- 1School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of pharmacy, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of psychiatry, School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
Background: Acute malnutrition is a major global public health problem, particularly in low-and middle-income countries. A targeted supplementary feeding program is an approach recommended to address moderate acute malnutrition in food-insecure settings. Preventing and treating moderate acute malnutrition requires identifying factors shown to affect the treatment outcome and duration of stay on treatment. This study aimed to determine the time to recovery from moderate acute malnutrition and its predictors among children aged 6–59 months in Fedis Woreda East Hararghe Zone, Eastern Ethiopia, from January 1 to December 31, 2022.
Methods: A facility-based retrospective cohort study was conducted on 567 children with moderate acute malnutrition in Fedis Woreda, East Hararghe Zone, eastern Ethiopia. A multi-stage sampling technique was employed, and data was collected using a structured checklist. Data were extracted from randomly selected records after obtaining ethical clearance. Data were cleaned, coded, entered into EpiData 4.6, and analyzed using STATA/SE version 14. Descriptive statistics and analytic analysis schemes, including bivariable and multivariable Cox proportional hazards models, were conducted, and finally, statistical significance was considered at p < 0.05.
Results: The overall median time to recovery was 16 weeks. The major predicting factors for time to recovery among children aged 6–59 months were admission with a mid-upper arm circumference of 12.1–12.4 centimeters (AHR = 1.02, 95% CI: 1.01–1.19), access to transportation to facilities (AHR = 0.62, 95% CI: 0.36–0.81), children using specialized nutritious foods (RUSF; AHR = 1.96, 95% CI: 1.36–3.11), and children who had diarrhea (AHR = 0.4, 95% CI: 0.31–0.71).
Conclusion: The study found a median recovery time of 16 weeks for children with targeted supplementary feeding. Significant predictors included admission with a MUAC of 12.1–12.4 centimeters, transportation access, RUSF use, and the presence of diarrhea. These findings highlighted the importance of these factors in determining and improving recovery from moderate-acute malnutrition.
Introduction
Malnutrition refers to deficiencies or excesses in nutrient intake, an imbalance of essential nutrients, or impaired nutrient utilization (1). Acute malnutrition is one of the three main types of under-nutrition, affecting potentially all categories of the population but especially vulnerable groups such as children under five, pregnant and lactating women, and people living with a disease or chronic illness (2). Acute malnutrition results from a sudden reduction in food intake or diet quality, and it is often combined with pathological causes. It is classified as moderate acute malnutrition (MAM)/ wasted or severe acute malnutrition (SAM)/ severely wasted (3). Severe acute malnutrition is defined as a very low weight for height (WFH) below -3z scores of the median WHO growth standards, and/ or MUAC <11.5 cm, and/ or presence of nutritional edema (4). Moderate acute malnutrition (MAM), defined as having a weight-for-height Z-score (WHZ) −3 and − 2, without edema and/or mid-upper arm circumference (MUAC) 11.5 to <12.5 cm (5). It is associated with increased mortality and morbidity among children under 5 years of age (6, 7).
Children with MAM face a greater risk of morbidity from infectious diseases, weakened immune systems, and impaired physical and cognitive development (7–9). Moreover, beyond deterioration to severe acute malnutrition, a recent study suggested that repeated episodes of moderate acute malnutrition in children can eventually lead to stunting over time with irreversible inter-generational growth failure (10).
Targeted Supplementary Feeding is implemented in food insecure situations, including in emergencies, in order to treat MAM and prevent children with MAM from becoming severely malnourished (falling into SAM). It is usually indicated when MAM and SAM prevalence rates are between 10 and 14% or 5–9% with aggravating circumstances (11). In Ethiopia, 7% of children 6–59 months of age are wasted, with 70% of these having MAM, and about 35 to 57% of the deaths in under-five children are attributable to malnutrition (12). Malnutrition among children is a critical problem because its effects are long-lasting, go beyond childhood, and affect academic performance, physical development, and mental development throughout their lives (13).
Globally, an estimated 47 million children younger than 5 years had acute malnutrition, of which 70% were attributed to moderate acute malnutrition (14). Africa and Asia bear the greatest share of moderate-acute malnutrition (7). Acute malnutrition prevalence varies across regions and countries, with a high burden remaining in low-and middle-income countries, with an estimated figure of 7.7, 2.0, and 0.7% in South Asia, Sub-Saharan Africa, and Latin America, respectively (15). Ethiopia has made substantial progress in reducing the prevalence of malnutrition in the past two decades (16, 17). However, childhood under-nutrition, particularly moderate acute malnutrition, remains a major challenge (18). Moreover, the progress made has been uneven across the administrative regions of Ethiopia, as the prevalence of moderate acute malnutrition ranges from the highest of 21% in the Somali region to the lowest of 2% in Addis Ababa (19).
Previous studies conducted in various regions of Ethiopia have been focused on the management of severe acute malnutrition (20–23). However, the management of moderate acute malnutrition should also be a public health and development priority (24). Preventing and treating MAM requires understanding the factors shown to affect the management outcomes and duration of stay on treatment (25). Though the recovery time of MAM is within a wide statistical range, no study reported MAM treatment outcomes, particularly in the eastern part of Ethiopia. This study seeks to shed light on the time to recovery from MAM and its predictors among children aged 6–59 months in Fedis Woreda, East Hararghe Zone, eastern Ethiopia.
Materials and methods
Study design, and setting
This study employed an institution-based retrospective cohort study and was conducted from January 1 to December 30, 2022, in Fedis woreda, East Hararghe Zone, Oromia region, located 541 km to the east of Addis Ababa and 24 km to the south of Harar Town.
Fedis Woreda is situated in the East Hararghe Zone of eastern Ethiopia. The district has an estimated population of 168,770. To address food insecurity, Fedis Woreda has implemented targeted and blanket food supply programs. The health infrastructure consists of five government health centers and 21 health posts, all offering services for children with moderate acute malnutrition (MAM) and pregnant and lactating women (PLW). Data for this study was extracted from February 1, 2023, to March 30, 2023.
Population and sampling
The study population consisted of children aged 6 to 59 months who were diagnosed with moderate malnutrition and enrolled in the targeted supplementary feeding (TSF) program at selected health posts in Fedis Woreda from January 1 to December 30, 2022. Records of all eligible 6-59-month-old children who were identified from the registration book and identified to have moderate acute malnutrition were included in the study, whereas records with incomplete information like missed age, sex, and MUAC were excluded from four health posts.
The sample size was determined using both a single and double population proportion formula. The maximum sample was achieved by using a double proportion formula by considering the assumptions: 95% confidence level, 80% power, one-to-one ratio, proportion [p1 = 43.8%, p2 = 56.2% (26), and 10% of non-respondents]. The final sample size was 567.
In the study area, 8 out of the 21 health posts in the woreda were randomly selected using a lottery method to ensure representativeness. The assumption was made that the populations around these health posts were relatively homogeneous. The management protocol for moderate acute malnutrition (MAM) was standardized across all health post-levels in the woreda. A sampling frame was created for children undergoing MAM management in the eight selected health posts. Probability proportional to size sampling was used to allocate samples to each health post based on their population size.
Finally, children were selected for the study through simple random sampling within each health post, using their unique identification numbers, to ensure a representative sample from the selected institutions.
Data collection methods and quality control
Data for the study was extracted from the registration book using a well-designed data extraction form. Data were collected by eight trained health extension workers and supervised by two BSc nurses. The records of eligible children were retrieved from the registration book, and their individual cards were reviewed. Relevant information, including admission medical history, physical examination findings, follow-up anthropometry measurements, clinical features, routine medications, and outcome status, was recorded.
A pre-test of the data collection tool was conducted in the Fedis district. Completed questionnaires were checked for completeness and consistency. Data cleaning was done daily, and then feedback was given to data collectors. The principal investigator supervised secondary data collection from the beneficiary registration book to ensure accuracy. The collected data was carefully reviewed to ensure completeness and consistency. Each questionnaire received a unique code for identification.
Data processing and statistical analysis
Data entry was performed using EpiData 4.6 and checked for errors and missing values. Subsequently, the data was exported to Stata version 14.0 for further analysis. Descriptive statistics such as frequencies, percentages, and summary measures were done to describe the variables of interest.
In the study, the Life table method was utilized to estimate the probabilities of recovery. Both bivariate and multivariable Cox proportional-hazard regression models were done to identify predictors of the time to recovery. Independent variables with a p-value of less than 0.25 in the bivariate analysis were included in the final multivariate model. The results were reported as adjusted hazard ratios (AHR) with a 95% confidence interval, indicating the presence, strength, and direction of the association between the predictors and the time to recovery.
Results
Socio demographic characteristics of participants
The study included a sample of 567 children aged 6 to 59 months with moderate acute malnutrition from eight health posts in Fedis Woreda, Eastern Hararghe zone. The average age of the children in the program was 16.48 months, with a standard deviation of 18 months. Among the participants, 285 (50.3%) were male, and 432 (76.2%) resided in rural areas. The primary caregivers for the children were predominantly mothers, accounting for 95% of the cases (Table 1).
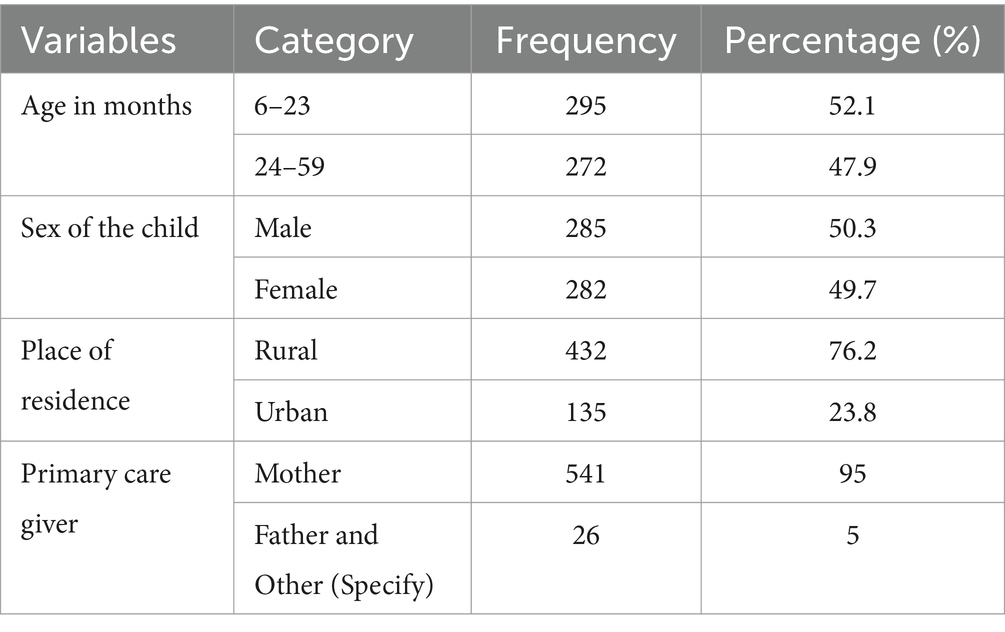
Table 1. Socio-demographic characteristics of children 6–59 months children in Fedis Woreda, east Hararghe, Ethiopia, 2022.
Family and health care related characteristics of study populations
Among the participants, 87.5% of them recovered from the program, while 12.5% did not. Also, 60% of participants were admitted with a MUAC measurement of 11.5–12.0 cm and 40% with 12.1–12.5 cm. Additionally, 93.6% used ready-to-use supplementary feeding, and 6.4% used Super Cereal Plus. 60% received vitamin A supplementation and 40% did not; 87.8% were new admissions and 12.2% were re-admissions; 77.1% traveled over 60 min to the distribution center; and 22.9% traveled less than 60 min. Further, 90.7% of caregivers received health and nutritional education, while 9.3% did not. Among the children, 9% had diarrhea, with 90.7% experiencing watery diarrhea and 8% experiencing bloody diarrhea (Table 2).
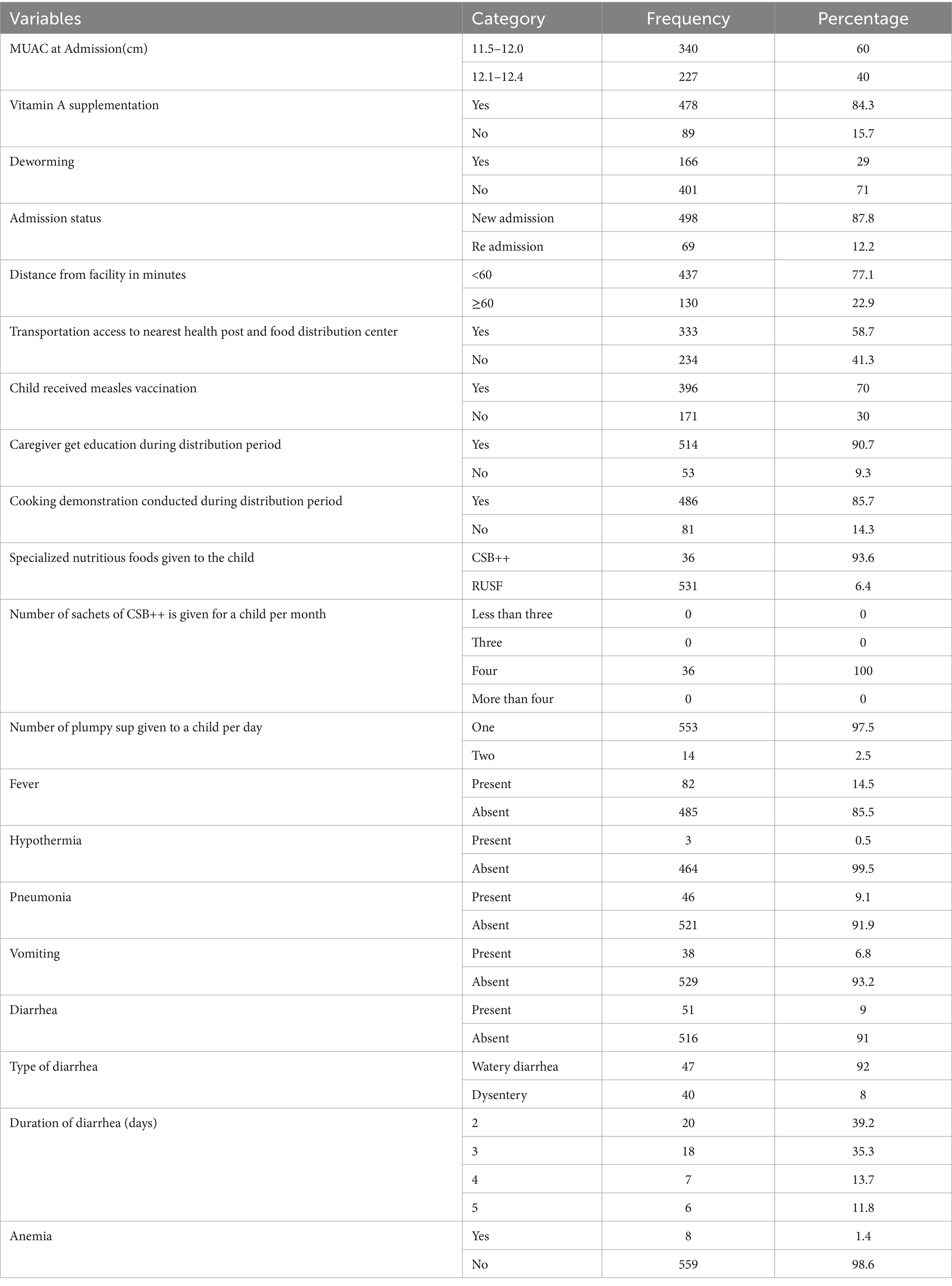
Table 2. Family and healthcare related characteristics of study population of time to recovery from moderate acute malnutrition among 6–59 months children in Fedis Woreda, east Hararghe, Ethiopia, 2022.
Time to recovery from moderate acute malnutrition among 6–59 months children
In a study involving 567 children with moderate acute malnutrition (MAM) enrolled in targeted supplementary feeding, 87.5% (496) of the children successfully recovered within a median time of 16 weeks (interquartile range: 5.4). However, 12.5% (71) did not recover. The study found that male children had a shorter median recovery time (15 weeks, interquartile range: 6) compared to female children (17 weeks, interquartile range: 7). Furthermore, the analysis revealed that children aged 24–59 months were 1.30 times more likely to recover from MAM within 16 weeks (adjusted hazard ratio: 1.30, 95% CI: 1.11–1.56) compared to those aged 6–23 months. Additionally, female children with MAM had an 8% lower likelihood of recovery within 16 weeks compared to male MAM children (Table 3).
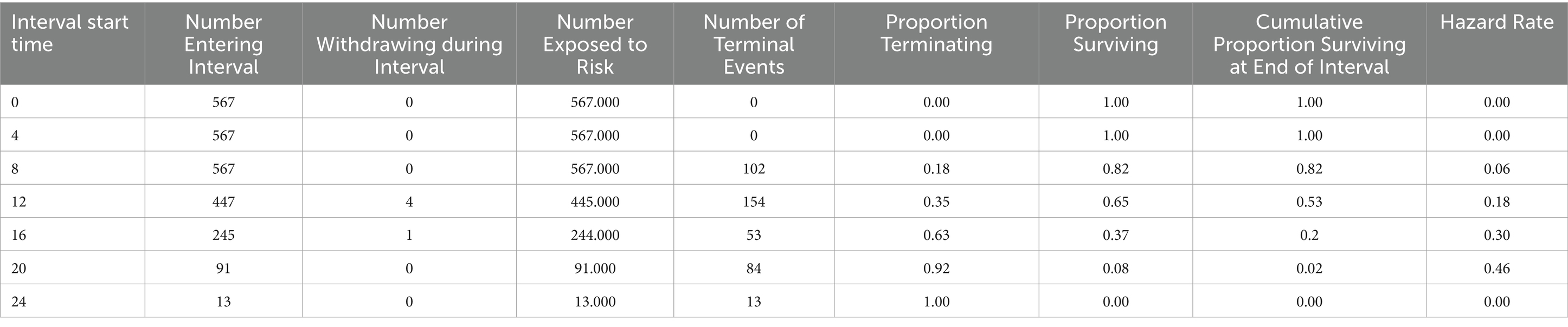
Table 3. Life table of time to recovery of MAM children at different week among 6–59 months children in Fedis Woreda, east Hararghe, Ethiopia, 2022.
Predictors of time to recovery
This study examined several factors associated with the time to recovery of moderate acute malnutrition (MAM) treatment. The bivariate analysis revealed significant associations between the primary child care responsibility, admission MUAC, Vitamin A supplementation, admission status, transport access to the nearest TSFP distribution center, measles vaccination, types of treatment food, and co-morbidities such as fever and diarrhea, with the dependent variable (time to recovery) at a p-value of less than 0.25 (Table 4). Furthermore, the multivariate Cox regression analysis identified admission MUAC, transport access to the nearest health facility, types of specialized food, and diarrhea as significant predictors of the time to recovery in MAM treatment, with a p-value of less than 0.05 (Table 5).
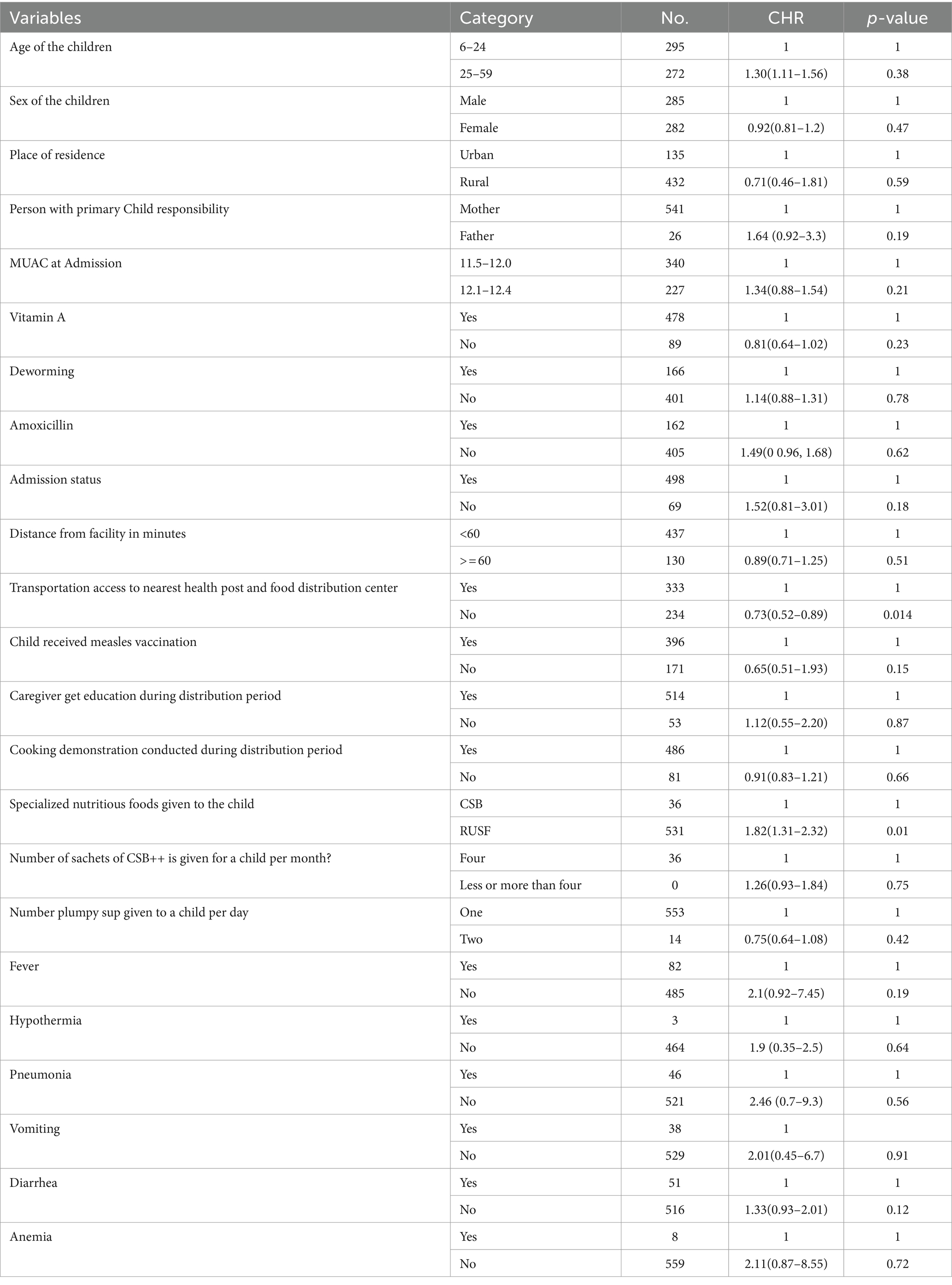
Table 4. Bivariate cox-regression of predictors of time to recovery from moderate acute malnutrition among 6–59 months children in Fedis Woreda, east Hararghe, Ethiopia, 2022.
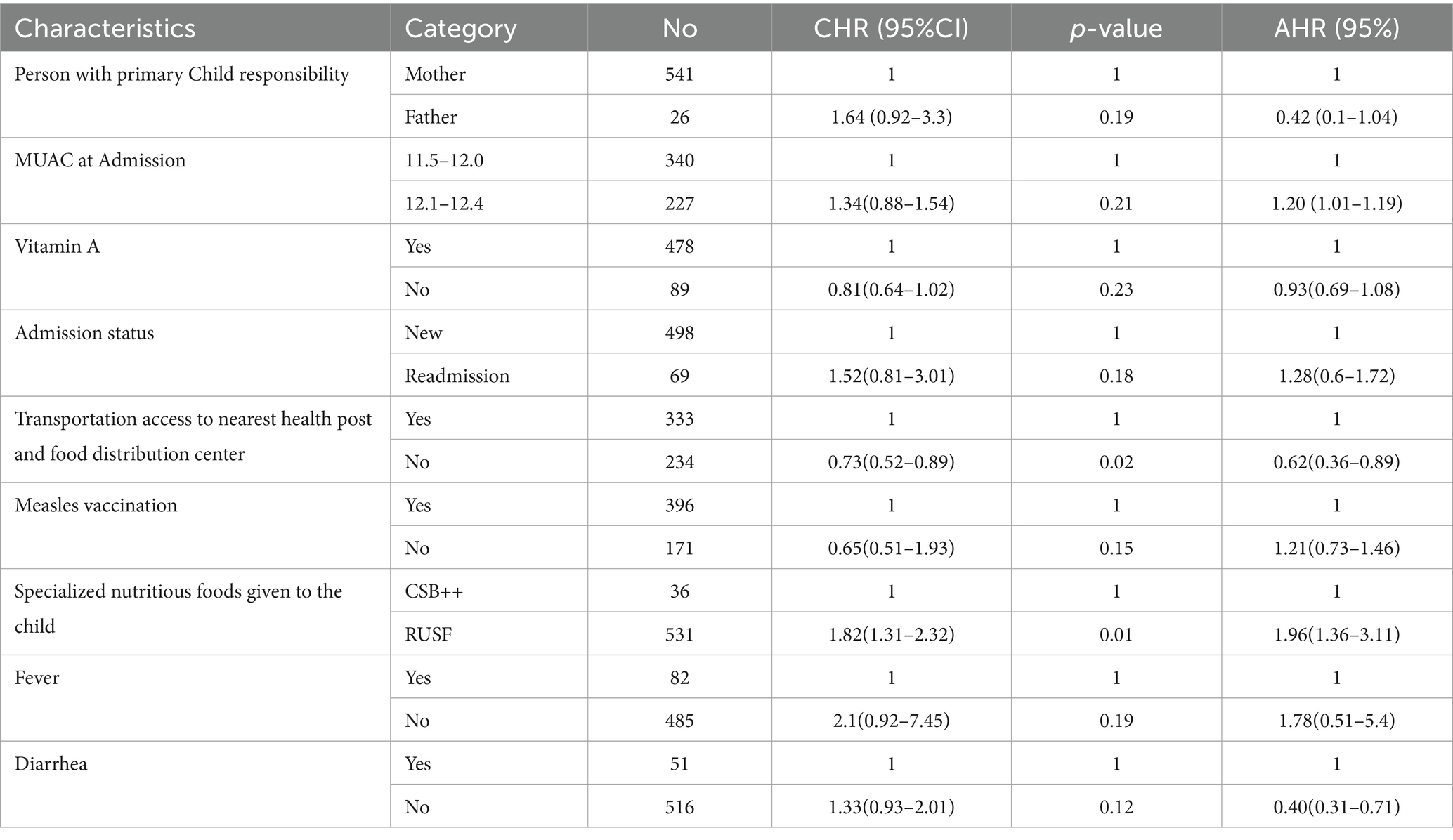
Table 5. Multivariable cox-regression analysis for predictors to time to recovery from MAM among 6–59 months of children in Fedis Woreda, east Hararghe, Ethiopia, 2022.
The study conducted a multivariable Cox-regression analysis to identify predictors of the time to recovery for children with moderate acute malnutrition (MAM) enrolled in the Fedis Woreda targeted supplementary feeding program (Table 5). After controlling for confounding variables, the analysis yielded significant findings. Firstly, children admitted with a mid-upper arm circumference (MUAC) measurement of 12.1–12.4 centimeters had a 1.02 times higher likelihood of early recovery compared to those with MUAC between 11.5 and 12.0 centimeters. Secondly, families without access to transportation had a 38% lower likelihood of recovery compared to those with transportation access. Additionally, children who received ready-to-use supplementary feeding were 1.96 times more likely to recover within 16 weeks compared to those who received super cereal plus. Lastly, children with diarrhea had a 69% lower likelihood of recovery within 16 weeks compared to those without diarrhea. These findings emphasize the importance of factors such as MUAC at admission, transportation access, type of supplementary feeding, and the presence of diarrhea in influencing the time to recovery for children with MAM.
Discussion
The study assessed the time to recovery from MAM and its predictors among children aged 6–59 months treated at a targeted supplementary feeding program at Fedis Woreda. The study found that the median time to recovery for children with moderate acute malnutrition (MAM) was 16 weeks. This duration aligns with the national standard malnutrition guidelines in Ethiopia, which also recommend a 16-week time frame (15). A similar study conducted in Darolebu reported a median recovery time of 16 weeks as well (27). However, in a study conducted in Shalla District, the median time to recovery was slightly lower at 15 weeks with an interquartile range (IQR) of 5 weeks (28). These comparisons provide a context for the recovery time observed in the current study, highlighting its consistency with national guidelines and other studies conducted in the region.
The study demonstrated an impressive overall recovery rate of 87.5%, surpassing the acceptable threshold set by the Sphere International Standard, which establishes a minimum recovery rate of 75% (29). This noteworthy achievement may be attributed to the regular follow-up provided by non-governmental organizations involved in the program as well as the continuous health education support delivered by health extension service workers at the local level. These factors likely played a crucial role in promoting successful recovery among the children with moderate acute malnutrition in the study.
The study findings revealed that children admitted with a mid-upper arm circumference (MUAC) measurement of 12.1–12.4 had a 1.02 times higher likelihood of early recovery within 16 weeks compared to children with MUAC between 11.5–11.9 (AHR = 1.02; 95% CI: 1.01–1.19). This observation aligns with previous studies conducted by James et al. and Kumsa and Silassie (18, 28). These studies collectively indicate that early screening for moderate acute malnutrition in children, coupled with the provision of supplementary feeding, leads to improved outcomes. Furthermore, the study found that children with the highest MUAC measurement at enrolment had a significantly reduced risk of remaining with moderate acute malnutrition and a higher chance of recovering. This highlights the importance of early detection and intervention in achieving better outcomes for children with moderate-acute malnutrition.
The study findings highlighted the significant impact of transport access to the nearest health facility providing targeted supplementary feeding services on the time to recovery. It was observed that families without transport access had a 38% lower proportion of children recovering from moderate acute malnutrition (MAM) compared to those with transportation access (AHR 0.62, 95% CI 0.36–0.89). This result is consistent with a study conducted in Ethiopia by Shanka et al. (30). The findings suggest that children who have access to transportation are more likely to receive timely and accessible services, leading to a better prognosis and improved recovery from MAM.
This study found that children who received ready-to-use supplementary food (RUSF) had a significantly higher likelihood of timely recovery from moderate acute malnutrition (MAM) within 16 weeks compared to those who received a corn-soy blend with oil (CSB++). The findings are consistent with studies conducted in Sidama Zone (31), Shala District (28), and Daro Labu District in Ethiopia, as well as in Malawi (32). These studies consistently demonstrate that children treated with RUSF had better recovery outcomes compared to those treated with CSB++. The sharing of CSB++ with other household members and the irregularity in daily cooking and cooking time were potential factors contributing to the lower recovery rates associated with CSB++. The absence of cooking demonstrations by governmental and non-governmental organizations at health posts may have contributed to a lack of awareness at the community level. Similarly, another study conducted in Jimma, Ethiopia, showed that MAM children treated with CSB+ and oil under the targeted supplementary feeding program (TSFP) had a lower rate of timely recovery compared to children treated with super cereals. Overall, the findings indicate that treating MAM children with ready-to-use supplementary food (RUSF) is more effective than using CSB++.
The study found that the presence of diarrhea in children with moderate acute malnutrition (MAM) admitted to the targeted supplementary feeding program (TSFP) had a significant impact on recovery outcomes. Children who had diarrhea were 69% less likely to recover within the 16-week timeframe compared to those who did not have diarrhea. This suggests that the presence of diarrhea acts as a barrier to timely recovery from MAM. By recognizing the association between diarrhea and delayed recovery in MAM children, healthcare providers can prioritize comprehensive care that targets both the nutritional needs and gastrointestinal health of these children.
This study is not without its own limitations. The study used the recorded data of the discharged children to determine the time-to-recovery from moderate acute malnutrition and identify its predictors among children aged 6–59 months who were admitted to the targeted supplementary feeding program in Fedis Woreda. As a result, this study was restricted to using medical records to determine time to recovery because it was not possible to include additional factors such as parental education and economic position, a history of breastfeeding, and other aspects. Another limitation of this study is the completeness of the health posts’ records. Additionally, factors like the wealth index, one of the determinants of malnutrition, are not evaluated.
Conclusion and recommendations
In general, this study emphasizes the significance of early screening, access to transportation, appropriate supplementary foods, and effective management of diarrhea in determining the recovery outcomes of children with moderate acute malnutrition (MAM) within targeted supplementary feeding programs (TSFPs). Early detection and timely intervention, along with transportation access, play crucial roles in promoting timely recovery. The use of ready-to-use supplementary foods (RUSF) is associated with higher chances of recovery compared to corn-soy blends with oil (CSB++). However, the presence of diarrhea poses a significant barrier to recovery. By addressing these factors comprehensively, stakeholders can enhance recovery outcomes and reduce the burden of MAM in children.
The health extension workers should create public awareness and give health education on signs and symptoms of malnutrition that enhance early identification of the case and timely use of routine treatments. Early detection of co-morbidities like diarrhea is expected to reduce moderate acute malnutrition. Additionally, the woreda health office should work on expanding health facilities, building infrastructure like an all-season dry road, and supplying RUSF that will help the beneficiaries. Also, non-governmental organizations should provide technical and logistic support to health facilities working on TSFP for effective implementation and capacitate the health extension workers and health workers working on managing MAM, and they should ensure an adequate supply of RUSF and monitor its distribution to ensure proper utilization. Furthermore, the researcher should further examine how engagement with the community and caregivers through the implementation of nutrition education activities, counseling, and home visits contributes to successful program delivery and the improvement of intervention outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Haramaya University’s Institutional Health Research Ethics Review Committee, with reference number C|AC|p1|D|a1|3,123|22. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
BM: Formal analysis, Methodology, Writing – original draft, Writing – review & editing. BG: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. BN: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. MK: Conceptualization, Methodology, Supervision, Writing – original draft, Writing – review & editing. OK: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. JD: Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. RK: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. DF: Conceptualization, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We extend our gratitude and appreciation to the management and staff of the Fedis Health Bureau and the health posts for their valuable support and cooperation throughout the data collection process. Their assistance was instrumental in the successful implementation of the study and the acquisition of the necessary data.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hayashi, C, Krasevec, J, Kumapley, R, Mehra, Deonis M, and Borghi, E, editors. Levels and trends in child malnutrition. UNICEF/WHO/ World Bank Group joint child malnutrition estimates: key findings of the 2017 edition. New York: UNICEF, WHO, World Bank Group (2017).
2. Hobbs, BK, and Bush, A, editors. Acute malnutrition: an everyday emergency: A 10-point plan for tackling acute malnutrition in under-fives. SAGE Open Medicine (2014).
3. Sylvie Chamois, MG, and Grellety, Y. (2007). Ethiopia Protocol for the management of Severe Acute Malnutrition. 2007 01/03/2007 00:00:00 [cited Ethiopia; (0):[0 p.]. Available at: https://www.ennonline.net/samprotocolethiopia.
4. Grellety, E, and Golden, MH. Severely malnourished children with a low weight-for-height have a higher mortality than those with a low mid-upper-arm-circumference: I. Empirical data demonstrates Simpson's paradox. Nutr J. (2018) 17:1–21. doi: 10.1186/s12937-018-0384-4
5. Susan Thurstans, PT, Velly, Devrig, and Middleton, W. (2011). 2011 Edition of the Sphere Handbook Humanitarian Charter and Minimum Standards in Humanitarian Response. 01/08/2011 00:00:00 [cited n/a; (41):[36 p.]. Available at: https://www.ennonline.net/fex/41/edition.
6. Prost, A, Nair, N, Copas, A, Pradhan, H, Saville, N, Tripathy, P, et al. Mortality and recovery following moderate and severe acute malnutrition in children aged 6-18 months in rural Jharkhand and Odisha, eastern India: a cohort study. PLoS Med. (2019) 16:e1002934. doi: 10.1371/journal.pmed.1002934
7. Black, RE, Victora, CG, Walker, SP, Bhutta, ZA, Christian, P, de Onis, M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (London, England). (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
8. Berry, L, Dawes, A, and Biersteker, L, editors. Getting the basics right: an essential package of services and support for ECD. Essential services for young children (2013).
9. Fabiansen, C, Phelan, KP, Cichon, B, Ritz, C, Briend, A, Michaelsen, KF, et al. Short children with a low midupper arm circumference respond to food supplementation: an observational study from Burkina Faso. Am J Clin Nutr. (2016) 103:415–21. doi: 10.3945/ajcn.115.124644
10. Richard, SA, Black, RE, Gilman, RH, Guerrant, RL, Kang, G, Lanata, CF, et al. Diarrhea in early childhood: short-term association with weight and long-term association with length. Am J Epidemiol. (2013) 178:1129–38. doi: 10.1093/aje/kwt094
11. Lagrone, L, Cole, SM, Schondelmeyer, AC, Maleta, KM, and Manary, MJ. Locally produced ready-to-use supplementary food is an effective treatment of moderate acute malnutrition in an operational setting. Ann Trop Paediatr. (2010) 30:103–8. doi: 10.1179/146532810X12703901870651
12. Ayana, AB, Hailemariam, TW, and Melke, ASJBN. Determinants of acute malnutrition among children aged 6–59 months in public hospitals, Oromia region, West Ethiopia: a case–control study. Ann Trop Paediatr. (2015) 1:1–11. doi: 10.1186/s40795-015-0031-9
13. Teshome Bekele, WJC . Predictors of community-based health Insurance in Ethiopia via multilevel mixed-effects modelling: evidence from the 2019 Ethiopia Mini demography and health survey. Clinico Econ Outcomes Res. (2022) 14:547–62. doi: 10.2147/CEOR.S368925
14. Govender, I, Rangiah, S, Kaswa, R, and Nzaumvila, D. Malnutrition in children under the age of 5 years in a primary health care setting. South African family practice: Official J South African Acad Family Practice/Primary Care. (2021) 63:e1–6. doi: 10.4102/safp.v63i1.5337
15. Reginald Annan, PW, and Brown, R. Management of Moderate Acute Malnutrition (MAM): current knowledge and practice. (2014) 06/01/2015 00:00:00; (0):[0 p.]. Available at: https://www.ennonline.net/managementofmamcurrentknowledgeandpractice.
16. Ahmed, KY, Abrha, S, Page, A, Arora, A, Shiferaw, S, Tadese, F, et al. Trends and determinants of underweight and overweight/obesity among urban Ethiopian women from 2000 to 2016. BMC Public Health. (2020) 20:1276. doi: 10.1186/s12889-020-09345-6
17. Zegeye, B, Shibre, G, Idriss-Wheeler, D, and Yaya, S. Trends in inequalities in childhood stunting in Ethiopia from 2000 to 2016: a cross sectional study. J Public Health (Oxf). (2021) 43:655–63. doi: 10.1093/pubmed/fdaa051
18. James, P, Sadler, K, Wondafrash, M, Argaw, A, Luo, H, Geleta, B, et al. Children with moderate acute malnutrition with no access to supplementary feeding Programmes experience high rates of deterioration and no improvement: results from a prospective cohort study in rural Ethiopia. PLoS One. (2016) 11:e0153530. doi: 10.1371/journal.pone.0153530
19. Schmidt, E, and Dorosh, P, editors. A sub-national hunger index for Ethiopia: Assessing progress in region-level outcomes. International Food Policy Research Institute (IFPRI). (2009).
20. Mengesha, MM, Deyessa, N, Tegegne, BS, and Dessie, Y. Treatment outcome and factors affecting time to recovery in children with severe acute malnutrition treated at outpatient therapeutic care program. Glob Health Action. (2016) 9:30704. doi: 10.3402/gha.v9.30704
21. Teshome, G, Bosha, T, and Gebremedhin, S. Time-to-recovery from severe acute malnutrition in children 6–59 months of age enrolled in the outpatient treatment program in Shebedino, southern Ethiopia: a prospective cohort study. BMC Pediatr. (2019) 19:33. doi: 10.1186/s12887-019-1407-9
22. Tekeste, A, Wondafrash, M, Azene, G, and Deribe, K. Cost effectiveness of community-based and in-patient therapeutic feeding programs to treat severe acute malnutrition in Ethiopia. Cost effectiveness and resource allocation: C/E. (2012) 10:4. doi: 10.1186/1478-7547-10-4
23. Wondim, A, Tigabu, B, and Kelkay, MM. Time to recovery from severe acute malnutrition and its predictors among admitted children aged 6-59 months at the therapeutic feeding Center of Pawi General Hospital, Northwest Ethiopia: a retrospective follow-up study. Int J Pediatr. (2020) 2020:1–9. doi: 10.1155/2020/8406597
24. Wegner, CW, Loechl, C, and Mokhtar, N. Moderate acute malnutrition: uncovering the known and unknown for more effective prevention and treatment. Food Nutr Bull. (2015) 36:S3–8. doi: 10.1177/15648265150361S101
25. Wa, A, Jara, D, Alemayehu, M, and Burrowes, S. Risk factors associated with poor health outcomes for children under the age of 5 with moderate acute malnutrition in rural fagita lekoma district, Awi zone, Amhara, Ethiopia, 2016. BMC Nutrition. (2017) 3:88. doi: 10.1186/s40795-017-0208-5
26. Sadeta, K . Time to recovery from moderate acute malnutrition and its predictors among 6-59 months children targeted for supplementary feeding in Shalla District, west Arsi zone, Ethiopia, vol. 2018. Europe PMC plus (2019).
27. Rashid, MY, Kebira, JY, Oljira, L, and Dheresa, M. Time to recovery from moderate acute malnutrition and its predictors among children 6–59 months of age enrolled in targeted supplementary feeding program in Darolebu District, eastern Ethiopia: a retrospective cohort study. Front Public Health. (2022) 10:10. doi: 10.3389/fpubh.2022.914837
28. Kumsa, K, and Silassie, W. Time to recovery from moderate acute malnutrition and its predictors among 6–59 months children targeted for supplementary feeding in Shalla District, West Arsi Zone, Ethiopia, vol. 2018. Frontiers in Public Health (2019).
29. Ayalneh, AA, Fetene, DM, and Lee, T-J. Inequalities in health care utilization for common childhood illnesses in Ethiopia: evidence from the 2011 Ethiopian demographic and health survey. Front Public Health. (2017) 16:1–9. doi: 10.1186/s12939-017-0561-7
30. Shanka, NA, Lemma, S, and Abyu, DM. Therapy. Recovery rate and determinants in treatment of children with SevereAcute malnutrition using outpatient therapeutic feeding program inKamba district, south West Ethiopia. J Nutr Disord Ther. (2015) 5:1–9. doi: 10.4172/2161-0509.1000155
31. Karakochuk, C, van den Briel, T, Stephens, D, and Zlotkin, S. Treatment of moderate acute malnutrition with ready-to-use supplementary food results in higher overall recovery rates compared with a corn-soya blend in children in southern Ethiopia: an operations research trial. Am J Clin Nutr. (2012) 96:911–6. doi: 10.3945/ajcn.111.029744
32. LaGrone, LN, Trehan, I, Meuli, GJ, Wang, RJ, Thakwalakwa, C, Maleta, K, et al. A novel fortified blended flour, corn-soy blend "plus-plus," is not inferior to lipid-based ready-to-use supplementary foods for the treatment of moderate acute malnutrition in Malawian children. Am J Clin Nutr. (2012) 95:212–9. doi: 10.3945/ajcn.111.022525
Keywords: time to recovery, moderate acute malnutrition, targeted supplementary feeding program, East Hararghe, Eastern Ethiopia
Citation: Melaku B, Gebremichael B, Negash B, Kitessa M, Kassa O, Dereje J, Kefelegn R and Firdisa D (2024) Time to recovery from moderate acute malnutrition and its predictors among children aged 6–59 months in Fedis Woreda, East Hararghe Zone, Eastern Ethiopia. Front. Nutr. 11:1369419. doi: 10.3389/fnut.2024.1369419
Edited by:
Nirmal Kumar Mohakud, KIIT University, IndiaReviewed by:
Praveen Kumar, Lady Hardinge Medical College and Associated Hospitals, IndiaBarbara Sawicka, University of Life Sciences of Lublin, Poland
Copyright © 2024 Melaku, Gebremichael, Negash, Kitessa, Kassa, Dereje, Kefelegn and Firdisa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dawit Firdisa, ZmlyZGlzYWRhd2l0QGdtYWlsLmNvbQ==
†ORCID: Dawit Firdisa, http://orcid.org/0009-0000-2258-0550
 Berhanu Melaku1
Berhanu Melaku1 Berhe Gebremichael
Berhe Gebremichael Belay Negash
Belay Negash Obsan Kassa
Obsan Kassa Jerman Dereje
Jerman Dereje Dawit Firdisa
Dawit Firdisa