016/j.jaip.2019.12.028
17. Cui, A, Xiao, P, Ma, Y, Fan, Z, Zhou, F, Zheng, J, et al. Prevalence, trend, and predictor analyses of vitamin D deficiency in the us population, 2001-2018. Front Nutr. (2022) 9:965376. Epub 2022/10/21. doi: 10.3389/fnut.2022.965376
18. Eid, A, Khoja, S, AlGhamdi, S, Alsufiani, H, Alzeben, F, Alhejaili, N, et al. Vitamin D supplementation ameliorates severity of generalized anxiety disorder (gad). Metab Brain Dis. (2019) 34:1781–6. doi: 10.1007/s11011-019-00486-1
19. Akpinar, S, and Karadag, MG. Is vitamin D important in anxiety or depression? What is the truth? Curr Nutr Rep. (2022) 11:675–81. doi: 10.1007/s13668-022-00441-0
20. Zaromytidou, E, Koufakis, T, Dimakopoulos, G, Drivakou, D, Konstantinidou, S, Rakitzi, P, et al. Vitamin D alleviates anxiety and depression in elderly people with prediabetes: a randomized controlled study. Meta. (2022) 12:884. doi: 10.3390/metabo12100884
21. Miyamoto, M, Hanatani, Y, and Shibuya, K. Increased vitamin D intake may reduce psychological anxiety and the incidence of menstrual irregularities in female athletes. PeerJ. (2022) 10:e14456. doi: 10.7717/peerj.14456
22. Kalueff, AV, Lou, YR, Laaksi, L, and Tuohimaa, P. Increased anxiety in mice lacking vitamin D receptor gene. Neuroreport. (2004) 15:1271–4. doi: 10.1097/01.wnr.0000129370.04248.92
23. Callegari, ET, Reavley, N, Gorelik, A, Garland, SM, Wark, JD, and Safe, DST. Serum 25-Hydroxyvitamin D and mental health in young Australian women: results from the Safe-D study. J Affect Disord. (2017) 224:48–55. doi: 10.1016/j.jad.2016.10.002
24. Virdis, A, Dell'Agnello, U, and Taddei, S. Impact of inflammation on vascular disease in hypertension. Maturitas. (2014) 78:179–83. doi: 10.1016/j.maturitas.2014.04.012
25. Domingueti, CP, Dusse, LM, Md, C, de Sousa, LP, Gomes, KB, and Fernandes, AP. Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complicat. (2015) 30:738–45. doi: 10.1016/j.jdiacomp.2015.12.018
26. Ma, J, and Li, K. Negative association between serum vitamin D levels and depression in a young adult us population: a cross-sectional study of Nhanes 2007-2018. Nutrients. (2023) 15:2947. doi: 10.3390/nu15132947
27. Kouba, BR, Camargo, A, Gil-Mohapel, J, and Rodrigues, ALS. Molecular basis underlying the therapeutic potential of vitamin D for the treatment of depression and anxiety. Int J Mol Sci. (2022) 23:7077. doi: 10.3390/ijms23137077
28. Zhu, CZ, Zhang, Y, Wang, T, Lin, Y, Yu, J, Xia, Q, et al. Vitamin D supplementation improves anxiety but not depression symptoms in patients with vitamin D deficiency. Brain Behav. (2020) 10:10. doi: 10.1002/brb3.1760
29. Al Anouti, F, Grant, WB, Thomas, J, AlBlooshi, S, and Karras, S. Associations between dietary intake of vitamin D, sun exposure, and generalized anxiety among college women. Nutrients. (2022) 14:5327. doi: 10.3390/nu14245327
30. Eyles, DW, Smith, S, Kinobe, R, Hewison, M, and McGrath, JJ. Distribution of the vitamin D receptor and 1α-hydroxylase in human brain. J Chem Neuroanat. (2005) 29:21–30. doi: 10.1016/j.jchemneu.2004.08.006
31. Nakajo, T, Katayoshi, T, Kitajima, N, and Tsuji-Naito, K. 1,25-Dihydroxyvitamin D attenuates Il-1β secretion by suppressing Nlrp1 Inflammasome activation by upregulating the Nrf2-ho-1 pathway in epidermal keratinocytes. Redox Biol. (2021) 48:102203. doi: 10.1016/j.redox.2021.102203
32. Yamini, P, Ray, RS, and Chopra, K. Vitamin D attenuates cognitive deficits and Neuroinflammatory responses in Icv-Stz induced sporadic Alzheimer's disease. Inflammopharmacology. (2018) 26:39–55. doi: 10.1007/s10787-017-0372-x
33. Luthold, RV, Fernandes, GR, Carolina Franco-de-Moraes, A, Folchetti, LGD, and Ferreira, SRG. Gut microbiota interactions with the immunomodulatory role of vitamin D in Normal individuals. Metabolism. (2017) 69:76–86. doi: 10.1016/j.metabol.2017.01.007
34. Assa, A, Vong, L, Pinnell, LJ, Avitzur, N, Johnson-Henry, KC, and Sherman, PM. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. (2014) 210:1296–305. doi: 10.1093/infdis/jiu235
Keywords: serum vitamin D, anxiety, NHANES, smoothed curve fitting, weighted logistic regression
Citation: Wen Z, Bai L, Wu S, Chen J, Jama HA and Sawmadal JD (2024) Association of serum vitamin D with anxiety in US adults: a cross-sectional study. Front. Nutr. 11:1371170. doi: 10.3389/fnut.2024.1371170
Received: 16 January 2024; Accepted: 27 February 2024;
Published: 14 March 2024.
Edited by:
Nazlı Nur Aslan Çin, Karadeniz Technical University, TürkiyeReviewed by:
Hülya Yardımcı, Ankara University, TürkiyeCopyright © 2024 Wen, Bai, Wu, Chen, Jama and Sawmadal. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zongliang Wen, d2VuemxAeHpobXUuZWR1LmNu
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.