
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 05 January 2024
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1249638
This article is part of the Research Topic Protective and Healing Effects of Natural Compounds on Brain Disease and Brain Injury View all 4 articles
Background: The nutrition support team (NST) works to improve malnutrition in hospitalized patients, and its role is expanding as more hospitals adopt NST. This study aimed to identify the clinical characteristics of NST-referred patients admitted to a tertiary hospital. The study focused on two groups: those who achieved the target calories, approximately 75% or more of their caloric needs relative to their body weight regardless of the period after the first NST referral, and those who improved their calorie intake 1 week after NST therapy. This study also analyzed the important factors affecting the achievement of target calorie intake and improvement in calorie intake to discover the focus of future NST therapy.
Methods: This study examined 1,171 adult patients (aged ≥18 years) who were referred to the NST from all the departments within a tertiary hospital at least twice, with a minimum one-week interval between referrals, between January 1, 2019, and December 31, 2020. The study participants consisted of patients receiving <75% of their required caloric intake at the time of their first NST referral. Patients were categorized and compared according to whether they achieved their target calorie intake regardless of the period after the first NST referral and whether they improved their calorie intake 1 week after the NST therapy. We then identified factors affecting target caloric achievement and improvement in calorie intake.
Results: The group that achieved the target calorie intake had a lower proportion of neuro department patients (31.3%), a higher proportion of patients receiving intensive care unit (ICU) care (31.9%), and a longer ICU stay (p < 0.001) than the group that did not achieve the target calorie intake. Neuro department admission negatively affected target caloric achievement [adjusted odds ratio (aOR) = 0.305, 95% confidence interval (CI) = 0.150–0.617], whereas the length of ICU stay positively affected target caloric achievement (aOR = 1.025, 95% CI = 1.007–1.043). The proportion of neuro department patients was also low (42.5%) in the group with improved calorie intake 1 week after NST therapy. Neuro department admission was a negative factor (aOR = 0.376, 95% CI = 0.264–0.537) affecting the improvement in calorie intake.
Conclusions: NST therapy significantly improved clinical outcomes for inpatients at nutritional risk. Because achieving target calories and improving calorie intake in neuro department patients is difficult, it is necessary to actively refer them to NST to achieve the target calories and improve calorie intake. Furthermore, because a longer ICU stay positively affects target calorie achievement, the system for ICU nutrition therapy should be expanded and implemented for general-ward patients, including neurological patients.
Developed countries, such as the United States, began establishing a nutrition support team (NST) in the late 1960s to improve the malnutrition issue of hospitalized patients (1). South Korea also began implementing intensive nutrition treatment in the late 1990s by creating teams of experts interested in nutrition support. As medical insurance began to cover nutrition treatment in August 2014, it became possible to run NST more systematically. Since then, many hospitals with inpatient beds get interested in organizing and operating NSTs, and the importance of NSTs is growing steadily. While the number of hospitals interested in NST therapy has increased, there is a lack of studies examining the qualitative benefits of NST therapy for the patient's nutrition and the critical factors for increasing nutritional intake (2).
Additionally, patients with neurological diseases are at higher risk of malnutrition due to factors like dysphagia, reduced consciousness, cognitive decline, muscle weakness, and neuropsychological issues (3). However, studies on specialized nutritional support methods for this patient group are currently limited. Therefore, the present study aimed to identify the future focus of NST therapy by analyzing how NST activities influence patients admitted to tertiary care institutions with an emphasis on neurological patients to achieve target calories or improve calorie intake, and critical factors affecting target caloric achievement and improvement in calorie intake.
This study included 5,153 adult patients (aged ≥18 years) referred to the NST from all the departments within a tertiary hospital between January 1, 2019 and December 31, 2020. Among them, 1,490 patients met the inclusion criteria by being referred to NST at least twice, with a minimum one-week interval between referrals. The exclusion criteria for this study encompassed patients who had adequate caloric intake (≥75% of required calories) from the time of the first referral. A total of 309 patients meeting this exclusion criterion were excluded from the analysis. Additionally, 10 patients with insufficient nutritional evaluation data were also excluded, resulting in the final analysis of data from 1,171 patients. Information on referred patients was analyzed retrospectively using electronic medical records and NST patient care sheets. This study was approved by the hospital's Institutional Review Board (2022-09-001). The requirement for consent was waived due to the study's retrospective nature (2022-09-001).
Indications for referral to NST were: (1) blood albumin level ≤ 3.0 g/dl, (2) receiving enteral nutrition (EN), (3) receiving parenteral nutrition (PN), (4) being treated in an intensive care unit (ICU), or (5) deemed to require intensive nutrition therapy based on the medical opinion of the treating physician.
This study evaluated each patient's baseline information, clinical characteristics, and clinical course using electronic medical records and NST patient care sheets. The baseline information included age, sex, body mass index (BMI), clinical department, and the primary care physician‘s NST team membership status. Clinical characteristics and courses included serum albumin levels (<3.0 g/dL), utilization of EN or PN, spontaneous feeding, nil per os status, ascites, edema, jaundice, dialysis, reduced appetite, difficulty chewing, difficulty swallowing, diarrhea, constipation, presence of pressure ulcers, the initial stage of pressure ulcers at first NST referral, change in the stage of pressure ulcers between first NST referral and discharge, provision ICU care, length of ICU care, and acute physiology and chronic health evaluation II score at ICU admission. Additionally the assessment involved daily caloric intake measured by a clinical nutritionist, achievement of target calories, number of weeks to achieve the target calories (only for patients who achieved it), improvement in calorie intake at the second NST referral 1 week after the first referral, and basic blood test results.
The daily caloric intake at the initial NST referral was not determined based on nutritional support. Subsequent nutritional support following the NST referral was administered according to the recommendations of the NST. Commercial formulas were used for both enteral and parenteral nutrition in adherence to this hospital regulations, with the specific type determined by factors such as the underlying disease (e.g., diabetes or kidney disease) and the type of intravenous line (peripheral or central). For patients engaging in spontaneous feeding, a total of 2100 kcal/day was supplied, including regular meals and provided snacks. The calorie requirement was calculated based on the individual patient's weight status, taking into account factors such as obesity or underweight.
Inpatient medical departments were categorized into the neuro (neurology and neurosurgery) and non-neuro (allergy and clinical immunology, cardiology, endocrinology, gastroenterology, hemato-oncology, infectology, nephrology, rheumatology, pulmonology, cardiothoracic surgery, general surgery, orthopedic surgery, and plastic surgery). They were also categorized into internal medicine departments (allergy and clinical immunology, cardiology, endocrinology, gastroenterology, hemato-oncology, infectology, nephrology, rheumatology, pulmonology, and neurology) and surgical departments (cardiothoracic surgery, general surgery, orthopedics, plastic surgery, and neurosurgery). When a primary care physician of patient completed NST-related training accredited by the Health Insurance Review & Assessment Service and actively participated as a member of the NST team, they were defined as members of the NST team. EN was limited to caloric supply through a feeding tube, such as a nasogastric or percutaneous endoscopic gastrostomy tube, whereas spontaneous feeding was defined as oral feeding without a tube. The presence and stage of a pressure ulcer were classified into five stages (stages 0–4) using the pressure ulcer assessment sheet in the medical records. The target calorie was defined as ≥75% of the caloric requirement based on weight-based calorie needs. Target caloric achievement was defined as attaining ≥75% of the calorie requirement regardless of the period it is achieved after the first NST referral. The calorie intake improvement was defined as any degree of enhancement in calorie provision when comparing the calorie supply at the second NST referral, referred 1 week after the first NST referral, to the initial calorie supply.
To compare patients' clinical characteristics and courses in this study, patients were divided into a “target caloric achievement group” and a “non- achievement group.” In addition, the patients were divided into a “calorie intake improvement group” and a “non- improvement group.” Then, this study compared the clinical characteristics and courses of the two groups respectively, and identified factors affecting the achievement of target calories and improvement in calorie intake.
First, this study observed differences in demographics, clinical characteristics, nutritional status, general conditions, and laboratory findings between target caloric achievement group and non- achievement group, and between calorie intake improvement group and non- improvement group. This study further analyzed factors that influenced the differences between the two groups, respectively. Pearson's chi-square or Fisher's exact test was used for categorical variables, whereas the t-test was used for continuous variables. Pearson's chi-square test was performed, and when the expected frequency of each cell was <5, >20% of the cells were interpreted as Fisher's exact test values. In addition, this study performed a multivariate logistic regression analysis to identify factors influencing the target caloric achievement group and calorie intake improvement group. Statistical significance was set at p < 0.05 (two-tailed). All statistical analyses were performed using SPSS (version 26.0; IBM Corp., Armonk, NY, USA).
This study analyzed and compared the target caloric achievement group with the non-achievement group, among the 1,171 patients referred to NST, aiming to determine the difference between the two groups (Table 1). Of all patients, 37.2% achieved their target calories within an average of approximately 1.62 weeks. The target caloric achievement group had more female patients (44.0% vs. 35.8%), was older (70.8 ± 13.8 vs. 68.9 ± 14.7), had a lower BMI (21.54 ± 3.69 vs. 22.85 ± 3.79), and had a higher proportion of non-neuro patients (69.0% vs. 44.1%) than the non-achievement group. Furthermore, the target caloric achievement group had a higher proportion of patients receiving treatment in the ICU (31.9% vs. 25.4%) and had longer ICU stay (29.87 ± 26.79 vs. 19.99 ± 17.26) than the non-achievement group. Notably, the target caloric achievement group had more physicians with NST training than the non-achievement group (31.0% vs. 25.6%). The target caloric achievement group had a lower proportion of those receiving EN (32.3% vs. 38.8%) and a higher proportion of those with low albumin levels (48.4% vs. 32.2%), receiving PN (60.6% vs. 51.8%), and fasting (56.4% vs. 48.2%) than the non-achievement group. In addition, the target caloric achievement group had a higher proportion of patients with edema (6.7% vs. 3.7%) than the non-achievement group; however, the proportions of patients with difficulty chewing (28.9% vs. 37.1%), difficulty swallowing (23.4% vs. 29.3%), and diarrhea (0.7% vs. 2.4%) were lower in the target caloric achievement group. The plasma hemoglobin and serum albumin levels were significantly (p < 0.001) lower in the target caloric achievement group than in the non-achievement group.
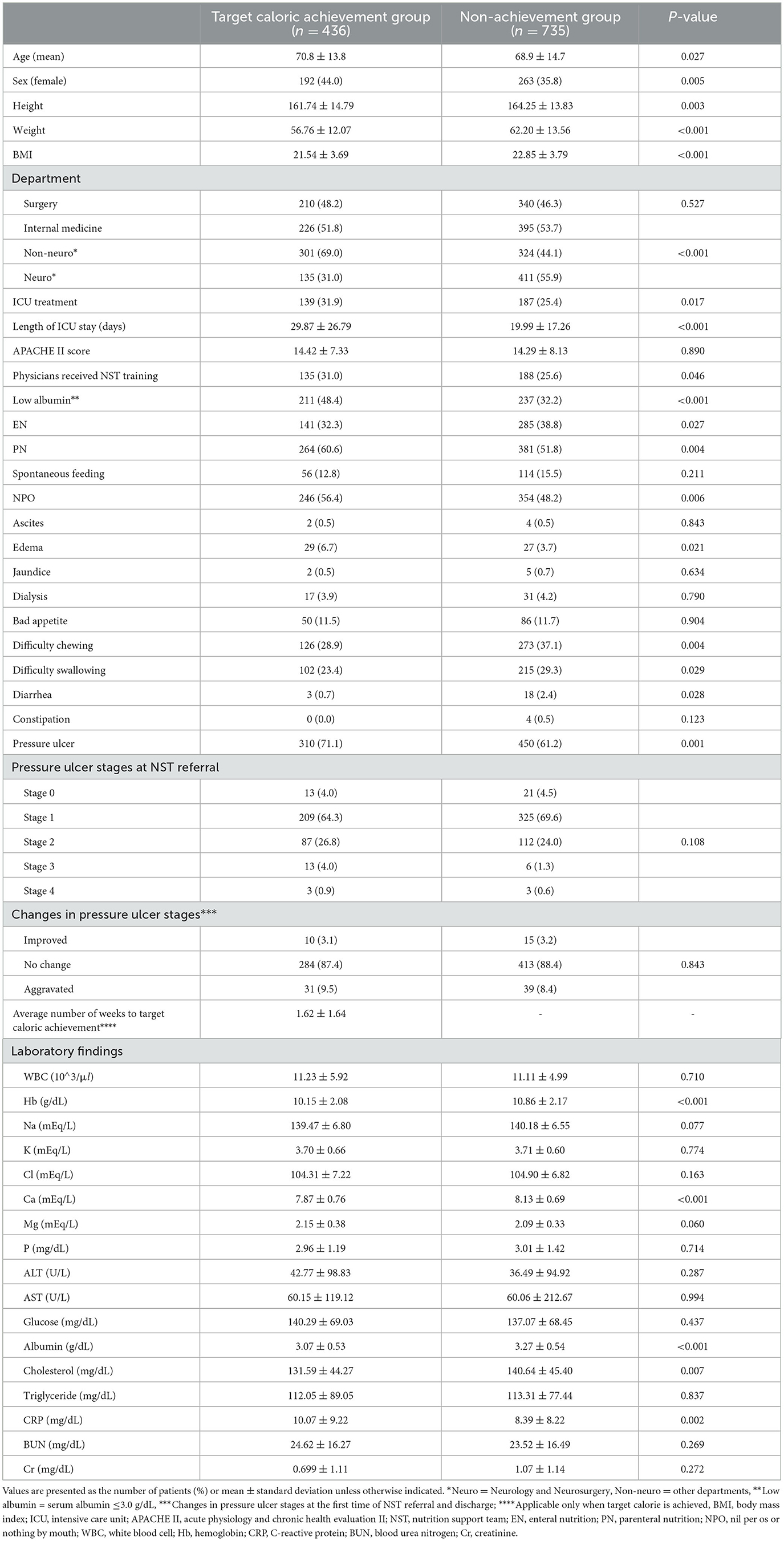
Table 1. Comparison of clinical characteristics between target caloric achievement group and non-achievement group.
This study analyzed and compared the calorie intake improvement group and the non-improvement group (Table 2). The calorie intake improvement group accounted for 73.6% of all patients referred to NST and had a higher proportion of female patients (40.7% vs. 33.7%), was older (70.3 ± 14.3 vs. 67.8 ± 14.7), and had a lower BMI (22.06 ± 3.77 vs. 23.19 ± 3.78) than the non-improvement group. The calorie intake improvement had a higher proportion of internal medicine (55.3% vs. 46.6%) and non-neuro (57.5% vs. 41.7%) patients than the non-improvement group. The calorie intake improvement group had a lower portion of patients receiving PN (50.6% vs. 67.6%) and those with diarrhea (1.3% vs. 3.2%) than the non-improvement group. For patients who achieved the target calories, the calorie intake improvement group achieved it faster than the non-improvement group (1.49 ± 1.66 vs. 2.71 ± 1.03).
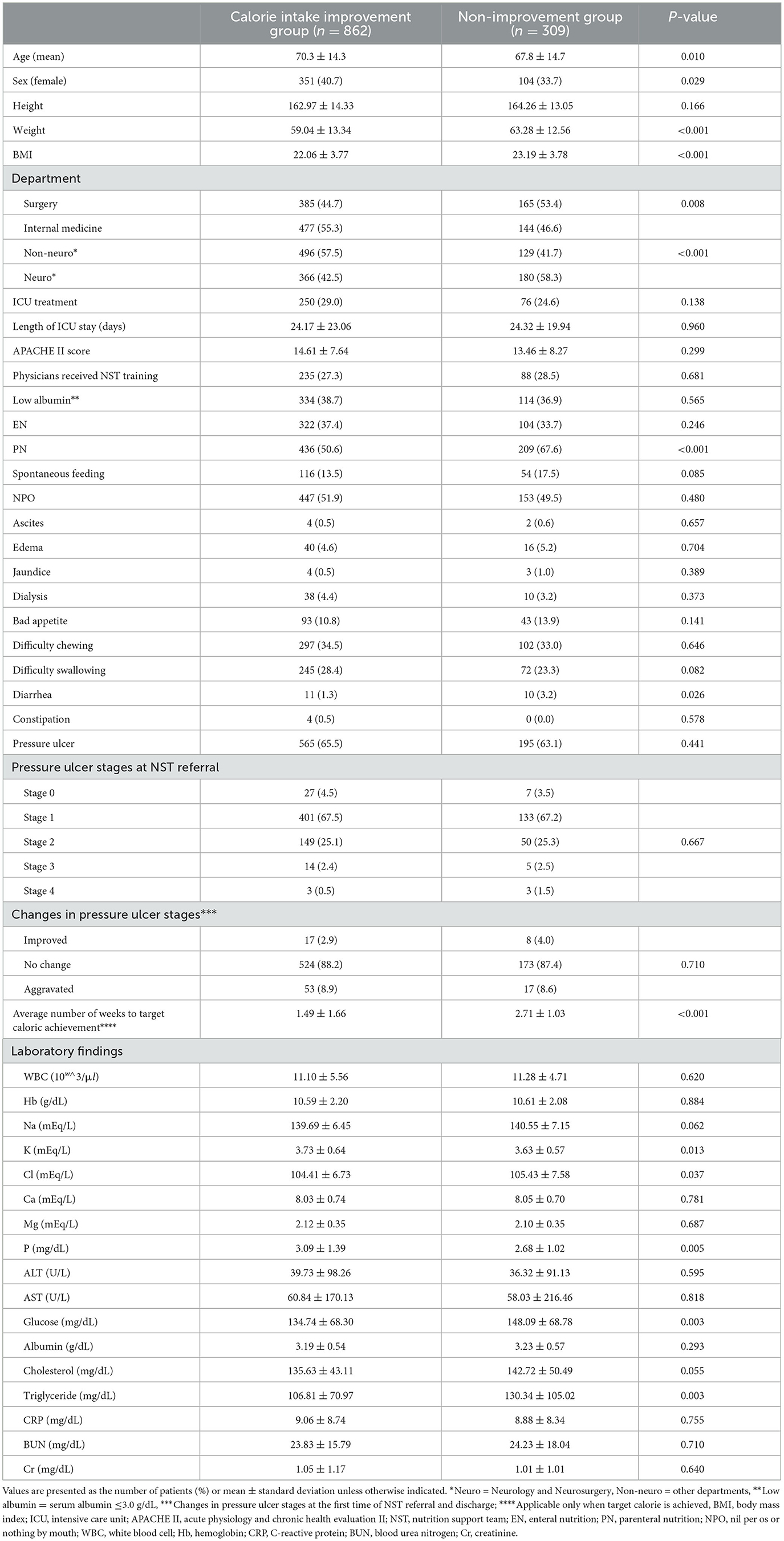
Table 2. Comparison of clinical characteristics between calorie intake improvement group and non-improvement group.
Analyzing the factors affecting target caloric achievement (Table 3), we found that old age positively influenced achieving the target calorie intake [adjusted odds ratio (aOR) = 1.029, 95% confidence interval (CI) = 1.009–1.050] and non-neuro department patients were more likely to achieve the target calorie intake than neuro department patients (aOR = 0.305, 95% CI = 0.150–0.617). Furthermore, a longer ICU stay positively influenced achieving the target calorie intake (aOR = 1.025, 95% CI = 1.007–1.043).
Analyzing the factors affecting the improvement in calorie intake 1 week after NST referral (Table 4), we found that the lower the BMI, the more improved the calorie supply (aOR = 0.939, 95% CI = 0.905–0.975), and non-neuro department admission positively influenced calorie intake improvement (aOR = 0.376, 95% CI = 0.264–0.537). In addition, receiving PN (aOR = 0.365, 95% CI = 0.269–0.495) or the presence of diarrhea (aOR = 0.263, 95% CI = 0.103–0.677) negatively affected calorie intake improvement.
The present study compared the group that achieved the target calorie intake with the group that did not and the group that improved calorie intake 1 week after the first NST referral with the group that did not and found many significant clinical differences. Furthermore, the multivariate analysis of factors influencing the achievement of the target calorie intake and the improvement in calorie intake 1 week after NST revealed that neuro department admission was a negative factor in both cases.
In the present study, the proportion of neuro department patients was significantly lower in the target caloric achievement group than in the non-achievement group, and in the calorie intake improvement group than in the non-improvement group. The multivariate analysis also revealed that neuro department admission was a negative factor in all cases. Neuro patients are known to be more prone to malnutrition due to dysphagia, decreased consciousness, decreased cognitive function, decreased muscle strength, and various neuropsychological disturbances. Among these, dysphagia is known as the major factor (3). Furthermore, neuro patients received EN more commonly than non-neuro patients because of dysphagia or decreased consciousness (4). EN is a nutrition supply method preferred to PN if the patient's digestive function is not compromised. However, it may be impossible to supply sufficient nutrition using EN alone because there are often restrictions on increasing the amount of feeding due to the risk of aspiration and gastrointestinal complications, such as vomiting, diarrhea, regurgitation, and abdominal distention (5). Achieving the target calories or improving calorie intake could be difficult for neuro patients because of their characteristics, particularly the high incidence of dysphagia and decreased consciousness, resulting in a high proportion of patients receiving EN. Notably, the proportion of patients receiving EN was significantly higher in the group that did not achieve the target calorie intake in the present study; however, EN was not a significant factor compared with the other variables affecting the target caloric achievement.
Caloric restriction or fasting may delay the progression of some neurologic diseases or even treat them (6, 7). Preventing or treating metabolic syndrome, a major risk factor for neurologic diseases, can prevent neurologic diseases and help delay the progression of neurodegenerative diseases such as Alzheimer's and Parkinson's diseases. Therefore, neurological patients may practice caloric restriction or fasting. However, neurological patients admitted to tertiary hospitals, such as the present study's participants, have more acute neurological conditions, such as stroke and encephalitis, than chronic neurological conditions (8). The role of fasting in acute infections, including acute central nervous system infections, has not been studied enough, suggesting that fasting could be harmful in viral infection cases (9). Therefore, caloric restriction or fasting should be avoided until there is sufficient evidence that either is beneficial in most neurologic conditions, and further studies on how to ensure adequate nutrition for patients with neurologic diseases should be conducted.
Critically ill patients treated in the ICU are more vulnerable to malnutrition because they are often in a heightened pro-inflammatory state, which can worsen their nutritional status (10). Malnutrition has been known to increase morbidity and mortality, and increased intakes of energy and protein can improve the clinical outcomes of ICU patients (11). Therefore, several nutritional therapies have been proposed to improve the nutrition intake of ICU patients, and studies have shown that these therapies reduce energy deficit and length of hospital stay (12). The present study's results showed that longer ICU stay positively influenced achieving the target calories of ICU patients. This may be because more effort is put into nutritional therapy for ICU patients because they are more likely to be malnourished, and more medical nutrition therapy, such as EN and PN, is frequently used in ICU settings (13). Additionally, more aggressive NST treatment was provided to ICU patients because NST referral indications included ICU treatment in this medical institution.
For patients in the surgery department, the impact of various invasive surgical procedures and diagnostic tests, along with the physiological and chemical responses to surgery, may negatively influence nutritional status (14). The result of this study also revealed a lower proportion of surgery department patients in the calorie intake improvement group. However, this factor did not emerge as statistically significant when compared to other variables influencing calorie intake improvement. Additionally, the surgery department in this study encompassed a group including cardiothoracic surgery, general surgery, orthopedics, plastic surgery, and neurosurgery. The specific types of surgery associated with calorie intake improvement were not identified, indicating a limitation of the present study. Further follow-up studies are suggested to explore this aspect. Serum albumin and plasma hemoglobin are commonly regarded as laboratory parameters reflecting nutritional status, and they are typically measured at lower concentrations in patients with malnutrition (15). In particular, studies evaluating the role of serum albumin as a biomarker reflecting the severity of malnutrition have identified lower serum albumin concentrations in patient groups at high risk of malnutrition. However, when patients with acute illnesses are included, the predictive value of these biomarkers significantly diminishes, indicating a stronger association with inflammatory markers rather than malnutrition (16). The result of this study revealed significantly lower levels of plasma hemoglobin and serum albumin in the target caloric achievement group. It is important to note that the laboratory results used in this study represent values at the time of the first NST referral and do not reflect values after NST support. In cases where both plasma hemoglobin and serum albumin levels are low at the initial NST referral, increased attention to nutritional status by the primary care physician and NST is anticipated, potentially explaining the lower values observed in the target caloric achievement group. Furthermore, these two factors did not emerge as statistically significant contributors to target caloric achievement in our study.
Recently, the effects of NST therapy were reported in a multicenter trial (17). In inpatients at nutritional risk, the use of nutritional support contributed to improvements in the patients‘ clinical outcomes (18). In this study, the proportion of primary care physicians with NST training was significantly higher in the target caloric achievement group; however, it was not a significant factor compared with other factors affecting the target caloric achievement. Furthermore, while less than half of the patients achieved the target calories (37.2%), a substantial 73.6% showed at least some improvement in calorie intake 1 week after NST referral. Given that NST referral is expected to have a positive impact on calorie intake improvement, even if only slightly, it becomes evident that a more proactive approach to NST referrals and encouraging physicians to undergo NST training is essential.
This study had some limitations. First, because this study could not include and analyze some clinical data, such as underlying diseases and admission diagnoses of the participants, caution should be exercised in interpreting the results because other potential factors could have influenced this study's results. Second, this study could also have selection bias because data were collected and analyzed retrospectively. Third, this study is a single-center study, which may have limitations as the results cannot be extrapolated. However, despite these limitations, this study is the first to explore the effectiveness of intensive nutrition therapy in relatively many patients referred to NST and the factors that contributed to the outcomes. We expect this study's results will profoundly impact the focus and direction of NST.
NST therapy significantly improved clinical outcomes for inpatients at nutritional risk. Because neuro patients experience difficulties achieving target calories and improving calorie intake, actively implementing NST referral for these patients is necessary to improve calorie supply. In addition, considering that a longer ICU stay positively influences achieving target calories, implementing and expanding the system for nutrition therapy in ICU to general-ward patients, including neurological patients, is necessary. Finally, we look forward to seeing further research exploring other effective ways, such as dysphagia screening or assessment, to improve caloric supply in neurological patients.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving humans were approved by Chosun University Hospital (2022-09-001). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
JB, HR, and HK: conceptualization. JB, S-YK, HR, and HK: methodology. HR: software. HK: validation, supervision, and funding acquisition. S-YK: investigation and visualization. JB and HR: resources. JB and HK: writing—original draft preparation. HR and HK: writing—review and editing. All authors read and agreed to the published version of the manuscript.
This study was supported by a research fund from Chosun University, 2023.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
NST, nutrition support team; EN, enteral nutrition; PN, parenteral nutrition; ICU, intensive care unit; BMI, body mass index; aOR, adjusted odds ratio; CI, confidence interval.
1. Mistiaen P, Van den Heede K. Nutrition support teams: a systematic review. JPEN J Parenter Enteral Nutr. (2020) 44:1004–20. doi: 10.1002/jpen.1811
2. Sul JY, Kim JG. The present and future of nutrition support team. Surg Metab Nutr. (2019) 10:1–4. doi: 10.18858/smn.2019.10.1.1
3. Burgos R, Bretón I, Cereda E, Desport JC, Dziewas R, Genton L, et al. ESPEN guideline clinical nutrition in neurology. Clin Nutr. (2018) 37:354–96. doi: 10.1016/j.clnu.2017.09.003
4. Bong JB, Chung JY, Kim SY Ryu HU, Shin BS, Kang HG. Characteristics and clinical course of patients referred to the NST. Front Nutr. (2023) 10:1071541. doi: 10.3389/fnut.2023.1071541
5. Wanden-Berghe C, Patino-Alonso MC, Galindo-Villardón P, Sanz-Valero J. Complications associated with enteral nutrition: CAFANE study. Nutrients. (2019) 11:2041. doi: 10.3390/nu11092041
6. de Carvalho TS. Calorie restriction or dietary restriction: how far they can protect the brain against neurodegenerative diseases? Neural Regen Res. (2022) 17:1640–4. doi: 10.4103/1673-5374.332126
7. Phillips MCL. Fasting as a therapy in neurological disease. Nutrients. (2019) 11:2501. doi: 10.3390/nu11102501
8. Rizos T, Jüttler E, Sykora M, Poli S, Ringleb PA. Common disorders in the neurological emergency room–experience at a tertiary care hospital. Eur J Neurol. (2011) 18:430–5. doi: 10.1111/j.1468-1331.2010.03170.x
9. Wang A, Huen SC, Luan HH, Yu S, Zhang C, Gallezot JD, et al. Opposing effects of fasting metabolism on tissue tolerance in bacterial and viral inflammation. Cell. (2016) 166:1512–25. doi: 10.1016/j.cell.2016.07.026
10. Lew CCH, Yandell R, Fraser RJL, Chua AP, Chong MFF, Miller M. Association between malnutrition and clinical outcomes in the intensive care unit: a systematic review. JPEN. (2017) 41:744–58. doi: 10.1177/0148607115625638
11. Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. (2009) 35:1728–37. doi: 10.1007/s00134-009-1567-4
12. Soguel L, Revelly JP, Schaller MD, Longchamp C, Berger MM. Energy deficit and length of hospital stay can be reduced by a two-step quality improvement of nutrition therapy: the intensive care unit dietitian can make the difference. Critical Care Med. (2012) 40:412–9. doi: 10.1097/CCM.0b013e31822f0ad7
13. Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Bischoff SC, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nut. (2019) 38:48–79. doi: 10.1016/j.clnu.2018.08.037
14. Kim MK, Choi YS, Suh SW, Lee SE, Park YG, Kang H. Target calorie intake achievements for patients treated in the surgical intensive care unit. Clinical Nutr Research. (2021) 10:107. doi: 10.7762/cnr.2021.10.2.107
15. Keller U. Nutritional laboratory markers in malnutrition. J Clin Med. (2019) 8:775. doi: 10.3390/jcm8060775
16. Zhang Z, Li J, Gu D, He Y, Xie X, Yang Y. Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and meta-analysis. Nutrients. (2017) 9:829. doi: 10.3390/nu9080829
17. Schuetz P, Fehr R, Baechli V, Geiser M, Deiss M, Gomes F, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet. (2019) 393:2312–21. doi: 10.1016/S0140-6736(18)32776-4
Keywords: nutritional support, malnutrition, caloric restriction, enteral nutrition, neurology
Citation: Bong JB, Kim S-Y, Ryu HU and Kang HG (2024) Factors affecting target caloric achievement and calorie intake improvement: the nutrition support team's role. Front. Nutr. 10:1249638. doi: 10.3389/fnut.2023.1249638
Received: 29 June 2023; Accepted: 11 December 2023;
Published: 05 January 2024.
Edited by:
Jasmina Dimitrova-Shumkovska, Saints Cyril and Methodius University of Skopje, North MacedoniaReviewed by:
Lakshmi Ranganathan, Senior Researcher, Chennai, IndiaCopyright © 2024 Bong, Kim, Ryu and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han Uk Ryu, aW9yeTI1MkBuYXZlci5jb20=; Hyun Goo Kang, aGdrYW5nQGpibnUuYWMua3I=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.