- 1Nutrition Program, Department of Natural Sciences, Lebanese American University, Beirut, Lebanon
- 2Department of Healthier Populations, Regional Office for the Eastern Mediterranean, World Health Organization, Cairo, Egypt
- 3Global Public Health Consultant, Muscat, Oman
- 4Department of Mental Health and Non-Communicable Diseases, Regional Office for the Eastern Mediterranean, World Health Organization, Cairo, Egypt
Malnutrition takes a heavy toll on the populations of the Eastern Mediterranean Region (EMR), with gender related socioeconomic risk factors impacting undernutrition and obesity in both women and men. This perspective article, a derivative of a report by the World Health Organization, reviews the scientific literature on the effect of gender on malnutrition related outcomes in the EMR. Results revealed that biological and gender-related socioeconomic risk factors play a role for undernutrition and obesity in both women and men. Malnutrition can be negatively influenced by gender-biased cultural standards, habits, structural determinants, differential exposures, and health system gaps. This can result, for example, in women tending to focus on familial and household related needs, at the expense of their own health and physical mobility and on suffering more food insecurity, undernutrition, micronutrient deficiencies and obesity compared to men in the EMR. Conflict and crisis situations negatively affect both genders, but generally put women at a higher risk of adverse. Women’s socially limited autonomy in mobility is also an obstacle to access to health services in the EMR, including those related to nutrition. Multi-level approaches are needed to address gender issues to enable a more equitable distribution of resources and reduce the impact of malnutrition in the EMR.
Background
The double burden of malnutrition, the co-existence of under nutrition and obesity, affects nearly 2.3 billion people globally (1). Malnutrition takes a heavy toll on the health and well-being of the population of the Eastern Mediterranean Region (EMR), a heterogenous Region with wide economic, social, cultural and health disparities among countries (2). While some EMR countries, especially those affected by conflict, continue to experience high levels of food insecurity, undernutrition, and micronutrient deficiencies, others have been experiencing a nutrition transition (Table 1), with a shift toward unhealthy diets and sedentary lifestyles resulting in 53% of women, 45% of men and 8% of school-age children or adolescents in the Region being obese, respectively (5).
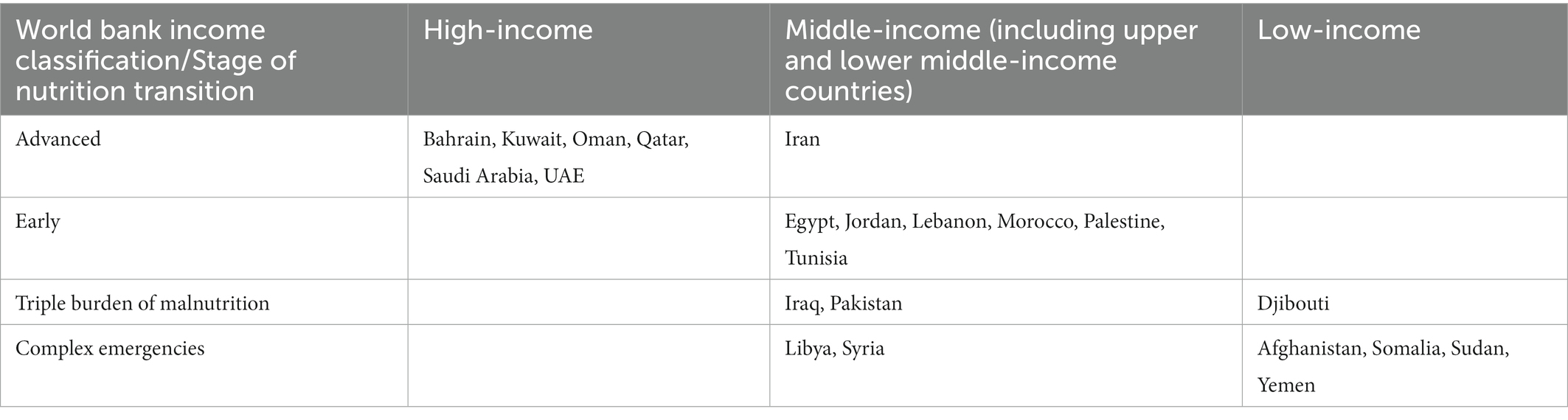
Table 1. Classification of countries in the Eastern Mediterranean Region according to the stage of nutrition transition and the World bank income classification (3, 4).
Malnutrition has social, economic and environmental determinants and the stark health inequalities between and within countries explain the wide variation in the prevalence of under and over-nutrition in the EMR (6, 7). Gender is a key determinant of health, resulting from a combination of both sex-linked biology and gender-related social influences on health outcomes including malnutrition (8, 9). Gender inequality adversely affects the health of women and men, girls and boys as it influences exposure to gender-biased cultural standards, norms and expectations, structural causes, differential exposures and vulnerabilities and health system gaps (10). In relevance to malnutrition, gender inequality has been linked with a greater percentage of low birth weight infants and childhood mortality around the world (11). Childhood stunting has recently shown to have a heavy health cost on productivity in North Africa and the Middle east, costing 1,035–1,339 million dollars of monthly loss for the private sector (12).
Recent gender analyzes by the United Nations Development Program showed that the EMR’s Gender Development Index (GDI), a measure of the gender gap in human development is below the world average and that of the least developed countries (13). Within the EMR, the GDI was highest in Qatar and lowest in Yemen (5) (Figure 1). The life expectancy of women in the EMR is 71 years compared to 68 years in men. Yet, women are expected to live 1.7 years of these 3 years in illness (5); this gender paradox reflects how even though women live longer than men, they face higher rates of illness (14). Health inequalities are partly driven by and intersect with gender differences in educational attainment, labor force participation as well as other determinants of health like class, age and disability status (15).
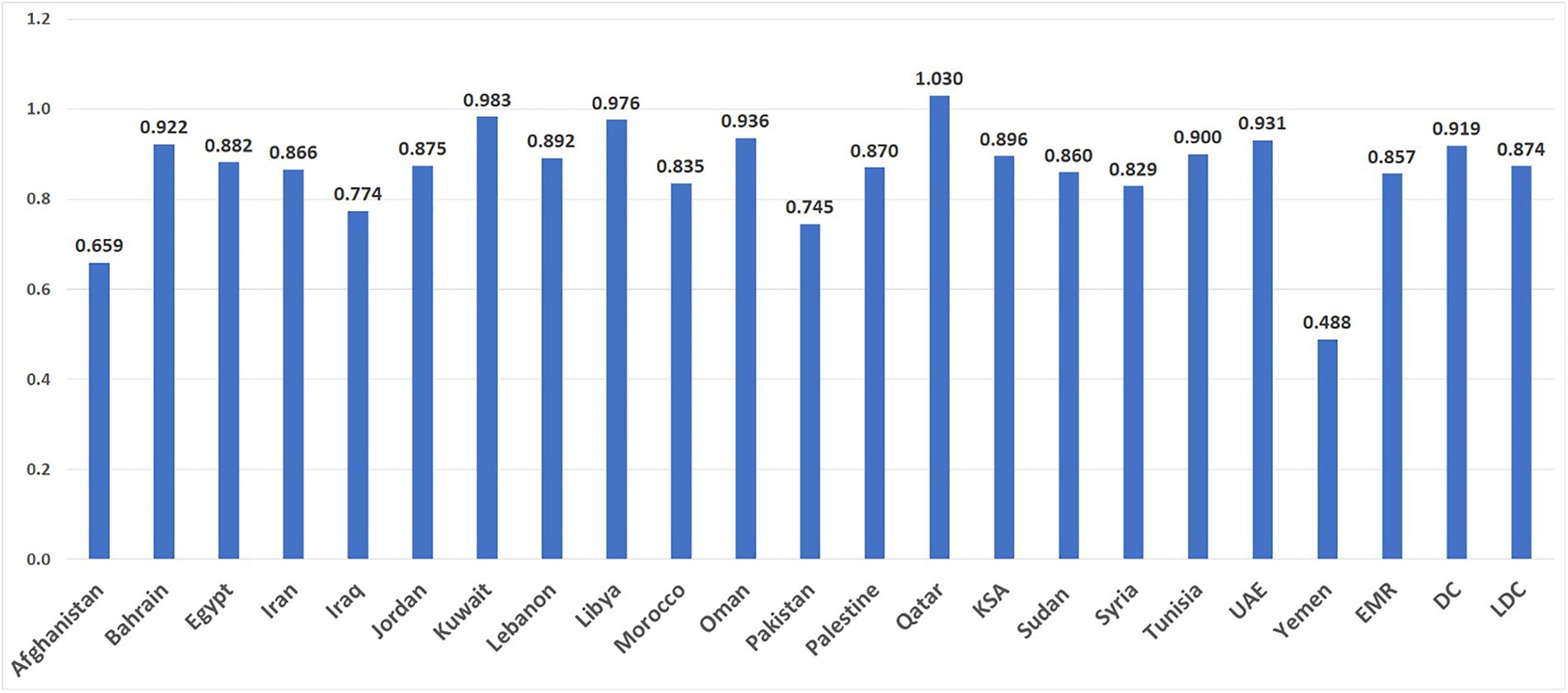
Figure 1. The Gender Development Index (GDI) is an indicator of the gender gap assessing the male and female ratios for the following indicators: Life expectancy at birth, expected years of schooling, mean years of schooling, and estimated gross national income per capita. Higher GDI scores reflect greater human and gender development (13) DC: Developing Countries; EMR: Average of countries in the Eastern Mediterranean Region; LDC: Least Developed Countries. KSA: Kingdom of Saudi Arabia; UAE: United Arab Emirates.
This paper explores the underlying risk factors and consequences of gender discrimination and the unequal power dynamics contributing to malnutrition in the Region and identifies public health actions and literature gaps for further exploration at the intersection of gender and malnutrition. This article is a derivative of a larger project and report on gender and health conducted by the WHO Regional Office of the EMR which included available evidence between years 2000 and 2019 (16).
Conceptual framework
The analysis of the interplay between gender and malnutrition in the WHO regional report and in this manuscript is guided by Sen and Ostlin’s conceptual framework, which describes both structural and intermediary determinants of gendered health outcomes (15, 16). Structural determinants can be in the form of economic, social, and/or political forces. Intermediary factors comprise the gender norms and power dynamics stemming from discriminatory standards, practices, and behaviors as well as differential exposure and vulnerabilities to diseases, which are connected to biases in health systems and in research. Power structures impact different aspects of people’s lives including health and the complexity of such impact can only be understood through the intersectional conceptualization of gender as a social determinant of health (15).
Prevalence of malnutrition in the EMR
EMR countries are in different phases of the nutrition transition depending on their socio-economic, political and urbanization contexts as well as the extent of technological development, access to information, food processing and mass media growth (17). Given the heterogeneity between countries, an elucidation of where countries stand in the nutrition transition process helps the reader better understand the link between gender and the different forms of malnutrition (Table 1). The Gulf Cooperation Council countries are in the advanced phase characterized by an elevated prevalence of obesity, a moderate prevalence of undernutrition and selected micronutrient deficiencies (18). Countries such as Egypt, Jordan, Lebanon, Morocco, Palestine, and Tunisia are classified in an ‘early’ nutrition phase with a moderate prevalence of obesity (even though increasing) and undernutrition (4). Countries such as Djibouti, Iraq and Pakistan have a triple burden of malnutrition with the coexistence of acute and chronic malnutrition, micronutrient deficiencies and an increase in obesity rates (18). Countries such as Afghanistan, Libya, Somalia, Sudan, Syria and Yemen are going through complex emergency situations characterized by severe child and maternal malnutrition and prevalent micronutrient deficiencies (4).
The overall regional prevalence of undernutrition is estimated to be 19%. The highest levels of stunting, wasting, and underweight (among children) are observed in Afghanistan, Djibouti, Pakistan, Somalia, Sudan, and Yemen (19, 20). Micronutrient deficiencies due to low intake and/or status are common in the EMR. It has been estimated that for every three EMR residents, one has micronutrient deficiencies (4). EMR countries record a high rate of iron deficiency and anemia ranging from 20 to 47% among women of reproductive age (15–49 years) (5, 19). Even though most of its countries are considered sunny, the EMR bears a heavy burden of Vitamin D deficiency (21), with up to 83% of EMR residents being Vitamin D deficient, as compared to less than 20% of North Europe residents where it is less sunny (22, 23). While EMR countries, especially those affected by conflict, continue to experience high levels of food insecurity, undernutrition, and micronutrient deficiencies, physical inactivity, overweight and obesity are also common (Figure 2). In the EMR, 47% of adults are overweight or obese compared to 39% globally. The differences between men and women is wider compared to the worldwide rates (53% in women vs. 45% in males in the EMR compared to 40% vs. 39% in women and men, respectively, in the world) (25).
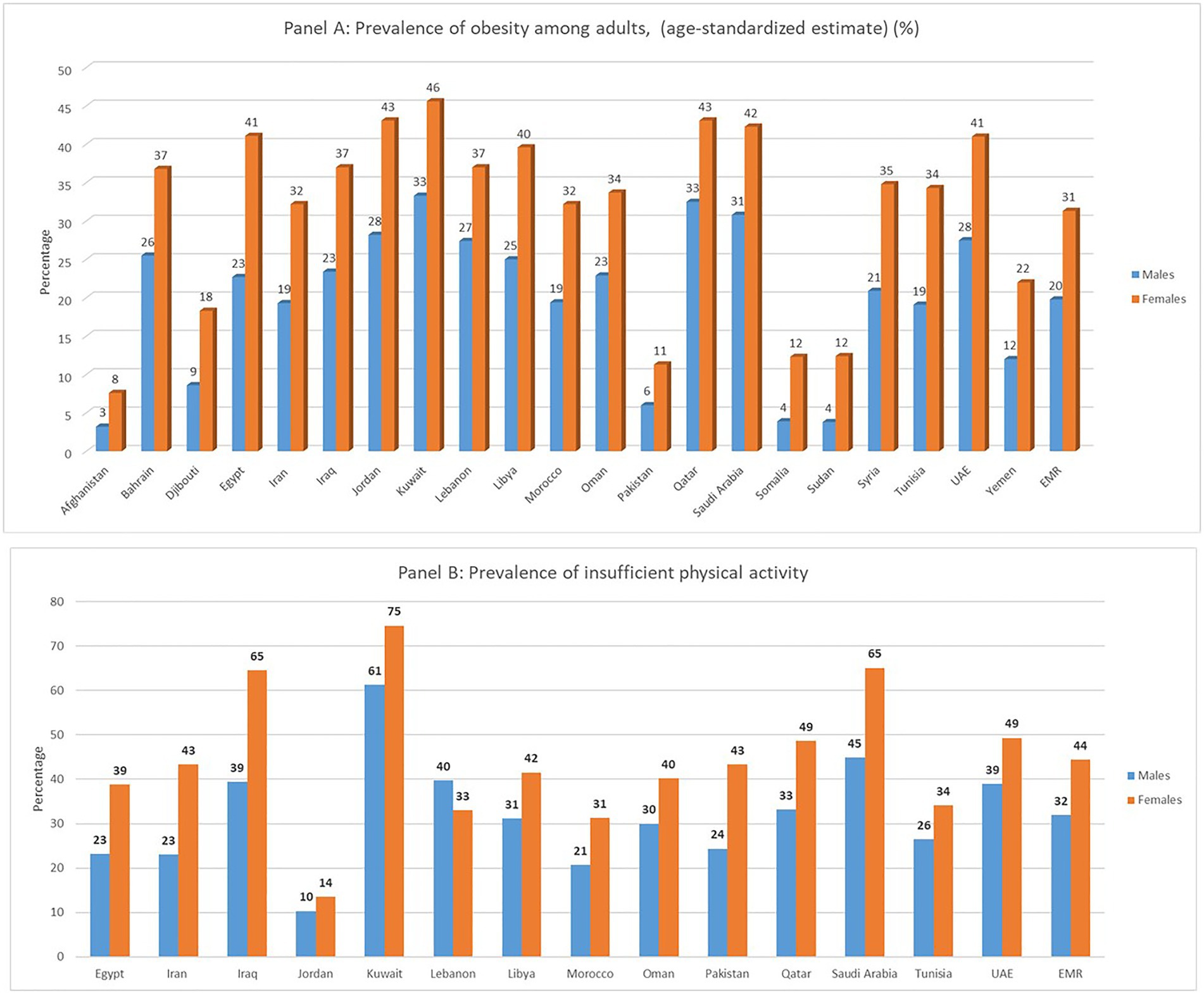
Figure 2. Prevalence of age-standardized obesity Panel (A) and insufficient physical activity Panel (B) among adults aged 18 years or older, by country and sex in the Eastern Mediterranean Region (EMR) (24).
Social cultural, structural and behavioral determinants of malnutrition
Gender is a key determinant of malnutrition resulting from a combination of both sex-linked biology and gender-related social influences on health outcomes (8). Across the region, women’s triple burden of productive, reproductive, and social roles is associated with more time dedicated to familial and household nutrition-related needs and less for attending to their own needs. At the same time, gender norms limit women’s physical mobility and further exacerbate gender and health inequalities in malnutrition (16).
In its socio-economic and political heterogeneity, the EMR is characterized by conflict-related emergency and humanitarian contexts, which play a major structural role in malnutrition. For instance, in Yemen, where the ongoing conflict has resulted in the displacement of around 3.3 million people, malnutrition and undernutrition currently affect 3 million people including 1.5 million children, 1.1 million pregnant and lactating women, and 400,000 acutely malnourished children, putting them at high risk of famine (19). Gender inequality in malnutrition can be further exacerbated when combined with other factors such as conflict or crisis, generally putting women at higher risk of more adverse outcomes. For example, collecting water or food can expose women to gender-based violence, leaving them and their children at increased risk of undernutrition and malnutrition, as a consequence of the inability to perform those tasks (26). In humanitarian crises, women and girls are more vulnerable to malnutrition as the social norms can result in them eating less during food scarcity in favor of men and boys (26). Women, in fact, tend to reduce their own food intake in order to allow other family members to eat, especially male children and men (26, 27). On the other hand, while men and boys are favored when it comes to access to food, they can also suffer from malnutrition during conflict or crisis owing to a lack of cooking skills and access to food distribution (28).
Risk factors
Women and girls have increased biological, socioeconomic, and behavioral risk factors for malnutrition than men and boys. Firstly, with regards to the biological risk factors, women require more protein, energy and micronutrients than usual when pregnant and lactating (29). In view of women’s cyclical loss of iron during menstruation and childbearing time, their nutrition status is particularly vulnerable to micronutrient deficiencies (29). EMR countries record a high rate of iron deficiency and anemia, which ranges from 20 to 47% among women of reproductive age (15–49 years) (5). The highest rates were reported among Egyptian women (47%), adolescents (47%), and children (38%), and the lowest were found among Saudi school-aged children (12%) and elderly (13%) (30). In terms of biological risk factors for obesity, men have a higher likelihood of storing visceral fat compared to pre-menopausal women, which increases their risk of developing type 2 diabetes, cardiovascular events, and death (31, 32). Females have higher deposits of subcutaneous fat than men and see their stores of adipose tissues and visceral fat increase after menopause, heightening the adverse events associated with obesity (33).
Secondly, in relation to socioeconomic factors, some of the household-level predictors of stunting among women in the Region are their low status, inadequate dietary habits during pregnancy and lactation, inappropriate intra-household food allocation, widespread poverty, and poor access to clean water (34, 35). A study from Pakistan found correlations between malnutrition and low-income households and identified lack of maternal literacy to be strongly correlated with malnutrition (36). In relation to vitamin D, being a woman has been identified as a significant predictor of Vitamin D deficiency in the Region with rates of deficiencies reaching 96% in some countries (37, 38). This is due to social and religious variables like skin covering and veiling that constitute a risk factor for Vitamin D deficiency in most, though not all, studies in the EMR (23, 37, 39–44). Women of lower socio-economic status have increased risk of malnutrition due to their limited access to healthy foods, stressful lifestyles, and limited physical activity (25, 45). Notably, the socioeconomic factors driving malnutrition in the EMR reflect a complex reality as obesity rates are highest in some of the Region’s wealthiest countries: Kuwait (42.5% in men, 47.1% in women), Qatar (39.5% in men, 43.2% in women), and Bahrain (32.3% in men, 40.3% in women) (46).
Finally, behavioral risk factors do affect malnutrition differently. In the EMR, one of the top contributing risk factors to obesity and NCDs is the high prevalence of physical inactivity (47). It is estimated that the EMR is the second highest region in the prevalence of physical inactivity globally (35%), with women being less active than men in most countries (48). One study found that physical inactivity ranges from 60% in Jordan, to 95% in Egypt and 98% in KSA (49). Males have been found to engage in more physical activity than women in most EMR countries except for Lebanon (50). In Jordan, one study revealed higher inactivity rates among males while the WHO data reflected the opposite (24, 51). Further to this, when disaggregating for sex, young women in the region have higher rates of physical inactivity compared to the global figures (52). The social limitations of women’s physical mobility in the Region constitute a major factor for inactivity (53). For example, youth centers in Egypt catering for lower socio-economic groups were criticized for being open to male youth only, although on paper they were supposed to be accessible to both sexes (54).
Access to health care services
Women’s socially limited autonomy in mobility not only exacerbate ‘lifestyle’ risk factors such as food consumption and physical inactivity, but also represent one of biggest obstacles to access and utilization of health services in the Region. These gender-related social norms not only limit women’s mobility but also restrict autonomy in decision-making regarding their health and well-being. One study from Afghanistan found that the lack of autonomy for women is an important obstacle to antenatal visits (55). The most recent regional health profile indicated that antenatal care is insufficient in the EMR, with coverage of at least four clinic visits for antenatal care is under 80% for 10 countries, and as low as 3.3% in Somalia (5).
Another barrier toward gender-sensitive universal access to health is the lack of culturally acceptable health services, including the scarcity of female health providers to attend female patients. For example, a study in Jordan, found that some women favored private service providers rather than public, in part due to the increased availability of female obstetricians; however, those attending private providers used public hospitals for birth, which creates discontinuity and fragmentation in maternal-neonatal healthcare, and in child healthcare services (56).
Health outcomes
Health outcomes from malnutrition can be serious and wide-ranging (25). Across the EMR, iron deficiency is one of the leading determinants of adolescent disability-adjusted life years, especially in low- and middle-income countries, contributing to 20% of maternal deaths (25). Moreover, maternal malnutrition has been linked to low birth weight, and growth retardation in children (57, 58), which in turn results in high infant morbidity and mortality rates, adding to health care costs and undermining the economic human resource potential nationally (59). Malnutrition in mothers jeopardizes the quality of care they can offer their children by reducing the meaningful mother–child interaction that is necessary for proper growth (60). Experience from low-income and conflict-affected countries in the EMR like Yemen, Somalia, Afghanistan, Sudan and Djibouti shows that poor female nutrition early in life reduces learning potential, increases reproductive and maternal health risks, and lowers productivity (2, 7). This situation contributes to women’s diminished ability to gain access to other assets later in life and undermines attempts to eliminate gender inequalities (61). In essence, women with poor nutrition are caught in a vicious circle of poverty and malnutrition.
The effects of obesity and overweight on health outcomes are also complex and multifaceted. Overweight and obesity increase the risk in both men and women of chronic diseases such as hypertension, diabetes and is associated with a higher mortality (62, 63). Although obesity has negative health outcomes among both men and women, studies have shown that obese women are more likely to develop diabetes than obese men (64). However, obese men are more likely to develop chronic pulmonary disease and chronic kidney disease than women. Obesity also has a bidirectional relationship with mental illnesses. Individuals with a mental illness have an increased risk of obesity; and obesity is associated with psychiatric disorders including but not limited to mood disorders, anxiety, and personality disorders (65). The association of obesity and depression can be particularly significant among women (66).
Policy implications
This perspective piece summarized the malnutrition chapter of the WHO’s regional report on gender and health in the EMR (16). This paper is among the first of its kind to utilize a gender-analysis of nutrition disparities across the Region. Given the timeframe of the original report, it is unfortunate that some articles may have been missed for this piece. The limited availability of age and sex-disaggregated data, along with limited gender-analyzes, is another limitation affecting the understanding of the root-causes behind the epidemiological trends and overall health disparities across the Region (5, 10, 16). Nevertheless, on the basis of the solid findings featured in this manuscript, policymakers and practitioners alike would benefit from the below recommendations.
Given the co-existence of under and over-nutrition in countries of the Region, and even within households, policies and nutrition interventions should target specific age and gender groups (16). At the same time, efforts are needed to improve the overall quality of household diets ensuring that all members have access to healthy foods. Improving water and sanitation infrastructure and supporting women to exclusively breast-feed babies would go a long way in not only promoting health and well-being but also reducing underweight and stunting among children and addressing the intergenerational cycle of malnutrition (16). However, a much stronger region-specific evidence base is critical in identifying the most appropriate combination of interventions and policies that would successfully address gender and malnutrition in the EMR. As reflected in the regional gender and health report, routine gender analysis and in-depth understanding of gender differences in dietary habits and their determinants can guide the development of gender-sensitive nutrition policies and culturally acceptable health services. A gendered approach to food security during conflict is also necessary to address malnutrition issues (16).
Because of their triple productive, reproductive, and social roles, poor female nutrition can have substantial effects on our community. Malnutrition among women negatively affects women’s learning potential and productivity and increases reproductive, maternal and children’s health risks. It is hence of primary importance to identify means of eliminating relevant gender inequalities. (9, 26). Addressing gender discrimination and power inequalities can improve women’s status including her own nutritional status and that of their children (16). Recommendations to address gender inequalities include working toward a paradigm shift to eradicate the structural obstacles underlying the problem in the region (16). A comprehensive and multilevel approach to confront the power dynamics underpinning gender inequities in the various socio-cultural systems is much needed (67).
Conclusion
Malnutrition in the EMR is a leading health issue resulting in various health inequalities. This review described the interaction between gender and malnutrition and identified the serious impact of gendered systems and norms on malnutrition in the EMR. Gender norms and stereotypes as well as gender-based inequalities have been associated with a higher prevalence of food insecurity, undernutrition, micronutrient deficiencies and obesity, and have contributed to worse health outcomes, with differing manifestations for both men and women. The gender dimension in malnutrition intersects with individual determinants such as lack of education, unemployment, and low income as well as structural determinants such as culture, socio-economic factors, and political stability. It is therefore of primary importance to address malnutrition from a gender perspective. An intersectoral, multi-level, gender-sensitive approach is needed to reduce the impact of malnutrition and address gender-related health inequalities in the EMR.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
AA-J, ME-A, JJ, MK, RM, AR, and HS: conceptualization. JJ, MK, RM, AR, and HS: methodology. JJ, MK, RM, AR, and HS: investigation. JJ, MK, RM, AR, and HS: writing–original draft preparation and writing–review and editing. All authors have read and agreed to the published version of the manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Popkin, BM, Corvalan, C, and Grummer-Strawn, LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. (2020) 395:65–74. doi: 10.1016/S0140-6736(19)32497-3
2. The World Health Organization. Build Back Fairer: Achieving Health Equity in the Eastern Mediterranean Region: Report of the Commission on Social Determinants of Health in the Eastern Mediterranean Region-executive Summary. Geneva, World Health Organization: (2022).
3. The World Bank. World Bank Country and Lending Groups, Country Classification. Washington, DC: The World Bank (2022).
4. Hwalla, N, Al Dhaheri, AS, Radwan, H, Alfawaz, HA, Fouda, MA, Al-Daghri, NM, et al. The prevalence of micronutrient deficiencies and inadequacies in the Middle East and approaches to interventions. Nutrients. (2017) 9:229. doi: 10.3390/nu9030229
5. The World Health Organization. Health and Well-being Profile of the Eastern Mediterranean Region: An Overview of the Health Situation in the Region and its Countries in. Geneva: World Health Organization (2020).
6. Ghattas, H, Jamaluddine, Z, and Akik, C. Double burden of malnutrition in children and adolescents in the Arab region. Lancet Child Adolesc Health. (2021) 5:462–4. doi: 10.1016/S2352-4642(21)00162-0
7. Nasreddine, L, Ayoub, JJ, and Al Jawaldeh, A. Review of the nutrition situation in the eastern Mediterranean region. East Mediterr Health J. (2018) 24:77–91. doi: 10.26719/2018.24.1.77
8. Traissac, P, El Ati, J, Gartner, A, Gharbia, HB, and Delpeuch, F. Gender inequalities in excess adiposity and anaemia combine in a large double burden of malnutrition gap detrimental to women in an urban area in North Africa. Public Health Nutr. (2016) 19:1428–37. doi: 10.1017/S1368980016000689
9. Hansford, F. The nutrition transition: a gender perspective with reference to Brazil. Gend Dev. (2010) 18:439–52. doi: 10.1080/13552074.2010.521990
10. Al-Shammari, N, and Al Rakhis, M. Impact of gender inequality on economic growth in the Arab region. Research. Appl Econ. (2017) 9:18–31. doi: 10.3389/fpubh.2016.00033
11. Marphatia, AA, Cole, TJ, Grijalva-Eternod, C, and Wells, JC. Associations of gender inequality with child malnutrition and mortality across 96 countries. Glob Health Epidemiol Genomics. (2016) 1:e6. doi: 10.1017/gheg.2016.1
12. Akseer, N, Tasic, H, Onah, MN, Wigle, J, Rajakumar, R, Sanchez-Hernandez, D, et al. Economic costs of childhood stunting to the private sector in low-and middle-income countries. EClinicalMedicine. (2022) 45:101320. doi: 10.1016/j.eclinm.2022.101320
13. United Nations Development Programme. Gender Development Index (GDI). Human Development Reports. New York: United Nations Development Programme (2020).
14. Equitas. Gender and Sexual Identity Lexicon. Montreal, Canada: International Centre for Human Rights Education (2017).
15. Sen, G., George, A., Ostlin, P., and Ramos, S. Unequal, Unfair, Ineffective and Inefficient Gender Inequity in Health: Why it Exists and how we can Change it. (2007).
16. The World Health Organization. Gender and Health in the Eastern Mediterranean Region. Geneva: World Health Organization.
17. Food and Agriculture Organization. The Food and Agriculture Organization of the United Nations, Gender, Food Security and Nutrition in Protracted Crises. Rome, Italy: Food and Agriculture Organization (2016).
18. Aboul Enein, BH, Bernstein, J, and Neary, A. Dietary transition and obesity in selected Arabic-speaking countries: a review of the current evidence. East Mediterr Health J. (2016) 22:763–70. doi: 10.26719/2016.22.10.763
19. Food and Agriculture Organization. The Food and Agriculture Organization of the United Nations, Yemen Famine Prevention Plan January-June Contributing to Improved Food Security and Nutrition. Rome: Food and Agriculture Organization (2019).
20. The World Health Organization. Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030. Geneva: World Health Organization (2019).
21. Elrayah, EE, Rogers, L, Doggui, R, and Al-Jawaldeh, A. Vitamin D insufficiency and deficiency in the eastern Mediterranean region (EMR)–misconceptions in public health practice: a scoping review 2019-2020. J Nutr Sci Vitaminol. (2020) 66:389–95. doi: 10.3177/jnsv.66.389
22. Lips, P, Cashman, KD, Lamberg-Allardt, C, Bischoff-Ferrari, HA, Obermayer-Pietsch, B, Bianchi, ML, et al. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency: a position statement of the European calcified tissue society. Eur J Endocrinol. (2019) 180:P23–54. doi: 10.1530/EJE-18-0736
23. Husain, NE, Badie Suliman, AA, Abdelrahman, I, Bedri, SA, Musa, RM, Osman, HE, et al. Vitamin D level and its determinants among Sudanese women: does it matter in a sunshine African country? J family med. Prim Care. (2019) 8:2389–94. doi: 10.4103/jfmpc.jfmpc_247_19
24. The World Health Organization. BMI In: TGH Observatory, editor. Nutrition. Geneva: World Health Organization (2022)
25. The World Health Organization. Regional Office for the Eastern, Strategy on Nutrition for the Eastern Mediterranean Region 2020–2030. Cairo: World Health Organization. Regional Office for the Eastern Mediterranean (2019).
26. International Accounting Standards Committee. The Gender Handbook for Humanitarian Action International Accounting Standards Committee (2017).
27. The World. Food Programme, Support for Food Security and Nutrition for Conflict-Affected and Chronically Vulnerable Populations Standard Project Report. (2016).
28. Ibnouf, FO. Challenges and possibilities for achieving household food security in the Western Sudan region: the role of female farmers. Food Secur. (2011) 3:215–31. doi: 10.1007/s12571-011-0118-3
29. Food and Agriculture Organization. The Food and Agriculture Organization of the United Nations, Gender, Food Security and Nutrition in Protracted Crises. Women and Girls as Agents of Resilience. Rome, Italy: Food and Agriculture Organization (2016).
30. Hwalla, N, Weaver, CM, Mekary, RA, and El Labban, S. Public health nutrition in the Middle East. Front Public Health. (2016) 4:33. doi: 10.3389/fpubh.2016.00033
31. O’Neil, A, Scovelle, AJ, Milner, AJ, and Kavanagh, A. Gender/sex as a social determinant of cardiovascular risk. Circulation. (2018) 137:854–64. doi: 10.1161/CIRCULATIONAHA.117.028595
32. Christen, T, Trompet, S, Noordam, R, van Klinken, JB, van Dijk, KW, Lamb, HJ, et al. Sex differences in body fat distribution are related to sex differences in serum leptin and adiponectin. Peptides. (2018) 107:25–31. doi: 10.1016/j.peptides.2018.07.008
33. Palmer, BF, and Clegg, DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. (2015) 402:113–9. doi: 10.1016/j.mce.2014.11.029
34. Schmidt, M, Johannesdottir, SA, Lemeshow, S, Lash, TL, Ulrichsen, SP, Bøtker, HE, et al. Obesity in young men, and individual and combined risks of type 2 diabetes, cardiovascular morbidity and death before 55 years of age: a Danish 33-year follow-up study. BMJ Open. (2013) 3:e002698. doi: 10.1136/bmjopen-2013-002698
35. Musaiger, AO. Overweight and obesity in eastern mediterranean region: prevalence and possible causes. J Obes. (2011) 2011:1–17. doi: 10.1155/2011/407237
36. Shafqat, N, Manzoor, S, and Abbasi, S. Relationship of sociodemographic factors with malnutrition in preschool children: a community based study. Pak J Med Res. (2013) 52:120–5.
37. Chakhtoura, M, Rahme, M, Chamoun, N, and Fuleihan, GE-H. Vitamin D in the middle east and North Africa. Bone Rep. (2018) 8:135–46. doi: 10.1016/j.bonr.2018.03.004
38. Vatandost, S, Jahani, M, Afshari, A, Amiri, MR, Heidarimoghadam, R, and Mohammadi, Y. Prevalence of vitamin D deficiency in Iran: a systematic review and meta-analysis. Nutr Health. (2018) 24:269–78. doi: 10.1177/0260106018802968
39. El Rifai, NM, Abdel Moety, GAF, Gaafar, HM, and Hamed, DA. Vitamin D deficiency in Egyptian mothers and their neonates and possible related factors. J Matern Fetal Neonatal Med. (2014) 27:1064–8. doi: 10.3109/14767058.2013.849240
40. El Koumi, MA, Ali, YF, and Abd El Rahman, RN. Impact of maternal vitamin D status during pregnancy on neonatal vitamin D status. Turk J Pediatr. (2013) 55:371–7.
41. Saadi, HF, Nagelkerke, N, Benedict, S, Qazaq, HS, Zilahi, E, Mohamadiyeh, MK, et al. Predictors and relationships of serum 25 hydroxyvitamin D concentration with bone turnover markers, bone mineral density, and vitamin D receptor genotype in Emirati women. Bone. (2006) 39:1136–43. doi: 10.1016/j.bone.2006.05.010
42. Al Attia, HM, and Ibrahim, MA. The high prevalence of vitamin D inadequacy and dress style of women in the sunny UAE. Arch Osteoporos. (2012) 7:307–10. doi: 10.1007/s11657-012-0104-1
43. Batieha, A, Khader, Y, Jaddou, H, Hyassat, D, Batieha, Z, Khateeb, M, et al. Vitamin D status in Jordan: dress style and gender discrepancies. Ann Nutr Metab. (2011) 58:10–8. doi: 10.1159/000323097
44. Alzaheb, RA. The prevalence of hypovitaminosis D and its associated risk factors among women of reproductive age in Saudi Arabia: a systematic review and meta-analysis. Clinical medicine insights. Womens Health. (2018) 11:18767884. doi: 10.1177/1179562X18767884
45. Hajiahmadi, M, Shafi, H, and Delavar, MA. Impact of parity on obesity: a cross-sectional study in Iranian women. Med Princ Pract. (2015) 24:70–4. doi: 10.1159/000368358
46. The Global Burden of Disease. Burden of Obesity in the Eastern Mediterranean Region: Findings from the Global Burden of Disease 2015 Study. Int J Public Health. (2018) 63:165–76. doi: 10.1007/s00038-017-1002-5
47. World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Geneva: World Health Organization (2019).
48. The World Health Organization In: World Health Organization, editor. Promoting Physical Activity in the Eastern Mediterranean Region through a Life-course Approach. Geneva: (2014)
49. Alshaikh, MK, Filippidis, FT, Al-Omar, HA, Rawaf, S, Majeed, A, and Salmasi, A-M. The ticking time bomb in lifestyle-related diseases among women in the Gulf cooperation council countries; review of systematic reviews. BMC Public Health. (2017) 17:1–17. doi: 10.1186/s12889-017-4331-7
50. Abbasi, F, Hejazi, E, and Hakimzade, R. Lived experience of elementary school teachers about the opportunities and challenges of teaching in the educational network of students (SHAD): a phenomenological study. J Res Teach. (2020) 8:1–24.
51. Sharkas, GF, Saheb, T, Arqoub, K, and Haddadin, R. Sedentary lifestyle among adults in Jordan. Family Med Community Health. (2007) 4:4–8. doi: 10.15212/FMCH.2015.0148
52. Guthold, R, Stevens, GA, Riley, LM, and Bull, FC. Worldwide trends in insufficient physical activity from 2001 to 2016: a pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob Health. (2018) 6:e1077–86. doi: 10.1016/S2214-109X(18)30357-7
53. Mabry, R, Koohsari, MJ, Bull, F, and Owen, N. A systematic review of physical activity and sedentary behaviour research in the oil-producing countries of the Arabian Peninsula. BMC Public Health. (2016) 16:1–22. doi: 10.1186/s12889-016-3642-4
54. Selim, M., Abdel-Tawab, N.G., El Sayed, K., Elbadawy, A., and El Kalaawy, H. The Ishraq Program for out-of-School Girls: From Pilot to Scale-up. (2013).
55. Mumtaz, S, Bahk, J, and Khang, Y-H. Current status and determinants of maternal healthcare utilization in Afghanistan: analysis from Afghanistan demographic and health survey 2015. PLoS One. (2019) 14:e0217827. doi: 10.1371/journal.pone.0217827
56. Alyahya, MS, Khader, YS, Batieha, A, and Asad, M. The quality of maternal-fetal and newborn care services in Jordan: a qualitative focus group study. BMC Health Serv Res. (2019) 19:1–16. doi: 10.1186/s12913-018-3827-x
57. Farrag, NS, Cheskin, LJ, and Farag, MK. A systematic review of childhood obesity in the Middle East and North Africa (MENA) region: prevalence and risk factors meta-analysis. Adv Pediatr Res. (2017) 4:8. doi: 10.12715/apr.2017.4.8
58. Habibi, M, Laamiri, FZ, Aguenaou, H, Doukkali, L, Mrabet, M, and Barkat, A. The impact of maternal socio-demographic characteristics on breastfeeding knowledge and practices: an experience from Casablanca, Morocco. Int J Pediatr Adolesc Med. (2018) 5:39–48. doi: 10.1016/j.ijpam.2018.01.003
59. Oniango, R., and Mukudi, E., Nutrition and Gender: A Foundation for Development. Geneva. ACC/SCN. (2002), pp. 18–23.
60. Blossner, M, De Onis, M, and Prüss-Üstün, A. Malnutrition: Quantifying the Health Impact at National and Local Levels. Geneva: World Health Organization (2005).
61. The United Nations Economic and Social Commission for Western Asia. Gender Justice and Equality before the law: Analysis of Progress and Challenges in the Arab States Region. Beirut, Lebanon: The United Nations Economic and Social Commission for Western Asia (2018).
62. Csige, I, Ujvárosy, D, Szabó, Z, Lőrincz, I, Paragh, G, Harangi, M, et al. The impact of obesity on the cardiovascular system. J Diabetes Res. (2018) 2018:3407306. doi: 10.1155/2018/3407306
63. Turer, CB, Brady, TM, and De Ferranti, SD. Obesity, hypertension, and dyslipidemia in childhood are key modifiable antecedents of adult cardiovascular disease: a call to action. Am Heart Assoc. (2018) 137:1256–9. doi: 10.1161/CIRCULATIONAHA.118.032531
64. Huebschmann, AG, Huxley, RR, Kohrt, WM, Zeitler, P, Regensteiner, JG, and Reusch, JEB. Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia. (2019) 62:1761–72. doi: 10.1007/s00125-019-4939-5
65. Avila, C, Holloway, AC, Hahn, MK, Morrison, KM, Restivo, M, Anglin, R, et al. An overview of links between obesity and mental health. Curr Obes Rep. (2015) 4:303–10. doi: 10.1007/s13679-015-0164-9
66. Pereira-Miranda, E, Costa, PR, Queiroz, VA, Pereira-Santos, M, and Santana, ML. Overweight and obesity associated with higher depression prevalence in adults: a systematic review and meta-analysis. J Am Coll Nutr. (2017) 36:223–33. doi: 10.1080/07315724.2016.1261053
Keywords: malnutrition, inequity, gender disparities, Eastern Mediterranean Region, obesity, wasting (malnutrition)
Citation: Jabbour J, Khalil M, Ronzoni AR, Mabry R, Al-Jawaldeh A, El-Adawy M and Sakr H (2023) Malnutrition and gender disparities in the Eastern Mediterranean Region: The need for action. Front. Nutr. 10:1113662. doi: 10.3389/fnut.2023.1113662
Edited by:
Ahmed Mohammed Alwan, Mashhad University of Medical Sciences, IranReviewed by:
Hasanain A. J. Gharban, University of Wasit, IraqHasaneen Kudhair Albadry, Alkut College University, Iraq
Razieh Anari, National Nutrition and Food Technology Research Institute, Iran
Copyright © 2023 Jabbour, Khalil, Ronzoni, Mabry, Al-Jawaldeh, El-Adawy and Sakr. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jana Jabbour, amFuYS5qYWJib3VyQGxhdS5lZHUubGI=
†These authors contributed equally to this work and share first authorship
‡These authors share senior authorship
§ORCID: Jana Jabbour https://orcid.org/0000-0002-0576-1031
Ayoub Al-Jawaldeh https://orcid.org/0000-0001-7387-8277
 Jana Jabbour
Jana Jabbour Merette Khalil2†
Merette Khalil2† Ruth Mabry
Ruth Mabry Ayoub Al-Jawaldeh
Ayoub Al-Jawaldeh Maha El-Adawy
Maha El-Adawy