
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 28 February 2023
Sec. Clinical Nutrition
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1098010
This article is part of the Research Topic Waist-to-Height Ratio is a Simple Tool for Assessing Central Obesity and Consequent Health Risk View all 8 articles
 Golaleh Asghari1,2
Golaleh Asghari1,2 Ali Nikparast2
Ali Nikparast2 Maryam Mahdavi3
Maryam Mahdavi3 Pooneh Dehghan4
Pooneh Dehghan4 Majid Valizadeh3
Majid Valizadeh3 Farhad Hosseinpanah3
Farhad Hosseinpanah3 Fereidoun Azizi5
Fereidoun Azizi5 Farzad Hadaegh6*
Farzad Hadaegh6*Background: There is debate regarding which anthropometric indices is the most appropriate predictor of cardiovascular disease (CVD) among adolescents. The purpose of this study was to investigate the association of body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), and waist-to-height ratio (WHtR) in adolescents with high carotid intima-media thickness (cIMT) in early adulthood, as the surrogate marker of CVD in a cohort study.
Methods: A total of 875 Iranian adolescents (female = 421) aged 10–17 years old were entered the study. The cIMT was measured in early adulthood (20–38 years old) after 18.2 (median) years of follow-up and defined as > 90th percentile for sex and age groups. The gender specific association between a 1-SD increase in each anthropometric measures with high cIMT was examined using multivariate logistic regression analysis adjusted for age, smoking, family history of CVD, systolic blood pressure, total cholesterol, and fasting blood sugar. In the multivariable analysis, the interaction between sex and age groups with anthropometric measures were significant (all p-values < 0.05).
Results: Among males, all anthropometric measures including BMI, WC, WHR, and WHtR were associated with high cIMT; the corresponding odds ratios were 1.43 (1.05–1.94), 1.63 (1.22–2.19), 1.33 (1.03–1.71), and 1.41 (1.07–1.87), respectively. However, after considering the related adulthood anthropometric measurements, the association remained significant for WC 1.48 (1.04–2.10) and WHR [1.28 (0.99–1.66), P = 0.06]. Moreover, among early adolescent boys aged 10–14 years, all of the anthropometric measures were significantly associated with high cIMT in the multivariate analysis that included the related adulthood anthropometric measures. The area under the curve (AUC) for the anthropometric measurements among males ranged from 0.576 for WHtR up to 0.632 for WC, without any superiority between them. Among females, only in linear regression analysis, a significant association were found between the higher value of WC and WHtR with cIMT measurement in adulthood; however, the risk reached to null after considering adult anthropometric measures.
Conclusion: General and central obesity measures were significantly associated with high cIMT only among Iranian male adolescents, the relationship that were more prominent among pre-pubertal males.
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality, accounting for nearly 17.9 million deaths annually and approximately 32% of all deaths worldwide (1). Despite the decline in CVD mortality in many industrialized countries, at least three out of four premature deaths were occur in low- and middle-income countries due to CVD and other non-communicable diseases (1). Atherosclerosis, as a lifelong disease, is known as one of the major causes of CVD. Although the clinical manifestations of atherosclerosis usually appear after midlife, the disease process has a long silent stage that is initiated as early as childhood (2). Therefore, early identification of individuals with subclinical atherosclerosis is crucial to implementing primary preventative strategies to reduce CVD risk in adulthood (3).
Several studies have shown a link between childhood cardiometabolic risk factors, including elevated blood pressure, glucose intolerance, abnormal blood lipids, and obesity, with the development of subclinical and clinical CVD in adulthood (4–7). Carotid intima-media thickness (cIMT), as measured by ultrasonography, is a validated, sensitive, and reproducible technique for detecting and quantifying subclinical atherosclerosis in asymptomatic individuals that corresponds with the development of coronary artery disease and has been identified as a predictor of future cardiovascular events as well as all-cause mortality (8). According to the meta-analysis conducted in 2013, one standard deviation increase in cIMT increased the risk of myocardial infarction and stroke by 26 and 31%, respectively (9). Furthermore, increased cIMT was found to be more strongly associated with mortality and cardiovascular endpoints in individuals younger than 50 years (10).
In spite of the efforts of the World Health Organization to achieve the goal of “halting the increase in obesity prevalence by 2025,” none of the countries have met this objective, and it is predicted that one out of eight children and adolescents in the world will be obese by 2030 (11). According to a systematic review investigating childhood risk factors and adulthood CVDs risk, 19 of the 20 studies have reported a significant association between childhood adiposity and thicker cIMT in adulthood (4). In a study published by Hosseinpanah et al. childhood body mass index (BMI) was found to be a strong predictor of cIMT in early adulthood (12). Furthermore, another study indicated that one standard deviation increase in adolescent BMI corresponded to a 2.3 μm increase in cIMT in ages between 27 and 30 years (13). Although BMI is the most commonly used index for the evaluation of general obesity, it does not consider body fat distribution and abdominal fat mass, which is particularly associated with increased CVD risk (14).
According to our knowledge, this study represents the first of its kind to examine the association between childhood central obesity measurements, including waist circumference (WC), waist-to-hip ratios (WHR), and waist-to-height ratio (WHtR), in addition to body mass index (BMI) and risk of high cIMT in early adulthood. Therefore, in this prospective study, we investigate the association between childhood adolescent anthropometric indices, including BMI, WC, WHR, and WHtR, with high cIMT in early adulthood during about two decades of follow-up.
The current longitudinal study was performed within the framework of the Tehran Lipid and Glucose Study (TLGS). The TLGS is an ongoing large scale population-based prospective study aiming to investigate and prevent non-communicable diseases (NCDs) risk factors and promote a healthy lifestyle to reduce these risk factors (15). The study participants were followed up every 3 years according to standard methods to monitor their demographics, lifestyle, biochemical profile, clinical information, and anthropometric indices. The baseline survey was a cross-sectional study including 15005 participants aged ≥ 3 years old who were selected using a multistage random sampling method in district 13 of Tehran, conducted from 1999 to 2001. Survey 2 (2002–2005), survey 3 (2006–2008), survey 4 (2009–2011), survey 5 (2012–2015), and survey 6 (2016–2019) were prospective follow-up surveys; this cohort is still being followed up.
At the recruitment, we collected data on 2,660 participants aged between 10 and 17 years old. Exclusions included those with prevalent cancer (n = 1), corticosteroid users (n = 8), and those without follow up till survey 5 or 6 (n = 981), leaving 1,670 participants. Out of these individuals, following phone contact with them, 711 individuals did not attend the medical center or express their willingness to participate in the cIMT measurement. Of the remaining individuals who measured the cIMT (n = 959), (missing data of cIMT, n = 5) the data of valid IMT were available on 954 cases. Finally, after excluding those with prevalent CVD (n = 8), and those with missing data on covariates at the end of study (n = 71), 875 individuals (Male = 454) were entered into our data analysis. The study protocol has been approved by the institutional ethics committee of the Research Institute for Endocrine Sciences, affiliated to the Shahid Beheshti University of Medical Sciences, and was conducted in accordance with the principles of the Declaration of Helsinki. At the beginning of this study, written informed consent was obtained from all parents or legal guardians of participants under 18. As well, all participants ≥ 18 years signed a written informed consent form before participating in the investigations.
A detailed description of the TLGS protocol and laboratory procedures has been provided elsewhere (15). Briefly, obtaining demographic information and taking anthropometric measurements were performed by trained examiners in accordance with standardized protocols. Weight was measured while the participants were minimally dressed and without shoes, using a digital scale (Seca 707, Hanover, MD, USA) and recorded to the nearest 100 g. Height was measured while standing, without shoes, with shoulders held in a normal position, using a tape meter. Waist circumference (WC) was measured at the midpoint level (umbilicus level) while the subjects were in a standing position using an un-stretched tape meter, without any pressure on the body surface, and hip circumference (HC) was measured over light clothing at the widest girth of the hip using a tape meter. These measurements were recorded to the nearest 0.1 cm. Body mass index [BMI = weight (kg)/square of height (m2)], waist-to-hip ratio [WHR = waist circumference (cm)/hip circumference (cm)], and waist-to-height ratio [WHtR = waist circumference (cm)/height circumference (cm)] were calculated. Systolic and diastolic blood pressures were measured by a qualified physician in a seated position following the participant’s rest for 15 min, using a standard mercury sphygmomanometer (calibrated by the Iranian Institute of Standards and Industrial Researches) with the cuff placed on the right brachial at the heart level. Blood pressure was measured twice, at least a 30-s interval, and then the average of two measurements was recorded as the participant’s blood pressure. After 12–14 h of overnight fasting, blood samples were taken from all subjects and centrifuged within 30–45 min of collection. All blood analyses were conducted at the TLGS research laboratory on the day of blood collection using commercially available laboratory kits (Pars Azmoon Inc., Tehran, Iran) adapted to a Selectra 2 auto analyzer (Vital Scientific, Spankeren, Netherlands). Fasting plasma glucose (FPG) was assayed using the glucose oxidase based on the enzymatic colorimetric technique. Inter- and intra-assay coefficients of variation were both 2.2% for serum glucose. Serum total cholesterol (TC) and triglycerides (TGs) were also measured by enzymatic calorimetric methods with cholesterol esterase and cholesterol oxidase, and glycerol phosphate oxidase, respectively. Inter- and intra-assay coefficients of variation were 2 and 0.5% for TC and 1.6 and 0.6% for TGs, respectively. High-density lipoprotein cholesterol (HDL-C) was assayed following the precipitation of the apolipoprotein B-containing lipoproteins with phosphotungstic acid. The low-density lipoprotein Cholesterol (LDL-C) was calculated by the Friedewald formula based on the serum TC, TG, and HDL-C concentrations expressed in mg/dl if the serum TG concentrations were less than 400 mg/dL (16).
Two qualified radiologists, who were blinded to the study participant’s details, measured the intima-media thickness of extra carinal carotid arteries based on B-mode ultrasound imaging techniques using a linear 7.5–10 MHz probe (Samsung Medison SonoAce R3 ultrasound machine). The measurement was done on both right and left carotids in the supine position, with the neck extended and slightly rotated to the opposite side as a first step, transverse carotid scan was conducted to evaluate the subject’s anatomy, locate atherosclerotic plaques (if present), and determine the site of maximal wall thickening in the near or far wall. Afterward, longitudinal scans with different angles were obtained from the artery. In order to obtain optimal gray scale imaging of the carotid artery, measurements on plaque-free arterial segments were implemented according to optimal B-mode imaging criteria, which is defined as Clear visualization of far wall arterial interfaces with completely anechoic luminal content. A scan depth adjustment was attempted in order to bring the arterial lumen to the center of the image while setting the focal zone at the level of the arterial lumen. Generally, IMT was regarded as a hypo-echoic band between the arterial wall’s echogenic intimal and adventitial surfaces. The cIMT was calculated by measuring three locations on either side of the distal segment of the common carotid artery between the leading edge of the first and second echogenic lines. The average measurements were taken as the final measurement on each side. IMT measurements were sporadically conducted on the distal segments of both sides of the internal carotid artery and carotid bulb in subjects who met the optimal technique and image criteria. In the present study, as measurements taken along the left common carotid artery (LCCA) displayed less inter- and intra-observer variation and were more in line with laboratory test results, we used left common carotid artery far wall measurements (LCCA) for defining high cIMT. In order to test the rate of reliability agreement, cIMT was measured by both radiologists in a subsample of 30 participants, consisting of 66.7% females with the mean age and BMI of 41.7 ± 10.7 years and 24.4 ± 5.5 kg/m2, respectively. The degree of agreement between the two radiologists with regard to the cIMT measurements was evaluated using the inter-class correlation coefficient (ICC) and their 95% confidence intervals based on the two-way mixed-effects model. According to the ICC analysis, the ICC values and 95% CI were 0.79 and 0.55–0.90, respectively. In general, the ICC ranges between 0 and 1, where values between 0.75 and 0.9 indicate good reliability (17).
Family history of premature cardiovascular diseases was defined as a prior history of myocardial infarction, stroke, or sudden cardiac death in a male first-degree relative or father grandparent < 55 years old and in a female first-degree relative or mother grandparents < 65 years old. A high cIMT (as a surrogate for subclinical atherosclerosis) was defined as CIMT greater than the 90th percentile values specific for sex and age group (18). Smoking habits were classified into two groups: (a) current smokers, (b) past/never smokers.
Baseline characteristics of subjects were shown as a mean ± standard deviation (SD) and median and inter-quartile range (IQR) 25–75 for normally distributed continuous variables and skewed-distributed continuous variables, respectively. Categorical variables of baseline characteristics were presented as frequency (percentages). Characteristics of participants at baseline and the end of follow-up between sex as well as respondent and non-respondent (those with missing data on covariates, those who did not have any follow up, and those who did not participate in the cIMT measurement) were compared using an independent sample t-test, Mann–Whitney U test, and Chi-square test as appropriate. In order to examine the effect modification of sex and age groups on the impact of each anthropometric measures for high cIMT, logistic regression analyses were conducted. In the multivariable models, the interaction between sex and age groups with BMI, WC, and WHtR were significant (all p-values < 0.05). Therefore, all analysis were conducted separately for boys and girls in two age groups.
The association between different adolescent anthropometric indices and high cIMT in early adulthood were evaluated by calculating the multiple-adjusted odds ratios (ORs) using logistic regression analysis. ORs and 95% confidence intervals (CIs) were evaluated per 1-SD of BMI, WC, WHR, and WHtR as continuous variables for the total boys and girls as well as in age-stratified groups in each gender. Multiple linear regression was also used to investigate the effect of each adolescent anthropometric indices in cIMT in early adulthood. Accordingly, three adjusted models were constructed: Model 1 was adjusted for age, family history of CVD, and smoking; Model 2: further adjusted for systolic blood pressure, total cholesterol, and fasting plasma glucose; Model 3: Model 2 + adulthood relevant anthropometric measurements (i.e., for waist circumference, adulthood waist circumference was included as another covariate). The area under the receiver-operating characteristic curve (AUC) and 95% confidence interval was used to evaluate the predictive ability of each adolescent anthropometric indices, followed by a comparison of all adolescent anthropometric indices using the Delong test (19). In addition, Youden’s index (sensitivity + specificity-1) was used to obtain the best cut-off from the ROC curve. The values for the maximum of the Youden’s index were considered the optimal cut-off points (20). All statistical analyses were conducted using SPSS version 20 (SPSS, Chicago, IL, USA) regarding a two-tailed P-value of < 0.05 as a significant.
At the recruitment time, the study population included 454 boys and 421 girls with mean ages of 13.3, and 13.5, years old respectively; the corresponding values for BMI were 19.6 and 20.1 (Kg/m2), respectively. The characteristics and cardiometabolic profile of the participants according to gender are shown in Table 1. At baseline, girls had significantly higher WC, HC, WHtR, TC, TG, and LDL-C than boys. However, boys were taller compared to girls and had higher values of WHR, SBP, and HLD-C. No significant differences were seen regarding age, weight, BMI, DBP, and FPG between boys and girls.
After the median (IQR) follow-up duration 18.2 (17.8–18.8) years, cIMT was measured in early adulthood (the mean age was 32.1 ± 2.3 years), and the mean value was 0.55 ± 0.09 mm. As shown in Table 1, at the end of the follow-up, the mean age of cIMT measurement was significantly higher among females than males. Also, females had significantly higher mean values of cIMT than males, however, the values of weight, BMI, WC, and WHR were higher in the latter. The males were more likely to be smoker than females. Although, no significant differences in WHtR and prevalence of family history of CVDs between genders were found.
The characteristics of respondents and non-respondents are provided in Supplementary Table 1. The respondents were younger, constituted a greater proportion of males, and had lower values of WC, HC, and DBP, however, no significant differences were found for other baseline characteristics between them.
Table 2 demonstrates the odds ratio and 95% confidence intervals of each adolescent anthropometric indices for high cIMT (> 90th percentile) in early adulthood using multivariable logistic regression. In females, no significant association were found between each adolescent anthropometric indices and risk of high cIMT in early adulthood even in model 1. In male, all adolescent anthropometric indices were significantly associated with high cIMT in early adulthood in model 1 with ORs ranging from 1.35 for WHR to 1.60 for WC; after controlling multiple cardiometabolic risk factors (Model 2), all adolescent anthropometric indices were significantly associated with high cIMT in early adulthood, with ORs ranging from 1.33 for WHR to 1.63 for WC (all p-values < 0.05 for both models). After considering adulthood relevant anthropometric measurements as a confounder (model 3), all of the associations significantly attenuated excluding WC [1.48 (95% CI: 1.04–2.10)] and WHR [1.28 (95% CI: 0.99–1.66), p-value = 0.06]. According to age- and sex-stratified analysis, no significant association was found between each anthropometric indices and risk of high cIMT in early adulthood except in boys aged 15–17 years old. A 1-SD increase in each adolescent anthropometric indices in boys aged 10–14 years old, were significantly increased the risk of high cIMT in model 3, the corresponding values for BMI, WC, WHR, and WHtR were 1.81 (1.13–2.92), 2.04 (1.31–3.18), 1.36 (1.02–1.83), and 1.85 (1.22–2.80), respectively.
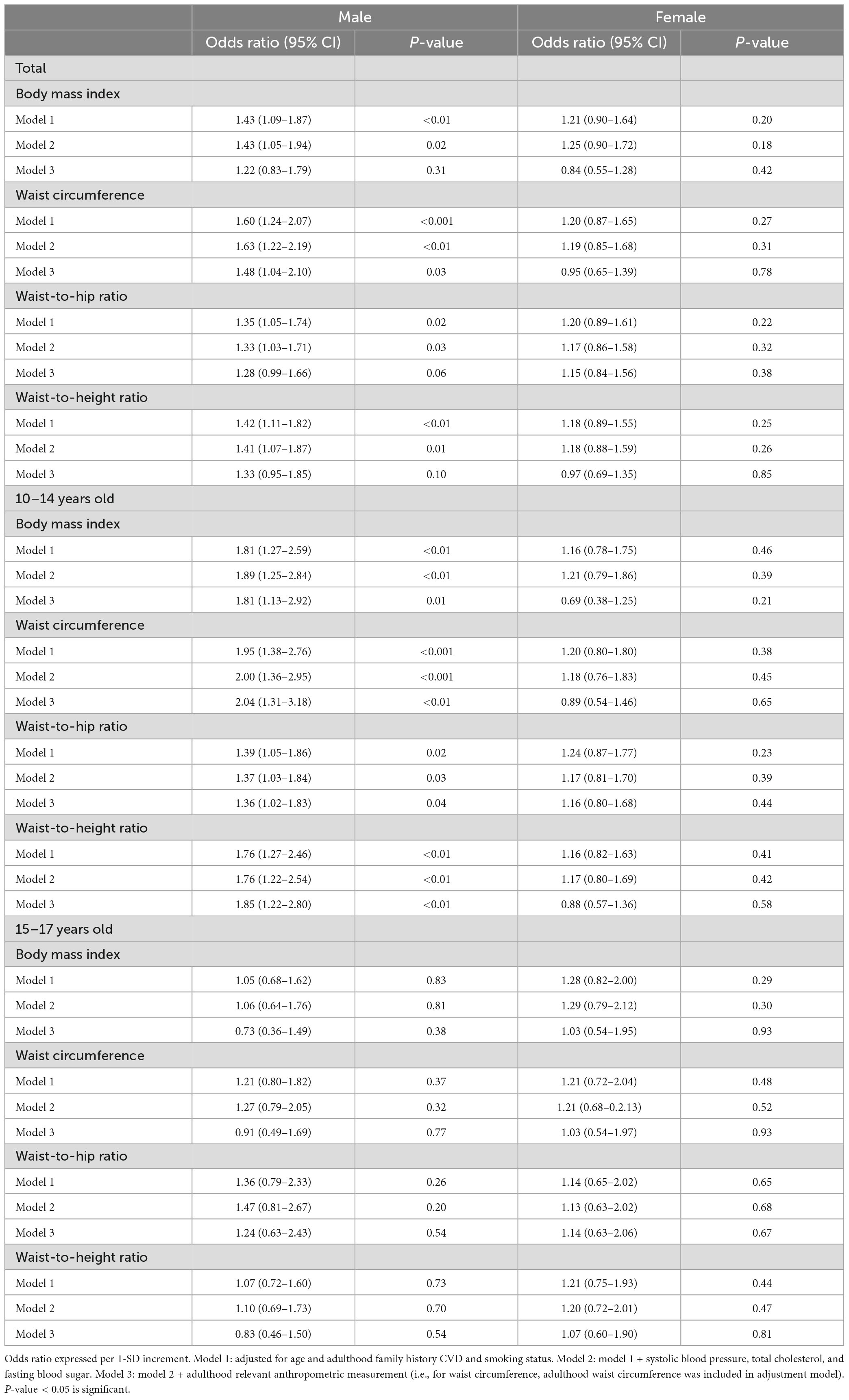
Table 2. Sex and age group stratified association of adolescent anthropometric indices with high carotid intima-media thickness (≥ 90th percentiles) in early adulthood.
The early adolescent males were generally had better cardiometabolic health status both at the baseline and at the end of the follow up compared to late adolescent ones, however, no differences were found in term of cIMT between these groups (Supplementary Table 2). Among male participants, in the early adolescent group, regardless of baseline anthropometric measures, no significant associations were found for other confounder/mediators, however for late adolescent group the adulthood cholesterol level was significantly associated with high cIMT. Moreover, among female, in the early adolescent group, baseline FPG and the adulthood general and central adiposity measures were remained as significant predictors of high cIMT, however, no significant association were found for confounder/mediators in later adolescent ones (data not shown).
Sex and age group stratified association of adolescent anthropometric indices with cIMT (in mm) in early adulthood is also shown in Supplementary Table 3 using linear regression analysis. Accordingly, the result among males were generally in the line with the main analysis conducted using multivariate logistic regression. Importantly among females, however, in contrast to logistic regression analysis we found a significant association between WC, WHR, and WHtR and higher value of high cIMT in model 1, the relationship that remained significant only for WHtR after further adjustment for cardiometabolic risk factors (model 2).
Figure 1 illustrates the area under the receiver operating curve (AUC) and 95% confidence intervals, sensitivity, specificity, and cut-off values of each adolescent anthropometric indices in boys for predicting high cIMT in early adulthood. The AUC levels ranged from 0.632 (95% CI: 0.585–0.676) for WC to 0.576 (95% CI: 0.529–0.622) for WHtR, the corresponding cut-off points were 72 (cm), and 0.47, respectively. Supplementary Table 4 shows the comparison of AUCs of adolescent anthropometric indices in boys. No significant differences were observed between the AUCs of adolescent anthropometric indices (all p-values > 0.05). However, we found a signal for higher discriminatory power of WC compared to BMI and WHtR in boys (p-value = 0.07).
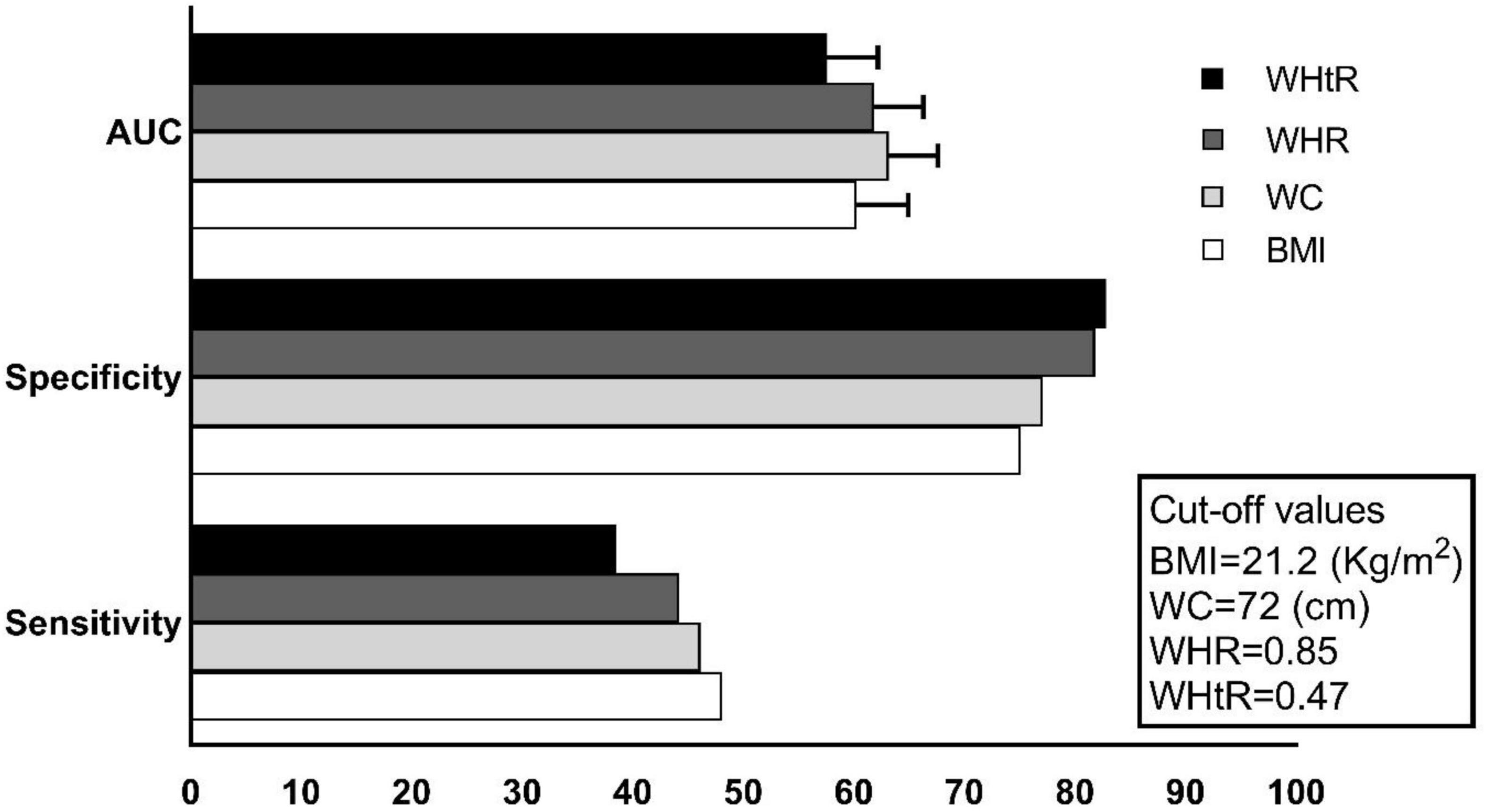
Figure 1. The area under the curves (AUCs*100), sensitivity (%), specificity (%), and cut-off values of adolescent anthropometric indices for predicting high cIMT in boys.
This community-based study of Iranian adolescents with a two-decade follow-up period showed that anthropometric indices, including BMI, WC, WHR, and WHtR, can predict the risk of high cIMT in early adulthood among boys; however, these associations were not found in girls. Considering adjustment for a large set of covariates (including obesity mediators, and corresponding adulthood anthropometric measurements) among boys WC and WHR were significant predictors, although these relationships were tended to be significant for the latter. Importantly, among early but not late adolescent males, all of the anthropometric measurements were significantly associated with high cIMT. Among Iranian females, we found generally in linear regression analysis, a significant association between the higher value of WC and WHtR with cIMT measurement in adulthood, however, these risks reach to null after considering adult anthropometric measures. Regarding the discriminatory power of anthropometric measurement as assessed by AUC, no differences were found between the predictive performance of anthropometric measures in boys for high cIMT, however, a signal for higher discriminatory power of WC compared with BMI and WHtR were found (p-value = 0.07).
A number of prospective studies have demonstrated a link between pediatric obesity by measuring BMI, which represents general obesity, or triceps skinfold thickness (TSF), and the risk of thicker cIMT in adulthood (Table 3). In accordance with our findings, the international Childhood Cardiovascular Cohort (i3C) Consortium has shown that childhood BMI significantly predicted thicker cIMT in adulthood (21). Furthermore, the pooled analysis of four longitudinal studies, including the Bogalusa Heart Study, the Insulin Study, Childhood Determinants of Adult Health, and the Cardiovascular Risk in Young Finns Study, have demonstrated that childhood BMI was associated with high cIMT (> 90th percentile) in adulthood after two decades of follow up (22).

Table 3. Description of papers that evaluated the association between childhood adiposity and carotid intima-media thickness (cIMT) in adulthood.
The result of our study has shown that the predictive power of all anthropometric indices for the prediction of high cIMT in early adulthood was attenuated and only remained significant in WC among males after adjustment of adulthood relevant anthropometric measurements. Summarizing the results of a majority of longitudinal cohort studies, the positive associations between childhood BMI and thicker cIMT in adulthood were generally reduced after adjustment for adulthood BMI (23) or became non-significant (13, 24, 25). These findings may provide some clues that the patterns of adiposity anthropometric indices trajectories from childhood to adulthood also plays an important role in predicting the thicker cIMT in adulthood along with childhood adiposity. Juonala et al. have demonstrated that childhood adiposity was associated with thicker cIMT in adulthood, but this association can be attributed to significant changes in BMI from childhood to adulthood (24). They also reported that the corresponding adulthood cIMT values in individuals who were obesity gainers from childhood to adulthood compared to individuals who had been persistently obese were comparable. As well, the cIMT values tended to be lower, yet comparable, in individuals who had been consistently non-obese and those who had been obesity reducers from childhood to adulthood. However, The Cardiovascular Risk in Young Finns Study has indicated that the effect of childhood obesity on the risk of high cIMT, even with the normalization of high BMI in later life, has not been completely eliminated (26). To our knowledge, no study compare the association between central adiposity measures with high cIMT in early adulthood.
We also found that the association between adolescent anthropometric indices and risk of high cIMT in early adulthood was observed only among boys. In line with our findings, in an I3C consortium of 6,380 participants, Juonala et al. have demonstrated that the mentioned association was seen in boys (18). In contrast, another I3C Consortium has shown that no significant differences between gender were observed for the predictive power of childhood BMI for the risk of high cIMT in adulthood (21). Additionally, Ceponiene et al. have indicated that higher childhood BMI was associated with thicker cIMT in women adults; that this association was not independent of adult cardiometabolic risk factors (27). In the current study when we examined cIMT as a continuous rather than categorical variable as the outcome we found that Tehranian girls with higher WC had significantly higher values of cIMT in the presence of cardiometabolic risk factors. Considering the observational nature of our study, it is not possible for us to explain the sex difference in the association between anthropometric measures and subclinical atherosclerosis in early adulthood; however, previously we reported the prominent role of general and central adiposity measures in the development of CVD among adult men rather than women (28).
Studies that have evaluated childhood obesity and the risk of high cIMT in adulthood have mainly measured BMI as an obesity indicator (as shown in Table 3), which may fail to reflect central obesity (29). The results from NHANES III, including the 15,184 participants aged 18–90 years old, showed that central adiposity increased the risk of CV mortality among individuals with normal BMI (30). Wang et al. in the cohort of Chinese children, demonstrated that compared with persistently normal WC, gaining in abdominal obesity, whether as incident or persistent, were significantly associated with the short-term risk of high cIMT during a 2-year follow-up in childhood (31).
As an important finding, in our subgroup analysis by age group, we found that the unfavorable impact of increasing value for general and central adiposity indices on cIMT thickening were more prominent among early adolescent boys. According to the findings of the I3C consortium, Jounala et al. have shown that childhood BMI after age 9 years was significantly associated with high cIMT in adulthood (21). In addition, Raitakari et al. have demonstrated that greater BMI in adolescents aged 12–18 years old was significantly associated with thicker cIMT in adulthood (32). Importantly, other cardiometabolic risk factors besides anthropometric measurements specially baseline fasting glucose among early adolescent girl and adulthood cholesterol level among late adolescent boys had significant association with high cIMT in our study (data not shown); the role of these obesity mediators in the development of atherosclerosis were addressed in other studies as well (21, 33).
In light of these findings, it is reasonable to conclude that childhood adiposity beginning in early puberty, may cause progressive damage to the common carotid artery in adulthood.
Our study has several strengths. It is important to point out that not only childhood cardiometabolic confounders but also adulthood relevant anthropometric indices were considered in our analysis. However, there are also some limitations to be considered. First, although we adjusted major confounding variables in our analyses, residual or unmeasured factors, such as physical activity, dietary intakes, adipokines and cytokines, pubertal status, and genetic background were not considered in our data analysis. Second, we should point out that the respondents were generally healthier than non-respondents, however, the magnitude of the difference between these groups were not clinically important. Third, we conducted this study among Tehranian adolescents, so we cannot generalize our findings to other parts of the country, especially the rural zones.
The present study was the first to evaluate the predictive power of general and central childhood adiposity indices and the risk of high cIMT in early adulthood not only in the Eastern Mediterranean Region but also worldwide. Childhood general and central anthropometric indices significantly predicted the high cIMT as the surrogate marker of CVD in early adulthood only among male adolescents without any differences in predictive power between the anthropometric indices. Following further adjustment for adulthood relevant anthropometric indices, generally, all of the male anthropometric indices except WC and WHR were no longer significant predictors of high cIMT in early adulthood. No superiority in the discriminatory ability for high cIMT among anthropometric indices was found in adolescent males. The predictive ability of high cIMT in early adulthood were prominent among pre-pubertal boys.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of the Research Institute for Endocrine Sciences (RIES) of Shahid Beheshti University of Medical Sciences. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
FHa contributed to the conception and design of the study. PD contributed to the acquisition of the ultrasound data. MM analyzed the data. GA and AN took lead in the literature review and writing the manuscript in consultation with FHa. All authors reviewed and approved the final draft of the manuscript.
This study was supported in part by Grant No. 43003845-1 from the Shahid Beheshti University of Medical Sciences.
We thank all children and families participating in the study. We would like to acknowledge the staff of the TLGS study for their important contribution.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2023.1098010/full#supplementary-material
1. World Health Organization [WHO]. Cardiovascular diseases: fact sheets. Geneva: World Health Organization (2021).
2. McGill H, McMahan C, Herderick E, Malcom G, Tracy R, Strong J. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. (2000) 72:1307S–15S. doi: 10.1093/ajcn/72.5.1307s
3. Alsheikh-Ali A, Kitsios G, Balk E, Lau J, Ip S. The vulnerable atherosclerotic plaque: scope of the literature. Ann Intern Med. (2010) 153:387–95. doi: 10.7326/0003-4819-153-6-201009210-00272
4. Pool L, Aguayo L, Brzezinski M, Perak A, Davis M, Greenland P, et al. Childhood risk factors and adulthood cardiovascular disease: a systematic review. J Pediatr. (2021) 232:118–26.e23. doi: 10.1016/j.jpeds.2021.01.053
5. Koskinen J, Kytö V, Juonala M, Viikari J, Nevalainen J, Kähönen M, et al. Childhood risk factors and carotid atherosclerotic plaque in adulthood: the cardiovascular risk in young finns study. Atherosclerosis. (2020) 293:18–25. doi: 10.1016/j.atherosclerosis.2019.11.029
6. Tasdighi E, Barzin M, Mahdavi M, Valizadeh M, Dehghan P, Moghaddam A, et al. Association of childhood obesity phenotypes with early adulthood carotid intima-media thickness (CIMT): tehran lipid and glucose study. Nutr Metab Cardiovasc Dis. (2022) 32:249–57. doi: 10.1016/j.numecd.2021.09.020
7. Valizadeh M, Tasdighi E, Barzin M, Hariri R, Mahdavi M, Dehghan P, et al. Association of childhood metabolic syndrome and metabolic phenotypes with the carotid intima-media thickness (CIMT) in early adulthood: tehran lipid and glucose study. Int J Cardiol. (2022) 348:128–33. doi: 10.1016/j.ijcard.2021.12.010
8. Oren A, Vos L, Uiterwaal C, Grobbee D, Bots M. Cardiovascular risk factors and increased carotid intima-media thickness in healthy young adults: the atherosclerosis risk in young adults (ARYA) study. Arch Intern Med. (2003) 163:1787–92. doi: 10.1001/archinte.163.15.1787
9. van den Oord S, Sijbrands E, ten Kate G, van Klaveren D, van Domburg R, van der Steen A, et al. Carotid intima-media thickness for cardiovascular risk assessment: systematic review and meta-analysis. Atherosclerosis. (2013) 228:1–11. doi: 10.1016/j.atherosclerosis.2013.01.025
10. Lorenz M, von Kegler S, Steinmetz H, Markus H, Sitzer M. Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the carotid atherosclerosis progression study (CAPS). Stroke. (2006) 37:87–92. doi: 10.1161/01.STR.0000196964.24024.ea
11. World Obesity Atlas 2022. One billion people globally estimated to be living with obesity by 2030. London: World Obesity Federation (2022).
12. Hosseinpanah F, Seyedhoseinpour A, Barzin M, Mahdavi M, Tasdighi E, Dehghan P, et al. Comparison analysis of childhood body mass index cut-offs in predicting adulthood carotid intima media thickness: tehran lipid and glucose study. BMC Pediatr. (2021) 21:494. doi: 10.1186/s12887-021-02963-y
13. Oren A, Vos L, Uiterwaal C, Gorissen W, Grobbee D, Bots M. Change in body mass index from adolescence to young adulthood and increased carotid intima-media thickness at 28 years of age: the atherosclerosis risk in young adults study. Int J Obes Relat Metab Disord. (2003) 27:1383–90. doi: 10.1038/sj.ijo.0802404
14. Menke A, Muntner P, Wildman R, Reynolds K, He J. Measures of adiposity and cardiovascular disease risk factors. Obesity. (2007) 15:785–95. doi: 10.1038/oby.2007.593
15. Azizi F, Ghanbarian A, Momenan A, Hadaegh F, Mirmiran P, Hedayati M, et al. Prevention of non-communicable disease in a population in nutrition transition: tehran lipid and glucose study phase II. Trials. (2009) 10:5. doi: 10.1186/1745-6215-10-5
16. Friedewald W, Levy R, Fredrickson D. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. (1972) 18:499–502. doi: 10.1093/clinchem/18.6.499
17. Koo T, Li MYA. Guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. (2016) 15:155–63. doi: 10.1016/j.jcm.2016.02.012
18. Juonala M, Magnussen C, Berenson G, Venn A, Burns T, Sabin M, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. (2011) 365:1876–85. doi: 10.1056/NEJMoa1010112
19. DeLong E, DeLong D, Clarke-Pearson D. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. (1988) 44:837–45. doi: 10.2307/2531595
20. Youden W. Index for rating diagnostic tests. Cancer. (1950) 3:32–5. doi: 10.1002/1097-0142(1950)3:1<32::AID-CNCR2820030106>3.0.CO;2-3
21. Juonala M, Magnussen C, Venn A, Dwyer T, Burns T, Davis P, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the cardiovascular risk in young finns study, the childhood determinants of adult health study, the bogalusa heart study, and the muscatine study for the international childhood cardiovascular cohort (i3C) consortium. Circulation. (2010) 122:2514–20. doi: 10.1161/CIRCULATIONAHA.110.966465
22. Koskinen J, Juonala M, Dwyer T, Venn A, Thomson R, Bazzano L, et al. Impact of lipid measurements in youth in addition to conventional clinic-based risk factors on predicting preclinical atherosclerosis in adulthood: international childhood cardiovascular cohort consortium. Circulation. (2018) 137:1246–55. doi: 10.1161/CIRCULATIONAHA.117.029726
23. Freedman D, Patel D, Srinivasan S, Chen W, Tang R, Bond M, et al. The contribution of childhood obesity to adult carotid intima-media thickness: the Bogalusa heart study. Int J Obesity. (2008) 32:749–56. doi: 10.1038/sj.ijo.0803798
24. Juonala M, Raitakari M, Viikari SA, Raitakari O. Obesity in youth is not an independent predictor of carotid IMT in adulthood. The cardiovascular risk in young finns study. Atherosclerosis. (2006) 185:388–93. doi: 10.1016/j.atherosclerosis.2005.06.016
25. Yan Y, Hou D, Liu J, Zhao X, Cheng H, Xi B, et al. Childhood body mass index and blood pressure in prediction of subclinical vascular damage in adulthood: Beijing blood pressure cohort. J Hypertens. (2017) 35:47–54. doi: 10.1097/HJH.0000000000001118
26. Buscot M, Thomson R, Juonala M, Sabin M, Burgner D, Lehtimäki T, et al. Distinct child-to-adult body mass index trajectories are associated with different levels of adult cardiometabolic risk. Eur Heart J. (2018) 39:2263–70. doi: 10.1093/eurheartj/ehy161
27. Ceponiene I, Klumbiene J, Tamuleviciute-Prasciene E, Motiejunaite J, Sakyte E, Ceponis J, et al. Associations between risk factors in childhood (12-13 years) and adulthood (48-49 years) and subclinical atherosclerosis: the Kaunas cardiovascular risk cohort study. BMC Cardiovasc Disord. (2015) 15:89. doi: 10.1186/s12872-015-0087-0
28. Hadaegh F, Zabetian A, Sarbakhsh P, Khalili D, James W, Azizi F. Appropriate cutoff values of anthropometric variables to predict cardiovascular outcomes: 7.6 years follow-up in an Iranian population. Int J Obesity. (2009) 33:1437–45. doi: 10.1038/ijo.2009.180
29. Ross R, Neeland I, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. (2020) 16:177–89. doi: 10.1038/s41574-019-0310-7
30. Sahakyan K, Somers V, Rodriguez-Escudero J, Hodge D, Carter R, Sochor O, et al. Normal-weight central obesity: implications for total and cardiovascular mortality. Ann Intern Med. (2015) 163:827–35. doi: 10.7326/M14-2525
31. Wang H, Sun J, Zhang Z, Yang L, Zhao M, Bovet P, et al. Waist circumference change and risk of high carotid intima-media thickness in a cohort of Chinese children. J Hypertens. (2021) 39:1901–7. doi: 10.1097/HJH.0000000000002881
32. Raitakari O, Juonala M, Kähönen M, Taittonen L, Laitinen T, Mäki-Torkko N, et al. Cardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the cardiovascular risk in young finns study. JAMA. (2003) 290:2277–83. doi: 10.1001/jama.290.17.2277
33. Yajnik C, Katre P, Joshi S, Kumaran K, Bhat D, Lubree H, et al. Higher glucose, insulin and insulin resistance (HOMA-IR) in childhood predict adverse cardiovascular risk in early adulthood: the Pune children’s study. Diabetologia. (2015) 58:1626–36. doi: 10.1007/s00125-015-3602-z
34. Davis P, Dawson J, Riley W, Lauer R. Carotid intimal-medial thickness is related to cardiovascular risk factors measured from childhood through middle age: the Muscatine study. Circulation. (2001) 104:2815–9. doi: 10.1161/hc4601.099486
35. Li S, Chen W, Srinivasan S, Bond M, Tang R, Urbina E, et al. Childhood cardiovascular risk factors and carotid vascular changes in adulthood: the Bogalusa heart study. JAMA. (2003) 290:2271–6. doi: 10.1001/jama.290.17.2271
36. Freedman D, Dietz W, Tang R, Mensah G, Bond M, Urbina E, et al. The relation of obesity throughout life to carotid intima-media thickness in adulthood: the Bogalusa heart study. Int J Obesity. (2004) 28:159–66. doi: 10.1038/sj.ijo.0802515
37. Ferreira I, Twisk J, van Mechelen W, Kemper H, Seidell J, Stehouwer C. Current and adolescent body fatness and fat distribution: relationships with carotid intima-media thickness and large artery stiffness at the age of 36 years. J Hypertens. (2004) 22:145–55. doi: 10.1097/00004872-200401000-00024
38. Li S, Chen W, Srinivasan S, Tang R, Bond M, Berenson G. Race (black-white) and gender divergences in the relationship of childhood cardiovascular risk factors to carotid artery intima-media thickness in adulthood: the Bogalusa heart study. Atherosclerosis. (2007) 194:421–5. doi: 10.1016/j.atherosclerosis.2006.08.026
39. Juonala M, Viikari J, Kähönen M, Taittonen L, Laitinen T, Hutri-Kähönen N, et al. Life-time risk factors and progression of carotid atherosclerosis in young adults: the cardiovascular risk in young finns study. Eur Heart J. (2010) 31:1745–51. doi: 10.1093/eurheartj/ehq141
40. Magnussen C, Koskinen J, Chen W, Thomson R, Schmidt M, Srinivasan S, et al. Pediatric metabolic syndrome predicts adulthood metabolic syndrome, subclinical atherosclerosis, and type 2 diabetes mellitus but is no better than body mass index alone: the Bogalusa heart study and the cardiovascular risk in young finns study. Circulation. (2010) 122:1604–11. doi: 10.1161/CIRCULATIONAHA.110.940809
41. Huynh Q, Blizzard L, Sharman J, Magnussen C, Schmidt M, Dwyer T, et al. Relative contributions of adiposity in childhood and adulthood to vascular health of young adults. Atherosclerosis. (2013) 228:259–64. doi: 10.1016/j.atherosclerosis.2013.02.022
42. Su T, Liao C, Chien K, Hsu S, Sung F. An overweight or obese status in childhood predicts subclinical atherosclerosis and prehypertension/hypertension in young adults. J Atheroscler Thromb. (2014) 21:1170–82. doi: 10.5551/jat.25536
43. Koskinen J, Magnussen C, Sabin M, Kähönen M, Hutri-Kähönen N, Laitinen T, et al. Youth overweight and metabolic disturbances in predicting carotid intima-media thickness, type 2 diabetes, and metabolic syndrome in adulthood: the cardiovascular risk in young finns study. Diabetes Care. (2014) 37:1870–7. doi: 10.2337/dc14-0008
44. Johnson W, Kuh D, Tikhonoff V, Charakida M, Woodside J, Whincup P, et al. Body mass index and height from infancy to adulthood and carotid intima-media thickness at 60 to 64 years in the 1946 British birth cohort study. Arterioscler Thromb Vasc Biol. (2014) 34:654–60. doi: 10.1161/ATVBAHA.113.302572
45. Du Y, Zhang T, Sun D, Li C, Bazzano L, Qi L, et al. Effect of serum adiponectin levels on the association between childhood body mass index and adulthood carotid intima-media thickness. Am J Cardiol. (2018) 121:579–83. doi: 10.1016/j.amjcard.2017.11.029
Keywords: obesity, child, adolescent, carotid intima-media thickness, atherosclerosis, adulthood, longitudinal cohort study
Citation: Asghari G, Nikparast A, Mahdavi M, Dehghan P, Valizadeh M, Hosseinpanah F, Azizi F and Hadaegh F (2023) Diagnostic performance of different anthropometric indices among Iranian adolescents for intima media thickness in early adulthood: A prospective study and literature review. Front. Nutr. 10:1098010. doi: 10.3389/fnut.2023.1098010
Received: 14 November 2022; Accepted: 06 February 2023;
Published: 28 February 2023.
Edited by:
Jimmy Chun Yu Louie, Swinburne University of Technology, AustraliaReviewed by:
Chris Ho Ching Yeung, University of Texas Health Science Center at Houston, United StatesCopyright © 2023 Asghari, Nikparast, Mahdavi, Dehghan, Valizadeh, Hosseinpanah, Azizi and Hadaegh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Farzad Hadaegh, ZnpoYWRhZWdoQGVuZG9jcmluZS5hYy5pcg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.