
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 23 January 2024
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1302323
This article is part of the Research TopicChallenges, Opportunities, and Actions for Improved Maternal and Child NutritionView all 10 articles
 Leonie Burgard1
Leonie Burgard1 Sara Jansen2
Sara Jansen2 Clarissa Spiegler1
Clarissa Spiegler1 Anna-Kristin Brettschneider2
Anna-Kristin Brettschneider2 Andrea Straßburg1
Andrea Straßburg1 Ute Alexy3
Ute Alexy3 Stefan Storcksdieck genannt Bonsmann1
Stefan Storcksdieck genannt Bonsmann1 Regina Ensenauer2
Regina Ensenauer2 Thorsten Heuer1*
Thorsten Heuer1*Background: Nutrition in the first years of life is a cornerstone for child development and long-term health, yet there is a lack of current data on energy and nutrient intake among toddlers and preschoolers in Germany.
Objective: To analyze energy and nutrient intake in toddlers (1- to 2-year-olds) and preschoolers (3- to 5-year-olds) in Germany and compare the results with the Dietary Reference Values (DRVs) by the European Food Safety Authority.
Design: Dietary intake was assessed by weighed food record data (3 + 1 day) of 890 children from the representative cross-sectional Children’s Nutrition Survey to Record Food Consumption (KiESEL), carried out in 2014–2017 as a module of the German Health Interview and Examination Survey for Children and Adolescents Wave 2. For the calculation of energy and nutrient intake, the German Nutrient Database BLS 3.02, LEBTAB, and a supplement database were used.
Results: Median intakes of energy and most nutrients met or exceeded the DRVs in both toddlers and preschoolers. However, low intakes relative to DRVs were found for vitamin D (6–9% of DRV, including supplements) and iodine (57–65% of DRV). Age specific downward deviations were observed for iron intake in toddlers (75% of DRV) and for calcium intake in preschoolers (67–77% of DRV). In contrast, intakes were high for saturated fatty acids (SFA) (14–16 E%), mono-/disaccharides (60–87 g/day), and protein [2.1–2.6 g/(kg body weight*day)].
Conclusion: Nutrient imbalances in toddlers and preschoolers in Germany, which are partly age-related, give rise to concern. Research is needed to determine if routine vitamin D supplementation should be extended beyond infancy. Public health efforts to increase the rate of use of iodized salt and to reduce the intake of SFA and mono-/disaccharides in children’s diets are to be strengthened.
Nutrition is a key factor in child development (1), substantially influencing not only physical but also mental and cognitive health (2). Moreover, early life nutrition has been found to have long-term effects on health, which include modulating the risk for non-communicable diseases such as obesity, diabetes mellitus, and cardiovascular disease (3, 4). At the same time, young children are particularly vulnerable to nutrient deficiencies, as nutrient requirements per kg body weight are high (5). In the midst of the overweight and obesity pandemic in the European Region, affecting an estimated 7.9% of children under the age of 5 and 29.5% of children aged 5 to 9 years (6), excessive energy and macronutrient intake appears to be accompanied with micronutrient deficiencies (7).
While the European Food Safety Authority (EFSA) has identified vitamin D, iron, and – in some countries – iodine as critical micronutrients among infants and young children below the age of 3 years (8), there is no such scientific opinion referring to critical nutrients in preschoolers. However, vitamin D and iodine are likely to be critical nutrients in older children as well, as an evaluation of the German food-based dietary guidelines for children and adolescents demonstrated that even adherence to the recommendations does not ensure adequate vitamin D and iodine intake (9).
Considering the long-term nature of nutrition-associated health consequences, the promotion of optimal nutrient intake in the earliest stages of life is pivotal. This in turn requires a comprehensive understanding of the various phases of child nutrition throughout early development and of potential levers for improvement. Yet, the last national dietary survey analyzing food consumption and nutrient intake in toddlers and preschoolers in Germany was the VELS study, carried out in children aged 1–4 years from 2001 to 2002 (10).
The Children’s Nutrition Survey to Record Food Consumption (Kinder-Ernährungsstudie zur Erfassung des Lebensmittelverzehrs, KiESEL), conducted between 2014 and 2017, offers the most recent representative data on food consumption for children aged 6 months to 5 years in Germany (11). Based on the KiESEL data, this study’s objective is to assess whether energy and nutrient intake in children aged 1–5 years in Germany comply with the Dietary Reference Values (DRVs) by EFSA (12). Furthermore, the study seeks to explore differences in nutrient intake specific to sex and age group, i.e., toddlers and preschoolers.
KiESEL is a representative cross-sectional study performed by the German Federal Institute for Risk Assessment (Bundesinstitut für Risikobewertung, BfR) from 2014 to 2017. Originally, the study was designed to obtain current data on children’s food consumption for exposure assessment (11). Subsequent analysis of data on nutrient intake was performed by the Max Rubner-Institut (MRI). The study is a module of the German Health Interview and Examination Survey for Children and Adolescents Wave 2 (Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland Welle 2, KiGGS Wave 2), which is part of the national health monitoring by the Robert Koch Institute (11). KiESEL was approved by the ethics committee of the Berlin Chamber of Physicians (Eth–28/13). Written informed consent was obtained from the primary caregiver of each child enrolled in the study. KiESEL was further approved by the German Federal Commissioner for Data Protection and Freedom of Information. To ensure adherence to the quality standards in nutritional epidemiology, the STROBE-nut reporting guidelines were used during manuscript preparation (13) (Supplementary Table 1).
The KiESEL sample was randomly selected from the gross sample of KiGGS Wave 2 (11). The sample of KiGGS Wave 2 was drawn from official residency registries of 167 representative German cities and municipalities originally chosen for the KiGGS baseline study (14). The total KiESEL sample includes n = 1104 children aged 0.5–5 years (11). The present analyses refer to a subsample of children aged ≥1 to ≤5 years (n = 890), after excluding children with missing food record data (n = 96) and infants aged ≥6 to ≤11 months (n = 118), as this age group is subject to a separate analysis. A participant flow chart is provided in Supplementary Figure 1. Children were assigned to two age groups based on their age at the beginning of data collection, namely toddlers (≥1 to ≤2 years) and preschoolers (≥3 to ≤5 years). Owing to the time lag between recruitment and data collection, the group of preschoolers additionally included n = 62 (6.2%) children aged 6 years. Note that all age specifications refer to completed years of life, e.g., the age group “1 year” refers to children aged 1.0–1.9 years. The KiESEL study design and survey protocol are reported elsewhere (11, 14).
Dietary assessment included a parent-administered food record, which was conducted on three consecutive days plus one independent day, scheduled 2–16 weeks later (3 + 1 design). To facilitate data collection, parents received face-to-face instructions during an initial home visit. They were provided with digital kitchen scales and a journal with pre-printed log pages explicitly inquiring about specific details of the foods and beverages consumed (e.g., preparation method, brand) and the place and time of the respective eating occasion. In cases where weighing was unfeasible, consumed amounts were estimated using package labels, household measures, or the KiESEL picture book visualizing different portion sizes. In child day-care facilities, a simplified food record was completed. If ambiguities were found in the protocol entries, the parents were contacted for clarification (11).
Data collection in KiESEL also included anthropometric measurements and a standardized questionnaire on nutritional behavior including a food propensity questionnaire, e.g., on seldomly eaten foods, which were performed by trained nutritionists during the home visit (11). To characterize the study population, data on socioeconomic status (SES) collected in KiGGS Wave 2 were used. The categories low, medium, and high SES reflect parental level of education, employment status, and income (equally weighted).
Amounts of human milk were estimated based on the age of the child and the frequency of feeding. Following the approach by Briefel et al. (15), the amount of human milk per feed was set at 89 ml for children aged 12–17 months and at 59 ml for children aged ≥18 months. The maximum daily human milk consumption observed in this KiESEL sub-sample was considered plausible, hence no upper daily limits were applied.
For the calculation of energy and nutrient intake, the food record data were either linked to the German Food Composition Database (Bundeslebensmittelschlüssel, BLS), version 3.02 (16), or to LEBTAB (17), considering all details of a food item as specified in the protocols (e.g., preparation method, brand). LEBTAB is a food composition database that contains a wide range of foods intended for infants and young children, such as follow-on formula or fortified toddler cereals. As far as included in the BLS, fortification of other foods, e.g., fruit juices and cereals, was also accounted for. Data on vitamin A are provided as retinol equivalents, vitamin E as α-tocopherol equivalents, vitamin K as phylloquinone, niacin as niacin equivalents, and folate/folic acid as folate equivalents.
The use of supplements was recorded using a free-text box within the food record (14). When the quantity and/or dosage of a supplement was not specified, amounts were derived as median from comprehensive protocol entries, referring to similar products in children of the same age. Protocol entries were linked to a supplement database (18), which was developed by the BfR and complemented by the MRI. To incorporate both dietary supplements and medicinal products such as vitamin D preparations for the prevention of rickets, the generic term “supplements” is used. The term “vitamin D-containing supplements” refers to all supplement preparations in which vitamin D has been specified as a component, i.e., mono and combination preparations with vitamin D. With the exception of vitamin D, nutrient intake from supplements was not considered in the analyses.
Following the EFSA protocol (19), misreporting of energy intake was identified using the Goldberg cut-off method updated by Black. Children aged ≥1 to ≤3 years were assigned a Physical Activity Level (PAL) of 1.4 and those ≥4 years a PAL of 1.6. Basal metabolic rate was calculated with the Schofield equations as a function of the child’s age, sex, height, and body weight (19). The ratio of reported energy intake to estimated basal metabolic rate was compared to calculated cut-off values (Supplementary Table 2). In line with the EFSA recommendation, under- and over-reporters were not excluded as this would introduce unknown bias (19).
A weighting factor was applied to approximate the sample’s sociodemographic structure to that of the German population. The weighting factor was developed by the Robert Koch Institute for the total KiESEL sample based on the factors sex, age, region, regional structure (e.g., rural area, large city), and household education level, fitted to data from official statistics (Microcensus 2015, except for household educational level Microcensus 2013 (20)).
For statistical analyses, the software SAS, version 9.4 (SAS Institute, Inc., Cary, NC, USA), was used. Statistical measures of energy and nutrient intake of the sample [median, 95% confidence interval (CI) of the median, and the 5th and 95th percentiles (hereafter P5 and P95, respectively)] were calculated from individual values derived as the mean of all protocol days per child. As nutrient intake distributions are frequently skewed, medians were calculated for each age group instead of means. Significant differences were identified by non-overlapping 95% CIs of medians for metric data and by chi-square tests (α = 0.05) for categorical data.
The DRVs by EFSA were used as measures for comparison (Supplementary Tables 3, 4). Intakes were additionally displayed as % of DRVs (median, interquartile range, minimum, maximum), derived from the individual intakes as % of sex- and age-specific DRV. In some cases, more than one DRV was applied for one KiESEL age group. For example, this was necessary for calcium, as the DRVs for calcium refer to 1- to 3-year-olds and to 4- to 10-year-olds, while the KiESEL age groups refer to 1- to 2-year-olds and to 3- to 5-year-olds.
Wherever possible, this report refers to the Population Reference Intake (PRI). In cases where PRIs have not yet been established, the Adequate Intake (AI) was used. Both are designed to cover the requirements of nearly all healthy individuals in a given reference population (12). Thus, an individual intake below a given reference value does not necessarily indicate an actual deficit but rather an increased probability of inadequate intake. Moreover, it should be noted that DRVs for young children are often derived from extrapolations from other age groups due to lacking data (21). DRVs for energy are provided as Average Requirements (ARs), whereas those for fat and carbohydrates are set as Reference Intake Ranges for Macronutrients (RIs) (12).
The characteristics of the sample are described in Table 1. Compared to medium and high SES, the lowest proportion of children came from families with a low SES (<15%). Regarding misreporting of energy intake, 5.6% of parents were identified as under-reporters and 1.1% as over-reporters of their children’s food consumption. Supplement use was frequent only in 1-year-olds, with supplement use being reported for one in three at least once during the protocol period (Table 2). Among those, vitamin D-containing supplements were most commonly administered.
Daily energy and nutrient intakes in toddlers and preschoolers are depicted in Tables 3, 4. Median daily energy intakes were in the range of the respective sex- and age-specific ARs for both toddlers and preschoolers (Supplementary Table 3 and Table 3). With regard to intakes expressed as % of DRVs (Supplementary Table 4 and Figures 1, 2), protein intakes per kg body weight corresponded to about 2.5 times the PRIs in both toddlers and preschoolers, while carbohydrate intakes were within the RIs (Supplementary Table 4 and Table 3). Fat intakes were below the RI in toddlers but not in preschoolers. Also, median fiber intakes in toddler girls (but not in toddler boys) and preschoolers fell short of the DRVs and corresponded to 85 and 90% of the AIs, respectively. Mono-/disaccharides accounted for about half the total carbohydrate intake and made up approximately a quarter of the total energy intake (Table 3). Regarding fatty acids, SFA contributed to about 15 percent of energy intake (E%).
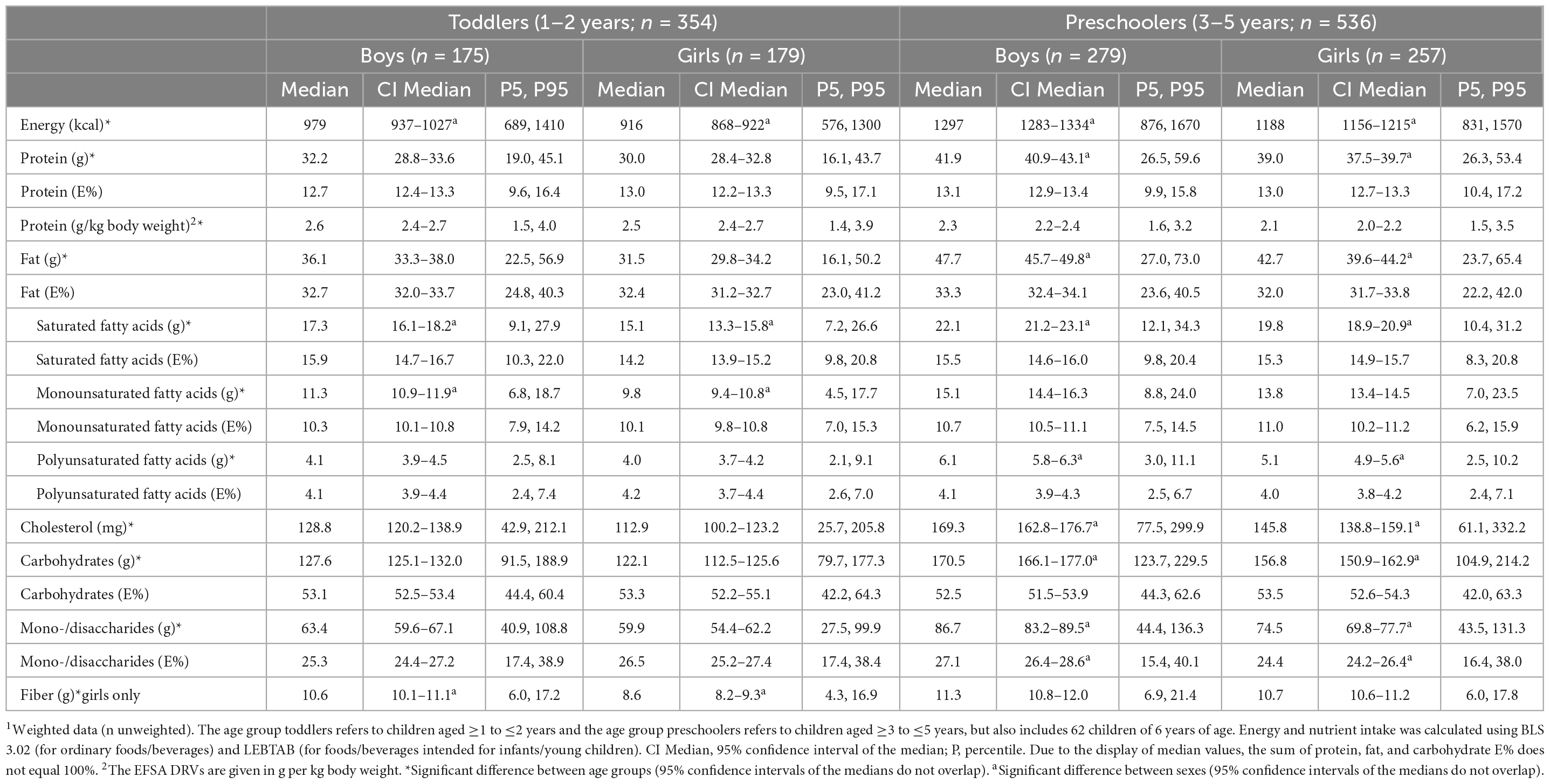
Table 3. Daily energy and macronutrient intake from food and beverages in KiESEL toddlers and preschoolers stratified by sex1.
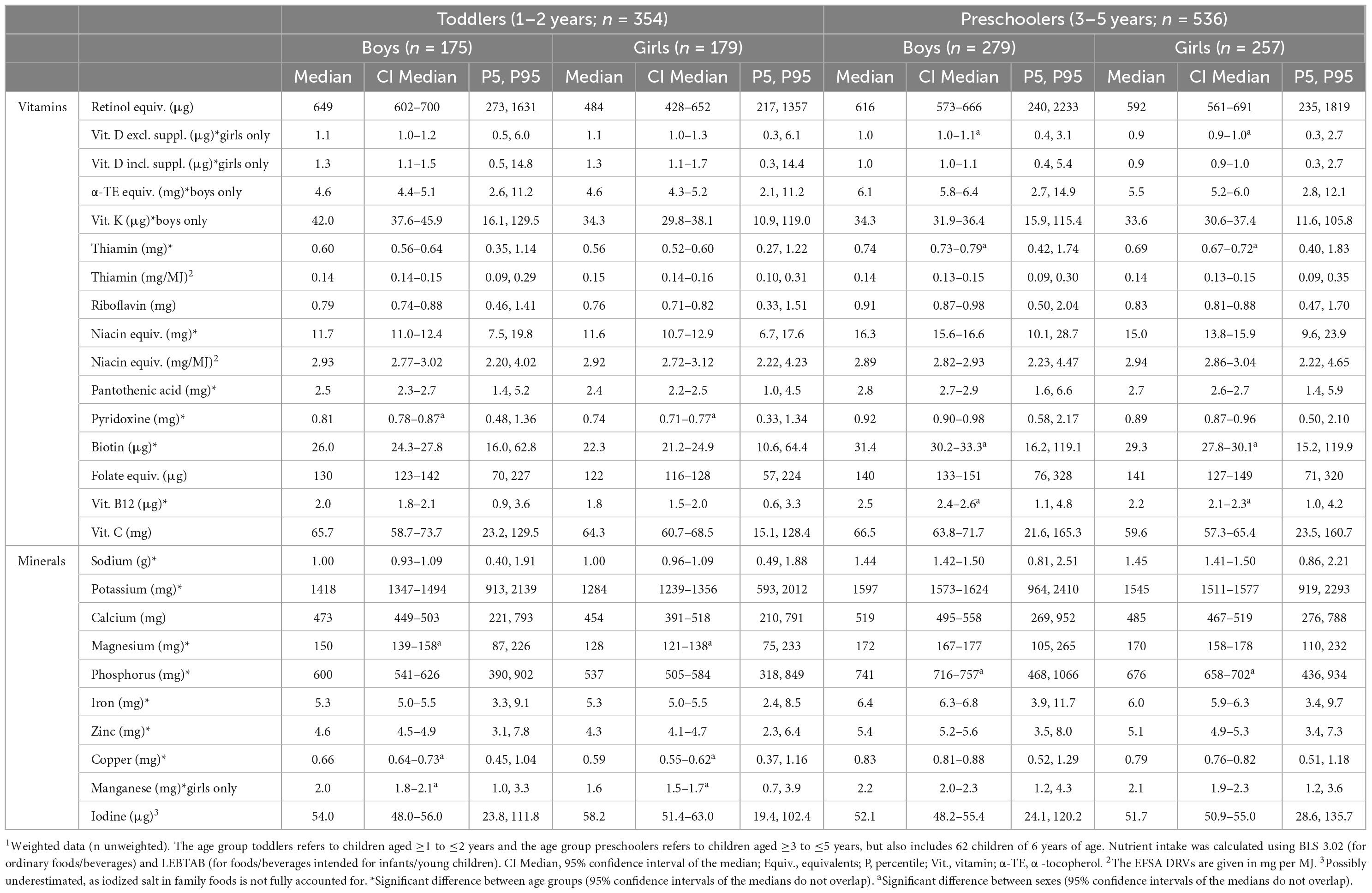
Table 4. Daily micronutrient intake from food and beverages in KiESEL toddlers and preschoolers stratified by sex1.
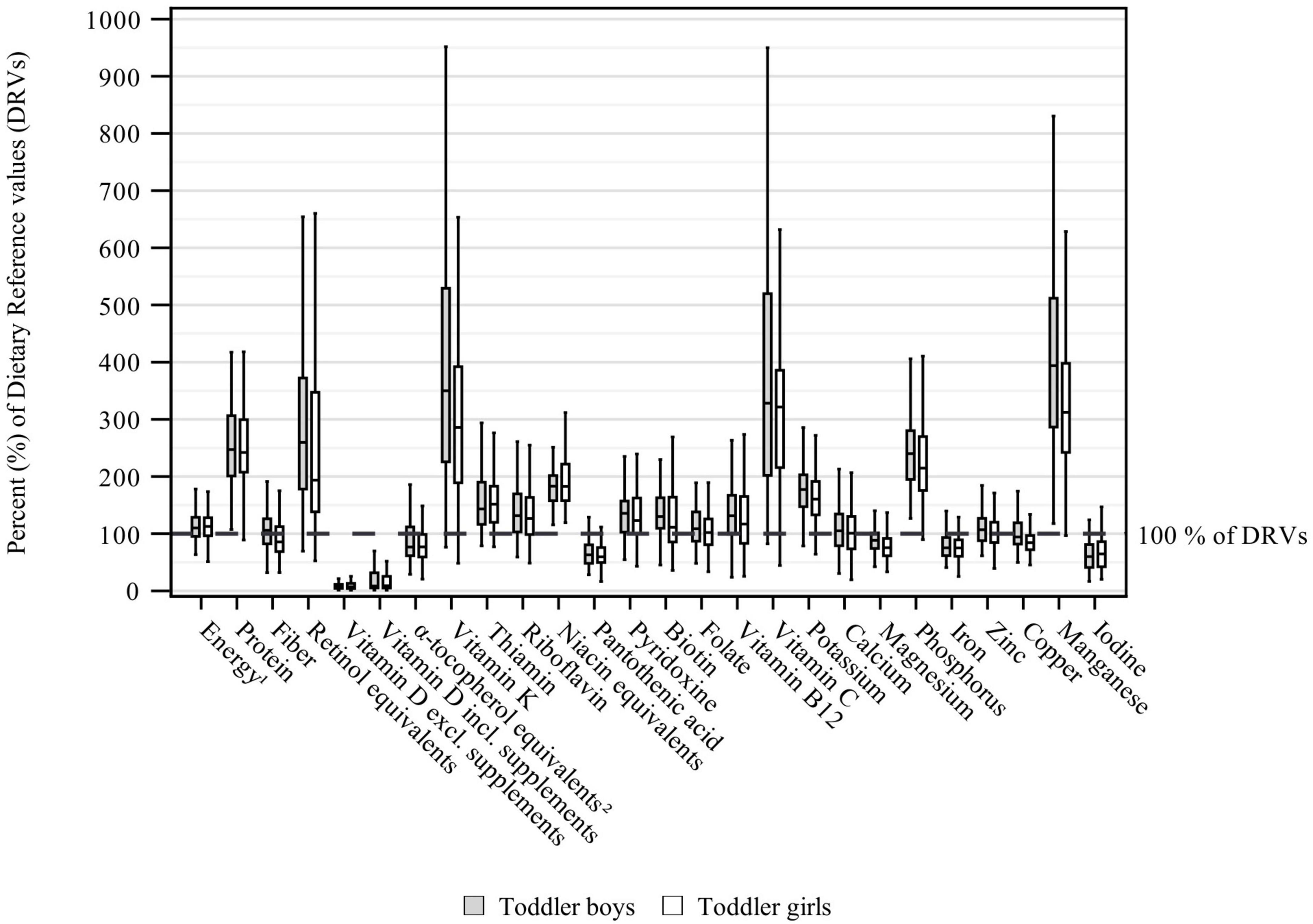
Figure 1. Daily energy and nutrient intake from food and beverages in toddlers (aged ≥1 to ≤2 years) stratified by sex and expressed as % of the EFSA DRVs (12) (weighted data; box and whisker plots with median, interquartile range, and minimum-maximum; whisker length limited to 1.5 times the interquartile range, outliers excluded). 1Assuming a PAL of 1.4.2The EFSA DRVs include α-tocopherol only, while KiESEL intakes are given as α-tocopherol equivalents.
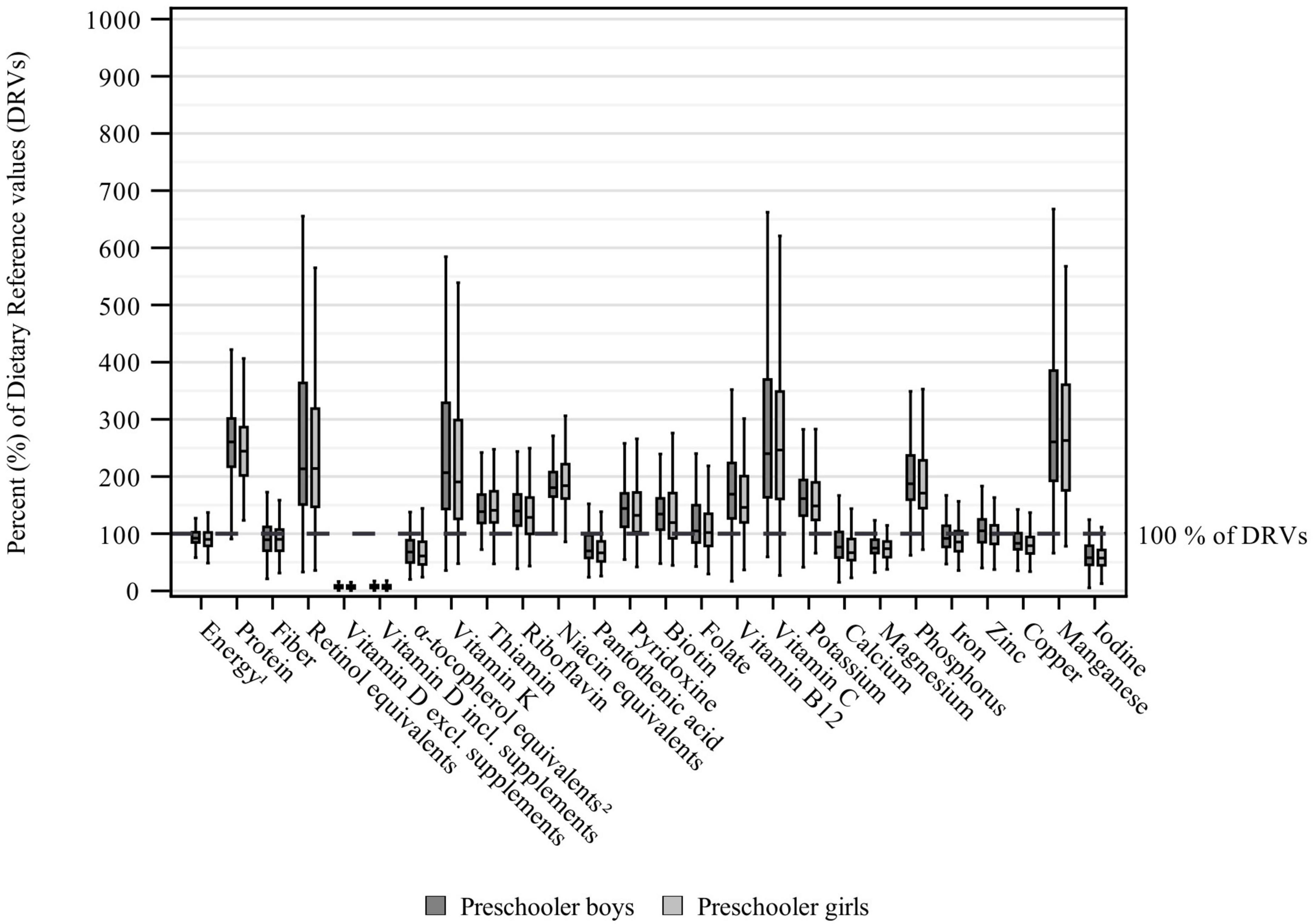
Figure 2. Daily energy and nutrient intake from food and beverages in preschoolers (aged ≥3 to ≤5 years) stratified by sex and expressed as % of the EFSA DRVs (12) (weighted data; box and whisker plots with median, interquartile range, and minimum-maximum; whisker length limited to 1.5 times the interquartile range, outliers excluded). The age group preschoolers refers to children aged ≥3 to ≤5 years, but also includes 62 children of 6 years of age. 1Assuming a PAL of 1.4 for preschoolers 3 years of age and a PAL of 1.6 for preschoolers ≥4 years of age. 2The EFSA DRVs include α-tocopherol only, while KiESEL intakes are given as α-tocopherol equivalents.
The difference in energy intake between boys and girls was more pronounced in preschoolers (median Δ 109 kcal) than in toddlers (median Δ 63 kcal). Consequently, sex-specific differences in daily median macronutrient intakes were predominantly observed in preschoolers (protein, fat, SFA, polyunsaturated fatty acids, cholesterol, carbohydrates, mono-/disaccharides) and less in toddlers (SFA, monounsaturated fatty acids, fiber). Differences in the contribution to energy intake (E%) were only found for mono-/disaccharides in preschoolers. For all differences, intake was consistently higher amongst boys than girls.
Except for vitamin D, α-tocopherol equivalents, and pantothenic acid, median vitamin intakes met or exceeded the applicable DRVs in both toddlers and preschoolers (Figures 1, 2). The largest shortfall relative to the DRVs was found for vitamin D, with median intakes corresponding to less than 10% of the AI for both age groups and sexes, regardless of individual supplement use. Depending on age group and sex, median intakes of α-tocopherol equivalents corresponded to 61–77% and median intakes of pantothenic acid to 60–67% of the AIs, respectively. Total vitamin intakes were largely higher in preschoolers than in toddlers or showed no differences between age groups, except that girls’ vitamin D intakes and boys’ vitamin K intakes were higher in toddlers than in preschoolers. Sex-specific differences in vitamin intake were found more frequently in preschoolers (vitamin D without supplements, thiamin, biotin, vitamin B12) than in toddlers (pyridoxine), with consistently higher intakes in boys than in girls (Table 4).
Among the minerals, median intakes below the DRVs were found for iodine, iron, calcium (preschoolers only), magnesium, and copper. The largest gap in intake relative to the DRVs was found for iodine, with median intakes corresponding to 57–65% of the AI. Median iron intakes corresponded to around 75% of the PRI in toddlers. In preschoolers, median iron intakes were higher, at 92% of the PRI in boys and 85% of the PRI in girls. While median calcium intakes in toddlers met the DRV, the intakes in preschooler boys and girls corresponded to 77 and 67% of the PRIs, respectively, and did not meet the ARs either [390 mg/day for 3-year-olds and 680 mg/day for 4- to 6-year-olds (12)]. Relating to both age groups, median magnesium intakes were equivalent to 74–89% of the AI. For copper, median intakes reached 79–94% of the AI. Overall, mineral intake was higher in preschoolers than in toddlers. However, for calcium and manganese (in boys), the difference between age groups was not significant. Sex-specific differences were found for magnesium, copper and manganese in toddlers, and for phosphorus in preschoolers, all showing higher intakes in boys (Table 4).
This representative study identified nutrient imbalances in young children in Germany up to school entry age, showing vitamin D and iodine intakes well below DRVs, irrespective of age and sex, as well as age-specific non-attainment of DRVs for iron in toddlers and calcium in preschoolers. In contrast, high intakes were found for SFA, mono-/disaccharides, and protein in both age groups.
For vitamin D, the majority of requirement is usually covered by endogenous synthesis in the skin. However, the EFSA AI is based on the premise of minimal cutaneous vitamin D synthesis (12) and may overestimate dietary requirements in case of sufficient sun exposure. According to the European Academy of Paediatrics (EAP), vitamin D deficiency is likely to affect a considerable proportion of healthy European children (22). For Germany, KiGGS data showed a prevalence of vitamin D deficiency (25-hydroxyvitamin D <30 nmol/L) of 5.7% (girls) and 4.9% (boys) in 1- to 2-year-olds and 9.1% (girls) and 11.5% (boys) in 3- to 6-year-olds (23). All European countries recommend vitamin D supplementation in infants (22). In some countries, this recommendation is extended to older children (24), but not in Germany (25). This is reflected by the higher proportion of vitamin D supplement users in KiESEL children of 1 year of age compared to children aged ≥2 years. Given the overall low percentage of supplement users in both age groups, vitamin D intake was likely inadequate with insufficient sun exposure. Vitamin D intakes reported for other European countries, seemed to be higher than in KiESEL, though still below the AI (26–34). In contrast to Germany, some of these countries have mandatory vitamin D fortification policies and/or a broader range of products to which vitamin D may be added voluntarily (35).
Iodine was confirmed as being another critical nutrient in both age groups. While iodine in fortified infant and toddler foods was considered, iodine from iodized salt could only be accounted for if explicitly reported for homemade dishes, as the preset recipes of the BLS contain non-iodized salt by default. However, according to an analysis of iodine exposure levels within the total diet BfR-MEAL-study, 1- to 6-year-olds in Germany have a high risk of inadequate intake, even under the premise of household use of iodized salt (36). A German regional cohort study (DONALD) found that the median 24-h urine iodine excretion in children aged 6–12 years decreased from 2012 onward and reached a minimum of 58.9 μg/d in 2018 (37), classified as mild iodine deficiency (38). This is thought to be due to a decrease in the use of iodized salt (37), described as a key iodine source in German preschoolers (39). Other European surveys showed iodine intakes twice as high (26, 27, 30, 31, 34), and in Danish preschoolers even three times as high as in KiESEL (32), likely explained by the mandatory iodine fortification of household salt and salt for commercial bread production in Denmark (40). In contrast, the use of fortified salt is voluntary in Germany (36). The German food-based dietary guidelines for children and adolescents recommend that households use iodized salt and choose foods with iodized salt over foods with unfortified salt for intakes to meet DRVs (9). In KiESEL, around 74% of parents stated using mainly iodized salt (36). However, the rate of use in the German food industry is estimated at 29% (41), which makes it challenging for households to choose foods with iodized salt. The apparently lower iodine intake in KiESEL in a European comparison may also be explained by mean consumption of milk and milk products (26, 30, 32, 34) and fish being lower (27, 30, 32, 34), which are important sources of iodine.
The present analysis also suggests age-specific deficits in intake for iron in toddlers and calcium in preschoolers. Though reaching only two-thirds of the PRI, toddlers’ iron intake seemed to be lower midfield in a European comparison (26–31) and met the AR of 5 mg/day (12). Worth noting, KiESEL infants (≥6 to ≤11 months) even had iron intakes less than the AR (own unpublished data, 2022). Thus, both infancy and toddlerhood appear to be associated with a higher likelihood of low iron intake than preschool age. One possible explanatory factor might be a higher consumption of meat and meat products at older ages [e.g., 5-year-olds showed an over 1.5 times higher meat consumption per kcal energy intake than 1-year-olds in KiESEL (own unpublished data, 2023)].
Calcium intake, on the other hand, appeared to be potentially critical in preschoolers only, which could be related to the PRI being considerably higher in preschoolers than in toddlers [800 vs. 450 mg/day (12)]. According to EFSA, a median intake equal to the AR reflects a risk of inadequate intake in 50% of individuals (42). Consequently, more than half of KiESEL preschoolers were at risk of insufficient calcium intake. Calcium intake in KiESEL preschoolers seemed lower than in other European surveys (27, 28, 32–34), which may too be related to mean consumption of milk and milk products being lower (28, 32, 34, 43).
In contrast, protein intakes in KiESEL toddlers and preschoolers might be too high. There is emerging evidence supporting a link between high protein intake in early life and later risk of obesity (44). However, in the absence of applicable upper intake levels for the period beyond complementary feeding, a final conclusion on protein intake is not possible. Though intakes in KiESEL exceeded DRVs, available data on protein intake (E%) from other European studies suggest them being at the lower end of the spectrum (26, 28–32, 34).
In the absence of an intake threshold below which no adverse effects exist, the EFSA recommends SFA intake to be as low as possible (12). The WHO set a recommended limit of 10 E% (45), which was clearly exceeded in both KiESEL toddlers and preschoolers, pointing to an unfavorable fatty acid pattern with regard to the risk of cardiovascular disease in later life (46). This observation is in line with a review concluding that the intake of SFA in children aged 1–7 years worldwide was mostly above recommended maximum thresholds, especially in Europe (47). In a European comparison, SFA intakes in KiESEL appeared to be mid-range (26, 28–30, 32, 34).
Similarly, the WHO recommends reducing free sugar intake to <10 E% (48), while EFSA could not identify a level of intake without adverse effects (49). A high intake is likely to facilitate adverse food preferences in early life, e.g., for sweet taste (5), and promote weight gain (48). In KIESEL, free sugars from soft drinks, sweets, fruit juices, cakes, milk and milk products, breakfast cereals, and spices/seasoning sauces corresponded to an estimated 12 E% in toddlers (in boys and girls) and 18 and 17 E% in preschooler boys and girls, respectively (own unpublished data, 2023), estimates derived as in Heuer (50). Intakes were thus too high, particularly in preschoolers. Based on an EFSA analysis, the mean free sugar intake in Europe ranged between 4 and 18 E% in toddlers and 8 and 20 E% in children aged 3–9 years (49).
The present analysis shows a number of differences in nutrient intake between boys and girls that are expected to be related to the higher energy intake in boys compared to girls. Worth noting is that on average preschool boys consumed disproportionately more mono-/disaccharides than their female peers. Boys in the older KiESEL age group consumed more sweets and soft drinks compared to girls (mean: + 19 g/day and + 42 g/day, respectively) (51), likely making them more affected by the adverse effects of free sugar intake.
With nutrition in the early years of life being a key determinant of lifelong health, it is fundamental from a public health perspective to rigorously invest in measures targeting this decisive early phase of life. The present study offers valuable guidance for public health service providers and policymakers as to which nutrients and groups at risk to prioritize and assists in ensuring efficient, need-based resource allocation.
Key strengths of this study are the representative sampling approach and the use of a weighting factor to correct for deviations from the German population, but also the level of detail of data provided by weighed food records (52). Besides, the joint use of the two food composition databases BLS and LEBTAB improves the matching of food items. However, despite the use of a weighting factor, children of parents with low SES were somewhat underrepresented, limiting generalizability. Also, weighed food records entail a high respondent burden, potentially inducing changes in dietary behavior (52), and may be confounded by social desirability bias (53). Besides, a comprehensive assessment of nutrient deficiency risk also requires the analysis of relevant biomarkers. However, feasibility is limited due to high costs, limited parental compliance (54), and a lack of reliable biomarkers (55).
Toddlers and preschoolers in Germany show nutrient imbalances consisting of non-attainment of several micronutrient DRVs (particularly vitamin D and iodine), accompanied by unfavorable macronutrient distribution (high share of SFA, mono-/disaccharides, and potentially also protein). Research is urgently needed to determine if routine vitamin D supplementation should be extended beyond infancy. Measures to increase the rate of use of iodized salt by both the food industry and households as well as to lower the intake of SFA and mono-/disaccharides during early childhood are to be strengthened.
The data analyzed in this study is subject to the following licenses/restrictions: Data described in the manuscript, code book, and analytic code will be made available upon request pending application and approval. Requests to access these datasets should be directed to TH, dGhvcnN0ZW4uaGV1ZXJAbXJpLmJ1bmQuZGU=.
The study involving humans was approved by the Ethics Committee of the Berlin Chamber of Physicians (Eth-28/13). The study was conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
LB: Conceptualization, Formal analysis, Methodology, Writing – original draft. SJ: Conceptualization, Methodology, Writing – review and editing. CS: Conceptualization, Methodology, Writing – review and editing. A-KB: Conceptualization, Methodology, Writing – review and editing. AS: Conceptualization, Methodology, Project administration, Writing – review and editing. UA: Writing – review and editing. SS: Conceptualization, Methodology, Writing – review and editing. RE: Conceptualization, Methodology, Writing – review and editing. TH: Conceptualization, Methodology, Project administration, Supervision, Writing – review and editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The Children’s Nutrition Survey to Record Food Consumption (KiESEL) was funded by the German Federal Institute for Risk Assessment (BfR). The present analysis was funded by the Max Rubner-Institut (MRI), Federal Research Institute of Nutrition and Food. Both institutes (incl. the open access publication fee) are financed by the German Federal Ministry of Food and Agriculture (BMEL).
We would like to thank Anne Hirchenhein, Lena Hörz, Valeska Maifeld, Tobias Ottenheym, and Romina Pizarro Gutiérrez for their active support with data preparation and analysis, Fiona Finkbeiner for linguistic revision, Dr. Carolin Krems, Dr. Andrea Schlune, and Dr. Friederike Wittig for their assistance in developing methodological procedures, Prof. Dr. Ingrid Hoffmann for scientific guidance, Dr. Silvia Roser for revising the manuscript, and Prof. Dr. Ute Nöthlings from the University of Bonn for the provision of LEBTAB data. Special thanks go to the German Federal Institute for Risk Assessment for providing the KiESEL data and in particular to Dr. Oliver Lindtner, Nicole Nowak, Anna Holy, and Dr. Anke Weißenborn for sharing their rich expertise with the KiESEL study data. Lastly, we are most grateful to all participating families.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1302323/full#supplementary-material
AI, Adequate Intake; AR, Average Requirement; BfR, German Federal Institute for Risk Assessment (Bundesinstitut für Risikobewertung); BLS, German Nutrient Database (Bundeslebensmittelschlüssel); CI, Confidence Interval; DRV, Dietary Reference Value; EFSA, European Food Safety Authority; E%, percentage of energy intake; KiESEL, Children’s Nutrition Survey to Record Food Consumption (Kinder-Ernährungsstudie zur Erfassung des Lebensmittelverzehrs); KiGGS, German Health Interview and Examination Survey for Children and Adolescents (Studie zur Gesundheit von Kindern und Jugendlichen in Deutschland); MRI, Max Rubner-Institut; P, Percentile; PAL, Physical Activity Level; PRI, Population Reference Intake; RI, Reference Intake Range for Macronutrients; SES, socioeconomic status.
1. Corkins MR, Daniels SR, de Ferranti SD, Golden NH, Kim JH, Magge SN, et al. Nutrition in children and adolescents. Med Clin North Am. (2016) 100:1217–35. doi: 10.1016/j.mcna.2016.06.005
2. Cohen Kadosh K, Muhardi L, Parikh P, Basso M, Jan Mohamed HJ, Prawitasari T, et al. Nutritional support of neurodevelopment and cognitive function in infants and young children – An update and novel insights. Nutrients. (2021) 13:199. doi: 10.3390/nu13010199
3. Berti C, Cetin I, Agostoni C, Desoye G, Devlieger R, Emmett PM, et al. Pregnancy and infants’ outcome: nutritional and metabolic implications. Crit Rev Food Sci Nutr. (2016) 56:82–91. doi: 10.1080/10408398.2012.745477
4. Iglesia Altaba I, Larqué E, Mesa MD, Blanco-Carnero JE, Gomez-Llorente C, Rodríguez-Martínez G, et al. Early nutrition and later excess adiposity during childhood: a narrative review. Horm Res Paediatr. (2022) 95:112–9. doi: 10.1159/000520811
5. Alles MS, Eussen SRBM, van der Beek EM. Nutritional challenges and opportunities during the weaning period and in young childhood. Ann Nutr Metab. (2014) 64:284–93. doi: 10.1159/000365036
6. World Health Organization [WHO].WHO European Regional Obesity Report 2022. (2022). Available online at: https://apps.who.int/iris/bitstream/handle/10665/353747/9789289057738-eng.pdf (accessed May 23, 2023).
7. Zaragoza-Jordana M, Closa-Monasterolo R, Luque V, Ferré N, Grote V, Koletzko B, et al. Micronutrient intake adequacy in children from birth to 8 years. Data from the childhood obesity project. Clin Nutr. (2018) 37:630–7. doi: 10.1016/j.clnu.2017.02.003
8. EFSA Panel on Dietetic Products, Nutrition and Allergies [NDA]. Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J. (2013) 11:3408. doi: 10.2903/j.efsa.2013.3408
9. Kersting M, Kalhoff H, Lücke T. Von Nährstoffen zu Lebensmitteln und Mahlzeiten: das Konzept der Optimierten Mischkost für Kinder und Jugendliche in Deutschland [From nutrients to food and meals: the concept of the optimized mixed diet for children and adolescents in Germany]. Aktuel Ernahrungsmed. (2017) 42:304–15. doi: 10.1055/s-0043-116499
10. Deutsche Gesellschaft für Ernährung e. V. [DGE]. The Nutrition Report 2008 Summary. Bonn: DGE (2008). Available online at: https://www.dge.de/fileadmin/public/doc/en/DGE-Nutrition-Report-summary-2008.pdf (accessed January 11, 2023).
11. Nowak N, Diouf F, Golsong N, Höpfner T, Lindtner O. KiESEL – the children’s nutrition survey to record food consumption for the youngest in Germany. BMC Nutr. (2022) 8:64. doi: 10.1186/s40795-022-00527-6
12. European Food Safety Authority [EFSA]. Dietary reference values for nutrients: summary report. EFSA Support Public. (2017) 14:e15121. doi: 10.2903/sp.efsa.2017.e15121
13. Lachat C, Hawwash D, Ocké MC, Berg C, Forsum E, Hörnell A, et al. Strengthening the Reporting of Observational Studies in Epidemiology - nutritional epidemiology (STROBE-nut): an extension of the STROBE statement. Nutr Bull. (2016) 41:240–51. doi: 10.1111/nbu.12217
14. Golsong N, Nowak N, Schweter A, Lindtner O. KiESEL – the children’s nutrition survey module in KiGGS Wave 2. J Health Monit. (2017) 2, (Suppl. 3):S28–35. doi: 10.17886/rki-gbe-2017-106
15. Briefel RR, Kalb LM, Condon E, Deming DM, Clusen NA, Fox MK, et al. The feeding infants and toddlers study 2008: study design and methods. J Am Diet Assoc. (2010) 110, (Suppl. 12):S16–26. doi: 10.1016/j.jada.2010.09.005
16. Hartmann B, Heuer T, Hoffmann I. The German nutrient database: effect of different versions on the calculated energy and nutrient intake of the German population. J Food Compost Anal. (2015) 42:26–9. doi: 10.1016/j.jfca.2015.01.001
17. Sichert-Hellert W, Kersting M, Chahda C, Schäfer R, Kroke A. German food composition database for dietary evaluations in children and adolescents. J Food Compost Anal. (2007) 20:63–70. doi: 10.1016/j.jfca.2006.05.004
18. Bundesinstitut für Risikobewertung [BfR].[German Federal Institute for Risk Assessment]. Nahrungsergänzungsmitteldatenbank der KiESEL-Studie [Dietary supplement database of the KiESEL study]. (2019). Available online at: https://www.bfr.bund.de/de/publikationsliste_kiesel-241325.html (accessed November 15, 2022).
19. European Food Safety Authority [EFSA].Example of a Protocol for Identification of Misreporting (Under- and Overreporting of Energy Intake) based on the PILOT-PANEU Project. (2013). Available online at: www.efsa.europa.eu/sites/default/files/efsa_rep/blobserver_assets/3944A-8-2-1.pdf (accessed January 25, 2023).
20. Forschungsdatenzentren der Statistischen Ämter des Bundes und der Länder.Microcensus. (2023). Available online at: https://www.forschungsdatenzentrum.de/en/household/microcensus (accessed June 5, 2023).
21. Koletzko B. Nutrient intake values: concepts and applications. In: Koletzko B, Bhutta Z, Cai W, Dhansay M, Duggan C, Makrides M, et al. editors. Pediatric Nutrition in Practice. (Vol. 124), Basel: World Rev Nutr Diet. Karger (2022). p. 41–6.
22. Grossman Z, Hadjipanayis A, Stiris T, Del Torso S, Mercier JC, Valiulis A, et al. Vitamin D in European children – statement from the European Academy of Paediatrics (EAP). Eur J Pediatr. (2017) 176:829–31. doi: 10.1007/s00431-017-2903-2
23. Rabenberg M, Scheidt-Nave C, Busch MA, Thamm M, Rieckmann N, Durazo-Arvizu RA, et al. Implications of standardization of serum 25-hydroxyvitamin D data for the evaluation of vitamin D status in Germany, including a temporal analysis. BMC Public Health. (2018) 18:845. doi: 10.1186/s12889-018-5769-y
24. Braegger C, Campoy C, Colomb V, Decsi T, Domellof M, Fewtrell M, et al. Vitamin D in the healthy European paediatric population. J Pediatr Gastroenterol Nutr. (2013) 56:692–701. doi: 10.1097/MPG.0b013e31828f3c05
25. Reinehr T, Schnabel D, Wabitsch M, Bechtold-Dalla Pozza S, Buhrer C, Heidtmann B, et al. Vitamin D supplementation after the second year of life: Joint position of the Committee on Nutrition, German Society for Pediatric and Adolescent Medicine (DGKJ e.V.), and the German Society for Pediatric Endocrinology and Diabetology (DGKED e.V.). Mol Cell Pediatr. (2019) 6:3. doi: 10.1186/s40348-019-0090-0
26. van Rossum CTM, Buurma-Rethans EJM, Dinnissen CS, Beukers MH, Brants HAM, Dekkers ALM, et al. The diet of the Dutch: Results of the Dutch National Food Consumption Survey 2012–2016. Netherlands: Rijksinstituut voor Volksgezondheid en Milieu (RIVM) [National Institute for Public Health and the Environment]. (2020). Available online at: https://www.rivm.nl/bibliotheek/rapporten/2020-0083.pdf (accessed January 25, 2023).
27. Agence nationale de sécurité sanitaire de l’alimentation de I’environnement et du travail [ANSES].Etude Individuelle Nationale des Consommations Alimentaires 3 (INCA 3). Avis de l’ANSES. Rapport d’expertise Collective [Third Individual and National Survey on Food Consumption (INCA 3). ANSES opinion. Collective expertise report]. (2017). Available online at: https://www.anses.fr/fr/system/files/NUT2014SA0234Ra.pdf (accessed January 25, 2023).
28. Irish Universities Nutrition Alliance [IUNA].National Pre-School Nutrition Survey (2010–2011). University College Cork and University College Dublin. (2012). Available online at: https://irp-cdn.multiscreensite.com/46a7ad27/files/uploaded/The%20National%20Pre-School%20Nutrition%20Survey%20%282010-2011%29.pdf (accessed January 25, 2023).
29. Brunner TA, Casetti L, Haueter P, Müller P, Nydegger A, Spalinger J. Nutrient intake of Swiss toddlers. Eur J Nutr. (2018) 57:2489–99. doi: 10.1007/s00394-017-1521-0
30. Trolle E, Gondolf UH, Ege M, Kørup K, Ygil KH, Christensen T. Danskernes Kostvaner Spæd- og småbørn 2006–2007 [Dietary Survey of Infants and Young Children 2006–2007]. Søborg: DTU Fødevareinstituttet [DTU National Food Institute] (2013). Available online at: https://orbit.dtu.dk/files/84054319/Rapport_Danskernes_kostvaner_sp_d_og_sm_b_rn_rev_12_12_13_1_.pdf (accessed January 25, 2023).
31. Bates B, Collins D, Jones K, Page P, Roberts C, Steer T, et al. List of tables for Years 9–11 of the UK NDNS Rolling Programme (2016/17–2018/19). A survey carried out on behalf of Public Health England and the Food Standards Agency. (2020). Available online at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/943623/NDNS_from_years_1_to_9_data_tables__1_.zip (accessed January 25, 2023).
32. Pedersen AN, Christensen T, Matthiessen J, Knudsen VK, Sørensen MR, Biltoft-Jensen AP, et al. Danskernes Kostvaner 2011–2013. Hovedresultater [Dietary habits in Denmark 2011–2013. Main results]. Søborg: DTU Fødevareinstituttet [DTU National Food Institute] (2015). Available online at: https://backend.orbit.dtu.dk/ws/portalfiles/portal/110628064/Rapport_Danskernes_Kostvaner_2011_2013.pdf (accessed January 25, 2023).
33. Cuadrado-Soto E, López-Sobaler AM, Jiménez-Ortega AI, Aparicio A, Bermejo LM, Hernández-Ruiz Á, et al. Usual dietary intake, nutritional adequacy and food sources of calcium, phosphorus, magnesium and vitamin D of Spanish children aged one to <10 Years. Findings from the EsNuPI Study. Nutrients. (2020) 12:1787. doi: 10.3390/nu12061787
34. De Ridder K, Bel S, Brocatus L, Lebacq T, Ost C, Teppers E. Enquête de Consommation Alimentaire. Résumé des Résultats 2014–2015 [Food Consumption Survey. Summary of Results 2014–2015]. Bruxelles: Institut Scientifique de Santé Publique (2016). Available online at: https://fcs.wiv-isp.be/nl/Gedeelde%20%20documenten/FRANS/Resume_FR_finaal_web.pdf (accessed January 25, 2023).
35. Niedermaier T, Gredner T, Kuznia S, Schöttker B, Mons U, Lakerveld J, et al. Vitamin D food fortification in European countries: the underused potential to prevent cancer deaths. Eur J Epidemiol. (2022) 37:309–20. doi: 10.1007/s10654-022-00867-4
36. Bundesinstitut für Risikobewertung [BfR].Rückläufige Jodzufuhr in der Bevölkerung: Modellszenarien zur Verbesserung der Jodaufnahme bei Kindern und Jugendlichen. Stellungnahme [Declining iodine Intake in the Population: Model Scenarios for Improving Iodine Intake in Children and Adolescents. Opinion]. (2022). Available online at: https://www.bfr.bund.de/cm/343/ruecklaeufige-jodzufuhr-in-der-bevoelkerung.pdf (accessed January 23, 2023).
37. Remer T, Hua Y, Esche J, Thamm M. The DONALD study as a longitudinal sensor of nutritional developments: iodine and salt intake over more than 30 years in German children. Eur J Nutr. (2022) 61:2143–51. doi: 10.1007/s00394-022-02801-6
38. World Health Organization [WHO].Urinary Iodine Concentrations for Determining Iodine Status in Populations. Geneva: WHO (2013). Available online at: https://apps.who.int/iris/bitstream/handle/10665/85972/WHO_NMH_NHD_EPG_13.1_eng.pdf (accessed January 23, 2023).
39. Johner SA, Thamm M, Nöthlings U, Remer T. Iodine status in preschool children and evaluation of major dietary iodine sources: a German experience. Eur J Nutr. (2013) 52:1711–9. doi: 10.1007/s00394-012-0474-6
40. Nyström HF, Brantsæter AL, Erlund I, Gunnarsdottir I, Hulthén L, Laurberg P, et al. Iodine status in the Nordic countries – past and present. Food Nutr Res. (2016) 60:31969. doi: 10.3402/fnr.v60.31969
41. Bissinger K, Busl L, Dudenhöfer C, Fast D, Heil EA, Herrmann R, et al. Repräsentative Markterhebung zur Verwendung von Jodsalz in handwerklich und industriell gefertigten Lebensmitteln. Abschlussbericht zum Forschungsprojekt zur Bereitstellung wissenschaftlicher Entscheidungshilfe für das Bundesministerium für Ernährung und Landwirtschaft (BMEL) [Representative Market Survey on the use of Iodized Salt in Artisanal and Industrially Produced foods. Final Report on the Research Project for the Provision of Scientific Decision Guidance for the German Federal Ministry of Food and Agriculture (BMEL)]. Justus-Liebig-University Gießen. (2018). Available online at: https://service.ble.de/ptdb/index2.php?detail_id=151927&site_key=141&stichw=Jodsalz&zeilenzahl_zaehler=2&pId=151927&dId=4542600 (accessed January 25, 2023).
42. EFSA Panel on Dietetic Products, Nutrition and Allergies [NDA]. Scientific opinion on principles for deriving and applying dietary reference values. EFSA J. (2010) 8:1458. doi: 10.2903/j.efsa.2010.1458
43. Plaza-Díaz J, Molina-Montes E, Soto-Méndez MJ, Madrigal C, Hernández-Ruiz Á, Valero T, et al. Clustering of dietary patterns and lifestyles among Spanish children in the EsNuPI study. Nutrients. (2020) 12:2536. doi: 10.3390/nu12092536
44. Lind MV, Larnkjær A, Mølgaard C, Michaelsen KF. Dietary protein intake and quality in early life: impact on growth and obesity. Curr Opin Clin Nutr Metab Care. (2017) 20:71–6. doi: 10.1097/mco.0000000000000338
45. Word Health Organization [WHO].Saturated Fatty Acid and Trans-Fatty Acid Intake for Adults and Children: WHO Guideline. Geneva: World Health Organization (2023). Available online at: https://www.who.int/publications/i/item/9789240073630 (accessed December 6, 2023).
46. Te Morenga L, Montez JM. Health effects of saturated and trans-fatty acid intake in children and adolescents: systematic review and meta-analysis. PLoS One. (2017) 12:e0186672. doi: 10.1371/journal.pone.0186672
47. Monnard C, Fleith M. Total fat and fatty acid intake among 1–7-year-old children from 33 countries: comparison with international recommendations. Nutrients. (2021) 13:3547. doi: 10.3390/nu13103547
48. World Health Organization [WHO].Guideline: Sugars Intake for Adults and Children. Geneva: Department of Nutrition for Health and Development WHO (2015). Available online at: https://apps.who.int/iris/bitstream/handle/10665/149782/9789241549028_eng.pdf (accessed January 25, 2023).
49. Turck D, Bohn T, Castenmiller J, de Henauw S, Hirsch-Ernst KI, Knutsen HK. Tolerable upper intake level for dietary sugars. EFSA J. (2022) 20:e07074. doi: 10.2903/j.efsa.2022.7074
50. Heuer T. Zuckerkonsum in Deutschland [Sugar consumption in Germany]. Aktuel Ernahrungsmed. (2018) 43, (Suppl. 1):S8–11. doi: 10.1055/a-0659-8828
51. Spiegler, C, Jansen S, Burgard L, Wittig F, Brettschneider AK, Schlune A, et al. Unfavorable food consumption in children up to school entry age: results from the nationwide German KiESEL study. (under review) (2023).
52. Food and Agriculture Organization of the United Nations [FAO].Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings. Rome: FAO (2018).
53. Bailey RL. Overview of dietary assessment methods for measuring intakes of foods, beverages, and dietary supplements in research studies. Curr Opin Biotechnol. (2021) 70:91–6. doi: 10.1016/j.copbio.2021.02.007
54. Nicholl A, O’Sullivan TA. Keep calm and carry on: parental opinions on improving clinical dietary trials for young children. Nutrients. (2018) 10:1166. doi: 10.3390/nu10091166
Keywords: energy intake, nutrient intake, toddlers, preschoolers, nutrition survey, Germany
Citation: Burgard L, Jansen S, Spiegler C, Brettschneider A-K, Straßburg A, Alexy U, Storcksdieck genannt Bonsmann S, Ensenauer R and Heuer T (2024) Unfavorable nutrient intakes in children up to school entry age: results from the nationwide German KiESEL study. Front. Nutr. 10:1302323. doi: 10.3389/fnut.2023.1302323
Received: 26 September 2023; Accepted: 13 December 2023;
Published: 23 January 2024.
Edited by:
Roberta Masella, National Institute of Health (ISS), ItalyReviewed by:
Katarzyna Magdalena Brukało, Medical University of Silesia, PolandCopyright © 2024 Burgard, Jansen, Spiegler, Brettschneider, Straßburg, Alexy, Storcksdieck genannt Bonsmann, Ensenauer and Heuer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thorsten Heuer, dGhvcnN0ZW4uaGV1ZXJAbXJpLmJ1bmQuZGU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.