
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 05 July 2024
Sec. Nutritional Epidemiology
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1353086
 Sileshi Tilahun1
Sileshi Tilahun1 Kedir Teji Roba2
Kedir Teji Roba2 Hirbo Shore Roba2
Hirbo Shore Roba2 Jemal Ahmed Nure2
Jemal Ahmed Nure2 Teshome Sosengo3
Teshome Sosengo3 Behailu Hawulte Ayele2
Behailu Hawulte Ayele2 Melat B. Maruta4
Melat B. Maruta4 Adera Debella5
Adera Debella5 Addis Eyeberu5
Addis Eyeberu5 Ibsa Mussa2*†
Ibsa Mussa2*†Background: Globally, five million children under the age of five died in 2021. Asia and African countries contributed to 69% and 27.2% of wasting, respectively. In Ethiopia, out of 901 (10.1%) under-five children, 632 (8.1%) were found to be moderately wasted, and 269 (3.0%) were severely wasted. The purpose of this study was to assess the prevalence of wasting and its associated factors among children between the ages of 6 and 59 months in Habro Woreda, Oromia, Eastern Ethiopia.
Methods: A community-based cross-sectional study was conducted in Habro Woreda from 25 August to 20 September 2020. In total, 306 participants were included in this study through a systematic sampling technique. Data were collected using a pretested structured questionnaire through a face-to-face interview, entered into EpiData version 3.1, and analyzed using SPSS version 25. Predictors were assessed using a multivariate logistic regression analysis model and reported using an adjusted odds ratio (AOR) with a 95% confidence interval (CI). Statistical significance was set at p < 0.05.
Results: Overall, the prevalence of wasting among children aged 6–59 months in the Habro district was 28%, with a 95% confidence interval [26.5, 32.2%]. Factors such as mothers illiterate [AOR = 3.4; 95% CI: 1.14–10.47], households without latrines [AOR = 2.91; 95% CI: 1.33–6.37], food-insecure households [AOR = 4.11; 95% CI: 1.87–9], households that did not receive home visits [AOR = 4.2; 95% CI: 1.92–9.15], did not eat a variety of food [AOR = 7.44; 95% CI: 2.58–21.45], sick children after discharge from the program [AOR = 6.55; 95% CI: 2.85–15.02], readmitted children [AOR = 3.98; 95% CI: 1.43–15.07], and wasting 3.42 [AOR = 3.42; 95% CI: 1.24–9.45] were factors statistically associated with outcome variables.
Conclusion: This study noted that the prevalence of wasting among children aged 6–59 months following discharge from the Outpatient Therapeutic Program remains high. Educational status of the mother, availability of a latrine, separate kitchen in the household, household food insecurity, household dietary diversity, home visit, and admission type were significantly associated with wasting of children after discharge from the outpatient therapeutic program. Therefore, efforts that target these factors should be maximized to reduce the occurrence of wasting among children aged 6–59 months after discharge from the outpatient therapeutic program.
Many economically disadvantaged countries struggle with malnutrition as a serious public health issue (1). Malnutrition exists either in the form of undernutrition or overnutrition. Inadequate intake of carbohydrates, protein, vitamins, and mineral supply to the cells of the body to satisfy the physiological requirements are the immediate causes of undernutrition (2–4). In developing countries, poverty and high food costs are major causes of undernutrition (5). Malnutrition is classified into two types: acute (wasting) and chronic (6, 7).
Malnutrition results in over two million deaths of children under 5 years annually (8). Worldwide, socio-demographic, childcare, environmental health, and sanitation risk variables have a significant impact on the prevalence of wasting among children under 5 years (9–13). Evidence-based interventions (i.e., interventions targeting pathways of wasting in life cycles, including in-utero environment, the early period of infancy, and a focus on the process and identification of wasting rather than the state of being wasted) are recommended to overcome the problem of wasting (14, 15).
In 2022, an estimated 45 million children under five (6.8%) were affected by wasting; out of which, 13.6 million (2.1%) were severely wasted (16). More than three-quarters of all children with severe wasting live in Asia, and another 22% live in Africa (13). A study in Ethiopia found that out of 901 children (10.1%) under five 632 (8.1%) were moderately wasted, and 269 (3.0%) were severely wasted (17). According to the Ethiopia Mini-Demographic and Health Survey (EMDHS), 7.2% of children in Ethiopia were wasted (18). The survey indicated the regional variations in the percentage prevalence of wasting in under-five children: 21% in Somalia, 14% in Afar, 13% in Gambella, 2% in Addis Ababa, and 4% in Harari (18), 14.7% in Wolkite town (19), 13.4% in Bulehora district (20), 10% in Northwest Ethiopia (21), 11% in Adi-Harush and Hitsats Refugee Camps (22), and 7.2% in Wukro town (9) Tigray Region, 11.1% in Dilla town (10), and 28.2% in Hawassa Zuria district (11).
Despite the commitment of various stakeholders and the fact that the government of Ethiopia has already achieved remarkable progress in reducing under-five mortality in the last decades and designed multi-sectorial approaches to address malnutrition, the prevalence of wasting and factors influencing wasting in children aged between 6–59 months remain unabated in the study area (12, 23, 24). To the best of our knowledge, documentation of evidence regarding wasting at the country level and the study area is lacking. Therefore, this study aimed to assess the prevalence of wasting and associated factors among children aged between 6 and 59 months in Habro Woreda, Oromia, East Ethiopia.
A community-based cross-sectional study was conducted from 25 August to 20 September 2020, among children aged 6–59 months, 6 months after discharge from an outpatient therapeutic program in Habro Woreda, Oromia, Eastern Ethiopia. Habro Woreda is located about 320 km east of Addis Ababa, the capital city of Ethiopia. Habro Woreda has 1 general hospital, 7 type B functional health centers, and 32 functional health posts. In 2020, there were approximately 44,240 under-five children and 55,765 households in the region, with a total population size of 269,272. According to a projection by the Ethiopian Central Statistical Agency in 2011, the population was 190,455 (17). With a mostly rural population (88%), the area is characterized by a high population density (242/km2), fragmented farmland ownership, and limited income-generating opportunities. However, the major source of income was cash crops, mainly focused on chat cultivating and chat trading. We used the strengthening the reporting of observational studies in epidemiology (STROBE) cross-sectional checklist for this study (25).
All children aged 6–59 months who lived in the Habro district served as the study population. Mothers who had resided for at least 6 months in the study area and had a child aged 6–59 months were included. However, children with evidence of physical impairments, serious illness or mental impairments, children whose names differed from those present on the outpatient therapeutic program registration logbook, children who had left the selected study area, and mothers or caregivers who were unable to communicate were excluded from the study.
A questionnaire was developed after reviewing related studies in different literature, with some questions adopted from the related studies and contextualized to align with the study objectives and data extraction form accordingly. Data were collected using a pretested and structured interviewer-administered questionnaire to collect data on socio-demographic characteristics, environmental hygiene and sanitation characteristics, and childcare practice and health characteristics, which comprised the three survey components. The wording and sequence of questions were designed in such a way that the sequence of ideas (from general to specific and from easy to difficult questions) was maintained. Standard anthropometric measurements were taken from all subjects during data collection. We use the Waterlow height-for-age (%) method of classification (26). Length was measured for children who were < 87 cm or those too weak to stand in supine (lying down). However, if the children were more than 87 cm in height, their height was recorded using a stadiometer to the nearest 1 cm. To ensure the quality of data, seven skilled health professionals who had completed BSc Nursing and one supervisor who was proficient in both Afaan Oromo and Amharic collected the data, and the task was closely supervised by the investigators. Data collectors and supervisors received 4 days of training in the data-gathering processes. Initially, we translated the questions while keeping the purpose of the questionnaire and the intent of the questions in mind. It was translated by group members who were bilingual experts. To ensure the accuracy of the translation, the questionnaire was translated back into English by someone who had not seen the original version and was unfamiliar with the questionnaire's context. The back-translated version was then compared with the original, and any differences in meaning were corrected. Then, to ensure cross-validity, we attempted to interview a set of respondents in English and another set in the local language, such as Afaan Oromo and Amharic; their responses were then compared to identify differences in understanding. Finally, pretesting was conducted to identify questions that were poorly understood, ambiguous, or elicited hostile or other undesirable responses. We attempted to conduct a pretest using the already translated questionnaire. We tried to implement all the steps in pretesting, such as obtaining an evaluation of a questionnaire and testing the revised questionnaire through its paces with friends and colleagues. We statistically calculated Cronbach's alpha, which is a measure used to assess the quality of the instruments we used. The outcome was 0.87, which was within acceptable ranges.
Wasting (Yes/No).
Socio-demographic variables: Child age, child sex, maternal educational status, maternal occupation, family size, religion, ethnicity, and household food security.
Environmental health-related variables: Availability of latrine, hand washing practice, solid waste disposal, and availability of liquid waste disposal pit.
Child caring practice and health characteristics: Exclusive breastfeeding, dietary diversity score, meal frequency, vaccination status, history of diarrhea in the past 2 weeks, ever used family planning, and place of delivery.
Wasting: Wasting is defined as the child's weight-for-height Z-score (WHZ) < -2 SD from the median WHO reference values; WHZ ≥-3SD and < -2SD indicates moderate wasting; and WHZ < -3SD indicates severe wasting (19, 27).
Undernutrition: A mid-upper arm circumference (MUAC) below 12.5 cm indicates acute undernutrition; MUAC ≥ 11.5 cm and < 12.5 cm indicates moderate acute undernutrition; and MUAC < 11.5 cm indicates severe acute undernutrition (19, 27).
Household food security: It is measured by whether the respondent worries that the household is lacking enough food for the past 4 weeks (4, 19).
Food secure: If the respondent does not worry about the household lacking enough food for the past few weeks (4, 19).
Food insecurity: The lack of regular access to enough safe and nutritious food for normal growth and development and active and healthy life. This may be due to the unavailability of food and/or a lack of resources to obtain food (4, 19, 28).
Mildly food insecure: It is when a respondent rarely worries about food (once or twice in the past 4 weeks) (4, 19, 28).
Moderately food insecure: It is when a respondent sometimes worries about food (3 to 10 times in the past 4 weeks) (4, 19, 28).
Severely food insecure: It is when a respondent often worries about food (more than 10 times in the past 4 weeks) (4, 19, 28).
Household dietary diversity: Food intake that includes all of the diversified dietary needs of the organism in the correct proportion (29).
Diarrhea: It is defined as having three or more loose, watery stools in 24 h in the 2 weeks before the survey (30).
Improved drinking water: Drinking water that is obtained from piped water into dwellings, public taps, protected dug wells, protected springs, and rainwater (29).
Wasting: A nutritional deficiency condition of recent onset related to sudden food deprivation or malabsorption of nutrients, resulting in weight loss and weight-for-height below −2 SD, but resolved upon treatment (31).
Moderate wasting: Weight-for-height below −2 Z-score of children under 5 years of age (32).
Severe wasting: Weight-for-height or length < -3 Z-score of children under 5 years of age (31).
There were a number of biases involved while conducting this research, and the researcher took explicit measures to avoid them. One of the biases was social desirability and recall bias, and to avoid it, the researcher paraphrased the questions in a way that was not socially desirable and made an attempt to provide a clue for the intended question that needed to be answered.
The sample size was determined by using the single population proportion formula, considering the following assumptions:
where n = minimum sample size required for the study, Z = standard normal distribution (Z = 1.96), with a confidence interval of 95% and α= 0.05, p = proportion of wasting taken from proportion of wasting taken from the Ethiopian Demographic Health Survey, which is 10% (33), d = maximum acceptable margin of sampling error (d) = 5% = 0.05, and design effect = 1.5. Therefore, the final total sample size, including the contingency (10%) of the non-response rate, was 188. The sample size for the second objective (factors) was also determined by using the double population proportion formula for a cross-sectional study by considering the following assumptions: power = 80%, CI = 95%, and ratio = 1:1. The largest sample size from those samples was taken and the final sample size was calculated to be 306 children paired with their mothers or caregivers.
In this study, a three-stage sampling strategy was followed. In the first stage, four health centers and three health posts were randomly selected and included. The number of study units to be sampled from each health facility was determined using proportional allocation to size based on the number of client flows in the current year (2019), ensuring equal weighting despite varying numbers of health centers and posts (34). Children aged 6–59 months who had recovered from the OTP program (November 2019–February 2020) were recruited from the OTP registration logbook. Then, the systematic random sampling method was employed to select each study subject. The sampling fraction of the Kth interval was calculated as (N/n = 640/306 = 2.1~.2). Based on the client's registration logbook number, the starting participant was determined by using the lottery method, and every second discharged child was included until the required sample was achieved (33). The eligible participants who did not make themselves available during the data collection period in the selected Kebele were revisited up to three times, and if they did not make themselves available after three visits, the data collector skipped that household and interviewed the next household as a substitute. Finally, a total of 306 study samples were selected using a systematic sampling procedure. Then, each patient was given a unique code.
A multilingual specialist (Afaan Oromo and Amharic) created the questionnaire first in English and then translated it into the local languages. To maintain uniformity, it was then translated back into English. Data collectors and supervisor were trained on how to use the data-gathering instrument and processes. A pretest was conducted with 5% of the research participants under comparable conditions prior to the real data collection. Regular supervision was provided by investigators and competent research supervisors.
First, the obtained data were reviewed for completeness and consistency. They were then cleaned, coded, and entered into EpiData version 3.1 for further analysis. The entered data was transferred to SPSS version 25 for analysis. Descriptive and summary statistics were collected and reported using frequency tables and figures. A binary logistic regression model was constructed to test for a connection between independent factors and the outcome variable. Hosmer–Lemeshow statistics and Omnibus tests were used to evaluate the model's fitness. To determine the genuine determinants of the outcome variables, a multivariable analysis was performed. Using the standard error and co-linearity statistics, a multi-collinearity test was performed to assess for the presence of correlation between independent variables, and no collinearity effects were observed. As a result, the variance inflation factor (VIF) was 0.951. The odds ratio (OR) and 95% confidence interval (CI) were used to determine the direction and degree of the statistical connection. In all bivariable and multivariable analyses, a p-value of 0.05 was considered statistically significant.
In this study, a total of 306 children aged 6–59 months were included. Out of the total study participants, 156 (51%) were boys, and the mean age of the study children and their mothers was 30 (SD+6.5) months and 29.4 (SD+10.8) years, respectively. Regarding religion, most of the caregivers 278 (90.8%) were Muslim. Of the participants, 138 (45.1%) mothers and caregivers of children belong to an age group of 21–29 years. With regard to educational status, most of the mothers or caregivers 217 (70.9%) were illiterate. The majority 288 (94.1) of the caregivers were housewives (Table 1).

Table 1. Socio-demographic characteristics associated with children aged 6–59 months in Habro Woreda, East Ethiopia 2020 (n = 306).
Among the total households, 195 (63.7%) had a latrine, and of those households that had a latrine, only 19 (9.7%) of them had a handwashing facility. A total of 215 (70.3%) households had access to improved sources of drinking water, 209 (68.3%) households lacked proper waste disposal facilities, and 39 (12.7%) households had no separate kitchens (Table 2).
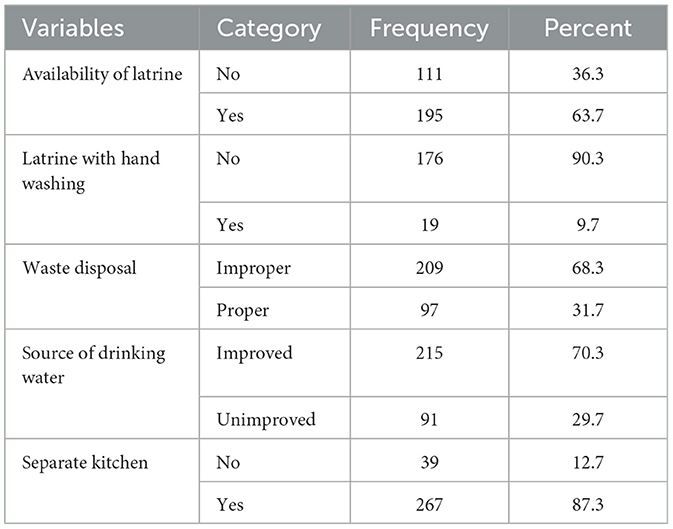
Table 2. Environmental- and sanitation-related associated with children aged 6–59 months after 6 months following discharge from OTP in Habro Woreda, East Ethiopia 2020 (n = 306).
Among the children, 134 (28.4%) had a history of illness, and of these, 56 (64.4%), 21 (24.1%), and 10 (11.5%) had diarrhea, pneumonia, and fever, respectively. Among those children with diarrhea, about 9 (2.9%) did not get oral rehydration solution (ORS) or zinc. Furthermore, about 126 (41.2%) of children did not take vitamin A supplementation within the last 6 months after being discharged from OTP. In their lifetime, 123 (40.2%) of the children had not received the measles vaccine (Table 3).
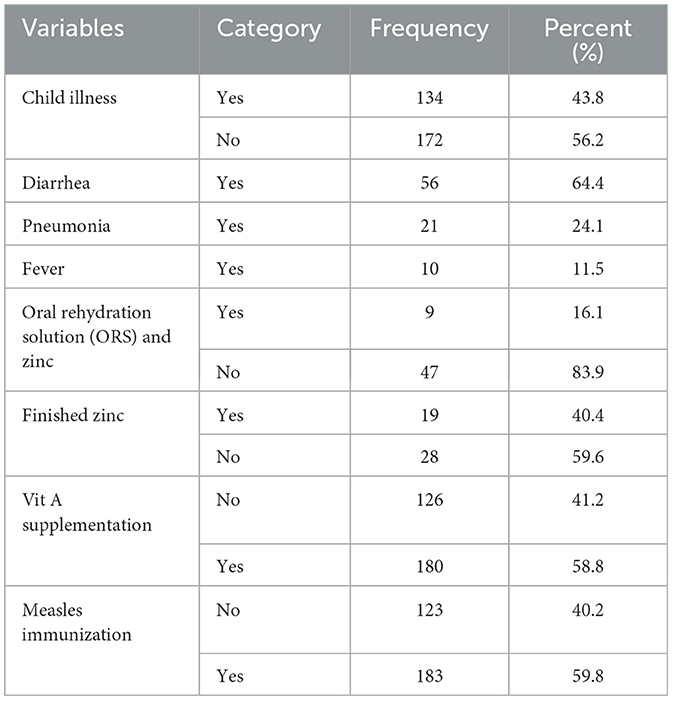
Table 3. Treatment outcomes of children aged 6–59 months after 6 months following discharge from OTP in Habro Woreda, East Ethiopia 2020 (n = 306).
Of the total respondents, 257 (84.0%) of the study participants' household family members chewed khat, with 215 (83.7%) of them chewed khat daily. Of the total households, 212 (69.3%) of children's family members smoked cigarettes, and among these, 82 (59.6%) were heavy smokers (Table 4).
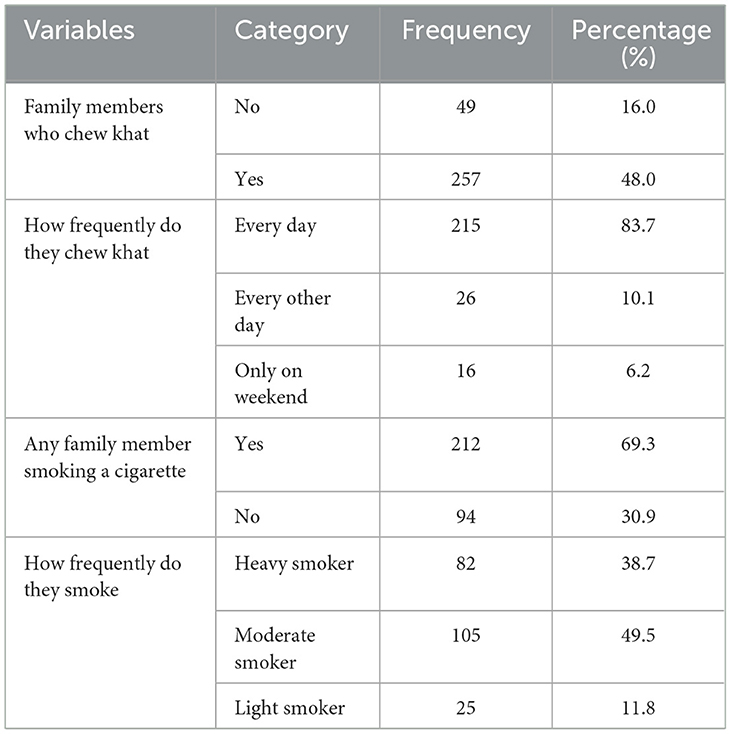
Table 4. Substance abuse among family members of the children aged 6–59 months after 6 months of discharge from OTP in Habro Woreda, East Ethiopia 2020 (n = 306).
According to this study, 92.2% of children consumed foods made from grains, roots, and tuber products; 54.6% consumed foods rich in vitamin A-rich fruits and vegetables; 53.9% consumed foods made from pulses, legumes, and nuts; 35.3% consumed other fruits and vegetables; and 28.8% consumed milk and dairy products (Figure 1).
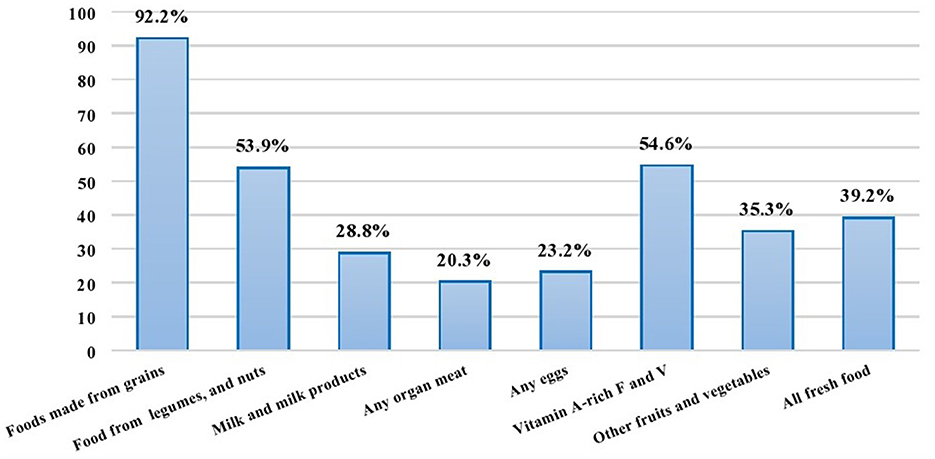
Figure 1. Food groups consumed by children aged 6–59 months in Habro Woreda, Eastern Ethiopia, 2020 (n = 306).
According to the household food insecurity access scale, 138 households (45.1%) were food insecure, whereas 168 households (54.9%) were food secure. Nearly 63 (45.7%) reported concern about not having enough food to eat in the household, and 75 (54.3%) reported that household members went to bed hungry (Figure 2).
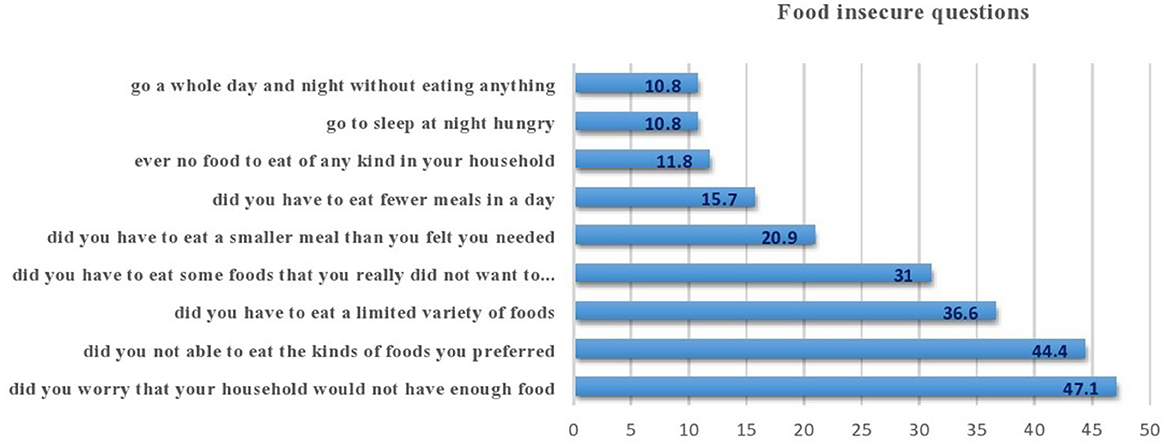
Figure 2. Status of food insecurity among children aged 6–59 months in Habro Woreda, Eastern Ethiopia, 2020 (n = 306).
The prevalence of wasting among children aged 6–59 months following exit from the outpatient therapeutic program within the last 11 months was 28.0%. At admission, 272 (88.9%) of the children were newly admitted to OPT. Out of them, 183 (59.8%) children did not receive a home visit or follow-up by health workers within the last 11 months following exit from an outpatient program (Table 5).
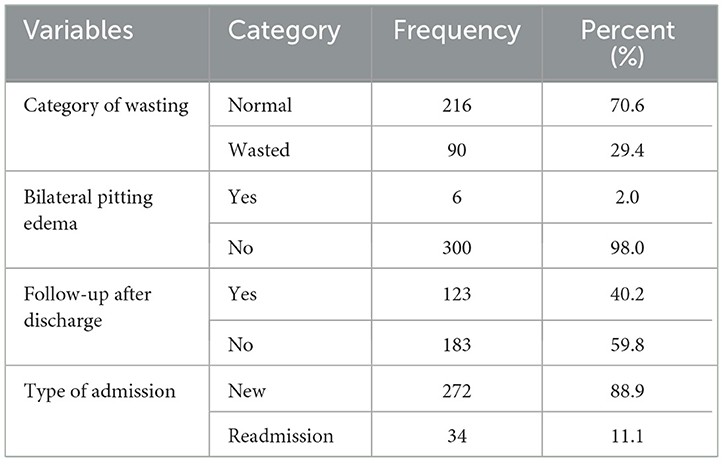
Table 5. Anthropometric status of children aged 6–59 months after 6 months following exit from OTP in Habro Woreda, East Ethiopia 2020 (n = 306).
The prevalence of wasting among children aged 6–59 months following exit from the outpatient therapeutic program within the last 11 months was 28.0% (95% CI: 26.5–32.2%). Of these, 7.7% was severely wasted and 20.3% was moderately wasted (Figure 3).
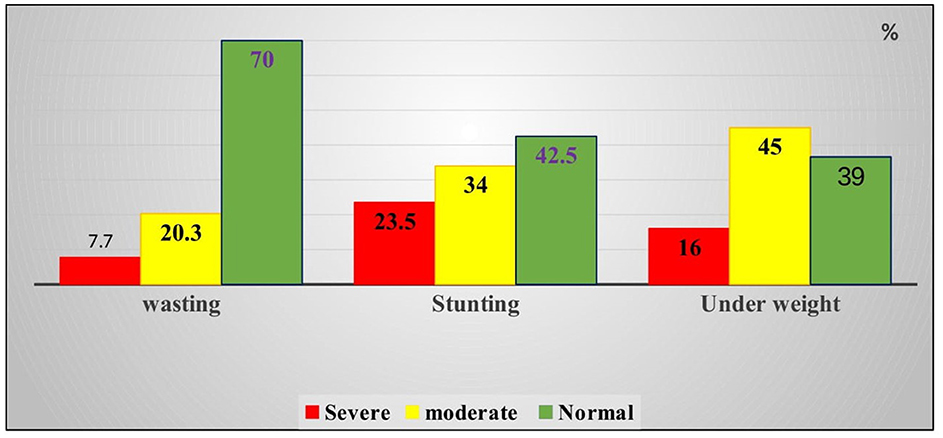
Figure 3. Percentage of wasting, stunting, and underweight among children aged 6–59 months in Habro Woreda, East Ethiopia, 2020 (n = 300 for wasting and underweight, n = 306 for stunting).
First, bivariate analysis was conducted, and variables with a p-value of < 0.25 were included in multivariate analysis. In the multivariate analysis, variables with a p-value of < 0.05 were declared statistically significant predictors of wasting. Variables such as the gender of the household head, educational status of the mother, availability of latrine, source of drinking water, separate kitchen, smoking, household food insecurity, household dietary diversity, home visit, child illness, vitamin A supply for the last 6 months, and admission type were significantly associated with child wasting in the bivariate binary logistic regression. However, in the multivariable logistic regression, factors such as the educational status of the mother, availability of a latrine, separate kitchen, household food insecurity, household dietary diversity, home visit, and admission type were significantly associated with wasting.
Accordingly, children born to mothers who were illiterate were 3.4 [AOR = 3.4; 95% CI: 1.14–10.47] times more likely to be wasted as compared to those whose mothers who were literate. Similarly, children from households without latrines were 2.9 [AOR = 2.91; 95% CI: 1.33–6.37] times more likely to encounter wasting than their counterparts. The households that do not have separate kitchens were 3.42 [AOR = 3.42; 95% CI: 1.24, 9.45] times more likely to encounter waste than their counterparts. Similarly, the odds of experiencing wasting among children from food-insecure households were 4.11 [AOR = 4.11; 95% CI: 1.87–9] times higher than those of their counterparts.
Moreover, the odds of household dietary diversity were 7.44 [AOR =7.44; 95% CI: 2.58, 21.45] times higher among households consuming five or more food groups than those consuming four or less food groups. Furthermore, children who did not receive home visits after discharge from the outpatient therapeutic program by health workers were 4.2 [AOR = 4.2; 95% CI: 1.92–9.15] times more likely to be wasted when compared to children who received follow-up visits. Finally, readmitted children were 3.98 [AOR = 3.98; 95% CI: 1.43–15.07] times more likely to be wasted than new admissions (Table 6).
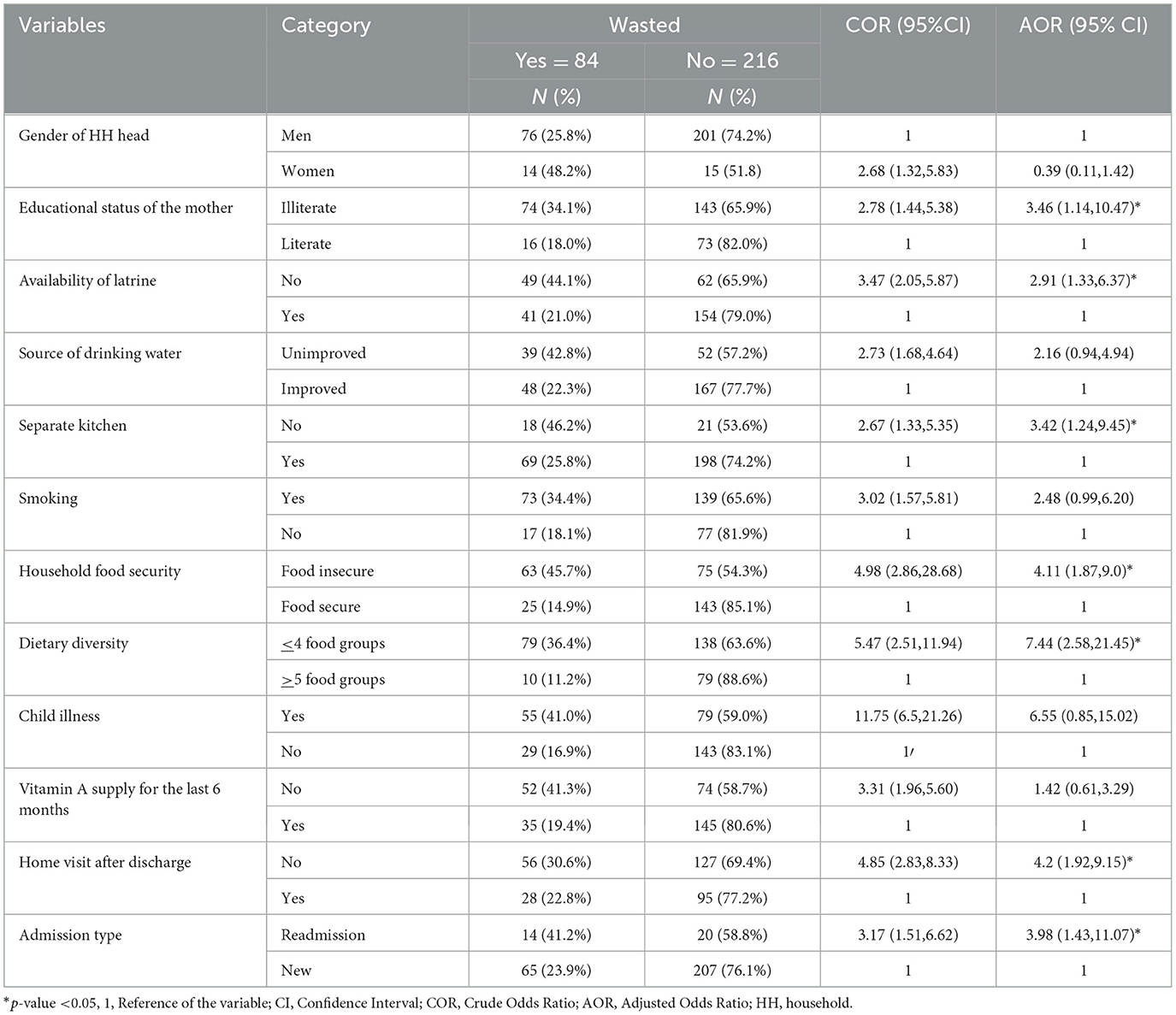
Table 6. Factors associated with wasting of children aged 6–59 months after 6 months following discharge from OTP in Habro Woreda, East Ethiopia 2020 (n = 306).
This study was carried out to assess the prevalence and associated factors among children aged 6–59 months after 6 months post-discharge from an outpatient therapeutic program in Habro Woreda, Oromia, Eastern Ethiopia. The result of this study showed that the prevalence of wasting among children aged 6–59 months after 6 months of discharge from the outpatient therapeutic program was 28% (95% CI: 26.5–32.2%). Moreover, the current study revealed that the educational status of the mother, availability of a latrine, separate kitchen, household food insecurity, household dietary diversity, home visit, and admission type were significantly associated with wasting.
According to this study, children born to mothers or caregivers who were illiterate were 3.46 times more likely to experience wasting than their counterparts. This is in line with the studies conducted in Northern Ethiopia (35) and Gurage, Central Ethiopia (20). This is probably because education explicitly enhances the knowledge and awareness of caregivers/mothers to utilize optimal, balanced, and healthy food, which ultimately prevents the likelihood of getting wasted.
In this study, children from households without latrines were significantly associated with wasting. Specifically, the odds of developing wasting among children from households without latrines were 2.91 times higher than their counterparts. This is in agreement with the studies conducted in different settings (4, 19, 22, 31, 36, 37). One plausible explanation could be that those without latrines are explicitly predisposed to diarrheal diseases, which in turn hugely and profoundly affect their nutritional status, ultimately leading to wasting (38–41). Moreover, other sanitation problems related to food are more likely to occur in children who live in households without latrines. More importantly, the lack of latrines might be tied to low socioeconomic status, and limited knowledge and awareness of the importance of having latrines, thereby playing a role in exacerbating problems related to wasting (42, 43).
In the present study, a lack of a separate kitchen was found to be an independent predictor of wasting among children. Accordingly, those children from households who did not have a separate kitchen were 3.42 times more likely to experience wasting than their counterparts. This is in line with the study conducted in West Ethiopia (44). One possible reason could be related to the fact that those households without kitchens are probably of low socioeconomic status, which vividly indicates that the individual households are affected by the problems. A more compelling argument might be that households might utilize solid fuel because of their lower socioeconomic status, which plays a critical role in increasing their likelihood of developing oxidative stress, a condition characterized by an imbalance of free radicals and antioxidants in the body and leads to cell damage (35, 45). Smoking solid fuel is a significant risk factor for respiratory disorders, vascular, and organ diseases owing to its high content of harmful chemicals and reactive oxygen species (ROS). These diseases can lead to depression and lack of appetite for food, which in turn causes wasting among children (35, 45–47). Another plausible explanation could be that solid fuel exposure from cooking and heating may result in overlapping effects and constitute cumulative damage to human health, which clearly also includes wasting (48).
The current study confirmed that children who came from food-insecure households and households that consumed less than or equal to four food groups were more likely to develop wasting than their respective counterparts. This result is supported by the studies conducted in Nepal (49), Tanzania (50), and Ghana (51). Household food insecurity and consumption of low-diversity foods are associated with wasting. The probable cause of food insecurity and lack of diversification of food groups is the low socioeconomic position or low monthly income, which affects households' purchasing power, which in turn reduces access to food (52). Children who consume diverse diets are less likely to be undernourished than those who consume a less diverse diet (53–56). Appropriate education should be given to caregivers of children or mothers on the diversification of food to feed their children and nourish them with a balanced diet.
There might be potential recall bias among respondents when they are answering questions related to past events, and laboratory investigations and related data were not collected in this study. Moreover, being cross-sectional, the study does not address the seasonal variation of child nutritional status or the cause-and-effect relationship between wasting and associated factors, and it uses a single outcome measurement technique. In this study, the variable mid-upper arm circumference (MUAC) at admission, MUAC at discharge, and following child discharge linked or non-supplemental to the feeding program were not included.
This study showed that the educational status of the mother, availability of a latrine, separate kitchen, household food insecurity, household dietary diversity, home visit, and admission type are significantly associated with the wasting of children after discharge from an outpatient therapeutic program. Therefore, efforts that target these factors should be maximized to reduce the occurrence of wasting among children aged 6–59 months after discharge from the outpatient therapeutic program.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethical clearance was obtained from the Institutional Health Research Ethics Review Committee (IHRERC) of the College of Health and Medical Sciences, Haramaya University. Informed written/verbal consent was obtained from all subjects and/or the children's parents or caregivers or legal guardian(s). Confidentiality and privacy of every respondent's information were ensured and maintained by using codes instead of the participant's name. Participants were also informed that they have the full right to refuse participation or withdraw at any time from the research. All methods were performed in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
ST: Conceptualization, Data curation, Formal analysis, Writing – original draft. KR: Methodology, Writing – original draft. HR: Methodology, Writing – review & editing. JN: Conceptualization, Data curation, Writing – original draft. TS: Data curation, Methodology, Writing – review & editing. BA: Conceptualization, Methodology, Writing – original draft. MM: Conceptualization, Methodology, Writing – review & editing. AD: Conceptualization, Methodology, Writing – review & editing. AE: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. IM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors acknowledge the Haramaya University and West Hararghe health bureau for their cooperation during the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. Guideline: updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization (2013).
2. Jolly R. UNICEF (United Nations Children's Fund): Global Governance that Works. London: Routledge (2014). doi: 10.4324/9781315795508
3. European Commission. DG ECHO Thematic Policy Document No. 4 Nutrition: Addressing Nutrition in Emergencies. Brussels: European Commission (2013).
4. Hoseini BL, Saeidi M, Rezaei AM, Khademi G. Child malnutrition at different world regions in (1990-2013). Int J Pediatr. (2015) 3:921–32. doi: 10.22038/ijp.2015.4748
5. WHO. Department of Maternal, Newborn, Child and Adolescent Health (MCA): Progress Report 2014–15. Geneva: World Health Organization (2016).
6. EDHS CSA and ICF. Central Statistical Agency (CSA) [Ethiopia] and ICF (2016) Ethiopia demographic and health survey 2016: Key indicators report. Addis Ababa, Ethiopia, and Rockville, Maryland, USA (2016).
7. UNICEF. Joint Child Malnutrition Estimates: Levels and Trends in Child Malnutrition. Geneva: World Health Organization (2020).
8. McGuire S. World Health Organization. Comprehensive implementation plan on maternal, infant, and young child nutrition. Geneva, Switzerland, 2014. Adv Nutr. (2015) 6:134. doi: 10.3945/an.114.007781
9. Gebru TT, Abady GG, Teklu FG, Tesfamichael YA, Bitow MT, Tekola KB, et al. Assessment of wasting and associated factors among under five children of Wukro town, Tigray regional, North Ethiopia: a cross sectional study. Pan African Med J. (2019) 33:931. doi: 10.11604/pamj.2019.33.330.18808
10. Wete AT, Zerfu TA, Anbese AT. Magnitude and associated factors of wasting among under five orphans in Dilla town, southern Ethiopia: 2018: a cross-sectional study. BMC Nutr. (2019) 5:1–10. doi: 10.1186/s40795-019-0295-6
11. Tsedeke W, Tefera B, Debebe M. Prevalence of acute malnutrition (wasting) and associated factors among preschool children aged 36–60 months at Hawassa Zuria, South Ethiopia: a community based cross sectional study. J Nutr Food Sci. (2016) 6:2. doi: 10.4172/2155-9600.1000466
12. Gizaw Z, Woldu W, Bitew BD. Acute malnutrition among children aged 6–59 months of the nomadic population in Hadaleala district, Afar region, northeast Ethiopia. Ital J Pediatr. (2018) 44:1–10. doi: 10.1186/s13052-018-0457-1
13. UNICEF. Levels and Trends in Child Malnutrition: UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates, Key Findings of the 2023 Edition. Geneva: World Health Organization (2023).
14. Frison S, Angood C, Khara T, Bahwere P, Black RE, Briend A, et al. Prevention of child wasting: results of a Child Health & Nutrition Research Initiative (CHNRI) prioritisation exercise. PLoS ONE. (2020) 15:e0228151. doi: 10.1371/journal.pone.0228151
15. Angood C, Khara T, Dolan C, Berkley JA, WaSt Technical Interest Group. Research priorities on the relationship between wasting and stunting. PLoS ONE. (2016) 11:e0153221. doi: 10.1371/journal.pone.0153221
16. UNICEF. Levels and Trends in Child Malnutrition. Esocialsciences. Geneva: World Health Organization (2022).
17. Gebremeskel MG, Tirore LL, Derilo HT. Determinants of wasting among under-five children in Ethiopia: Multilevel ordinal logistic regression analysis of EDHS 2016. J Family Med Prim Care. (2022) 11:3777–83. doi: 10.4103/jfmpc.jfmpc_1993_21
18. ICF and EPHIEEa. Ethiopia Mini Demographic and Health Survey 2019: key Indicators. Rockville, Maryland, USA: EPHI and ICF (2019).
19. Yeshaneh A, Mulu T, Gasheneit A, Adane D. Prevalence of wasting and associated factors among children aged 6-59 months in Wolkite town of the Gurage zone, Southern Ethiopia, 2020. A cross-sectional study. PLoS ONE. (2022) 17:e0259722. doi: 10.1371/journal.pone.0259722
20. Rahman AM. A review on child and maternal health status of Bangladesh. CHRISMED J Health Res. (2018) 5:1–7. doi: 10.4103/cjhr.cjhr_65_17
21. Girma A, Woldie H, Mekonnen FA, Gonete KA, Sisay M. Undernutrition and associated factors among urban children aged 24–59 months in Northwest Ethiopia: a community based cross sectional study. BMC Pediatr. (2019) 19:1–11. doi: 10.1186/s12887-019-1595-3
22. Brhane H, Mohammed B, Yeshita HY, Gonete KA. Prevalence and associated factors of acute malnutrition among 6–59 month children in adi-harush and Hitsats refugee camps in Tigray region Northern Ethiopia, 2017. Am J Life Sci. (2018) 6:57–64. doi: 10.11648/j.ajls.20180605.11
23. Dessie ZB, Fentie M, Abebe Z, Ayele TA, Muchie KF. Maternal characteristics and nutritional status among 6–59 months of children in Ethiopia: further analysis of demographic and health survey. BMC Pediatr. (2019) 19:1–10. doi: 10.1186/s12887-019-1459-x
24. Amare ZY, Ahmed ME, Mehari AB. Determinants of nutritional status among children under age 5 in Ethiopia: further analysis of the 2016 Ethiopia demographic and health survey. Global Health. (2019) 15:1–11. doi: 10.1186/s12992-019-0505-7
25. Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. (2007) 370:1453–7. doi: 10.1016/S0140-6736(07)61602-X
26. Agin H, Arslanköylü A, Yener N, Anil A, Dursun O, Kendirli T, et al. Nutrition in pediatric intensive care units. Turkish J Pediatr Emer Intens Care Med. (2023) 10:66–83. doi: 10.4274/cayd.galenos.2023.49002
27. WHO Multicentre Growth Reference Study Group, de Onis M. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr. (2006) 95:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x
28. Tomita A, Ramlall S, Naidu T, Mthembu SS, Padayatchi N, Burns JK. Major depression and household food insecurity among individuals with multidrug-resistant tuberculosis (MDR-TB) in South Africa. Soc Psychiat Psychiatr Epidemiol. (2019) 54:387–93. doi: 10.1007/s00127-019-01669-y
29. Stobaugh HC, Rogers BL, Webb P, Rosenberg IH, Thakwalakwa C, Maleta KM, et al. Household-level factors associated with relapse following discharge from treatment for moderate acute malnutrition. Br J Nutr. (2018) 119:1039–46. doi: 10.1017/S0007114518000363
30. Dessalegn M, Kumie A, Tefera W. Predictors of under-five childhood diarrhea: Mecha District, west Gojam, Ethiopia. Ethiop J Health Dev. (2011) 25:192–200.
31. Motbainor A, Taye A. Wasting in under five children is significantly varied between rice producing and non–producing households of Libokemkem district, Amhara region, Ethiopia. BMC Pediatr. (2019) 19:300. doi: 10.1186/s12887-019-1677-2
32. Kassie GW, Workie DL. Exploring the association of anthropometric indicators for under-five children in Ethiopia. BMC Public Health. (2019) 19:764. doi: 10.1186/s12889-019-7121-6
33. Belina D, Belachew W, Hiko A, Duguma A, Hasen I, Urji A, et al. Assessments of challenges and marketing channels of skin and hide in Eastern Ethiopia. J Veter Sci Technol. (2018) 9:1–8. doi: 10.4172/2157-7579.1000510
34. Ergano K, Getachew M, Seyum D, Negash K. Determinants of community based maternal health care service utilization in South Omo pastoral areas of Ethiopia. J Med Med Sci. (2012) 3:112–21.
35. Cha SR, Jang J, Park SM Ryu SM, Cho SJ, Yang SR. Cigarette smoke-induced respiratory response: insights into cellular processes and biomarkers. Antioxidants. (2023) 12:1–30. doi: 10.3390/antiox12061210
36. Ayana AB, Hailemariam TW, Melke AS. Determinants of acute malnutrition among children aged 6–59 months in public hospitals, Oromia region, West Ethiopia: a case–control study. BMC Nutr. (2015) 1:1–11. doi: 10.1186/s40795-015-0031-9
37. EDHS Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and IC (2016).
38. Dires S, Mareg M. The magnitude of wasting and associated factors among children aged 2-5 years in southern Ethiopia: a cross-sectional study. Biomed Res Int. (2021) 2021:6645996. doi: 10.1155/2021/6645996
39. Ferdous F, Das SK, Ahmed S, Farzana FD, Latham JR, Chisti MJ, et al. Severity of diarrhea and malnutrition among under five-year-old children in rural Bangladesh. Am J Trop Med Hyg. (2013) 89:223–8. doi: 10.4269/ajtmh.12-0743
40. Melese B, Paulos W, Astawesegn FH, Gelgelu TB. Prevalence of diarrheal diseases and associated factors among under-five children in Dale District, Sidama zone, Southern Ethiopia: a cross-sectional study. BMC Public Health. (2019) 19:1235. doi: 10.1186/s12889-019-7579-2
41. Anil G. Prevalence of diarrhoea and its association with wasting, age, and gender in children below the age of five years. Int J Med Res Rev. (2014) 2:291–5. doi: 10.17511/ijmrr.2014.i04.04
42. Adzawla W, Alhassan H, Jongare AI. Explaining the effects of socioeconomic and housing characteristics on the choice of toilet facilities among Ghanaian households. J Environ Public Health. (2020) 2020:4036045. doi: 10.1155/2020/4036045
43. Getu BD, Azanaw KA, Zimamu LY, Adal GM, Tibebu NS, Emiru TD, et al. Wasting and its associated factors among children aged from 6 to 59 months in Debre Tabor town, Amhara region of Ethiopia, 2019: a multicentre community-based cross-sectional study. BMJ Open. (2023) 13:e071679. doi: 10.1136/bmjopen-2023-071679
44. Shama AT, Wakuma O, Debelo S, Terefa DR, Cheme MC, Lema M, et al. Prevalence and associated factors of stunting and thinness among primary school-aged children in Gudeya Bila district, West Ethiopia: a cross-sectional study. BMJ Open. (2023) 13:e072313. doi: 10.1136/bmjopen-2023-072313
45. Chair SY, Choi KC, Chong MS, Liu T, Chien WT. Household air pollution from solid fuel use and depression among adults in rural China: evidence from the China Kadoorie Biobank dat. BMC Public Health. (2023) 23:1081. doi: 10.1186/s12889-023-16038-3
46. Masschelin PM, Cox AR, Chernis N, Hartig SM. The impact of oxidative stress on adipose tissue energy balance. Front Physiol. (2020) 10:1638. doi: 10.3389/fphys.2019.01638
47. Ahmed M, Neville MJ, Edelmann MJ, Kessler BM, Karpe F. Proteomic analysis of human adipose tissue after rosiglitazone treatment shows coordinated changes to promote glucose uptake. Obesity. (2010) 18:27–34. doi: 10.1038/oby.2009.208
48. Savini ICM, Evangelista D, Gasperi V, Avigliano L. Obesity-associated oxidative stress: strategies finalized to improve redox state. Int J Mol Sci. (2013) 14:10497–538. doi: 10.3390/ijms140510497
49. Nepali S, Simkhada P, Davies IG. Association between wasting and food insecurity among children under five years: findings from Nepal demographic health survey 2016. BMC Public Health. (2020) 20:1027. doi: 10.1186/s12889-020-09146-x
50. Khamis AG, Mwanri AW, Ntwenya JE, Kreppel K. The influence of dietary diversity on the nutritional status of children between 6 and 23 months of age in Tanzania. BMC Pediatr. (2019) 19:518. doi: 10.1186/s12887-019-1897-5
51. Wemakor A, Laari J. Association between household dietary diversity and nutritional status of children (6–36 months) in Wenchi Municipality, Brong Ahafo Region, Ghana. Nutrire. (2018) 43:22. doi: 10.1186/s41110-018-0081-2
52. Jarso H, Workicho A, Alemseged F. Survival status and predictors of mortality in severely malnourished children admitted to Jimma University Specialized Hospital from 2010 to 2012, Jimma, Ethiopia: a retrospective longitudinal study. BMC Pediatr. (2015) 15:76. doi: 10.1186/s12887-015-0398-4
53. Zeinalabedini M, Zamani B, Nasli-Esfahani E, Azadbakht L. A systematic review and meta-analysis of the association of dietary diversity with undernutrition in school-aged children. BMC Pediatr. (2023) 23:269. doi: 10.1186/s12887-023-04032-y
54. Marinda PA, Chalula F, Khayeka-Wandabwa C, Audain K, Thilsted SH. Dietary diversity and nutritional status of children aged 6–59 months from rural fishing and non-fishing communities in Zambia. Sci African. (2023) 19:e01527. doi: 10.1016/j.sciaf.2022.e01527
55. Abitew DB, Worku A, Mulugeta A, Bazzano AN. Rural children remain more at risk of acute malnutrition following exit from community based management of acute malnutrition program in South Gondar Zone, Amhara Region, Ethiopia: a comparative cross-sectional study. PeerJ. (2020) 8:e8419. doi: 10.7717/peerj.8419
Keywords: wasting, children, outpatient, discharge, Ethiopia
Citation: Tilahun S, Roba KT, Roba HS, Nure JA, Sosengo T, Ayele BH, Maruta MB, Debella A, Eyeberu A and Mussa I (2024) Prevalence of wasting and associated factors among children aged 6–59 months in Habro district, Eastern Ethiopia: a cross-sectional study. Front. Nutr. 11:1353086. doi: 10.3389/fnut.2024.1353086
Received: 15 December 2023; Accepted: 18 June 2024;
Published: 05 July 2024.
Edited by:
Sisay Abebe Debela, Suzhou University, ChinaReviewed by:
Asmamaw Deguale Worku, Yekatit 12 Hospital Medical College, EthiopiaCopyright © 2024 Tilahun, Roba, Roba, Nure, Sosengo, Ayele, Maruta, Debella, Eyeberu and Mussa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ibsa Mussa, aWJzYW11c3NhOTNAZ21haWwuY29t
†ORCID: Ibsa Mussa orcid.org/0000-0002-6318-4092
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.