- 1Bahir Dar Zuria District Health Office, Bahir Dar, Ethiopia
- 2Department of Nutrition and Dietetics, School of Public Health, College of Medicine and Health Science, Bahir Dar University, Bahir Dar, Ethiopia
- 3Department of Public Health, College of Medicine and Health Science, Injibara University, Injibara, Ethiopia
- 4Department of Public Health, College of Health Science, Debre Markos University, Debre Markos, Ethiopia
- 5Department of Public Health, College of Health Science, Debre Tabor University, Debre Tabor, Ethiopia
Background: The inadequacy of iodine in salt is the a contributing factor behind lack of awareness and poor economic performance in developing countries. To address the issue of iodine deficiency, universal salt iodization has been implemented globally. Nevertheless, it is imperative to closely monitor the sufficiency of iodine in salts to achieve its intended objective at the household level in the Bahir Dar Zuria district.
Objective: To assess the adequacy of iodized salt and its associated factors among households in the Bahir Dar Zuria district, Northwest Ethiopia.
Methods: A community-based cross-sectional study was conducted from May to June 2022 among households in Bahir Dar Zuria district. The data were gathered from 825 households that were chosen using a multistage sampling process. Iodometric titration was used to assess the amount of iodine in salt. The data were gathered using a structured questionnaire that was administered by an interviewer. For data entry and analysis, EpiData version 3.01 and SPSS version 25.0 were used, respectively. To evaluate the association between explanatory factors and the outcome variable, binary logistic regression was conducted, and significance was determined at alpha 0.05.
Result: This study analyzed a total of 825 households. Of these, only 384 [46.5, 95% CI, 43.5–50.5%] households had adequately iodized salt at home. Age increase of 1 year [AOR = 1.04, 95% CI = 1.02–1.06], being an urban resident [AOR = 3.18, 95% CI = 1.84–5.48], diploma and above educational attainment [AOR = 3.74, 95% CI = 1.99–7.02], checking salt by asking the seller [AOR = 2.21, 95% CI = 1.26–3.88], storing salts in closed containers [AOR = 1.57, 95% CI = 1.13–2.19], and storing salts in a dry and cool area [AOR = 2.72, 95% CI =1.37–5.42] were associated with the adequacy of iodized salt at the household level.
Conclusion and recommendation: The percentage of households in the district (46.5%) that had enough iodized salt in their homes is still extremely low and falls short of the targeted level for the country. At the household level, adequate iodized salt was found to be associated with age, place of residence, level of education, checking salt iodization while purchasing, place of salt storage, and cover use for salt containers. Therefore, increasing the accessibility of iodized salt at the household level is essential.
Background
Iodine is a trace element for the synthesis of thyroid hormones, which are required for the body’s growth, development, and control of metabolic processes (1). Iodine Deficiency Diseases (IDDs) arise when the body does not receive the required quantity of iodine daily (2). IDD is a preventable public health problem on a global, regional, and national scale (3). More than 120 nations throughout the world use the well-established method of iodizing salt to avoid IDDs. At the household level, the iodine content of salt should be adequate [>15 parts per million (PPM)] (4). Ethiopia is a salt-producing country that has backed a mandated salt iodization effort and is working with UNICEF and Micronutrient initiatives to boost iodized salt use to >90%, lowering Iodine Deficiency (ID) rates (5).
Globally, more than 25% of the world’s population suffers from iodine deficiency illnesses, which remain a severe public health concern (3, 6). The number of iodine-deficient countries has decreased during the past decade from 54 to 25, while the number of countries with a sufficient intake of iodine increased from 67 to 116 (7). The percentage of people who consume enough iodized salt varies from 2 to 98% at the national and neighborhood levels (4). The combined estimate of goiter among Ethiopian children was 40.50%, and Ethiopian women had a cumulative goiter rate of more than 35.8% nationwide (8).
Inadequate iodine consumption or storage can lead to psychological growth abnormalities (cretinism, dwarfism), goiter, muscular dystrophy, spontaneous miscarriages, and hypothyroidism (2, 9). Low dietary iodine intake is the primary cause of iodine insufficiency. Populations are frequently impacted when the iodine content of the soil is reduced as a result of repeated water leaching and severe rainfall. Such soil does not contain enough iodine for crops to grow (10). The factors affecting inadequate intake of iodized salt in households are age, sex, occupational status, educational status, religion (11), salt container, knowledge regarding iodized salt availability (12), residence, duration of storage, and checking the status of salt while purchasing (13, 14).
In 2011 and 2015, the Ethiopian government demonstrated its unwavering commitment to battling ID by implementing mandatory universal salt iodization and a health sector transformation strategy to make iodized salt available to 80% of households. With the second National Nutrition Programme 2016–2020 and the 2019 National Food and Nutrition Policy playing a crucial role in tackling numerous nutrition concerns, Ethiopia has a rich nutrition policy environment (15). In 2016, the government established the second National Nutrition Program (NNP) cycle, which focused on the first 1,000 days of life, to control micronutrient deficiencies in the most vulnerable populations by 2030, one of the program’s main goals (16). However, the prevalence of IDD is more common in the research location, showing that iodized salt will not be available at the household level (17).
To the best of our knowledge, no research using the titration approach has been done in the current study area to evaluate how well-iodized salt is used in households. The Iodometric Titration Method (gold standard) (IDTM) (18) was used to measure the amount of iodine present in the salt used in each household; therefore, this study aims to determine the adequacy of iodized salt and its associated factors at the household level in the Bahir Dar Zuria district, Northwest Ethiopia, 2022.
Materials and Methods
Study design, area, and period
A community-based, cross-sectional study was conducted in the Bahir Dar Zuria district of Northwest Ethiopia from May 20 to June 30, 2022. The Bahir Dar Zuria district is one of the 14 districts in the West Gojjam Zone and is located around Bahir Dar City, approximately 560 kilometers from Addis Ababa. The district is situated at an altitude of 1,700–2,300 meters above sea level. Approximately 1,035 mm of rain falls on the district each year on average. The minimum and maximum temperatures are 10°C and 32°C, respectively. According to a survey of the land in this woreda, 21% of it is arable, 9% is pasture, 8% is forest or shrubland, 36% is submerged under water, and the remaining 26% is unusable land.
Sample size determination and sampling technique
The sample size was determined using the following presumptions and the formula for a single population proportion, , 4% with margin error, 28.9% projected percentage of households with adequate iodized salt, 95% confidence level (19). The total sample size is 850 when the design effect of 1.5 and the 15% non-response rate are taken into account. A multistage sampling procedure was used to choose the study participants. From a total of 36 rural and urban kebeles, 5 rural and 4 urban kebeles were randomly chosen by lottery method. Based on the size of the households, the sample size was proportionally assigned to each of the chosen kebeles, and households from each of the kebeles were again chosen using systematic random sampling techniques.
Data collection tools and procedures
The data were gathered using a structured face-to-face interviewer-administered questionnaire that was tailored to the local context and adapted from pertinent research to incorporate all the factors in the evaluation tool. The data were gathered by nine experienced diploma nurses and five lab technicians, under the supervision of three BSc nurses. After carefully interviewing the respondents of the chosen households in the community, a 50 g sample of salt was carefully taken and placed in an airtight plastic bag. By releasing iodine from the salt and titrating the iodine with sodium thiosulphate while utilizing starch as an external indicator, the iodine content of the salt was discovered. The iodine levels of the salt samples were examined using an iodometric titration technique in the laboratory of the Ethiopian Public Health Institute. Approximately 3 tablespoons (50 g) of salt will dissolve in roughly one hundred milliliters (100 ml) of purified water. To convert all of the iodate present to free iodine, 30 mg of potassium iodide powder was added after the pH was brought down to 2.8 using 0.6% hydrochloric acid. Utilizing newly prepared starch as the endpoint indication, the freed iodine was titrated with a freshly prepared 0.004 M sodium thiosulphate solution. Iodine concentration in parts per million (PPM) was estimated using the standard conversion table for iodine determination, and the thiosulphate level in the burette was noted. Each household’s three triplicate samples had their mean calculated (20).
The wealth index was calculated using data on the possession of various consumer goods by the household, including television; number of oxen, sheep, and cars; and details about the home, including the type of flooring, the type of drinking water source, the number of restrooms, and other elements that were indicative of financial security. The assessment methods for urban and rural respondents are different and those tools were taken from the Ethiopian Demographic and Health Survey. The resulting asset scores were generated by the principal component analysis and were standardized to a normal distribution with a mean of zero and a standard deviation of one. These standardized scores are then used to establish the breakpoints that designate the three groups of wealth quintiles as poor, middle, and rich (16). The multicollinearity of the analysis was checked by the variance inflation factor (VIF).
Operational definition
Iodine levels of the salt
If the tested salt had an iodine content ≥15 PPM, it was considered to be adequately iodized; nevertheless, if the result was <15 PPM, it was assumed to be inadequately iodized (21).
Knowledge about iodized salt
Participants were thought to have good knowledge of iodized salt if their scores for knowledge questions were above the mean and poor knowledge if their scores were below the mean (19).
Data processing and analysis
After being coded, cleaned, and entered using EPI Data version 3.01, the data were transferred to SPSS version 25.0 for further processing and analysis. The frequency distribution, percentages, and proportions were ascertained using descriptive analysis. A binary logistic regression model was used to ascertain the associations between dependent and independent variables with a 95% confidence level. Adjusted odds ratio (AOR) with 95% CI in multivariable logistic regression and a p-value of <0.05 were used to determine the significant association, which included all explanatory factors with a p-value of <0.25 in the bivariable analysis. The odds ratio was used to determine how strongly the independent and dependent variables were associated. Hosmer and Lemeshow test (p = 0.11) was used to assess the model’s fitness.
Results
Socio-demographic characteristics of respondents
Out of 850 households, 825 respondents were interviewed, which gives a 97.1% response rate. Out of these participants, 748 (90.7%) were female respondents. The respondents’ average age was 33.15 + 8.84 years, with ages ranging from 19 to 63. The majority of respondents (95.6%) identified as Orthodox Christians; 85% were married; and 41.2% were illiterate. A total of 748 (78.5%) of the study’s households had families with less than five members (Table 1).
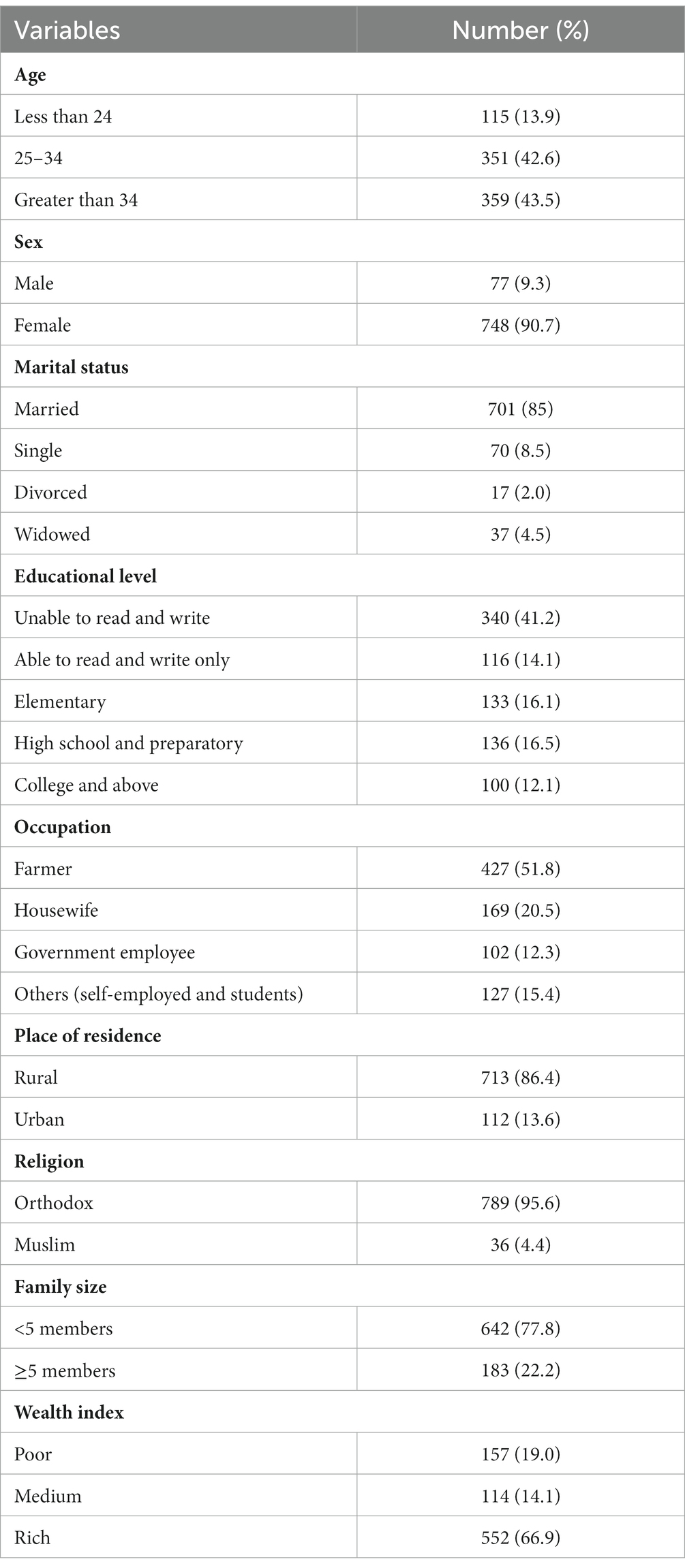
Table 1. Socio-demographic characteristics of respondents at households in Bahir Dar Zuria district, Northwest Ethiopia, 2022 (n = 825).
Knowledge about iodized salt and IDD
When asked if the respondents had ever heard of iodized salt, 825 (100%) responded that they had heard information about iodized salt from a variety of sources. Of them, 603 (73.1%) heard it from health professionals. A total of 486 (58.7%) respondents thought packed salt was iodized salt. However, 590 (71.5%) of respondents did not know that iodine deficiency disease is common in Ethiopia. According to this study’s findings, 442 respondents (or 53.6%) had overall good knowledge about iodized salt (Table 2).
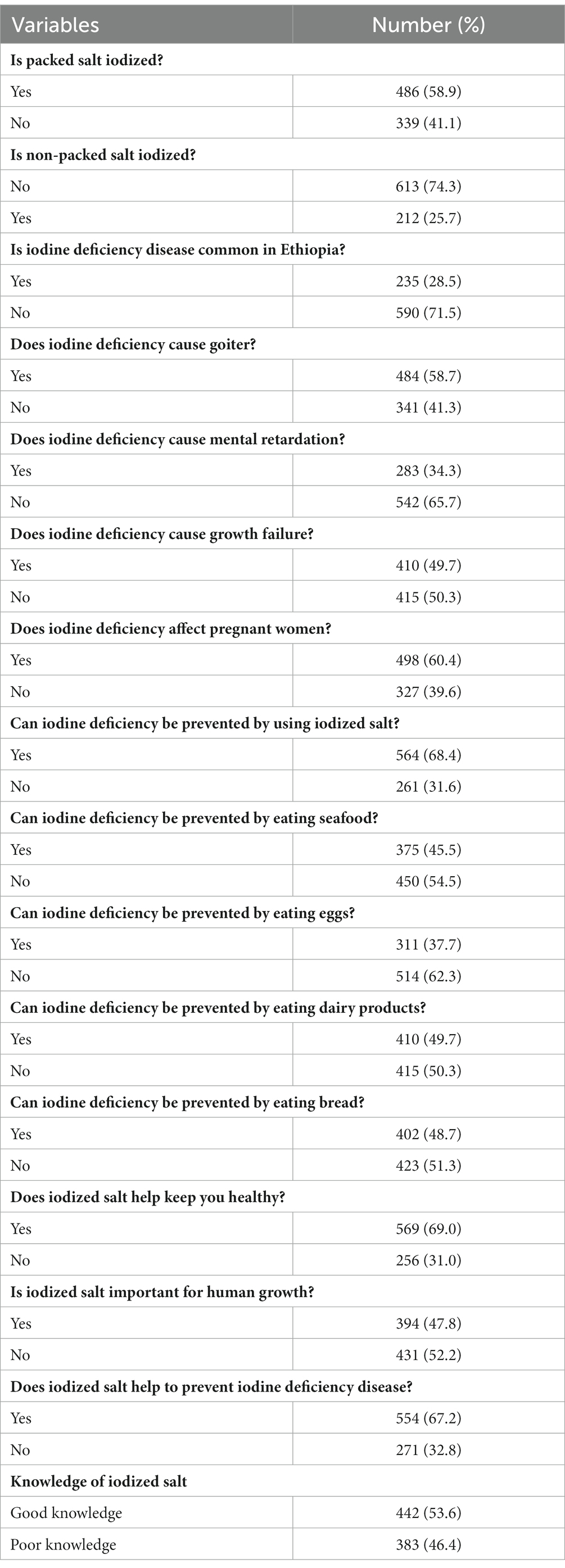
Table 2. Knowledge of respondents regarding iodized salt and IDD in households in the Bahir Dar Zuria district, Northwest Ethiopia, 2022 (n = 825).
Practice related to salt handling in the households
A total of 774 (93.8%) of the respondents said they kept their salt in a cool, dry location. However, 568 (68.8%) of the respondents kept the salt for more than 2 months after purchasing (Table 3).
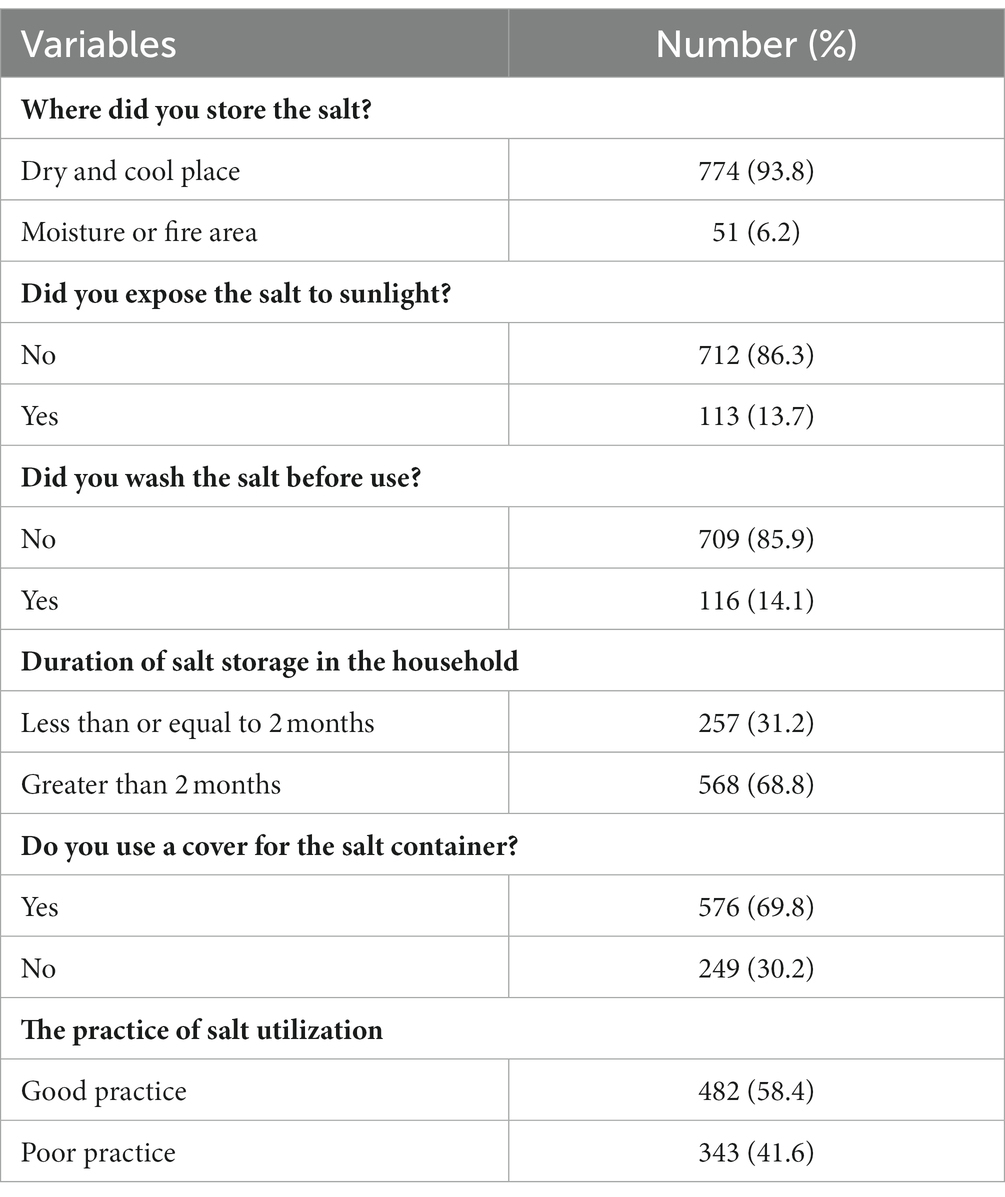
Table 3. Salt handling practice of the respondents in households in the Bahir Dar Zuria district, Northwest Ethiopia, 2022 (n = 825).
Accessibility and market related factors
A total of 433 (53%) respondents traveled less than 30 min to get iodized salt and 425 (51.5%) bought salt from the open market without reading the packs/labels (Table 4).
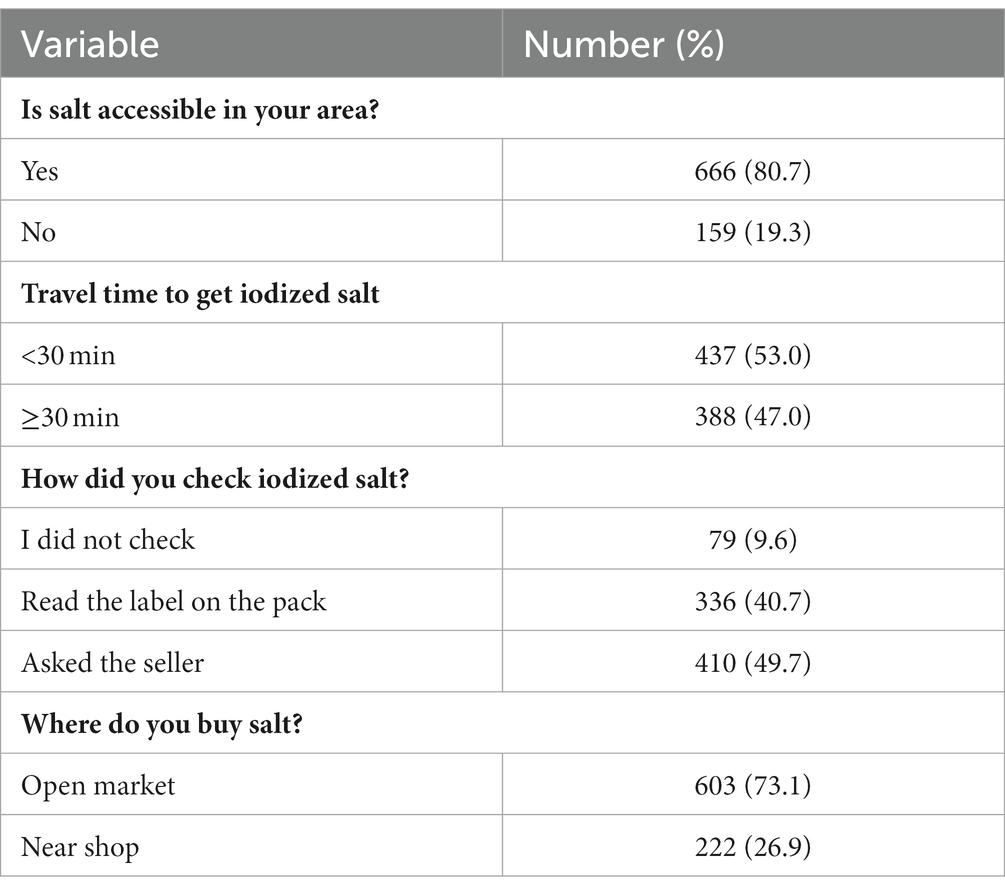
Table 4. Accessibility market related factors of iodized salt in households in the Bahir Dar Zuria district, Northwest Ethiopia, 2022 (n = 825).
Factors associated with adequacy of iodized salt
Out of a total of 825 households, 384 (46.5%) [95% CI: 43.5–50.5%] have enough iodized salt at home, according to this study. Nine variables (age of the respondent, educational status, residence, knowledge about iodized salt and IDD, place of storage, duration of storage, cover use for salt container, place where they bought salt, and method of checking whether or not the salt is iodized) found to have a p-value of <0.25 in the bivariate binary logistic regression analysis were selected for the multivariable binary logistic regression model.
However, after adjusting for each of the previous variables using a multivariable binary logistic regression model, only the age of the respondent, educational status, residence, place of storage, cover use for the salt container, and method of checking whether the salt is iodized or not while buying were significant factors associated with the adequacy of iodized salt at a p-value < 0.05. Accordingly, the odds of having adequate iodized salt in the home increased by 4% for every year that the respondent’s age rose [AOR = 1.04, 95% CI = 1.02–1.06], and people who lived in urban areas were 3.18 times more likely to have adequate iodized salt than people who lived in rural areas [AOR = 3.18, 95% CI = 1.84–5.48]. The probabilities of having adequate iodized salt were 2.02 and 3.74 times higher in people with a primary education and a diploma or above, respectively [AOR = 2.02, 95% CI =1.26–3.24] and [AOR = 3.74, 95% CI = 1.99–7.02]. Similarly, participants who kept their salt in a dry, cool area and asked the seller to check the degree of iodization had probabilities of having adequate iodized salt that were 2.72 and 2.21 times higher, respectively, than those who did not [AOR = 2.72, 95% CI =1.37–5.42] and [AOR = 2.21, 95% CI = 1.26–3.88]. Compared to households that stored their salt in open containers, households that utilized covers on their salt containers were 57% more likely to have adequate iodized salt [AOR = 1.57, 95% CI = 1.13–2.19] (Table 5).
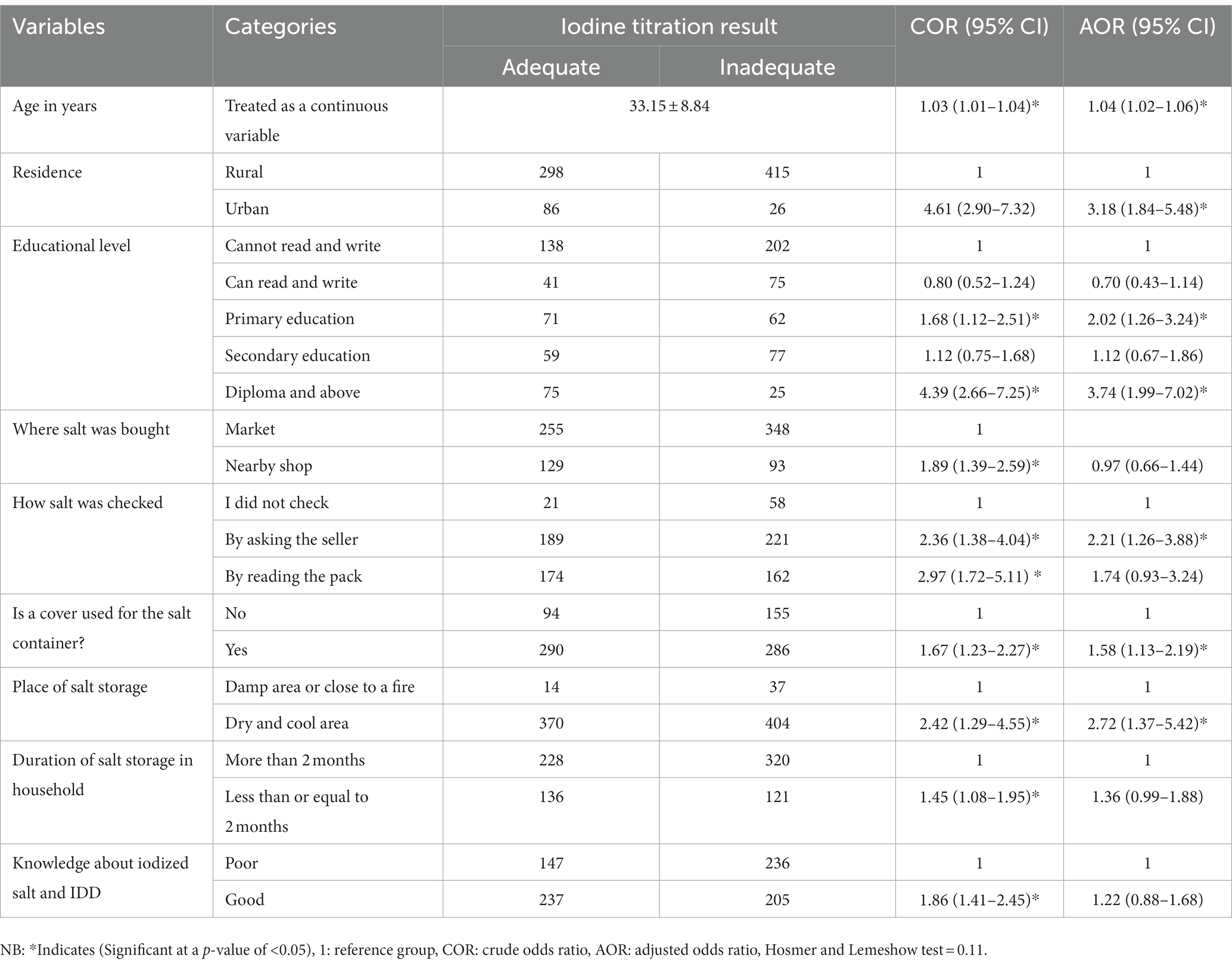
Table 5. Factor association with the adequacy of iodized salt in households in the Bahir Dar Zuria district, Northwest, Ethiopia, 2022 (n = 825).
Discussion
One of the most well-liked and effective public health initiatives for the global eradication of IDD is the universal iodization of salt (22). According to the legislation on salt released by the Ethiopian Council of Ministers in March 2011, all salt meant for human consumption must be iodized, and any such iodized salt must comply with the specifications for iodized salt stipulated by the appropriate authorities (23). However, this study found that 46.5% of households used adequate iodized salt (15 PPM), with a 95% confidence interval (CI) of [43–50.5%]. This research supports the findings of Jabitanan and West Gojjam (48.3%) (24).
The World Health Organization’s goal of eradicating iodine deficiency illnesses (≥90%) is substantially exceeded by this finding (1). According to the findings of this study, the proportion of households with adequate iodized salt is less than in earlier studies from Combolcha (68.8%) (25), Assella (62.5%) (26), and Dera (57.4%) (27), Oromia Regional State, South East Ethiopia (61.1%) (28), Southeast Ethiopia (56.6%) (28), Kolfe Keraniyo, Addis Ababa (95.5%) (29), Sidama Zone (65%) (30), China (89%) (31), Ghana (75.6%) (32), and India (75%) (33). This may be a result of the market’s accessibility and availability of iodized salt, as well as laws, policies, and ongoing follow-up and monitoring of the use of iodized salt in various nations.
The figures reported in this study, however, are higher than those that had previously been reported in Mecha (25.7%) (34), Dega Damot, West Gojjam (4.6%) (21), Jijiga town (40.8%) (14), Maychew, North Ethiopia (33%) (12), Gondar town (28.9%) (19), Addis Ababa (20%), Dire Dawa (7.5%) (35), Bale (32.7%) (36), Wollega (23.6%) (37), Arba Minch (41.8%) (38), Wolayita Sodo (37.7%) (20), and Volta region, Ghana (24.2%) (39). This variation may be due to a difference in the study’s execution period. The coverage of iodized salt increased from 28.4% in 2000 to 89% in 2016, according to the Ethiopian Demography and Health Survey (16). Even while national surveys show that the use of iodized salt in households has increased over time, the iodine content of the salt is still fairly low. Additionally, it could be the result of variations in the accessibility and availability of iodized salt on the market, iodine fortification regulations, and monitoring of iodized salt consumption in certain nations.
In this study, age, place of residence, level of education, checking of salt iodization while buying, place of salt storage, and cover use for salt containers were identified as significantly associated factors with the adequacy of iodized salt in the households. As age grew by one unit, the probability that the household had adequate iodized salt increased by 1.04 times. This result is supported by studies in Bahir Dar (40) and Arba Minch (38). This might be because age increases the ability to ask the seller, understand, and read the information on iodized salt.
The odds of having adequate iodized salt were 3.18 times higher in urban residents than in rural residents. This finding aligns with studies in Jibat Woreda, West Shoa Zone, Ethiopia (41), Nejo Woreda, Oromia Region, Ethiopia (42), and Bangladesh (43). This might be due to access to pure water, proper handling of salt, and checking of salt at the time of purchase. Urban residents had the opportunity to purchase and have a variety of sources that deliver the importance of iodized salt.
The odds of having adequately iodized salt in the household were 2.02 and 3.74 times higher in participants who attended primary education and had a diploma or higher, respectively. The result of studies done in Dera, Northwest Ethiopia (27), Mecha, Northwest Ethiopia (34), Jibat Woreda, West Shoa Zone, Ethiopia (41), Myichew Northern Ethiopia (12), Volta region Ghana (39), Bangladesh (43), and Pakistan (44) support this finding. This may be because education has the power to alter and read the levels of information on iodized salt. This and the fact that the majority of respondents mentioned a lack of sufficient knowledge and awareness of the benefits of iodized salt as their reasons for not purchasing it suggest that education facilitates access to and the use of iodized salt.
The study also found that the salt storage container and place were significant factors that affected how much iodized salt was adequate in the household. At the household level, edible salt can maintain more of its iodine content when stored in dry, covered containers. Other comparable studies carried out in the Lay Armachiho district and Gondar validated this conclusion (19, 45). This could be because salt that is kept in a moist environment collects moisture and becomes wet, which pushes the iodide component to the bottom of the container. Furthermore, if the container is opened when it’s hot, the salt may shed moisture from the surface, and as iodine is volatile, this could result in iodine loss.
Furthermore, households who asked the sellers about the iodization of the salt while buying salt had a 2.21 times higher likelihood of having adequate iodized salt than those who did not. This may be because members of the households do not understand or cannot comprehend the exact expiration date and iodized salt notifications. Similar research by Arba Minch (30) showed that the adequacy of iodized salt in household salt was not found to be associated with food handler knowledge or practice (30).
Conclusion
The amount of iodized salt that is adequate for households in the district is less than what the WHO recommends. Additionally, we discovered that the existence of adequate iodized salt in a household was related to factors such as age, place of residence, level of education, checking of salt iodization while buying, place of salt storage, and cover use for salt containers. To increase the iodine content of salt at the household level, women should be encouraged to pursue education, and it should be recommended that households store their iodized salt in a dry environment in a closed container, and customers inquire about the seller or study the salt’s packaging when making their purchases.
Strengths and limitations
This investigation used the gold standard iodometric titration measurement to determine the iodine content in households. However, this research was entirely quantitative. If it were combined with qualitative research, it might be more quantifiable. Therefore; future researchers will be conducting ca strong design and the most accurate and reliable urine concentration measurement. The use of urine concentration measurement increases the accuracy and dependability of sample measurement. Additional research also required to determine whether salt iodine loss occurs at the salt’s manufacturing facility, during transportation, or in the storage.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Bahir Dar University, College of Medicine and Health Science. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because Oral consent was obtained from each respondents. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ET, OS, GE, YD, MB, TK, and AD made substantial contributions to conception and design, managing the data, or analysis and interpretation of data, took part in drafting the article or revising it critically for important intellectual content, agreed to submit it to the current journal, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
We would like to thank Bahir Dar University for giving us ethical clearance to conduct this study. Our deepest gratitude is also extended to the study participants of this research for their consent and wholehearted participation and for devoting their time, without which this research would not have been successful.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
EDHS, Ethiopian Demographic and Health Survey; IDD, Iodine Deficiency Disorders; IDTM, Iodometric Titration Method; IRB, Institutional Review Board; NNP, National Nutrition Program; PPM, Parts Per Million; UNICEF, United Nations Children’s Fund; USI, Universal Salt Iodization; WHO, World Health Organization.
References
1. WHO. GUIDELINE: fortification of food-grade salt with iodine for the prevention and control of iodine deficiency disorders. Who Guideline. (2014):1–43.
2. WHO/UNICEF/ICCIDD. Assessment of iodine deficiency disorders and monitoring their elimination. World Health Organization. (2014) 28:1–108.
3. Shaikh, F, Jafry, SIA, and Khan, AA. Factors affecting the consumption of iodized salt by pregnant women in Karachi. Pak J Med Sci. (2022) 38:577–82. doi: 10.12669/pjms.38.3.4991
4. Alamneh, AA, Leshargie, CT, Desta, M, Birhanu, MY, Assemie, MA, Denekew, HT, et al. Availability of adequately iodized salt at the household level in Ethiopia: a systematic review and meta-analysis. PLoS One. (2021) 16:e0247106–12. doi: 10.1371/journal.pone.0247106
5. Adish, A, Chuko, T, Abay, A, Assey, V, and Desta, T. Ethiopia: breaking through with a new iodized salt law. IDD Newsletter. (2013) 41:7–8.
6. Dinka, AW, Kebebe, T, and Nega, G. Iodine level of salt and associated factors at household level in Gidami District, Oromia region, Ethiopia: a cross-sectional study. Nutr Diet Suppl. (2021) 13:9–16. doi: 10.2147/nds.s284944
7. Situation, H, No, R, and Status, F. UNICEF/EAPRO East Asia and Pacific regional office. The East Asia Pacific regional workshop on achievement of universal salt iodization for optimal iodine nutrition: A meeting report. Bangkok: UNICEF (2015).
8. Gebretsadikan, TM, and Troen, AM. Progress and challenges in eliminating iodine deficiency in Ethiopia: a systematic review. BMC Nutr. (2016) 2:1–12. doi: 10.1186/s40795-016-0051-0
9. Asadul, M, Rahanur, M, Ghosh, S, and Rahman, T. Heliyon impact of knowledge, attitude, and practice on iodized salt consumption at the household level in selected coastal regions of Bangladesh. Heliyon. (2021) 7:e06747. doi: 10.1016/j.heliyon.2021.e06747
10. World Health Organisation (WHO). Iodine deficiency disorders in the who African region: report of THE regional director. Reginal office for Africaeginal office for Africa (2008) 58:1–5.
11. Muktar, M, Roba, KT, and Gebremichael, BMB. Iodine deficiency and its associated factors among primary school children in Anchar district, eastern Ethiopia. Pediatric Health, Medicine and Therapeutics Publish. (2018) 9:89–95. doi: 10.2147/PHMT.S165933
12. Gidey, B, Alemu, K, Atnafu, A, Kifle, M, and Tefera, YSH. Availability of adequate iodized salt at household level and associated factors in rural communities in Laelay Maychew District, northern Ethiopia: a cross sectional study. J Nutr Health Sci. (2015) 1:1–9. doi: 10.15744/2393-9060.1.403
13. Desta, AA, Kulkarni, U, Abraha, K, Worku, S, and Sahle, BW. Iodine level concentration, coverage of adequately iodized salt consumption and factors affecting proper iodized salt utilization among households in North Ethiopia: a community based cross sectional study. BMC Med Educ. (2019) 5:28. doi: 10.1186/s40795-019-0291-x
14. Senbeta, AM, Mamo, FT, Desalegn, BB, and Daba, AK. Knowledge and practices of iodized salt utilization, health consequences, and iodine concentration on dietary salts at retailer and households in Jigjiga town, Somali, Ethiopia. Cogent Food Agricult. (2021) 7:7. doi: 10.1080/23311932.2021.1911421
15. Truebswasser, U, Genye, T, and Bossuyt, A. Review of the nutrition policy landscape in Ethiopia 2010 – 2020. International Food Policy Research Institute. (2020) Available at: http://www.nipn.ephi.gov.et/sites/default/files/inline-files/Nutrition_Policy_Landscape_FINAL_Report.pdf
16. Central Statistical Agency(CSA). Ethiopian demographic and health survey(EDHS), Federal Democratic Republic of Ethiopia, Addis Ababa, Ethiopia. Maryland: ICF international Calverton (2016).
17. Gebremichael, G, Demena, M, Egata, G, and Gebremichael, B. Prevalence of goiter and associated factors among adolescents in Gazgibla District, Northeast Ethiopia. Global Adv Health Med. (2020) 9:216495612092362–5. doi: 10.1177/2164956120923624
18. Yadav, K, Kumar, R, Chakrabarty, A, and Pandav, C. A reliable and accurate portable device for rapid quantitative estimation of iodine content in different types of edible salt. Indian J Public Health. (2015) 59:204–9. doi: 10.4103/0019-557x.164658
19. Gebremariam, HG, Yesuf, ME, and Koye, DN. Availability of adequately iodized salt at household level and associated factors in Gondar town, Northwest Ethiopia. ISRN Public Health. (2013) 5:392. doi: 10.11591/.v5i4.4841
20. Kumma, WP, Haji, Y, Abdurahmen, J, and Mehretie, AY. Factors affecting the presence of adequately iodized salt at home in Wolaita, southern Ethiopia: community based study. Int J Food Sci. (2018) 2018:1–9. doi: 10.1155/2018/4394908
21. Afework, A, Mulu, W, Abate, A, and Lule, A. Handling and adequacy of iodine at household level: community based cross-sectional survey in Dega Damot District, west Gojjam zone, Amhara regional State, Ethiopia. bioRxiv. (2019). doi: 10.1101/586677
22. Jain, S, Kilyani, M, and Dylan Walters, NK. The need for Investment in Information. Forensic Intelligence. (2020):248–71. doi: 10.1201/b10137-13
23. FRP. Ethiopian Council of Ministers. Salt iodization Council of Ministers Regulation. Addis Ababa, Ethiopia. Federal Negarit Gazette. (2014) 20:8686–95.
24. Woyraw, W, and Getachew Hailu, GM. K smos Publishers concentration of iodine in iodized common salt at household level. Adv. Nutr. Food Sci. (2018) 1:1–10.
25. Mekonnen, TC, Eshete, S, Wasihun, Y, Arefaynie, M, and Cherie, N. Availability of adequately iodized salt at household level in Dessie and Combolcha towns, South Wollo, Ethiopia. BMC Public Health. (2018) 18:1–9. doi: 10.1186/s12889-018-6066-5
26. Hawas, SBLS. Proper utilization of Adequatly iodized salt at house hold level and associated Factores in Asella town Arsi zone Ethiopia: a community based cross sectional study. J Food Process Technol. (2016) 7:07. doi: 10.4172/2157-7110.1000573
27. Anteneh, ZA, Engidayehu, M, and Abeje, G. Iodine content of dietary salt at household level and associated factors using Iodometric titration methods in Dera District, Northwest Ethiopia. BMC Nutr. (2017) 3:1–7. doi: 10.1186/s40795-017-0203-x
28. Bulli, AT, Aredo, MT, and Hailu Fekadu, AHR. Proper utilization of iodized salt and associated factors among rural community of HETOSA district, Oromia regional STATE, SOUTH East Ethiopia. Angew Chem Int Ed. (2020) 6:951–2. doi: 10.1101/2020.06.04.133926
29. Ayigegn, H, Wolde, T, Geleta, D, Haile, K, and Alemu, A. Adequately iodized salt and associated factors at household level in Kolfe keraniyo sub-city, Addis Ababa, Ethiopia. J Food Nutr Sci. (2020) 8:1–8. doi: 10.11648/j.jfns.20200802.12
30. Tafere, GSB. High variability of iodine in iodized salt and urine from rural households in Sidama zone, southern Ethiopia: a cross-sectional study. Afr J Food Agric Nutr Dev. (2020) 20:15235–51. doi: 10.18697/ajfand.89.17520
31. Fan, L, Su, X, Shen, H, Liu, P, Meng, F, Yan, J, et al. Iodized salt consumption and iodine deficiency status in China: a cross-sectional study. Global Health J. (2017) 1:23–37. doi: 10.1016/S2414-6447(19)30076-4
32. Agbozo, F, Der, JB, Glover, NJ, and Ellahi, B. Household and market survey on availability of adequately iodized salt in the Volta region, Ghana. Int J Health Promot Educ. (2017) 55:110–22. doi: 10.1080/14635240.2016.1250658
33. Sai Deepika, P, Thirumala Rao, B, Vamsi, A, Valleswary, K, and Chandra, SM. A cross sectional study on proper use of iodized salt in communities of rural areas and its relevant factors in Prakasam district, Andhra Pradesh, India. Int J Commun Med Public Health. (2019) 6:1083. doi: 10.18203/2394-6040.ijcmph20190590
34. Tariku, WB, and Mazengia, AL. Knowledge and utilization of iodized salt and its associated factors at household level in Mecha District, Northwest Ethiopia. J Nutr Metab. (2019) 2019:1–8. doi: 10.1155/2019/9763830
35. Yaye, AB, Baraki, N, and Endale, BS. Availability of adequately iodized salt at household level and associated factors in Dire Dawa, eastern Ethiopia. Int J Public Health Sci. (2016) 5:392. doi: 10.11591/ijphs.v5i4.4841
36. Kalu, TA. Coverage of iodized salt and associated factors at household level in Goba town, bale zone, South East Ethiopia, 2015. Sci J Public Health. (2016) 4:346. doi: 10.11648/j.sjph.20160404.22
37. Yazew, T. Availability of adequately iodized salt at household level and its associated factors in Horro Woreda, Horro Guduru Wollega zone, Oromia, Ethiopia. Pathol Lab Med. (2020) 4:20. doi: 10.11648/j.plm.20200401.14
38. Ajema, D, Bekele, M, Yihune, M, Tadesse, H, Gebremichael, G, and Mengesha, MM. Socio-demographic correlates of availability of adequate iodine in household salt: a community-based cross-sectional study. BMC Res Notes. (2020) 13:1–6. doi: 10.1186/s13104-020-04983-w
39. Sarah, NA, Prince, AK, Yao, AS, Geoffrey, AA, Wisdom, TK, and Margaret, K. Knowledge on iodized salt use and iodine content of salt among households in the Hohoe municipality, Volta Region – Ghana. Central Afr J Public Health. (2016) 2:1–10. doi: 10.11648/j.cajph.20160201.11
40. Mersha, T, Derso, T, Jemal, M, Kedir, S, and Mohammed, B. Determine the iodine content of salt at the household level and its predictors in Bahirdar town, Northwest Ethiopia. Pan Afr Med J. (2022) 41:260. doi: 10.11604/pamj.2022.41.260.17910
41. Gemede, HF, and Tamiru, B, Fite MB. Knowledge, Practice, and availability of iodized salt and associated factors in Jibat Woreda, west Shoa zone, Ethiopia. Int J Food Sci (2021);2021. doi: 10.1155/2021/5562390, 1–10
42. Gutema, EA, Mangistu, M, and Tura, JB. Jour n a l o f W om ens H e determinants and availability of adequately iodized salt at household level in Nejo Woreda, Oromia region, Ethiopia, 2019, community based cross sectional study. J Women’s Health Care. (2022) 11:581. doi: 10.35248/2167-0420.22.11.581
43. Khan, JR, Biswas, RK, Sheikh, MT, and Huq, M. Factors associated with the availability of iodized salt at household level: a case study in Bangladesh. Public Health Nutr. (2019) 22:1815–23. doi: 10.1017/S1368980018003907
44. Lowe, N, Westaway, E, Munir, A, Tahir, S, Dykes, F, Lhussier, M, et al. Increasing awareness and use of iodised salt in a marginalised community setting in north-West Pakistan. Nutrients. (2015) 7:9672–82. doi: 10.3390/nu7115490
Keywords: adequacy, availability, iodized salt, households, Bahir Dar Zuria, Ethiopia
Citation: Temech EC, Said O, Endalik G, Demilew YM, Belay MA, Kassie TD and Dessie AM (2023) Adequacy of iodized salt and its associated factors among households in the Bahir Dar Zuria district, Northwest Ethiopia, 2022. Front. Nutr. 10:1215613. doi: 10.3389/fnut.2023.1215613
Edited by:
Tao Feng, Shanghai Institute of Technology, ChinaReviewed by:
Mohammad Ali Mohsenpour, Shiraz University of Medical Sciences, IranMahdi Shadnoush, Shahid Beheshti University of Medical Sciences, Iran
Copyright © 2023 Temech, Said, Endalik, Demilew, Belay, Kassie and Dessie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mahider Awoke Belay, bWFoaWRlcnNlbGFtQGdtYWlsLmNvbQ==
 Emebet Chalachew Temech1
Emebet Chalachew Temech1 Mahider Awoke Belay
Mahider Awoke Belay Tadele Derbew Kassie
Tadele Derbew Kassie Anteneh Mengist Dessie
Anteneh Mengist Dessie