
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 06 June 2024
Sec. Nutritional Epidemiology
Volume 11 - 2024 | https://doi.org/10.3389/fnut.2024.1336864
This article is part of the Research Topic Nutrition and Sustainable Development Goal 2: Zero Hunger View all 24 articles
 Hiwot Altaye Asebe1*†
Hiwot Altaye Asebe1*† Zufan Alamrie Asmare2
Zufan Alamrie Asmare2 Kusse Urmale Mare3
Kusse Urmale Mare3 Bizunesh Fantahun Kase4
Bizunesh Fantahun Kase4 Tsion Mulat Tebeje5
Tsion Mulat Tebeje5 Yordanose Sisay Asgedom6
Yordanose Sisay Asgedom6 Abdu Hailu Shibeshi7
Abdu Hailu Shibeshi7 Afewerk Alemu Lombebo8
Afewerk Alemu Lombebo8 Kebede Gemeda Sabo9
Kebede Gemeda Sabo9 Bezawit Melak Fente10
Bezawit Melak Fente10 Meklit Melaku Bezie11
Meklit Melaku Bezie11 Beminate Lemma Seifu12
Beminate Lemma Seifu12Background: Despite various interventions to combat child malnutrition in sub-Saharan Africa, wasting remains a critical public health concern for children aged 6–59 months. Wasting is a significant predictor of child survival and development, with a heightened risk of mortality among children. However, there is a lack of recent comprehensive data on the prevalence, severity level, and factors contributing to wasting in this age group.
Objective: To identify the severity levels of wasting and its individual and community-level factors contributing to wasting among children aged 6–59 months in Sub-Saharan African countries.
Methods: This research utilized Demographic and Health Survey data from 34 Sub-Saharan African countries, spanning the period from 2007 to 2022. The study included a weighted sample of 180,317 6–59-month-old children. We employed a multilevel proportional odds model to identify factors predicting the severity of wasting. Adjusted odds ratios and 95% confidence intervals were reported to demonstrate significant relationships (p < 0.05) in the final model.
Results: In Sub-Saharan Africa, 7.09% of children aged 6–59 months experience wasting (95% CI: 6.97, 7.20%). Among these children, the prevalence of moderate wasting is 4.97% (95% CI: 4.90, 5.10%), while severe wasting affects 2.12% (95% CI: 2.0, 2.20%). Factors such as term/post-term babies, wealth, frequency of feeding, improved toilet facilities, water sources, employed and educated mothers, rural residence, high community maternal education, and community media exposure are strongly associated with a lower chance of experiencing severe form of wasting. Conversely, birth order, family size, breastfeeding, diarrhea, cough, and fever, high community poverty, female household heads, and all Sub-Saharan Africa regions are linked to higher levels of wasting.
Conclusion: The study findings underscore the persistent challenge of wasting among Sub-Saharan Africa’s children, with 7.09% affected, of which 4.97% experience moderate wasting and 2.12% severe wasting. The identified predictors of wasting highlight the complex interplay of socio-economic, environmental, and health-related determinants. To address this issue improve access to healthcare and nutrition services, enhance sanitation infrastructure, promote women’s empowerment, and implement community-based education programs. Additionally, prioritize early detection through routine screening and strengthen health systems’ capacity to provide timely interventions.
Wasting in under-five children is a serious global health issue (1). The World Health Organization (WHO) defines wasting as low weight-for-height or less than −2 SD (1). This typically signifies a recent and drastic reduction in weight, although it can also be a long-lasting condition.
Wasting in children is a critical health issue that arises from inadequate nutrition or repeated illnesses. It weakens the immune system, increases the risk of mortality, and can lead to long-term developmental issues, especially when it’s severe (2, 3). In 2022, 45 million children under the age of 5, which is 6.8% of this age group, were affected by wasting. Out of these, 13.7 million (2.1%) were experiencing severe wasting (4). More than three-quarters of all children with severe wasting live in Asia and another 22 percent live in Africa (5).
Though various strategies have been implemented to combat child malnutrition in Sub-Saharan Africa, wasting remains critically prevalent. This persistent high rate of malnutrition continues to be a major obstacle to achieving better health outcomes for children in the region (6, 7). In sub-Saharan Africa in 2017, 7.1% of children under five were wasted, or about 13.8 million children. Of these, 4 million were severely wasted (8). Furthermore, an estimated 6.3 million children under 5 in six countries in Africa’s Sahel region will be malnourished this year (9). In the East and Southern African region, over 1.5 million children are lacking critical treatment for severe malnutrition, which could save their lives (10). Childhood wasting has severe consequences, including increased mortality, susceptibility to illness, developmental delays, and long-term impacts on the economic and social potential and progress of the countries (11, 12). In countries where child mortality rates are high, being underweight contributes to approximately 15% of the overall burden on disability-adjusted life years (DALY) (13).
Previous studies revealed that inadequate energy and nutrient intake, nutrient loss due to infection, or a combination of both low energy or protein intake and high nutrient loss, maternal characteristics such as BMI, and education, as well as socio-economic condition and availability of services including water, sanitation, and hygiene, family size, and parental occupation were significant factors associated with wasting (14–19).
Several studies have proven that wasting among 6–59-month-old children is a serious public health problem in SSA. However, there is a paucity of recent evidence on the prevalence, severity level, and predictors of wasting in this age group in SSA. In addition, even though wasting has an ordinal nature, previous studies treat wasting as a binary outcome (have wasting vs. have no wasting). Therefore, simply classifying waste as either present or absent can miss important details and is not helpful for those who need to make choices or develop public health programs. Thus, this study identified both the individual and community-level predictors of wasting among children aged 6–59 months in SSA using a multilevel ordinal logistic regression model. Knowing the nuanced severity levels of wasting enables policymakers to refine strategies, enhancing public health programming and decision-making across the region.
We used the 2007 to 2022 DHS data from 34 Sub-Saharan African countries. The DHS is a survey conducted every 5 years to provide updated health and related indicators. The study subjects were chosen using a two-stage stratified sampling method. The first stage involved randomly selecting enumeration areas (EAs). The second step involved selecting households from the EAs. Each country’s survey comprises various datasets, such as those for men, women, children, births, and households. We used the Kids Record (KR) file. We selected relevant data from the KR dataset based on previous research. We then combined this data with another dataset using the STATA command “append using.” The total weighted sample size in this study was 180,317.
Our dependent variable was severity levels of wasting among 6–59 months children, We classified it into three ordinal categories.; (ordinal variable, which was categorized as severely wasted if a child’s WHZ score was below −3 SD, moderately wasted (− 3 ≤ WHZ < − 2), and not wasted WHZ ≥ − 2 SD).
The predictor variables were based on two sources: individual-level and community-level factors.
Household factors: wealth index, sex of household head, family size, number of under-five children in the household, visit to a health facility, source of drinking water, and type of toilet facility (16, 20).
Maternal characteristics: maternal education and maternal working status, maternal media exposure (16, 21, 22).
Child characteristics: age of child, sex of child, twin status, order of birth, duration of pregnancy (preterm, term, post-term), breastfeeding status, fever, diarrhea, and cough within the past 2 weeks, and number of times a child feeds (23–26).
Community-level factors: a place of residence, SSA region, community poverty, media exposure, and maternal literacy.
Media exposure was measured by adding up three variables: watching television, listening to the radio, and reading newspapers. Mothers who were exposed to at least one of the three media sources listed were categorized as having media exposure. Mothers who were not exposed to any of the three media sources were categorized as not having media exposure. Three community-level variables were created: community maternal education, community media exposure, and community poverty. We derived these by aggregating individual-level data on maternal education, media exposure, and wealth status within each cluster or enumeration area. These variables were then classified as higher community maternal education, media exposure, and poverty based on the national median value of the proportion of maternal education and poverty. This classification was done since the distribution of these variables was not normal.
Protected drinking water sources: include piped water, public taps, standpipes, tube wells, boreholes, protected dug wells and springs, rainwater, and bottled water (27).
Unprotected drinking water sources: include unprotected wells and springs, surface water (river, dam, lake, pond, stream, canal, irrigation channel), tanker trucks, carts with small tanks, and others (27).
Improved toilet facilities: include flush/pour flush toilets to piped water systems, septic tanks, and pit latrines; ventilated improved pit (VIP) latrines, pit latrines with slabs, and composting toilets (27).
Unimproved toilet facilities: include flush to somewhere else, flush do not know where, pit latrine without a slab/open pit, no facility/bush/field, bucket toilet, hanging toilet/latrine, and others (27).
The statistical software STATA, version 17, was employed for data management and analysis. The WHO Anthro software was employed to generate WHZ scores. Descriptive results were presented using frequencies and percentages. Wasting, being a polychotomous variable with an ordinal nature, underwent analysis through an ordinal logistic regression model. Several types of ordinal logistic regression models were considered, such as the proportional odds model, partial proportional odds model with restrictions, partial proportional odds model without restrictions, continuous ratio model, and stereotype model. The proportional odds model, often utilized in epidemiological studies, was selected due to its frequent application.
This model assumes that the relationship between independent variables and the outcome variable is proportional; meaning the effect of each independent variable on the outcome is consistent across categories. The Brant test was conducted to assess the proportional odds assumption. Results indicated that the assumption was met (p > 0.05). Since the DHS data had a hierarchical structure, with children and mothers grouped within clusters, it was crucial to consider the variation between these clusters. To address this, a multilevel proportional odds model was used.
We calculated Likelihood Ratio (LR) tests, Variance Partition Coefficients (VPCs), and Median Odds Ratios (MORs) to figure out how much wasting changed between different clusters.
The VPC tells us how much of the total variation in wasting can be explained by the differences between the clusters, compared to the variation within each cluster. (28). The VPC was calculated using the formula.
Where π2/3 represents the variance of the standard logit distribution and σμ2 is the cluster variance.
The MOR measures the heterogeneity in wasting among clusters on the odds ratio scale. It represents the median odds ratio between the cluster with a high likelihood of wasting and the cluster at lower risk when individuals are randomly selected from two clusters (EAs) (29).
In the multilevel logistic regression analysis, four distinct models were developed. The initial model, known as the null model, did not include any explanatory variables and was used to gauge the degree of cluster variation in wasting. The second model incorporated variables at the individual level, while the third model was adjusted for variables at the community level. The fourth model was a comprehensive one, integrating both individual and community-level variables. We compared the models using their deviance, represented by the -2Log-Likelihood Ratio (LLR). The model with the smallest deviance was deemed to be the most suitable for the data.
In the null model, unobserved factors at the community level accounted for approximately 1.05% of the total variation in wasting (VPC = 1.05%). This finding did not necessarily favor a multilevel ordinal model over a single-level one. However, further examination with the LR test, it was revealed that the multilevel ordinal logistic regression model outperformed the single-level ordinal logistic regression analysis. Additionally, the MOR suggested that transferring children from clusters with lower likelihoods of higher wasting levels to clusters with higher likelihoods could lead to 1.2 times higher levels of wasting. Therefore, the LR test and MOR supported the use of a multilevel ordinal logistic regression model.
Variables with a p-value of<0.25 in the bivariable multilevel proportional odds model were included for consideration in the multivariable multilevel proportional odds model. In the multivariable model, the strength of association was represented by the AOR with a 95% CI, and statistical significance was determined at p < 0.05.
The current study utilized publicly available survey data from the MEASURE DHS program, eliminating the requirement for ethical review and informed consent. Permission to access and utilize the dataset for this research was obtained from http://www.dhsprogram.com. The datasets used do not contain any personal identifiers such as names or household addresses.
The study encompassed a total of 180,317 children between the ages of 6 and 59 months. Out of the total, 90,978 (50.45%) were males. About 39.8% of mothers did not receive any formal education. Around 21.85% of the children experienced fever, 21.25% had a cough, and 15.93% reported diarrhea within 2 weeks. Over half of the mothers (54.37%) were not exposed to any media, and the vast majority (83.45%) of the children were term babies (Table 1).
Among the study participants 41.2% were from West Africa, and 35.61% were from East Africa More than two-thirds (68.96%) of participants were rural residents. Concerning community maternal literacy, media exposure, and poverty, about 95,993 (53.24%), 83,406(46.26%), and 90,917(50.42%) of the participants were from the community with the highest levels of maternal literacy, media exposure, and poverty, respectively (Table 2).
7.09% of children 6–59 months in SSA are wasted (95% CI: 6.97, 7.20%). The percentage of wasted children varies from 4.30% in Southern Africa to 7.1% in West Africa. By the severity of wasting, the prevalence of moderate and severe wasting among children of the 6–59 month age group in Sub-Saharan Africa were 4.97% (95% CI: 4.90, 5.10%) and 2.12% (95% CI: 2.0, 2.20%), respectively (Table 3).
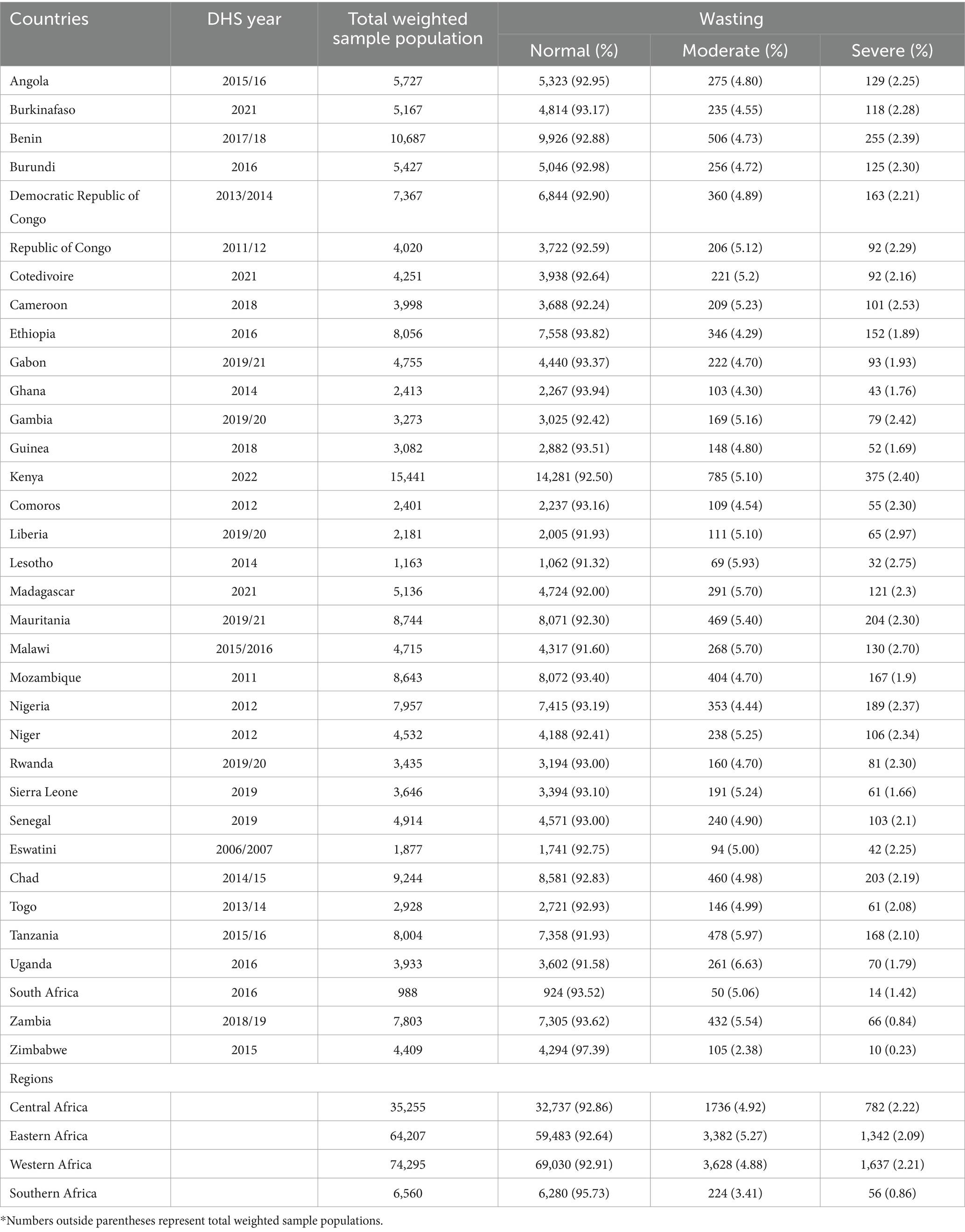
Table 3. Prevalence of wasting among 6–59 months children in sub-Saharan African countries evidence from DHS data (n = 180,317).
Being born term/post-term, family wealth, frequency of child feeding, improved toilet facilities, improved water sources, health facility visit, employed mother, rural residence, formal maternal education, media exposure, high community maternal education, high community media exposure were strongly linked to a lower chance of having a more severe form of wasting. In contrast, higher birth order, family size, breastfeeding status, diarrhea, cough, and fever in the past 2 weeks, high community poverty, female household heads, and all sub-Saharan Africa regions were strongly linked with higher levels of wasting.
The likelihood of having higher levels of wasting among children who feed 3to4 times a day decreased by 37% (AOR = 0.63, 95% CI: 0.59–0.66) compared to children who did not get food. The odds of having higher levels of wasting have decreased by 8% (AOR = 0.92, 95% CI: 0.87–0.98) for children born at term compared to preterm children. Children of mothers with primary and secondary education were at reduced risk of having severe wasting by 33 and 23%, respectively, than children of mothers without formal education. Children who never breastfed had1.72 times (AOR = 1.17, 95% CI: 1.6–1.84) times higher odds of having higher levels of wasting compared to those who still breastfed.
Children born sixth or later were 1.15 times (AOR = 1.15, 95% CI: 1.08–1.23) more likely to experience higher levels of wasting than first-born children. The likelihood of children experiencing higher levels of wasting was reduced by 53% (AOR = 0.47, 95% CI: 0.44–0.51) for those from middle-income households and by 51% (AOR = 0.49, 95% CI: 0.46–0.53) for those from rich households when compared to children from low-income households.
Children who had experienced diarrhea in the past 2 weeks were 1.53 times more likely (AOR = 1.53, 95% CI: 1.45–1.60) to exhibit higher levels of wasting compared to children who had not experienced diarrhea.
Children in East and West African regions had 1.42 times (AOR = 1.42, 95% CI: 1.25–1.61) and 1.19 times (AOR = 1.19, 95% CI: 1.04–1.36) higher odds of higher levels of wasting than those in South Africa.
A 16%(AOR = 0.84, 95% CI: 0.80–0.88) reduction in the odds of higher levels of wasting is observed among children who live in communities with higher levels of maternal education, compared to children who live in communities with lower levels of maternal education (Tables 4, 5).
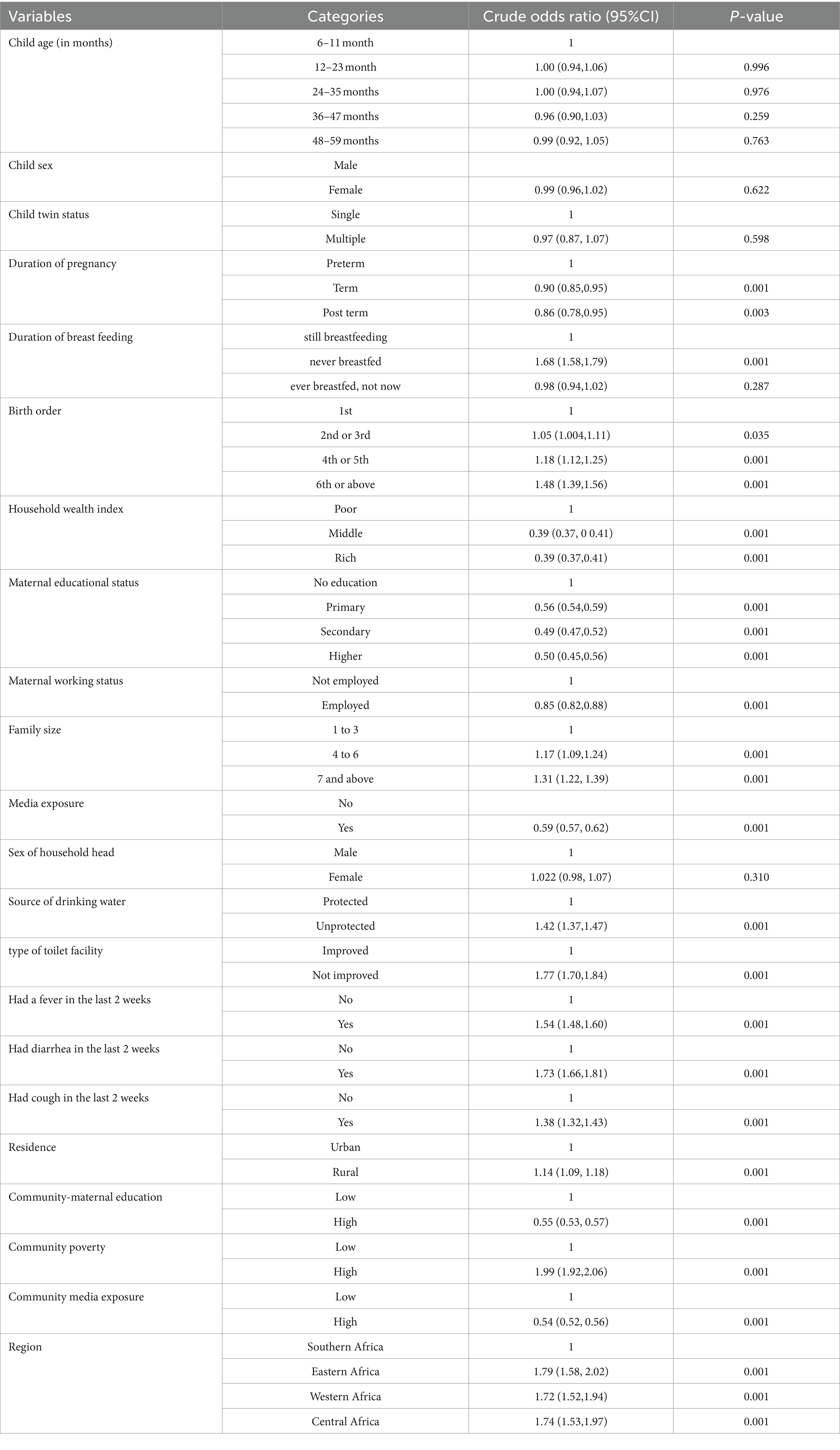
Table 4. Bivariable multilevel proportional ordinal logistic regression analysis of individual and community level variables associated with levels of wasting among children aged 6–59 month in sub-Saharan African countries.
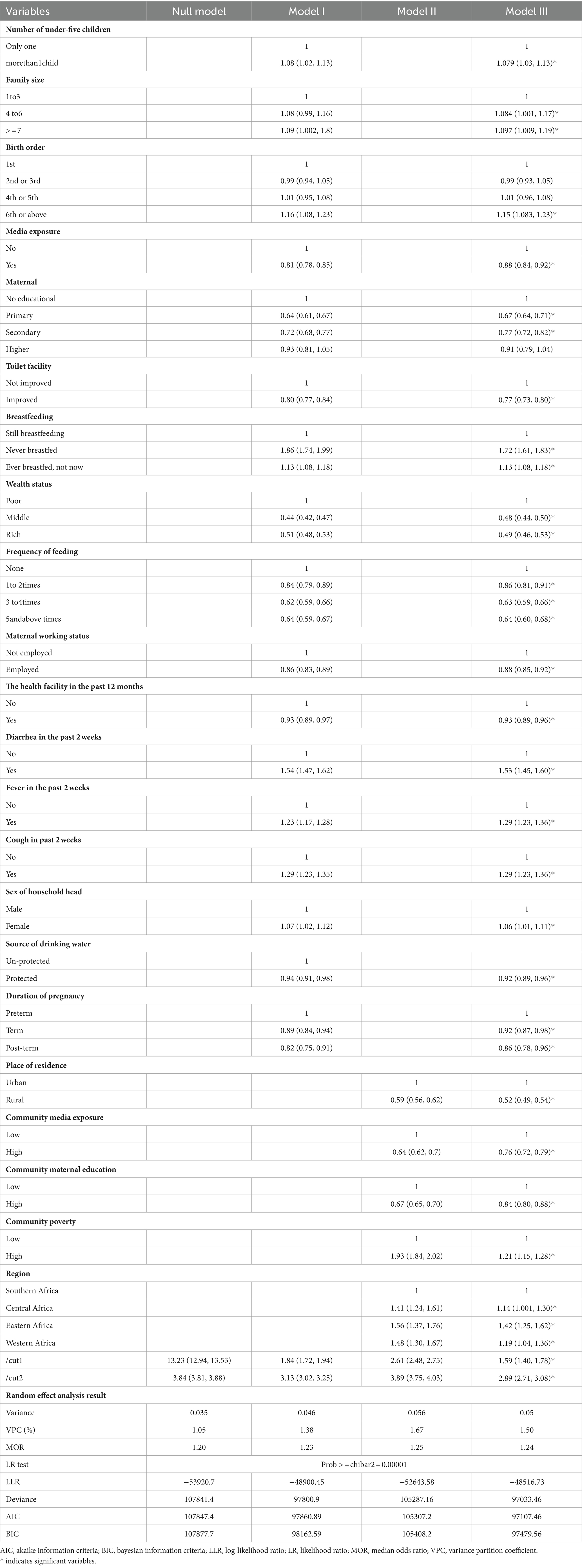
Table 5. Multilevel ordinal logistic regression analysis of individual and community level variables associated with severity levels of wasting among children aged 6–59 months in sub-Saharan African countries.
The primary objective of this study was to delve into the severity levels of wasting and pinpoint both individual and community-level factors that contribute to wasting among children aged 6–59 months in Sub-Saharan African countries. This aim stems from the pressing need to address the critical issue of child malnutrition, particularly wasting, which poses a significant threat to child health and survival in these regions.
Our findings reveal a diverse range of severity levels of wasting, highlighting the complexity of the issue at hand. The factors contributing to these levels are multifaceted, encompassing both individual and community-level elements. This underscores the necessity for a comprehensive approach to tackling wasting, one that goes beyond addressing individual nutritional needs and includes broader community and societal interventions their own nutritional challenges. Empowering communities to address their own nutritional challenges is paramount for effective intervention strategies in combating wasting among children in Sub-Saharan Africa (30). By involving local stakeholders in identifying priorities, designing solutions, and implementing programs tailored to their specific needs and contexts, a participatory approach fosters ownership and ensures the sustainability of interventions (6). Furthermore, integrating individual and community-level interventions can yield synergistic effects, amplifying the impact on reducing wasting and improving child health outcomes. Community-level interventions complement individual efforts by creating supportive environments that reinforce healthy behaviors and access to resources (31, 32). Recognizing the significance of community-level factors, policy changes must prioritize these interventions in health programming and decision-making processes. This may necessitate reallocating resources, forging stronger partnerships with community-based organizations, and incorporating community perspectives into policy development. Such measures are essential for addressing wasting effectively and promoting child health across Sub-Saharan Africa.
In this study wasting, a serious form of malnutrition, affects 7.09% (95% CI, 6.9, 7.20%) of children aged 6–59 months in Sub-Saharan African countries (SSA), with prevalence varying across regions, indicating that wasting is a significant health issue in SSA. This higher than theglobal prevalence of wasting (6.8%) among under five children (33) and studies conducted in Brazil and China (34, 35). This is because children in SSA have been malnourished for a long time as a result of enduring poverty in the region (36). Additionally, the low economic status of many African countries can restrict people’s ability to obtain enough nutritious food, which can lead to wasting (37).
Children from households in the middle and upper wealth quintiles are less likely to experience severe wasting than children from households in the poor wealth quintile. This conclusion aligns with these studies (16, 20, 24, 38–42). The potential explanation for this is that insufficient financial resources often lead to limited access to nutritious food, as impoverished families may struggle to afford a balanced diet that provides essential vitamins and minerals. Additionally, impoverished living conditions may expose children to unsanitary environments and unsafe water sources, increasing the risk of infections that further exacerbate nutritional challenges. Limited access to healthcare and educational resources within impoverished communities can also hinder parents’ awareness of proper nutrition practices, perpetuating the cycle of poor dietary habits (43–45).
Children who had diarrhea, fever, and cough in the past 2 weeks were more likely to be wasted than children who did not have these illnesses (17, 46–48). This is because infections significantly compromise children’s nutritional status by disrupting their dietary intake, absorption, and metabolism. Illnesses such as fever, cough, and diarrhea increase the body’s metabolic demands, necessitating higher energy and nutrient intake. However, the accompanying symptoms, such as decreased appetite, difficulty breathing, and gastrointestinal disturbances, often lead to reduced food consumption and nutrient absorption. Diarrhea, in particular, exacerbates the situation by causing rapid loss of fluids and essential nutrients. Moreover, the cyclical relationship between malnutrition and susceptibility to infections perpetuates a vicious cycle that poses long-term threats to a child’s overall health and well-being (49).
Children who fed less than three times per day were more prone to being wasted than their counterparts. This finding was aligned with the findings from similar studies (17, 50, 51). This is because, when a child is not fed regularly, it often leads to a chronic energy deficit, where the calories consumed are insufficient to meet the energy expenditure required for growth and development. This imbalance can result in the body utilizing its stores for energy, leading to unintended weight loss and a higher risk of wasting. Inadequate intake of essential nutrients, such as proteins and micronutrients, due to infrequent meals, further exacerbates the problem, compromising the child’s ability to build and maintain tissues. Additionally, irregular feeding patterns can disrupt metabolic processes, impacting the body’s ability to utilize nutrients efficiently (52).
The current study found that children who are part of a family with more than four members are at greater risk of being wasted than those from families with fewer than four members. This result is consistent with research done in Vietnam and Bangladesh (53, 54). This is attributable to larger families may face more financial pressure when it comes to food consumption, which could potentially lead to poorer nutritional status among the children.
The present results showed that employed and educated mothers were less likely to have wasted children than those who are not employed and uneducated. Unemployed mothers may face challenges due to financial constraints, such as providing nutritious food at the required frequency, ensuring adequate care, and accessing health care services. This finding is in line with research done in Nigeria, Ethiopia, and Afganistan (55–57).
Children in rural areas are less likely to be malnourished than children in urban areas. This finding is consistent with previous studies (58–60) On the other hand, some studies have found the opposite (18, 61, 62) the reason behind this is, that malnutrition is more common in rural areas due to factors such as low education levels, low social status, poor water quality, and high rates of infectious disease. However, rapid urbanization and the resulting high levels of poverty and hunger are now thought to be the main causes of malnutrition in urban areas (63).
Protected water sources and improved toilet facilities reduce the risk of wasting among children. This finding agrees with this stud (64–65). This is because a child who lives in a community with improved sanitation is less likely to be exposed to fecal matter in the environment, which reduces the risk of diarrhea and other infections and they will have a good appetit (66).
Maternal media exposure reduces the level of wasting among their children compared to their counterparts. This finding corresponds to the study conducted in North Africa (66). This can be explained by, improved access to information empowering mothers to adopt healthier behaviors and adhere to recommended feeding practices, ultimately contributing to better child nutrition outcomes. Furthermore, media exposure can also influence social norms and community perceptions regarding nutrition, fostering an environment that supports and encourages proper child-feeding practices (70).
This study indicates that children from households headed by females are more likely to experience wasting compared to those from households headed by males. This is in line with the study conducted in Nepal (57). The justification behind this conclusion is that female heads of households often carry a double burden in caring for their dependents and being the sole breadwinner of the family. This can lead to stress and limited time for proper child care, including feeding practices (67).
The findings of our study should be considered with certain restrictions. The cross-sectional design of the DHS data prevents us from determining cause-and-effect relationships. Furthermore, our study only accounted for children who were alive during the data collection period, omitting any fatalities that might have resulted from wasting-related complications (indicating survivor bias). However, despite these constraints, our study possesses several notable advantages. It utilizes a combined, nationally representative DHS survey encompassing 34 sub-Saharan African countries. Additionally, the substantial sample size of our study ensures adequate power to discern the genuine impact of the independent variables.
The study findings underscore the persistent challenge of wasting among children aged 6–59 months in Sub-Saharan Africa, with 7.09% affected, of which 4.97% experience moderate wasting and 2.12% severe wasting. The identified factors associated with wasting highlight the complex interplay of socio-economic, environmental, and health-related determinants. To address this issue effectively, interventions should adopt a multifaceted approach that targets vulnerable populations, improves access to healthcare and nutrition services, enhances sanitation infrastructure, promotes women’s empowerment, and implements community-based education programs. Additionally, prioritizing early detection through routine screening and strengthening health systems’ capacity to provide timely interventions are crucial steps toward reducing the burden of wasting and improving child health outcomes in the region.
Publicly available datasets were analyzed in this study. This data can be found here: Data is available online and you can access at: www.measuredhs.com.
Ethical approval was not required for the studies involving humans because The current study utilized publicly available survey data from the MEASURE DHS program, eliminating the requirement for ethical review and informed consent. Permission to access and utilize the dataset for this research was obtained from http://www.dhsprogram.com. The datasets used do not contain any personal identifiers such as names or household addresses. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements because The current study utilized publicly available survey data from the MEASURE DHS program, eliminating the requirement for ethical review and informed consent. Permission to access and utilize the dataset for this research was obtained from http://www.dhsprogram.com. The datasets used do not contain any personal identifiers such as names or household addresses.
HA: Conceptualization, Data curation, Formal analysis, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. ZA: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. KM: Conceptualization, Formal analysis, Methodology, Writing – original draft. BK: Data curation, Methodology, Writing – original draft. TT: Conceptualization, Software, Writing – original draft. YA: Formal analysis, Writing – original draft. AH: Methodology, Software, Writing – review & editing. AL: Writing – original draft, Writing – review & editing. KS: Data curation, Writing – review & editing. BF: Data curation, Writing – original draft, Writing – review & editing. MB: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. BS: Conceptualization, Data curation, Methodology, Software, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We would like to gratefully acknowledge the DHS programs, for the permission to use all the relevant DHS data for this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AIC, Akaike Information Criteria; AOR, Adjusted Odds Ratio; BIC, Bayesian Information Criteria; CI, Confidence Interval; DHS, Demographic health survey; EAs, Enumeration areas; LLR, Log-likelihood ratio; LR, Likelihood ratio; POM, Proportional Odds Model; PPOM, Partial Proportional Odds Model; SSA, Sub-Saharan Africa; WHO, World Health Organizations; WHZ, Z-score for Weight-for-Height; MOR, median odds ratio; VPC, variance partition coefficent.
1. WMGRS Groupde Onis, M. WHO child growth standards based on length/height, weight and age. Acta Paediatr. (2006) 95:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x,
2. UNICEF INDIA Care for Severly Wasted Children. Available at: https://www.unicef.org/india/what-we-do/care-severely-wasted-children (Accessed November 1, 2023).
3. Obembe, TA, Adenuga, WU, and Asuzu, MC. Determinants of wasting among schoolchildren in a southwestern state of Nigeria: implications to strengthen the nutritional component of primary health-care model. J Family Med Prim Care. (2018) 7:671–7. doi: 10.4103/jfmpc.jfmpc_324_17
4. United Nations Children’s Fund (UNICEF), World Health Organization (WHO). International Bank for Reconstruction and Development/the World Bank In: Levels and trends in child malnutrition: UNICEF / WHO / World Bank Group joint child malnutrition estimates: Key findings of the 2023rd edition. New York: UNICEF and WHO (2023)
5. UNICEF/WHO/World Bank Group Joint ChildMalnutrition Estimates Levels and trends in child malnutrition: key findings of the 2023edition.
6. Akombi, BJ, Agho, KE, Hall, JJ, Wali, N, Renzaho, AM, and Merom, D. Stunting, wasting and underweight in sub-Saharan Africa: a systematic review. Int J Environ Res Public Health. (2017) 14:863. doi: 10.3390/ijerph14080863
7. WHO. Global nutrition targets 2025: Breastfeeding policy brief (WHO/NMH/NHD14. 7). Geneva: World Health Organization. (2014).
8. Strategic plan to reduce malnutrition in Africa adopted by WHO Member States. Available at: https://afro.who.int/news/strategic-plan-reduce-malnutrition-africa-adopted-who-member-states
9. Scale-up action to combat child malnutrition in Africa’s Sahel. Available at: https://news.un.org/en/story/2022/04/1115662.
10. lack treatment for severe wasting in Eastern and Southern Africa. Available at: https://news.un.org/en/story/2022/01/1110282 (Accessed November 1, 2023).
11. WHO. Interpretation guide. Nutrition landscape information system (NLIS) Country Profile. 2017. p. 50. Available at: www.who.int/nutrition (Accessed September 10, 2021).
12. Briend, A, Khara, T, and Dolan, C. Wasting and stunting—similarities and differences: policy and programmatic implications. Food Nutr Bull. (2015) 36:S15–23. doi: 10.1177/15648265150361S103
13. Rodgers, A, Ezzati, M, Vander Hoorn, S, Lopez, AD, Lin, R-B, Murray, CJL, et al. Distribution of major health risks: findings from the global burden of disease study. PLoS Med. (2004) 1:e27. doi: 10.1371/journal.pmed.0010027
14. United Nations Children’s Fund (UNICEF), World Health Organization, International Bank for Reconstruction and Development/The World Bank. Levels and trends in child malnutrition: key findings of the 2019 Edition of the Joint Child Malnutrition Estimates. Geneva: World Health Organization (2019).
15. Balogun, TB, and Yakubu, AM. Recent illness, feeding practices and father’s education as determinants of nutritional status among preschool children in a rural Nigerian community. J Trop Pediatr. (2015) 61:92–9. doi: 10.1093/tropej/fmu070
16. Harding, KL, Aguayo, VM, and Webb, P. Factors associated with wasting among children under five years old in South Asia: implications for action. PLoS One. (2018) 13:e0198749. doi: 10.1371/journal.pone.0198749
17. Verma, P, and Prasad, JB. Stunting, wasting and underweight as indicators of under-nutrition in under five children from developing countries: a systematic review. Diabetes Metab Syndr Clin Res Rev. (2021) 15:102243. doi: 10.1016/j.dsx.2021.102243
18. Dabale, GA, and Sharma, M. Determinants of wasting among under-five children in Ethiopia:(a multilevel logistic regression model approach). Int J Stat Med Res. (2014) 3:368–77. doi: 10.6000/1929-6029.2014.03.04.5
19. Khan, S, Zaheer, S, and Safdar, NF. Determinants of stunting, underweight and wasting among children < 5 years of age: evidence from 2012-2013 Pakistan demographic and health survey. BMC Public Health. (2019) 19:358. doi: 10.1186/s12889-019-6688-2
20. Hossain, MM, Abdulla, F, and Rahman, A. Prevalence and determinants of wasting of under-5 children in Bangladesh: quantile regression approach. PLoS One. (2022) 17:e0278097. doi: 10.1371/journal.pone.0278097
21. Rahman, A, Chowdhury, S, and Hossain, D. Acute malnutrition in Bangladeshi children: levels and determinants. Asia Pacific J Public Health. (2009) 21:294–302. doi: 10.1177/1010539509335399
22. Iftikhar, A, Bari, A, Bano, I, and Masood, Q. Impact of maternal education, employment and family size on nutritional status of children. Pak J Med Sci. (2017) 33:1401–5. doi: 10.12669/pjms.336.13689
23. Karlsson, O, Kim, R, Guerrero, S, Hasman, A, and Subramanian, S. Child wasting before and after age two years: a cross-sectional study of 94 countries. EClin Med. (2022) 46:101353. doi: 10.1016/j.eclinm.2022.101353
24. Yeshaneh, A, Mulu, T, Gasheneit, A, and Adane, D. Prevalence of wasting and associated factors among children aged 6-59 months in Wolkite town of the Gurage zone, southern Ethiopia, 2020. A cross-sectional study. PLoS One. (2022) 17:e0259722. doi: 10.1371/journal.pone.0259722
25. Paré, BC, Dahourou, DL, Kabore, A, Sana, A, Kinda, R, Ouaro, B, et al. Prevalence of wasting and associated factors among 6 to 23 months old children in the Sahel region of Burkina Faso. Pan Afr Med J. (2019) 34:164. doi: 10.11604/pamj.2019.34.164.19886
26. Wali, N, Agho, KE, and Renzaho, AMN. Wasting and associated factors among children under 5 years in five south Asian countries (2014–2018): analysis of demographic health surveys. Int J Environ Res Public Health. (2021) 18:4578. doi: 10.3390/ijerph18094578
27. Improved sanitation facilities and drinking-water sources. Available at: https://www.who.int/data/nutrition/nlis/info/improved-sanitation-facilities-and-drinking-water-sources.
28. Rodrıguez, G, and Elo, I. Intra-class correlation in randomeffects models for binary data. Stata J. (2003) 3:32–46. doi: 10.1177/1536867X0300300102
29. Merlo, J, Ohlsson, H, Lynch, KF, Chaix, B, and Subramanian, S. Individual and collective bodies: using measures of variance and association in contextual epidemiology. J Epidemiol Community Health. (2009) 63:1043–8. doi: 10.1136/jech.2009.088310
30. WHO. (2021). The UNICEF/WHO/WB Joint Child Malnutrition Estimates (JME) group released new data for 2021.
31. Sakeah, E, Bawah, AA, Asuming, PO, Debpuur, C, Welaga, P, Awine, T, et al. Impact of community health interventions on maternal and child health indicators in the upper east region of Ghana. BMC Pregnancy Childbirth. (2023) 23:298. doi: 10.1186/s12884-023-05577-7
32. Otiti, MI, and Allen, SJ. Severe acute malnutrition in low- and middle-income countries. Paediatr Child Health. (2021) 31:301–7. doi: 10.1016/j.paed.2021.05.001
33. Elmighrabi, NF, Fleming, CAK, and Agho, KE. Wasting and underweight in northern African children: findings from multiple-Indicator cluster surveys, 2014–2018. Nutrients. (2023) 15:3207. doi: 10.3390/nu15143207
34. Li, H, Yuan, S, Fang, H, Huang, G, Huang, Q, Wang, H, et al. Prevalence and associated factors for stunting, underweight and wasting among children under 6 years of age in rural Hunan Province, China: a community-based cross-sectional study. BMC Public Health. (2022) 22:483. doi: 10.1186/s12889-022-12875-w
35. Horta, BL, Santos, RV, Welch, JR, Cardoso, AM, dos Santos, JV, Assis, AMO, et al. Nutritional status of indigenous children: findings from the first National Survey of indigenous People’s health and nutrition in Brazil. Int J Equity Health. (2013) 12:23. doi: 10.1186/1475-9276-12-23
36. Harttgen, K, Klasen, S, and Vollmer, S. Economic growth and child undernutrition in sub-Saharan Africa. Popul Dev Rev. (2013) 39:397–412. doi: 10.1111/j.1728-4457.2013.00609.x
37. Ahmad, D, Afzal, M, and Imtiaz, A. Effect of socioeconomic factors on malnutrition among children in Pakistan. Future Bus J. (2020) 6:30. doi: 10.1186/s43093-020-00032-x
38. Bloss, E, Wainaina, F, and Bailey, RC. Prevalence and predictors of underweight, stunting, and wasting among children aged 5 and under in Western Kenya. J Trop Pediatr. (2004) 50:260–70. doi: 10.1093/tropej/50.5.260
39. Yalew, B, Amsalu, F, and Bikes, D. Prevalence and factors associated with stunting, underweight and wasting: a community based cross sectional study among children age 6-59 months at Lalibela town, northern Ethiopia. J Nutr Disorders Ther. (2014) 4:13–14.
40. Motbainor, A, and Taye, A. Wasting in under five children is significantly varied between rice producing and non-producing households of Libokemkem district, Amhara region, Ethiopia. BMC Pediatr. (2019) 19:1–11. doi: 10.1186/s12887-019-1677-2
41. Amadu, I, Seidu, A-A, Duku, E, Frimpong, JB, Jnr, JEH, Aboagye, RG, et al. Risk factors associated with the coexistence of stunting, underweight, and wasting in children under 5 from 31 sub-Saharan African countries. BMJ Open. (2021) 11:e052267. doi: 10.1136/bmjopen-2021-052267
42. Siddiqa, M, Zubair, A, Kamal, A, Ijaz, M, and Abushal, T. Prevalence and associated factors of stunting, wasting and underweight of children below five using quintile regression analysis (PDHS 2017–2018). Sci Rep. (2022) 12:20326. doi: 10.1038/s41598-022-24063-2
43. Amare, D, Negesse, A, Tsegaye, B, Assefa, B, and Ayenie, B. Prevalence of undernutrition and its associated factors among children below five years of age in bure town, west Gojjam zone, Amhara National Regional State, Northwest Ethiopia. Adv Public Health. (2016) 2016:1–8. doi: 10.1155/2016/7145708
44. Siddiqui, F, Salam, RA, Lassi, ZS, and Das, JK. The intertwined relationship between malnutrition and poverty. Front Public Health. (2020) 8:453. doi: 10.3389/fpubh.2020.00453
45. van Cooten, MH, Bilal, SM, Gebremedhin, S, and Spigt, M. The association between acute malnutrition and water, sanitation, and hygiene among children aged 6–59 months in rural E thiopia. Matern Child Nutr. (2019) 15:e12631. doi: 10.1111/mcn.12631
46. Awoke, A, Ayana, M, and Gualu, T. Determinants of severe acute malnutrition among under five children in rural Enebsie Sarmidr District, east Gojjam zone, north West Ethiopia, 2016. BMC Nutr. (2018) 4:1–8. doi: 10.1186/s40795-018-0211-5
47. Fekadu, H, Adeba, A, Garoma, S, and Berra, W. Prevalences of wasting and its associated factors of children among 6–59 months age in Guto Gida district, Oromia regional state, Ethiopia. J Food Process Technol. (2014) 5:2. doi: 10.4172/2157-7110.1000289
48. Habtamu, E, Chilo, D, and Desalegn, D. Determinants of wasting among children aged 6–59 months in Wonago woreda, South Ethiopia. A facility-based unmatched case-control study. PLoS One. (2022) 17:e0269380. doi: 10.1371/journal.pone.0269380
49. Rodríguez, L, Cervantes, E, and Ortiz, R. Malnutrition and gastrointestinal and respiratory infections in children: a public health problem. Int J Environ Res Public Health. (2011) 8:1174–205. doi: 10.3390/ijerph8041174
50. Egata, G, Berhane, Y, and Worku, A. Predictors of acute undernutrition among children aged 6 to 36 months in east rural Ethiopia: a community based nested case-control study. BMC Pediatr. (2014) 14:1–10. doi: 10.1186/1471-2431-14-91
51. Olack, B, Burke, H, Cosmas, L, Bamrah, S, Dooling, K, Feikin, DR, et al. Nutritional status of under-five children living in an informal urban settlement in Nairobi, Kenya. J Health Popul Nutr. (2011) 29:357–63. doi: 10.3329/jhpn.v29i4.8451
52. Saunders, J, and Smith, T. Malnutrition: causes and consequences. Clin Med (Lond). (2010) 10:624–7. doi: 10.7861/clinmedicine.10-6-624
53. Lesiapeto, MS, Smuts, CM, and Hanekom, SM. Risk factors of poor anthropometric status in children under five years of age living in rural districts of the eastern cape and KwaZulu-Natal provinces, South Africa. South Afri J Clin Nutr. (2010) 23:202–7. doi: 10.1080/16070658.2010.11734339
54. Islam, MM, Alam, M, Tariquzaman, M, Kabir, MA, Pervin, R, Begum, M, et al. Predictors of the number of under-five malnourished children in Bangladesh: application of the generalized poisson regression model. BMC Public Health. (2013) 13:1–8. doi: 10.1186/1471-2458-13-11
55. Danso, F, and Appiah, MA. Prevalence and associated factors influencing stunting and wasting among children of ages 1 to 5 years in Nkwanta south municipality, Ghana. Nutrition. (2023) 110:111996. doi: 10.1016/j.nut.2023.111996
56. Donatus, E, Nwadiaro, E, Idu, R, and Eja, K. A study of malnutrition-dependent factors among under-five children in Ekureku community, Abi local government area of Cross River state, Nigeria. British J Med Med Res. (2017) 21:1–10. doi: 10.9734/BJMMR/2017/30204
57. Pradhan, A. Factors associated with nutritional status of the under five children. Asian J Med Sci. (2010) 1:6–8. doi: 10.3126/ajms.v1i1.2927
58. Amare, ZY, Ahmed, ME, and Mehari, AB. Determinants of nutritional status among children under age 5 in Ethiopia: further analysis of the 2016 Ethiopia demographic and health survey. Glob Health. (2019) 15:62. doi: 10.1186/s12992-019-0505-7
59. Kavosi, E, Hassanzadeh Rostami, Z, Kavosi, Z, Nasihatkon, A, Moghadami, M, and Heidari, M. Prevalence and determinants of under-nutrition among children under six: a cross-sectional survey in Fars province, Iran. Int J Health Policy Manag. (2014) 3:71–6. doi: 10.15171/ijhpm.2014.63
60. Janevic, T, Petrovic, O, Bjelic, I, and Kubera, A. Risk factors for childhood malnutrition in Roma settlements in Serbia. BMC Public Health. (2010) 10:1–8. doi: 10.1186/1471-2458-10-509
61. Tariku, A, Bikis, GA, Woldie, H, Wassie, MM, and Worku, AG. Child wasting is a severe public health problem in the predominantly rural population of Ethiopia: a community based cross–sectional study. Arch Public Health. (2017) 75:1–9. doi: 10.1186/s13690-017-0194-8
62. Almasian Kia, A, Rezapour, A, Khosravi, A, and Afzali, AV. Socioeconomic inequality in malnutrition in Under-5 children in Iran: evidence from the multiple Indicator demographic and health survey, 2010. J Prev Med Public Health. (2017) 50:201–9. doi: 10.3961/jpmph.17.028
63. Ghosh, S, and Shah, D. Nutritional problems in urban slum children. Indian Pediatr. (2004) 41:682–96.
64. Alaofè, H, and Asaolu, I. Maternal and child nutrition status in rural communities of Kalalé District, Benin: the relationship and risk factors. Food Nutr Bull. (2019) 40:56–70. doi: 10.1177/0379572118825163
65. Rahman, A. Significant risk factors for childhood malnutrition: evidence from an Asian developing country. Sci J Public Health. (2016) 4:16–27. doi: 10.11648/j.sjph.s.2016040101.14
66. Water, Sanitation and Hygiene (WASH). Available at: https://www.unicef.org/wash.
67. Yoosefi Lebni, J, Mohammadi Gharehghani, MA, Soofizad, G, khosravi, B, ziapour, A, and Irandoost, SF. Challenges and opportunities confronting female-headed households in Iran: a qualitative study. BMC Womens Health. (2020) 20:183. doi: 10.1186/s12905-020-01046-x
68. Fact sheet-malnutrition -Worldhealthorganization (WHO). Available at: https://www.who.int/news-room/fact-sheets/detail/malnutrition (Accessed June 9, 2021.
69. Seifu, BL, and Tesema, GA. Individual-and community-level factors associated with anemia among children aged 6-23 months in sub-Saharan Africa: evidence from 32 sub-Saharan African countries. Arch Public Health. (2022) 80:183. doi: 10.1186/s13690-022-00950-y
Keywords: wasting, 6–59 months children, SSA, multilevel ordinal logistic regression analysis, DHS
Citation: Asebe HA, Asmare ZA, Mare KU, Kase BF, Tebeje TM, Asgedom YS, Shibeshi AH, Lombebo AA, Sabo KG, Fente BM, Bezie MM and Seifu BL (2024) The level of wasting and associated factors among children aged 6–59 months in sub-Saharan African countries: multilevel ordinal logistic regression analysis. Front. Nutr. 11:1336864. doi: 10.3389/fnut.2024.1336864
Received: 11 November 2023; Accepted: 22 May 2024;
Published: 06 June 2024.
Edited by:
Juan E. Andrade Laborde, University of Florida, United StatesReviewed by:
Abebew Aklog Asmare, Mekdela Amba University, EthiopiaCopyright © 2024 Asebe, Asmare, Mare, Kase, Tebeje, Asgedom, Hailu Shibeshi, Lombebo, Sabo, Fente, Bezie and Seifu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hiwot Altaye Asebe, aGl3b3RhYmVyYTk2QGdtYWlsLmNvbQ==
†ORCID: Hiwot Altaye Asebe https://orcid.org/0000-0003-3232-2066
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.