
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 06 October 2023
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1200077
This article is part of the Research Topic Anthropometric Assessment View all 13 articles
Background: Mid-upper arm circumference (MUAC) is a potentially credible alternative method for body mass index (BMI) to assess nutritional status. We aimed to assess the correlation between MUAC and BMI- Z-score and to identify a reliable MUAC cut-off point to detect underweight (BMI- Z-score of < −2 standard deviation) Sudanese adolescents.
Methods: A cross-sectional study was conducted in eastern Sudan. After obtaining adolescents’ age and sex, their weight, height, and MUAC were measured using the standard procedures. The MUAC (cm) cut-off corresponding to underweight was calculated using receiver operating characteristic (ROC) curve analysis.
Results: In total, 390 adolescents were enrolled in the study and 205 (52.6%) of them were females. The median (interquartile range, IQR) age was 15.1 (14.0–16.3) years. The medians (IQR) of MUAC and BMI- Z-score were 22.0 (20.0–24.0) cm and − 0.62 (−1.5–0.3), respectively. MUAC was positively correlated with BMI Z-score in all participants (r = 0.534, p < 0.001), in females (r = 0.715, p < 0.001), and in males (r = 0.404, p < 0.001). Of the 390 enrolled adolescents, 61(15.6%) were underweight. The MUAC cut-off for underweight was ≤21.2 cm in all participants (Youden’s Index, YI = 0.50; sensitivity = 82.0%; specificity = 68.0%, AUROCC = 0.78), in females (YI = 0.66, sensitivity = 86.0%, specificity = 80.0%, AUROCC = 0.87), and in males (YI = 0.32, sensitivity = 80.0%, specificity = 52.0%, AUROCC = 0.69).
Conclusion: MUAC has good accuracy results and can be adopted for community-based screening of underweight adolescents.
Adolescence is defined by “The World Health Organization (WHO)” as an age between 10 and 19 years. Adolescents constitute 16% of the global population and the majority (90%) live in low-and middle-income countries (1, 2). Adolescence represents the period of development that starts at puberty and ends at adulthood, which reflects the physiological pattern (3). Adolescents are vulnerable to several risk factors for adult non-communicable diseases, communicable diseases, nutritional diseases, and malnutrition (4). Malnutrition among adolescents is associated with several medical problems such as increased risk of contracting communicable diseases, delayed growth, lower intellectual quotient, impaired cognitive maturation, and behavioral problems (5). Undernutrition is associated with poverty, violence, food insecurity, impaired sexual and reproductive health, and risk of contracting communicable and non-communicable diseases (3). Recent data showed that children and adolescents were at risk of malnutrition globally, and it was among the main causes of mortality: 225,906 deaths in 2013 (approximately 34 deaths per 100,000) which significantly varied between developing and developed countries with 38.5 per 100,000 and 0.2 per 100,000, respectively, (2).
Several anthropometric measurements such as weight, height, weight for height, head circumference, body mass index (BMI), mid-upper arm circumference (MUAC), and triceps skinfold thickness have been proposed to assess nutritional status (6). BMI may be affected by fluid overload, edemas, and muscle mass (7). However, the MAUC is a practical and cheap method. It is a simple measurement as it does not require difficult tools or expert frontline professionals compared to the requirements for measuring BMI (8). MAUC may be useful instead of BMI in different medical problems such as cancer, growth failure (9), among pregnant adolescents (10), and cerebral palsy (11). MUAC could be used as an alternative to BMI to evaluate nutritional status among adolescents in different countries, especially in countries with low resources (8, 12–14).
Malnutrition is a significant health problem in Sudan and it has economic, educational, and productivity impacts (15). There are no published data on the reliability of MUAC measurement in detecting the nutritional status of Sudanese adolescents. Thus, obtaining specific MUAC cut-offs for certain populations of adolescents could be an important method in countries with fewer resources like Sudan. Moreover, Sudan has suffered and is still suffering from civil war, tribal tension, famines, displaced people, and refugee crises, and thus requires a practical, simple, and cheap method to assess nutrition status. We aimed to assess the correlation between MUAC and BMI- Z-score and to identify a reliable MUAC cut-off point to detect underweight (BMI- Z-score of < −2 standard deviation) Sudanese adolescents.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) standard checklists were followed (16). The methods followed in this study have been previously described in our previous work among adults with the same objectives. In summary: a multistage sampling study was conducted in eastern Sudan (New Halfa) during the period of January to February 2021. Four out of seven sectors, which are the lowest administrative units, were selected using a simple random method. The total sample size of 390 participants (both males and females) was distributed between the selected four sectors according to the size of the sector itself. Then, adolescents (10–19 years of age) and their parents in households were selected via a lottery method. If there was no adolescent in the selected household or they refused to participate or had met one of the exclusion criteria, the next household was chosen.
Apparently healthy adolescent males and females who were residents in the area of the study, whose age was (≥10 years – ≤19 years), and who had signed consent by their guardians for participation.
Age below 10 years and above 19 years; adolescent pregnant women; adolescents with chronic diseases such as diabetes, thyroid diseases, and heart failure; critically ill patients with severe acute illness; athletes; those on hormonal medication; those who had any apparent congenital dysmorphism; adolescents on chronic medications; and those who refused to participate.
The eligible adolescents were interviewed and their sex and birth dates (confirmed from identity cards) were recorded. Anthropometric measures (weight, height, and MUAC) were taken twice and the mean of measurements was taken. The measurements followed the standard procedures using calibrated instruments. A third measurement was performed in case of considerable variation between the first two readings (differences of >100.0 g for weight, 0.5 cm for height, and 0.2 cm for MUAC). After taking off their shoes and removing heavy clothing and objects from their pockets, the participants were then weighed (to the nearest 10.0 g). Their standing height was measured (to the nearest 1 mm) by a stadiometer with their feet positioned together at the heels with the back of the heels. MUAC was measured (to the nearest 1 mm) in sitting or standing posture using a non-stretchable MUAC measuring tape which was placed at mid between the olecranon process of the left ulna and the acromion process of the left scapula. BMI was computed as weight in kg/height in m2 (17). Thereafter, BMI Z-scores were calculated using the WHO international growth reference data for children and adolescents (18).
A sample of 390 adolescents was calculated to obtain the significant minimum difference in the correlation (r = 0.15) between BMI Z-scores and MUAC. The sample (390 adolescents) had an 80% power and a difference of 5% at α = 0.05 (19).
Data were analyzed using IBM SPSS version 25. Shapiro–Wilk tests were used to check the normality of the continuous data. A non-parametric Mann–Whitney U test was used to assess the difference in variables between the groups (males and females). Scatterplots with fitted linear regression lines were computed to evaluate the association between MUAC and BMI z-score for all adolescents and for each sex separately. The sensitivity and the specificity were computed and Youden’s Index (YI) was calculated as YI = sensitivity + specificity-1. The MUAC cut-off with the highest YI-value represented the optimal statistically-derived cut-off (20). The area under the receiver operating characteristic curve (AUROCC) was obtained for all adolescents and for females and males separately. A value of p less than 0.05 was considered statistically significant.
In total, 390 adolescents were enrolled in the study and 205 (52.6%) of them were females. The median (IQR) age was 15.1 (14.0–16.3) years. The medians (IQR) of MUAC and BMI- Z-score were 22.0 (20.0–24.0) cm and − 0.62 (−1.5–0.3), respectively. Compared with males, females were significantly older, taller, and had higher MAUC and BMI Z-scores (Table 1).
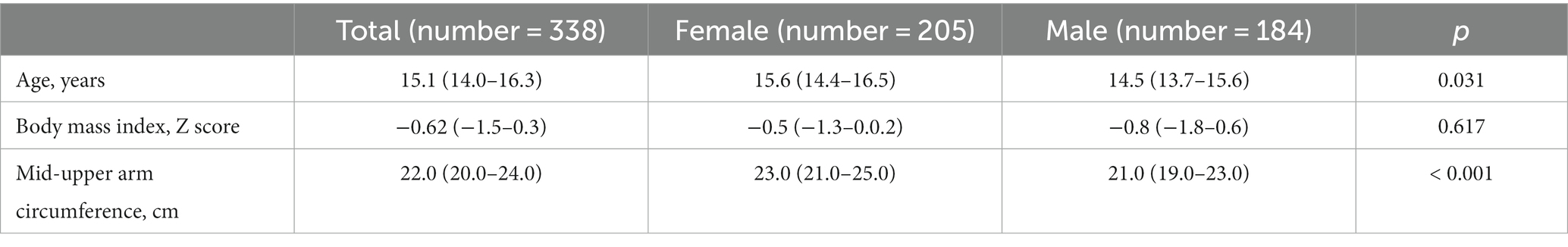
Table 1. Comparing medians (interquartile range) of anthropometric profile between adolescent boys and girls in eastern Sudan, 2021.
There was a significant positive correlation between MUAC and BMI Z-score (r = 0.534 (p < 0.001) in all participants, in females [r = 0.715 (p < 0.001)], and in males [r = 0.404 (p < 0.001; Figure 1)].
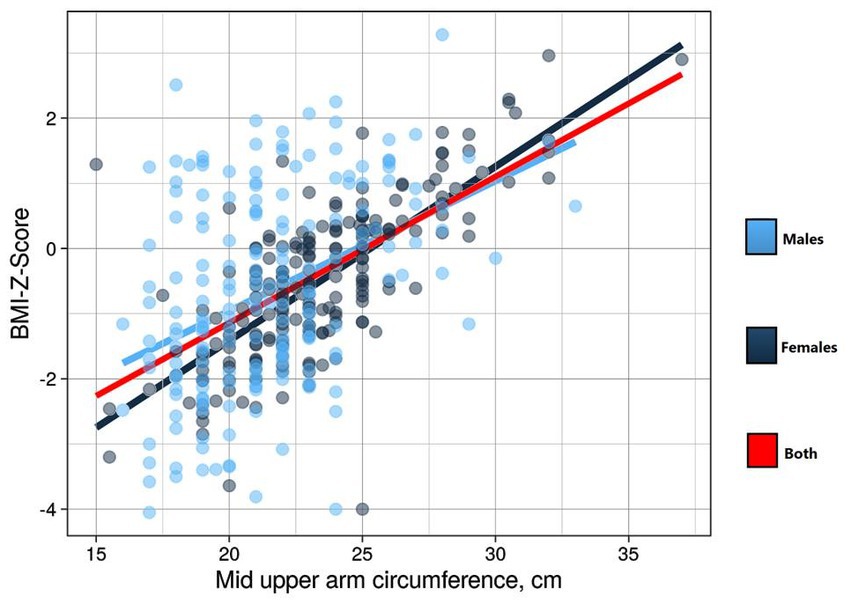
Figure 1. Curve estimation for assessing the linear relationship between mid-upper arm circumference and body mass index Z-score in adolescents in eastern Sudan 2021.
Of the 390 enrolled participants, 61(15.6%) were underweight. The best statistically derived MUAC cut-off based on BMI z-scores for underweight was ≤21.25 cm in all participants (YI = 0.50; sensitivity = 82.0%; specificity = 68.0%) with a good predictive value (AUROCC = 0.78, 95.0% CI = 0.73–0.84), in females (YI = 0.66, sensitivity = 86.0%, specificity = 80.0%), (AUROCC = 0.87, 95.0% CI = 0.79–0.95), and in males (YI = 0.32, sensitivity = 80.0%, specificity = 52.0%), with a good predictive value (AUROCC = 0.69, 95.0% CI = 0.60–0.77; Table 2; Figure 2).
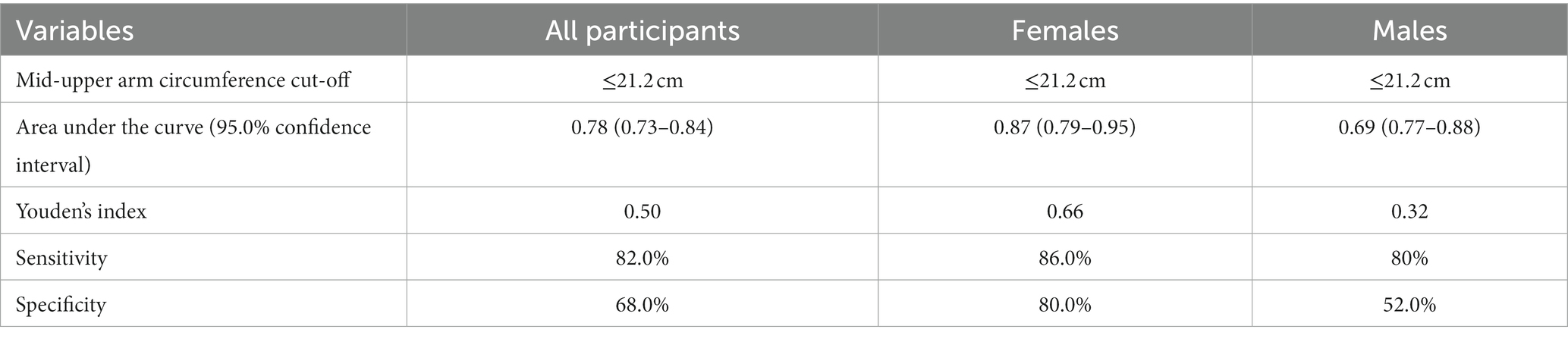
Table 2. Mid-upper arm circumference cut-off points for the diagnosis of underweight adolescents in eastern Sudan, 2021.
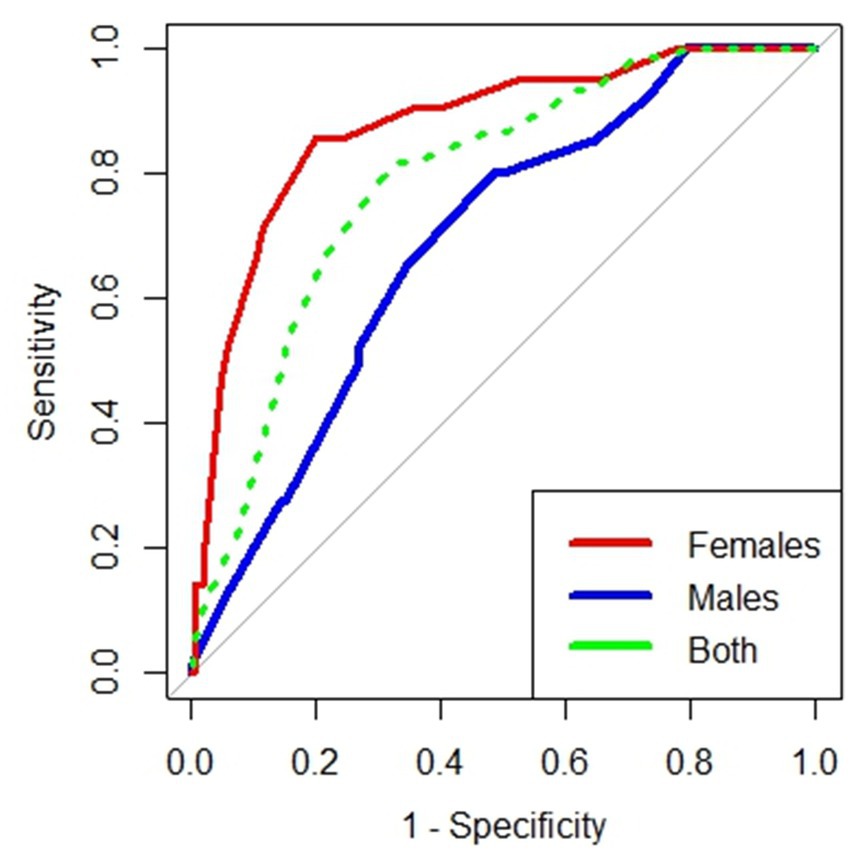
Figure 2. Receiver operating curve of mid-upper arm circumference for diagnosing underweight adolescents in eastern Sudan 2021.
Our study showed a positive correlation between BMI Z-scores and MUAC in all adolescents and in each sex separately. This goes with similar previous findings reported among adolescents in Ethiopia (r = 0.81) (13) and in Tanzania [females (R = 0.846) versus males (r = 0.459)] (21).
The best statistically derived MUAC cut-off for underweight adolescents in this study was ≤21.2 cm which showed similar results in females and males separately. The MUAC cut-off observed in our results to detect underweight adolescents was almost similar to that obtained in Tanzania in adolescents (18.5–22.0 cm, sensitivity = 40.0%, specificity = 92.5%) aged 15–17 years old (21) and in India (≤21.6 cm, sensitivity = 75.4%, specificity = 87.1%, and AUROCC = 0.91; age 15–19 years) (12). In Tanzania (21), they enrolled adolescents aged 15–17 years old and we enrolled adolescents aged ≥10 years –≤19 years and this could explain the difference in our results and the results from Tanzania. However, the MUAC cut-off which is proposed to detect underweight in the current study is slighter higher than that reported in Turkey for males (≤20.50 cm sensitivity = 60.9%, specificity = 87.4%, and AUROCC = 0.791) and females (≤20.50 cm sensitivity = 45.0.8%, specificity = 87.8%, and AUROCC = 0.748) (22), in India (≤19.4 cm sensitivity = 84.0%, specificity = 81.4% and AUROCC = 0.86) for females aged 10–14 years (12) and in another study for males (≤19.2 cm sensitivity = 82.2%, specificity = 68.9% and AUROCC = 0.77) and females (≤19.4 cm sensitivity = 87.7%, specificity = 70.9% and AUROCC =0.79) aged 10–14 years (14). Additionally, a markedly higher MUAC cut-off of more than 21.25 cm was reported among adolescents in Ethiopia (≤23.3 cm, sensitivity = 87.9%, specificity = 75.9% and AUROCC = 0.90) for males and (≤22.6 cm, sensitivity = 100% specificity = 88.2% and AUROCC = 0.97) for females (13), in India (≤22.0 cm sensitivity = 77.0%, specificity = 79.6% and AUROCC =) in adolescents aged 15–19 years (8), and in males (≤22.9 cm sensitivity = 81.9%, specificity = 75.1% and AUROCC = 0.82) and females (≤21.7 cm sensitivity = 87.9%, specificity = 77.8% and AUROCC = 0.84) aged 10–14 years (14). The different MUAC cut-off points for different populations are summarized in Table 3. The variation in MUAC cut-offs in different studies may be explained by the difference in adipose tissue as well as in skeletal muscle mass observed in some children which could be due to differences in ethnicity (23). Moreover, a significant difference according to sex and age in undernutrition was observed in some studies (24–26). Hence, no universal agreement on the MUAC cut-off point to screen malnutrition among children and adolescents (27, 28). Therefore, adopting local references of MUAC for epidemiological and anthropological studies is recommended (29). Several previous studies reported that MUAC could be an alternative tool to detect underweight/thinness among adolescents (8, 13, 21, 27–29). MAUC is useful in different clinical situations, e.g., in cases of adolescents who have edema (7), chronic disorders and growth failure (9, 30, 31), cerebral palsy (11) severe learning disabilities (32), and anorexia nervosa (33, 34). Additionally, MUAC has also been adopted for many years for assessing nutritional status in certain conditions, like famines or refugee crises, where ordinary methods for height and weight measurements are difficult to perform (35). Furthermore, adopting a restricted MUAC cut-off for discharging children from severe acute malnutrition treatment can predict and prevent relapses and hospital readmission (36). Likewise, it has been shown to predict the worsening of nutritional status in low-income countries with laboratory indicators for hemoglobin, ferritin, zinc, serum albumin, and plasma retinol concentrations as dependent variables (37). Moreover, MUAC has emerged as the measurement that was most preferred by participants because it is less distressing than routinely used measurement techniques for weight and skin fold (34). Interestingly a simplified method of MAUC-based weight estimation can be used for the administration of many drugs and fluid regimens in emergency medicine that are weight-dependent in patients and when no standard adult weight estimation tools exist or are difficult to perform (27, 38, 39).
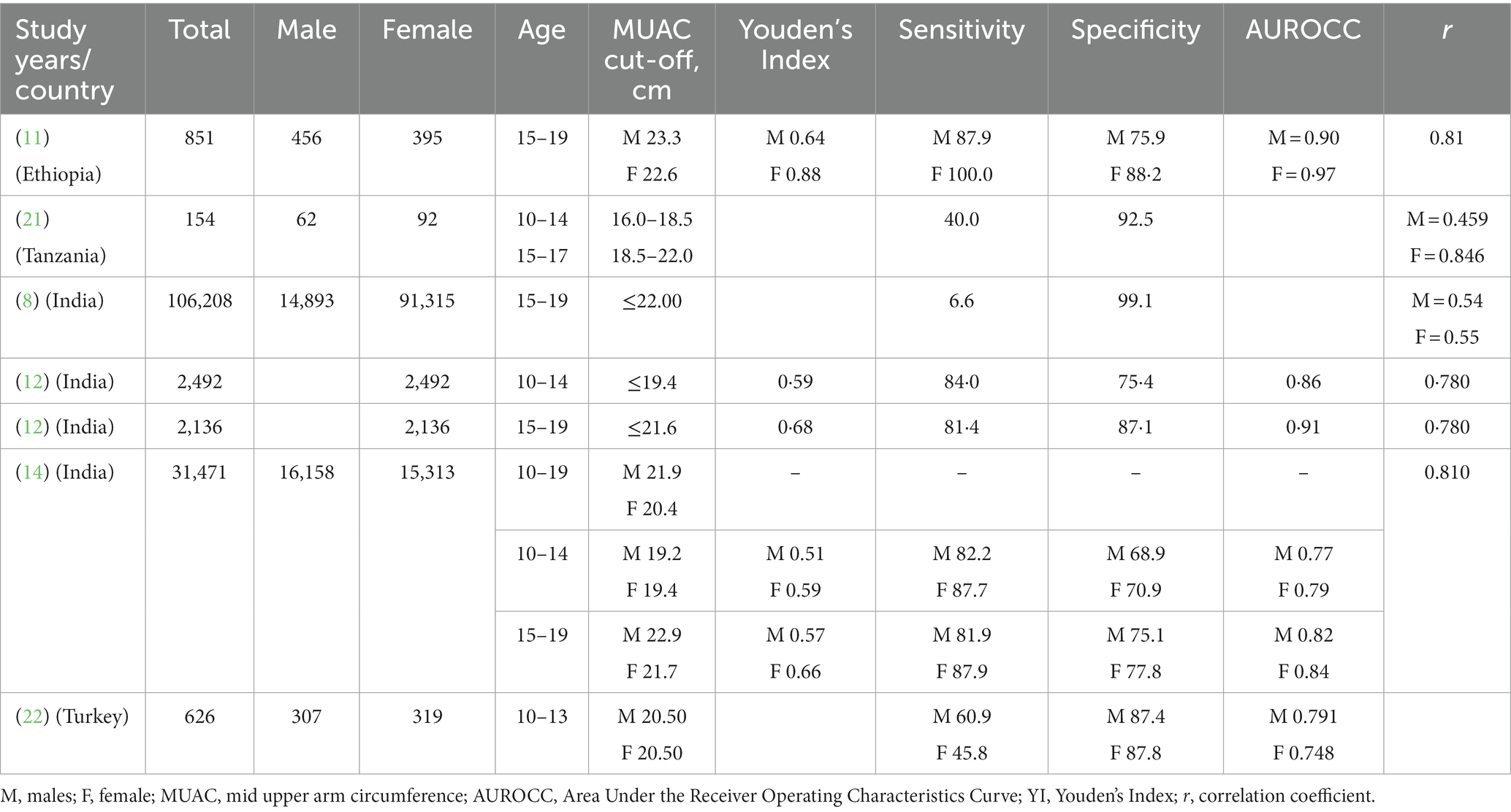
Table 3. Specificity, correlation coefficients and the area under the receiver operating characteristic curve (AUROC) from different studies on underweight adolescents using mid-upper arm circumference and body mass index Z-scores.
Our study is a community-based study and enrolled both males and females and these are strengths of this study. One limitation of the present study is that the data for MUAC cut-off from this area might be different from other areas in Sudan. Moreover, height, weight, and MUAC are all measurements that are subjected to measurement error due to inter-observer differences in measurement or miscalculation error (40). A larger sample size might have strengthened the prevalence of the outcome and the analysis.
Our study proposes the cut-offs based on MUAC (≤22.5 cm) as an alternative for BMI for community-based screening of underweight adolescents.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by this study complies with the Declaration of Helsinki. Ethics approval was obtained from the Ethics Committee of the Faculty of Medicine of Gadarif University, Sudan (Reference number #2021.03). Written informed consent was collected from each participant. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
IM and SO conceived the study and supervised data collection. AA, AA-N, and IA supervised the work, guided the analysis, critically reviewed the manuscript, prepared the analysis plan, performed the data analysis, and wrote the first draft of the paper. All authors reviewed and approved the final manuscript.
The researchers would like to thank the Deanship of Scientific Research, Qassim University for funding the publication of this project.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AUROCC, Area Under the Receiver Operating Characteristics Curve; BAZ, BMI-for-age Z-score; BMI, Body mass index; CI, Confidence interval; cm, centimeter; IQR, Interquartile range; kg, kilogram; ROC, receiver operating characteristic curve; m, meter; MUAC, mid-upper arm circumference; YI, Youden’s Index; SPSS, Statistical Package for the Social Sciences; STROBE, The Strengthening the Reporting of Observational Studies in Epidemiology; WHO, The World Health Organization.
1. WHO. Health for the world’s adolescents: a second chance in the second decade: summary (2014). Available at: https://apps.who.int/iris/handle/10665/112750
2. Vos, T, Kyu, HH, Pinho, C, Wagner, JA, Brown, JC, Bertozzi-Villa, A, et al. Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: findings from the global burden of disease 2013 study. JAMA Pediatr. (2016) 170:267. doi: 10.1001/jamapediatrics.2015.4276
3. Patton, GC, Sawyer, SM, Santelli, JS, Ross, DA, Afifi, R, Allen, NB, et al. Our future: a lancet commission on adolescent health and wellbeing. Lancet. (2016) 387:2423–78. doi: 10.1016/S0140-6736(16)00579-1
4. Kassebaum, NJ, Reiner, RC, Olsen, HE, Ikeda, CT, Echko, MM, Ballestreros, KE, et al. Diseases, injuries, and risk factors in child and adolescent health, 1990 to 2017: findings from the global burden of diseases, injuries, and risk factors 2017 study. JAMA Pediatr. (2019) 173:e190337. doi: 10.1001/jamapediatrics.2019.0337
5. Onyango, AW. Promoting healthy growth and preventing childhood stunting: a global challenge. Matern Child Nutr. (2013) 9:1–5. doi: 10.1111/mcn.12092
6. Ruggiero, A, Maurizi, P, Rinninella, E, Triarico, S, Triarico, S, and Cintoni, M. Clinical tools to assess nutritional risk and malnutrition in hospitalized children and adolescents. Eur Rev Med Pharmacol Sci. (2017) 21:2690–701.
7. Romero-Corral, A, Somers, VK, Sierra-Johnson, J, Thomas, RJ, Collazo-Clavell, ML, Korinek, J, et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes. (2008) 32:959–66. doi: 10.1038/ijo.2008.11
8. Roy, A, and Sekher, TV. Mid upper arm circumference as an alternative measure to assess the nutritional status of adolescents: a study in India based on NFHS-4 data. J Biosoc Sci. (2022) 54:617–28. doi: 10.1017/S0021932021000298
9. Khadilkar, AV, Khadilkar, VV, Gondhalekar, KM, Kajale, NA, Karkera, PH, Prasad, M, et al. Reference centile curves for mid-upper arm circumference for assessment of under- and overnutrition in school-aged Indian children and adolescents. Nutrition. (2021) 91-92:111401. doi: 10.1016/j.nut.2021.111401
10. Yimer, B, and Wolde, A. Prevalence and predictors of malnutrition during adolescent pregnancy in southern Ethiopia: a community-based study. BMC Pregnancy Childbirth. (2022) 22:130. doi: 10.1186/s12884-022-04460-1
11. Jahan, I, Muhit, M, Al Imam, MH, Ghose, R, Chhetri, AB, Badawi, N, et al. Nutritional status of children with cerebral palsy in Gorkha, Nepal: findings from the Nepal cerebral palsy register. Nutrients. (2021) 13:2537. doi: 10.3390/nu13082537
12. Sethi, V, Gupta, N, Pedgaonkar, S, Saraswat, A, Dinachandra Singh, K, Rahman, HU, et al. Mid-upper arm circumference cut-offs for screening thinness and severe thinness in Indian adolescent girls aged 10-19 years in field settings. Public Health Nutr. (2019) 22:2189–99. doi: 10.1017/S1368980019000594
13. Sisay, BG, Haile, D, Hassen, HY, and Gebreyesus, SH. Mid-upper arm circumference as a screening tool for identifying adolescents with thinness. Public Health Nutr. (2021) 24:457–66. doi: 10.1017/S1368980020003869
14. Nitika, T. Discriminatory performance of mid-upper arm circumference for identifying thin and severely thin adolescents: a secondary data analysis using comprehensive National Nutrition Survey. Nepal J Epidemiol. (2021) 11:1023–33. doi: 10.3126/nje.v11i2.33926
15. Abu-Fatima, O, Abbas, AAG, Racalbuto, V, Smith, L, and Pizzol, D. Child undernutrition in Sudan: the social and economic impact and future perspectives. Am J Trop Med Hyg. (2021) 104:1149.
16. Cuschieri, S. The STROBE guidelines. Saudi J Anaesth. (2019) 13:S31–4. doi: 10.4103/sja.SJA_543_18
17. WHO Consultation on Obesity and World Health Organization Obesity: preventing and managing the global epidemic: report of a WHO consultation. (2000), Available at: https://apps.who.int/iris/handle/10665/42330
18. Croft, TN, Aileen, MJ, and Marshall, CKA. Guide to DHS statistics, vol. 7. Rockville, Maryland, USA: ICF (2018).
19. Bujang, MA, and Baharum, N. Sample size guideline for correlation analysis. World J Soc Sci Res. (2016) 3:37. doi: 10.22158/wjssr.v3n1p37
20. Hughes, G. Youden’s index and the weight of evidence revisited. Methods Inf Med. (2015) 54:576–7. doi: 10.3414/ME15-04-0007
21. Lillie, M, Lema, I, Kaaya, S, Steinberg, D, and Baumgartner, JN. Nutritional status among young adolescents attending primary school in Tanzania: contributions of mid-upper arm circumference (MUAC) for adolescent assessment. BMC Public Health. (2019) 19:1582. doi: 10.1186/s12889-019-7897-4
22. Mercan, Y, Kafadar, GC, Arikan, SH, and Pancar, N. An investigation of anthropometric measurements of early adolescents and determination of BMI-for-age-based neck circumference and BMI-for-age-based mid-upper-arm circumference cut-off points. Clin Nutr ESPEN. (2022) 48:414–20. doi: 10.1016/j.clnesp.2022.01.008
23. Oyhenart, EE, Castro, LE, Garraza, M, Cesani, MF, Torres, MF, Quintero, FA, et al. Comparative study of mid-upper arm circumference, arm muscle area and arm fat area percentiles in Argentinean and US children aged 4-14 years. Nutr Hosp. (2019) 36:552–62. doi: 10.20960/nh.02426
24. Senbanjo, IO, and Oshikoya, KA, Njokanma OF. Upper arm composition and nutritional status of school children and adolescents in Abeokuta Southwest Nigeria. World J Pediatr. (2014) 10:336–42. doi: 10.1007/s12519-014-0470-4
25. Ozturk, A, Budak, N, Cicek, B, Mazicioglu, MM, Bayram, F, and Kurtoglu, S. Cross-sectional reference values for mid-upper arm circumference, triceps skinfold thickness and arm fat area of Turkish children and adolescents. Int J Food Sci Nutr. (2009) 60:267–81. doi: 10.1080/09637480701663854
26. Thurstans, S, Opondo, C, Seal, A, Wells, J, Khara, T, Dolan, C, et al. Boys are more likely to be undernourished than girls: a systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob Heal. (2020) 5:4030. doi: 10.1136/bmjgh-2020-004030
27. Talma, H, Van Dommelen, P, Schweizer, JJ, Bakker, B, Kist-Van Holthe, JE, Chinapaw, JMM, et al. Is mid-upper arm circumference in Dutch children useful in identifying obesity? Arch Dis Child. (2019) 104:159–65. doi: 10.1136/archdischild-2017-313528
28. Chaput, JP, Katzmarzyk, PT, Barnes, JD, Fogelholm, M, Hu, G, Kuriyan, R, et al. Mid-upper arm circumference as a screening tool for identifying children with obesity: a 12-country study. Pediatr Obes. (2017) 12:439–45. doi: 10.1111/ijpo.12162
29. Oyhenart, EE, Torres, MF, Garraza, M, Cesani, MF, Navazo, BR, Castro, LE, et al. Reference percentiles for mid-upper arm circumference, upper arm muscle and fat areas in the argentine child and adolescent population (4–14 years old). Arch Argent Pediatr. (2019) 117:E347–55. doi: 10.5546/aap.2019.eng.e347
30. Yaprak, DS, Yalçın, B, Pınar, AA, and Büyükpamukçu, M. Assessment of nutritional status in children with cancer: significance of arm anthropometry and serum visceral proteins. Pediatr Blood Cancer. (2021) 68:e28752. doi: 10.1002/pbc.28752
31. Revuelta Iniesta, R, Paciarotti, I, Davidson, I, McKenzie, JM, Brougham, MFH, and Wilson, DC. Nutritional status of children and adolescents with cancer in Scotland: a prospective cohort study. Clin Nutr ESPEN. (2019) 32:96–106. doi: 10.1016/j.clnesp.2019.04.006
32. Hardy, J, Kuter, H, Campbell, M, and Canoy, D. Reliability of anthropometric measurements in children with special needs. Arch Dis Child. (2018) 103:757–62. doi: 10.1136/archdischild-2017-314243
33. Fernandez-del-Valle, M, Larumbe-Zabala, E, Graell-Berna, M, and Perez-Ruiz, M. Anthropometric changes in adolescents with anorexia nervosa in response to resistance training. Eat Weight Disord. (2015) 20:311–7. doi: 10.1007/s40519-015-0181-4
34. Lam, PY, Marshall, SK, Devi Harjit, G, Coelho, JS, and Cairns, J. Pinch, cinch or step: evaluating the effectiveness and acceptability of mid upper arm circumference measurements in adolescents with eating disorders. Eat Behav. (2016) 22:72–5. doi: 10.1016/j.eatbeh.2016.03.023
35. James, WPT, Mascie-Taylor, GCN, Norgan, NG, Bistrian, BR, Shetty, PS, and Ferro-Luzzi, A. The value of arm circumference measurements in assessing chronic energy deficiency in third world adults. Eur J Clin Nutr. (1994) 48:883–94.
36. Guesdon, B, Katwal, M, Poudyal, AK, Bhandari, TR, Counil, E, and Nepali, S. Anthropometry at discharge and risk of relapse in children treated for severe acute malnutrition: a prospective cohort study in rural Nepal. Nutr J. (2021) 20:32. doi: 10.1186/s12937-021-00684-7
37. Kulathinal, S, Freese, R, Korkalo, L, Ismael, C, and Mutanen, M. Mid-upper arm circumference is associated with biochemically determined nutritional status indicators among adolescent girls in Central Mozambique. Nutr Res. (2016) 36:835–44. doi: 10.1016/j.nutres.2016.04.007
38. Ruiz Brunner, MLM, Cieri, ME, Butler, C, and Cuestas, E. Development of equations and software for estimating weight in children with cerebral palsy. Dev Med Child Neurol. (2021) 63:860–5. doi: 10.1111/dmcn.14857
39. Cattermole, GN, and Manirafasha, A. Accuracy of weight estimation methods in adults, adolescents and children: a prospective study. Emerg Med J. (2021) 38:718–23. doi: 10.1136/emermed-2020-209581
Keywords: body mass index, Z-score, mid-upper arm circumference, underweight, adolescents
Citation: Musa IR, Omar SM, AlEed A, Al-Nafeesah A and Adam I (2023) Mid-upper arm circumference as a screening tool for identifying underweight adolescents. Front. Nutr. 10:1200077. doi: 10.3389/fnut.2023.1200077
Received: 04 April 2023; Accepted: 18 September 2023;
Published: 06 October 2023.
Edited by:
Asima Karim, University of Sharjah, United Arab EmiratesReviewed by:
Hurtado José Antonio, University of Alicante, SpainCopyright © 2023 Musa, Omar, AlEed, Al-Nafeesah and Adam. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Abdullah Al-Nafeesah, YS5hbG5hZmVlc2FoQHF1LmVkdS5zYQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.