- 1Department of Anesthesiology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, Henan, China
- 2Henan Medical School of Zhengzhou University, Zhengzhou, Henan, China
- 3General ICU, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Objective: Previous cohort trials have shown that skipping breakfast increases the risk of obesity or overweight in children. However, this finding remains controversial. Through a meta-analysis, this study systematically evaluated the effect of skipping breakfast on the prevalence of obesity or overweight in children.
Methods: We performed a literature search for studies published until March 19, 2023. using the Cochrane, PubMed, and Embase databases. Based on the inclusion and exclusion criteria, observational studies on the relationship between skipping breakfast and overweight/obesity in children and adolescents were analyzed. Three investigators independently screened the relevant literature, extracted the data, and assessed the risk of bias. The quality of the included studies was assessed using the Newcastle-Ottawa Scale (NOS). A random-effects model was used. The odds ratio (OR) with its 95% confidence interval (CI) was used to indicate the effect size.
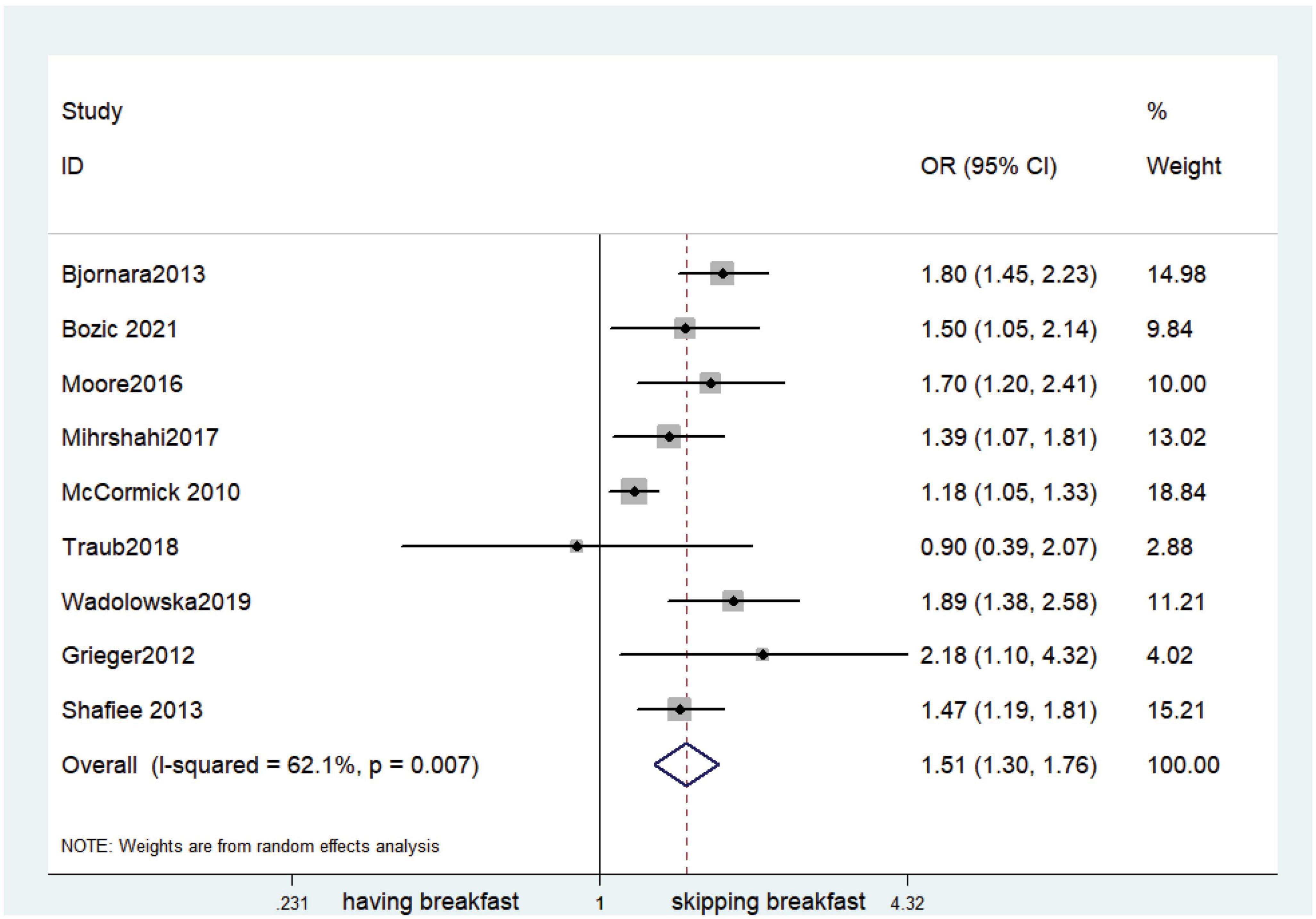
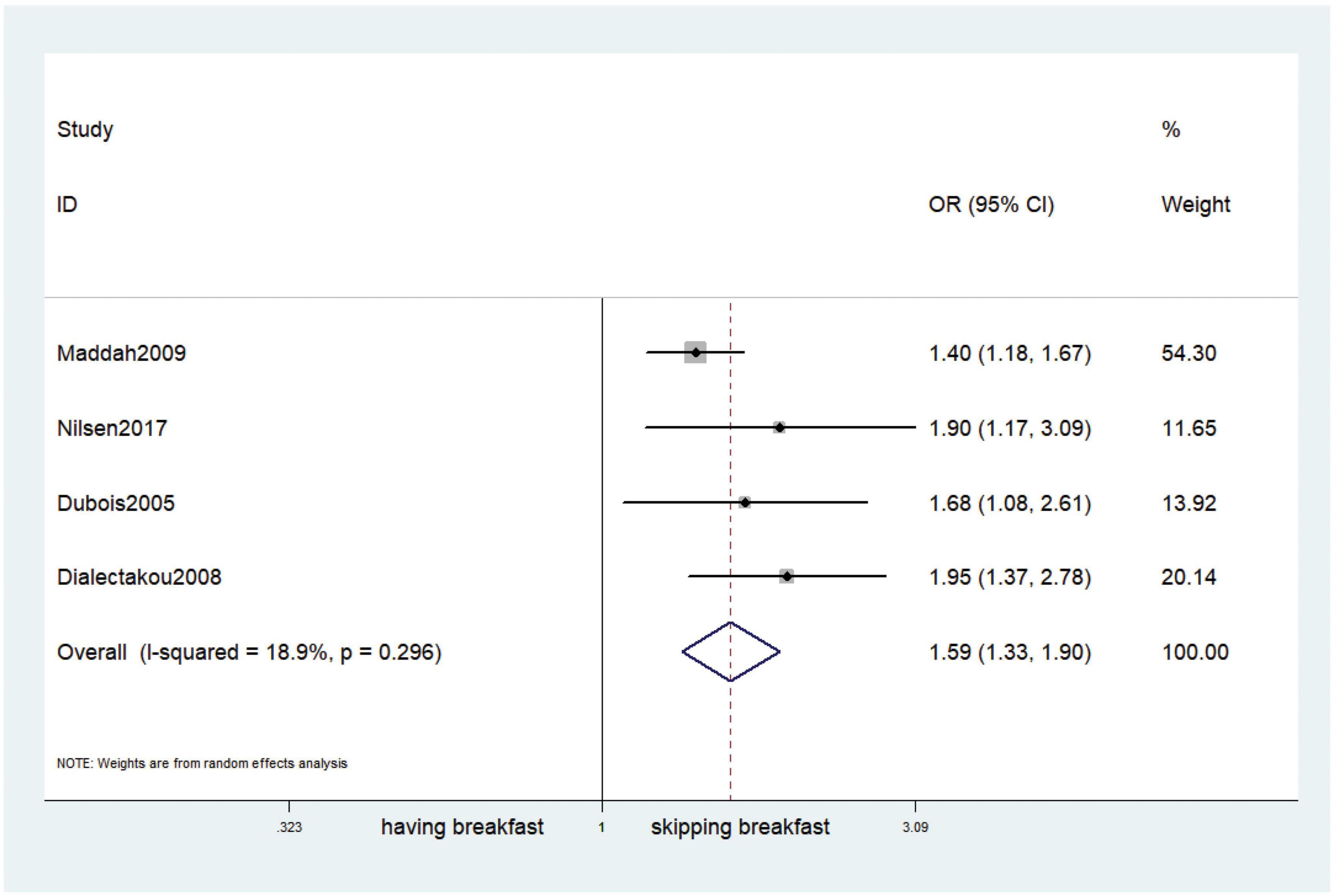
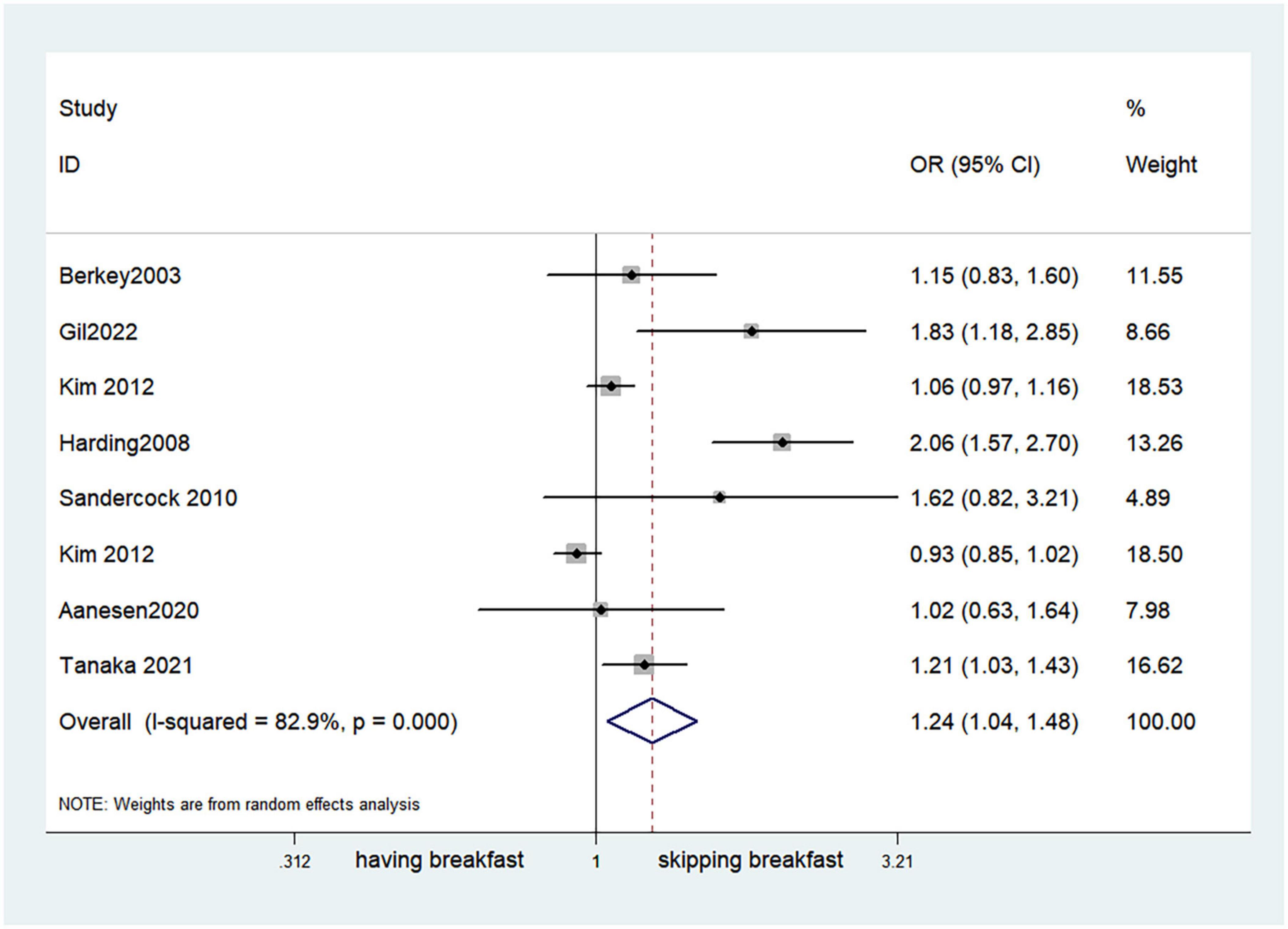
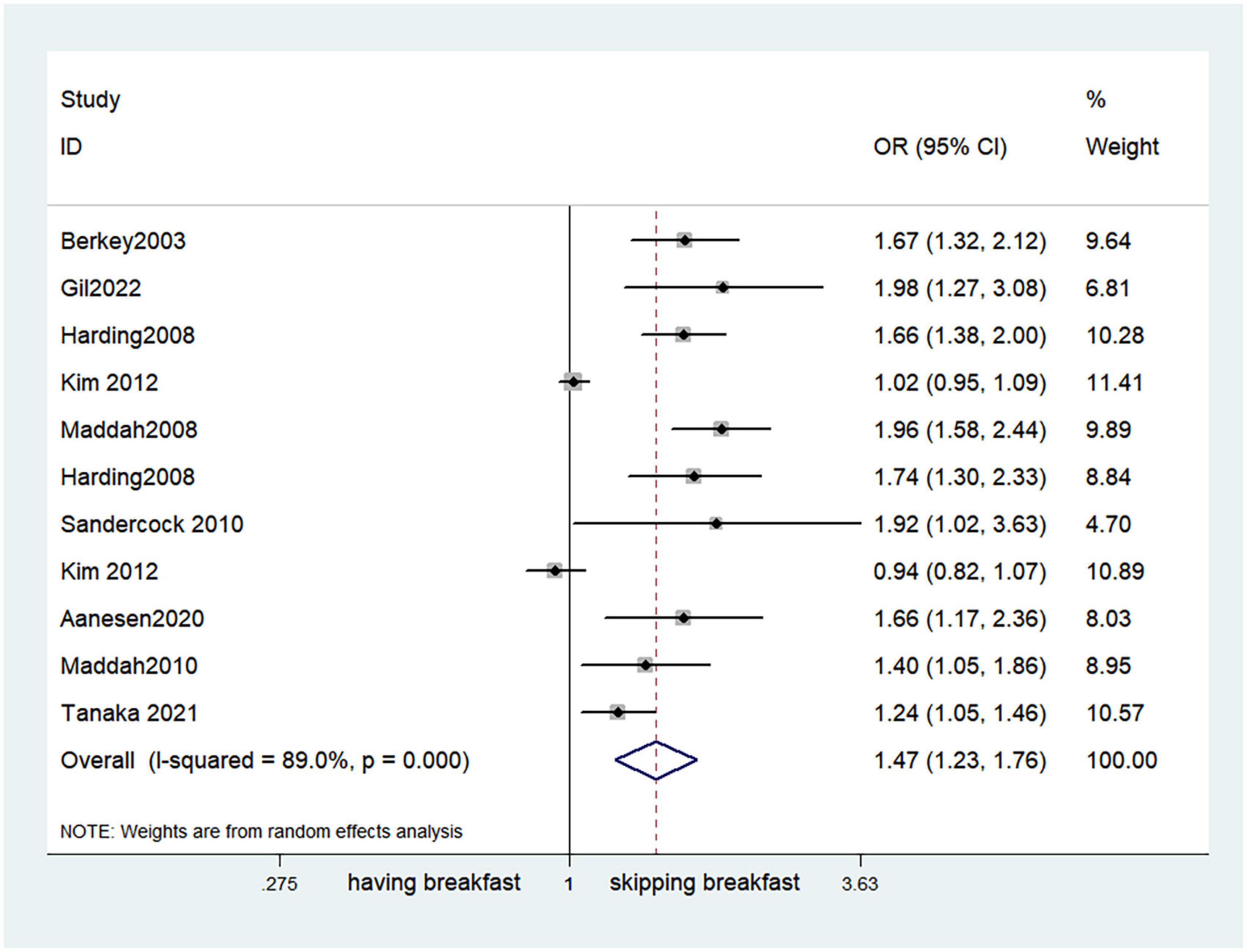
Results: A total of 40 retrospective studies with 323,244 children ranging in age from 2 to 20 years were included in this study. The results of this meta-analysis showed that children and adolescents who skipped breakfast had a significantly higher prevalence of obesity or overweight than those who ate breakfast (OR, 1.59; 95% CI, 1.33–1.90; P < 0.001). Skipping breakfast was positively associated with overweight in children and adolescents (OR, 1.37; 95% CI, 1.23–1.54; P < 0.001). Similarly, skipping breakfast was positively associated with obesity in children and adolescents (OR, 1.51; 95% CI, 1.30–1.76; P < 0.001). The effect was also different by sex, with girls being the most affected (OR, 1.47; 95% CI, 1.23–1.76; P < 0.001). There was also a correlation between skipping breakfast and abdominal obesity in children (OR, 0.65; 95% CI, 0.55–0.77; P < 0.001).
Conclusion: This meta-analysis suggested that skipping breakfast is associated with an increased risk of overweight/obesity in children and adolescents. The findings provide support for a possible protective role of breakfast against excessive weight gain in children and adolescents. However, more rigorous study designs with validated and standardized measures of relevant variables are needed.
Introduction
The prevalence of obesity or overweight in children and adolescents has been increasing significantly since the 1980s. According to reports by the World Health Organization (WHO) (Global Strategy on Diet), the world obesity rate among people under 18 years of age increased from 11 million to 124 million over three decades. Although studies have confirmed that the prevalence of childhood obesity is now stabilizing and may be declining slightly in specific subgroups, it is still at extremely high levels. Children with obesity are likely to remain obese for the rest of their lives and experience a variety of other complications. The continued high prevalence of childhood obesity will place a significant burden on society. There is evidence that obese children and adolescents are at greater risk of obesity and other chronic diseases such as diabetes, cardiovascular disease, and dyslipidemia during adulthood (1–3). Therefore, the primary prevention of childhood obesity is of utmost importance. One main factor that can be ascribed to childhood obesity and overweight is skipping breakfast.
The underlying potential mechanism for this situation is still unknown. A previous study reported that skipping breakfast may be connected to lower satiety during the day and an increase in the consumption of high-fat snacks, which can be summarized as appetite control, energy intake and diet quality (4). These variations can lead to subsequent overeating and impaired insulin sensitivity. The causes of obesity are diverse. They are interconnected and affect each other in complex ways, and we cannot solve the problem of obesity with a single-sided solution. Prevention in multiple aspects of the socioecological framework is needed (5–7). The daily frequency of eating, eating occasions and times, and eating patterns can influence the digestion and absorption of calories and energy balance (8–10). Moreover, a study across 12 countries also showed that the human developmental environment, socioeconomic factors, cultural practices and the accessibility of school breakfast programs affect the frequency of eating breakfast among children (11). Regarding the latent factors of skipping breakfast in children, previous research has disclosed that there is a correlation between parents’ breakfast habits and those of their children. Children tend to skip breakfast if their parents skipped breakfast when they were 1.5 years old (12). Additionally, parental knowledge and awareness levels are also associated with children’s dietary models (13). Children have their own problems that can be exacerbated when they mimic their parents’ bad behaviors (14, 15). By precisely examining these issues, we can see that there are some differences among subgroups, such as groups classified by sex and age. Previous studies have shown that the most vulnerable group is children aged from 2 to 5 years old (16, 17). Girls are more vulnerable, because they are more likely to be exposed to an in utero environment with high sugar and undernutrition, which lead to disrupted glucose homeostasis, resulting in an increased risk of obesity and overweight (18–21). Furthermore, the cultural perspective of thinness and beauty in modern society has resulted in differences in dietary intake (22, 23).
Obviously, eating breakfast has many advantages such as improved performance in school, improved cognition (24, 25), and reductions in tardiness, absenteeism and psychosocial problems (26). Daily breakfast consumption among children and adolescents is considered an important preventive measure against obesity or overweight (27). The USDA Center for Nutrition Policy and Promotion (CNPP) conducted a systematic review (15 studies published from 2000 to 2010) on the relationship between breakfast consumption and obesity in children (28) to inform the 2010 Dietary Guidelines for Americans (DGA). The DGA committee reported that the pediatric population that skipped breakfast had an increased and moderate risk of obesity, with a stronger association found in adolescents.
The goal of this study was to provide explanations by reviewing previous studies of obesity or overweight in children and adolescent in relation to skipping breakfasts. Our research scope covered almost all related articles published in the past 25 years. Because of the large amount of extracted data, our data are more convincing and reliable. At the same time, our study involved a broader exploration of possible influencing factors, and in-depth discussions to elucidate the mechanisms that may be related to the experimental results, especially the reasons for the differences between boys and girls, as well as the mechanisms for obesity caused by skipping breakfast. We carefully compared the impact of skipping breakfast on obesity between boys and girls and on abdominal obesity in children and adolescents, which was rarely mentioned in previous meta-analyses. By understanding these differences and the underlying mechanisms, we can target relevant dietary strategies, according to different populations, physical activity levels, and types of obesity diseases, which is of great importance in improving childhood obesity.
Methods
Inclusion and exclusion criteria
Inclusion criteria
The inclusion criteria were as follows:(1) observational studies; (2) studies including children and adolescents aged 2–20 years; (3) studies including a comparison between skipping and eating breakfast in children and adolescents; (4) studies including patient outcomes of obesity, overweight, or abdominal obesity; (5) studies for which valid information could be extracted from the article, including the study duration, number of study participants, age of study participants, and outcome indicators related to the participants; (6) full text articles that could be searched and downloaded from PubMed, Embase, and the Cochrane Library; (7) studies in which the target population was children and adolescents; and (8) studies reporting either the relative risk (RR) or odds ratio (OR) and 95% confidence interval (CI).
Exclusion criteria
The exclusion of studies was performed by three researchers as follows: (1) secondary studies such as reviews and meta-analyses; (2) articles for which valid data could not be extracted or the full text could not be downloaded from the database; (3) studies that did not clearly specify the exposure factor as “skipping breakfast led to obesity”; (4) studies with non-peer-reviewed material; (5) studies including participants diagnosed with diseases relevant to the purpose of the study or hospitalized patients; and (6) studies in which overweight or obesity was considered an exposure and skipping breakfast was considered an outcome.
Information sources
We conducted a comprehensive search in the PubMed, Embase, and Cochrane English databases for literature published before March 19, 2023. We searched for relevant studies using MeSH, Emtree, title abstracts, and keywords for the search terms “breakfast” “children,” “adolescent,” “obese” and “obesity” (shown in Supplementary Table 1).
Literature screening
We manually screened the articles to identify those with a significant correlation between skipping breakfast and obesity or overweight in children and adolescents. First, we judged the research direction of the articles by evaluating the abstract and title. Articles that could not be judged through the abstract and title were downloaded and the full text was read. After the initial screening, three researchers jointly judged the articles that could be included and extracted the data. When there was controversy regarding whether an article should be included, one or more authoritative researchers were asked to decide.
Data extraction
Data on the number of children with obesity, the number of children who ate breakfast and the number of children who did not eat breakfast, ORs with their 95% confidence intervals for the effect of not eating breakfast on the prevalence of obesity or overweight, as well as relevant continuous variable indicators were extracted from the included literature. A screening flow diagram was created based on the search results (Figure 1). Information such as the name of the author, the year of publication, the type of study, the sample size, age, and the main findings of the included studies are shown in Table 1. Article quality was evaluated according to the Newcastle-Ottawa Scale (NOS), as shown in Table 2.
Statistical analysis
All statistical analyses were conducted using STATA12.0. Our statistics were pooled with the random-effects model. This model was deemed more appropriate than the fixed-effects model because the studies included in this meta-analysis represented samples from different populations. Studies that reported rate ratios were converted to ORs using the methods defined in the Cochrane Handbook for Systematic Reviews of Interventions. Summary statistics are expressed as ORs and 95% CIs. Statistical heterogeneity was assessed using the I2 statistic. Publication bias was assessed qualitatively by visual inspection of the inverted funnel. Egger’s test was performed to assess small study effects. Statistical tests were two-tailed, and the statistical significance threshold was P < 0.05. For cross-sectional studies, sensitivity analyses based on funnel plots and Egger tests were used to show the robustness of the results and to confirm the presence of publication bias. To check the robustness of the results, a sensitivity analysis was performed. A funnel plot can visually represent a graph as an inverted funnel with good symmetry, which indicates less bias. To test the relationship between skipping breakfast and the risk of obesity, the pooled RR and 95% CI for skipping breakfast versus not skipping breakfast were calculated using a random effects model. Furthermore, we used the I2 test to assess the heterogeneity of the included studies; an I2 value greater than 50% was considered to indicate substantial heterogeneity. To determine the source of the heterogeneity among the included studies, subgroup analyses were performed if there were at least 2 studies in each category. Egger regression asymmetry tests were used. Egger regression and funnel plots used to evaluate publication bias.
Results
Literature search results
Three researchers used the PubMed, Embase, and Cochrane Library electronic databases to search for literature based on the search terms “child,” “children,” “adolescent,” “breakfast,” “obese,” and “obesity.” There were 3491 articles, including 1082 articles retrieved from PubMed, 2,144 articles retrieved from Embase, and 257 articles retrieved from the Cochrane Library. After the manual screening of titles and abstracts, 129 articles were initially included. Of these, 83 articles did not have extractable or calculable data. One article had an experimental population other than children and adolescents, and 6 papers were secondary studies such as reviews and meta-analyses. After excluding all studies that did not meet the inclusion criteria, 40 studies were ultimately retained and included in this study. The flow chart of the literature screening process is shown in Figure 1.
Basic characteristics of the included literature
A total of 40 studies including 8 longitudinal studies and 32 cross-sectional studies, were included in this meta-analysis (12, 16, 29–66). The total number of patients included in the 40 studies was 323,244. The researchers extracted data related to author information, the year of publication, the study type, the sample size, age, and main findings from the 40 studies to determine the basic characteristics of the articles (Table 1).
Quality evaluation of included literature
In this meta-analysis, 3 reviewers independently assessed the quality of the 40 articles by using the Newcastle-Ottawa Scale (NOS). The objective assessments for the following dimensions yielded a maximum score of 9; study population selection (no more than 4 points), comparability of cohort design and analysis (no more than 2 points), and adequacy of outcome measures (no more than 3 points). Score of 7–9 were considered to indicate high quality (low risk of bias). One article had a score of 5, and the remaining articles had scores ≥ 6. Eight of the included articles had a quality assessment score of 8. Twenty articles had a score of 7, and 11 articles had a score of 6, indicating a low risk of bias based on the NOS. The articles were of high quality, were designed in a reasonable manner, had reliable data, and could be included in the meta-analysis. The results of the quality assessment are shown in Table 2.
Outcomes
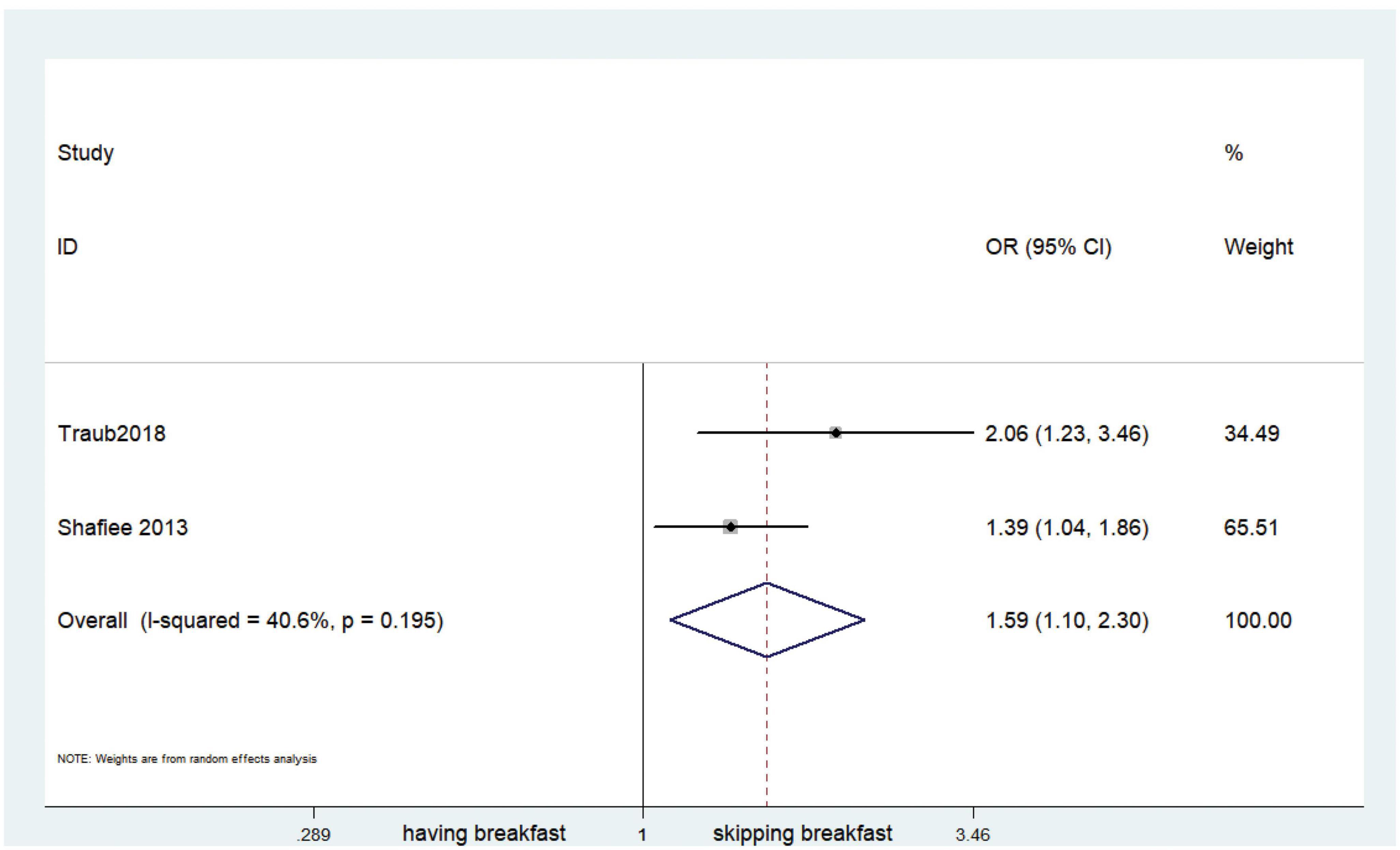
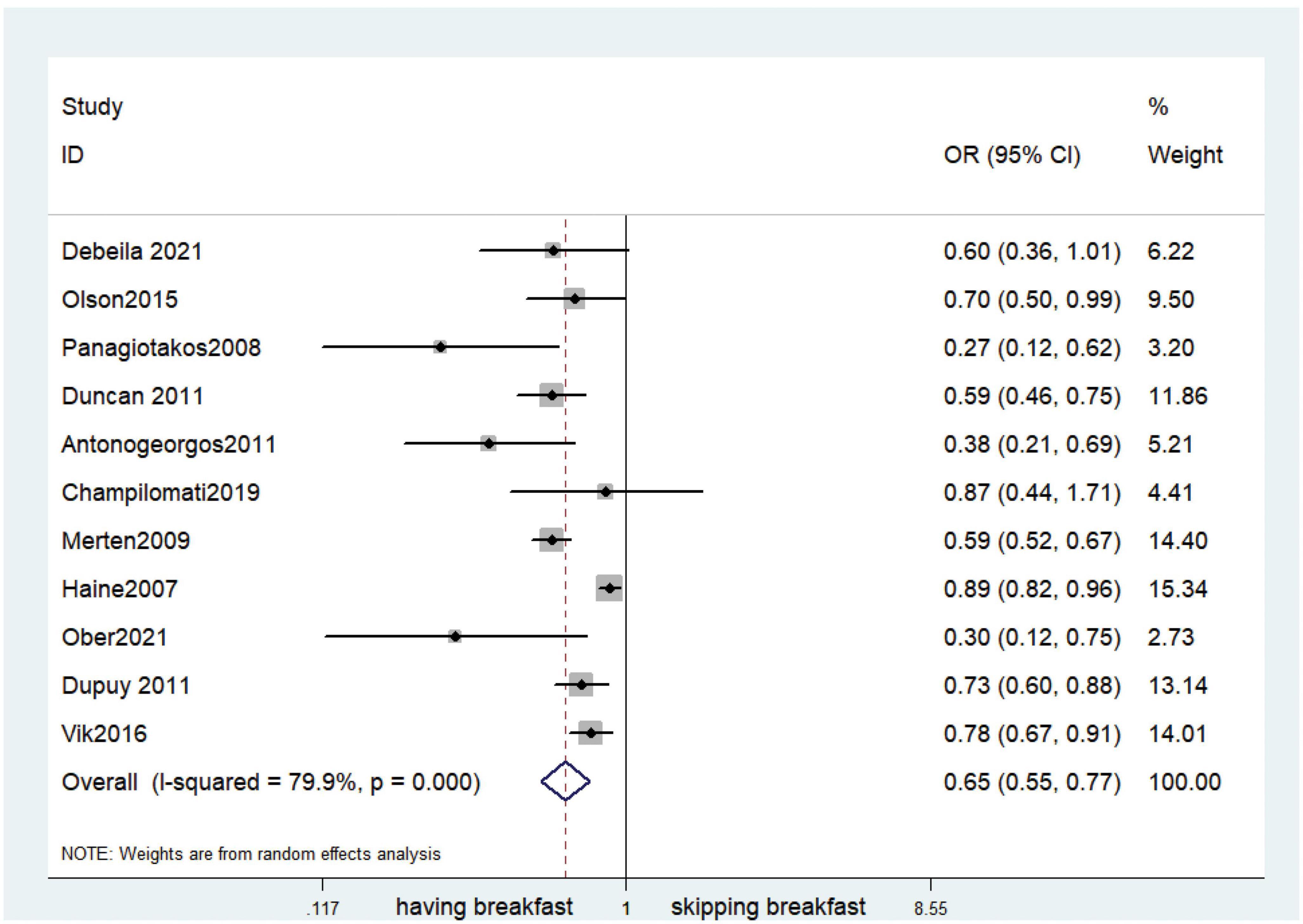
Fifteen observational studies (12, 32, 34, 35, 38, 39, 41, 44, 45, 47, 49, 52, 53, 57, 64) showed that skipping breakfast was positively associated with overweight in children and adolescents (OR, 1.37; 95% CI, 1.23–1.54; P < 0.001; Figure 2). Nine studies (32, 38, 39, 47, 49, 57, 63, 64, 66) illustrated that skipping breakfast was positively associated with obesity in children and adolescents (OR, 1.51; 95% CI, 1.30–1.76; P < 0.001; Figure 3). Four articles (43, 45, 54, 58) provided data on the effect of skipping breakfast on overweight or obesity in children and adolescents (OR, 1.59; 95% CI, 1.33–1.90; P < 0.001; Figure 4). In the cross-sectional study, the subgroup analysis of sex showed 19 effect values extracted from 10 observational studies (16, 30, 31, 33, 37, 48, 50, 54, 62), and the results showed that skipping breakfast had different effects on obesity in boys and girls. Subgroup analysis of the cross-sectional studies showed an association between skipping breakfast and the risk of obesity in boys (OR, 1.24; 95% CI, 1.04–1.48; P = 0.014; Figure 5) and girls (OR, 1.47; 95% CI, 1.23–1.76; P < 0.001; Figure 6). The analysis by sex was performed because girls are more likely to skip breakfast than boys, as well as to determine the differential impact of breakfast on boys and girls. There is literature indicating that skipping breakfast has a statistically significant effect on obesity in girls, while the correlation between skipping breakfast and obesity in boys is not statistically significant (33). One study indicated that skipping breakfast was not associated with childhood obesity (40). We analyzed abdominal obesity in children, and 3 articles (63, 64, 67) reported the effect on abdominal obesity; 2 (63, 64) mentioned the effect of skipping breakfast on abdominal obesity, and 1 (67) mentioned that eating breakfast reduced the risk of abdominal obesity. Forest plotting was performed using the data from the two articles on the effect of skipping breakfast on abdominal obesity and showed a positive association between skipping breakfast and abdominal obesity (OR, 1.59; 95% CI, 1.10–2.30; P = 0.013; Figure 7). Because only two articles were included, the heterogeneity was high (P = 0.195). In addition, the age, sex, living environment, family atmosphere and other factors of the respondents will had an impact on the survey, creating heterogeneity among the study results. There were also 11 articles (29, 36, 40, 42, 46, 51, 56, 59–61, 65) that described the effect of eating breakfast on overweight or obesity risk in children and adolescents (OR, 0.65; 95% CI, 0.55-.77; P < 0.001; Figure 8).
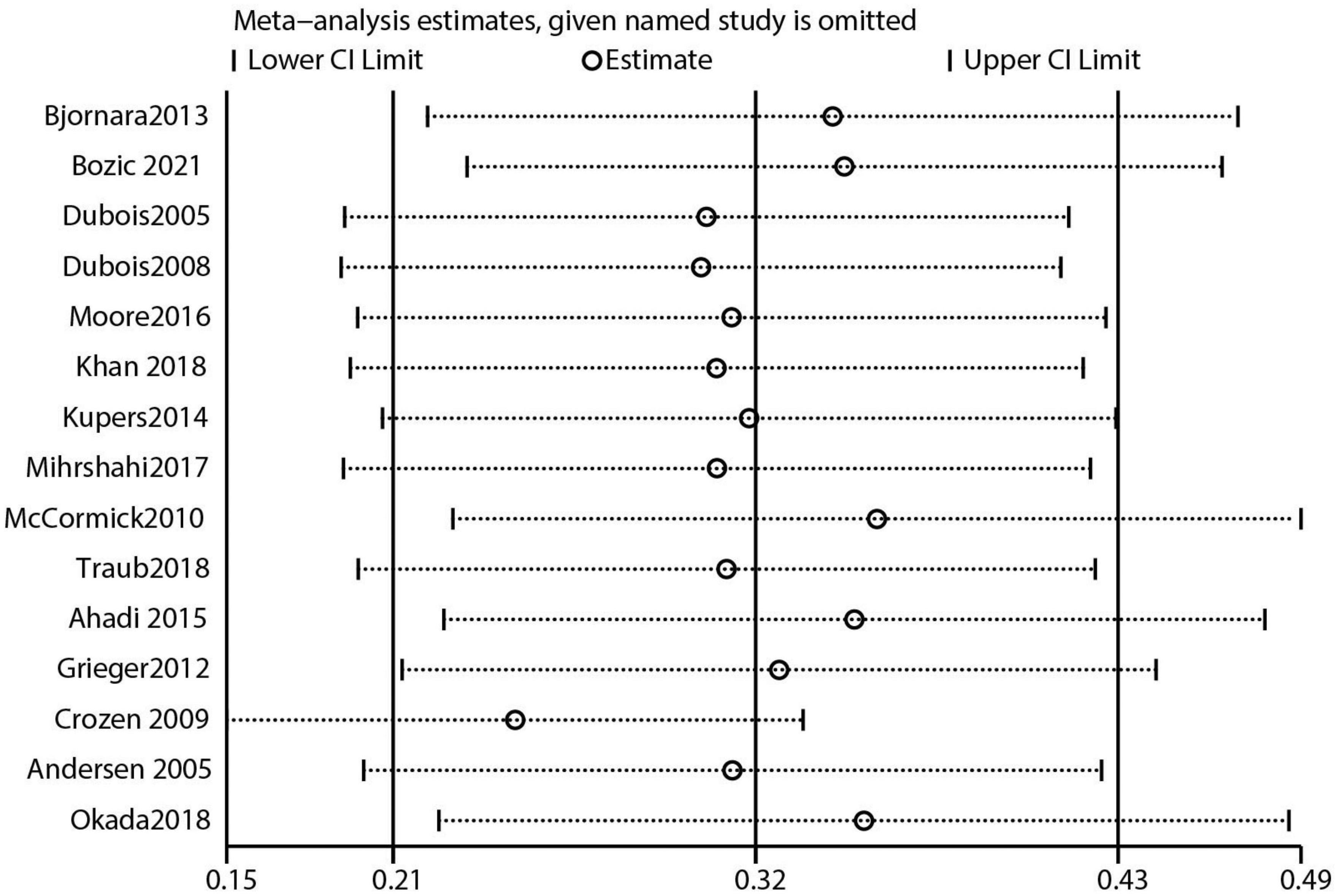
Sensitivity analysis and publication bias
The 40 included studies were mainly those with high quality assessment scores (NOS scores). After performing leave-one-out sensitivity analysis, combined effect sizes, and all effect sizes were included in the total 95% CI effect size, indicating good stability of the results. The data results are shown in Figure 9 and Supplementary Figures 1–4. The funnel plot visually represents the graph as an inverted funnel with good symmetry, indicating less bias. The results of data analysis are shown in Supplementary Figures 5–9. According to the results of the Egger test, studies that reported the effect of skipping breakfast on overweight risk in children had some publication bias (Supplementary Figure 10; P = 0.004). However, studies that reported the effect of skipping breakfast on obesity risk had no major bias (Supplementary Figure 11; P = 0.060). Studies that reported the effect of eating breakfast on obesity or overweigh risk had some bias (Supplementary Figure 12; P = 0.023). Additionally, there was some publication bias among studies that reported the effect of skipping breakfast on childhood obesity or overweight risk in boys (Supplementary Figure 13; P = 0.062), but no major publication bias was observed in studies that reported the same in girls (Supplementary Figure 14; P = 0.003).
Discussion
In this study, we summarized 40 high-quality articles on the effect of skipping breakfast on OW/OB risk in children and adolescents. In the screening process, we excluded secondary research articles such as review articles and meta-analyses, extracted data from 40 articles, and used STATA 12.0 software to perform various analyses and to draw different graphs. In this study, we addressed whether skipping breakfast causes OW/OB in children and adolescents, and whether skipping breakfast causes different results in different sexes (male and female children and adolescents). The results were that skipping breakfast increased the prevalence of OW/OB (OR, 1.59; 95% CI, 1.33–1.90; P < 0.001; Figure 4) in children and adolescents. Most articles in this meta-analysis were cross-sectional studies. However, cross-sectional studies cannot make judgment about causality. Eight other cohort studies on such issues were included in our study, and the results were consistent with our hypothesis. These results are consistent with those of previous cross-sectional studies and several small prospective cohort studies conducted outside Europe (45, 68). There is a significant association between skipping breakfast and OW/OB in children and adolescents (69, 70). The relationship between skipping breakfast and obesity or overweight risk in children and adolescents is complicated by a number of factors. Confounding factors are a major threat in observational studies, and in the course of studying the effects of skipping breakfast on OW/OB risk in children and adolescents, possible influencing factors may include socioeconomic status, region, smoking, watching TV, etc. In previous studies (30, 35, 51, 59), these factors were apparently related to obesity. For socioeconomic status, the reason may be that children in areas with poor economic conditions are more likely to skip breakfast, thus leading to obesity (59). For smoking, people who smoke generally have poor lifestyle habits and are more likely to skip breakfast, which leads to obesity. Children who like to watch TV and use computers for long periods of time are often sedentary, lack of activity and exercise, and are more likely to develop obesity (35).
Environments may differ from each other. Human development levels, social factors, schools providing breakfast, and cultural differences may lead to different prevalence rates. In a study of children aged 9–16 years in twelve countries around the world, significant differences were found in Australia, Finland, and Kenya. Horikawa et al. found that skipping breakfast led to a 75% increased risk of OW/OB in children and adolescents in the Asia-Pacific region and the prevalence may be higher in rural children than in urban children (27).
In our screening, there appeared to be a stronger association between eating or not eating breakfast and the risk of obesity and overweight in girls (OR, 1.47; 95% CI, 1.23–1.76; P < 0.001; Figure 6) (30, 31, 48, 50, 55). Women are more likely to be exposed to high-glucose environments, and the presence of a uterus may be associated with the disruption of homeostasis by glucose and increased adiposity (33). In a previous study (71), we identified four different neuronal populations with respect to glucose sensitivity: the non-glucose sensing (NGS), glucose-exciting (GE), non-adapting glucose-inhibited (GI) and adapting glucose-inhibited (AdGI) populations. When extracellular glucose decreased, the activity of GE, non-adaptive GI, and AdGI neurons changed. More importantly that the relative percentage of glucose-sensitive subtypes (AdGI, non-adaptive GI, GE, and NGS neurons) within the VL-VMN was sexually dimorphic. In women, AdGI neurons and non-adapting GI neurons occur at approximately the same proportion, while in men, AdGI neurons occur approximately half as often as non-adapting GI neurons. When glucose decreased, the degree of depolarization of male and female non-adapting GI neurons was similar, but males had 2-fold increased IR due to decreased glucose compared to female, indicating increased excitability of these neurons under low-glucose conditions, which makes females more likely to develop obesity than males (71). Moreover, depending on cultural perception, girls may choose to eat less, which also includes skipping breakfast, mainly to maintain a thin body as a beauty standard (55). Middle school girls who skip breakfast are more likely to report lower levels of physical activity than those who eat breakfast regularly, which may be a contributing factor. In addition, girls with overweight and obesity may avoid exercise because they are more self-aware of their bodies (72). The development of breakfast habits in children is closely related to the habits of parents. In a Japanese study that included 42,663 children, 12–32% of their parents skipped breakfast by the time the children were one and a half years old, and this habit was mimicked by their children (27).
Children who eat breakfast differ significantly from those who do not eat breakfast in terms of diet composition. Children who do not eat breakfast have elevated daily energy fat intake, along with a reduced intake of protein, vitamins and minerals, and a stronger appetite for fat, such as fat-rich snacks, which leads to higher total plasma cholesterol levels. Additionally, the intake of breakfast cereals seems to play an important role. A study on adults found that those who ate cooked breakfast cereals had a significantly lower BMI than those who ate meat, eggs, dairy products, etc., for breakfast (73). Other studies found that there is a high prevalence of overweight among people who did not eat breakfast cereals compared to those who did (74, 75).
The mechanism of breakfast regulation in the development of obesity is very complex, and thus far, there is no clear mechanism to elucidate the relationship between them. In reviewing previous studies, we found that the possible mechanisms are mainly as follows:
Eating breakfast regularly may result in greater metabolic function, and a fiber rich breakfast may improve postprandial glycemic response, satiety, and insulin sensitivity (18). Second, skipping breakfast increases total energy intake. In a weight loss intervention trial with adolescents aged 11–16 years, it was found that an increase in energy consumption during breakfast led to a decrease in total energy intake, with an increase in the total energy intake of 171 kcal/day (76). Additionally, children who eat breakfast regularly have enhanced activity, which is considered one of the reasons for the causal relationship between skipping breakfast and OW/OB risk in children and adolescents. A recent study conducted by Professor Daniela Jakubowicz elaborated on the metabolic mechanism. His team clarified that skipping breakfast has an important connection with the clock gene that could regulate the glucose level, called the insulin response, a reaction that could lower iGLP-1 and damage the insulin response. Skipping breakfast was associated with a significantly higher post lunch and post dinner glycemic response than eating breakfast. Skipping breakfast can also lead to impaired insulin secretion after lunch and dinner, manifested by delayed insulin peaks and decreased plasma insulin and C-peptide concentrations. In addition, after lunch and dinner, the iGLP-1 response to skipping breakfast was lower than the iGLP-1 response to eating breakfast. In contrast, plasma free fatty acid and glucagon levels were significantly elevated after lunch and dinner in response to skipping breakfast. Therefore, breakfast is essential for glucose homeostasis throughout the day, including islet and incretin hormone function (77). Skipping breakfast also leads to a reduction in the expressions of gene, such as Per1, Cry1, Ror, Sirt1, and Clock, which regulate the secretion of circadian hormones and postprandial glycaemia (78). A relevant clinical trial also showed an association between overactivity in the hypothalamic-pituitary-adrenal (HPA) axis, leading to disordered cortisol rhythms (79).
The possible mechanism of abdominal obesity remains uncertain. A previous study (63) reported that people who rarely ate breakfast had lower total energy intake, but a higher body mass index than those who ate breakfast. People who typically eat breakfast consume more energy, carbohydrates, and fiber, and fat accounts for a lower percentage of the total calories; Additionally, people who eat breakfast every day appear to be more active than those who do not. This diet has the potential to improve energy balance and possibly improve glucose and insulin parameters, leading to increased satiety and a lower prevalence of abdominal obesity.
The 40 articles included retrospective cohort studies and retrospective observational studies, which had a positive effect in demonstrating that skipping breakfast can increase the prevalence of OW/OB in children and adolescents, and can provide a theoretical basis for the development healthy eating strategies and policies. We screened a large number of studies containing keywords such as children, breakfast, and obesity. We gradually censored and filtered them to ultimately obtain 40 articles that fit the study topic, and the results obtained were more objective and precise. The sample size of each of the 40 articles was very large, and the obtained results were also highly credible. Finally, the sensitivity analysis indicated that the stability of the data results was good.
The limitations are that most of the included studies were cross-sectional studies that had limitations such as lack of causality and generalization. Second, some studies were not found, and we mostly chose to exclude papers published in local languages. We only included published reports and did not search for unpublished articles. Furthermore, some studies were very old, and there may be a slight gap between previous research results and current developments. Another potential limitation arises from the various definitions of skipping breakfast. The criteria for skipping breakfast in the trials included in this review varied from study to study and sometimes did not allow for direct comparisons.
Conclusion
The findings provide support for a possible positive role of breakfast in preventing excessive obesity in children and adolescents. However, drawing causal conclusions from the collective evidence is limited by methodological constraints and inconsistencies, including the study design, follow-up duration and frequency, exposure and outcome assessment, and limited consideration of confounding, mediating, and modifying variables. More rigorous study designs with validated and standardized measures of relevant variables are needed. Second, the mechanisms regarding the modulation of obesity by eating breakfast remain unclear and need to be further explored.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
KW, YN, ZL, and BD designed the ideas for this study. YN, ZL, BD, CE, and LG performed all the procedures and data analysis. KW wrote the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1222536/full#supplementary-material
References
1. Reilly J, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. (2011) 35:891–8.
2. Baker JO, Sørensen T. Childhood body-mass index and the risk of coronary heart disease in adulthood. N Engl J Med. (2007) 357:2329–37.
3. Craig L, Love J, Ratcliffe B, McNeill G. Overweight and cardiovascular risk factors in 4- to 18-year-olds. Obes Facts. (2008) 1:237–42.
4. Betts J, Richardson J, Chowdhury E, Holman G, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. (2014) 100:539–47. doi: 10.3945/ajcn.114.083402
5. Micklesfield L, Lambert E, Hume D, Chantler S, Pienaar P, Dickie K, et al. Socio-cultural, environmental and behavioural determinants of obesity in black South African women. Cardiovasc J Afr. (2013) 24:369–75. doi: 10.5830/CVJA-2013-069
6. Swinburn B, Sacks G, Hall K, McPherson K, Finegood D, Moodie M, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. (2011) 378:804–14. doi: 10.1016/S0140-6736(11)60813-1
7. Kopelman PJ, Butland B. Executive summary: foresight ‘tackling obesities: future choices’ project. Obes Rev. (2007) Suppl. 1:vi–ix. doi: 10.1111/j.1467-789X.2007.00344.x
8. Rampersaud G, Pereira M, Girard B, Adams J, Metzl J. Breakfast habits, nutritional status, body weight, and academic performance in children and adolescents. J Am Diet Assoc. (2005) 105:743–60. doi: 10.1016/j.jada.2005.02.007
9. Ma Y, Bertone E, Stanek E, Reed G, Hebert J, Cohen N, et al. Association between eating patterns and obesity in a free-living US adult population. Am J Epidemiol. (2003) 158:85–92. doi: 10.1093/aje/kwg117
10. Garaulet M, Gomez-Abellan P. Timing of food intake and obesity: a novel association. Physiol Behav. (2014) 134:44–50.
11. Zakrzewski J, Gillison F, Cumming S, Church T, Katzmarzyk P, Broyles S, et al. Associations between breakfast frequency and adiposity indicators in children from 12 countries. Int J Obes Suppl. (2015) 5(Suppl. 2):S80–8. doi: 10.1038/ijosup.2015.24
12. Okada C, Tabuchi T, Iso H. Association between skipping breakfast in parents and children and childhood overweight/obesity among children: a nationwide 10.5-year prospective study in Japan. Int J Obes. (2018) 42:1724–32. doi: 10.1038/s41366-018-0066-5
13. O’Dea J, Wagstaff S. Increased breakfast frequency and nutritional quality among schoolchildren after a national breakfast promotion campaign in Australia between 2000 and 2006. Health Educ Res. (2011) 26:1086–96. doi: 10.1093/her/cyr042
14. Vereecken C, Dupuy M, Rasmussen M, Kelly C, Nansel T, Al Sabbah H, et al. Breakfast consumption and its socio-demographic and lifestyle correlates in schoolchildren in 41 countries participating in the HBSC study. Int J Public Health. (2009) 54:180–90. doi: 10.1007/s00038-009-5409-5
15. Fismen AS, Torsheim T, Samdal O. A school based study of time trends in food habits and their relation to socio-economic status among Norwegian adolescents, 2001-2009. Int J Behav Nutr Phys Act. (2014) 11:115. doi: 10.1186/s12966-014-0115-y
16. Yaguchi-Tanaka Y, Tabuchi T. Skipping breakfast and subsequent overweight/obesity in children: a nationwide prospective study of 2.5- to 13-year-old children in Japan. J Epidemiol. (2021) 31:417–25. doi: 10.2188/jea.JE20200266
17. Alsharairi N, Somerset S. Skipping breakfast in early childhood and its associations with maternal and child BMI: a study of 2-5-year-old Australian children. Eur J Clin Nutr. (2016) 70:450–5. doi: 10.1038/ejcn.2015.184
18. Ardeshirlarijani E, Namazi N, Jabbari M, Zeinali M, Gerami H, Jalili R, et al. The link between breakfast skipping and overweigh/obesity in children and adolescents: a meta-analysis of observational studies. J Diabetes Metab Disord. (2019) 18:657–64. doi: 10.1007/s40200-019-00446-7
19. Monzani A, Ricotti R, Caputo M, Solito A, Archero F, Bellone S, et al. A systematic review of the association of skipping breakfast with weight and cardiometabolic risk factors in children and adolescents. What should we better investigate in the future? Nutrients. (2019) 11:387. doi: 10.3390/nu11020387
20. Ma X, Chen Q, Pu Y, Guo M, Jiang Z, Huang W, et al. Skipping breakfast is associated with overweight and obesity: a systematic review and meta-analysis. Obes Res Clin Pract. (2020) 14:1–8.
21. Ricotti R, Caputo M, Monzani A, Pigni S, Antoniotti V, Bellone S, et al. Breakfast skipping, weight, cardiometabolic risk, and nutrition quality in children and adolescents: a systematic review of randomized controlled and intervention longitudinal trials. Nutrients. (2021) 13:3331. doi: 10.3390/nu13103331
22. Dearden L, Bouret S, Ozanne S. Sex and gender differences in developmental programming of metabolism. Mol Metab. (2018) 15:8–19.
23. Barstad L, Juliusson P, Johnson L, Hertel J, Lekhal S, Hjelmesaeth J. Gender-related differences in cardiometabolic risk factors and lifestyle behaviors in treatment-seeking adolescents with severe obesity. BMC Pediatr. (2018) 18:61. doi: 10.1186/s12887-018-1057-3
24. Sjoberg A, Hallberg L, Hoglund D, Hulthen L. Meal pattern, food choice, nutrient intake and lifestyle factors in the goteborg adolescence study. Eur J Clin Nutr. (2003) 57:1569–78. doi: 10.1038/sj.ejcn.1601726
25. Ritchie LS, Stevens M, Schmidt M, Schreiber G, Striegel-Moore R, Wang M, et al. Dietary patterns in adolescence are related to adiposity in young adulthood in black and white females. J Nutr. (2007) 137:399–406. doi: 10.1093/jn/137.2.399
26. Fischer K, Colombani P, Langhans W, Wenk C. Cognitive performance and its relationship with postprandial metabolic changes after ingestion of different macronutrients in the morning. Br J Nutr. (2001) 85:393–405. doi: 10.1079/bjn2000269
27. Horikawa C, Kodama S, Yachi Y, Heianza Y, Hirasawa R, Ibe Y, et al. Skipping breakfast and prevalence of overweight and obesity in Asian and Pacific regions: a meta-analysis. Prev Med. (2011) 53:260–7. doi: 10.1016/j.ypmed.2011.08.030
28. Blondin S, Anzman-Frasca S, Djang H, Economos C. Breakfast consumption and adiposity among children and adolescents: an updated review of the literature. Pediatr Obes. (2016) 11:333–48. doi: 10.1111/ijpo.12082
29. Dupuy M, Godeau E, Vignes C, Ahluwalia N. Socio-demographic and lifestyle factors associated with overweight in a representative sample of 11-15 year olds in France: results from the WHO-Collaborative Health Behaviour in School-aged Children (HBSC) cross-sectional study. BMC Public Health. (2011) 11:442. doi: 10.1186/1471-2458-11-442
30. Kim J, So W. Association between frequency of breakfast eating and obesity in Korean adolescents. Iranian J Publ Health. (2012) 41:55–7.
31. Maddah M, Nikooyeh B. Obesity among Iranian adolescent girls: location of residence and parental obesity. Health Popul Nutr. (2010) 28:61–6. doi: 10.3329/jhpn.v28i1.4524
32. Thompson-McCormick JT, Bainivualiku A, Khan A, Becker A. Breakfast skipping as a risk correlate of overweight and obesity in school-going ethnic Fijian adolescent girls. NIH Public Access. (2010) 19:372–82.
33. Aanesen A, Katzmarzyk P, Ernstsen L. Breakfast skipping and overweight/obesity in first grade primary school children: a nationwide register-based study in Iceland. Clin Obes. (2020) 10:e12384. doi: 10.1111/cob.12384
34. Ahadi Z, Qorbani M, Kelishadi R, Ardalan G, Motlagh M, Asayesh H, et al. Association between breakfast intake with anthropometric measurements, blood pressure and food consumption behaviors among Iranian children and adolescents: the CASPIAN-IV study. Public Health. (2015) 129:740–7. doi: 10.1016/j.puhe.2015.03.019
35. Andersen L, Lillegaard I, Overby N, Lytle L, Klepp K, Johansson L. Overweight and obesity among Norwegian schoolchildren: changes from 1993 to 2000. Scand J Public Health. (2005) 33:99–106. doi: 10.1080/140349404100410019172
36. Antonogeorgos G, Panagiotakos D, Papadimitriou A, Priftis K, Anthracopoulos M, Nicolaidou P. Breakfast consumption and meal frequency interaction with childhood obesity. Pediatr Obes. (2012) 7:65–72.
37. Berkey C, Rockett H, Gillman M, Field A, Colditz G. Longitudinal study of skipping breakfast and weight change in adolescents. Int J Obes Relat Metab Disord. (2003) 27:1258–66.
38. Bjornara H, Vik F, Brug J, Manios Y, De Bourdeaudhuij I, Jan N, et al. The association of breakfast skipping and television viewing at breakfast with weight status among parents of 10-12-year-olds in eight European countries; the ENERGY (European energy balance research to prevent excessive weight Gain among Youth) cross-sectional study. Public Health Nutr. (2014) 17:906–14. doi: 10.1017/S136898001300061X
39. Bozic P, Djordjic V, Markovic L, Cvejic D, Trajkovic N, Halasi S, et al. Dietary patterns and weight status of primary school children in Serbia. Front Public Health. (2021) 9:678346. doi: 10.3389/fpubh.2021.678346
40. Champilomati G, Notara V, Prapas C, Konstantinou E, Kordoni M, Velentza A, et al. Breakfast consumption and obesity among preadolescents: an epidemiological study. Pediatr Int. (2020) 62:81–8.
41. Croezen S, Visscher T, Ter Bogt N, Veling M, Haveman-Nies A. Skipping breakfast, alcohol consumption and physical inactivity as risk factors for overweight and obesity in adolescents: results of the E-MOVO project. Eur J Clin Nutr. (2009) 63:405–12. doi: 10.1038/sj.ejcn.1602950
42. Debeila S, Modjadji P, Madiba S. High prevalence of overall overweight/obesity and abdominal obesity amongst adolescents: an emerging nutritional problem in rural high schools in Limpopo Province South Africa. Afr J Prim Health Care Fam Med. (2021) 13:e1–9. doi: 10.4102/phcfm.v13i1.2596
43. Dialektakou K, Vranas P. Breakfast skipping and body mass index among adolescents in Greece: whether an association exists depends on how breakfast skipping is defined. J Am Diet Assoc. (2008) 108:1517–25. doi: 10.1016/j.jada.2008.06.435
44. Dubois L, Girard M, Potvin Kent M, Farmer A, Tatone-Tokuda F. Breakfast skipping is associated with differences in meal patterns, macronutrient intakes and overweight among pre-school children. Public Health Nutr. (2009) 12:19–28.
45. Dubois L, Girard M, Potvin Kent M. Breakfast eating and overweight in a pre-school population: is there a link? Public Health Nutr. (2006) 9:436–42. doi: 10.1079/phn2005867
46. Duncan K. Modifiable risk factors for overweight and obesity in children and adolescents from São Paulo Brazil. BMC Public Health. (2011) 11:585. doi: 10.1186/1471-2458-11-585
47. Fayet-Moore F, Kim J, Sritharan N, Petocz P. Impact of breakfast skipping and breakfast choice on the nutrient intake and body mass index of Australian children. Nutrients. (2016) 8:487.
48. Lopez-Gil J, Sanchez-Miguel P, Tapia-Serrano M, Garcia-Hermoso A. Skipping breakfast and excess weight among young people: the moderator role of moderate-to-vigorous physical activity. Eur J Pediatr. (2022) 181:3195–204.
49. Grieger J, Cobiac L. Comparison of dietary intakes according to breakfast choice in Australian boys. Eur J Clin Nutr. (2012) 66:667–72. doi: 10.1038/ejcn.2011.220
50. Harding S, Teyhan A, Maynard M, Cruickshank J. Ethnic differences in overweight and obesity in early adolescence in the MRC DASH study: the role of adolescent and parental lifestyle. Int J Epidemiol. (2008) 37:162–72. doi: 10.1093/ije/dym252
51. Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity. (2007) 15:2748–60.
52. Khan A, Khan S, Burton N. Missing breakfast is associated with overweight and obesity in Bangladeshi adolescents. Acta Paediatr. (2019) 108:178–9. doi: 10.1111/apa.14553
53. Kupers L, de Pijper J, Sauer P, Stolk R, Corpeleijn E. Skipping breakfast and overweight in 2- and 5-year-old Dutch children-the GECKO Drenthe cohort. Int J Obes. (2014) 38:569–71. doi: 10.1038/ijo.2013.194
54. Maddah M, Nikooyeh B. Factors associated with overweight in children in Rasht, Iran: gender, maternal education, skipping breakfast and parental obesity. Public Health Nutr. (2009) 13:196–200. doi: 10.1017/S1368980009990589
55. de March Ronsoni R, Feijo R Jr, Melo L, Schwingel F, Filho W, de Albernaz Muniz R, et al. The use of Levosimendan for myocardiopathy due to acute Chagas’ disease. Int J Cardiol. (2009) 136:233–5. doi: 10.1016/j.ijcard.2008.04.043
56. Merten M, Williams A, Shriver L. Breakfast consumption in adolescence and young adulthood: parental presence, community context, and obesity. J Am Diet Assoc. (2009) 109:1384–91. doi: 10.1016/j.jada.2009.05.008
57. Mihrshahi S, Drayton B, Bauman A, Hardy L. Associations between childhood overweight, obesity, abdominal obesity and obesogenic behaviors and practices in Australian homes. BMC Public Health. (2017) 18:44. doi: 10.1186/s12889-017-4595-y
58. Nilsen B, Yngve A, Monteagudo C, Tellstrom R, Scander H, Werner B. Reported habitual intake of breakfast and selected foods in relation to overweight status among seven- to nine-year-old Swedish children. Scand J Public Health. (2017) 45:886–94. doi: 10.1177/1403494817724951
59. Ober P, Sobek C, Stein N, Spielau U, Abel S, Kiess W, et al. And yet again: having breakfast is positively associated with lower BMI and healthier general eating behavior in schoolchildren. Nutrients. (2021) 13:1351. doi: 10.3390/nu13041351
60. Olson J, Aldrich H, Callahan T, Matthews E, Gance-Cleveland B. Characterization of childhood obesity and behavioral factors. J Pediatr Health Care. (2016) 30:444–52.
61. Panagiotakos D, Antonogeorgos G, Papadimitriou A, Anthracopoulos M, Papadopoulos M, Konstantinidou M, et al. Breakfast cereal is associated with a lower prevalence of obesity among 10-12-year-old children: the PANACEA study. Nutr Metab Cardiovasc Dis. (2008) 18:606–12. doi: 10.1016/j.numecd.2007.05.005
62. Sandercock G, Voss C, Dye L. Associations between habitual school-day breakfast consumption, body mass index, physical activity and cardiorespiratory fitness in english schoolchildren. Eur J Clin Nutr. (2010) 64:1086–92. doi: 10.1038/ejcn.2010.145
63. Shafiee G, Kelishadi R, Qorbani M, Motlagh M, Taheri M, Ardalan G, et al. Association of breakfast intake with cardiometabolic risk factors. J Pediatr. (2013) 89:575–82.
64. Traub M, Lauer R, Kesztyus T, Wartha O, Steinacker J, Kesztyus D, et al. Skipping breakfast, overconsumption of soft drinks and screen media: longitudinal analysis of the combined influence on weight development in primary schoolchildren. BMC Public Health. (2018) 18:363. doi: 10.1186/s12889-018-5262-7
65. Vik F, Te Velde S, Van Lippevelde W, Manios Y, Kovacs E, Jan N, et al. Regular family breakfast was associated with children’s overweight and parental education: results from the ENERGY cross-sectional study. Prev Med. (2016) 91:197–203. doi: 10.1016/j.ypmed.2016.08.013
66. Wadolowska L, Hamulka J, Kowalkowska J, Ulewicz N, Gornicka M, Jeruszka-Bielak M, et al. Skipping breakfast and a meal at school: its correlates in adiposity context. report from the ABC of healthy eating study of polish teenagers. Nutrients. (2019) 11:1563. doi: 10.3390/nu11071563
67. Odegaard A, Jacobs D Jr, Steffen L, Van Horn L, Ludwig D, Pereira M. Breakfast frequency and development of metabolic risk. Diabetes Care. (2013) 36:3100–6.
68. Utter J, Scragg R, Schaaf D, Fitzgerald E, Wilson N. Correlates of body mass index among a nationally representative sample of New Zealand children. Int J Pediatr Obes. (2007) 2:104–13.
69. Lehto R, Ray C, Lahti-Koski M, Roos E. Meal pattern and BMI in 9-11-year-old children in Finland. Public Health Nutr. (2011) 14:1245–50. doi: 10.1017/S1368980010003034
70. Tin S, Ho S, Mak K, Wan K, Lam T. Breakfast skipping and change in body mass index in young children. Int J Obes. (2011) 35:899–906.
71. Santiago A, Clegg D, Routh V. Estrogens modulate ventrolateral ventromedial hypothalamic glucose-inhibited neurons. Mol Metab. (2016) 5: 823–33.
72. Tee E, Nurliyana A, Norimah A, Mohamed H, Tan S, Appukutty M, et al. Breakfast consumption among Malaysian primary and secondary school children and relationship with body weight status - Findings from the mybreakfast study. Asia Pac J Clin Nutr. (2018) 27:421–32. doi: 10.6133/apjcn.062017.12
73. Cho S, Dietrich M, Brown C, Clark C, Block G. The effect of breakfast type on total daily energy intake and body mass index: results from the Third National Health and Nutrition Examination Survey (NHANES III). J Am Coll Nutr. (2003) 22:296–302. doi: 10.1080/07315724.2003.10719307
74. Deshmukh-Taskar P, Nicklas T, O’Neil C, Keast D, Radcliffe J, Cho S. The relationship of breakfast skipping and type of breakfast consumption with nutrient intake and weight status in children and adolescents: the National Health and Nutrition Examination Survey 1999-2006. J Am Diet Assoc. (2010) 110:869–78. doi: 10.1016/j.jada.2010.03.023
75. Williams B, O’Neil C, Keast D, Cho S, Nicklas T. Are breakfast consumption patterns associated with weight status and nutrient adequacy in African-American children? Public Health Nutr. (2009) 12:489–96. doi: 10.1017/S1368980008002760
76. Rolland-Cachera M, Thibault H, Souberbielle J, Soulie D, Carbonel P, Deheeger M, et al. Massive obesity in adolescents: dietary interventions and behaviours associated with weight regain at 2 y follow-up. Int J Obes Relat Metab Disord. (2004) 28:514–9. doi: 10.1038/sj.ijo.0802605
77. Jakubowicz D, Wainstein J, Ahren B, Landau Z, Bar-Dayan Y, Froy O. Fasting until noon triggers increased postprandial hyperglycemia and impaired insulin response after lunch and dinner in individuals with type 2 diabetes: a randomized clinical trial. Diabetes Care. (2015) 38:1820–6.
78. Jakubowicz D, Wainstein J, Landau Z, Raz I, Ahren B, Chapnik N, et al. Influences of breakfast on clock gene expression and postprandial glycemia in healthy individuals and individuals with diabetes: a randomized clinical trial. Diabetes Care. (2017) 40:1573–9. doi: 10.2337/dc16-2753
Keywords: breakfast, children, adolescents, obesity, overweight
Citation: Wang K, Niu Y, Lu Z, Duo B, Effah CY and Guan L (2023) The effect of breakfast on childhood obesity: a systematic review and meta-analysis. Front. Nutr. 10:1222536. doi: 10.3389/fnut.2023.1222536
Received: 17 May 2023; Accepted: 22 August 2023;
Published: 06 September 2023.
Edited by:
Roberta Zupo, University of Bari Aldo Moro, ItalyReviewed by:
Naser Alsharairi, Griffith University, AustraliaNicolas Padilla-Raygoza, Institute of Public Health of the State of Guanajuato (ISAPEG), Mexico
Copyright © 2023 Wang, Niu, Lu, Duo, Effah and Guan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kun Wang, d2FuZ2t1bjYyNjIwMjNAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Kun Wang
Kun Wang Yifan Niu2†
Yifan Niu2† Zhenzhen Lu
Zhenzhen Lu Boyang Duo
Boyang Duo Clement Yaw Effah
Clement Yaw Effah