
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 08 January 2024
Sec. Nutrition and Metabolism
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1251861
This article is part of the Research Topic Nutritional Approaches in Chronic Liver Diseases View all 17 articles
 Pushpamala Ramaiah1*
Pushpamala Ramaiah1* Kamilya Jamel Baljon1
Kamilya Jamel Baljon1 Sana A. Alsulami1
Sana A. Alsulami1 Grace M. Lindsay1
Grace M. Lindsay1 Lathamangeswari Chinnasamy2
Lathamangeswari Chinnasamy2Objectives: There are only limited studies investigating the impact of dietary quality indicators, such as dietary quality index (DQI), dietary diversity score (DDS), and alternative healthy eating index (AHEI), on metabolic dysfunction-associated fatty liver disease (MASLD). Furthermore, these indicators may have different components that could lead to varying results. Therefore, this study aims to assess the nutritional quality indicators and their potential association with MASLD.
Methods: The study included 128 recently diagnosed MASLD patients and 256 controls aged between 20 and 60 years. The dietary intake of participants was evaluated using a validated semi-quantitative food frequency questionnaire that consisted of 168 items. In this study, the method used to evaluate dietary diversity was based on five main food groups, specifically bread and grains, vegetables, fruits, meat, and dairy. The AHEI-2010 was computed using data collected from the FFQ.
Results: After adjusting for confounders in the fully adjusted model, a significant negative correlation was observed between DDS and the risk of MASLD (OR 0.41, 95% CI 0.20, 0.97). Participants in the top quartile of AHEI had a 76% lower risk of MASLD compared with those in the bottom quartile after controlling for all potential confounders in the fully adjusted model (OR 0.24, 95% CI 0.12, 0.56).
Conclusion: The results of our study suggest that there is a significant association between adherence to a high-diversity diet and a reduced likelihood of developing MASLD. Similarly, we observed a similar association between adherence to the AHEI diet and a lower risk of MASLD.
Metabolic dysfunction-associated fatty liver disease (MASLD) is a prevalent cause of liver abnormalities worldwide and has become increasingly common in Asia in recent years (1–3). Its global prevalence is estimated to be between 20 and 30% in Western countries and 5% and 18% in Asia (2). This disease can lead to several liver abnormalities, including non-alcoholic steatohepatitis (NASH), cirrhosis, liver failure, and liver cancer, and is believed to be the primary cause of cirrhosis of the liver (4, 5). The strong correlation between MASLD, obesity, and metabolic syndrome is well established, and the disease is also an independent risk factor for cardiovascular diseases (5, 6). Therefore, identifying risk factors for fattyliver disease is crucial. The increasing incidence of MASLD in Asia makes it particularly important to understand the risk factors associated with the disease in this region. It is essential to continue researching this disease to develop effective prevention and treatment strategies, to reduce the burden of MASLD worldwide.
Lifestyle interventions, particularly a well-balanced diet, have been found to be significantly associated with preventing and managing MASLD (7). However, it is important to understand the complete composition of dietary intake as an alternative approach to establishing a link between diet and disease (8). This method considers the collaborative and opposing interactions of different dietary components and addresses the limitation of studying individual dietary components (8). By evaluating the overall dietary pattern, researchers can examine the combined effect of multiple nutrients on health outcomes, including MASLD. It can also provide a more comprehensive understanding of the role of diet in the development and progression of MASLD. Therefore, the assessment of dietary diversity and quality, as well as the identification of specific dietary patterns, is essential in the prevention and management of MASLD. A recent study showed that higher adherence to a nutritional pattern characterized by fructose, vitamin C, vitamin A, pyridoxine, and potassium, primarily from fruits, vegetables, and nuts, is inversely associated with MASLD risk (9). Another study indicated that healthy and Western dietary patterns may be associated with the risk of MASLD. It was stated that these results can be used for developing interventions in order to promote healthy eating for the prevention of MASLD (10).
Dietary Quality Indices (DQIs) such as alternative healthy eating index (AHEI) and dietary diversity score (DDS) have been developed to provide an overall picture of chronic nutritional intake, providing insight into the characteristics of diet-related diseases (11–13). The Dietary Diversity Score (DDS) is an index used to evaluate the overall dietary intake. It is associated with a higher consumption of macronutrients and micronutrients, better diet adequacy, and higher intake of fiber, antioxidants, and other nutrients (14). Previous research has shown that a higher DDS can help reduce certain risk factors associated with MASLD, such as diabetes (15), hypertension, and cardiovascular risk factors (16). These findings suggest that a diverse diet can provide the necessary nutrients to maintain good health and reduce the risk of chronic diseases. Therefore, evaluating dietary diversity is important in developing effective strategies for preventing and managing MASLD.
To the best of our knowledge, there are only limited studies investigating the impact of dietary quality indicators, such as DQI, DDS, and AHEI, on MASLD. Furthermore, these indicators may have different components that could lead to varying results. Therefore, this study aims to assess the nutritional quality indicators and their potential association with metabolic dysfunction-associated fatty liver disease in a case–control study. By analyzing the dietary habits of individuals with and without MASLD, this study provides a better understanding of the role of diet quality in the development and prevention of the disease in this population.
This was a cross-sectional study conducted at Umm Al-Qura University Medical Center, Makkah, Kingdom of Saudi Arabia, in patients attending Liver and Gastroenterology Clinic. The research study enrolled 128 individuals who had been recently diagnosed with MASLD and 256 healthy controls ranging in age from 20 to 60 years old. Individuals who were diagnosed with fatty liver based on laboratory tests and liver ultrasound indicating the presence of steatosis were included in the fatty liver group. The diagnosis of fatty liver was made by a specialist doctor. MASLD was defined as elevated liver enzymes, specifically alanine aminotransferase (ALT) levels >31 mg/dl and 41 mg/dl and aspartate aminotransferase (AST) levels >31 mg/dl and 47 g/dl in women and men, respectively. On the other hand, healthy individuals who had normal laboratory test results (ALT levels <31 UI/L and 41 UI/L and AST levels < 31 UI/L and 37 UI/L in women and men, respectively) and normal liver sonography indicating no stages of hepatic steatosis were considered as the control group (17).
The study excluded participants who had specific dietary habits due to medical conditions or weight loss and those with certain medical conditions such as kidney and liver disease (e.g., viral infections, autoimmune liver disease, hemochromatosis, Wilson's disease, and alcoholic fatty liver disease), cardiovascular disease, diabetes mellitus and malignancies, thyroid disease, and autoimmune diseases. Additionally, individuals taking drugs that could harm the liver or promote weight gain were also excluded. The study also excluded participants who completed <35 items on the food frequency questionnaire or underreported/overreported their daily energy intake (<800 kcal or more than 4,500 kcal per day), but these participants were replaced with the new ones. All participants provided informed written consent before being included in the study.
The dietary intake of the participants was evaluated using a validated semi-quantitative food frequency questionnaire that consisted of 168 items (18). Participants were asked to report their average food consumption over the past few years by selecting one of the following options: never or less than once a month, 3–4 times a month, once a week, 2–4 times a week, 5–6 times a week, once a day, 2–3 times a day, 4–5 times a day, or 6 times or more a day. The amount of each food item was converted into grams using standard household measurements, and the frequencies of consumed foods were transformed into daily intakes. The nutrient composition of all foods was determined using modified Nutritionist IV software, which provided information on EPA, DHA, sodium levels, and other micronutrients (19). Additionally, the National Nutrient Database of the US Department of Agriculture (USDA) was used in other studies to obtain daily nutrient information such as EPA and DHA for each participant (20). The N4 software output was used to obtain the sodium content of the food. The FFQ questionnaire also included an item on the salt intake of participants. The use of a standardized questionnaire and food composition tables allowed for the accurate assessment of the dietary intake of participants and ensured that the data obtained were reliable and comparable. The smoking status of the study subjects was obtained using the results of a general questionnaire that the subjects completed. Data on physical activity were obtained via a short form of the validated International Physical Activity Questionnaire (IPAQ), which was presented as metabolic equivalent task-minutes per week (MET-min/week).
The method used to evaluate dietary diversity in this study was based on the approach developed by Kant et al. (21, 22). This study considered five main food groups, which were derived from the USDA Food Guide Pyramid, specifically bread and grains, vegetables, fruits, meat, and dairy. These food groups were further divided into 23 subgroups to capture the diversity within each group. To determine the diversity score for each group, the consumption of half a serving of each subgroup was considered. Each of the five food groups could receive a maximum diversity score of 2 out of 10 (5 × 2 = 10). The total diversity score was calculated by summing up the scores from each of the five main food groups. The methodology facilitated a thorough evaluation of the extent of dietary variety and furnished significant perspectives on the general dietary patterns of the subjects.
The AHEI-2010 was computed using data collected from the FFQ. This method incorporates various aspects of the original HEI developed by Kennedy et al. (23, 24) and considers eleven components, namely, fruits, vegetables, whole grains, nuts and legumes, long-chain n-3 fats (DHA and EPA), PUFA, wine consumption, sugar-sweetened drinks and fruit juice, red and processed meats, trans-fat, and Na intake. However, since our database lacked data on wine consumption and trans-fat, only nine components were evaluated in our study. Each individual was assigned a score for each component based on their decile ranking, with the highest decile receiving a score of 10 and the lowest decile receiving a score of 1. Individuals in other deciles were given corresponding scores. Conversely, individuals with the highest intake of sugar-sweetened drinks and fruit juice, red and processed meats, and Na were given a score of 1, while those with the lowest consumption of these components were given a score of 10. The total AHEI score for each participant was then calculated by summing up the scores for these ten components, which ranged from 9 to 81. This method allowed for the evaluation of dietary quality based on multiple components and provided a comprehensive assessment of the overall dietary habits of participants.
Statistical analyses were performed using Statistical Package for Social Sciences software version 21 (SPSS Inc., Chicago, IL, USA). The significance level was determined as P < 0.05. The normality of variables was checked by Kolmogorov–Smirnov and histogram tests. The study compared the general characteristics and dietary intakes of cases and controls using appropriate statistical tests such as independent sample t-test and χ2. After constructing the DDS and AHEI scores as described previously, energy-adjusted scores were obtained using the residual method (25). Participants were then categorized into quartiles based on the cutoff points obtained from the control group, and one-way ANOVA and χ2 tests were used to assess continuous and categorical variables across these quartiles. The association of DDS and AHEI with MASLD was evaluated using binary logistic regression in different models, with the first quartile of DDS and AHEI serving as the reference category.
The general characteristics and dietary intake of the participants are presented in Table 1. There was no significant difference between the two study groups in terms of age and gender (p > 0.05). However, compared with the control group, MASLD patients had a higher BMI, were more smokers, and had less physical activity (p < 0.05). In addition, MASLD patients had higher dietary intakes of calories, carbohydrates, fats, refined grains, high-fat dairy, and red and processed meats than controls (p < 0.05). The control group had higher dietary intakes of whole grains, vegetables, vitamin C, selenium, vitamin E, and vitamin A than MASLD patients (p < 0.05). There were no significant differences between the two groups in dietary intake.
Table 2 presents the dietary intakes of cases and controls in various quartiles of DDS and AHEI scores. Individuals in the top quartile of DDS had higher consumption of fruits, vegetables, carbohydrates, protein, fiber, whole grains, nuts, and legumes when compared with those in the bottom quartile. Moreover, those in the fourth quartile of AHEI had lower intakes of fat, refined grains, high-fat dairy products, and red and processed meat in comparison to participants in the first quartile. No other significant differences were observed in terms of dietary intakes across quartiles of DDS and AHEI scores.
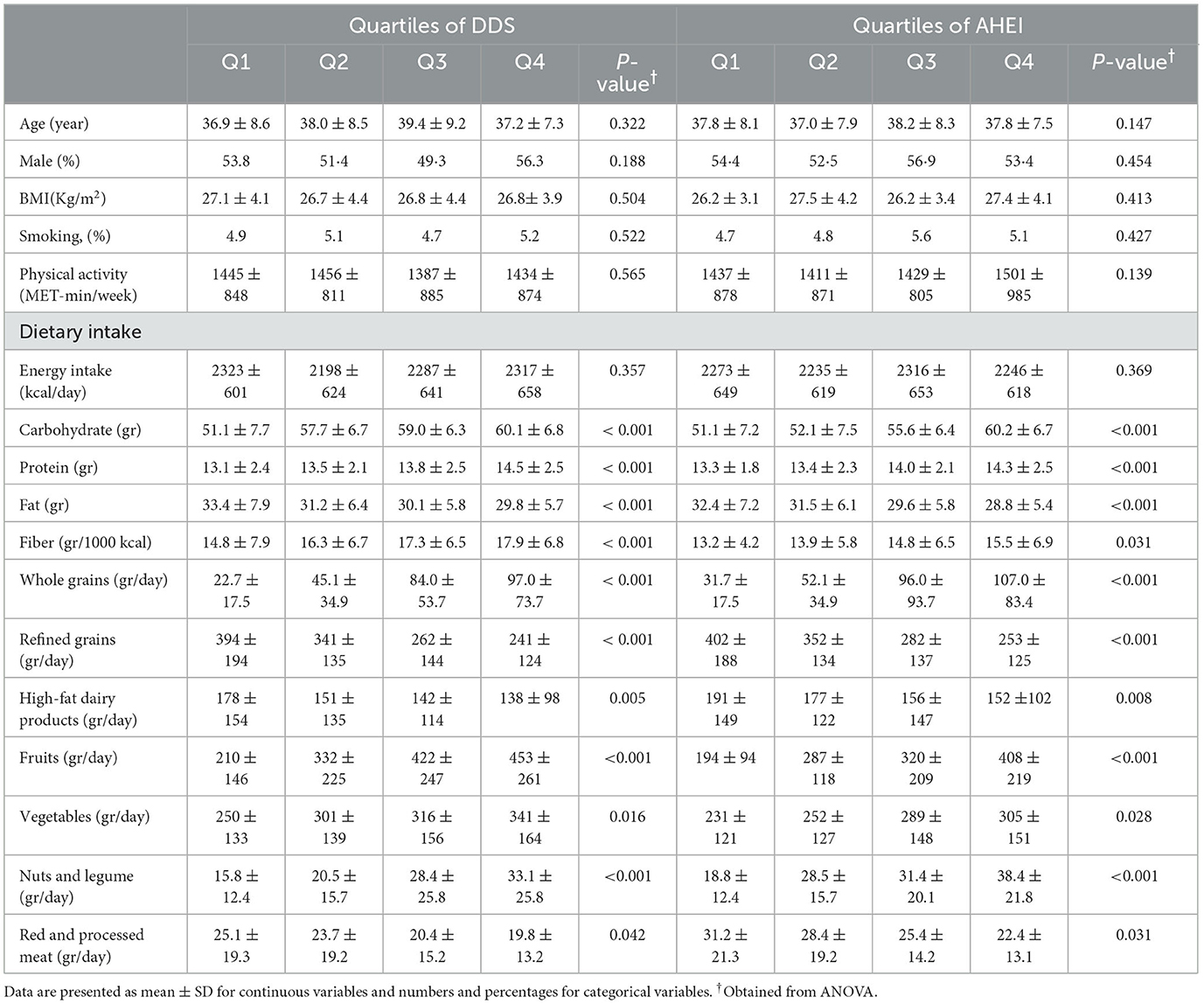
Table 2. Dietary and nutrient intakes of study participants across quartiles (Q) of DDS and AHEI scores.
Table 3 shows the multivariable-adjusted OR and 95% CI for MASLD across quartiles of DDS and AHEI. After adjusting for age, sex, body mass index, smoking, and physical activity, a significant negative correlation was observed between DDS and the risk of MASLD (OR 0.44, 95% CI 0.19, 0.94). This finding remained consistent after further controlling for dietary energy intake, with participants in the highest quartile of DDS being 59% less likely to have MASLD than those in the lowest quartile (OR 0.41, 95% CI 0.20, 0.97). Additionally, a significant inverse association was found between AHEI and the odds of MASLD. Participants in the top quartile of AHEI had a 76% lower risk of MASLD compared with those in the bottom quartile after controlling for all potential confounders in the fully adjusted model (OR 0.24, 95% CI 0.12, 0.56).
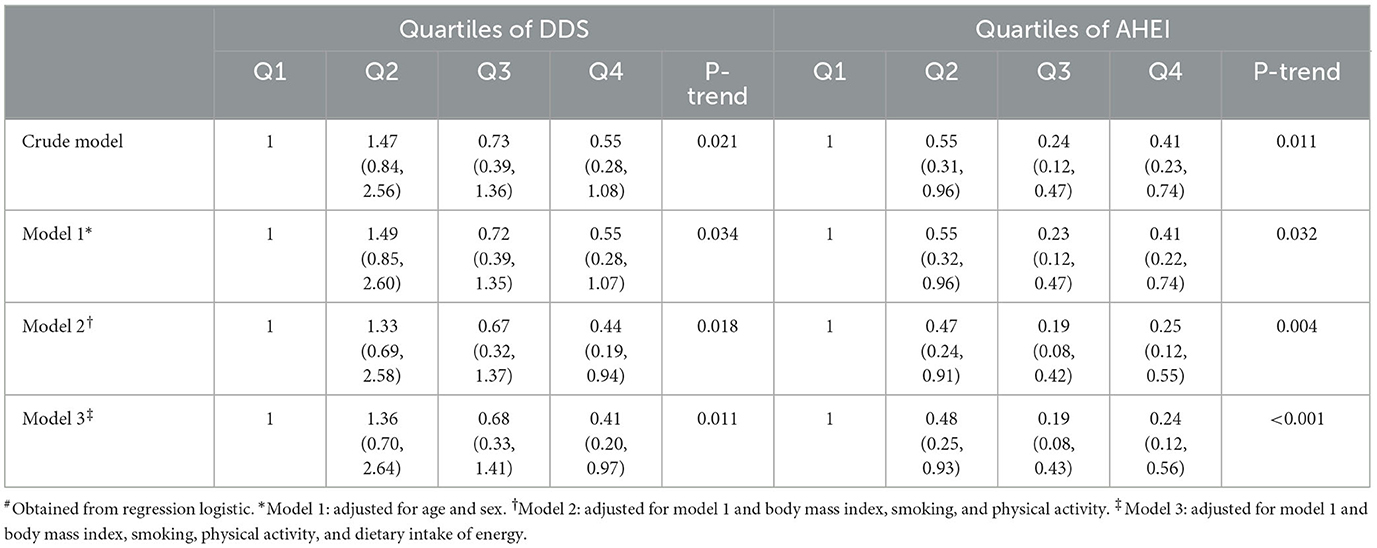
Table 3. Risk for MASLD according to quartiles (Q) of DDS and AHEI scores (odds ratios and 95 % confidence intervals)#.
Our study revealed that there is a negative relationship between the Dietary Diversity Score (DDS) and the risk of MASLD. We took into account several variables that could potentially affect this relationship, such as age, sex, body mass index, smoking, physical activity, and energy intake, and found an inverse association between DDS and MASLD. We also observed a similar inverse relationship between AHEI and MASLD, both before and after controlling for the aforementioned confounders.
Numerous studies have shown that an overall dietary pattern, rather than focusing on individual foods or nutrients, is a better predictor of overall diet quality and is associated with various diseases. In particular, DDS and AHEI have been used as indicators of diet quality in relation to non-communicable diseases such as cardiovascular disease, polycystic ovaries, and some cancers (26–29). In the present study, a high DDS was found to be associated with decreased odds of MASLD. This finding is consistent with previous research that has shown an inverse association between DDS and the risk of diabetic nephropathy (29) and bladder cancer (30). In another study, by emphasizing the higher diversity scores for vegetables and fewer diversity scores for meat and refined grains, high DDS is inversely correlated with the risk of MASLD (15).
One possible explanation for the protective association of a diverse diet against MASLD is its high nutrient content, including antioxidants. Several studies have demonstrated an inverse association between dietary intake of antioxidants and the risk of MASLD (31, 32). Additionally, diets with a high DDS tend to be rich in fruits and vegetables, which have also been shown to be protective against MASLD (33). Such diets are also typically high in fiber, which can reduce the risk of MASLD (34, 35). However, it should be noted that not all studies have found a significant association between dietary diversity and the risk of certain diseases, such as breast cancer (36). In some cases, confounding factors may not have been adequately adjusted to determine the independent association between dietary diversity and disease risk. Overall, increasing the diversity score of one's diet by emphasizing higher diversity scores for vegetables and fewer diversity scores for meat and refined grains may be beneficial to managing MASLD (15).
The current study found that a higher level of adherence to the AHEI was associated with a reduced likelihood of MASLD. Previous research has also shown that healthy dietary patterns are associated with a lower risk of MASLD, while Western dietary patterns are linked to an increased risk of this disease (10). In a large population-based study in Germany, individuals with the highest AHEI scores were less likely to develop colorectal cancer compared with those with the lowest scores (37). In a meta-analysis of observational studies, a high adherence to the AHEI dietary pattern was associated with a reduced risk of all-cause mortality and cardiovascular and cancer mortality (38).
Additionally, a study found that AHEI scores were significantly higher among individuals with high levels of sensitive C-reactive protein (Hs-CRP), which is a marker of inflammation in the body (39). A systematic review and meta-analysis of observational studies also showed that high adherence to the AHEI was associated with a reduced risk of cancer mortality (38). Fruit consumption has also been shown to play a preventive role in the incidence of MASLD (33, 40). Furthermore, dietary intake of antioxidants is higher among individuals who have greater adherence to the AHEI (41). A high AHEI score is also associated with a lower intake of red and processed meats, which are known risk factors for MASLD (42, 43).
This study has several limitations that should be taken into consideration when interpreting the results. First, the study design was a case–control study, which is prone to several types of bias, including selection and recall bias. Although case–control studies are cost-effective and quick to conduct, they are highly vulnerable to bias. Recall bias is a particular concern in this study, as cases may recall their previous diet differently in light of their MASLD diagnosis. Additionally, dietary assessment occurred after diagnosis, which can further exacerbate recall bias. It is also possible that cases may have altered their diet before diagnosis due to early symptoms of the disease, leading to attenuation of the estimates. However, it is worth noting that MASLD-related symptoms may prompt patients to consume healthier foods rather than unhealthy ones. Furthermore, with all epidemiological studies that use food frequency questionnaire (FFQ), misclassification of study participants is unavoidable. Despite the efforts of the researchers to control for several confounding factors, the possibility of residual confounding cannot be entirely ruled out. It is important to acknowledge these limitations when interpreting the findings of this study and consider them in any future research in this area.
The results of our study suggest that there is a significant association between adherence to a high-diversity diet and a reduced likelihood of developing MASLD. Specifically, our findings indicate that individuals who closely followed a diverse diet had lower odds of developing MASLD. Similarly, we observed a similar association between adherence to the AHEI diet and a lower risk of MASLD. Participants who had greater adherence to the AHEI diet were found to have a lower likelihood of developing MASLD compared with those who had the lowest adherence to this dietary pattern. These results highlight the importance of consuming a diverse and healthy diet in reducing the risk of MASLD.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical approval of this study was obtained from the Ethical Committee of Umm Al-Qura University (ID: HAPO-02-K-012-2023-02-345) Makkah, Kingdom of Saudi Arabia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
PR and KJ conceptualized and designed the study and supervised the project. SA participated in the data acquisition and literature review of the articles. GL analyzed and interpreted the data. PR, KJ, and LC drafted the initial manuscript. All authors approved the final version of the manuscript.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Amarapurkar DN, Hashimoto E, Lesmana LA, Sollano JD, Chen PJ, Goh KL, et al. How common is non-alcoholic fatty liver disease in the Asia–Pacific region and are there local differences? J Gastroenterol Hepatol. (2007) 22:788–93. doi: 10.1111/j.1440-1746.2007.05042.x
2. Masarone M, Federico A, Abenavoli L, Loguercio C, Persico M. Non alcoholic fatty liver: epidemiology and natural history. Rev Recent Clin Trials. (2014) 9:126–33. doi: 10.2174/1574887109666141216111143
3. Chitturi S, Wong VWS, Farrell G. Nonalcoholic fatty liver in Asia: firmly entrenched and rapidly gaining ground. J Gastroenterol Hepatol. (2011) 26:163–72. doi: 10.1111/j.1440-1746.2010.06548.x
4. Caldwell SH, Oelsner DH, Iezzoni JC, Hespenheide EE, Battle EH, Driscoll CJ. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. (1999) 29:664–9. doi: 10.1002/hep.510290347
5. Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. (2006) 43:S99–S112. doi: 10.1002/hep.20973
6. Wong VW-S, Wong GL-H, Yip GW-K, Lo AO-S, Limquiaco J, Chu WC-W, et al. Coronary artery disease and cardiovascular outcomes in patients with non-alcoholic fatty liver disease. Gut. (2011) 60:1721–7. doi: 10.1136/gut.2011.242016
7. Musso G, Gambino R, De Michieli F, Cassader M, Rizzetto M, Durazzo M, et al. Dietary habits and their relations to insulin resistance and postprandial lipemia in nonalcoholic steatohepatitis. Hepatology. (2003) 37:909–16. doi: 10.1053/jhep.2003.50132
8. Allard JP, Aghdassi E, Mohammed S, Raman M, Avand G, Arendt BM, et al. Nutritional assessment and hepatic fatty acid composition in non-alcoholic fatty liver disease (NAFLD): a cross-sectional study. J Hepatol. (2008) 48:300–7. doi: 10.1016/j.jhep.2007.09.009
9. Salehi-Sahlabadi A, Teymoori F, Ahmadirad H, Mokhtari E, Azadi M, Seraj SS, et al. Nutrient patterns and non-alcoholic fatty liver disease in Iranian Adul: a case-control study. Front Nutr. (2022) 9:977403. doi: 10.3389/fnut.2022.977403
10. Salehi-Sahlabadi A, Sadat S, Beigrezaei S, Pourmasomi M, Feizi A, Ghiasvand R, et al. Dietary patterns and risk of non-alcoholic fatty liver disease. BMC Gastroenterol. (2021) 21:1–12. doi: 10.1186/s12876-021-01612-z
11. Alavian SM, Esmaillzadeh A, Adibi P, Azadbakht L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD). Hepatitis Monthly. (2013) 13:10943. doi: 10.5812/hepatmon.10943
12. Caswell BL, Talegawkar SA, Siamusantu W, West Jr KP, Palmer AC. A 10-food group dietary diversity score outperforms a 7-food group score in characterizing seasonal variability and micronutrient adequacy in rural Zambian children. J Nutr. (2018) 148:131–9. doi: 10.1093/jn/nxx011
13. Shiao SPK, Grayson J, Lie A, Yu CH. Predictors of the healthy eating index and glycemic index in multi-ethnic colorectal cancer families. Nutrients. (2018) 10:674. doi: 10.3390/nu10060674
14. Doustmohammadian A, Amirkalali B, Gholizadeh E, Khoonsari M, Faraji AH, Nikkhah M, et al. Mediators of dietary diversity score (DDS) on NAFLD in Iranian adults: a structural equation modeling study. Eur J Clin Nutr. (2023) 77:370–9. doi: 10.1038/s41430-022-01240-0
15. Ebrahimi Mousavi S, Dehghanseresht N, Dashti F, Khazaei Y, Salamat S, Asbaghi O, et al. The association between dietary diversity score and odds of nonalcoholic fatty liver disease: a case-control study. Eur J Gastroenterol Hepatol. (2022) 34:678–85. doi: 10.1097/MEG.0000000000002344
16. Azadbakht L, Mirmiran P, Esmaillzadeh A, Azizi F. Dietary diversity score and cardiovascular risk factors in Tehranian adults. Public Health Nutr. (2006) 9:728–36. doi: 10.1079/PHN2005887
17. Pezeshki A, Safi S, Feizi A, Askari G, Karami F. The effect of green tea extract supplementation on liver enzymes in patients with nonalcoholic fatty liver disease. Int J Prev Med. (2016) 7.173051: 1doi: 10.4103/2008-7802.173051
18. Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Dietary patterns, insulin resistance, and prevalence of the metabolic syndrome in women. Am J Clin Nutr. (2007) 85:910–8. doi: 10.1093/ajcn/85.3.910
19. Ghafarpour M, Houshiar-Rad A, Kianfar H, Ghaffarpour M. The Manual for Household Measures, Cooking Yields Factors and Edible Portion of Food. Tehran: Keshavarzi Press (1999).
20. Bowman SA, Friday JE, Moshfegh AJ. MyPyramid Equivalents Database, 2.0 for USDA Survey Foods, 2003–2004: Documentation and User Guide. Washington, DC: US Department of Agriculture (2008).
21. Kant AK, Schatzkin A, Harris TB, Ziegler RG, Block G. Dietary diversity and subsequent mortality in the first national health and nutrition examination survey epidemiologic follow-up study. Am J Clin Nutr. (1993) 57:434–40. doi: 10.1093/ajcn/57.3.434
22. Kant AK, Schatzkin A, Ziegler RG. Dietary diversity and subsequent cause-specific mortality in the NHANES I epidemiologic follow-up study. J Am Coll Nutr. (1995) 14:233–8. doi: 10.1080/07315724.1995.10718501
23. Kennedy E. Putting the pyramid into action: the healthy eating index and food quality score. Asia Pacific J Clin Nutr. (2008) 17:1–14. doi: 10.6133/apjcn.2008.17.s1.17
24. Kennedy E, Ohls J, Carlson S, Fleming K. The healthy eating index: design and applications. J Am Diet Assoc. (1995) 95:1103–8. doi: 10.1016/S0002-8223(95)00300-2
25. Newby P, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev. (2004) 62:177–203. doi: 10.1111/j.1753-4887.2004.tb00040.x
26. Arem H, Reedy J, Sampson J, Jiao L, Hollenbeck AR, Risch H, et al. The Healthy Eating Index 2005 and risk for pancreatic cancer in the NIH–AARP study. J Natl Cancer Inst. (2013) 105:1298–305. doi: 10.1093/jnci/djt185
27. Aigner A, Becher H, Jacobs S, Wilkens LR, Boushey CJ, Le Marchand L, et al. Low diet quality and the risk of stroke mortality: the multiethnic cohort study. Eur J Clin Nutr. (2018) 72:1035–45. doi: 10.1038/s41430-018-0103-4
28. Lim H, Cho G, Kim S. Evaluation of nutrient intake and diet quality of gastric cancer patients in Korea. Nutr Res Pract. (2012) 6:213–20. doi: 10.4162/nrp.2012.6.3.213
29. Rezazadegan M, Mirjalili F, Jalilpiran Y, Aziz M, Jayedi A, Setayesh L, et al. The association between dietary diversity score and odds of diabetic nephropathy: a case-control study. Front Nutr. (2022) 9:504. doi: 10.3389/fnut.2022.767415
30. Isa F, Xie L-P, Hu Z, Zhong Z, Hemelt M, Reulen RC, et al. Dietary consumption and diet diversity and risk of developing bladder cancer: results from the South and East China case–control study. Cancer Causes Control. (2013) 24:885–95. doi: 10.1007/s10552-013-0165-5
31. Lotfi A, Saneei P, Hekmatdost A, Salehisahlabadi A, Shiranian A, Ghiasvand R. The relationship between dietary antioxidant intake and physical activity rate with nonalcoholic fatty liver disease (NAFLD): a case–Control study. Clin Nutr ESPEN. (2019) 34:45–9. doi: 10.1016/j.clnesp.2019.09.004
32. Ore A, Akinloye OA. Oxidative stress and antioxidant biomarkers in clinical and experimental models of non-alcoholic fatty liver disease. Medicina. (2019) 55:26. doi: 10.3390/medicina55020026
33. Kim S-A, Shin S. Fruit and vegetable consumption and non-alcoholic fatty liver disease among Korean adults: a prospective cohort study. J Epidemiol Commun Health. (2020) 74:1035–42. doi: 10.1136/jech-2020-214568
34. Zhao H, Yang A, Mao L, Quan Y, Cui J, Sun Y. Association between dietary fiber intake and non-alcoholic fatty liver disease in adults. Front Nutr. (2020) 7:593735. doi: 10.3389/fnut.2020.593735
35. Zhang S, Zhao J, Xie F, He H, Johnston LJ Dai X, et al. Dietary fiber-derived short-chain fatty acids: a potential therapeutic target to alleviate obesity-related nonalcoholic fatty liver disease. Obesity Rev. (2021) 22:e13316. doi: 10.1111/obr.13316
36. Ko K-P, Kim S-W, Ma SH, Park B, Ahn Y, Lee JW, et al. Dietary intake and breast cancer among carriers and noncarriers of BRCA mutations in the Korean hereditary breast cancer study. Am J Clin Nutr. (2013) 98:1493–501. doi: 10.3945/ajcn.112.057760
37. Erben V, Carr PR, Holleczek B, Stegmaier C, Hoffmeister M, Brenner H. Dietary patterns and risk of advanced colorectal neoplasms: a large population based screening study in Germany. Prev Med. (2018) 111:101–9. doi: 10.1016/j.ypmed.2018.02.025
38. Onvani S, Haghighatdoost F, Surkan P, Larijani B, Azadbakht L. Adherence to the healthy eating index and alternative healthy eating index dietary patterns and mortality from all causes, cardiovascular disease and cancer: a meta-analysis of observational studies. J Hum Nutr Dietetics. (2017) 30:216–26. doi: 10.1111/jhn.12415
39. Khakpouri S, Safari M, Ghazizadeh H, Parizadeh SMR, Nematy M, Tayefi M, et al. The relationship between the healthy eating index and an alternate healthy eating index with the risk factors for cardiovascular disease in a population from northeastern. Transl. Metab. Syndr. Res. (2019) 2:1–6. doi: 10.1016/j.tmsr.2019.05.001
40. Berná G, Romero-Gomez M. The role of nutrition in non-alcoholic fatty liver disease: pathophysiology and management. Liver Int. (2020) 40:102–8. doi: 10.1111/liv.14360
41. Mirmiran P, Teymoori F, Asghari G, Azizi F. Diet quality and nonalcoholic fatty liver disease. Hepatobiliary Surg Nutr. (2019) 8:262. doi: 10.21037/hbsn.2018.12.14
42. Zelber-Sagi S, Ivancovsky-Wajcman D, Isakov NF, Webb M, Orenstein D, Shibolet O, et al. High red and processed meat consumption is associated with non-alcoholic fatty liver disease and insulin resistance. J Hepatol. (2018) 68:1239–46. doi: 10.1016/j.jhep.2018.01.015
Keywords: alternative healthy eating index, AHEI, dietary diversity score, DDS, metabolic dysfunction-associated fatty liver disease, MASLD, dietary quality indices, DQI
Citation: Ramaiah P, Jamel Baljon K, Alsulami SA, Lindsay GM and Chinnasamy L (2024) Diet quality indices and odds of metabolic dysfunction-associated fatty liver disease: a case-control study. Front. Nutr. 10:1251861. doi: 10.3389/fnut.2023.1251861
Received: 02 July 2023; Accepted: 02 November 2023;
Published: 08 January 2024.
Edited by:
Santiago Rodríguez Villafuerte, Hospital Vozandes, EcuadorReviewed by:
Te-Chih Wong, Chinese Culture University, TaiwanCopyright © 2024 Ramaiah, Jamel Baljon, Alsulami, Lindsay and Chinnasamy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pushpamala Ramaiah, cHVzaHBhbWFsYS5yYW1haWFoLm51cnNlQGdtYWlsLmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.