- 1PAPRSB Institute of Health Sciences, Universiti Brunei Darussalam, Gadong, Brunei
- 2Sultan Hassanal Bolkiah Institute of Education, Universiti Brunei Darussalam, Bandar Seri Begawan, Brunei
Background: The literature brings to light the unhealthy nutritional habits prevalent among Asian adolescents and their high level of body image dissatisfaction. This study aims to conduct a systematic review of the literature on the effect of nutritional education interventions on their nutritional knowledge and food intake behavior, attitude, practice, and body image.
Methods: We searched relevant published studies in PubMed, Web of Science, Scopus, Science Direct, and Springer using the PICO framework and performed a quality assessment using the 10-point checklist adapted from the National Institutes for Health tool.
Results: The majority of the nutritional education interventions improve unhealthy food intake and body image misperception, particularly on nutritional knowledge/self-efficacy, healthy dietary habits, physical activities, and fruit and vegetable intake. We also found a negative association with excess weight gain, obesity, and unethical weight reduction practices, leading to dissatisfaction with body image.
Conclusion: These interventions can help address dietary problems and body image perception and support the development of future interventions.
1 Introduction
Obesity and excess weight gain are increasingly common issues among adolescents. Unhealthy diet choices and reduced physical activity are also prevalent and lead to a persistent positive energy balance (1). This, in turn, leads to excess weight gain among children and adolescents (2). Adolescents are particularly affected because they have higher nutritional needs as they undergo rapid growth and development. Significant physical, psychological, and social changes occur throughout this formative period of life. However, insufficient intake of essential nutrients such as carbohydrates, proteins, fats, vitamins, and minerals may harm their immediate growth and long-term development. Yet, a troubling pattern emerges where many young individuals, instead of prioritizing nutritious foods, opt for calorie-dense, nutrient-poor foods to meet their food cravings and stave their hunger. According to multiple reports, adolescents are more likely to consume unhealthy foods such as refined carbohydrates (snacks and beverages with added sugar), caffeine, and junk food than they are to consume fruit, milk, and vegetables (3–5). The following evidence highlights this: Most adolescents skip meals frequently, only up to 50% consume fruits and vegetables and use dietary supplements, 13.9% of the total energy intake of Korean adolescents comes from free sugar, significantly higher than the 5% recommended by the World Health Organization (WHO) (6), 53.9% of the beverages consumed contain added sugar, accounting for 20.5% of the daily sugar intake and 12.5% of high school pupils use more caffeine than is advised (7). This preference is what leads to an imbalance in their diet, a situation that can only be rectified through decisive efforts guiding the formulation of effective strategies promoting healthier eating habits.
Moreover, body image misconceptions distort the perception of one’s body and set unrealistic expectations of how one should look. Social media and advertising significantly perpetuate these misconceptions by showing idealized and often unattainable body types. It was reported that 24.2% of adolescents in middle and high school had negative body image issues despite having a normal body mass index (BMI) (8). This negative self-impression of body image may result in severe physical and mental effects (9) and may lead to melancholy, low self-esteem, binge eating, eating disorders, consuming unhealthy foods, and excessive weight loss practices, and this is a growing concern around the world (10, 11). It has been identified as a global problem that transcends geographical boundaries and affects individuals of all income levels and linguistic backgrounds (12, 13). Since proper nutrition is vital in promoting adolescents’ physical and mental health, a multifaceted approach that includes nutritional education and support for individuals struggling with body image is required. It is crucial to encourage a healthy relationship with food, promote self-acceptance, and focus on overall well-being rather than external appearance. Negative attitudes toward food and a distorted body image not only contribute to obesity but also exert a profound influence on an individual’s mental and physical well-being (14). Developing healthy eating habits during adolescence could prevent obesity, type 2 diabetes, cardiovascular disease, and other disorders. They also promote mental alertness and increased cognitive function and catalyze positive thoughts about one’s appearance and self-worth. Nutritional interventions aimed at fighting obesity can also be used to decrease the incidence of excessive food intake and wrong body image assessment.
Nutritional education interventions aim to improve nutrition-related knowledge, attitudes and practices. This provides individuals with skills and information to help them improve their diet, lifestyle, behavior and emotional well-being. Some of the common methods to deliver nutrition education interventions include lectures and counseling. Increasingly, web resources, social media, video-based learning, mobile apps and game-based learning are also being used. In an educational setting, nutritional interventions are integrated into the classroom through nutrition programs, peer education and healthy school meal initiatives. The nutrition curriculum often includes concepts of food production and preparation, healthy eating by making the right food choices, lifestyle modification, and cultural aspects of nutrition. Hands-on assignments include cooking classes, kitchen safety and field trips. Notably, school meal programs typically include the promotion of locally and regionally produced foods or food products, which contributes to a comprehensive approach. The success of these interventional measures depends on the active involvement of parents, the community and teachers, with a focus on a holistic approach.
The literature highlights the unhealthy nutritional habits prevalent among Asian adolescents and multiple cross-sectional studies have identified this subpopulation as exhibiting the highest level of dissatisfaction with their body image. Improving nutritional education interventions would lower the incidence of obesity among them (5). We can further note that many educational interventions have succeeded in addressing unhealthy eating behavior and body image dissatisfaction in a large number of countries. However, to date, there are no studies that systematically review the efficacy of these interventions. This study fills this gap and thoroughly analyzes the impact of various nutritional education interventions on nutritional knowledge and related food intake behavior, attitude and practice, and body image in the Asian young and adolescent population.
2 Materials and methods
We aligned the systematic review methodology with our research goal of exploring the effect of nutritional educational intervention on nutritional knowledge, attitude, practice, and body image in the Asian young and adolescent population. This procedure followed the six-stage technique of a systematic literature review, beginning with the creation of protocols and continuing into eligibility criteria, search strategy, study evaluation, data extraction, and result synthesis.
2.1 Development
The review protocol explains the review’s historical context, the publications chosen for review, and how it tackles publication quality evaluation and data retrieval. We employed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements as recommended for conducting a systematic literature review (15).
2.2 Research question
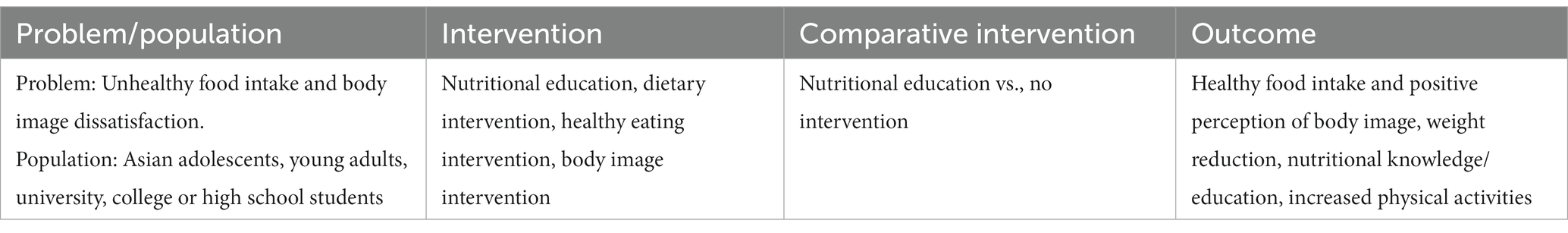
We used the problem/population, intervention, comparison, and outcome (PICO) framework to define the review questions. This framework informs the search string and the search strategy. Table 1 shows the list of terms comprising each of the four components of the PICO framework we have used to frame the two research questions. The review aims to answer two research questions: Research question 1 (RQ1): How does nutritional education intervention affect food intake behavior and its related outcomes? Research question 1 (RQ2): How does nutritional education intervention affect body image perception?
2.3 Search strategy
We selected and then searched five electronic databases PubMed, Web of Science, Scopus, Science Direct, and Springer. The search was conducted on the 17th of March, 2023. Search terms included terms such as ‘nutritional knowledge,’ ‘dietary intervention,’ ‘nutritional knowledge,’ ‘nutritional attitude,’ ‘eating practice,’ ‘body image perception,’ and ‘body image satisfaction’ and different Asian geographical locations. Search terms were combined using Boolean operators “AND” and “OR” in the title and abstract index. The search was limited to articles published between January 2000 and December 2022.
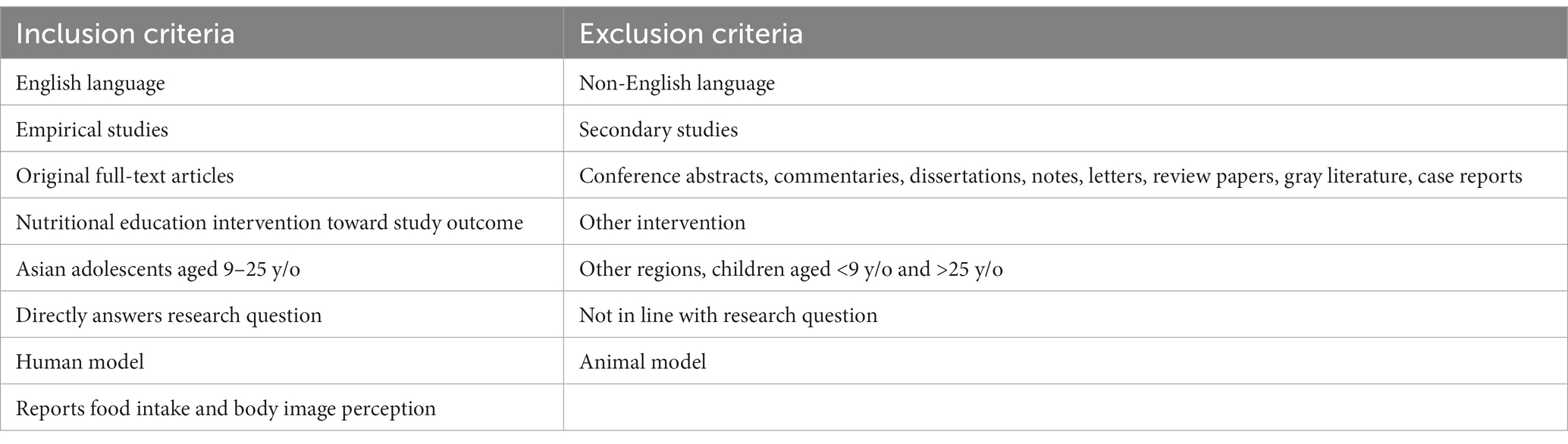
2.4 Eligibility criteria
We defined the criteria for including or excluding retrieved studies. Table 2 shows the inclusion and exclusion criteria. No studies were excluded based on the year of publication.
2.5 Article screening
We employed Covidence screening software to manage and screen the bibliographic data from the five electronic sources. The software automatically excluded duplicate articles. The references were upvoted on the software using the inclusion and exclusion criteria. We examined both article’s title and abstract to determine their alignment with the research objectives. Then we read the full text of the shortlisted papers. Two independent reviewers screened the article’s titles, abstracts, and full text to reduce bias. All eligible articles were thoroughly reviewed, and the discrepancy between the reviewers during the screening was resolved by discussion and consensus.
2.6 Study appraisal
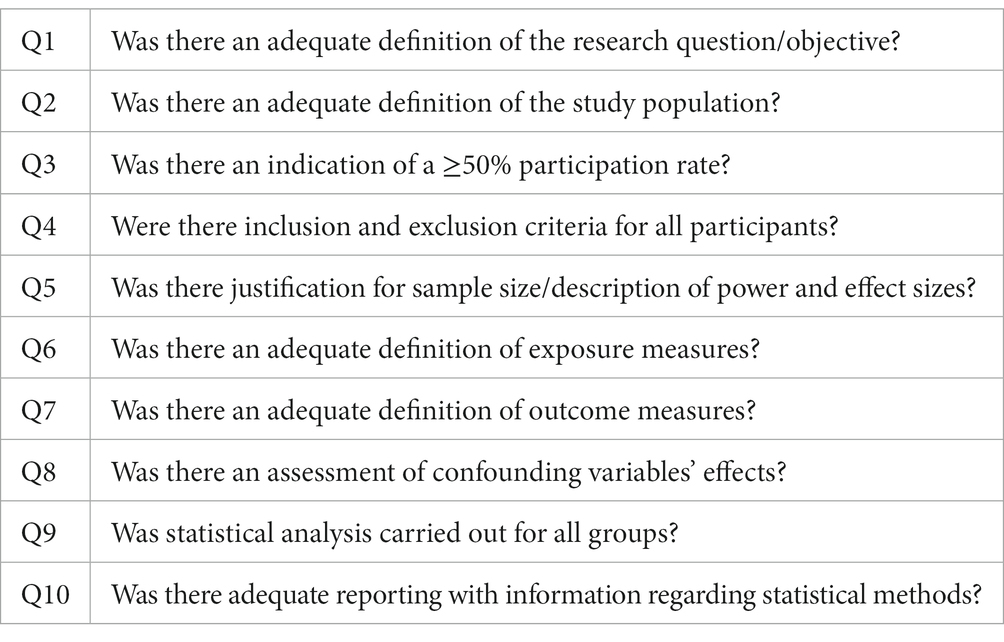
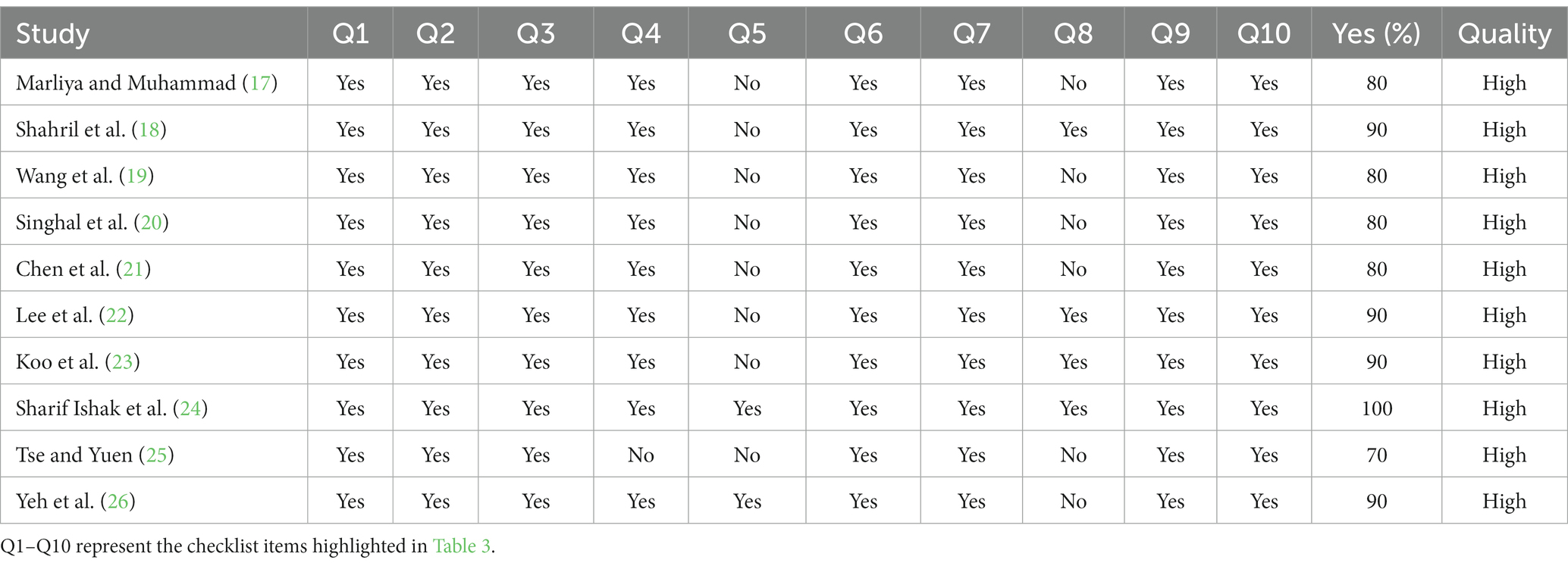
The objective of this appraisal was to evaluate the quality of the articles in terms of their methodology and to address the possibility of bias in their planning, execution, and analysis. Following the inclusion criteria, two critical reviewers conducted a rigorous evaluation of all articles selected for this systematic review. The quality assessment was performed using the 10-point checklist adapted from the National Institutes for Health tool (16) for appraising observational, cohort, and cross-sectional studies. Table 3 shows the 10 items on the checklist considered in this study which help assess the quality of the articles. The 10 items were evaluated using the dichotomous Yes or No rating method. The quality of evaluated studies was subcategorized as high (above 70% of Yes responses), moderately high (50–69% of Yes responses), or low (below 50% of Yes responses), depending on their assessment score.
2.7 Data extraction
Data was extracted from the studies using an electronic data extraction form developed with Microsoft Excel. The characteristics of each study were summarized under various headings, allowing the most important findings to be synthesized. The information extracted includes the following: (i) primary author’s information and affiliations, (ii) publication year, (iii) country, (iv) aim of the article, (v) study design, (vi) sample characteristics including the educational level of the participants, sample size, age and gender, (vii) description of the nutritional interventions used, (viii) duration of the experiment to follow-up period, (ix) method of assessing the intervention outcome, (x) outcome, (xi) statistical analysis, (xii) results, and (xiii) the main findings of the articles. After data extraction, we organized and summarized the article characteristics to answer the systematic review questions.
3 Results
This section presents the selection process of the papers in the systematic review and the results of both the quality assessment and data extraction.
3.1 Study selection
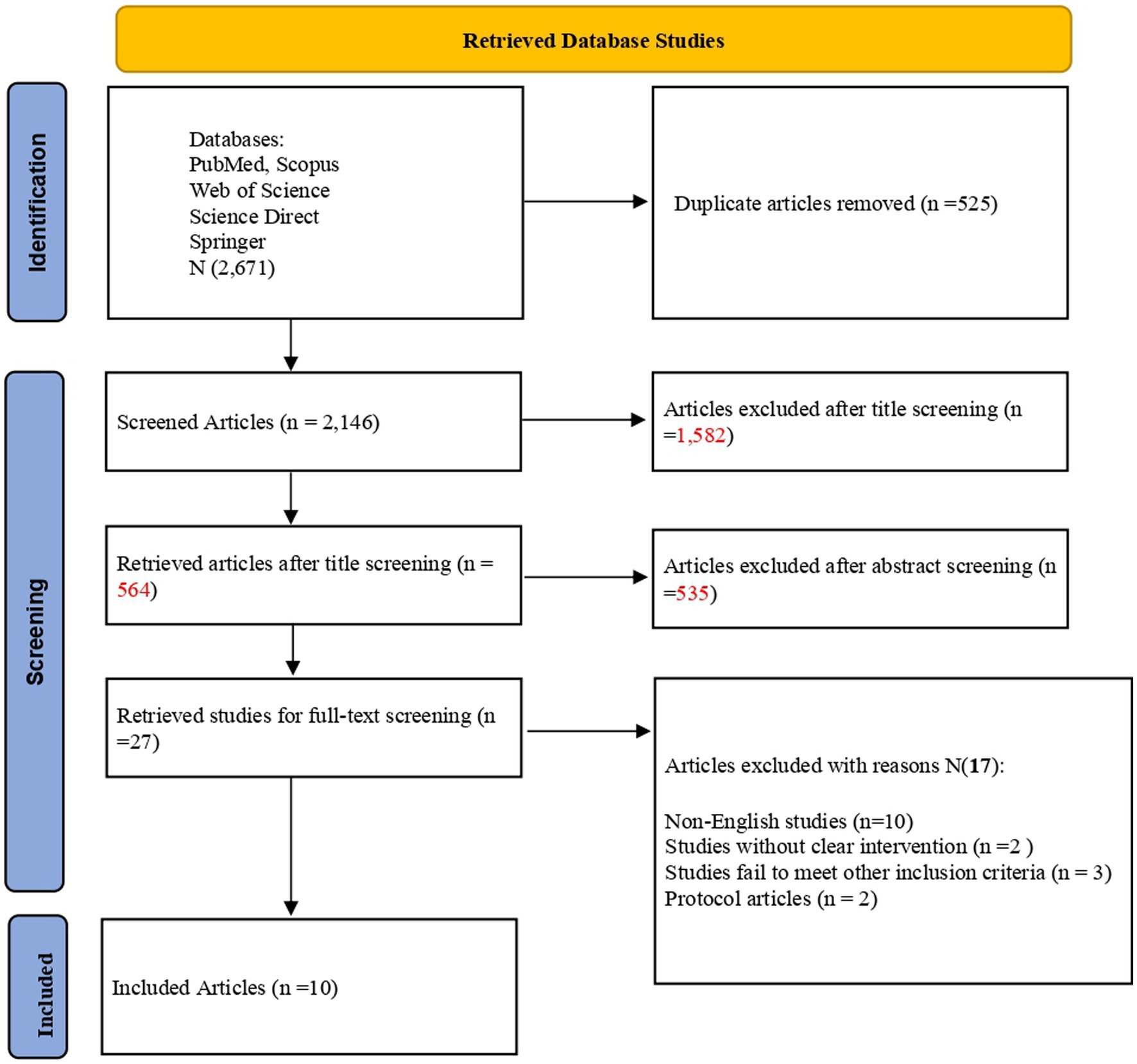
We retrieved 2,671 articles from the five electronic databases and exported them to the Covidence software for reference management. The software excluded 525 duplicate records. Screening the titles and abstracts of the remaining studies disqualified 2,119 articles as they did not align with the research question. Two independent reviewers evaluated the remaining 27 studies and based on the inclusion criteria excluded 17 studies. Finally, 10 articles met the inclusion criteria and were included in the review. Figure 1 displays the PRISMA chart that explains the screening procedure.
3.2 Quality assessment
We evaluated the 10 articles’ methodological and reporting quality. The detailed results are presented in Table 4 as outlined in Section 2.6. All of them obtained a score of more than 70% and thus were of good quality. Only 10% of the articles —one article— met all 10 items on the checklist and therefore scored 100%. Eight studies scored between 80 and 90%, while the remaining two studies scored 70%.
Specifically, we can note that all the studies had a defined research question and an adequate description of the study population, at least 50% of the study population had participated, both the exposure and outcome measures were adequately defined, statistical analysis had been conducted and they all had adequate reporting. As listed in Table 4, all the studies outlined inclusion and exclusion criteria for all participants (17–24, 26) except for Tse and Yuen (25). Conversely, only Sharifa Ishak et al. (24) and Yeh et al. (26) justified the sample size and described power and effect sizes. Finally, only four studies (18, 22–24) included an assessment of confounding variable effects.
3.3 Result synthesis
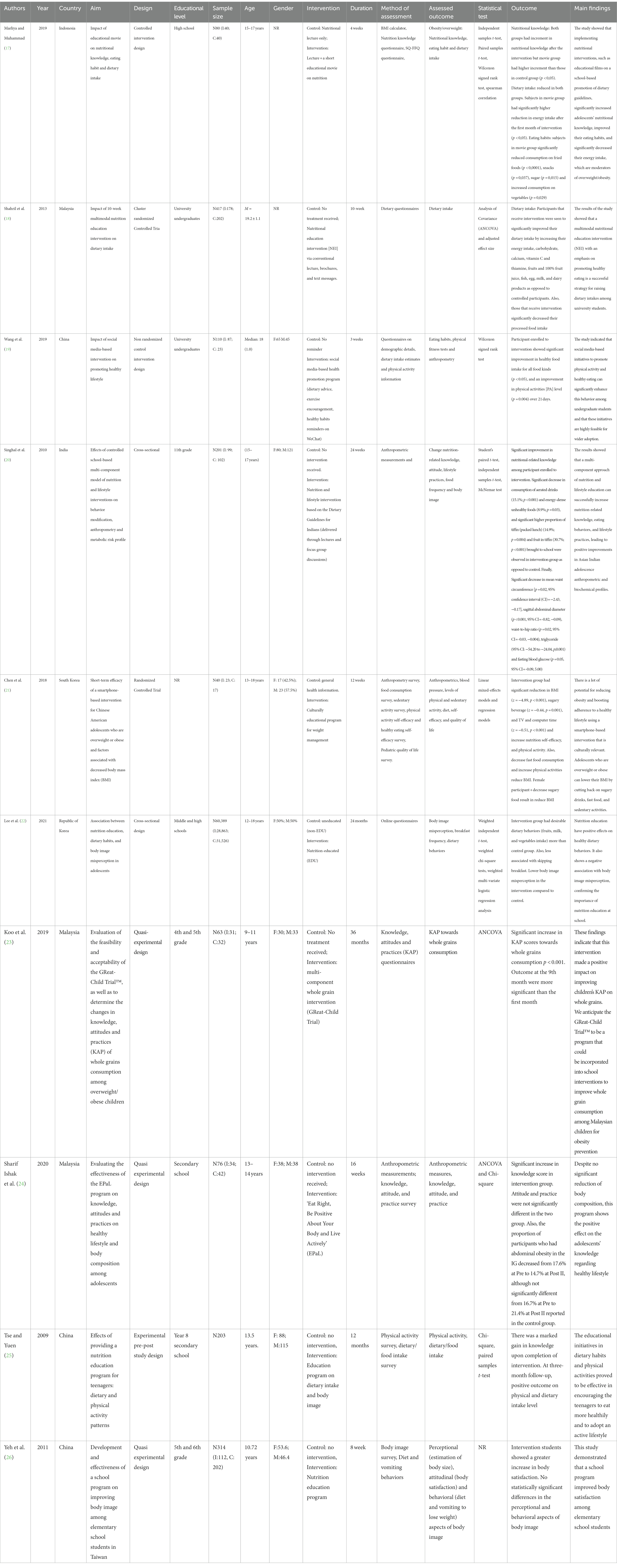
The selected studies covered five Asian countries. Most of the articles examined Malaysian (18, 23, 24) and Chinese adolescents (19, 25, 26), whereas others focused on Korean adolescents (21, 22), Indonesian adolescents (17), and Indian adolescents (20). The studies were published between 2009 and 2021. The study population of the reviewed articles included university undergraduates, middle and high school students, secondary school students, and 4th, 5th, 6th, 8th, and 11th-grade students. All the participants were aged 9–25 years old. Male students who participated in the experiments were slightly older than the female participants.
These studies adopted various study designs like randomized controlled trials (RCT) (17, 21), non-randomized controlled trials (19), cross-sectional (20, 22) quasi-experimental design (23, 24, 26), pre-post study design (25), and cluster RCT (18). Of the 61,893 Asian adolescents enrolled in the different studies, 29,670 participants received nutrition education intervention, whereas 32,223 did not.
The nutritional education interventions covered in the articles were the following: animation movies and lectures (17); a multimodal nutrition education module (18, 20); a WeChat app (19); iStartSmart for teens educational program using an online format consisting of a short video (21) and an e-book (22); GReat-Child Trial™ based on social cognitive theory improved knowledge, attitudes and practices (23); module delivery focused on healthy eating, positive body image, an active lifestyle (24); tailor-made nutritional education (25); and an educational program on body image (26). The duration of the experimental follow-up period varied across the studies, ranging from 3 to 36 weeks after the administration of the intervention.
The outcomes measured in the articles were the following: obesity and weight gain (17), dietary intake habits (18, 25), physical fitness tests (19), anthropometry (19–21, 24), nutritional change and blood pressure (21), sedentary activity (21), self-efficacy and quality of life (21), body image misperception (22), breakfast frequency (22), knowledge-attitude-practice towards whole grain consumption (23), level of physical activity (19, 21, 25) and perceptional, attitudinal, and behavioral aspects of body image (26).
The statistical analyses used by the authors to measure the significance of the outcomes included independent samples t-test (17, 20, 22), paired samples t-test (17, 20, 25), Wilcoxon signed rank test (17, 19), spearman correlation (17), analysis of covariance (ANCOVA) and adjusted effect size (18, 23, 24), McNemar test (20), linear mixed effects models and regress models (21), weighted chi-square test (22, 24), and weighted multivariate logistic regression analysis (22). One included study did not report statistical methods (26).
3.4 Intervention outcome
The interventions reviewed positively affected dietary intake behaviors and were especially effective in reducing the consumption of unhealthy food, thus leading to a reduction in body image misperception. Table 5 lists the 31 different outcomes covered by the 10 articles reviewed by source and a detailed synthesis of results is summarized in Table 6.
3.4.1 Nutritional education intervention and dietary knowledge
Five studies emphasized a significant improvement in dietary/nutritional knowledge among adolescents (17, 20, 21, 24, 25). These studies revealed high levels of knowledge across different areas of diet and nutrition after intervention. The participants demonstrated increased nutritional knowledge of dietary types, attitudes and behavior and physical activities, as well as a new awareness of body image following the intervention. In particular, their new knowledge included information about simple and complex carbohydrates, the concept of empty calories, sources, adverse effects of trans-fat, high-fat dairy products, dietary fiber, refined grains, whole grains, sugary contents, and glucose elevators.
3.4.2 Nutritional education intervention and dietary attitude and practice
All of the articles found interventions to have a significant effect on the nutritional attitudes and practices of Asian adolescents (17–26). These attitudes and practices revolve around healthy food intake behaviors such as increasing the consumption of fruits and vegetables (17–20, 22, 23) and the proportion of fruits in packed lunches brought to school (20), increasing the consumption of healthy carbohydrates, minerals and vitamins, whole grain, and dairy products (18, 20, 23, 25), and reducing the consumption of unhealthy foods (energy-dense, fried, sugary, processed, junk foods, snacks, carbonated drinks and excessive food intake) (17, 18, 20, 21, 25).
There was also a lower exposure to TV and screens, a lower intake of food in canteens, a lower consumption of fast food and a reduction in the number of participants skipping breakfast (20, 21, 23). One study reported that 93% of participants felt happy with the lifestyle changes made after the intervention (21), while another study reported a significant change in knowledge, attitudes, and practice (23). Conversely, one study reported an increase in knowledge but no change in practices and attitudes (24). Another study highlighted that more participants recognized that eating a serving of unhealthy foods would harm their health and thus decrease their intake of food from restaurants, kiosks, and eateries (20).
3.4.3 Nutritional education intervention and physical activity
Five studies identified that nutritional intervention significantly improved adolescent physical activity levels (19–22, 25). Reported physical activity included increasing the duration of quiet squats (19) and plank time (19), as well as incorporating 30–60 min of physical activity per day or participating in physical activity more than 4 days per week (20). These adolescents demonstrated less sedentary lifestyles, more hours of exercise (25), and more participation in household chores (25). There was also a significant increase in the number of adolescents who walked instead of taking transport as an activity (25).
3.4.4 Nutritional education intervention and body weight
Four studies highlighted the significant effect of a nutritional education intervention on adolescents’ body weight and its associated factors (20, 21, 23, 24). According to these studies, nutritional education interventions significantly reduced sagittal abdominal diameter (20), abdominal obesity (24), body mass index (21), fasting blood glucose level (20), waist circumference, and waist-to-hip ratio, which significantly altered anthropometry, body composition, and metabolic parameters (20). In another study, more participants correctly identified their body size at pre-intervention, post-intervention, and 3 months after the intervention (26).
3.4.5 Nutritional education intervention and body image
Several studies demonstrated lower body image misperception (23) and a significant increase in body image satisfaction 3 months after intervention (26). Surprisingly, no significant difference in the scores for vomiting behavior post-food intake was reported (26). An article reported slightly higher overall satisfaction with physical appearance and fewer participants who avoided clothes that made them look overweight (20).
4 Discussion
The systematic literature review analyzed the findings of 10 articles retrieved from five electronic databases—PubMed, Web of Science, Scopus, Science Direct, and Springer—which focus on the impact of nutritional education interventions on nutritional knowledge and related food intake behavior, attitude, practice, and body image among the Asian young and adolescent population. The PICO framework was used to formulate the review questions, ensuring a focused and systematic research strategy. All the articles met the inclusion criteria and were checked for methodological quality using the National Institutes for Health tool. The guidelines of the PRISMA and Cochrane were thoroughly followed.
The studies cover very different interventions and outcomes, but because of this diversity and the high degree of overlap between them, we can infer meaningful conclusions. We explored multiple interventions of nutrition education, including lectures, movies, social media, text messages and notes (17–19). These interventions impacted key factors such as nutritional knowledge/self-efficacy, healthy dietary habits, physical activity, and fruit and vegetable intake. The reviewed studies demonstrate the potential of nutritional educational interventions to address dietary problems and body image challenges during childhood and adolescence. No distinction due to age was observed, despite taking into account a wide age span.
Such interventions affected food intake behaviors and their related outcomes (RQ1). They improved dietary and nutritional knowledge (17, 20, 21, 24, 25). Empowering adolescents with accurate and relevant nutritional knowledge enables them to make informed dietary choices, resulting in healthier eating patterns. They effectively improved dietary attitudes and practices, leading to increased consumption of nutritious foods and reduced intake of unhealthy options. Many of the nutritional educational interventions also positively influenced physical activity levels among participants. Several studies showed that post-intervention participants had increased physical activity duration and decreased sedentary behavior. This is consistent with previous research which shows that nutritional interventions significantly enhance both physical activity and literacy (27–29). Physical activity is critical in maintaining overall health and preventing obesity and related health issues, making this an important benefit of the interventions. Enhanced literacy skills are crucial in understanding and applying nutritional knowledge, fostering a comprehensive approach to health.
Furthermore, the review found that the interventions significantly reduced obesity and weight gain among Asian adolescents through better food choices, healthier eating habits, and more physical activity. The studies showed a correlation between nutritional education and improved body mass index, waist circumference, and other anthropometric measures (20). Beyond weight loss, the focus is on enhancing overall well-being, recognizing that comprehensive health extends beyond weight management. These anthropometric measures are vital indicators of overall health and well-being. With well-structured nutritional education interventions, adolescents are encouraged to make better dietary decisions, leading to a better long-term lifestyle with less obesity (1, 2) and related disease risk.
The findings also suggested that nutritional education interventions affected body image perception (RQ2). They reduced misperception and increased satisfaction with body image among Asian adolescents (22, 23). These interventions have the potential to address unrealistic ideals and focus on long-term approaches that can reinforce positive mindset changes. Thus, they could be crucial in improving the overall health and well-being of Asian adolescents.
Future policymaking could draw from the findings of this review. In particular, this research underscores the importance of incorporating nutritional education programs in schools, universities, and other educational settings. It demonstrates that interventions can impact adolescents’ eating habits and body image perceptions, setting the foundation for a healthier future if proper education is provided at an early growing phase of development.
Increased awareness, literacy and knowledge about diets, as well as groundwork that empowers and encourages families to get involved, can reinforce the effectiveness of educational interventions. The research showed that creating supportive environments and providing practical tools that enable behavioral changes is crucial, leading to improved overall health and reduced risk of diet-related diseases (4). Well-structured interventions must educate adolescents to understand and interpret nutrition information on food packaging, as well as provide them with a new understanding of the long-term consequences of unhealthy food intake. An effective intervention will also promote behavioral change techniques that help adolescents set goals, plan their meals, and track their progress. Group-based educational interventions can encourage adolescents to adopt healthier eating habits with the support of their peers.
Nutritional knowledge does not always translate into behavioral change, as significant shifts in behavior often demand a multidisciplinary approach. This is consistent with the findings of Yun and colleagues, who demonstrated that although all students from the University Brunei Darussalam knew the importance of a balanced diet, more than 50% of the students skipped breakfast and consumed fried food at least three times a week (30). Hence, the university was encouraged to form a multi-disciplinary team to be responsible for designing and conducting various programs to promote physical activity and reduce unhealthy eating habits.
It is important to note that program design and mode of administration will dictate the effectiveness of any nutritional education intervention. In this sense, continued evaluation of these programs is essential. Interventions must be well targeted in terms of the recipient population and time frame. A regular and repetitive intervention (20) of adequate duration (24) seems to achieve better results. Some studies even suggest that customized nutrition education programs are needed in the future (18). The use of innovative technology specifically adapted to young people such as movies (17), text messaging (18), or mobile apps (19) can be useful from the point of view of participant satisfaction and to increase adherence rates. As such, peer education might be helpful to boost both (24). These innovative solutions are also generally cost-effective, scalable and easy to implement (19). If the intervention is to be successful, it is essential to target feasible objectives and to use clear, simple, and culturally appropriate messages (18, 21). It is also worth mentioning that nutritional interventions aimed at addressing obesity should never conflict with any negative effects on body image (26).
Apart from the large number of interventions and outcomes considered in the present review which demonstrate the potential of nutritional education interventions to address dietary problems and body image, other strengths of the reviewed studies include the fact that some of these innovative solutions have been explored and, overall, have shown positive compliance and a generally high rate of satisfaction, novel data have been collected, and a wide range of different methodological designs supported by robust statistical analysis have been implemented. As a matter of fact, our quality assessment yielded very good results, and all the reviewed articles were rated above 80%. Altogether, this provides a solid basis for future developments.
Notwithstanding the many merits of the methodologies used in the reviewed articles, some limitations emerge. These limitations may affect the generalization of the results, such as the use of relatively small sample sizes (17, 21), homogeneous samples (21), or unbalanced samples across genders (18), or focusing on a specific population (17, 24). They may affect the precision of measurement. For example, self-reported measures may have introduced potential biases (18, 22, 23), it was not possible to assess the quality of education or to ensure that it was provided equally in all cases (22, 24) and one study notes that it may be necessary to keep working on the design of a reliable measure of body image (26). These limitations may also threaten the study’s validity as some experimental designs did not involve random allocation in the intervention and control groups (19, 24, 26). Moreover, potential contamination bias may have occurred (26) and the use of non-blinded methods may have overestimated intervention effects (23). The cross-sectional nature of the study is also acknowledged (19) and some articles agree on the need to conduct future longitudinal designs to assess long-term effects (18).
Further research is needed to validate the benefits of current educational material and to further explore other innovative technologies such as game-based interventions. Furthermore, it would be highly desirable to have more evidence of the suitability and effectiveness of the programs in terms of target population, duration, participation, adherence rates or mode of administration. More empirical analyses of longitudinal data are needed to test the long-run effects of nutrition education interventions in schools, universities and other educational settings and whether they improve eating habits and good health later in life. Finally, further research is needed to investigate the factors that lead to behavior change. While have found that there is consistent evidence of correlations between nutrition knowledge and food intake and body image, we are aware it is also important to consider the different ways in which correlations between nutritional education and food intake or body image may arise.
5 Conclusion
This systematic review highlights the impact of nutritional education interventions on improving the overall health and well-being of Asian adolescents by promoting healthier food choices and fostering positive body image perceptions. We strongly recommend continuing efforts to integrate nutritional education programs into educational settings to combat adolescent obesity and related health issues effectively, with a multidisciplinary approach in mind. Further research is needed to investigate the factors that lead to behavior change. While we found that there is consistent evidence of correlations between nutrition knowledge and food intake and body image, we are aware it is also important to consider the different ways in which correlations between nutritional education and food intake or body image may arise. The results of this study emphasize the importance of nutrition education for Asian adolescents to promote healthier choices and maintain a positive body image. Integrating nutrition education into an educational setting is therefore a proactive step to address these issues comprehensively. The far-reaching implications of this research are recommendations for policymakers, educators and healthcare providers. If implemented effectively, nutrition education could significantly improve the health and well-being of Asian adolescents.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
BP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Writing – original draft. SNA: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing. SS: Conceptualization, Methodology, Supervision, Validation, Writing – review & editing. ZM: Supervision, Validation, Writing – review & editing. SRA: Conceptualization, Formal analysis, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The article processing fee was sponsored by Univerisiti Brunei Darussalam.
Acknowledgments
The authors would like to thank the Universiti Brunei Darussalam (UBD).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
10 References
1. D’Addesa, D, D’Addezio, L, Martone, D, Censi, L, Scanu, A, Cairella, G, et al. Dietary intake and physical activity of normal weight and overweight/obese adolescents. Int J Pediatr. (2010) 2010:785649. doi: 10.1155/2010/785649
2. Pereira, HRC, Bobbio, TG, Antonio, MRGM, and Barros Filho, ADA. Childhood and adolescent obesity: how many extra calories are responsible for excess of weight? Rev Paul Pediatr. (2013) 31:252–7. doi: 10.1590/s0103-05822013000200018
3. National Center for Chronic Disease Prevention and Health Promotion (U.S.). Comprehensive framework for addressing the school nutrition environment and services. Atlanta: Centers for Disease Control and Prevention (2019).
4. Cunha, CM, Costa, PRF, de Oliveira, LPM, Queiroz, VAO, Pitangueira, JCD, and Oliveira, AM. Dietary patterns and cardiometabolic risk factors among adolescents: systematic review and meta-analysis. Br J Nutr. (2018) 119:859–79. doi: 10.1017/s0007114518000533
5. Vanhelst, J, Beghin, L, Duhamel, A, De Henauw, S, Ruiz, JR, Kafatos, A, et al. Do adolescents accurately evaluate their diet quality? The HELENA study. Clin Nutr. (2017) 36:1669–73. doi: 10.1016/j.clnu.2016.10.019
6. World Health Organization. Guideline: sugars intake for adults and children. Geneva: World Health Organization (2015).
7. Park, JH, Hahm, M-I, Kim, SJ, and Min, IS. Association between high-caffeine energy drink intake and suicidal ideation in Korean adolescents. J. Korean Soc. Sch. Health. (2016) 29:71–80. doi: 10.15434/kssh.2016.29.2.71
8. So, ES. Perceptual body image and the relationship with weight control across the adult lifespan by sex in Koreans. J Public Health. (2017) 39:777–86. doi: 10.1093/pubmed/fdx021
9. Griffiths, S, Murray, SB, Bentley, C, Gratwick-Sarll, K, Harrison, C, and Mond, JM. Sex differences in quality-of-life impairment associated with body dissatisfaction in adolescents. J Adolesc Health. (2017) 61:77–82. doi: 10.1016/j.jadohealth.2017.01.016
10. Patton, GC, Sawyer, SM, Santelli, JS, Ross, DA, Afifi, R, Allen, NB, et al. Our future: a lancet commission on adolescent health and wellbeing. Lancet. (2016) 387:2423–78. doi: 10.1016/S0140-6736(16)00579-1
11. Baker, JH, Higgins Neyland, MK, Thornton, LM, Runfola, CD, Larsson, H, Lichtenstein, P, et al. Body dissatisfaction in adolescent boys. Dev Psychol. (2019) 55:1566–78. doi: 10.1037/dev0000724
12. Van den Berg, P, Paxton, SJ, Keery, H, Wall, M, Guo, J, and Neumark-Sztainer, D. Body dissatisfaction and body comparison with media images in males and females. Body Image. (2007) 4:257–68. doi: 10.1016/j.bodyim.2007.04.003
13. Bornioli, A, Lewis-Smith, H, Smith, A, Slater, A, and Bray, I. Adolescent body dissatisfaction and disordered eating: predictors of later risky health behaviors. Soc Sci Med. (2019) 238:112458. doi: 10.1016/j.socscimed.2019.112458
14. Haines, J, and Neumark-Sztainer, D. Prevention of obesity and eating disorders: a consideration of shared risk factors. Health Educ Res. (2006) 21:770–82. doi: 10.1093/her/cyl094
15. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
16. Study Quality Assessment Tools (2013). Available at: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
17. Marliya, M, and Muhammad, HFL. Introducing the new nutrition guideline to Indonesian overweight/obese adolescents using a short movie: the impact on nutritional knowledge, eating habit and dietary intake. Prog Nutr. (2019) 21:227–33. doi: 10.23751/pn.v21i1-S.5944
18. Shahril, MR, Wan Dali, WPE, and Lua, PL. A 10-week multimodal nutrition education intervention improves dietary intake among university students: cluster-randomised controlled trial. J Nutr Metab. (2013) 2013:658642. doi: 10.1155/2013/658642
19. Wang, M, Guo, Y, Zhang, Y, Xie, S, Yu, Z, Luo, J, et al. Promoting healthy lifestyle in Chinese college students: evaluation of a social media-based intervention applying the RE-AIM framework. Eur J Clin Nutr. (2021) 75:335–44. doi: 10.1038/s41430-020-0643-2
20. Singhal, N, Misra, A, Shah, P, and Gulati, S. Effects of controlled school-based multi-component model of nutrition and lifestyle interventions on behavior modification, anthropometry and metabolic risk profile of urban Asian Indian adolescents in North India. Eur J Clin Nutr. (2010) 64:364–73. doi: 10.1038/ejcn.2009.150
21. Chen, JL, Guedes, CM, and Lung, AE. Smartphone-based healthy weight management intervention for Chinese American adolescents: short-term efficacy and factors associated with decreased weight. J Adolesc Health. (2019) 64:443–9. doi: 10.1016/j.jadohealth.2018.08.022
22. Lee, JH, Lee, HS, Kim, H, Kwon, YJ, Shin, J, and Lee, JW. Association between nutrition education, dietary habits, and body image misperception in adolescents. Asia Pac J Clin Nutr. (2021) 30:512–21. doi: 10.6133/apjcn.202109_30(3).0018
23. Koo, HC, Poh, BK, and Ruzita, AT. GReat-child trial™ based on social cognitive theory improved knowledge, attitudes and practices toward whole grains among Malaysian overweight and obese children. BMC Public Health. (2019) 19:1574. doi: 10.1186/s12889-019-7888-5
24. Sharif Ishak, SIZ, Chin, YS, Taib, M, Nasir, M, Chan, YM, and Shariff, ZM. Effectiveness of a school-based intervention on knowledge, attitude and practice on healthy lifestyle and body composition in Malaysian adolescents. BMC Paediatr. (2020) 20:122. doi: 10.1186/s12887-020-02023-x
25. Tse, MMY, and Yuen, DTW. Effects of providing a nutrition education program for teenagers: dietary and physical activity patterns. Nurs Health Sci. (2009) 11:160–5. doi: 10.1111/j.1442-2018.2009.00443.x
26. Yeh, MC, Liou, YM, and Chien, LY. Development and effectiveness of a school programme on improving body image among elementary school students in Taiwan. J Adv Nurs. (2012) 68:434–43. doi: 10.1111/j.1365-2648.2011.05735.x
27. Beets, MW, Beighle, A, Erwin, HE, and Huberty, JL. After-school program impact on physical activity and fitness: a meta-analysis. Am J Prev Med. (2009) 36:527–37. doi: 10.1016/j.amepre.2009.01.033
28. Pate, RR, and O'Neill, JR. After-school interventions to increase physical activity among youth. Br J Sports Med. (2009) 43:14–8. doi: 10.1136/bjsm.2008.055517
29. Egan, CA, Webster, CA, Stewart, GL, Weaver, RG, Russ, LB, Brian, A, et al. Case study of a health optimizing physical education-based comprehensive school physical activity program. Eval Program Plann. (2019) 72:106–17. doi: 10.1016/j.evalprogplan.2018.10.006
Keywords: nutritional education, body image, Asian adolescents, perception, diet, food intake
Citation: Pushpa BS, Abdul Latif SN, Sharbini S, Murang ZR and Ahmad SR (2024) Nutrition education and its relationship to body image and food intake in Asian young and adolescents: a systematic review. Front. Nutr. 11:1287237. doi: 10.3389/fnut.2024.1287237
Edited by:
Mona Vintilă, West University of Timișoara, RomaniaReviewed by:
Hurtado José Antonio, University of Alicante, SpainRahayu Indriasari, Hasanuddin University, Indonesia
Arlette Setiawan, Padjadjaran University, Indonesia
Copyright © 2024 Pushpa, Abdul Latif, Sharbini, Murang and Ahmad. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Baladandapla Shivappa Pushpa, MjJoODkwNkB1YmQuZWR1LmJu
 Baladandapla Shivappa Pushpa
Baladandapla Shivappa Pushpa Siti Norhedayah Abdul Latif
Siti Norhedayah Abdul Latif Sharimawati Sharbini
Sharimawati Sharbini Zaidah Rizidah Murang
Zaidah Rizidah Murang Siti Rohaiza Ahmad
Siti Rohaiza Ahmad