
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Nutr., 04 July 2023
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1174945
This article is part of the Research TopicMalnutrition in Dysphagia: Nutritional Assessment and Management in Clinical PracticeView all 6 articles
Background: The proposal of the global leadership initiative in malnutrition (GLIM) criteria has received great attention from clinicians. The criteria are mainly used in the research environment and have the potential to be widely used in the clinic in the future. However, the prevalence of malnutrition and risk of future malnutrition based on a current diagnosis of malnutrition are worth exploring.
Methods: A systematic search of PubMed, Embase, and the Cochrane Library was performed from the earliest available date to 1 February 2023. According to the diagnostic criteria of the GLIM, we analysed the prevalence of malnutrition by directly adopting the GLIM criteria for diagnosis without a previous nutritional risk screening (one-step approach) and by adopting the GLIM criteria for diagnosis after a nutritional risk screening (two-step approach). The main outcome was the prevalence of malnutrition based on the one-and two-step approaches. Secondary outcomes were the future risk of malnutrition based on the GLIM diagnosis, including mortality within and beyond 1 year. primary outcomes were pooled using random-effects models, and secondary outcomes are presented as hazard ratios (HRs) and 95% confidence intervals (CIs).
Results: A total of 64 articles were included in the study, including a total of 47,654 adult hospitalized patients and 15,089 malnourished patients based on the GLIM criteria. Malnutrition was diagnosed by the one-step approach in 18 studies and by the two-step approach in 46 studies. The prevalence of malnutrition diagnosed by the one-and two-step approaches was 53% (95% CI, 42%–64%) and 39% (95% CI, 0.35%–0.43%), respectively. The prevalence of malnutrition diagnosed by the GLIM criteria after a nutritional risk screening was quite different; the prevalence of malnutrition diagnosed by the Nutritional Risk Screening 2002 (NRS2002) GLIM tool was 35% (95% CI, 29%–40%); however, the prevalence of malnutrition diagnosed by the Mini Nutrition Assessment (MNA) GLIM tool was 48% (95% CI, 35%–62%). Among the disease types, the prevalence of malnutrition in cancer patients was 44% (95% CI, 36%–52%), while that in acute and critically ill patients was 44% (95% CI, 33%–56%). The prevalence in patients in internal medicine wards was 40% (95% CI, 34%–45%), while that in patients in surgical wards was 47% (95% CI, 30%–64%). In addition, the mortality risk within 1 year (HR, 2.62; 95% CI, 1.95–3.52; I2 = 77.1%) and beyond 1 year (HR, 2.04; 95% CI, 1.70–2.45; I2 = 59.9%) of patients diagnosed with malnutrition by the GLIM criteria was double that of patients with normal nutrition.
Conclusion: The prevalence of malnutrition diagnosed by the GLIM criteria after a nutritional risk screening was significantly lower than the prevalence of malnutrition diagnosed directly by the GLIM criteria. In addition, the mortality risk was significantly greater among malnourished patients assessed by the GLIM criteria.
Systematic review registration: identifier CRD42023398454.
Malnutrition is a global problem, and studies have shown that malnutrition can lead to adverse clinical outcomes, including increased morbidity and mortality (1). Previous malnutrition screening tools, such as the Nutritional Risk Screening 2002 (NRS2002) tool, Mini Nutrition Assessment (MNA), and Malnutrition Universal Screening Tool (MUST), can only be used in certain patient populations, and the risk of malnutrition obtained from these screening tools varies widely. The global leadership initiative in malnutrition (GLIM) criteria launched by nutrition experts from various countries in 2018 have been verified to have high diagnostic sensitivity and specificity (2, 3), demonstrating important progress in the diagnosis of malnutrition. Related studies have reported the prevalence of malnutrition in adult hospitalized patients diagnosed by the GLIM criteria, ranging from 19% to 69.7% (4–8).
Currently, the prevalence of malnutrition in adult hospitalized patients based on the GLIM criteria is unclear, and the future malnutrition risk based on a current malnutrition diagnosis is also unknown. This study mainly explored the prevalence of malnutrition based on the GLIM criteria and the future risk of malnutrition based on a current malnutrition diagnosis.
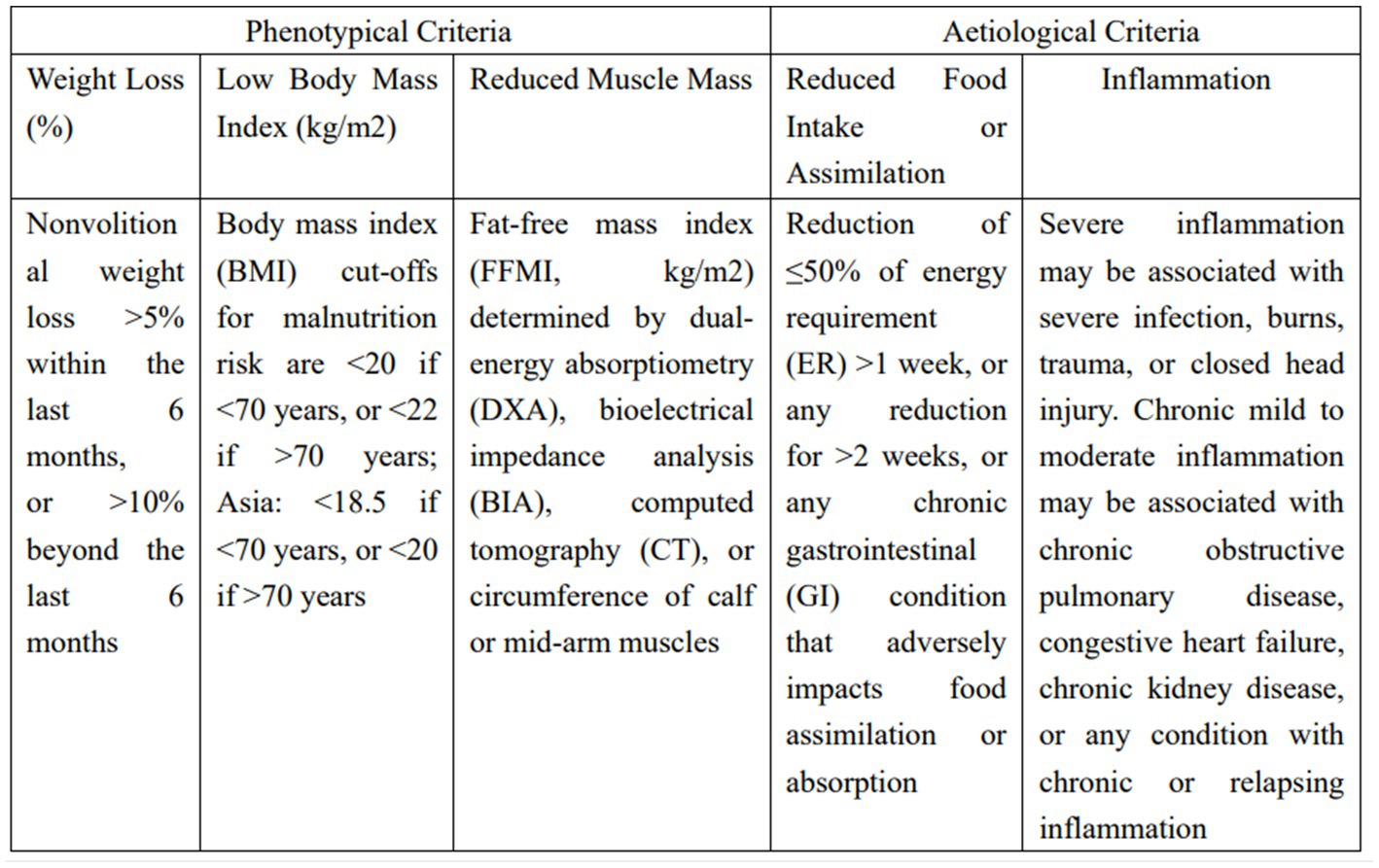
Figure 1. Global leadership initiative in malnutrition (GLIM) phenotypical and aetiological criteria for the diagnosis of malnutrition.
The meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) list, the Guidelines for Meta-Analysis of Observational Epidemiological Studies, and the study protocol (9). We performed a systematic literature search of PubMed, Embase, and the Cochrane Library (up to 10 February 2023) using a combination of MeSH/Emtree terms and title/abstract keywords. The keywords were “malnutrition” and “GLIM criteria”. Supplementary material shows the detailed search strategy. Figure 2 illustrates the complete search strategy. The titles and abstracts of all identified studies were screened by two junior researchers, and articles irrelevant to the research question were excluded. Subsequently, all remaining articles were comprehensively reviewed according to the selection criteria. References were also reviewed to identify other relevant studies. Any discrepancies were negotiated between two senior researchers.
The following inclusion criteria were adopted in this study: (1) the study was a randomized controlled trial, cohort study, case-control study, or cross-sectional study. (2) Based on the complete GLIM diagnostic criteria (Figure 1), there were clear phenotypical and aetiological criteria, including the one-step approach and two-step approach to analyse the prevalence of malnutrition; the one-step approach consisted of directly adopting the GLIM criteria for diagnosis without a previous nutritional risk screening, and the two-step approach consisted of adopting the GLIM criteria for diagnosis after first conducting a nutritional risk screening, with the GLIM criteria for the diagnosis of malnutrition including at least one phenotypical and one aetiological criterion. (3) The research population was hospitalized adults, with no limitations on the type of disease. The exclusion criteria were as follows: (1) the GLIM diagnostic criteria were incomplete, i.e., phenotypical or aetiological criteria were not evaluated or unclear. (2) Patients were nonhospitalized patients, including outpatients, those in nursing homes, and those in other related groups. (3) The study was a review article or case report.
Two junior researchers independently collected data via preestablished forms. Disagreements were resolved through discussion. The collected information mainly included author, year of publication, country or region, one-or two-step approach, initial nutritional risk screening tool, disease type, research design, and nutritional risk (survival and death) of malnourished patients.
A total of 64 articles were included in the study. We assessed nonrandomized studies using the Newcastle-Ottawa Quality Assessment Scale. Studies were assessed using three categories: study group selection (0–4 points); comparability (0–2 points); and exposure (0–3 points). A total score of ≤3 was considered to indicate low quality; 4–6, medium quality; and ≥7, high quality. These scores were used only to facilitate the interpretation of the meta-analysis results and not as criteria for the inclusion or exclusion of studies. Supplementary Table S2 shows the bias and quality of the included studies.
The primary objective of this meta-analysis was to investigate the prevalence of malnutrition and the nutritional risk in adult hospitalized patients based on the GLIM criteria. We calculated heterogeneity among studies using Cochran’s Q test and the I2 statistic. All p-values were two-tailed, and the results of all analyses were considered statistically significant at p ≤ 0.05, except the results of the heterogeneity and publication bias tests. If I2 > 50%, indicating large heterogeneity among different studies, we applied a random-effects model to calculate the pooled effect value and 95% confidence interval (CI). We also performed subgroup analysis by nutritional diagnostic tool, region and disease type. All statistical analyses were performed using STATA 17.0.
The relevant characteristics of the included literature are shown in Figure 5. There were a total of 64 studies with a total of 47,654 subjects. A total of 18 articles directly adopted the GLIM criteria for diagnosis without a previous nutritional risk screening, and the remaining 46 articles performed a nutritional risk screening first and then followed the GLIM criteria for diagnosis. The nutritional screening tools used included the NRS2002 tool, MUST, MNA, Subjective Global Assessment (SGA), or other risk screening tools and groups of several nutritional screening tools. The types of diseases included cancer, critical illness, COVID-19, stroke, dialysis, and inflammatory bowel disease. Among the 64 articles, 34 were from Asia (10–42), 20 were from Europe (4, 43–61), 9 were from America (62–70), and 1 was from Oceania (71). Of these, 16 studies reported on the future risk of malnutrition diagnosed based on the GLIM criteria (death of malnourished patients in ≤1 year), and 11 studies reported on the future risk of malnutrition diagnosed based on the GLIM criteria (death of malnourished patients in >1 year).
Figures 3 4 show the prevalence of malnutrition based on the GLIM criteria as determined by random-effect model analysis. Figure 4 shows the prevalence of malnutrition based on directly adopting the GLIM criteria for diagnosis (one-step approach), with a summarized prevalence of malnutrition of 53% (95% CI, 42%–64%). Figure 3 shows the prevalence of malnutrition based on the GLIM criteria for diagnosis after first conducting a nutritional risk screening (two-step approach), with a prevalence of 39% (95% CI, 0.35%–0.43%).
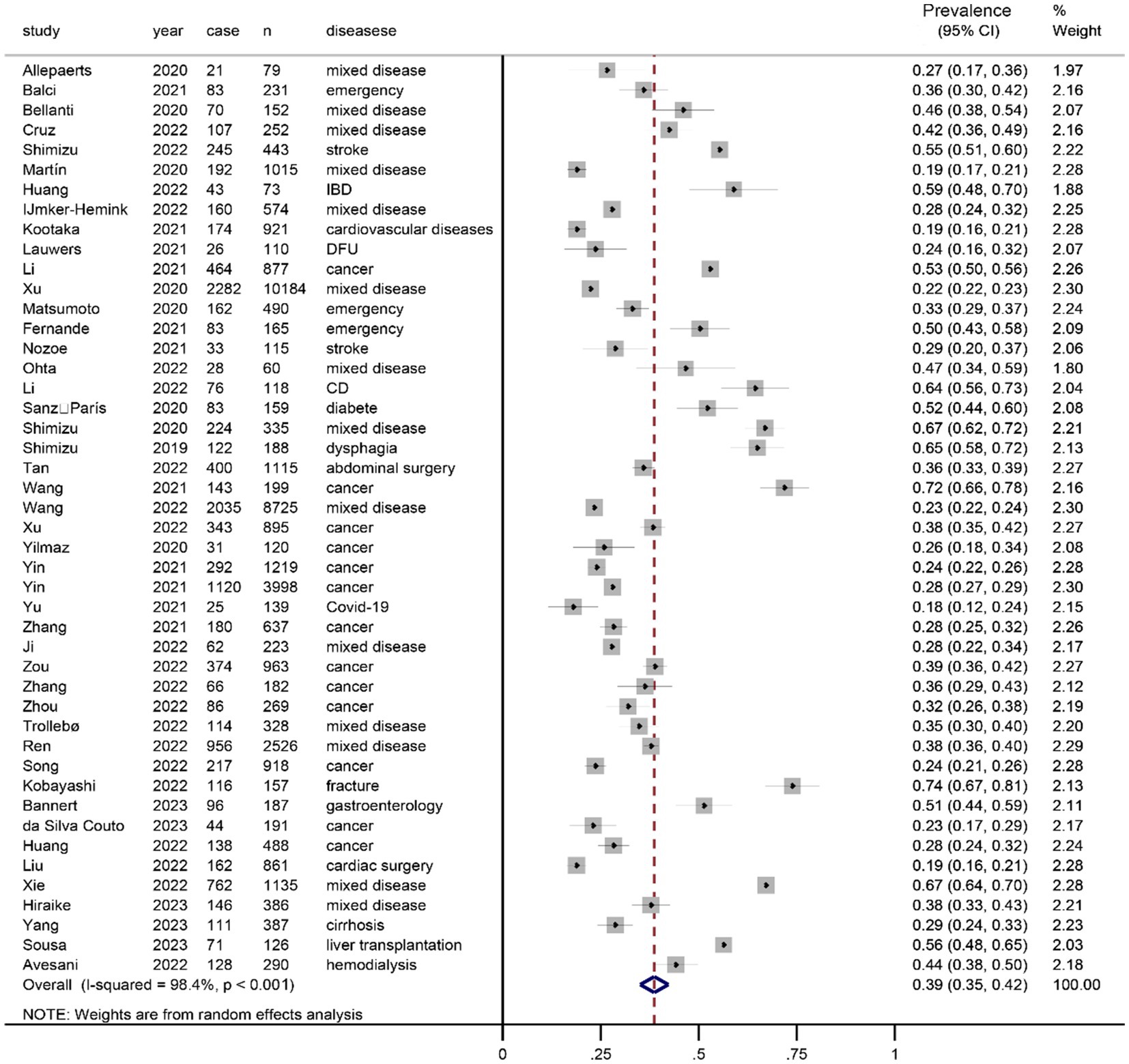
Figure 3. Prevalence of malnutrition diagnosed according to the GLIM criteria after a nutritional risk screening (two-step approach).
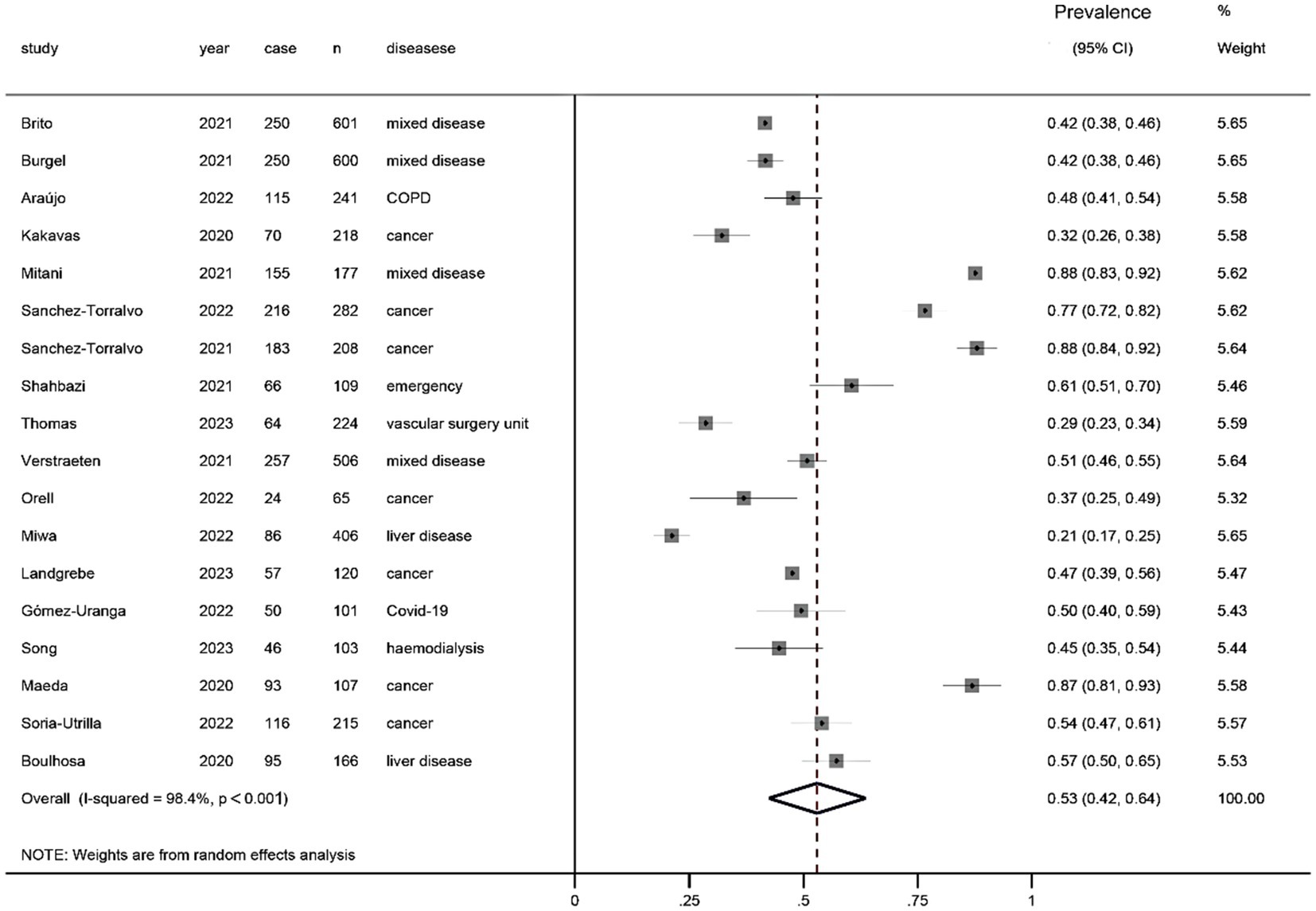
Figure 4. Prevalence of malnutrition diagnosed directly using the GLIM criteria without a nutritional risk screening (one-step approach).
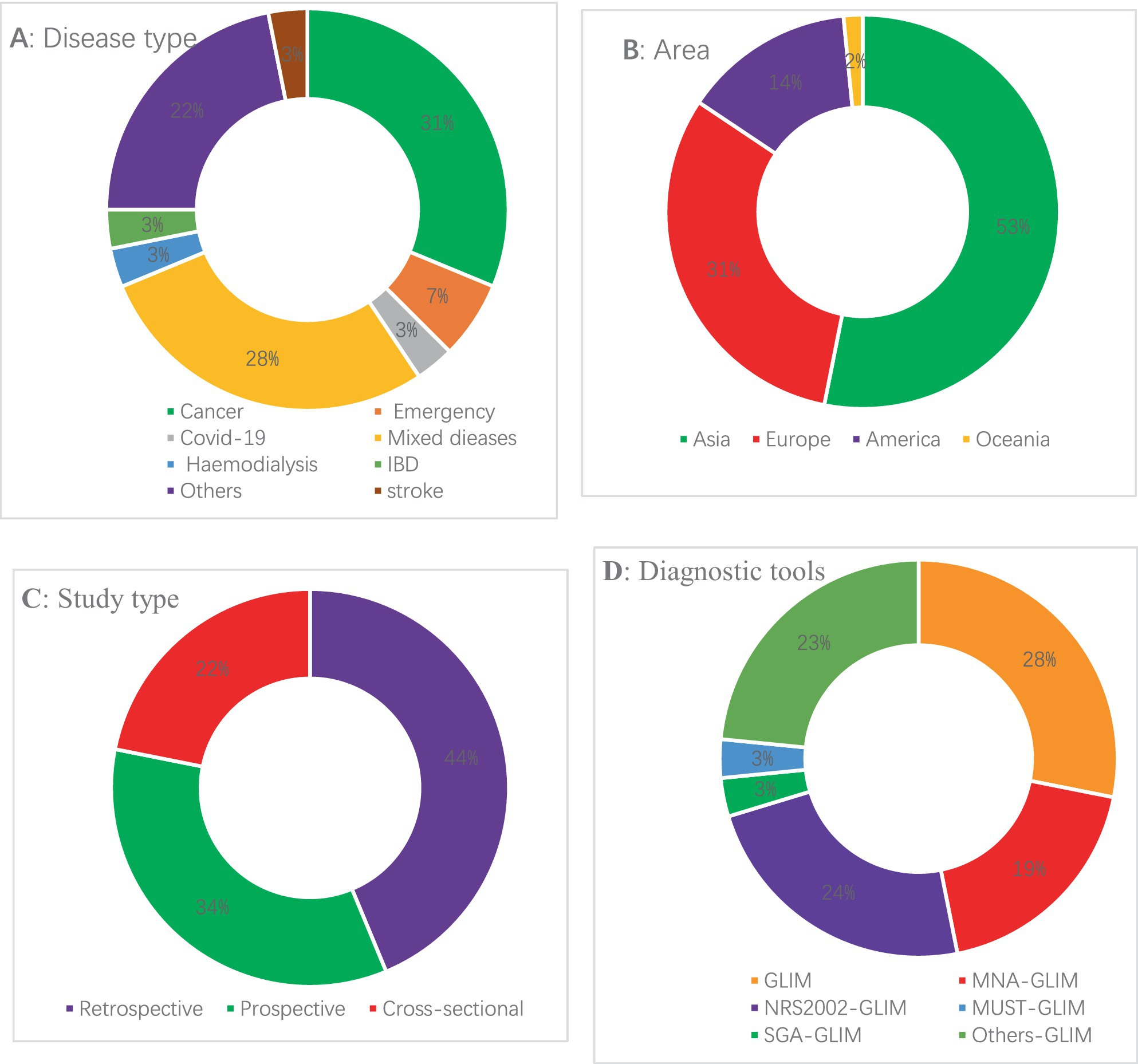
Figure 5. Baseline characteristics of the studies in the meta-analysis (see Supplementary Table S1 for details).
Figure 6 shows the mortality risk of malnourished patients diagnosed based on the GLIM criteria within 1 year (HR, 2.62; 95% CI, 1.95–3.52; I2 = 77.1%). Figure 7 shows the mortality risk of malnourished patients diagnosed based on the GLIM criteria beyond 1 year (HR, 2.04; 95% CI, 1.70–2.45; I2 = 59.9%).
The rates of malnutrition according to different screening tools cannot be compared equally as different tools were used in different cohorts. We simply report the malnutrition risk across cohorts, in each of which a different screening tool was used. As shown in Table 1, the prevalence of malnutrition obtained by the GLIM criteria after a nutritional risk screening was quite different; the prevalence of malnutrition diagnosed by the NRS2002 GLIM tool was 35% (95% CI, 29%–40%); however, the prevalence of malnutrition diagnosed by the MNA GLIM tool was 48% (95% CI, 35%–62%). The prevalence of malnutrition varied little by region. Among the disease types, the prevalence of malnutrition in cancer patients was 44% (95% CI, 36%–52%), while that in acute and critically ill patients was 44% (95% CI, 33%–56%). The prevalence in patients in internal medicine wards was 40% (95% CI, 34%–45%), while that in patients in surgical wards was 47% (95% CI, 30%–64%).
We diagnosed malnutrition as a complete diagnosis based on the GLIM criteria and excluded relevant studies without a complete diagnosis. In fact, the results show that the current diagnosis of malnutrition based on the GLIM criteria is confusing and that most studies do not report a complete diagnosis. Usually, according to the GLIM diagnostic criteria, the diagnosis of malnutrition first requires a nutritional risk screening, followed by a diagnosis according to the GLIM criteria (two-step approach) (3); however, some studies directly used the GLIM criteria to diagnose malnutrition (one-step approach). The prevalence of malnutrition diagnosed by the one-step approach was 53%, while that diagnosed by the two-step approach was 39%. The rate of a positive diagnosis by the one-step approach is higher than that by the two-step approach, possibly because the two-step approach considers not only the symptoms of malnutrition but also the adverse clinical outcomes of nutritional risk (72, 73). Due to the uncertainty of the phenotypical and aetiological components of the GLIM criteria, such as BMI, the criteria for elderly and young individuals are different, and differences may exist among different races (74). In addition, individual studies have used different nutritional risk screening tools and then used the GLIM criteria to obtain different prevalence rates of malnutrition. However, since the tools were not used in the same cohort, it is not yet possible to judge which screening tool is more efficient. For the diagnosis of malnutrition based on the GLIM criteria, a nutritional risk screening is performed first, and different screening tools have been used in different cohorts. The MUST is applicable to all adults but is recommended to be used in community settings (75); the MNA is more suitable for elderly populations (≥65 years old) (76); the NRS2002 tool is applicable to adults aged 18 to 90 years, but its main role is to identify patients with nutritional risk, not to assess the existing nutritional status (77). We pooled the prevalence of malnutrition across the cohorts, and the results showed that the prevalence of malnutrition diagnosed using the MNA GLIM tool was higher than that diagnosed by the NRS2002 GLIM tool, which is consistent with the related research results reported by Xu et al. (17). One reason may be that the MNA GLIM tool is mostly used in elderly patients, and the prevalence of malnutrition due to long-term chronic underlying diseases is high (76). However, the prevalence of malnutrition based on region showed little variation. It is speculated that this result may be due to the body fat content and corresponding BMI cut-off values being higher in European regions than in Asian regions (74, 75). In addition, we analysed the prevalence of malnutrition by disease type, including oncology, emergency, internal medicine, surgery, and COVID-19, and the results showed that the prevalence of malnutrition in surgical wards was slightly higher than that in internal medicine wards. There was also a small difference in the prevalence of malnutrition between oncology and emergency patients, but this analysis was simply based on an aggregation of different cohorts, and the results may be biased.
Involuntary weight loss, which is the most definitive diagnostic indicator of malnutrition, topped the GLIM framers vote. BMI is also a relatively clear quantitative index, and it is easy to obtain and convenient to apply. However, when the GLIM criteria were released, it was also pointed out that there are substantial regional differences in using BMI as a diagnostic standard for malnutrition (3). Reduced body mass index and body composition analysis can objectively and accurately measure body composition. The common methods are the dual energy X-ray absorptiometry method (DEXA) and bioelectrical impedance method. The DXA method mainly uses detectors to detect the absorption of X-rays by the tested parts, thereby calculating body fat composition, non-body fat composition and bone mineral content. These two methods are involved in the literature included in this study. In addition, some studies also use calf circumference for simplified measurement of muscle mass (6, 17). In the burden of disease/inflammation, albumin/prealbumin is one of the commonly used indicators to evaluate liver function, but it is often affected by exogenous infusion, so it cannot accurately evaluate nutritional status, and serum C-reactive protein (CRP) can be compared with good for assessing inflammatory status. Notably, some studies have compared the prevalence of malnutrition between GLIM and ESPEN, and the GLIM criteria have a higher detection rate of malnutrition than the ESPEN criteria (5, 34, 57), possibly because the GLIM criteria add aetiological diagnosis items (3).
In the relevant studies included in this paper, malnourished patients diagnosed according to GLIM criteria may have reported discharge or five-year mortality risk, and we extracted pooled effect values directly from the original papers and pooled them. In addition, in the relevant studies included in this article, most of the mortality rates of malnourished patients diagnosed based on the GLIM criteria were reported using the HR, but a few studies used the odds ratio (OR) to indicate the effect size. Considering that the HR includes the time factor, we partially replaced the ORs reported in the studies with HRs, which may have caused minor bias.
It has been reported that malnutrition diagnosed by the GLIM criteria is significantly associated with a poor prognosis (6, 15, 78); it will not only increase the complications of patients (79) and prolong the length of hospital stay (80) but also increase the mortality rate (73). Our results also showed that malnutrition based on the GLIM criteria was associated with significantly increased mortality within and beyond 1 year, but there was large heterogeneity, which may be due to the use of different screening tools in different patient populations (81). However, although the pooled heterogeneity was large, the pooled effect size was significant. Therefore, the diagnosis of malnutrition by the GLIM criteria can better predict the mortality risk of patients and requires timely nutritional support to improve long-term survival (3). In conclusion, our preliminary findings validate the ability of the “minimum criteria” (at least one phenotypical and one aetiological criterion) for the diagnosis of malnutrition using the GLIM criteria to predict adverse clinical outcomes.
The results of this systematic review and mate-analysis need to be interpreted with caution. First, the GLIM criteria were mainly studied based on a complete diagnosis; although the included articles had clear phenotypical and aetiological criteria, the results may have been biased due to differences in the assessment of BMI and muscle mass loss among studies. Second, regarding the assessment of mortality, most studies reported mortality data using the HR, while a few articles used the OR. We used the HR to indicate the pooled effect size for the articles, which may introduced a small bias. Finally, most articles were from Asia, and these conclusions may not apply to other geographic regions and populations.
The prevalence of malnutrition diagnosed by the GLIM criteria after a nutritional risk screening was significantly lower than the prevalence of malnutrition diagnosed directly by the GLIM criteria. In addition, the risk of mortality was significantly higher in malnourished patients assessed by the GLIM criteria. In the future, it is necessary to explore the effectiveness of the combination of different nutritional screening tools and the GLIM criteria for the nutritional diagnosis of relevant groups in a large cohort.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
WB and PZ contributed to the conception and design of the work. WB, YW, YiL, YuL, and HJ collected information and analyzed data used in the systematic review and meta-analysis. LD polished this article. PZ and HJ substantively revised it. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1174945/full#supplementary-material
1. Schuetz, P, Seres, D, Lobo, DN, Gomes, F, Kaegi-Braun, N, and Stanga, Z. Management of disease-related malnutrition for patients being treated in hospital. Lancet. (2021) 398:1927–38. doi: 10.1016/S0140-6736(21)01451-3
2. Huo, Z, Chong, F, Yin, L, Lu, Z, Liu, J, and Xu, H. Accuracy of the GLIM criteria for diagnosing malnutrition: a systematic review and meta-analysis. Clin Nutr. (2022) 41:1208–17. doi: 10.1016/j.clnu.2022.04.005
3. Cederholm, T, Jensen, GL, Correia, MITD, Gonzalez, MC, Fukushima, R, Higashiguchi, T, et al. GLIM criteria for the diagnosis of malnutrition—a consensus report from the global clinical nutrition community. Clin Nutr. (2019) 38:1–9. doi: 10.1016/j.clnu.2018.08.002
4. Orell, HK, Pohju, AK, Osterlund, P, Schwab, US, Ravasco, P, and Mäkitie, A. GLIM in diagnosing malnutrition and predicting outcome in ambulatory patients with head and neck cancer. Front Nutr. (2022) 9:1030619. doi: 10.3389/fnut.2022.1030619
5. Yin, L, Cheng, N, Chen, P, Zhang, M, Li, N, Lin, X, et al. Association of Malnutrition, as defined by the PG-SGA, ESPEN 2015, and GLIM criteria, with complications in esophageal cancer patients after esophagectomy. Front Nutr. (2021) 8:632546. doi: 10.3389/fnut.2021.632546
6. Zhang, X, Tang, M, Zhang, Q, Zhang, K-P, Guo, Z-Q, Xu, H-X, et al. The GLIM criteria as an effective tool for nutrition assessment and survival prediction in older adult cancer patients. Clin Nutr. (2021) 40:1224–32. doi: 10.1016/j.clnu.2020.08.004
7. Kiss, N, and Steer, B, de van der Schueren M, Loeliger, J, Alizadehsani, R, Edbrooke, L, Deftereos, I, Laing, E, and Khosravi, A. Comparison of the prevalence of 21 GLIM phenotypic and etiologic criteria combinations and association with 30-day outcomes in people with cancer: a retrospective observational study. Clin Nutr (2022) 41: 1102–1111. doi: 10.1016/j.clnu.2022.03.024
8. Kaźmierczak-Siedlecka, K, Skonieczna-Żydecka, K, Folwarski, M, Ruszkowski, J, Świerblewski, M, and Makarewicz, W. Influence of malnutrition stage according to GLIM 2019 criteria and SGA on the quality of life of patients with advanced cancer. Nutr Hosp. (2020) 37:1179–85. doi: 10.20960/nh.03185
9. Page, MJ, Moher, D, Bossuyt, PM, Boutron, I, Hoffmann, TC, Mulrow, CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. (2020) 2021:n160. doi: 10.1136/bmj.n160
10. Shimizu, A, Fujishima, I, Maeda, K, Murotani, K, Ohno, T, Nomoto, A, et al. Association between food texture levels consumed and the prevalence of malnutrition and sarcopenia in older patients after stroke. Eur J Clin Nutr. (2022) 76:1576–82. doi: 10.1038/s41430-022-01126-1
11. Shimizu, A, Maeda, K, Honda, T, Ishida, Y, Ueshima, J, Nagami, S, et al. Comparison between the global leadership initiative on malnutrition and the European Society for Clinical Nutrition and Metabolism definitions for the prevalence of malnutrition in geriatric rehabilitation care. Geriatr Gerontol Int. (2020) 20:1221–7. doi: 10.1111/ggi.14072
12. Shimizu, A, Maeda, K, Koyanagi, Y, Kayashita, J, Fujishima, I, and Mori, N. The global leadership initiative on malnutrition-defined malnutrition predicts prognosis in persons with stroke-related dysphagia. J Am Med Dir Assoc. (2019) 20:1628–33. doi: 10.1016/j.jamda.2019.07.008
13. Huang, S, Niu, Y, Liu, X, Gu, Z, Huang, A, and Wu, J. Characteristics of malnutrition according to global leadership initiative on malnutrition criteria in non-surgical patients with inflammatory bowel disease. Nutrition. (2022) 94:111514. doi: 10.1016/j.nut.2021.111514
14. Huang, Y, Chen, Y, Wei, L, Hu, Y, and Huang, L. Comparison of three malnutrition risk screening tools in identifying malnutrition according to global leadership initiative on malnutrition criteria in gastrointestinal cancer. Front Nutr. (2022) 9:959038. doi: 10.3389/fnut.2022.959038
15. Kootaka, Y, Kamiya, K, Hamazaki, N, Nozaki, K, Ichikawa, T, Nakamura, T, et al. The GLIM criteria for defining malnutrition can predict physical function and prognosis in patients with cardiovascular disease. Clin Nutr. (2021) 40:146–52. doi: 10.1016/j.clnu.2020.04.038
16. Li, Q, Zhang, X, Tang, M, Song, M, Zhang, Q, Zhang, K, et al. Different muscle mass indices of the global leadership initiative on malnutrition in diagnosing malnutrition and predicting survival of patients with gastric cancer. Nutrition. (2021) 89:111286. doi: 10.1016/j.nut.2021.111286
17. Xu, J-Y, Zhu, M-W, Zhang, H, Li, L, Tang, P-X, Chen, W, et al. A cross-sectional study of GLIM-defined malnutrition based on new validated calf circumference cut-off values and different screening tools in hospitalised patients over 70 years old. J Nutr Health Aging. (2020) 24:832–8. doi: 10.1007/s12603-020-1386-4
18. Xu, L, Shi, M, Huang, Z, Zhang, W, Zhang, H, Shen, X, et al. Impact of malnutrition diagnosed using global leadership initiative on malnutrition criteria on clinical outcomes of patients with gastric cancer. J Parenter Enter Nutr. (2022) 46:385–94. doi: 10.1002/jpen.2127
19. Matsumoto, Y, Iwai, K, Namikawa, N, Matsuda, S, Wakano, C, Heya, H, et al. The relationship between existing nutritional indicators and global leadership initiative on malnutrition (GLIM) criteria: a one-institution cross-sectional analysis. Clin Nutr. (2020) 39:3099–104. doi: 10.1016/j.clnu.2020.01.016
20. Mitani, A, Iwai, T, Shichinohe, T, Takeda, H, Kumagai, S, Nishida, M, et al. The combined usage of the global leadership initiative on malnutrition criteria and controlling nutrition status score in acute care hospitals. Ann Nutr Metab. (2021) 77:178–84. doi: 10.1159/000516994
21. Nozoe, M, Yamamoto, M, Masuya, R, Inoue, T, Kubo, H, and Shimada, S. Prevalence of malnutrition diagnosed with GLIM criteria and association with activities of daily living in patients with acute stroke. J Stroke Cerebrovasc Dis. (2021) 30:105989. doi: 10.1016/j.jstrokecerebrovasdis.2021.105989
22. Shahbazi, S, Hajimohammadebrahim-Ketabforoush, M, Vahdat Shariatpanahi, M, Shahbazi, E, and Vahdat, SZ. The validity of the global leadership initiative on malnutrition criteria for diagnosing malnutrition in critically ill patients with COVID-19: a prospective cohort study. Clin Nutr. (2021) 43:377–82. doi: 10.1016/j.clnesp.2021.03.020
23. Tan, S, Wang, J, Zhou, F, Tang, M, Xu, J, Zhang, Y, et al. Validation of GLIM malnutrition criteria in cancer patients undergoing major abdominal surgery: a large-scale prospective study. Clin Nutr. (2022) 41:599–609. doi: 10.1016/j.clnu.2022.01.010
24. Wang, Y, Jiang, H, Zhu, M, Deng, H, Wang, L, Wang, X, et al. Establishing a new body mass index cutoff value for malnutrition diagnosis using the global leadership initiative on malnutrition (GLIM) tool in Chinese older adults. J Parenter Enter Nutr. (2022) 46:1071–9. doi: 10.1002/jpen.2296
25. Wang, P, Chen, X, Liu, Q, Liu, X, and Li, Y. Good performance of the global leadership initiative on malnutrition criteria for diagnosing and classifying malnutrition in people with esophageal cancer undergoing esophagectomy. Nutrition. (2021) 91–92:111420. doi: 10.1016/j.nut.2021.111420
26. Yin, L, Lin, X, Li, N, Zhang, M, He, X, Liu, J, et al. Evaluation of the global leadership initiative on malnutrition criteria using different muscle mass indices for diagnosing malnutrition and predicting survival in lung cancer patients. J Parenter Enter Nutr. (2021) 45:607–17. doi: 10.1002/jpen.1873
27. Yin, L, Lin, X, Liu, J, Li, N, He, X, Zhang, M, et al. Classification tree-based machine learning to visualize and validate a decision tool for identifying malnutrition in cancer patients. J Parenter Enter Nutr. (2021) 45:1736–48. doi: 10.1002/jpen.2070
28. Yu, Y, Ye, J, Chen, M, Jiang, C, Lin, W, Lu, Y, et al. Malnutrition prolongs the hospitalization of patients with COVID-19 infection: a clinical epidemiological analysis. J Nutr Health Aging. (2021) 25:369–73. doi: 10.1007/s12603-020-1541-y
29. Zhang, Z, Wan, Z, Zhu, Y, Zhang, L, Zhang, L, and Wan, H. Prevalence of malnutrition comparing NRS 2002, MUST, and PG-SGA with the GLIM criteria in adults with cancer: a multi-center study. Nutrition. (2021) 83:111072. doi: 10.1016/j.nut.2020.111072
30. Zhang, Y, Jiang, L, Su, P, Yu, T, Ma, Z, Kang, W, et al. Visceral adipose tissue assessment enhances the prognostic value of GLIM criteria in patients with gastric cancer undergoing radical gastrectomy after neoadjuvant treatment. Nutrients. (2022) 14:5047. doi: 10.3390/nu14235047
31. Ji, T, Li, Y, Liu, P, Zhang, Y, Song, Y, and Ma, L. Validation of GLIM criteria on malnutrition in older Chinese inpatients. Front Nutr. (2022) 9:969666. doi: 10.3389/fnut.2022.969666
32. Zou, Y, Xu, H, Lyu, Q, Weng, M, Cui, J, Shi, H, et al. Malnutrition diagnosed by GLIM criteria better predicts long-term outcomes for patients with non-Hodgkin’s lymphoma: a prospective multicenter cohort study. Hematol Oncol. (2022):hon.3107. doi: 10.1002/hon.3107
33. Zhou, X, Liu, J, Zhang, Q, Rao, S, Wu, X, Zhang, J, et al. Comparison of the suitability between NRS2002 and MUST as the first-step screening tool for GLIM criteria in hospitalized patients with GIST. Front Nutr. (2022) 9:864024. doi: 10.3389/fnut.2022.864024
34. Ren, S-S, Zhu, M-W, Zhang, K-W, Chen, B-W, Yang, C, Xiao, R, et al. Machine learning-based prediction of in-hospital complications in elderly patients using GLIM-, SGA-, and ESPEN 2015-diagnosed malnutrition as a factor. Nutrients. (2022) 14:3035. doi: 10.3390/nu14153035
35. Song, H-N, Wang, W-B, Luo, X, Huang, D-D, Ruan, X-J, Xing, C-G, et al. Effect of GLIM-defined malnutrition on postoperative clinical outcomes in patients with colorectal cancer. Jpn J Clin Oncol. (2022) 52:466–74. doi: 10.1093/jjco/hyab215
36. Song, HC, Shin, J, Hwang, JH, and Kim, SH. Utility of the global leadership initiative on malnutrition criteria for the nutritional assessment of patients with end-stage renal disease receiving chronic hemodialysis. J Human Nutr Diet. (2023) 36:97–107. doi: 10.1111/jhn.13019
37. Kobayashi, H, Inoue, T, Ogawa, M, Abe, T, Tanaka, T, and Kakiuchi, M. Malnutrition diagnosed by the global leadership initiative on malnutrition criteria as a predictor of gait ability in patients with hip fracture. Injury. (2022) 53:3394–400. doi: 10.1016/j.injury.2022.08.004
38. Miwa, T, Hanai, T, Nishimura, K, Unome, S, Maeda, T, Ogiso, Y, et al. Usefulness of the global leadership initiative on malnutrition criteria to predict sarcopenia and mortality in patients with chronic liver disease. Hepatol Res. (2022) 52:928–36. doi: 10.1111/hepr.13816
39. Liu, Z, Shen, Z, Zang, W, Zhou, J, Yu, Z, Zhang, P, et al. Development and validation of global leadership initiative on malnutrition for prognostic prediction in patients who underwent cardiac surgery. Nutrients. (2022) 14:2409. doi: 10.3390/nu14122409
40. Xie, L, Jiang, J, Fu, H, Zhang, W, Yang, L, and Yang, M. Malnutrition in relation to muscle mass, muscle quality, and muscle strength in hospitalized older adults. J Am Med Dir Assoc. (2022) 23:722–8. doi: 10.1016/j.jamda.2021.11.025
41. Hiraike, T, Momoki, C, and Habu, D. Comparison of the adequacy of geriatric nutritional risk index with that of the mini nutritional assessment-short form and global leadership initiative on malnutrition criteria in assessing nutritional status to predict the 1-year prognosis of hospitalized Japanese older adults: a single-institutional cohort study. BMC Geriatr. (2023) 23:35. doi: 10.1186/s12877-023-03740-5
42. Yang, W, Guo, G, Cui, B, Li, Y, Sun, M, Li, C, et al. Malnutrition according to the global leadership initiative on malnutrition criteria is associated with in-hospital mortality and prolonged length of stay in patients with cirrhosis. Nutrition. (2023) 105:111860. doi: 10.1016/j.nut.2022.111860
43. Allepaerts, S, Buckinx, F, Bruyère, O, Reginster, JY, Paquot, N, and Gillain, S. Clinical impact of nutritional status and energy balance in elderly hospitalized patients. J Nutr Health Aging. (2020) 24:1073–9. doi: 10.1007/s12603-020-1527-9
44. Balci, C, Bolayir, B, Eşme, M, Arik, G, Kuyumcu, ME, Yeşil, Y, et al. Comparison of the efficacy of the global leadership initiative on malnutrition criteria, subjective global assessment, and nutrition risk screening 2002 in diagnosing malnutrition and predicting 5-year mortality in patients hospitalized for acute illnesses. J Parenter Enter Nutr. (2021) 45:1172–80. doi: 10.1002/jpen.2016
45. Bellanti, F, Lo Buglio, A, Quiete, S, Pellegrino, G, Dobrakowski, M, Kasperczyk, A, et al. Comparison of three nutritional screening tools with the new GLIM criteria for malnutrition and association with sarcopenia in hospitalized older patients. JCM. (2020) 9:1898. doi: 10.3390/jcm9061898
46. Ijmker-Hemink, V, Heerschop, S, Wanten, G, and van den Berg, M. Evaluation of the validity and feasibility of the GLIM criteria compared with PG-SGA to diagnose malnutrition in relation to one-year mortality in hospitalized patients. J Acad Nutr Diet. (2022) 122:595–601. doi: 10.1016/j.jand.2021.07.011
47. Kakavas, S, Karayiannis, D, Bouloubasi, Z, Poulia, KA, Kompogiorgas, S, Konstantinou, D, et al. Global leadership initiative on malnutrition criteria predict pulmonary complications and 90-day mortality after major abdominal surgery in cancer patients. Nutrients. (2020) 12:3726. doi: 10.3390/nu12123726
48. Lauwers, P, Hendriks, JMH, Van Bouwel, S, Verrijken, A, Van Dessel, K, Van Gils, C, et al. Malnutrition according to the 2018 GLIM criteria is highly prevalent in people with a diabetic foot ulcer but does not affect outcome. Clin Nutr. (2021) 43:335–41. doi: 10.1016/j.clnesp.2021.03.029
49. Ohta, M, Imamura, Y, Chebib, N, Schulte-Eickhoff, RM, Allain, S, Genton, L, et al. Oral function and nutritional status in non-acute hospitalised elders. Gerodontology. (2022) 39:74–82. doi: 10.1111/ger.12612
50. Sánchez-Torralvo, FJ, Ruiz-García, I, Contreras-Bolívar, V, González-Almendros, I, Ruiz-Vico, M, Abuín-Fernández, J, et al. CT-determined sarcopenia in GLIM-defined malnutrition and prediction of 6-month mortality in cancer inpatients. Nutrients. (2021) 13:2647. doi: 10.3390/nu13082647
51. Sánchez-Torralvo, FJ, Contreras-Bolívar, V, Ruiz-Vico, M, Abuín-Fernández, J, González-Almendros, I, Barrios, M, et al. Relationship between malnutrition and the presence of symptoms of anxiety and depression in hospitalized cancer patients. Support Care Cancer. (2022) 30:1607–13. doi: 10.1007/s00520-021-06532-y
52. Sanz-París, A, Martín-Palmero, A, Gomez-Candela, C, García-Almeida, JM, Burgos-Pelaez, R, Sanz-Arque, A, et al. GLIM criteria at hospital admission predict 8-year all-cause mortality in elderly patients with type 2 diabetes mellitus: results from VIDA study. J Parenter Enter Nutr. (2020) 44:1492–500. doi: 10.1002/jpen.1781
53. Verstraeten, LMG, van Wijngaarden, JP, Pacifico, J, Reijnierse, EM, Meskers, CGM, and Maier, AB. Association between malnutrition and stages of sarcopenia in geriatric rehabilitation inpatients: RESORT. Clin Nutr. (2021) 40:4090–6. doi: 10.1016/j.clnu.2021.02.007
54. Yilmaz, M, Atilla, FD, Sahin, F, and Saydam, G. The effect of malnutrition on mortality in hospitalized patients with hematologic malignancy. Support Care Cancer. (2020) 28:1441–8. doi: 10.1007/s00520-019-04952-5
55. Trollebø, MA, Skeie, E, Revheim, I, Stangeland, H, Erstein, M-AH, Grønning, MK, et al. Comparison of nutritional risk screening with NRS2002 and the GLIM diagnostic criteria for malnutrition in hospitalized patients. Sci Rep. (2022) 12:19743. doi: 10.1038/s41598-022-23878-3
56. Landgrebe, M, Tobberup, R, Carus, A, and Rasmussen, HH. GLIM diagnosed malnutrition predicts clinical outcomes and quality of life in patients with non-small cell lung cancer. Clin Nutr. (2023) 42:190–8. doi: 10.1016/j.clnu.2022.12.011
57. Bannert, K, Sautter, LF, Wiese, ML, Meyer, F, Ehlers, L, Fromhold-Treu, S, et al. Analysis of ESPEN and GLIM algorithms reveals specific drivers for the diagnosis of malnutrition in patients with chronic gastrointestinal diseases. Nutrition. (2023) 106:111887. doi: 10.1016/j.nut.2022.111887
58. Gómez-Uranga, A, Guzmán-Martínez, J, Esteve-Atiénzar, PJ, Wikman-Jorgensen, P, Núñez-Cruz, JM, Espinosa-del-Barrio, L, et al. Nutritional and functional impact of acute SARS-CoV-2 infection in hospitalized patients. J Clin Med. (2022) 11:2424. doi: 10.3390/jcm11092424
59. Maeda, K, Ishida, Y, Nonogaki, T, and Mori, N. Reference body mass index values and the prevalence of malnutrition according to the global leadership initiative on malnutrition criteria. Clin Nutr. (2020) 39:180–4. doi: 10.1016/j.clnu.2019.01.011
60. Soria-Utrilla, V, Sánchez-Torralvo, FJ, González-Poveda, I, Mera-Velasco, S, Porras, N, Toval-Mata, JA, et al. Prevalence of anxiety and depression symptoms and their relationship with nutritional status and mortality in patients with colorectal cancer. Int J Environ Res Public Health. (2022) 19:13548. doi: 10.3390/ijerph192013548
61. Avesani, CM, Sabatino, A, Guerra, A, Rodrigues, J, Carrero, JJ, Rossi, GM, et al. A comparative analysis of nutritional assessment using global leadership initiative on malnutrition versus subjective global assessment and malnutrition inflammation score in maintenance hemodialysis patients. J Ren Nutr. (2022) 32:476–82. doi: 10.1053/j.jrn.2021.06.008
62. Boulhosa, RSSB, Lourenço, RP, Côrtes, DM, Oliveira, LPM, Lyra, AC, and Jesus, RP. Comparison between criteria for diagnosing malnutrition in patients with advanced chronic liver disease: GLIM group proposal versus different nutritional screening tools. J Hum Nutr Diet. (2020) 33:862–8. doi: 10.1111/jhn.12759
63. Brito, JE, Burgel, CF, Lima, J, Chites, VS, Saragiotto, CB, Rabito, EI, et al. GLIM criteria for malnutrition diagnosis of hospitalized patients presents satisfactory criterion validity: a prospective cohort study. Clin Nutr. (2021) 40:4366–72. doi: 10.1016/j.clnu.2021.01.009
64. Burgel, CF, da Eckert, IC, Brito, JE, Rodrigues, FW, and Silva, FM. Accuracy of three tools for malnutrition diagnosis in hospitalised patients: comparison to subjective global assessment. J Human Nutr Diet. (2021) 34:935–44. doi: 10.1111/jhn.12907
65. Cruz, PLM, BLM, S, da Silva, JE, Lima, E, and Silva, RR. Clinical and nutritional predictors of hospital readmission within 30 days. Eur J Clin Nutr. (2022) 76:244–50. doi: 10.1038/s41430-021-00937-y
66. de Araújo, BE, Kowalski, V, Leites, GM, da Silva, FJ, and Silva, FM. AND-ASPEN and ESPEN consensus, and GLIM criteria for malnutrition identification in AECOPD patients: a longitudinal study comparing concurrent and predictive validity. Eur J Clin Nutr. (2022) 76:685–92. doi: 10.1038/s41430-021-01025-x
67. Galindo Martín, CA, Aportela Vázquez, VA, Becerril Hernández, F, Aguilar Medina, CR, Ayala Carrillo, SL, Chávez Flores, A, et al. The GLIM criteria for adult malnutrition and its relation with adverse outcomes, a prospective observational study. Clin Nutr. (2020) 38:67–73. doi: 10.1016/j.clnesp.2020.06.015
68. Muñoz Fernandez, SS, Garcez, FB, de Alencar, JCG, Cederholm, T, Aprahamian, I, Morley, JE, et al. Applicability of the GLIM criteria for the diagnosis of malnutrition in older adults in the emergency ward: a pilot validation study. Clin Nutr. (2021) 40:5447–56. doi: 10.1016/j.clnu.2021.09.024
69. da Silva, CA, Gonzalez, MC, Martucci, RB, Feijó, PM, Rodrigues, VD, de Pinho, NB, et al. Predictive validity of GLIM malnutrition diagnosis in patients with colorectal cancer. JPEN J Parenter Enteral Nutr. (2023) 47:420, jpen. 2475–8. doi: 10.1002/jpen.2475
70. da Silva E Sousa, FI, Medeiros, LT, RAM, B, AFCS, D, and CSC, M. Power of mortality prediction in patients awaiting liver transplantation according to the global leadership initiative on malnutrition criteria and subjective global assessment and Royal Free Hospital Global Assessment scores. Nutrition. (2023) 106:111889. doi: 10.1016/j.nut.2022.111889
71. Thomas, J, Delaney, C, and Miller, M. The ability of the global leadership initiative on malnutrition (GLIM) to diagnose protein–energy malnutrition in patients requiring vascular surgery: a validation study. Br J Nutr. (2023) 129:49–53. doi: 10.1017/S0007114522000344
72. Brown, D, Loeliger, J, Stewart, J, Graham, KL, Goradia, S, Gerges, C, et al. Relationship between global leadership initiative on malnutrition (GLIM) defined malnutrition and survival, length of stay and post-operative complications in people with cancer: a systematic review. Clin Nutr. (2023) 42:255–68. doi: 10.1016/j.clnu.2023.01.012
73. Matsui, R, Rifu, K, Watanabe, J, Inaki, N, and Fukunaga, T. Current status of the association between malnutrition defined by the GLIM criteria and postoperative outcomes in gastrointestinal surgery for cancer: a narrative review. J Cancer Res Clin Oncol. (2023) 149:1635–43. doi: 10.1007/s00432-022-04175-y
74. Banitt, AA, Kaur, H, Pulvers, KM, Nollen, NL, Ireland, M, and Fitzgibbon, ML. BMI percentiles and body image discrepancy in black and white adolescents. Obesity. (2008) 16:987–91. doi: 10.1038/oby.2008.21
75. Jobim Milanez, DS, Razzera, EL, da Silveira Knobloch, I, Lima, J, Bernardes, S, and Silva, FM. A scoping review on the GLIM criteria for malnutrition diagnosis: understanding how and for which purpose it has been applied in studies on hospital settings. Clin Nutr. (2023) 42:29–44. doi: 10.1016/j.clnu.2022.10.022
76. Dent, E, Hoogendijk, EO, Visvanathan, R, and Wright, ORL. Malnutrition screening and assessment in hospitalised older people: a review. J Nutr Health Aging. (2019) 23:431–41. doi: 10.1007/s12603-019-1176-z
77. Kondrup, J . Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. (2003) 22:321–36. doi: 10.1016/S0261-5614(02)00214-5
78. Oguri, M, Ishii, H, Yasuda, K, Sumi, T, Takahashi, H, and Murohara, T. Combined prognostic value of malnutrition using GLIM criteria and renal insufficiency in elderly heart failure. ESC Heart Fail. (2022) 9:704–11. doi: 10.1002/ehf2.13685
79. Hirose, S, Matsue, Y, Kamiya, K, Kagiyama, N, Hiki, M, Dotare, T, et al. Prevalence and prognostic implications of malnutrition as defined by GLIM criteria in elderly patients with heart failure. Clin Nutr. (2021) 40:4334–40. doi: 10.1016/j.clnu.2021.01.014
80. Ruiz, AJ, Buitrago, G, Rodríguez, N, Gómez, G, Sulo, S, Gómez, C, et al. Clinical and economic outcomes associated with malnutrition in hospitalized patients. Clin Nutr. (2019) 38:1310–6. doi: 10.1016/j.clnu.2018.05.016
Keywords: malnutrition, GLIM criteria, nutritional risk, systematic review, meta-analysis
Citation: Bian W, Li Y, Wang Y, Chang L, Deng L, Li Y, Jiang H and Zhou P (2023) Prevalence of malnutrition based on global leadership initiative in malnutrition criteria for completeness of diagnosis and future risk of malnutrition based on current malnutrition diagnosis: systematic review and meta-analysis. Front. Nutr. 10:1174945. doi: 10.3389/fnut.2023.1174945
Received: 27 February 2023; Accepted: 19 June 2023;
Published: 04 July 2023.
Edited by:
Kohei Yamaguchi, Tokyo Medical and Dental University, JapanReviewed by:
Sarah Damanti, Vita-Salute San Raffaele University, ItalyCopyright © 2023 Bian, Li, Wang, Chang, Deng, Li, Jiang and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hua Jiang, amlhbmdodWFAdWVzdGMuZWR1LmNu; Ping Zhou, enBfMzE5QDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.