- 1Gastroenterology and Liver Diseases Research Center, Research Institute for Gastroenterology and Liver Diseases, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 2Department of Clinical Nutrition and Dietetics, Faculty of Nutrition and Food Technology, National Nutrition and Food Technology, Research Institute, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Department of Nutrition, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
Background: More than half of patients with irritable bowel syndrome (IBS) report aggravating their symptoms with certain foods. Currently, Low fermentable oligo-, di-, and monosaccharides and polyols diet (LFD) is the most accepted dietary intervention for IBS. Recent randomized controlled trials (RCTs) have been suggested that gluten restriction may reduce the symptoms of patients with IBS. However, the results from these studies are conflicting. This study filled this knowledge gap by evaluating the impact of the gluten-free diet (GFD) on IBS symptoms.
Methods: A systematic search was carried out in Pubmed/Medline, Cochrane CENTRAL, Scopus, and Web of Science up to April 2023. A random-effect model was applied to estimate the standardized mean difference (SMD) and 95% confidence interval (95% CI) for each outcome.
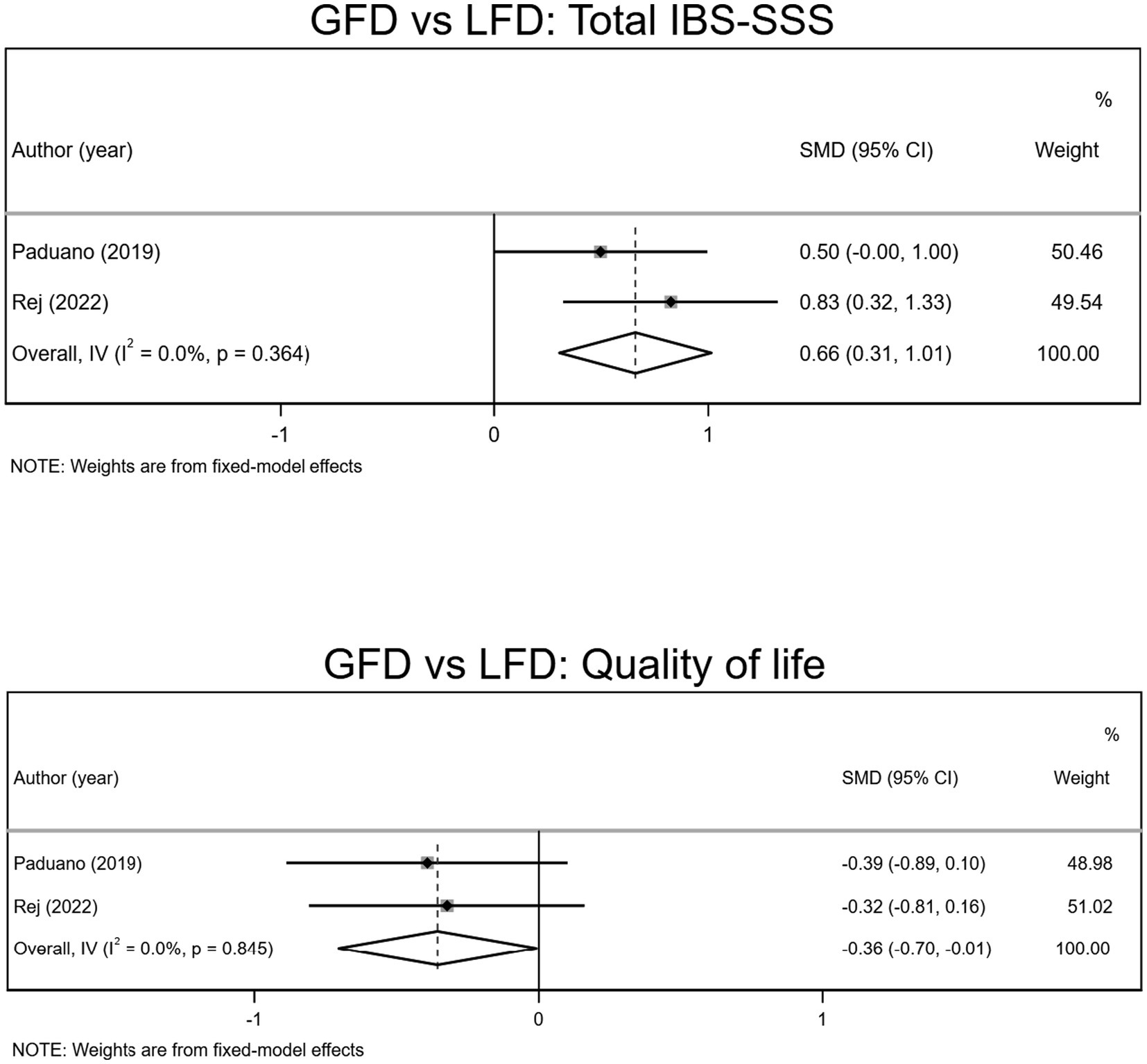
Results: A total of nine controlled trials were included in the meta-analysis. In contrast to gluten-containing diet, GFD was unable to reduce overall symptoms (SMD − 0.31; 95% CI −0.92, 0.31), bloating (SMD −0.37; 95% CI −1.03, 0.30), and quality of life (SMD −0.12, 95% CI −0.64, 0.39); but had a slight trend to reduce abdominal pain (SMD –0.68; 95% CI −1.36, −0.00). Also, LFD significantly reduced the IBS-Severity score system (SMD 0.66, 95% CI 0.31, 1.01) and improved quality of life (SMD −0.36, 95% CI −0.70, −0.01), compared to GFD.
Conclusion: A GFD is not robust enough to be routinely recommended for IBS patients, and its efficacy is significantly lower than that of an LFD. Only a certain subgroup of IBS patients may benefit from GFD; further studies are needed to target this subgroup.
1. Introduction
Irritable bowel syndrome (IBS) is a chronic symptom-based disorder of the gastrointestinal (GI) tract. Patients experience symptoms of altered bowel habits, with either constipation, diarrhea, or both, and abdominal pain. Based on pool prevalence analysis, it is estimated that the worldwide prevalence of IBS is 11.2%; however, this might vary from 1.1 to 45.0% according to the criteria used and the country (1). Currently, different first-line therapies, including exercise and pharmacologic options for managing symptoms, are recommended (2).
Even though patients benefit from pharmacological therapies, the results of surveys are indicative of patients’ tendency to dietary modifications, more specifically, foods containing high carbohydrates and fat (3), as 63% reported that their symptoms could be triggered by eating certain foods (4). Some studies suggest that patients with IBS may be intolerant to gluten in the absence of celiac disease (5), which is termed non-celiac gluten sensitivity (NCGS). In fact, patients report benefiting from avoiding gluten from their diet. It is also said that gluten reintroduction might worsen symptoms (6). The possibility that a subset of patients with IBS could fall into NCGS indicates the need to investigate the actual effect of a gluten-free diet (GFD) on the patients (7). Previously, it was shown that the evidence to recommend a GFD to reduce symptoms of patients with IBS is insufficient; although a GFD was associated with a reduced risk of experiencing overall symptoms, but this reduction was not statistically significant (8). So, the recent IBS guidelines do not recommend GFD in IBS. However, due to insufficient data, more trials comparing GFD head-to-head with a Low fermentable oligo-, di- and monosaccharides and polyols diet (LFD) are recommended (9).
The previous systematic review and meta-analysis in this field had some limitations and included merely two randomized controlled trials (RCTs) evaluating the effect of a GFD. Moreover, the analysis result of the included studies with GFD was only compared to a gluten-containing diet (GCD) (8). Since the publication of this study, there have been additional RCTs evaluating different aspects of gluten restriction in IBS. This study aims to update the impact of a GFD on GI symptoms and the quality of life of patients with IBS and compare its efficacy with an LFD to provide clinicians and dieticians an evidence-based assessment of diet therapy in IBS.
2. Methods
This study was conducted and reported according to the 2021 updated Preferred Reported Items for Systematic Reviews and Meta-analysis (PRISMA) statement (10).
2.1. Search strategy
We searched Pubmed/Medline, Cochrane CENTRAL, Scopus, and Web of Science for studies reporting the efficacy/effectiveness of GFD in patients with IBS, published up to April 27, 2023. The search terms were gluten, gluten-free, GFD, irritable bowel syndrome, IBS, irritable colon, and spastic colon (Supplementary Table S1). No language restrictions were imposed.
2.2. Study selection and eligibility criteria
The records found through database searching were merged, and the duplicates were removed using EndNote X20. Two authors independently screened the records by title/abstract and full texts to exclude those unrelated to the study.
All the eligible studies that were included in our analysis according to the PICOS strategy as follows: (1) Population: patients older than 16 years and with the diagnosis of IBS based on ROME III/IV criteria and exclusion of the celiac disease; (2) Intervention: elimination or restriction of gluten in daily diet; (3) Comparators: comparison with placebo, low-FODMAP diet, regular diet, or any non-gluten restricted diet(s); (4) Outcome: those which reported mean changes and their standard deviations (SDs) of GI symptoms including overall symptoms, abdominal pain, bloating, nausea, tiredness, satisfaction with stool consistency, and also quality of life, over the length of the study for both intervention and control groups; and (5) Study design: having a parallel or cross-over design in an RCT setting. Conference abstracts, reviews, experimental studies on animal models, and articles that their full-text or original data were not available were excluded.
2.3. Data extraction
A pre-specified Excel form was used to extract data from the included studies. Two independent reviewers extracted the following items from all eligible studies: first author’s name, publication year, country/ies where the research was conducted, study design, patients’ demographics (age and sex), IBS diagnostic criteria, celiac exclusion methods, prior diet before study initiation, treatment protocols, methodology, sample size, and mean changes and their SDs of all the mentioned outcomes. Data were inserted into Excel sheets, and any differences or disagreements were resolved by consensus or a third reviewer.
2.4. Assessment of risk of bias and GRADE methodology
The methodological quality of included trials was assessed using the Cochrane risk of bias tool on a domain-based evaluation in this meta-analysis (11). The overall evidence across the studies was sorted following the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology using the GRADEPro guideline development tool (GDT) (12).
2.5. Data synthesis and statistical analysis
In the GFD and control groups, mean and SD changes were applied for each variable to acquire the related effect sizes. If no SD changes were reported, they were calculated by taking into account the changes in the concentration of each variable during the trial. 95% confidence intervals (CIs), Interquartile ranges (IQRs), and standard errors (SEs) were converted to SDs (13). We also used a random-effects model that took into account variations between studies to get the overall effect sizes. I2 statistic test was applied for heterogeneity determination. I2 value>50% was characterized as significant heterogeneity between studies (14). Subgroup analyses were performed to find probable sources of heterogeneity based on the pre-defined variables such as intervention length (4 ≥ vs. >4 weeks), gluten dose (elimination vs. restriction), risk of bias (low risk vs. high risk of bias), and subtype of IBS (constipation, diarrhea, or mixed). Influence analysis was performed to determine if the overall effect size depended upon a certain study (15). Publication bias was evaluated statistically using Egger’s regression test and the funnel plot if more than five studies were identified (16). The meta-analysis was conducted using the STATA® version 17.0 (StataCorp, College Station, Lakeway, TX, United States). p value <0.05 was considered a significant level.
3. Results
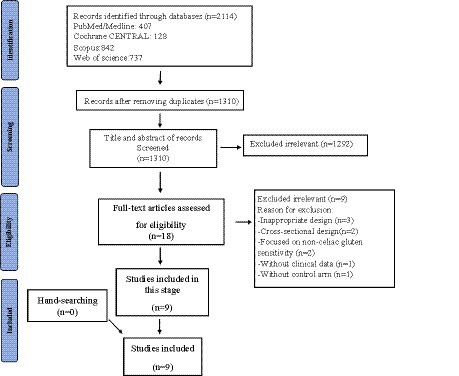
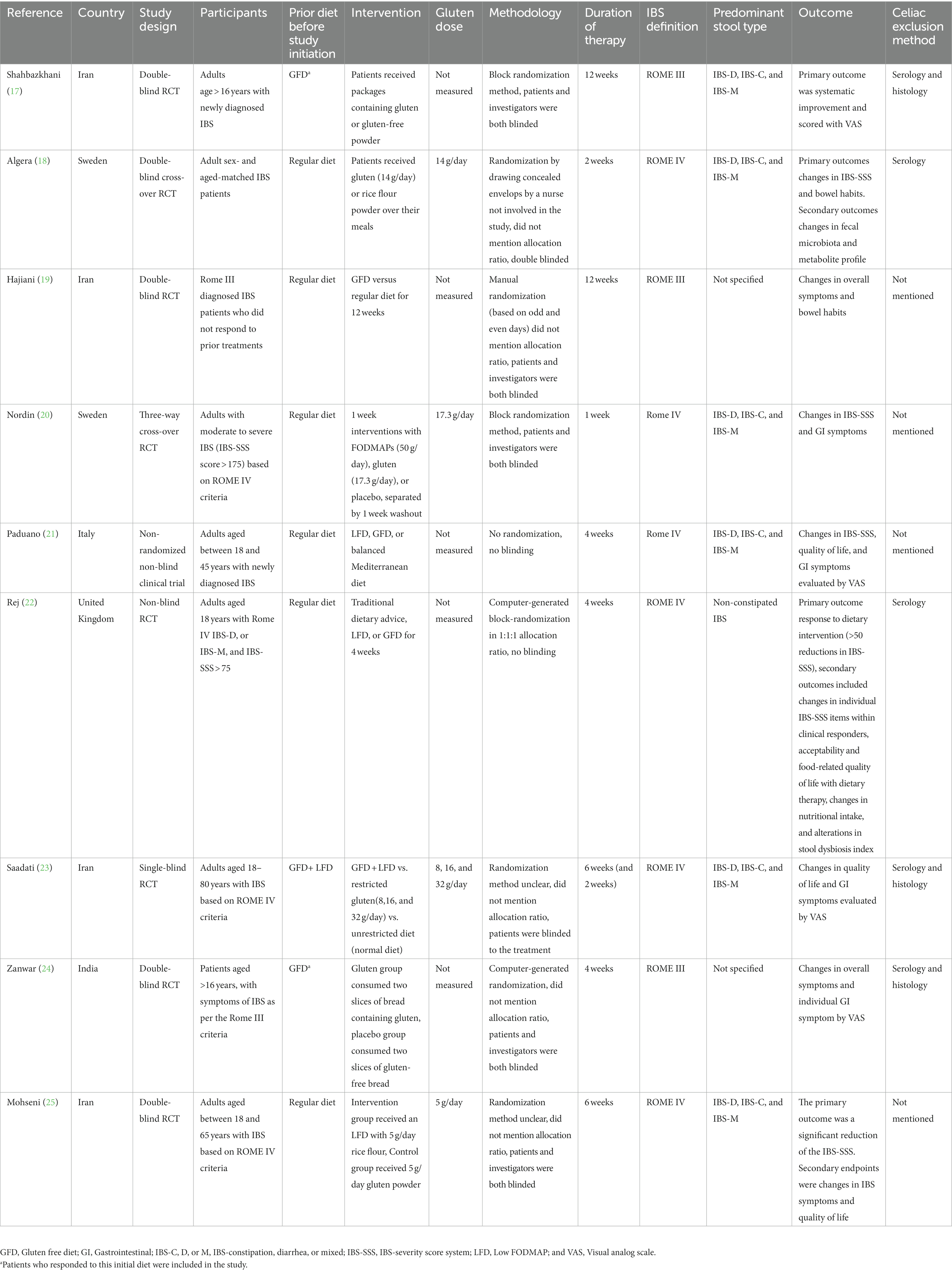
We investigated a total of 1,310 records found in the systematic search; after removing duplicates and full-text reviews, nine were chosen. Studies included and excluded through the review process are summarized in Figure 1; Supplementary Table S2. Among the included studies, there were six parallel and two cross-over RCTs and one non-randomized controlled trial. The studies originated from six countries: Iran (n = 4), Sweden (n = 2), and Italy, United Kingdom, and India (n = 1, for each one). The complete information on the included studies is shown in Table 1.
3.1. GFD vs. GCD
3.1.1. Overall symptoms
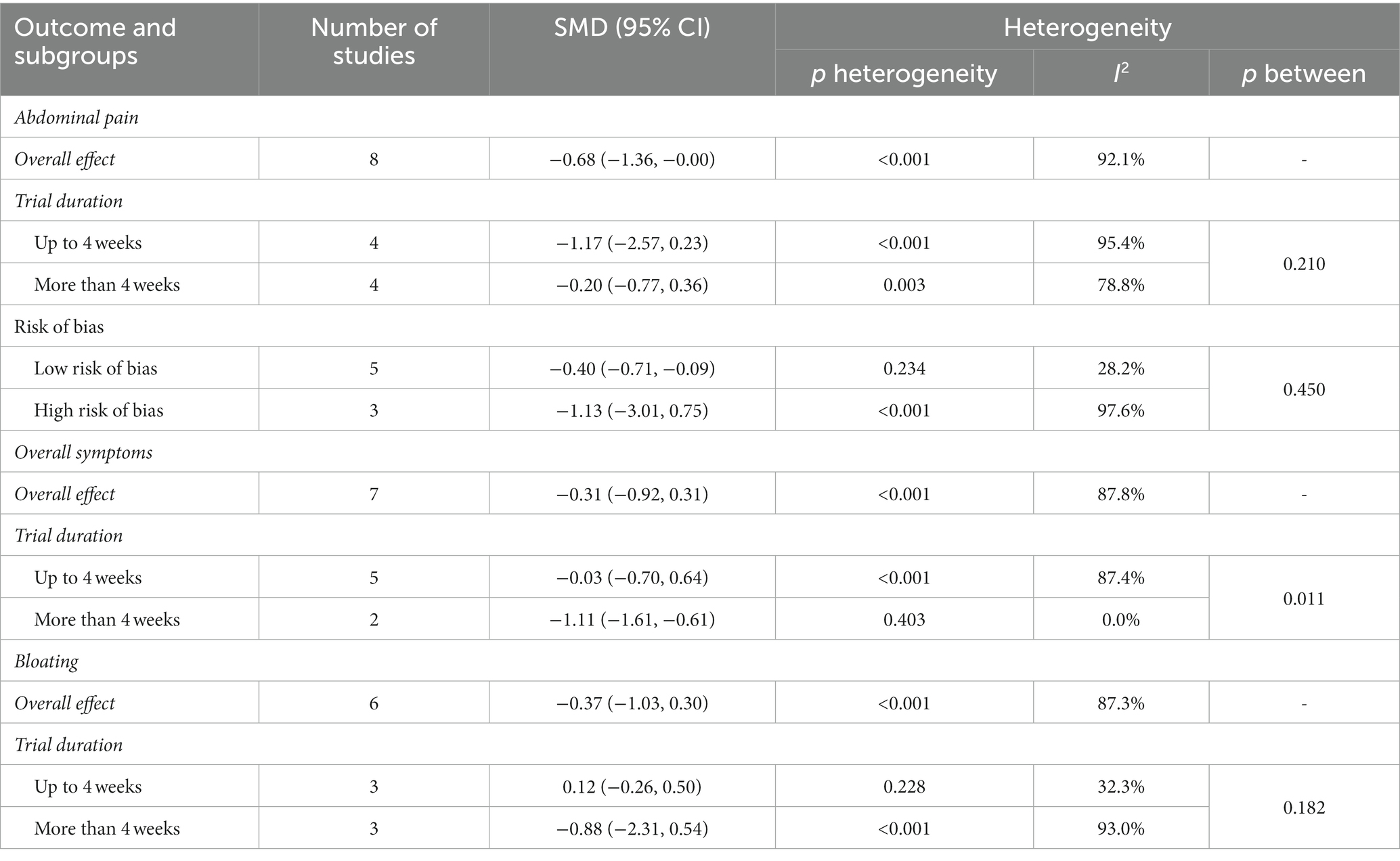
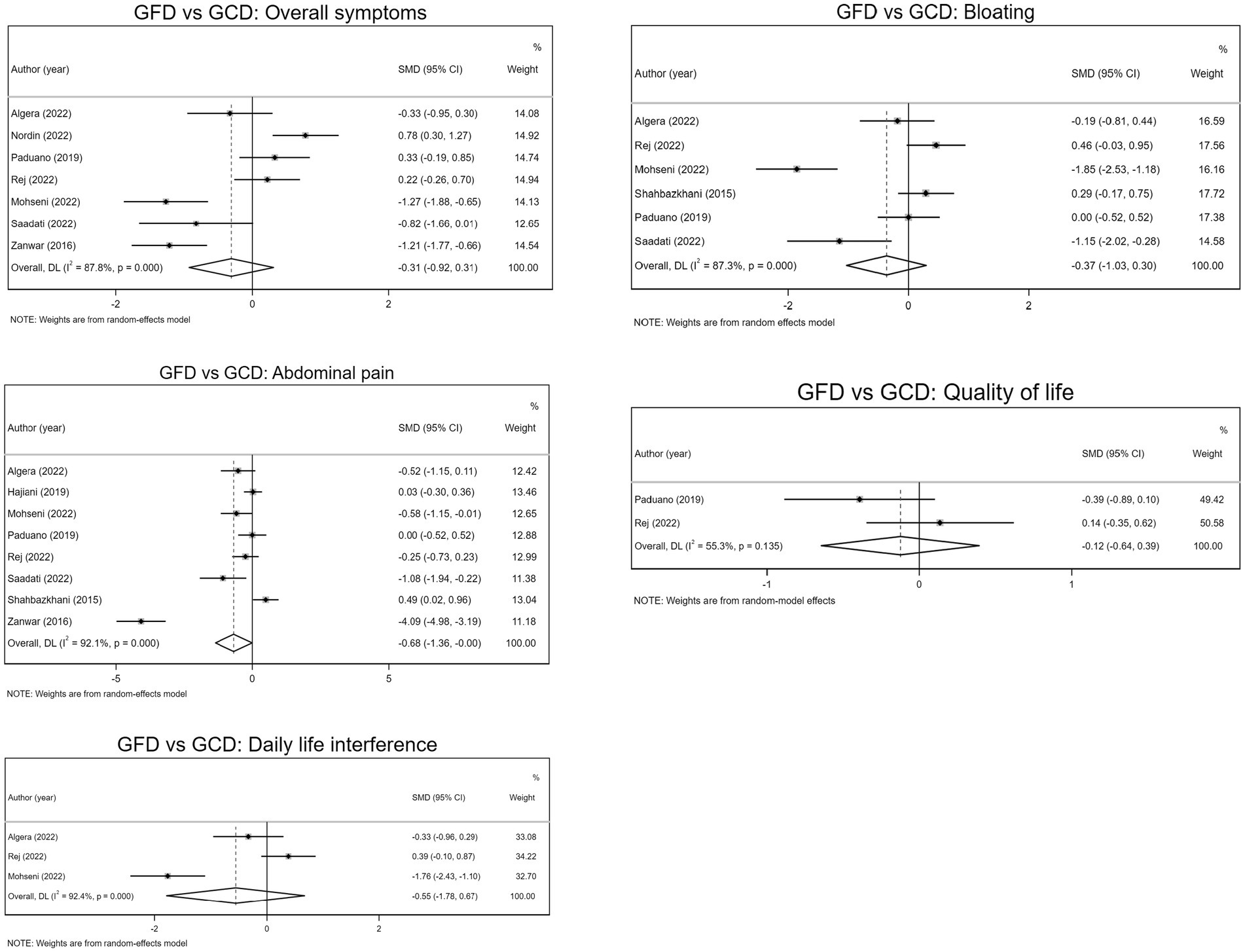
Seven trials evaluated overall symptoms as an outcome measure (intervention samples = 186/ control samples = 182). GFD resulted in a reduction of overall symptoms (SMD − 0.31; 95% CI −0.92, 0.31). Although this was not statistically significant. Subgroup analysis showed that overall symptoms significantly subsided after a period of more than 4 weeks on GFD (SMD −1.11; 95% CI −1.61, −0.61), whereas symptoms did not subside significantly in those who followed the diet for less than 4 weeks (SMD −0.03; 95% CI −0.70, 0.64; Table 2; Figure 2).
Influence analysis was done and did not indicate any evidence of sensitivity (Supplementary Table S3).
3.1.2. Abdominal pain
Pooled effect sizes from eight trials (intervention samples = 258/control samples = 252) indicated GFD significantly reduced abdominal pain compared to GCD (SMD –0.68; 95% CI −1.36, −0.00), while subgroup analysis showed no significant improvement of abdominal pain, regardless of the length of the trial. Also, subgroup analysis showed a significant reduction of abdominal pain in low risk of bias studies (SMD −0.40, 95% CI −0.71, −0.09), while no significant effect for high risk of bias studies (SMD −1.13; 95% CI −3.01, 0.75; Table 2; Figure 2).
Influence analysis indicated that the outcomes lack statistical significance when the exclusion of the five trials is taken into account (Supplementary Table S4).
3.1.3. Bloating
As indicated in Figure 2, pooled data from six studies (intervention samples = 158/control samples = 152) showed no significant reduction of bloating with GFD compared to GCD (SMD −0.37; 95% CI −1.03, 0.30). Additionally, subgroup analyzes showed that neither gluten restriction for less than 4 weeks nor for more than 4 weeks reduced bloating (Table 2).
Influence analysis was done and did reveal any evidence of sensitivity (Supplementary Table S5).
3.1.4. Quality of life
Two controlled trials evaluated quality of life as an outcome measure (intervention samples = 63/control samples = 67). The pooled data suggested GFD is unable to improve the quality of life of the patients with IBS (SMD −0.12, 95% CI −0.64, 0.39; Figure 2).
3.1.5. Daily life interference
Pooled data from three RCTs (intervention samples = 76/control samples = 79) showed no significant reduction of bloating with GFD compared to GCD (SMD −0.55; 95% CI −1.78, 0.67; Figure 2).
3.2. GFD vs. LFD
3.2.1. Total IBS-SSS
As indicated in Figure 3, pooled data from two trials (intervention samples = 63/control samples = 67) showed LFD significantly reduced IBS-SSS, compared to GFD (SMD 0.66, 95% CI 0.31, 1.01).
3.2.2. Quality of life
Two studies evaluated quality of life as an outcome measure (intervention samples = 63/control samples = 67). The pooled data suggested LFD significantly improves the quality of life of the patients with IBS, compared to GFD (SMD −0.36, 95% CI −0.70, −0.01; Figure 3).
3.3. Publication bias
We used Egger’s regression test and funnel plots to assess the possibility of publication bias if more than five studies were identified. There was a significant publication bias for abdominal pain (p = 0.035). However, no evidence of publication bias was observed for reports evaluating the influences of GFD on overall symptoms (p = 0.151), and bloating (p = 0.054). The funnel plots also proved these findings (Supplementary Figure S1).
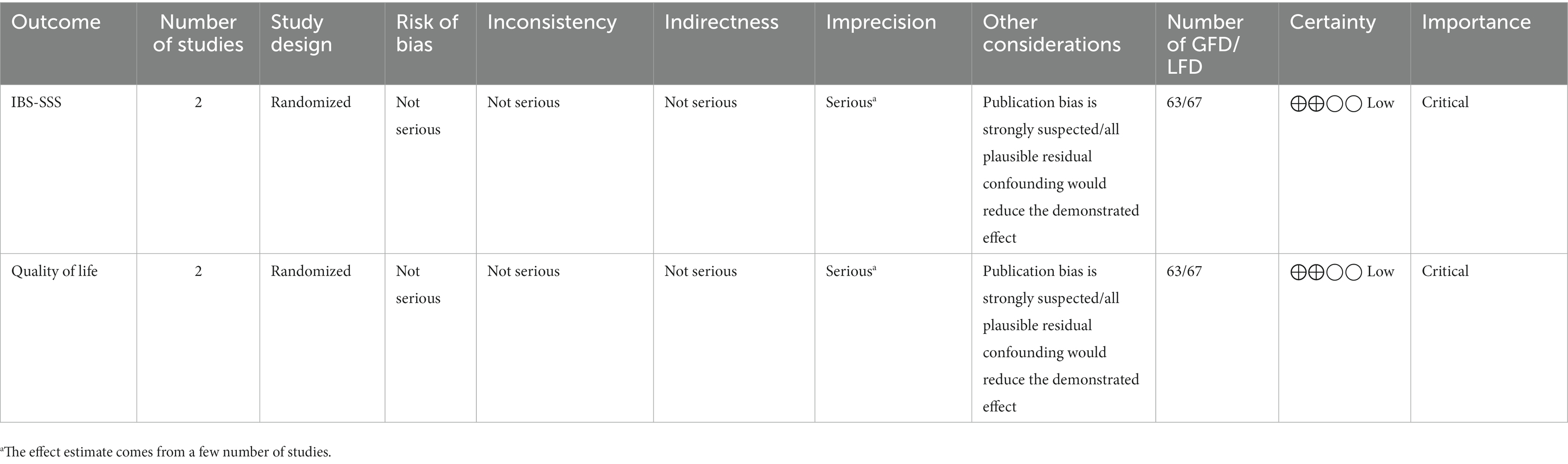
3.4. Risk of bias and GRADE
According to the Cochrane quality assessment tool, six studies had a low risk of bias, while three studies had a high risk of bias (Supplementary Table S6). An assessment of the quality of evidence using the GRADE criteria is presented in Tables 3, 4. The overall quality of the evidence was “very low” for GFD vs. GCD and “low” for GFD vs. LFD, as there were serious or very serious limitations in the terms of risk of bias, inconsistency, imprecision, and publication bias.
4. Discussion
In this study, we aimed to compare the efficacy of GFD to GCD and LFD in IBS. As shown, compared to GCD, GFD was unable to reduce overall symptoms, bloating, and quality of life, but it had a slight trend to reduce abdominal pain. However, it seems even this reduction in abdominal pain is also not much reliable, as the sensitivity analysis showed the results are strongly influenced by some trials. On the other hand, compared to GFD, LFD significantly improved patients’ symptoms and quality of life. These results suggest that, unlike an LFD, a GFD cannot be a routine recommendation for IBS patients.
Gluten-related GI disorders can be categorized as wheat allergy, celiac disease, or NCGS. NCGS is characterized by the distress following gluten consumption in the absence of celiac disease and IgE-mediated allergy (26). This condition is known to be an independent clinical condition and is associated with IBS (27). Notably, most individuals seeking medical options for gluten-induced GI symptoms are found to have no association with celiac disease or wheat allergy (28). As Kaukinen et al. reported, among 94 adults with abdominal symptoms following cereal ingestion, 9% were diagnosed with celiac disease, 8% with latent celiac, and 20% with cereal allergy. Thus, 63% of patients could not be in either the celiac or allergic group; however, they were affected by gluten foods and clinically benefitted from a GFD (29). Given the relatively high prevalence of anti-gliadin antibodies among patients with IBS, a suggested hypothesis was to introduce a subgroup of IBS who experience symptoms most likely manifested by anti-gliadin antibody production. These patients will experience symptom relief with gluten restriction (28, 30).
Importantly, it is shown that gut microbiota is under the influence of GFD, and fecal metabolites of microbiota could be a predictor of participants’ response to GFD (18). In line with these findings, a study by Dieterich et al. showed that Bacteroidetes numbers had a significant increase in patients on a GFD for 2 weeks in comparison with patients on an LFD. The microbial diversity and imbalance in NCGS can be a potential etiology of the patients’ symptoms (31). In fact, the gut microbiota is in dynamic interaction with the immune system, and a balanced microbiota enhances immune responses (32). A strong body of evidence demonstrated the role of inflammation and gluten-triggered immune reactions in GI symptoms of patients with IBS (31, 33). Low-grade inflammation is reported in biopsies from colonic mucosa of more than half of the patients with IBS, which is indicative of food hypersensitivity (34). The increased mast cells as well as increased expression of toll-like receptors (TLRs) in GI mucosa of NCGS patients, are evidences of immune system involvement (35). Furthermore, anti-gliadin immunoglobulin G (IgG) antibodies, which are reported to be predictors of response to GFD (30), are found in more than half of the NCGS patients, thus further supports the suggestion of an immune-mediated mechanism being involved (36). Limited gluten consumption through directly alleviating the pro-inflammatory state, as well as modulating the gut microbiota to further interact with the immune system could result in patients benefiting from GFD (24).
There is an extensive debate about the possible mechanisms by which GFD might impact IBS symptoms. It is suggested that symptoms of IBS patients are more likely to be induced by fructan rather than gluten (25, 37), and barley and wheat exacerbate the patients’ symptoms mainly due to their fructan content, while gluten might be responsible for symptoms of a few percent of subjects (25). As an RCT by Skodje et al. (37) showed, a gluten challenge resulted in no significant difference compared to placebo and fructan in patients’ symptoms, and a small daily amount of fructan, as fructan challenge, increased GI symptoms of participants. The results can be explained by the fact that many foods containing gluten, which is restricted in GFD, also contain fructan (38). However, the result of a food diary study by Algera and colleagues was not in agreement with these findings, as they found no association between fructan intake and the severity of GI symptoms in patients with IBS (39).
Interestingly, it is reported that patients with IBS who experienced more severe symptoms consumed less gluten and calories (39), but caution must be taken in drawing conclusions. Patients might avoid foods containing gluten and, as a result, consume fewer calories. Given that patients with IBS show more tendency to cut calorie intake, dietary counseling is also important in these individuals, especially regarding nutritional inadequacies (40).
To further assess the concept of IBS and NCGS overlap, we aimed to examine the hypothesis that subjects with IBS experience GI symptoms in a dose-dependent way. However, due to the heterogeneity of studies, we could not perform a dose–response analysis regarding the amount of dietary gluten and its potential association with patients’ symptoms. Nevertheless, current evidence supports no significant dose influence of gluten on IBS subjects. The studies by Saadati et al. (23) and Biesiekierski et al. (41) have evaluated gluten restriction. The authors of both trials did not find a dose-dependent pattern of the effects of gluten challenge on the symptoms of subjects with IBS. Even though, currently, no solid evidence has been provided to explain the possible mechanism, we believe that this might be explained through the fact that IBS is a large heterogeneous group consisting of individuals with possibly different etiologies which impose them to IBS symptoms. Thus, it would be rational to consider a subgroup as gluten-sensitive that might be responsive to gluten restriction (28).
Even though GFD might show limited improvement in particular symptoms of patients, it is noteworthy that in many regions, gluten-free products might not be widely available or financially affordable, which makes this dietary change seem to be inconvenient for some patients, thus might reduce patients’ adherence to the GFD. As in some included trials, an innegligible number of patients left the study as they were unable to cope with the dietary restrictions. A non-blinded RCT compared the impact of three types of diet, including the traditional dietary advice, GFD, and LFD, on subjects with non-constipation IBS. The results showed traditional dietary advice to have similar efficacy with LFD and GFD in non-constipated subjects with IBS. Given its accessibility and cost, the traditional diet is recommended as the first choice for this category of IBS patients. Furthermore, GFD and LFD were more expensive and more time-consuming to be prepared for subjects compared to the traditional dietary advice, thus had less acceptability, and the proportion of individuals who considered continuing a GFD was reported to be less than individuals who accepted LFD and these two diets were both less acceptable than traditional dietary advice (22). However, subjects’ adherence to GFD in another study was found to be high as the one-year follow-up showed all responders and 55% of non-responders were continuing GFD. Therefore, it can be assumed that patients’ diet adherence depends on the accessibility to GFD, which makes different studies report different rates (42).
Another controversy about GFD is the time required to see its effectiveness on IBS symptoms. In suspected cases of NCGS, the Salerno criteria recommends 6 weeks of GFD (43), but there is no agreement on the IBS settings. In our included studies, the length of the trials was 1–12 weeks. Considering the number of the studies and their length of intervention, studies were divided into two subgroups of less than 4 weeks and more than 4 weeks. Although the pooled data from eight studies showed a trend of reduction of abdominal pain, but this significance was lost for both subgroups, without between subgroup heterogeneity (p = 0.210).
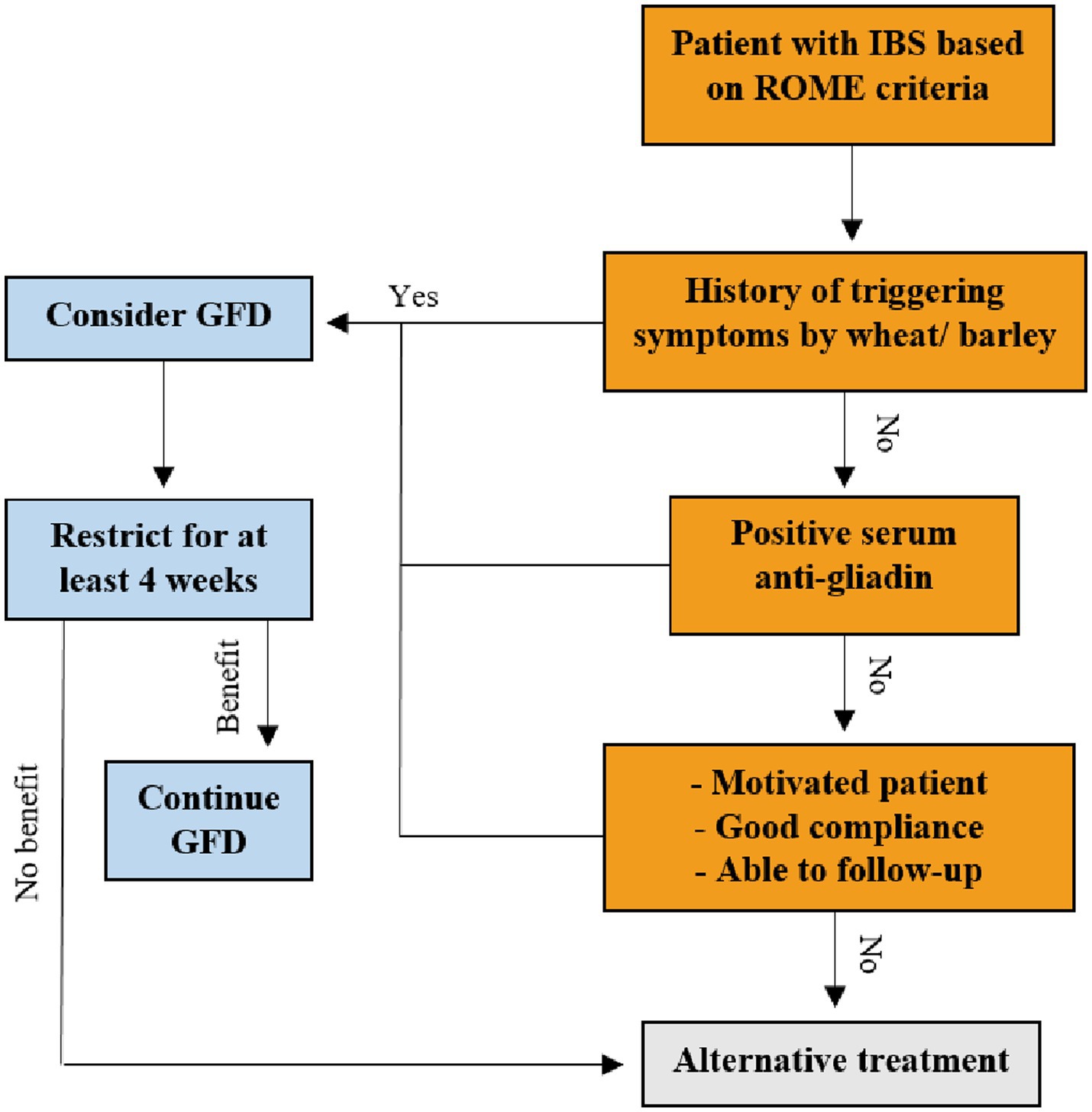
On the other hand, while pooled data from seven studies showed no effect for GFD on overall symptoms, subgroup analysis revealed a significant effect for more than 4 weeks of intervention and a significant between subgroup heterogeneity (p = 0.011). Thus, it seems the length of intervention has a crucial role in the effectiveness of GFD. However, the presence of only two studies in this subgroup makes it difficult to draw a firm conclusion. The data are generally controversial, but at least 4 weeks of GFD may be needed to evaluate its impact on IBS symptoms. The suggested algorithm for consideration of GFD for IBS is illustrated in Figure 4.
The present meta-analysis appears to contain several strengths and limitations. This study, to the best of our knowledge, is the first systematic review and meta-analysis evaluates the effect of GFD on the spectrum of GI symptoms of IBS and compares it with the LFD. The number of eligible studies has also extended remarkably since the topic was last evaluated. Finally, based on the GRADE guidelines, we rigorously evaluated the certainty of evidence across the studies. However, some limitations of this study should be taken into consideration. The relatively small number of trials in some effect sizes diminishes the robustness of the results. This applies more clearly in studies compared GFD with LFD, as there were just two studies in this group. The analysis revealed a high statistical heterogeneity. This may be due to the diversity of methodologies (different designs), differences in intervention type (GFD, GCD, LFD, TDA, and other types of diet) or intervention length (1 to 12 weeks), diagnostic criteria (ROME III or IV), and IBS subtype (constipation, diarrhea, or mixed). Moreover, almost half of the eligible studies were from Iran, limiting the study to reflect diverse global populations and generalizing the results. Also, as with any meta-analysis, limitations associated with potential publication bias should be regarded. Finally, due to insufficient or lack of data, this study was unable to evaluate the efficacy of GFD based on age, sex, or predominant stool type subgroups; determine the precise predictors of response to GFD; and compare the impact of GFD alone with its combination with the other diets. More studies are needed to fill this gap.
5. Conclusion
This is the first meta-analysis to assess the effects of GFD on IBS symptoms to this extent. The findings showed that a GFD is not robust enough to be a routine recommendation for IBS patients. Furthermore, GFD efficacy is significantly lower than that of an LFD. This diet might be beneficial for just a specific subgroup of IBS patients; further studies are needed to target this subgroup.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
EA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. DA: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. AS: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Writing – review & editing. SK: Data curation, Visualization, Writing – original draft. AH: Conceptualization, Methodology, Supervision, Writing – review & editing. HK-V: Data curation, Formal Analysis, Methodology, Software, Validation, Writing – review & editing. MA: Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1273629/full#supplementary-material
References
1. Lovell, RM, and Ford, AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. (2012) 10:712–721.e4. doi: 10.1016/j.cgh.2012.02.029
2. Moayyedi, P, Mearin, F, Azpiroz, F, Andresen, V, Barbara, G, Corsetti, M, et al. Irritable bowel syndrome diagnosis and management: a simplified algorithm for clinical practice. United European Gastroenterol J. (2017) 5:773–88. doi: 10.1177/2050640617731968
3. Böhn, L, Störsrud, S, Törnblom, H, Bengtsson, U, and Simrén, M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Off J Am Coll Gastroenterol. (2013) 108:634–41. doi: 10.1038/ajg.2013.105
4. Simrén, M, Månsson, A, Langkilde, AM, Svedlund, J, Abrahamsson, H, Bengtsson, U, et al. Food-related gastrointestinal symptoms in the irritable bowel syndrome. Digestion. (2001) 63:108–15. doi: 10.1159/000051878
5. Al-Toma, A, Volta, U, Auricchio, R, Castillejo, G, Sanders, DS, Cellier, C, et al. European Society for the Study of coeliac disease (ESsCD) guideline for coeliac disease and other gluten-related disorders. United European Gastroenterol J. (2019) 7:583–613. doi: 10.1177/2050640619844125
6. Biesiekierski, JR, Newnham, ED, Irving, PM, Barrett, JS, Haines, M, Doecke, JD, et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am J Gastroenterol. (2011) 106:508–14. doi: 10.1038/ajg.2010.487
7. Palmieri, B, Vadala, M, and Laurino, C. Gluten-free diet in non-celiac patients: beliefs, truths, advantages and disadvantages. Minerva Gastroenterol Dietol. (2019) 65:153–62. doi: 10.23736/S1121-421X.18.02519-9
8. Dionne, J, Ford, AC, Yuan, Y, Chey, WD, Lacy, BE, Saito, YA, et al. A systematic review and Meta-analysis evaluating the efficacy of a gluten-free diet and a low FODMAPs diet in treating symptoms of irritable bowel syndrome. Am J Gastroenterol. (2018) 113:1290–300. doi: 10.1038/s41395-018-0195-4
9. Vasant, DH, Paine, PA, Black, CJ, Houghton, LA, Everitt, HA, Corsetti, M, et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. (2021) 70:1214–40. doi: 10.1136/gutjnl-2021-324598
10. Page, MJ, McKenzie, JE, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
11. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
12. Guyatt, GH, Oxman, AD, Vist, GE, Kunz, R, Falck-Ytter, Y, Alonso-Coello, P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. (2008) 336:924–6. doi: 10.1136/bmj.39489.470347.AD
13. Hozo, SP, Djulbegovic, B, and Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. (2005) 5:1–10. doi: 10.1186/1471-2288-5-13
14. Higgins, JP, and Thompson, SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
15. Tobias, A. Assessing the influence of a single study in the meta-analysis estimate. Stata Tech Bull. (1999) 47:15–7.
16. Egger, M, Smith, GD, Schneider, M, and Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
17. Shahbazkhani, B, Sadeghi, A, Malekzadeh, R, Khatavi, F, Etemadi, M, Kalantri, E, et al. Non-celiac gluten sensitivity has narrowed the Spectrum of irritable bowel syndrome: a double-blind randomized placebo-controlled trial. Nutrients. (2015) 7:4542–54. doi: 10.3390/nu7064542
18. Algera, JP, Magnusson, MK, Öhman, L, Störsrud, S, Simrén, M, and Törnblom, H. Randomised controlled trial: effects of gluten-free diet on symptoms and the gut microenvironment in irritable bowel syndrome. Aliment Pharmacol Ther. (2022) 56:1318–27. doi: 10.1111/apt.17239
19. Hajiani, E, Masjedizadeh, A, Shayesteh, AA, Babazadeh, S, and Seyedian, SS. Comparison between gluten-free regime and regime with gluten in symptoms of patients with irritable bowel syndrome (IBS). J Family Med Prim Care. (2019) 8:1691–5. doi: 10.4103/jfmpc.jfmpc_464_18
20. Nordin, E, Brunius, C, Landberg, R, and Hellström, PM. Fermentable oligo-, di-, monosaccharides, and polyols (FODMAPs), but not gluten, elicit modest symptoms of irritable bowel syndrome: a double-blind, placebo-controlled, randomized three-way crossover trial. Am J Clin Nutr. (2022) 115:344–52. doi: 10.1093/ajcn/nqab337
21. Paduano, D, Cingolani, A, Tanda, E, and Usai, P. Effect of three diets (low-FODMAP, gluten-free and balanced) on irritable bowel syndrome symptoms and health-related quality of life. Nutrients. (2019) 11. doi: 10.3390/nu11071566
22. Rej, A, Sanders, DS, Shaw, CC, Buckle, R, Trott, N, Agrawal, A, et al. Efficacy and acceptability of dietary therapies in non-constipated irritable bowel syndrome: a randomized trial of traditional dietary advice, the low FODMAP diet, and the gluten-free diet. Clin Gastroenterol Hepatol. (2022) 20:2876–87.e15. doi: 10.1016/j.cgh.2022.02.045
23. Saadati, S, Sadeghi, A, Mohaghegh-Shalmani, H, Rostami-Nejad, M, Elli, L, Asadzadeh-Aghdaei, H, et al. Effects of a gluten challenge in patients with irritable bowel syndrome: a randomized single-blind controlled clinical trial. Sci Rep. (2022) 12:4960. doi: 10.1038/s41598-022-09055-6
24. Zanwar, VG, Pawar, SV, Gambhire, PA, Jain, SS, Surude, RG, Shah, VB, et al. Symptomatic improvement with gluten restriction in irritable bowel syndrome: a prospective, randomized, double blinded placebo controlled trial. Intest Res. (2016) 14:343–50. doi: 10.5217/ir.2016.14.4.343
25. Mohseni, F, Agah, S, Ebrahimi-Daryani, N, Taher, M, Nattagh-Eshtivani, E, Karimi, S, et al. The effect of low FODMAP diet with and without gluten on irritable bowel syndrome: a double blind, placebo controlled randomized clinical trial. Clin Nutr ESPEN. (2022) 47:45–50. doi: 10.1016/j.clnesp.2021.12.019
26. Cabanillas, B. Gluten-related disorders: celiac disease, wheat allergy, and nonceliac gluten sensitivity. Crit Rev Food Sci Nutr. (2020) 60:2606–21. doi: 10.1080/10408398.2019.1651689
27. Talley, NJ, and Walker, MM. Celiac disease and nonceliac gluten or wheat sensitivity: the risks and benefits of diagnosis. JAMA Intern Med. (2017) 177:615–6. doi: 10.1001/jamainternmed.2017.0695
28. Aziz, I, and Sanders, DS. The irritable bowel syndrome-celiac disease connection. Gastrointest Endoscopy Clin. (2012) 22:623–37. doi: 10.1016/j.giec.2012.07.009
29. Kaukinen, K, Turjanmaa, K, Mäki, M, Partanen, J, Venäläinen, R, Reunala, T, et al. Intolerance to cereals is not specific for coeliac disease. Scand J Gastroenterol. (2000) 35:942–6. doi: 10.1080/003655200750022995
30. Pinto-Sanchez, MI, Nardelli, A, Borojevic, R, De Palma, G, Calo, NC, McCarville, J, et al. Gluten-free diet reduces symptoms, particularly diarrhea, in patients with irritable bowel syndrome and antigliadin IgG. Clin Gastroenterol Hepatol. (2021) 19:2343–2352.e8. doi: 10.1016/j.cgh.2020.08.040
31. Dieterich, W, Schuppan, D, Schink, M, Schwappacher, R, Wirtz, S, Agaimy, A, et al. Influence of low FODMAP and gluten-free diets on disease activity and intestinal microbiota in patients with non-celiac gluten sensitivity. Clin Nutr. (2019) 38:697–707. doi: 10.1016/j.clnu.2018.03.017
32. Azimirad, M, Rostami-Nejad, M, Rostami, K, Naji, T, and Zali, MR. The susceptibility of celiac disease intestinal microbiota to Clostridium difficile infection. Am J Gastroenterol. (2015) 110:1740–1. doi: 10.1038/ajg.2015.360
33. Ohman, L, and Simrén, M. Pathogenesis of IBS: role of inflammation, immunity and neuroimmune interactions. Nat Rev Gastroenterol Hepatol. (2010) 7:163–73. doi: 10.1038/nrgastro.2010.4
34. Barbara, G, Stanghellini, V, De Giorgio, R, Cremon, C, Cottrell, GS, Santini, D, et al. Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable bowel syndrome. Gastroenterology. (2004) 126:693–702. doi: 10.1053/j.gastro.2003.11.055
35. Sapone, A, Lammers, KM, Casolaro, V, Cammarota, M, Giuliano, MT, De Rosa, M, et al. Divergence of gut permeability and mucosal immune gene expression in two gluten-associated conditions: celiac disease and gluten sensitivity. BMC Med. (2011) 9:23. doi: 10.1186/1741-7015-9-23
36. Volta, U, Tovoli, F, Cicola, R, Parisi, C, Fabbri, A, Piscaglia, M, et al. Serological tests in gluten sensitivity (nonceliac gluten intolerance). J Clin Gastroenterol. (2012) 46:680–5. doi: 10.1097/MCG.0b013e3182372541
37. Skodje, GI, Sarna, VK, Minelle, IH, Rolfsen, KL, Muir, JG, Gibson, PR, et al. Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterology. (2018) 154:529–539.e2. doi: 10.1053/j.gastro.2017.10.040
38. Algera, J, Colomier, E, and Simrén, M. The dietary management of patients with irritable bowel syndrome: a narrative review of the existing and emerging evidence. Nutrients. (2019) 11:2162. doi: 10.3390/nu11092162
39. Algera, JP, Störsrud, S, Lindström, A, Simrén, M, and Törnblom, H. Gluten and fructan intake and their associations with gastrointestinal symptoms in irritable bowel syndrome: a food diary study. Clin Nutr. (2021) 40:5365–72. doi: 10.1016/j.clnu.2021.09.002
40. Melchior, C, Algera, J, Colomier, E, Törnblom, H, Simrén, M, and Störsrud, S. Food avoidance and restriction in irritable bowel syndrome: relevance for symptoms, quality of life and nutrient intake. Clin Gastroenterol Hepatol. (2022) 20:1290–1298.e4. doi: 10.1016/j.cgh.2021.07.004
41. Biesiekierski, JR, Peters, SL, Newnham, ED, Rosella, O, Muir, JG, and Gibson, PR. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology. (2013) 145:320.e1–8.e3. doi: 10.1053/j.gastro.2013.04.051
42. Barmeyer, C, Schumann, M, Meyer, T, Zielinski, C, Zuberbier, T, Siegmund, B, et al. Long-term response to gluten-free diet as evidence for non-celiac wheat sensitivity in one third of patients with diarrhea-dominant and mixed-type irritable bowel syndrome. Int J Color Dis. (2017) 32:29–39. doi: 10.1007/s00384-016-2663-x
Keywords: gluten, irritable bowel syndrome, GFD, IBS, meta-analysis
Citation: Arabpour E, Alijanzadeh D, Sadeghi A, Khoshdel S, Hekmatdoost A, Kord-Varkaneh H and Abdehagh M (2023) Gluten restriction in irritable bowel syndrome, yes or no?: a GRADE-assessed systematic review and meta-analysis. Front. Nutr. 10:1273629. doi: 10.3389/fnut.2023.1273629
Edited by:
Silvia Salvatore, University of Insubria, ItalyReviewed by:
Saloni Sharma, National Agri-Food Biotechnology Institute, IndiaStefano Guandalini, The University of Chicago, United States
Copyright © 2023 Arabpour, Alijanzadeh, Sadeghi, Khoshdel, Hekmatdoost, Kord-Varkaneh and Abdehagh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Amir Sadeghi, YW1pcnNhZGVnaGltZEB5YWhvby5jb20=; Azita Hekmatdoost, YV9oZWttYXQyMDAwQHlhaG9vLmNvbQ==
†ORCID: Erfan Arabpour, https://orcid.org/0000-0003-0557-1278
Dorsa Alijanzadeh, https://orcid.org/0000-0002-8568-133X
Amir Sadeghi, https://orcid.org/0000-0002-9580-2676
Hamed Kord-Varkaneh, https://orcid.org/0000-0001-7675-4405
Mohammad Abdehagh, https://orcid.org/0000-0002-7177-1633
 Erfan Arabpour
Erfan Arabpour Dorsa Alijanzadeh
Dorsa Alijanzadeh Amir Sadeghi
Amir Sadeghi Sina Khoshdel
Sina Khoshdel Azita Hekmatdoost
Azita Hekmatdoost Hamed Kord-Varkaneh
Hamed Kord-Varkaneh Mohammad Abdehagh1†
Mohammad Abdehagh1†