- 1Generating Research Insights for Development (GRID) Council, Executive Office, Noida, Uttar Pradesh, India
- 2Department of Neonatology, Atal Bihari Vajpayee Institute of Medical Sciences and Dr. Ram Manohar Lohia Hospital, New Delhi, India
Background: Breastfeeding practices in institutional settings got disrupted during the COVID-19 pandemic. We reviewed the challenges faced and the “work-around” solutions identified for implementing recommended breastfeeding practices in institutionalized mother-newborn dyads in resource constrained settings during the pandemic with the aim to identify learnings that could be potentially adapted to the Indian and relatable contexts, for building resilient health systems.
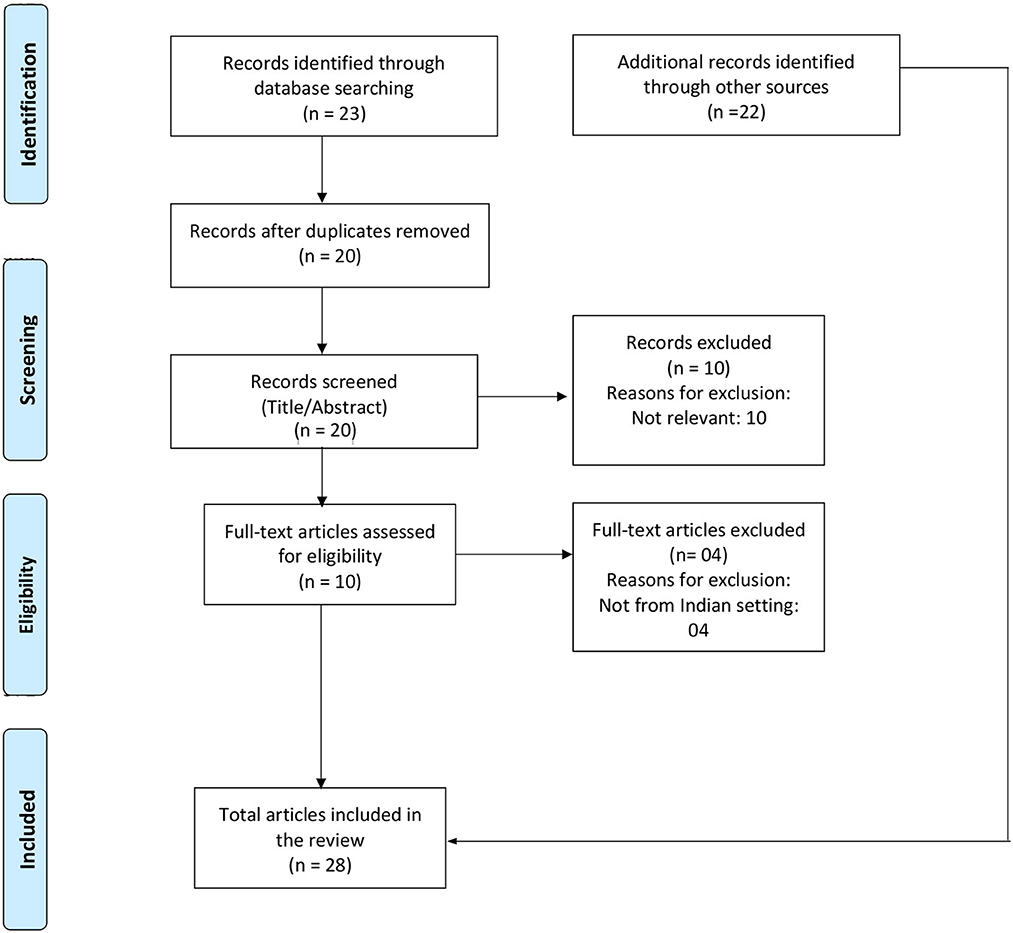
Methods: We conducted a scoping review of literature using the PRISMA ScR Extension guidelines. We searched the Medline via PubMed and Web of Science databases for literature published between 1st December 2019 and 15th April 2022. We included original research, reviews, and policy recommendations published in English language and on India while others were excluded. Further, we searched for relevant gray literature on Google (free word search), websites of government and major professional bodies in India. Three reviewers independently conducted screening and data extraction and the results were displayed in tabular form. Challenges and potential solutions for breastfeeding were identified and were categorized under one or more suitable headings based on the WHO building blocks for health systems.
Results: We extracted data from 28 papers that were deemed eligible. Challenges were identified across all the six building blocks. Lack of standard guidelines for crisis management, separation of the newborn from the mother immediately after birth, inadequate logistics and resources for infection prevention and control, limited health workforce, extensive use of formula and alternative foods, inconsistent quality of care and breastfeeding support, poor awareness among beneficiaries about breastfeeding practices (and especially, about its safety during the pandemic) were some of the challenges identified. The solutions primarily focused on the development of standard guidelines and operating procedures, restricted use of formula, use of telemedicine services for counseling and awareness and improving resource availability for risk mitigation through strategic mobilization.
Conclusion: The COVID-19 pandemic has provided rich learning opportunities for health system strengthening in India. Countries must strengthen learning mechanisms to identify and adapt best practices from within their health systems and from other relatable settings.
1. Introduction
Breastfeeding is one of the best known interventions to reduce neonatal and infant mortality (1). However, despite investment in efforts, the 2019 Global Breastfeeding Score Card by World Health Organization (WHO) and United Nations Children's Emergency Fund (UNICEF) reported that breastfeeding practices were universally in poor alignment with the recommendations, especially in resource constrained settings (2–5). The COVID-19 pandemic that hit in 2020 caused further disruption to routine institutional breastfeeding practices in India and other low and middle income countries, and the rates are likely to have suffered further (6, 7).
India has the largest annual birth cohort in the world; about 23 million babies are born in India every year which is almost equal to the annual birth cohort of the next three countries i.e., China, Nigeria and Pakistan taken together. There is strong commitment to improve breastfeeding practices in healthcare facilities in India. However, inconsistencies persist. As per the latest National Family Health Survey [NFHS-5 (2019–21); India's Demographic Health Survey], while 88.6% of the deliveries in India happen in institutional settings, only about 42% of mothers manage to breastfeed their newborn within an hour of delivery (early initiation of breastfeeding) (8). This suggests that there is much need for strengthening breastfeeding practices in institutionalized mother-newborn dyads (9–13). It must be acknowledged that the aforementioned statistics could be an oversimplification. While on one hand there are health facilities both in the government and in the private sector that have world-class practices and capacity, there are the ones that are compromised in terms of skill, capacity and motivation. Thus, India provides a rich context for health system learning that need not be limited to within-country consumption but of immense value for global debate and adaptation (14–16). In the past, learnings from India have influenced global health action for maternal and child health. For example, India was the first country to launch a family planning program. India's Anganwadi Program is the largest community-based program in the world for early childhood education and nutrition (17). Even for polio eradication and for strengthening newborn programs, insights from India have been leveraged by other countries (18, 19). As the largest member in the South East Asia Region, India has major influence in the region's health performance and policy decisions. Nevertheless, the Indian context continues to be heterogenous, resource inconsistent and complex with ample opportunity for improvement, standardization and cross-learning (20, 21).
The COVID-19 pandemic challenged the well-established practices of newborn care (22–24). At the beginning of the pandemic, the possibility of vertical or horizontal transmission was unknown, and it was not fully understood how neonates could be affected. Further, the pandemic posed challenges to the quality of care at health care institutions on various fronts including provisions for breastfeeding support to the mother and her newborn, kangaroo mother care (KMC), family participatory care, and human milk bank operations (6, 25, 26). Fears around the spread of COVID-19 infection, lack of resources, technical and infrastructural limitations and lack of coherent guidelines coincided with the simultaneous efforts toward protecting institutional practices for breastfeeding. Concerns revolved around practicing skin-to-skin contact (SSC), rooming-in and breastfeeding by COVID-19 suspected, probable or confirmed mothers.
In early 2020, WHO conducted a living systematic review, to identify studies including mothers with suspected or confirmed COVID-19 and their infants or young children, in order to assess the outcomes of COVID-19 infected mothers who were breastfeeding (27). It was found that the risk of COVID-19 infection was low and the infection was typically mild or asymptomatic in newborns, while the results of not breastfeeding and separation of mother and the newborn were significantly negative (27). Consequently, WHO recommended that mothers who were suspected, probable, or confirmed cases of COVID-19 should follow standard infant feeding practices along with necessary precautions for IPC. These recommendations included that for continuous and prolonged skin-to-skin contact immediately after birth, initiation of breastfeeding within 1 h of birth, rooming-in and exclusive breastfeeding. Mothers were advised to mandatorily take IPC precautions, including hand washing, using medical masks and cleaning of frequently touched surfaces (28). However, a survey of 33 countries conducted around that time showed that the guidelines in these countries were not in alignment with the recommendations from WHO (29). As knowledge accrued over the year 2020, many studies started reporting on neonatal outcomes and recommended approaches to handling of the mother-infant dyad during the COVID-19 pandemic. Gradually, countries' guidelines including those released by the Indian scientific bodies got in line with those from WHO (30, 31). Nevertheless, the chaos that prevailed in the meanwhile led to several work around solutions, some as innovations for resource optimization while many as temporary make-shift arrangements. These called for a careful compilation and gave an opportunity for critical learning.
This review was planned with a view to understand the breastfeeding related challenges in institutional settings during the COVID-19 pandemic and the approaches identified as measures to combat these challenges in resource constrained settings with India as a candidate example. The purpose was to collate scientific evidence on key interventions that may be useful in implementing recommended breastfeeding practices with resilience within institutional settings for mother-newborn dyads in India and relatable contexts in the event of a future pandemic/public health crisis.
2. Methods
The review followed the scoping review extension of Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA-ScR) guidelines.
2.1. Data sources and search strategy
We searched Medline via PubMed and Web of Science databases for the combinations of four sets of keywords. The first set consisted of the words: “mother”, “female”, “woman”, “neonate”, “newborn”, “infant”, “nursing mother”. The second set included: “pandemic,” “COVID-19”, “Coronavirus”, “SARS CoV-2”, “severe acute respiratory syndrome coronavirus 2”. The third set included: “breastfeeding”, “breast feed”, “lactation”. The fourth set included: “institutionalized”, “hospitalized”, “maternity ward”, “nursery”. The words in each set were separated by an OR Boolean. We used all word variations and the searches were done in the title and abstract as well as MeSH word search. The fourth set of words were searched in all fields. In the final search, we used combination of words from the four sets by placing AND between the search sets (detailed search strategy is presented in Supplementary Table 1). The search was conducted for the time frame of 1 December 2019 to 15 April 2022. All study designs were included. We restricted the search to articles from India with an aim to collate information for the Indian context. Further, we searched for relevant gray literature using similar keywords (for e.g., mother, breastfeeding, lactation, COVID-19, hospital, etc.) as that of the search strategy on Google (free word search), Government of India website (www.nhm.gov.in) and on websites of major professional bodies in India i.e., IAP, NNF, FOGSI, BPNI, IAPSM, IPHA, WHO, and UNICEF; we looked for policy documents, guidelines and advisories.
2.2. Article selection and data extraction
Three researchers (ND, DS, SN) independently screened the title and abstracts of the documents identified through the search, followed by screening those short-listed by reviewing the full text. The conflicts were resolved after discussion and fourth reviewer's comments, if necessary. Thereafter, information relevant to the study objectives was extracted onto a pre-defined data extraction tool. Extracted information included details about the study characteristics (authors, country, publication dates, study design, location), objectives, inclusion/exclusion criteria, major findings related to breastfeeding practices and potential solutions suggested by authors of the evidence gathered. The analysis and summary of gray literature were recorded in the same way as it was done for primary studies. Data extraction form is given in Supplementary File.
2.3. Data analysis
Challenges and potential solutions were identified from each study and from the gray literature were listed and categorized under one or more suitable headings based on the WHO building blocks for health systems (32). This framework describes health systems in terms of six core components or “building blocks” viz (i) leadership/governance, (ii) healthcare financing, (iii) health workforce, (iv) access to essential medicines, (v) service delivery, and (vi) health information systems, and has been a popular framework used for health systems research over the years. Studies conducted for assessing if the framework served the purpose for strengthening public health facilities in resource constrained settings have reported in its favor (33). We identified bottlenecks for each building block and they were tabulated as challenges with their potential solutions. Following working definitions were used:
• Bottleneck: any factor that hinders or limits the ability of a health system to deliver the care as per recommended guidelines and therefore poses a barrier to delivering high quality maternal and newborn care to improve health outcomes.
• Leadership/governance: refers to the management and governance of the health system, including policy development, regulation, and accountability, effectiveness of regulatory frameworks, new organizational practices and policies, capacity to assemble and manage resources.
• Healthcare financing: refers to the availability and use of financial resources to support the health system; efficient and effective healthcare financing system, effective budget consumption, ensuring financial sustainability, and cost-effective interventions.
• Health workforce: refers to the availability, distribution, and quality of health workers; number of health workers, their training and qualifications, motivation, appropriate and timely feedback.
• Access to essential medicines: refers to the availability and affordability of essential medicines, vaccines, and technologies; availability and affordability of essential medicines, the quality of medicines and technologies, effectiveness of procurement and supply chain management, networking with the external environment.
• Service Delivery: refers to the provision of essential health services to individuals and populations.; on-time services, mode of communication suitable to patients, and coverage of essential health services.
• Health information systems: refers to the availability and use of reliable health information to support decision-making, planning, and management; availability of health information technology, up-to-date and appropriate guidelines and protocols.
3. Results
3.1. Study selection
The database search generated 23 articles. After removing duplicates (n = 3) and irrelevant articles (n = 14), 6 articles were shortlisted. After adding the resources from gray literature (n = 22), a total of 28 documents were included in the review. The PRISMA flow diagram shows the details of the selection of the documents (Figure 1).
3.2. Study characteristics
The 28 documents selected included open letters (n = 5), original research articles (n = 4), press releases and news briefs (n = 3), guidance documents (n = 3), professional bodies' recommendations (n = 3), narrative/expert reviews (n = 2), commentaries (n = 2), updates and advisories (n = 2), position papers and alerts (n = 2), case report (n = 1), and clinical practice guidelines (n = 1). The included articles and their main findings are given in Supplementary Table 2.
3.3. Challenges to implementing recommended breastfeeding practices in institutionalized recently delivered mothers, and reported solutions
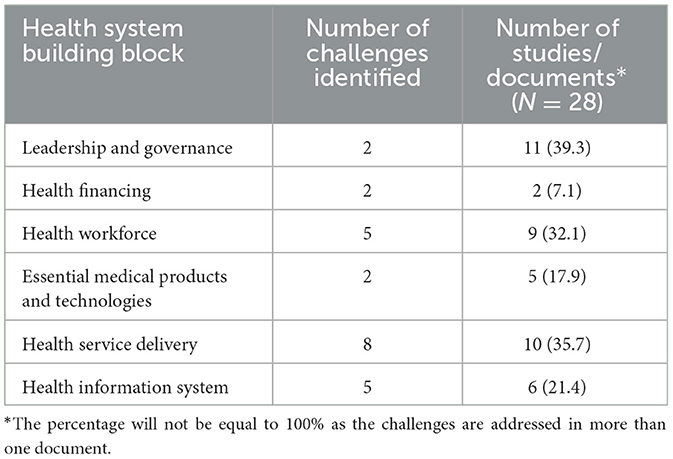
The primary challenge that surfaced from the study findings was the lack of accurate information on best practices for breastfeeding during a pandemic. This included the absence of standard guidelines, confusion among healthcare workers, and inadequate materials for educating and promoting breastfeeding during COVID-19. Most of the challenges identified were categorized under health service delivery, health workforce, and health management information systems. Specifically, 39.3% of the documents addressed challenges related to leadership and governance, while 35.7% addressed challenges related to health service delivery. In addition, challenges pertaining to the health workforce domain were found in approximately 32.1% of the documents, while 21.4% of the identified challenges fell under the health information system domain. Finally, around 17.9% and 7.1% of the documents included challenges related to the essential medicines and health financing domains, respectively (Table 1).
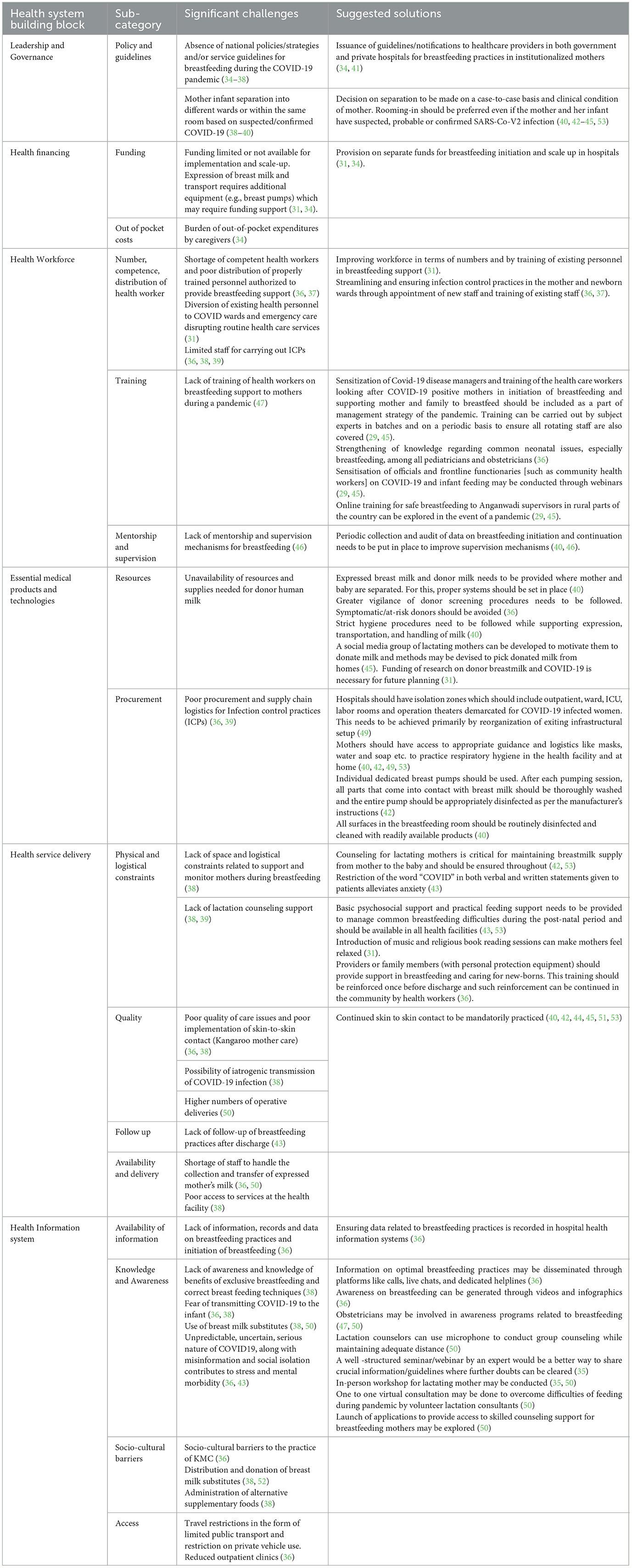
3.3.1. Leadership and governance
In the initial days, guidelines for breastfeeding during COVID-19 were not in place which led to poor decision-making and planning, and a lot of confusion and misinformation among the healthcare delivery staff as well as the mother and her family (34–38). For example, some guidelines recommended that mothers with COVID-19 should be separated from their infants (38–40). This could have contributed to restriction of skin-to-skin contact and rooming-in in recently delivered mother-newborn dyads. Timely issuance of guidelines/notifications to healthcare providers in all the institutions and case-to-case based decision making on separating mothers and infants were some of the solutions in the literature to overcome this challenge (34, 40–45).
3.3.2. Healthcare financing
Documents reported about the inadequacy of funds for scaling up breastfeeding initiation both in terms of deploying dedicated human resource and logistics (42, 44). For example, availability of donor milk or expressing milk were some of the measures mentioned in the guidelines when direct breastfeeding was not possible. However, maintenance and transportation of donor milk and equipment like breast pumps required additional funding support which was not adequately available. Provision of separate funds for breastfeeding initiation and scale up in hospitals was a probable solution suggested (42, 44).
3.3.3. Health workforce
Health workforce challenges primarily included shortage of health workers, lack of training in breastfeeding support and supervision in the hospitals (36, 37). Many healthcare workers were diverted to COVID-19 management tasks including contact tracing, laboratory testing, triaging and emergency care, leading to disruption of routine healthcare services (42). Additionally, there was a lot of confusion regarding breastfeeding practices during the pandemic. In such situation, health workers were unable to impart the usual counseling and support to mothers regarding breastfeeding (46). The documents recommended that responsive management practices be adopted for improving the workforce situation both in terms of quantity and quality by expeditiously recruiting and training human resources for health and strengthening their knowledge through webinars, online training, etc (36, 39, 42, 46–48).
3.3.4. Access to essential medicines, medical products, and technology
Lack of essential medicines and equipment was another set of challenges observed during the pandemic. Supply and logistics chain was disrupted; there was constant shortage of personal protective equipment (PPEs) and other essential medicines and equipment. Challenges were identified at two levels i.e., the facilities being historically under-resourced and procurement being relatively slow (36, 39). These being systemic challenges that may not be amenable to immediate correction, the reports suggested to focus on improving patient awareness and hospital staff for strengthened IPC for optimizing the need for resource reinforcement (36, 40, 42, 48, 49).
3.3.5. Health service delivery
Service delivery was affected mainly due to disruption in the availability and quality of breastfeeding support. Physical and logistical constraints like lack of space to monitor mothers during breastfeeding and lack of lactation counseling, poor quality of care issues and poor implementation of skin-to-skin contact and possibility of iatrogenic transmission of COVID-19 infection were some of the challenges under this domain (36, 38, 39, 43, 50). The guidelines mandated delivery of basic psychosocial and lactating support to mothers, training to providers and family members regarding breastfeeding support and continued SSC to streamline breastfeeding practices (36, 42–45, 51).
3.3.6. Health information system
A major challenge was the lack of information on breastfeeding initiation and practices in the health management information system (36). Community ownership and partnership related challenges included poor awareness among public regarding exclusive breastfeeding and correct breastfeeding techniques, fear of contracting infection and sociocultural barriers (36, 38, 50, 52). Subsequently, there was a lot of misinformation which led to stress and anxiety among mothers and other family members (36, 43). Awareness campaigns and workshops through videos, infographics, live chats and helplines by professionals and health workers was one potential solution to deal with this challenge (35, 36, 47). It was also suggested that systems should be put in place to ensure that data related to breastfeeding practices was adequately recorded in the hospital's health information database for informing subsequent action (50).
The details of the challenges and suggested solutions for these challenges have been listed in Table 2.
4. Discussion
This review highlights the issues surrounding breastfeeding practices in institutionalized recently delivered mother-newborn dyads in India during the COVID-19 pandemic. Separation of mother and the newborn immediately after birth, inadequate human resources and resources for infection control practices, besides unavailability of supportive guidelines and protocols made implementation of recommended breastfeeding practices difficult. Infrastructural gaps e.g., donor milk storage and milk transport support, resulted in use of alternative feeding methods like formula milk. Solutions suggested by the evidence primarily focused on timely issuance of standard guidelines and protocols, awareness generation, lactation support and training of health care professionals regarding methods and importance of optimal breastfeeding practices. Use of telemedicine technology and group sessions were suggested by few articles as alternative strategies. We observed that institutions could identify work around solutions for every challenge they faced though many of these could be temporary. Thus, we are encouraged to infer that there is hope to work toward improved health system preparedness for resilience during health emergencies.
In hospital settings, it has been reported that separation of the mother and the baby at birth and delay in initiating breastfeeding during the COVID-19 pandemic had lasting adverse effect on breast milk feeding outcomes even in well-resourced contexts (54). In their review, Spatz et al. go on further to report that lack of skin-to-skin contact, inadequate lactation support, and insufficient care and education for mothers served as additional challenges to breastfeeding during the pandemic (55). Kotlar et al. also revealed that weak healthcare infrastructure and resources negatively impacted maternal outcomes and breastfeeding practices (48). These were the major challenges identified in our review as well. In our review, bottlenecks were noted for all the six building blocks of health systems with the maximum number of challenges being identified in the blocks of health service delivery (n = 8), health workforce (n = 5) and health management information system (n = 5). Of the six building blocks, challenges in the leadership and governance block appeared in the maximum number of documents that we reviewed (in 11 of 28; 39.3%). Two challenges were noted in the leadership and governance block i.e., unavailability of guidelines and separation of the mother and the newborn at birth. Similarly, even if just two articles mentioned about challenges with health financing, these were quite serious ones—lack of resources for institutional infrastructure and inadequate cover for out-of-pocket expenditure. Thus, these two blocks could have offered significant operational and structural challenges to surge planning during the pandemic. In 2015, Dickson et in follow-through to the Every Newborn Action Plan and the Strategy for Ending Preventable Maternal Mortality (EPMM), did an in-depth analysis of health systems bottlenecks for scaling up quality interventions for newborn care in 12 low-and-middle-income countries in the Indian sub-continent and in Africa (56). They found that the major health system bottlenecks for breastfeeding were of health financing, health service delivery, health workforce, and essential medical products and technologies. Our findings concur with this. We, hence, observe that the pandemic uncovered inherent gaps in health systems for breastfeeding and if these gaps were plugged with contextual interventions, then the system could become more resilient.
We believe that the absence of clear, evidence-based guidelines in the local or regional context (block: leadership and governance) had a central role to play in the disruptions that the pandemic caused to institutional breastfeeding practices. Countries across the globe followed different approaches and protocols at the beginning of the pandemic. There were several modifications to international recommendations for breastfeeding at the hospital during the first year of the COVID-19 pandemic (57–59). Early in the pandemic, researchers through a collaborative effort conducted a review of 33 countries to assess the alignment of their national guidelines for maternal and child health practices during the pandemic with WHO recommendations. They found that none of these recommended all the aspects of the WHO guidance (29). India, like several other countries, had missed on many WHO recommended practices in the initial course of the pandemic (29, 30). Practices that had been overlooked initially were that of rooming-in, early initiation of breastfeeding and direct breastfeeding with infection control measures. However, in due course of time, India improved its alignment score by six points, as reported in a study by Gibble et al., where 101 countries' guidelines were scored based on their alignment with WHO recommendations (30). We, thus, appreciate the leadership that WHO recommendations could play in motivating member states in sustaining breastfeeding practices during public health emergencies despite resource constraints, and the intentionality of countries to make efforts for safeguarding recommended breastfeeding practices.
A system with a strong resource base is likely to be more resilient to disruptions. India's health system is impeded by years of under-investment.
India allocates 1.3% of the GDP to health which is much less than other countries where the average share is 3.6–7% (60). Furthermore, the country does not have a dedicated workforce for supporting breastfeeding practices, even in its most apex healthcare institutions. Consequently, the inherent fragility of the institutional practices for breastfeeding was obvious in the initial days of the pandemic. Nevertheless, it was also evident that the country's health system has the potential to learn and adapt. Putting the needful systems in place and consistently updating the existing capacity is needed to make the breastfeeding services strong and resilient to collateral damage from a pandemic. It is important to highlight the fact that recommendations against breastfeeding should not be made without sufficient evidence that they are necessary. At the same time, mass communication channels can be used to increase awareness regarding early initiation and continued exclusive breastfeeding among the general public to reduce myths and misinformation during pandemics.
4.1. Limitations
The major limitations of this review are that we did not take into account the breastfeeding practices after discharge, at home and thereafter. Understanding that the pandemic situation was exigent, we also acknowledge that available (published) literature may not be comprehensive. Further, we did not include articles from countries other than India. So, there is a likelihood of potentially relatable learnings that remain to be enumerated beyond that highlighted in this manuscript. While our analysis highlights that the challenges to breastfeeding existed across all the six pillars, these were complex and systemic. It is inadequately understood as to how populations and health systems respond to public health emergencies given their unique lived experiences, risk perceptions and preparedness (61). Nevertheless, breastfeeding practices continue to be amenable to socio-cultural influences, at least in resource constrained settings (62–64). The WHO building blocks for health systems does not allow for commentary on inter-dependencies between the blocks and with due consideration of the socio-cultural context; we accept this as a major limitation to our study since we have weaved our findings around these building blocks. The framework's inadequacies were obvious during the pandemic when global public health approaches demanded systems thinking with due attention to complexities. It is in the pandemic context that governance was identified as the major “under-pinning” of health system strengthening that cuts across all the building blocks (65).
5. Conclusion
The COVID-19 pandemic had a significant impact on the breastfeeding practices among institutionalized recently delivered mothers. Health service delivery, health workforce and health management information system were the most commonly affected areas. Nevertheless, the pandemic has provided rich learning opportunities for health system strengthening. A roadmap should be in place as a result from these learnings and experiences. Establishing learning loops at individual, team and at organizational levels can facilitate the adaptation of best practices from within and beyond institutional settings, and help optimize breastfeeding practices during future pandemics.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
ND and DS: tool development, literature search, data acquisition, data analysis, manuscript preparation, and manuscript editing. PP, RM, and SN: data acquisition, manuscript editing, and manuscript review. AMa: concepts, design, definition of intellectual content, tool development, manuscript editing, manuscript review, and guarantor. AMo: concepts, design, definition of intellectual content, tool development, data acquisition, data analysis, manuscript editing, and guarantor. All authors contributed to drafting of the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1142089/full#supplementary-material
References
1. International Baby Food Action Network (IBFAN) and United Nations Children's Fund (UNICEF). Suggestions for CRC Committee's- Concluding Observations on Infant and Young Child Feeding. International Baby Food Action Network (IBFAN) (2022).
2. World Health Organization, United Nations Children's F. Global Breastfeeding Scorecard, 2019: Increasing Commitment to Breastfeeding Through Funding and Improved Policies and Programmes. Geneva: World Health Organization. (2019).
3. Wang H, Bhutta ZA, Coates MM, Coggeshall M, Dandona L, Diallo K, et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study (2015). Lancet. (2016) 388:1725–74. doi: 10.1016/S0140-6736(16)31575-6
4. United Nations Children's Fund. Tracking Progress for Breastfeeding Policies and Programmes. Geneva: UNICEF and WHO (2017).
5. Takahashi K, Ganchimeg T, Ota E, Vogel JP, Souza JP, Laopaiboon M, et al. Prevalence of early initiation of breastfeeding and determinants of delayed initiation of breastfeeding: secondary analysis of the WHO Global Survey. Sci Rep. (2017) 7:44868–44868. doi: 10.1038/srep44868
6. Maria A, Mukherjee R, Upadhyay S, Pratima K, Bandyopadhyay T, Gupta R, et al. Barriers and enablers of breastfeeding in mother–newborn dyads in institutional settings during the COVID-19 pandemic: a qualitative study across seven government hospitals of Delhi, India. Front Nutr. (2022) 9:1052340. doi: 10.3389/fnut.2022.1052340
7. Rao SPN, Minckas N, Medvedev MM, Gathara D, N PY, Estifanos AS, et al. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers' voices and experiences. BMJ Global Health. (2021) 6:e004347. doi: 10.1136/bmjgh-2020-004347
8. International Institute for Population Sciences and MoHFW GOI. National Family Health Survey: Key Findings India. Ministry of health and Family Welfare (MoHFW) (2021).
9. Aguayo VM, Gupta G, Singh G, Kumar R. Early initiation of breast feeding on the rise in India. BMJ Glob Health. (2016) 1:e000043. doi: 10.1136/bmjgh-2016-000043
10. Patel A, Banerjee A, Kaletwad A. Factors associated with prelacteal feeding and timely initiation of breastfeeding in hospital-delivered infants in India. J Human Lactat. (2013) 29:572–8. doi: 10.1177/0890334412474718
11. Sharma A TP. Factors associated with early initiation of breastfeeding among mothers of tribal area of Madhya Pradesh, India: a community based cross sectional study. Int J Commu Med Public Health. (2016) 3:194–9. doi: 10.18203/2394-6040.ijcmph20151561
12. Badaya N, Jain S, Kumar N. Time of initiation of breastfeeding in various modes of delivery and to observe the effect of low birth weight and period of gestation on initiation of breastfeeding. Int J Contemp Pediatr. (2018) 5:ijcp20182555. doi: 10.18203/2349-3291.ijcp20182555
13. Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS. How many child deaths can we prevent this year? Lancet (London, England). (2003) 362:65–71. doi: 10.1016/S0140-6736(03)13811-1
14. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Global Health. (2018) 6:e1196. doi: 10.1016/S2214-109X(18)30386-3
15. Garg S, Bhatnagar N, Singh MM, Borle A, Raina SK, Kumar R, et al. Strengthening public healthcare systems in India; learning lessons in COVID-19 pandemic. J Family Med Primary Care. (2020) 9:5853. doi: 10.4103/jfmpc.jfmpc_1187_20
16. Das J, Holla A, Das V, Mohanan M, Tabak D, Chan B. In urban and rural India, a standardized patient study showed low levels of provider training and huge quality gaps. Health Affairs (Project Hope). (2012) 31:2774. doi: 10.1377/hlthaff.2011.1356
17. Muttreja P, Singh S. Family planning in India: the way forward. Indian J Med Res. (2018) 148:S1. doi: 10.4103/ijmr.IJMR_1807_18
18. Cochi SL, Hegg L, Kaur A, Pandak C, Jafari H. The global polio eradication initiative: progress, lessons learned, and polio legacy transition planning. Health Affairs. (2017) 35:277–83. doi: 10.1377/hlthaff.2015.1104
19. Thacker N, Vashishtha VM, Thacker D. Polio eradication in India: the lessons learned. Pediatrics. (2016) 138:4. doi: 10.1542/peds.2016-0461
20. Bisht R, Pitchforth E, Murray SF. Understanding India, globalisation and health care systems: a mapping of research in the social sciences. Global Health. (2012) 8:32. doi: 10.1186/1744-8603-8-32
21. Yazbeck AS, Peters DH. Health Policy Research in South Asia : Building Capacity for Reform. Washington, DC: World Bank. (2003).
22. Chmielewska B, Barratt I, Townsend R, Kalafat E, van der Meulen J, Gurol-Urganci I, et al. Effects of the COVID-19 pandemic on maternal and perinatal outcomes: a systematic review and meta-analysis. Lancet Glob Health. (2021) 9:e759–72. doi: 10.1016/S2214-109X(21)00079-6
23. Tripathi S, Gogia A, Kakar A. COVID-19 in pregnancy: a review. J Family Med Primary Care. (2020) 9:4536–40. doi: 10.4103/jfmpc.jfmpc_714_20
24. Inversetti A, Fumagalli S, Nespoli A, Antolini L, Mussi S, Ferrari D, et al. Childbirth experience and practice changing during COVID-19 pandemic: a cross-sectional study. Nursing Open. (2021) 8:3627–34. doi: 10.1002/nop2.913
25. Justman N, Shahak G, Gutzeit O, Ben Zvi D, Ginsberg Y, Solt I, et al. Lockdown with a price: the impact of the COVID-19 pandemic on prenatal care and perinatal outcomes in a tertiary care center. IMAJ. (2020) 22:533–7.
26. Greene NH, Kilpatrick SJ, Wong MS, Ozimek JA, Naqvi M. Impact of labor and delivery unit policy modifications on maternal and neonatal outcomes during the coronavirus disease 2019 pandemic. Am J Obstet Gynecol. (2020) 2:100234. doi: 10.1016/j.ajogmf.2020.100234
27. Breastfeeding and COVID-19. Available online at: https://www.who.int/news-room/commentaries/detail/breastfeeding-and-covid-19 (accessed June 1, 2023).
28. World Health O. Frequently Asked Questions: Breastfeeding and COVID-19: for Health Care Workers, 12 May 2020. Geneva: World Health Organization. (2020).
29. Vu DH, Cashin J, Gribble K, Marinelli K, Mathisen R. Misalignment of global COVID-19 breastfeeding and newborn care guidelines with World Health Organization recommendations. BMJ Nutr Prev Health. (2020) 3:e000184. doi: 10.1136/bmjnph-2020-000184
30. Gribble K, Cashin J, Marinelli K, Vu DH, Mathisen R. First do no harm overlooked: Analysis of COVID-19 clinical guidance for maternal and newborn care from 101 countries shows breastfeeding widely undermined. Front Nutr. (2023) 9, 1049610. doi: 10.3389/fnut.2022.1049610
31. National Neonatology. Forum IF of Oand GS of I and IA of P. In: Clinical Practice Guideline:Perinatal-Neonatal Management of COVID-19. (2021).
32. World Health Organization (WHO). Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: World Health Organization. (2010).
33. Manyazewal T. Using the World Health Organization health system building blocks through survey of healthcare professionals to determine the performance of public healthcare facilities. Arch Public Health. (2017) 75:50. doi: 10.1186/s13690-017-0221-9
34. Breastfeeding Promotion Network of India. Letter: Separating Covid Positive Mothers and Babies: Abandoning Breastfeeding. (2021).
35. Malik S, Joshi P, Gupta PK, Sharma S. Assessment of knowledge and opinion regarding breastfeeding practices during COVID-19 pandemic among paediatricians and obstetricians in India: an online survey. Sudanese J Paediat. (2021) 21:30. doi: 10.24911/SJP.106-1598349125
36. Sachdeva RC, Jain S, Mukherjee S, Singh J. Ensuring exclusive human milk diet for all babies in COVID-19 times. Indian Pediatr. (2020) 57:730. doi: 10.1007/s13312-020-1917-4
37. Anand P, Yadav A, Debata P, Bachani S, Gupta N, Gera R. Clinical profile, viral load, management and outcome of neonates born to COVID 19 positive mothers: a tertiary care centre experience from India. Eur J Pediatr. (2021) 180:547. doi: 10.1007/s00431-020-03800-7
38. Tomori C, Gribble K, Palmquist AEL, Ververs MT, Gross MS. When separation is not the answer: Breastfeeding mothers and infants affected by COVID-19. Mater Child Nutr. (2020) 16:4. doi: 10.1111/mcn.13033
39. Bhasin M, Nangia S, Goel S. Role of human milk banks amid COVID 19: perspective from a milk bank in India. Int Breastfeed J. (2020) 15:346. doi: 10.1186/s13006-020-00346-0
40. Breastfeeding Promotion Network of India. COVID-19 and Breastfeeding Information Update. (2020).
41. Sterken E. IBFAN news brief: breastfeeding protection in the time of COVID-19. J Human Lactat. (2020) 37:207–8. doi: 10.1177/0890334420964436
42. Breastfeeding Promotion Network of India. Letter: Concerns on separation of babies from Mothers and bottle feeding. (2020).
43. Kumar S, Rathore P, Shweta, Krishnapriya V, Haokip N, Thankachan A, et al. Why I can't breastfeed my new-born baby? Psychosocial dilemma of a COVID-Positive Post-LSCS mother. Indian J Palliat Care. (2020) 26:S150. doi: 10.4103/IJPC.IJPC_157_20
44. Chawla D, Chirla D, Dalwai S, Deorari AK, Ganatra A, Gandhi A, et al. Perinatal-neonatal management of COVID-19 infection—guidelines of the federation of obstetric and gynaecological societies of India (FOGSI), national neonatology forum of India (NNF), and Indian academy of pediatrics (IAP). Indian Pediatr. (2020) 57:536. doi: 10.1007/s13312-020-1852-4
45. Bharadva K, Bellad RM, Tiwari S, Somasekar R, Phadke M, Bodhankar U, et al. Breastfeeding in Coronavirus Disease (2019). (COVID-19): position statement of Indian academy of pediatrics and infant and young child feeding chapter. Indian Pediatr. (2022) 59:58. doi: 10.1007/s13312-022-2422-8
46. Breastfeeding Promotion Network of India. Gaps in Beliefs and Practices of Trained Breastfeeding Counsellors and Lactating Mothers Facing COVID-19 Pandemic in India. Breastfeeding Promotion Network of India (BPNI) (2020).
47. Nanavati R, Mascarenhas D, Goyal M, Haribalakrishna A, Nataraj G, A. single-center observational study on clinical features and outcomes of 21 SARS-CoV-2-infected neonates from India. Eur J Pediatr. (2021) 180:1895. doi: 10.1007/s00431-021-03967-7
48. Kotlar B, Gerson E, Petrillo S, Langer A, Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: a scoping review. Reprod Health. (2021) 18:10. doi: 10.1186/s12978-021-01070-6
49. Gandhi DA, et al. Good Clinical Practice recommendation on Pregnancy with COVID-19 infection. In: FOGSI. (2020). Available online at: https://www.fogsi.org/wp-content/uploads/covid19/fogsi_gcpr_on_pregnancy_with_COVID_19_version_1.pdf (accessed June 1, 2023).
50. Bhatt N. Breastfeeding in India is disrupted as mothers and babies are separated in the pandemic. BMJ. (2020) 25:370. doi: 10.1136/bmj.m3316
51. UNICEF-India. Guidance Note on Financial Contributions or Contributions In-Kind From Food and Beverage Companies. UNICEF (2020).
52. Breastfeeding Promotion Network of India. The Ration Support Containing Commercial Baby Foods may Cause More Harm than Good to Health of Babies. New Delhi: Breastfeeding Promotion Network of India (BPNI) (2022).
53. World Health O. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. Interim guidance. Pediatr Med Rodz. (2020) 16:9–26. doi: 10.15557/PiMR.2020.0003
54. Rostomian L, Angelidou A, Sullivan K, Melvin PR, Shui JE, Telefus Goldfarb I, et al. The effects of COVID-19 hospital practices on breastfeeding initiation and duration postdischarge. Breastfeed Med. (2022) 17:736–744. doi: 10.1089/bfm.2022.0039
55. Spatz DL, Davanzo R, Müller JA, Powell R, Rigourd V, Yates A, et al. Promoting and protecting human milk and breastfeeding in a COVID-19 world. Front Pediat. (2020) 8:633700. doi: 10.3389/fped.2020.633700
56. Dickson KE, Kinney MV, Moxon SG, Ashton J, Zaka N, Simen-Kapeu A, et al. Scaling up quality care for mothers and newborns around the time of birth: an overview of methods and analyses of intervention-specific bottlenecks and solutions. BMC Pregn Childbirth. (2015) 15:S1. doi: 10.1186/1471-2393-15-S2-S1
57. Davanzo R, Merewood A, Manzoni P. Skin-to-skin contact at birth in the COVID-19 era: in need of help! Am J Perinatol. (2020) 37:S1–4. doi: 10.1055/s-0040-1714255
58. Gwartney T, Duffy A. Maintaining safe breastfeeding practices during the COVID-19 pandemic: an overview of the evidence to inform clinical guidelines. Neonatal Network. (2021) 40:140–5. doi: 10.1891/11-T-719
59. Organization WH. Clinical Management of Severe Acute Respiratory Infection (SARI) When COVID-19 Disease is Suspected: Interim Guidance, 13 March 2020. (2020). Available online at: https://apps.who.int/iris/handle/10665/331446 (accessed June 1, 2023).
60. National Health Accounts Estimate Report 2018-19. In: NHA. Available online at: https://chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/nhsrcindia.org/sites/default/files/2022-09/NHA%202018-19_07-09-2022_revised_0.pdf (accessed May 4, 2023).
61. Palmquist AEL, Tomori C, Tumlinson K, Fox C, Chung S, Quinn EA. Pandemic policies and breastfeeding: A cross-sectional study during the onset of COVID-19 in the United States. Front Sociol. (2022) 7:958108. doi: 10.3389/fsoc.2022.958108
62. Ghosh S, Gidwani S, Mittal SK, Verma S. Socio-cultural factors affecting breast feeding and other infant feeding practices in an urban community. Indian Pediatr. (1976) 13:11.
63. Wanjohi M, Griffiths P, Wekesah F, Muriuki P, Muhia N, Musoke RN, et al. Sociocultural factors influencing breastfeeding practices in two slums in Nairobi, Kenya. Int Breastfeed J. (2016) 12:1–8. doi: 10.1186/s13006-016-0092-7
64. Hirani SAA, Richter S, Salami B, Vallianatos H. Sociocultural factors affecting breastfeeding practices of mothers during natural disasters: a critical ethnography in rural Pakistan. Glob Qual Nurs Res. (2023) 10:23333936221148808. doi: 10.1177/23333936221148808
Keywords: breastfeeding, COVID-19, maternal health, newborn care, hospital
Citation: Dudeja N, Sharma D, Maria A, Pawar P, Mukherjee R, Nargotra S and Mohapatra A (2023) Implementing recommended breastfeeding practices in healthcare facilities in India during the COVID-19 pandemic: a scoping review of health system bottlenecks and potential solutions. Front. Nutr. 10:1142089. doi: 10.3389/fnut.2023.1142089
Received: 11 January 2023; Accepted: 14 July 2023;
Published: 31 July 2023.
Edited by:
Nita Bhandari, Center for Health Research and Development, Society for Applied Studies, IndiaReviewed by:
Karleen Gribble, Western Sydney University, AustraliaJing Zhu, Beijing Academy of Science and Technology, China
Jennifer Cashin, FHI 360, United States
Copyright © 2023 Dudeja, Sharma, Maria, Pawar, Mukherjee, Nargotra and Mohapatra. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Archisman Mohapatra, YXJjaGlzbWFuLm1AdGhlZ3JpZGNvdW5jaWwub3Jn; Arti Maria, YXJ0aW1hcmlhQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work
 Nonita Dudeja1†
Nonita Dudeja1† Divita Sharma
Divita Sharma Priyanka Pawar
Priyanka Pawar Ritika Mukherjee
Ritika Mukherjee Archisman Mohapatra
Archisman Mohapatra