- 1Department of Gastroenterology, Xiyuan Hospital, China Academy of Chinese Medical Sciences, Beijing, China
- 2Department of Chinese Medicine, Eye Hospital, China Academy of Chinese Medical Sciences, Beijing, China
Background: Nigella sativa (N. sativa) consumption has been associated with various health outcomes; however, the results are not completely consistent.
Objectives: This overview of systematic reviews and meta-analyses aimed to evaluate the reporting and methodological quality, and to grade the available evidence of associations between N. sativa and health outcomes.
Methods: PubMed, Cochrane Library, Embase, and Scopus databases were searched from their inception to September 30, 2022. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 statement, Assessment of Multiple Systematic Reviews (AMSTAR) 2 checklist, and Grades of Recommendations, Assessment, Development and Evaluations (GRADE) systems were used to assess the reporting, methodological, and evidence quality for each meta-analysis, respectively. The results were synthesized in a narrative form.
Results: This overview included 20 eligible meta-analyses published in peer-reviewed journals between 2013 and 2021. The overall methodological quality was relatively poor, with only one moderate quality, four low quality, and 15 critically low quality studies. For reporting quality, items two, five, eight, nine, 15, and 24 need to improve. Among the 110 outcome indicators of the quality of evidence, five were graded as moderate, 17 as low, and 88 as very low. Risk of bias, inconsistency, and imprecision were the main downgrading factors.
Conclusion: This overview suggests that N. sativa is beneficial for various clinical outcomes. However, there are certain limitations to reporting and methodological quality. The clinical efficacy of N. sativa requires confirmation in high-quality, large-sample, randomized controlled trials.
1. Introduction
Nigella sativa (N. sativa) is an annual flowering plant of the Ranunculaceae family that grows widely in Middle Eastern and European countries (1). It has been used as a functional food, health product and medicine for thousands of years, suggesting that it may have some potential benefits for people (2–4). In traditional medicine, N. sativa is used for respiratory, digestive, and cardiovascular diseases, such as asthma, dyspepsia, and hypertension, and to improve liver and kidney function (5–9). Many scientific studies have demonstrated that N. sativa has a broad spectrum of positive pharmacological effects, including antiviral (10), anti-inflammatory (11), hypotensive (12), hypoglycemic (13) and antitumor (14) effects. These biological properties are related to the abundance of several phytochemicals, including thymoquinone, terpenes, saponins, flavonoids, and essential oils (8, 15). These promising active ingredients and their biological properties make N. sativa a powerful natural candidate for the prevention and control of diseases. In recent years, several meta-analyses based on randomized controlled trials (RCTs) of N. sativa have assessed its association with health outcomes. However, no review articles have evaluated the scientific quality and summarized the reported outcomes. Consequently, guidance for clinical users and physicians is limited.
Overview is a novel method for assessing the scientific quality of published systematic reviews and meta-analyses in a specific domain (16, 17). This method has been applied in many medical fields including acupuncture (18, 19), saffron (20) and dietary interventions (21). However, despite the number of systematic reviews and meta-analyses that have evaluated the association between N. sativa supplementation and health outcomes, there are no comprehensive reviews to assess the reporting and methodological quality and summarize the evidence. Therefore, the purpose of this review is to provide practical information for patients and those responsible for making treatment decisions.
2. Methods
The current overview of meta-analyses is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2009) statement (22).
2.1. Search strategy
PubMed, Embase, Scopus, and Cochrane Library databases were searched from their inception to September 30, 2022. We used the following search strategies: (“nigella sativa” or “black cumin” or “black seed” or “black caraway” or “kalonji” or “thymoquinone”) and (“systematic review” or “meta-analysis”). No language restrictions were imposed. In addition, we manually screened the reference lists of the selected studies to identify additional studies that met the criteria. The full search strategy is listed in Supplementary Table S1. First, two independent reviewers (Y.W. and Q.X.) screened the records based on the titles and abstracts after duplicates were removed. The full texts of potentially eligible records were downloaded for further evaluation. Any disagreements were resolved by consulting a third reviewer (Y.D.W.).
2.2. Inclusion and exclusion criteria
Articles were eligible if they were meta-analyses conducted using systematic reviews. Details of the inclusion criteria were as follows: (1) population: adults aged ≥18 years, with no restrictions on sex or race; (2) intervention: oral N. sativa intervention with any dose and treatment duration; (3) comparator: placebo, no treatment, or conventional therapy; (4) outcomes: any health outcomes, for example, blood glucose, serum lipids, liver function, etc.; and (5) study design: meta-analyses of RCTs. To clarify the therapeutic effects of N. sativa, studies on multiherbal interventions were excluded. Non-human studies, original studies, conference abstracts, and letters were also excluded. In addition, we excluded studies administrated by the topical use or injection, as these formulations have different compositions and mechanisms.
2.3. Data extraction
Two researchers (J.X.M. and J.X.Y.) independently extracted data, including first author, year of publication, country, sample size, number of RCTs in the meta-analysis, intervention/comparation, risk of bias assessment, reported outcomes, and safety. Any disagreements were resolved by consulting a third reviewer (Y.D.W).
2.4. Assessing the quality of included studies
2.4.1. Assessment of the reporting quality
We evaluated the reporting quality using the PRISMA 2009 statement (22). The PRISMA 2009 statement consists of 27 items in seven domains: title, abstract, introduction, methods, results, discussion, and funding. According to the reported completeness, each item was answered as “yes,” “partial yes,” or “no.”
2.4.2. Assessment of methodological quality
We evaluated the methodological quality of the included studies using the Assessment of Multiple Systematic Reviews (AMSTAR) 2 checklist (23). The AMSTAR-2 checklist consists of 16 items, and each item could be answered as “yes,” “partial yes” or “no.” The overall methodological quality of each study was then classified as “high,” “moderate,” “low” or “critically low.”
2.4.3. Grading the evidence quality
We used the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) system to assess evidence quality (24), which includes five domains: risk of bias, inconsistency, indirectness, imprecision, and publication bias. And the quality of evidence for each outcome was graded as “high,” “moderate,” “low” and “very low.”
Two researchers (X. L. and Y. B. T.) independently assessed the reporting, methodological, and quality of evidence. Any disagreements were resolved by consulting a third researcher (T.C.).
2.5. Statistical analysis
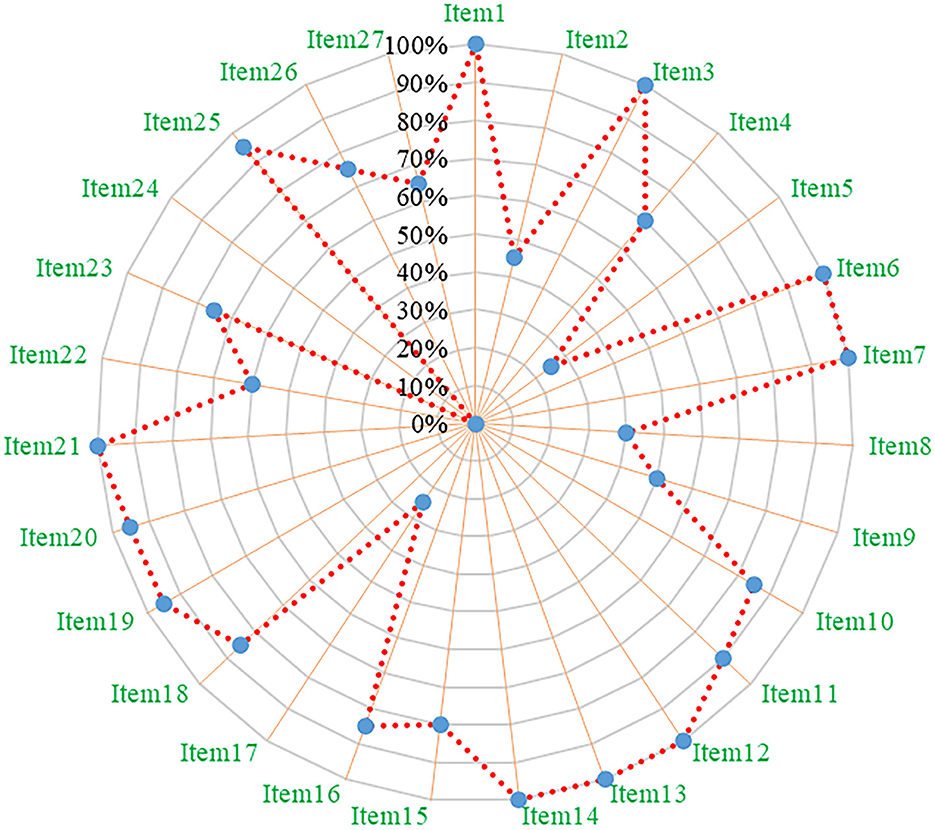
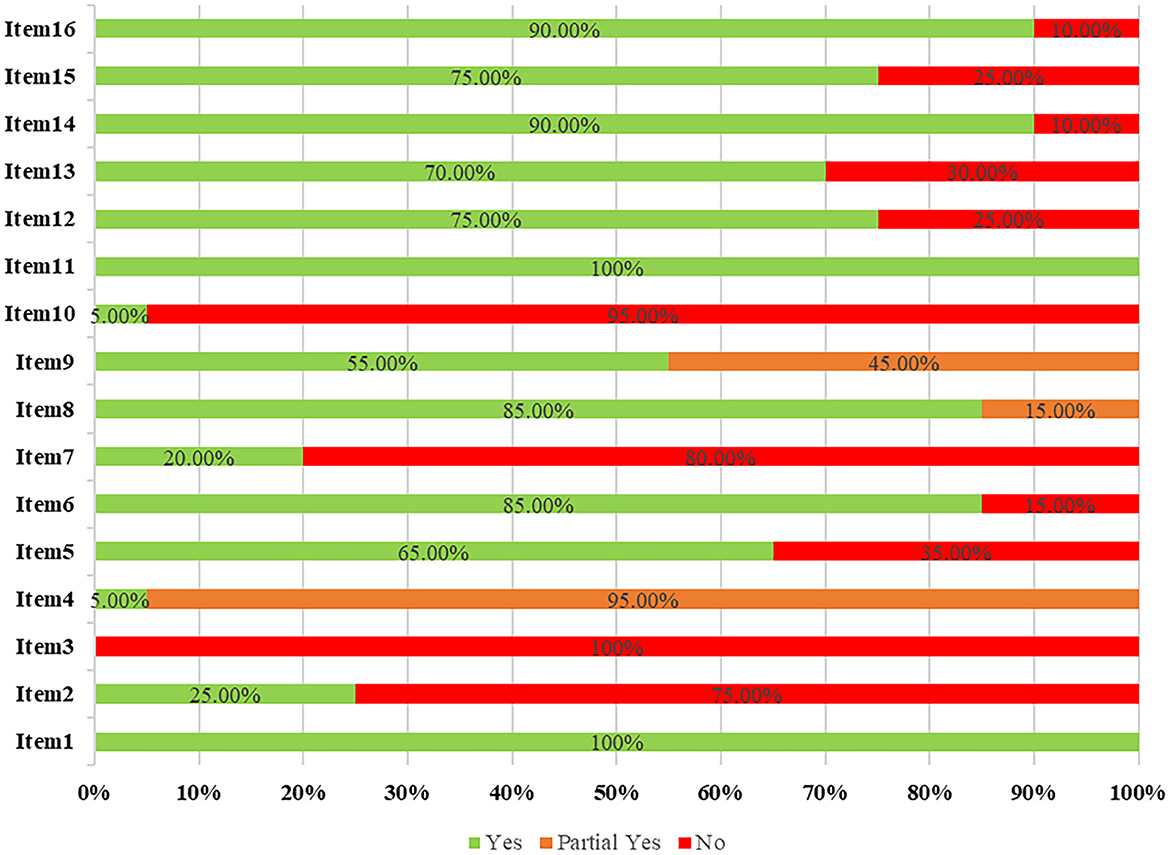
The efficacy and safety results reported in the included meta-analyses with N. sativa were synthesized in a narrative review, including risk ratio (RR), odds ratio (OR), mean difference (MD), weighted mean difference (WMD), and standard mean difference (SMD), along with P-value and a 95% confidence interval (CI). I2 was used to test for heterogeneity. In addition, we calculated compliance rates for PRISMA 2009 statement and AMSTAR 2 checklist item in meta-analyses, and reported the number and percentage of “yes,” “partial yes” or “no” responses. The reporting and methodological quality were visualized using a radar plot and bar chart, respectively. According to a previous study, a percentage of “yes” < 60% for an item indicates a need for improvement (25). Excel 2016 (Microsoft Corporation, WA, USA) was used for data analysis and visualization.
3. Results
3.1. Literature search results
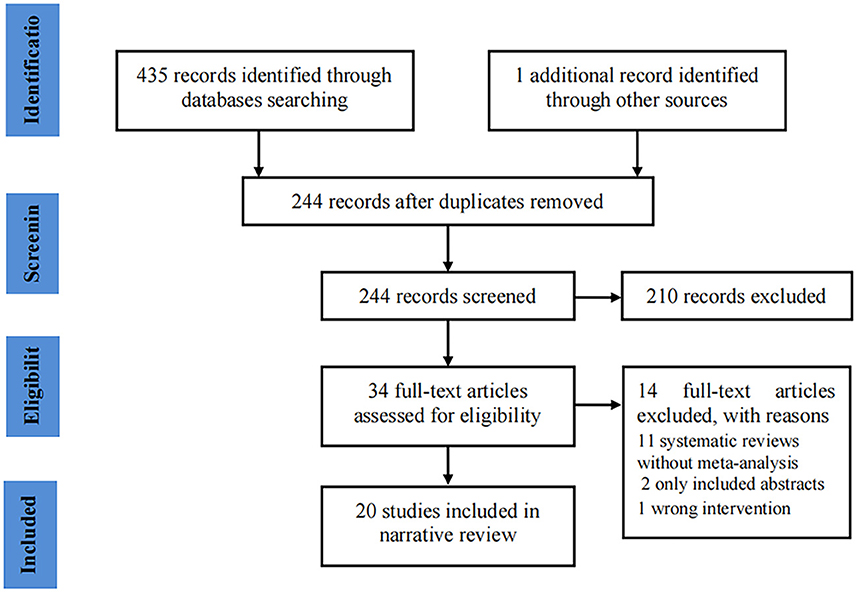
Our initial search identified 436 potential records. After removing duplicates, a total of 244 records remained. Subsequently, 210 records were excluded after screening titles and abstracts. The full texts of 34 records were further evaluated, and 20 records (26–45) were eventually included in the analysis (Figure 1 shows the flow chart of study selection).
3.2. Basic characteristics of the included literature
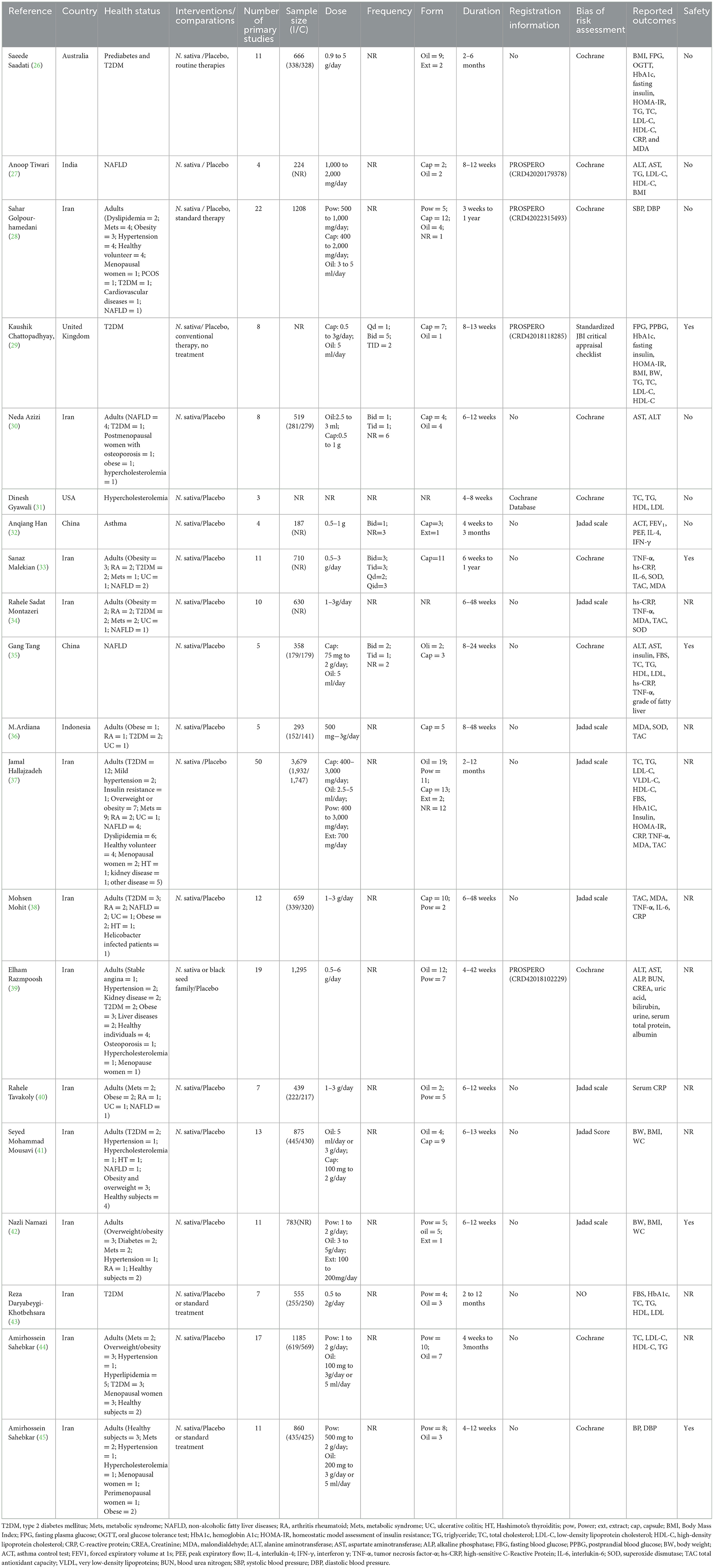
All meta-analyses were published in peer-reviewed journals between 2016 and 2022. These studies were conducted in seven regions: 13 from Iran (28, 30, 33, 34, 37–45), two from China (32, 35), and one each from Australia (26), India (27), United Kingdom (29), the USA (31), and Indonesia (36). The number of RCTs ranged from three to 50, with 187–3,679 subjects. Most studies have reported forms of N. sativa, including capsules, oils, and powders. Nineteen studies reported doses of N. sativa, ranging from 0.5 to 6 g or 2.5 to 5 ml daily (26–30, 32–45). Five studies reported the frequency of N. sativa administration, which varied between once, twice, and thrice a day (29, 32–35). The treatment duration ranged from 2 weeks to 1 year. Four studies registered protocols on the PROSER platform (27–29, 39) and one in the Cochrane library (31). In terms of the risk of bias tools, 10 studies used the Cochrane risk of bias tool (26–28, 30, 31, 33, 35, 39, 44, 45), nine studies used the Jadad scale (32, 34, 36–38, 40–43), and one used the standardized JBI critical appraisal checklist (29). Table 1 summarizes the basic characteristics of the included meta-analyses.
3.3. Results of reporting quality
According to the PRISMA 2009 statement, 20 of the 27 items had a “yes” response rate of more than 60%, indicating that the included meta-analyses contained relatively complete reporting quality. However, there were limitations related to the following items: item two (abstract: structured abstract), five (method: protocol and registration), eight (method: search), nine (method: study selection), 17 (result: study selection), 22 (result: risk of bias across studies), and 24 (discussion: summary evidence) (see Figure 2 and Supplementary Table S2).
3.4. Results of methodological quality
The results of the overall methodological quality evaluated using the AMSTAR-2 checklist revealed that only one study was of moderate quality, four studies were of low quality, and the other 15 meta-analyses were of critically low quality (Supplementary Table S3). Methodological quality limitations included the following items: item two (register protocol prior to conducting the review), three (explain selection of the study designs in the review), seven (provide a list of excluded studies and justify the exclusions), and 10 (report the source of funding for the individual studies) (see Figure 3 and Supplementary Table S3).
3.5. Results of the quality of evidence
There were 110 outcome indicators in 20 meta-analyses. Five were graded as moderate-quality, 17 as low-quality, and 88 as very-low-quality evidence. However, there is no high-quality evidence for this. The evidence was mostly downgraded owing to the risk of bias, inconsistency, and imprecision (Supplementary Table S4).
3.6. Therapeutic effect of N. sativa on health outcomes
3.6.1. Blood glucose and insulin secretion
Four studies evaluated the effects of N. sativa on glucose metabolism and insulin function (26, 29, 37, 43). All studies found that N. sativa reduced hemoglobin A1c (26, 29, 37, 43). Three studies observed that the consumption of N. sativa reduced fasting plasma glucose (FPG) levels (26, 37, 43), but one study found N. sativa had no effect on FPG in type-2 diabetes (29). In addition, N. sativa had no significant effect on the oral glucose tolerance test (OGTT) (26), fasting insulin levels (26, 29), homeostasis model assessment of insulin resistance (HOMA-IR) (26, 29, 37) and postprandial blood glucose (PPBG) (29).
3.6.2. Serum lipids
Eight studies evaluated the effects of N. sativa on lipid profiles (26, 27, 29, 31, 35, 37, 43, 45). Six studies found that N. sativa reduced total cholesterol (TC) in patients with metabolic disorders (26, 29, 31, 37, 43, 45), but one study showed that N. sativa had no effect on patients with non-alcoholic fatty liver disease (NAFLD) (35). Seven studies found that N. sativa significantly reduced triglyceride (TG) levels (27, 29, 31, 37, 45), although four studies revealed that it did not change TG levels (26, 31, 35, 43). Six studies found that N. sativa reduced low-density lipoprotein cholesterol (LDL-C) levels (26, 27, 29, 37, 43, 45), drawing consistent conclusions. Only one study showed a significant effect on high-density lipoprotein cholesterol (HDL-C) levels (27), whereas the remaining five studies found that N. sativa did not change HDL-C levels (26, 29, 31, 43, 45).
3.6.3. Blood pressure
Two studies evaluated the effects of N. sativa on blood pressure (28, 45). The results showed that N. sativa significantly reduced systolic and diastolic blood pressure in adults (28, 45).
3.6.4. Body composition
Five studies evaluated the effects of N. sativa on body parameters (26, 27, 29, 41, 42). Three studies reported that N. sativa significantly reduced body weight (BW) (29, 41, 42). Two studies observed that N. sativa significantly reduced the body mass index (BMI) (41, 42), however, three studies found no effect on BMI (26, 27, 29). One study showed that N. sativa reduced waist circumference (WC) (42), but another showed no effect on WC (41).
3.6.5. Inflammatory markers
Eight studies evaluated the effects of N. sativa on inflammatory markers (26, 32–35, 37, 38, 40). In adults, studies have observed that N. sativa intake significantly reduced tumor necrosis factor-α (TNF-α) (26, 33, 34), high-sensitivity C-reactive protein (hs-CRP) (34, 35), interleukin-6 (IL-6) (33), and C-reactive protein (CRP) (38, 40). However, other meta-analyses have shown that N. sativa supplementation had no effect on TNF-α (37, 38), hs-CRP (33), IL-6 (33), and CRP (37). In addition, one study observed that consumption N. sativa decreased interleukin-4 and increased interferon-γ in patients with asthma, but the difference was not statistically significant (32).
3.6.6. Oxidative stress factors
Six studies evaluated the effects of N. sativa on oxidative stress factors (26, 33, 34, 36–38). However, these results were contradictory. In adults, studies have shown that N. sativa reduced malondialdehyde (MDA) (26, 34, 38) and increased superoxide dismutase (SOD) (33, 34, 36) and total antioxidant capacity (TAC) (33, 34, 38). The remaining meta-analyses found that N. sativa had no significant effects on MDA (33, 36, 37) and TAC (36, 37).
3.6.7. Asthma
One study evaluated the effects of N. sativa on asthma (32). The results showed that N. sativa supplementation improved asthma control test scores and forced expiratory volume at 1s in patients with asthma, however, it had no significant effect on peak expiratory flow (32).
3.6.8. Liver and kidney parameters
Four studies evaluated the effects of N. sativa on liver parameters (27, 30, 35, 39) and one study evaluated kidney parameters (30). One study found that N. sativa significantly improves fatty liver grading in patients with NAFLD (35). Three studies reported that N. sativa reduced aspartate aminotransferase (AST) levels (27, 30, 35). However, one study reported that N. sativa failed to reduce AST levels (39). Two studies found N. sativa reduced alanine aminotransferase (ALT) levels (27, 35), whereas two other studies found N. sativa had no effect on ALT levels (30, 39). In addition, one study observed that the use of N. sativa significantly reduced the alkaline phosphatase levels (39). In terms of kidney parameters, N. sativa significantly reduced urea nitrogen, but had no effect on creatinine, bilirubin, and uric acid levels (30).
3.6.9. Safety
Five meta-analyses reported adverse events (29, 33, 35, 42, 45). The main adverse events were digestive symptoms such as stomach pain, diarrhea, nausea, and vomiting, as well as weakness and weight loss. However, no study has reported serious adverse events.
4. Discussion
In recent years, plant-based foods and herbs as therapeutic alternatives, have received a great deal of attention from both researchers and the general public (46, 47). Medicinal plants can be used for the treatment and prevention of various non-communicable diseases because they contain a wide range of bioactive phytochemicals and have different metabolic effects (48, 49). This is the first overview to synthesize the available meta-analyses for N. sativa and evaluate the reporting, methodological, and evidence quality. We found that N. sativa has a variety of potential effects on different indicators in clinical practice, including blood glucose, inflammatory markers, oxidative stress factors, serum lipids, blood pressure, liver and kidney parameters, and even asthma indicators. The therapeutic effects suggested that N. sativa has beneficial effects in various diseases and may be a promising complementary and alternative therapy.
The overall reporting quality of the meta-analyses was poor, highlighting the importance of future reviews to improve the standards. Regarding the PRISMA 2009 statement, items two, five, eight, nine, 17, 22, and 24 need significant improvement. In recent years, the problem of reproducibility and the waste of resources in biomedical research have caused considerable concern in the scientific community (50, 51). However, comprehensive and transparent reporting of the study design, study process, and final outcomes is key to avoiding these problems. Therefore, we strongly recommend that future meta-analyses of N. sativa should be performed in accordance with the PRISMA statement.
In terms of methodological quality, we found that items two, three, seven and 10 should be improved based on the AMSTAR-2 checklist. The registration of protocols can improve the transparency and help avoid the potential risk of bias (52, 53). It can also reduce duplicate work between different research groups and continue studies to date (54). The authors are encouraged to register their protocols in free and open databases, such as the PROSPERO platform and Cochrane Library, to avoid study bias (55). The AMSTAR-2 checklist requires review authors to explain why they chose a particular study design for meta-analysis (23), as systematic reviews should be “comprehensive” and specific study designs should be selected for different purposes. Furthermore, a comprehensive literature search strategy is the basis and a guarantee of meta-analysis. This helps to avoid missing data, leading to selective bias and obtaining the correct conclusions (56). In addition, the authors are required provide a full list of excluded studies and justify their exclusions, which can help the readers judge the extent of study inclusion and the accuracy of manuscript selection. Finally, the authors should clearly report a statement about funding sources and conflicts of interest. This can help other researchers judge the reliability of the conclusion and prevent bias that might favor funders (57). For example, authors may present favorable results and/or exaggerate the effects of drugs provided by industry funders (58). Therefore, the use of rigorous methodology reduces the risk of bias and improves the reliability of the conclusions.
The findings from the included meta-analyses suggested that N. sativa has potential efficacy in treating various diseases. However, according to the GRADE system, we found only five moderate quality, 17 low quality, and 88 very low quality studies, with an overall poor quality of evidence. The highest downgrading factor was the risk of bias. This was mainly due to RCTs with unclear or missing randomization, blinding, and allocation concealment. Therefore, in future studies, designers should pay more attention to the design and implementation processes. Another downgrading factor was inconsistency, with most studies showing high heterogeneity (I2 > 50%). This may be related to the different subjects, multiple forms of N. sativa supplements, and treatment duration. Future meta-analyses should explore potential heterogeneity based on subgroup, meta-regression, and sensitivity analyses. It is important for researchers to report in detail on the bioactive constituents of N. sativa and to transparently report on the N. sativa species, the dose and frequency of intervention administration, treatment duration, and adherence. Although most meta-analyses have provided certainty about the clinical efficacy of N. sativa, the overall sample size was low, suggesting that there remains a need for clinical evidence from high-quality, large-sample RCTs.
4.1. Strengths and limitations
This overview has several strengths and limitations. Regarding the strengths, this is the first overview to comprehensively summarize the clinical evidence of N. sativa supplementation and provide visualization of reporting and methodological quality. The results make up the knowledge gap regarding N. sativa supplements and can be used to guide further research and clinical decision-making. This study has several limitations. First, this overview only used a descriptive method, making it difficult to evaluate primary studies. Second, although two researchers who have been trained and passed the pre-test, independently conducted literature screening and quality evaluation, subjective factors cannot be eliminated and may affect objectivity. Third, because most studies did not mention adverse events, it is difficult to accurately assess the safety of N. sativa in clinical practice.
5. Conclusion
This overview suggests that N. sativa has the potential to improve different clinical outcomes, such as blood glucose, inflammatory markers, oxidative stress factors, serum lipids, blood pressure, liver and kidney parameters, and even asthma indicators. However, there are certain limitations in reporting and methodological quality, and future studies should improve the administration process. In addition, the clinical efficacy of N. sativa needs to be confirmed in high-quality, large-sample RCTs to generate more evidence-based clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
ZL designed and drafted the manuscript. YW, QX, JM, JY, XL, and YT performed the literature search, extracted the data, and assessed their quality. ZL, TC, and YW analyzed and interpreted the data. All the authors participated in this study and reviewed and agreed to publish this article.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82074420) and Scientific and Technological Innovation Project of the China Academy of Chinese Medical Sciences (CI2021A01005).
Acknowledgments
We would like to thank all authors who contributed to this review.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1107750/full#supplementary-material
References
1. Kooti W, Hasanzadeh-Noohi Z, Sharafi-Ahvazi N, Asadi-Samani M, Ashtary-Larky D. Phytochemistry, Pharmacology, and Therapeutic Uses of Black Seed (Nigella Sativa). Chin J Nat Med. (2016) 14:732–45. doi: 10.1016/S1875-5364(16)30088-7
2. Yimer EM, Tuem KB, Karim A, Ur-Rehman N, Anwar FL. Black cumin: a promising natural remedy for wide range of illnesses. Evid Based Complement Alternat Med. (2019) 2019:1528635. doi: 10.1155/2019/1528635
3. Niu Y, Wang B, Zhou L, Ma C, Waterhouse GIN, Liu Z, et al. A dietary supplement as an immune-modulator on the basis of bioactive components. Front Nutr. (2021) 8:722813. doi: 10.3389/fnut.2021.722813
4. Rahim MA, Shoukat A, Khalid W, Ejaz A, Itrat N, Majeed I, et al. A narrative review on various oil extraction methods, encapsulation processes, fatty acid profiles, oxidative stability, and medicinal properties of black seed (Nigella Sativa). Foods. (2022) 11:2826. doi: 10.3390/foods11182826
5. Saadat S, Aslani MR, Ghorani V, Keyhanmanesh R, Boskabady MH. The effects of Nigella Sativa on respiratory, allergic and immunologic disorders, evidence from experimental and clinical studies, a comprehensive and updated review. Phytother Res. (2021) 35:2968–96. doi: 10.1002/ptr.7003
6. Shoaei-Hagh P, Kamelan Kafi F, Najafi S, Zamanzadeh M, Heidari Bakavoli A, Ramezani J, et al. A randomized, double-blind, placebo-controlled, clinical trial to evaluate the benefits of nigella sativa seeds oil in reducing cardiovascular risks in hypertensive patients. Phytother Res. (2021) 35:4388–400. doi: 10.1002/ptr.7140
7. Gholamnezhad Z, Shakeri F, Saadat S, Ghorani V, Boskabady MH. Clinical and experimental effects of Nigella Sativa and its constituents on respiratory and allergic disorders. Avicenna J Phytomed. (2019) 9:195–212.
8. Anaeigoudari A, Safari H, Khazdair MR. Effects of Nigella Sativa, Camellia Sinensis, and Allium Sativum as food additives on metabolic disorders, a literature review. Front Pharmacol. (2021) 12:762182. doi: 10.3389/fphar.2021.762182
9. Razmpoosh E, Mirzavandi F, Sadeghi N, Safi S, Abdollahi N, Nadjarzadeh A, et al. The effect of Nigella Sativa on cardio-metabolic parameters: a protocol for a systematic review and meta-analysis. J Nutr Food Secur. (2022) 7:248–55. doi: 10.18502/jnfs.v7i2.9339
10. Esharkawy ER, Almalki F, Hadda TB. In Vitro potential antiviral Sars-Cov-19- activity of natural product thymohydroquinone and dithymoquinone from Nigella Sativa. Bioorg Chem. (2022) 120:105587. doi: 10.1016/j.bioorg.2021.105587
11. Mokhtari-Zaer A, Norouzi F, Askari VR, Khazdair MR, Roshan NM, Boskabady M, et al. The protective effect of Nigella Sativa extract on lung inflammation and oxidative stress induced by lipopolysaccharide in rats. J Ethnopharmacol. (2020) 253:112653. doi: 10.1016/j.jep.2020.112653
12. Enayatfard L, Mohebbati R, Niazmand S, Hosseini M, Shafei MN. The standardized extract of Nigella Sativa and its major ingredient, thymoquinone, ameliorates angiotensin ii-induced hypertension in rats. J Basic Clin Physiol Pharmacol. (2018) 30:51–8. doi: 10.1515/jbcpp-2018-0074
13. Tiji S, Bouhrim M, Addi M, Drouet S, Lorenzo JM, Hano C, et al. Linking the phytochemicals and the α-glucosidase and α-amylase enzyme inhibitory effects of seed extracts. Foods. (2021) 10:1818. doi: 10.3390/foods10081818
14. Shanmugam MK, Arfuso F, Kumar AP, Wang L, Goh BC, Ahn KS, et al. Modulation of diverse oncogenic transcription factors by thymoquinone, an essential oil compound isolated from the seeds of Nigella Sativa linn. Pharmacol Res. (2018) 129:357–64. doi: 10.1016/j.phrs.2017.11.023
15. Ahmad MF, Ahmad FA, Ashraf SA, Saad HH, Wahab S, Khan MI, et al. An updated knowledge of black seed (Nigella Sativa Linn): review of phytochemical constituents and pharmacological properties. J Herb Med. (2021) 25:100404. doi: 10.1016/j.hermed.2020.100404
16. Gates A, Gates M, Duarte G, Cary M, Becker M, Prediger B, et al. Evaluation of the reliability, usability, and applicability of amstar, amstar 2, and robis: protocol for a descriptive analytic study. Syst Rev. (2018) 7:85. doi: 10.1186/s13643-018-0746-1
17. Pollock M, Fernandes RM, Hartling L. Evaluation of amstar to assess the methodological quality of systematic reviews in overviews of reviews of healthcare interventions. BMC Med Res Methodol. (2017) 17:48. doi: 10.1186/s12874-017-0325-5
18. Lu T-T, Lu C-C, Li M-X, Ke L-X, Cai H, Yang K-H. Reporting and methodological quality of meta-analyses of acupuncture for patients with migraine: a methodological investigation with evidence map. J Integr Med. (2022) 20:213–20. doi: 10.1016/j.joim.2022.02.003
19. Choi T-Y, Ang L, Jun JH, Alraek T, Lee MS. Acupuncture and moxibustion for cancer-related fatigue: an overview of systematic reviews and meta-analysis. Cancers. (2022) 14:2347. doi: 10.3390/cancers14102347
20. Sadigi B, Yarani R, Mirghafourvand M, Travica N, Yousefi Z, Shakouri SK, et al. The effect of saffron supplementation on glycemic parameters: an overview of systematic reviews. Phytother Res. (2022) 36:3444–58. doi: 10.1002/ptr.7542
21. Ruan Y, Chen L, She D, Chung Y, Ge L, Han L. Ketogenic diet for epilepsy: an overview of systematic review and meta-analysis. Eur J Clin Nutr. (2022) 76:1234–44. doi: 10.1038/s41430-021-01060-8
22. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the prisma statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
23. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. Amstar 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. (2017) 358:j4008. doi: 10.1136/bmj.j4008
24. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. Grade guidelines: 1. introduction-grade evidence profiles and summary of findings tables. J Clin Epidemiol. (2011) 64:383–94. doi: 10.1016/j.jclinepi.2010.04.026
25. Lu C, Wu S, Ke L, Liu F, Shang W, Deng X, et al. Kanglaite (Coix Seed Extract) as adjunctive therapy in cancer: evidence mapping overview based on systematic reviews with meta-analyses. Front Pharmacol. (2022) 13:901875. doi: 10.3389/fphar.2022.901875
26. Saadati S, Naseri K, Asbaghi O, Abhari K, Zhang P, Li H-B, et al. Nigella Sativa supplementation improves cardiometabolic indicators in population with prediabetes and type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Front Nutr. (2022) 9:977756. doi: 10.3389/fnut.2022.977756
27. Tiwari A, G S, Meka S, Varghese B, Vishwakarma G, Adela R. The effect of nigella sativa on non-alcoholic fatty liver disease: a systematic review and meta-analysis. Hum Nutr Metabolism. (2022) 28:200146. doi: 10.1016/j.hnm.2022.200146
28. Golpour-Hamedani S, Hadi A, SafariMalekabadi D, Najafgholizadeh A, Askari G, Pourmasoumi M. The effect of Nigella supplementation on blood pressure: a systematic review and dose-response meta-analysis. Crit Rev Food Sci Nutr. (2022). doi: 10.1080/10408398.2022.2110566
29. Chattopadhyay K, Wang H, Kaur J, Nalbant G, Almaqhawi A, Kundakci B, et al. Effectiveness and safety of ayurvedic medicines in type 2 diabetes mellitus management: a systematic review and meta-analysis. Front Pharmacol. (2022) 13:821810. doi: 10.3389/fphar.2022.821810
30. Azizi N, Amini MR, Djafarian K, Shab-Bidar S. The effects of supplementation on liver enzymes levels: a systematic review and meta-analysis of randomized controlled trials. Clin Nutr Res. (2021) 10:72–82. doi: 10.7762/cnr.2021.10.1.72
31. Gyawali D, Vohra R, Orme-Johnson D, Ramaratnam S, Schneider RH. A systematic review and meta-analysis of ayurvedic herbal preparations for hypercholesterolemia. Medicina. (2021) 57:546. doi: 10.3390/medicina57060546
32. Han A, Shi D. The efficacy of Nigella Sativa supplementation for asthma control: a meta-analysis of randomized controlled studies. Postepy Dermatol Alergol. (2021) 38:561–5. doi: 10.5114/ada.2020.93220
33. Malekian S, Ghassab-Abdollahi N, Mirghafourvand M, Farshbaf-Khalili A. The effect of on oxidative stress and inflammatory biomarkers: a systematic review and meta-analysis. J Complement Integr Med. (2021) 18:235–59. doi: 10.1515/jcim-2019-0198
34. Montazeri RS, Fatahi S, Sohouli MH, Abu-Zaid A, Santos HO, Găman M-A, et al. The effect of Nigella Sativa on biomarkers of inflammation and oxidative stress: a systematic review and meta-analysis of randomized controlled trials. J Food Biochem. (2021) 45:e13625. doi: 10.1111/jfbc.13625
35. Tang G, Zhang L, Tao J, Wei Z. Effect of Nigella Sativa in the treatment of nonalcoholic fatty liver disease: a systematic review and meta-analysis of randomized controlled trials. Phytother Res. (2021) 35:4183–93. doi: 10.1002/ptr.7080
36. Ardiana M, Pikir BS, Santoso A, Hermawan HO, Al-Farabi MJ. Effect of supplementation on oxidative stress and antioxidant parameters: a meta-analysis of randomized controlled trials. Sci World J. (2020) 2020:2390706. doi: 10.1155/2020/2390706
37. Hallajzadeh J, Milajerdi A, Mobini M, Amirani E, Azizi S, Nikkhah E, et al. Effects of nigella sativa on glycemic control, lipid profiles, and biomarkers of inflammatory and oxidative stress: a systematic review and meta-analysis of randomized controlled clinical trials. Phytother Res. (2020) 34:2586–608. doi: 10.1002/ptr.6708
38. Mohit M, Farrokhzad A, Faraji SN, Heidarzadeh-Esfahani N, Kafeshani M. Effect of Nigella Sativa L. Supplementation on inflammatory and oxidative stress indicators: a systematic review and meta-analysis of controlled clinical trials complement. Ther Med. (2020) 54:102535. doi: 10.1016/j.ctim.2020.102535
39. Razmpoosh E, Safi S, Abdollahi N, Nadjarzadeh A, Nazari M, Fallahzadeh H, et al. The effect of nigella sativa on the measures of liver and kidney parameters: a systematic review and meta-analysis of randomized-controlled trials. Pharmacol Res. (2020) 156:104767. doi: 10.1016/j.phrs.2020.104767
40. Tavakoly R, Arab A, Vallianou N, Clark CCT, Hadi A, Ghaedi E, et al. The effect of Nigella Sativa L. Supplementation on serum c-reactive protein: a systematic review and meta-analysis of randomized controlled trials complement. Ther Med. (2019) 45:149–55. doi: 10.1016/j.ctim.2019.06.008
41. Mousavi SM, Sheikhi A, Varkaneh HK, Zarezadeh M, Rahmani J, Milajerdi A. Effect of Nigella Sativa supplementation on obesity indices: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. (2018) 38:48–57. doi: 10.1016/j.ctim.2018.04.003
42. Namazi N, Larijani B, Ayati MH, Abdollahi M. The effects of Nigella Sativa L. on obesity: a systematic review and meta-analysis. J Ethnopharmacol. (2018) 219:173–81. doi: 10.1016/j.jep.2018.03.001
43. Daryabeygi-Khotbehsara R, Golzarand M, Ghaffari MP, Djafarian K. Nigella Sativa improves glucose homeostasis and serum lipids in type 2 diabetes: a systematic review and meta-analysis. Complement Ther Med. (2017) 35:6–13. doi: 10.1016/j.ctim.2017.08.016
44. Sahebkar A, Beccuti G, Simental-Mendía LE, Nobili V, Bo S. Nigella Sativa (Black Seed) effects on plasma lipid concentrations in humans: a systematic review and meta-analysis of randomized placebo-controlled trials. Pharmacol Res. (2016) 106:37–50. doi: 10.1016/j.phrs.2016.02.008
45. Sahebkar A, Soranna D, Liu X, Thomopoulos C, Simental-Mendia LE, Derosa G, et al. A systematic review and meta-analysis of randomized controlled trials investigating the effects of supplementation with Nigella Sativa (Black Seed) on blood pressure. J Hypertens. (2016) 34:2127–35. doi: 10.1097/HJH.0000000000001049
46. Deutsch JK, Levitt J, Hass DJ. Complementary and alternative medicine for functional gastrointestinal disorders. Am J Gastroenterol. (2020) 115:350–64. doi: 10.14309/ajg.0000000000000539
47. Probst YC, Guan VX, Kent K. Dietary phytochemical intake from foods and health outcomes: a systematic review protocol and preliminary scoping. BMJ Open. (2017) 7:e013337. doi: 10.1136/bmjopen-2016-013337
48. Hannan MA, Rahman MA, Sohag AAM, Uddin MJ, Dash R, Sikder MH, et al. Black Cumin (L.): A comprehensive review on phytochemistry, health benefits, molecular pharmacology, and safety. Nutrients. (2021) 13:1784. doi: 10.3390/nu13061784
49. Butt MS, Sultan MT. Nigella Sativa: reduces the risk of various maladies. Crit Rev Food Sci Nutr. (2010) 50:654–65. doi: 10.1080/10408390902768797
50. Lu J, Xu B-B, Shen L-L, Wu D, Xue Z, Zheng H-L, et al. Characteristics and research waste among randomized clinical trials in gastric cancer. JAMA Netw Open. (2021) 4:e2124760. doi: 10.1001/jamanetworkopen.2021.24760
51. Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. (2009) 374:86–9. doi: 10.1016/S0140-6736(09)60329-9
52. Allers K, Hoffmann F, Mathes T, Pieper D. Systematic reviews with published protocols compared to those without: more effort, older search. J Clin Epidemiol. (2018) 95:102–10. doi: 10.1016/j.jclinepi.2017.12.005
53. Sideri S, Papageorgiou SN, Eliades T. Registration in the international prospective register of systematic reviews (prospero) of systematic review protocols was associated with increased review quality. J Clin Epidemiol. (2018) 100:103–10. doi: 10.1016/j.jclinepi.2018.01.003
54. Barbour V, Clark J, Jones S, Norton M. Best practice in systematic reviews: the importance of protocols and registration. PLoS Med. (2011) 8:e1001009. doi: 10.1371/journal.pmed.1001009
55. Chien PFW, Khan KS, Siassakos D. Registration of systematic reviews: prospero. BJOG. (2012) 119:903–5. doi: 10.1111/j.1471-0528.2011.03242.x
56. Qiu X, Wang C. Literature searches in the conduct of systematic reviews and evaluations. Shanghai Arch Psychiatry. (2016) 28:154–9.
57. Fabbri A, Parker L, Colombo C, Mosconi P, Barbara G, Frattaruolo MP, et al. Industry funding of patient and health consumer organisations: systematic review with meta-analysis. BMJ. (2020) 368:l6925. doi: 10.1136/bmj.l6925
Keywords: Nigella sativa, health outcomes, meta-analysis, overview, systematic review
Citation: Li Z, Wang Y, Xu Q, Ma J, Li X, Yan J, Tian Y, Wen Y and Chen T (2023) Nigella sativa and health outcomes: An overview of systematic reviews and meta-analyses. Front. Nutr. 10:1107750. doi: 10.3389/fnut.2023.1107750
Received: 25 November 2022; Accepted: 09 March 2023;
Published: 28 March 2023.
Edited by:
Mohamed Fawzy Ramadan, Umm Al-Qura University, Saudi ArabiaReviewed by:
Waseem Khalid, Government College University, Faisalabad, PakistanNaina Mohamed Pakkir Maideen, Dubai Health Authority, United Arab Emirates
Mohammad Reza Khazdair, Birjand University of Medical Sciences, Iran
Reham Hamza, Zagazig University, Egypt
Copyright © 2023 Li, Wang, Xu, Ma, Li, Yan, Tian, Wen and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yandong Wen, MzE4MDIwMDE4MkBjYWEuZWR1LmNu; Ting Chen, eGluZ2xpbmNoZW50aW5nQDE2My5jb20=
 Zhongyu Li1,2
Zhongyu Li1,2