
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 01 September 2023
Sec. Nutritional Epidemiology
Volume 10 - 2023 | https://doi.org/10.3389/fnut.2023.1073200
This article is part of the Research TopicSecondary Analysis of National Nutrition Surveys: From Science to PolicyView all 9 articles
Introduction: Emerging evidence indicates that children can be concurrently wasted and stunted (WaSt), increasing their mortality risk. However, more is needed to know about WaSt in Ethiopia. Therefore, this study aimed to determine the trends and predictors of WaSt using Ethiopian Demographic and Health Survey datasets from 2000 and 2019.
Methods: The study included a total weighted sample of 34,930 children aged 6–59 months. Descriptive and weighted multilevel mixed-effects (fixed and random effects) logistic regression analyses were carried out. The Intraclass Correlation Coefficient (ICC) and the Median Odds Ratio (MOR) were calculated.
Results: The prevalence of WaSt was 1,682 (4.82%) with a significantly decreasing trend, yielding a percent change of −57.51% (−69.37% to −23.52%) from 2000 to 2019. In the adjusted model, the odds of WaSt increased in boys, children with a shorter preceding birth interval, small birth size, delayed initiation of complementary foods, diarrhea, fever, and anemia, mother’s lack of formal education, and being a farmer, and poor/middle wealth index, and lack of mass media exposure. WaSt was inversely related to the child’s age. Adjusted ICC and MOR were 31.16% and 3.20%, respectively.
Conclusion and recommendations: The study highlights the importance of considering individual and community-level factors to address WaSt, such as timely initiation of complementary foods, improving access to health services, quality diet, and prevention of communicable diseases. Furthermore, programs that have positive impacts on formal education and employment opportunities for girls, as well as that increase access to mass media, are required.
Stunting (linear growth faltering) is chronic undernutrition that prevents children from reaching their physical and cognitive potential (1, 2). On the other hand, wasting (ponderal growth faltering) is a devastating emergency associated with higher mortality risk if not adequately treated (1). Globally, stunting and wasting affected 149.2 million and 45.4 million under-five children, respectively (3). Concurrent wasting and stunting (z scores lower than −2 in both weight for height and height for age) is the co-occurrence of wasting and stunting in a child (4). Until recently, it was believed that wasting and stunting occur independently in a child, and the interaction between them was not considered of public health importance (5). This hypothesis is mainly based on age: stunting increases with age but wasting decreases (4, 6). However, emerging evidence shows a child can have concurrent wasting and stunting (WaSt) (4, 5, 7–9).
The prevalence of WaSt varies according to the burden of wasting and stunting and geographic locations. For example, it was 5% in Karamoja, Uganda (8), 6.2% in Niakhar, Senegal (4), less than 3.5% in Mozambique (5), 5.8% in Kersa, Ethiopia (7), and 5% of Bangladeshi, Indian, and Pakistani children (10). A meta-analysis in 2017 showed that the pooled prevalence of WaSt in 84 countries was 3.0%, ranging from 0 to 8.0% (11). The exact cause of WaSt was not clearly determined. Still, it may share the underlying and fundamental causal factors of wasting and stunting, such as infectious diseases, environmental enteric dysfunction, a diet with inadequate nutrients, and suboptimal infant feeding and caring practices (12, 13). In the body of literature, male sex, child age, cough/ acute respiratory infection, diarrhea, malaria/fever in the last 2 weeks before the survey, multiparity, not treating drinking water at the point of use, conflict, and instability were found to be predictors of WaSt (7, 8, 14).
In the national and international guidelines that were prepared to manage malnutrition, there is no case definition for WaSt (15). Thus, children with WaSt get less attention in the health system and are treated as wasted children. However, they are not only wasted but also stunted, and the interaction between wasting and stunting makes them susceptible to poor health outcomes. As the severe acute malnutrition definition (presence of bilateral pitting edema or severe wasting) does not account for the stunting status of the child, the national and WHO guidelines have no room to identify those children at the highest risk of dying, prompt management, and monitoring either at the community or health institutions level (15). Although WaSt children had the highest mortality risk, they were neglected in the health system due to a lack of case definition and appropriate management protocol (9).
Globally, the Demographic and Health Surveillance (DHS) program was introduced by the United States Agency for International Development (USAID) in 1984 (16). However, in Ethiopia, the first survey was conducted in 2000 by the Central Statistical Agency (17). The surveys have generated nationally representative data on different topics, including demographics, maternal and child health, and nutrition, that provide estimates at the national and regional levels and for urban and rural areas (18). The DHS data was hierarchical or multilevel in structure, i.e., children were nested in the households, and households were nested in the enumeration areas (clusters). Households living in the same clusters may resemble each other more than those households from different clusters as they share similar multiple determinants of health and nutrition (19). Thus, the multilevel logistic regression analysis was carried out to identify predictors of WaSt because it incorporates cluster-specific random effects and leads to more accurate inferential decisions for hierarchical data (19–21).
Several studies have been conducted regarding wasting, stunting, and underweight in Ethiopia (22–28). However, little is known about the prevalence and predictors of WaSt. Thus, with a multi-level analysis approach, this study assessed the trends and predictors of WaSt among children 6–59 months using DHS data from 2000 to 2019.
The data for this study were drawn from nationally representative Ethiopian DHS data conducted in 2000, 2005, 2011, 2016, and 2019. DHS is a nationally representative household survey with a cross-sectional design. Data were collected on various topics, including child health and nutrition (18). It was retrieved from the (DHS) program’s official database website.1 The DHS is conducted every 5 years since 2000 and follows the standard sampling procedure, data collection, and coding (16). The children’s files were used for this study. The Demographic and Health Surveys (DHS) Program data archivist granted permission to use the data for the present study.
The DHS uses two-stage stratified sampling to recruit participants during the surveys. Regions/provinces are stratified into urban and rural areas at stage one. Enumeration areas or clusters from each region are sampled proportional to size. Then, a list of households within the selected EAs was generated as a sampling frame. Later in the second stage, a fixed number of households per cluster was selected from the sampling frame (18).
A total of 34,930 weighted samples (32,620 unweighted samples) were included in the descriptive study. Neither wasted nor stunted children comprise 16,178 (46.31%), while 1,682 (4.82%) were concurrently wasted and stunted. For the multi-level analysis, we included 17,859 weighted samples (17,382 unweighted samples) (Figure 1).
The outcome variable of the study was concurrent wasting and stunting (WaSt). WaSt is defined as a child being wasted and stunted simultaneously (14). The explanatory variables were categorized as individual-level (level-1) and community-level (level-2) factors. The selected child-level and household variables were based on previous studies (4, 5, 7, 8, 11). Child sex (male, female), age in months (6–11, 12–23, 24–35, 36–47, and 48–59 months), preceding birth interval (less than 2 years, 2 years, 3 years, and 4 years and above), birth size (small/very small, average/large), timely initiation of complementary foods (yes/no), received vitamin A in the last 6 months (yes/no), anemia (yes/no), diarrhea, cough, or fever in the 2 weeks before the survey (yes/no) were considered as child-level variables. Education status of the mother (no formal education, have formal education), occupation of the mother (not working, agriculture, business, and others), wealth status (poor, middle, rich), and women decide on health, purchases, and visits either alone or jointly with the partner (yes/no) were considered as household-level variables. In this analysis, individual-level characteristics (level-1) represent the summation of both child-level and household-level variables. Community-level (level-2) variables were residence (urban/rural), round time to get drinking water (water on premises, 30 min or less, more than 30 min), community media exposure (media exposure: newspaper, radio, TV at least once a week), type of toilet (improved, unimproved, or open defecation). The type of toilet is included under the community-level variable because some households use shared toilet facilities. Similarly, as the type of information disseminated may vary from cluster to cluster due to contextual, language, and regional variations, access to mass media was included under the community-level variable.
Data extraction, recoding, and analysis were carried out using STATA version 14 software. Weighted frequencies and percentages were computed for all variables using sampling weight (v005/1,000,000) to account for unequal probability of selection given different population sizes within enumeration areas/ clusters. Multicollinearity between variables was tested using the variance inflation factor (VIF), included those with a VIF less than 5 (19, 29). The cluster number (v001) was considered as a unit of analysis for the community-level factors. Variables with a p-value less than 0.05 in bivariate analysis were selected for multivariable analysis. The following four weighted multilevel logistic regression models: the empty model (with no independent variables), model II (adjusted for individual-level variables only), model III (adjusted for community-level variables only), and model IV (adjusted for both individual-level and community-level variables simultaneously) were fitted. Finally, an adjusted odds ratio (AOR) with a 95% confidence interval (CI) was reported. The Akaike information criterion (AIC), the Bayesian information criterion (BIC), and the log-likelihood ratio test were used to estimate the goodness of fit of the models, where the model with the highest value of the Log-likelihood test and with the lowest values of AIC and BIC was considered to be the best-fit model (21).
Variability across the clusters was measured by the likelihood ratio, Intraclass Correlation Coefficient (ICC), Median Odds Ratio (MOR), and Proportional Change in Variance (PCV). Children living in the same cluster may be more similar than those children living in other clusters as they share similar environments, public health facilities, and other area characteristics (19). The ICC represents the proportion of the total observed individual variation in the concurrent wasting and stunting attributable to between-cluster variation. If the ICC was close to 0, children with concurrent wasting and stunting from the same cluster were no more different from a random sample of children from the general population. On the other hand, if the ICC were close to 1, all children in the same cluster would have the same outcome (30).
The MOR measures how much variability in the WaSt exists between the clusters by comparing two children from two randomly selected different clusters, that is, the odds of WaSt between the child at the cluster with a higher risk of WaSt and the cluster with a lower risk of WaSt (31, 32).
The PCV measures the total variation in concurrent wasting and stunting attributed to individual and community-level factors in the multilevel model (31).
Where Va is the variance in the initial model and Vb is the variance of the model with more terms (31).
The median age of children was 32 months, with the 25th and 75th percentiles of 18 and 46 months. Among them, 17,795 (50.95%) were boys, 15,756 (55.13%) had a preceding birth interval of 2 years or less, and 8,749 (28.80%) had small/very small birth sizes. The prevalence of diarrhea, cough, and fever in the last 2 weeks before the survey was 17.64%, 24.18%, and 17.88%, respectively. Around three-fourths (74.56%) of children had timely initiation of complementary feeding (6–8 months). Only 10,113 (48.83%) of children were not anemic (Table 1).
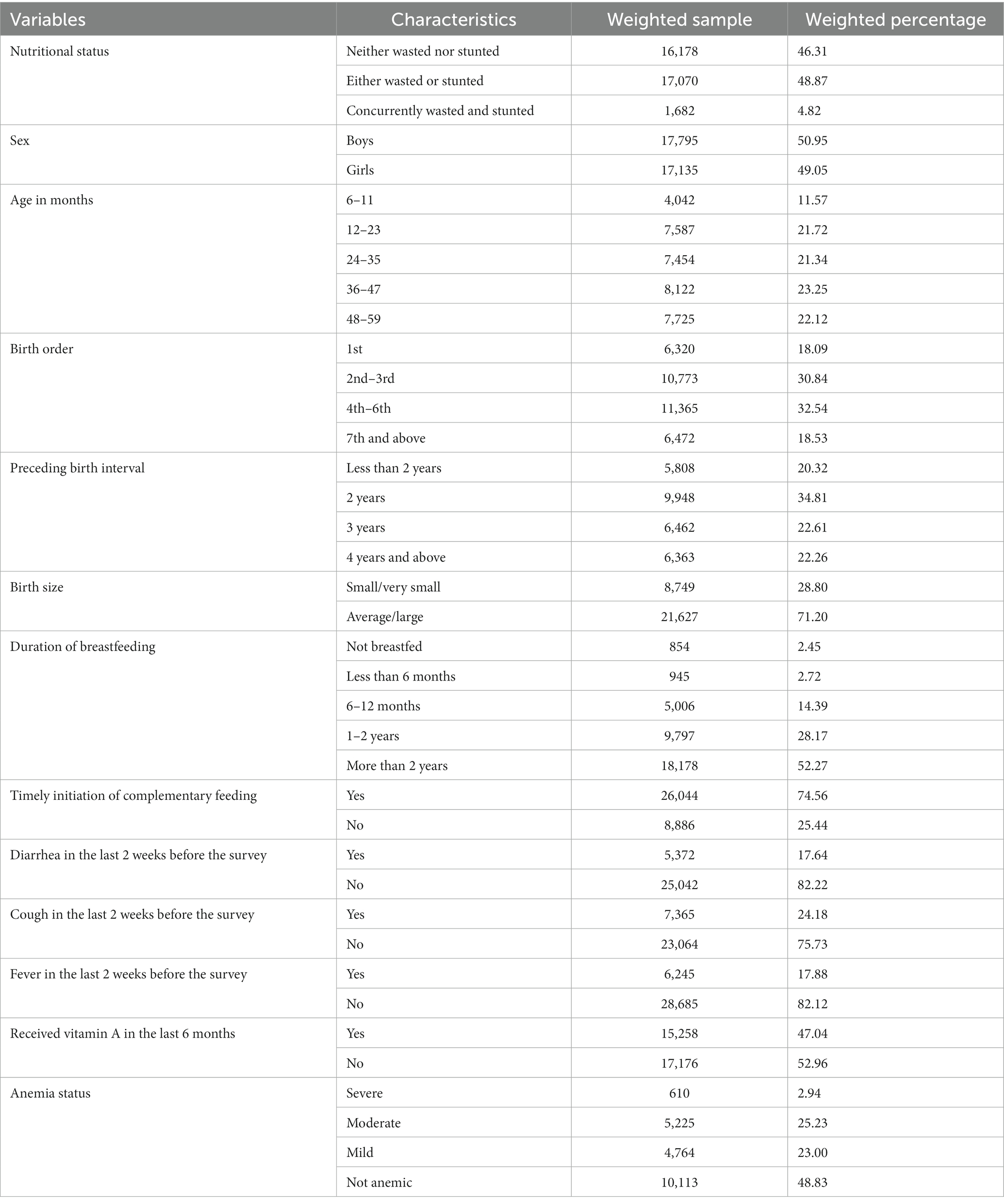
Table 1. Sociodemographic, nutrition and other child-level characteristics in Ethiopia; data from EDHS 2000–2019.
Females led around 4,637 (13.28%) households. Most mothers, 24,816 (71.04%), and more than half of the fathers, 16,249 (54.76%), had no formal education. Also, most mothers 14,580 (47.87%) were not working, while 23,441 (78.38%) fathers were farmers. 11,769 (45.41%) children were from poor households. Only 11,310 (34.56%) women reported that they could decide on health, purchases, and visits alone or jointly with their partner (Table 2).
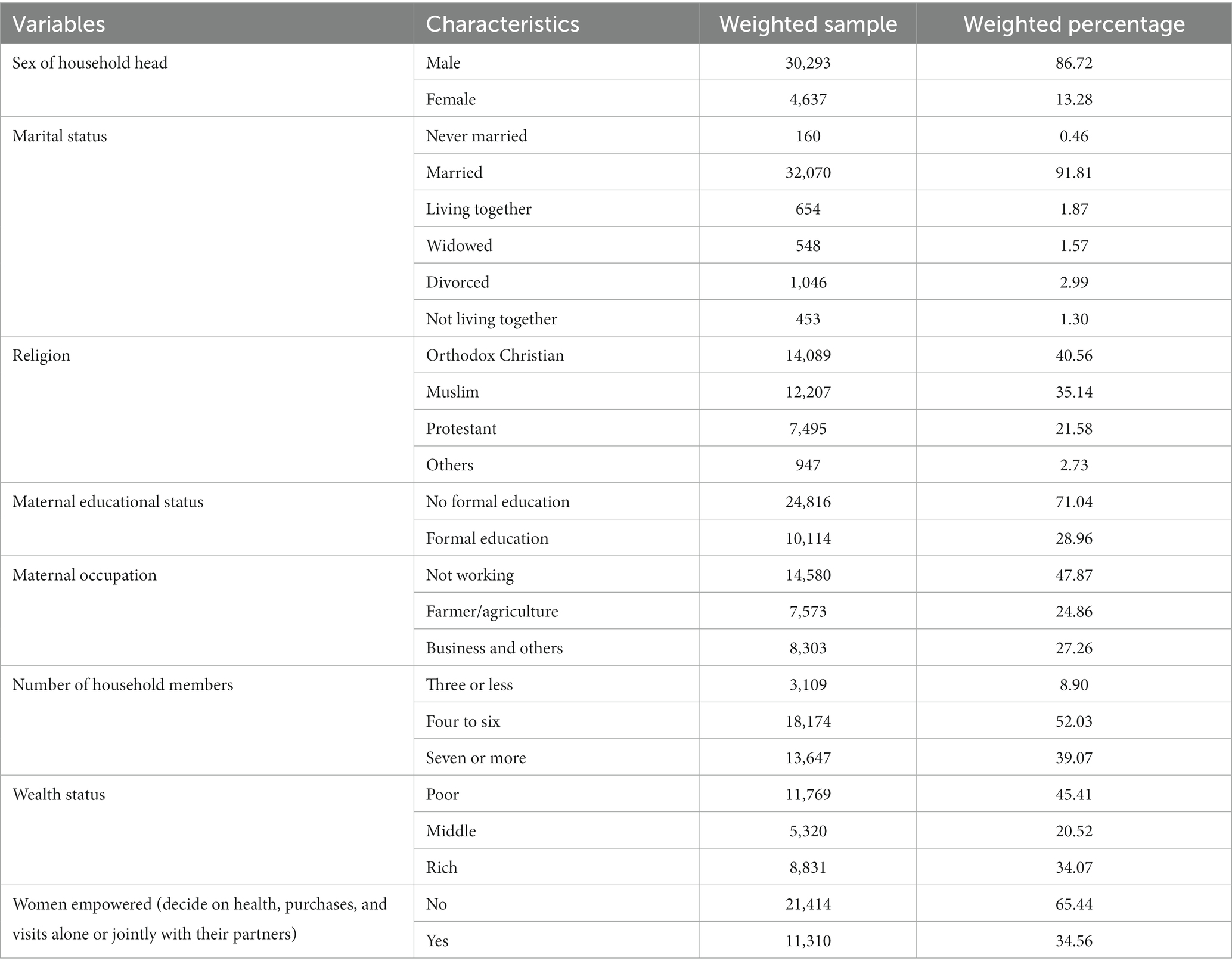
Table 2. Sociodemographic and other household characteristics of parents in Ethiopia; data from EDHS 2000–2019.
Most of the participants live in rural communities (87.33%), consume water from non-piped sources (84.59%), practice open defecation (53.85%), and have no access to newspaper, radio, or television at least once a week (86.03%) (Table 3).
The weighted prevalence of concurrent wasting and stunting was 7.39% in 2000 EDHS, 5.30% in 2005 EDHS, 4.52% in 2011 EDHS, 3.06% in 2016 EDHS, 3.14% in 2019 mini-EDHS, and the overall prevalence was 4.82% in Ethiopia. The prevalence of WaSt sharply increased from 6 to 11 months and peaked at 12 to 23 months. Then, it decreases slowly until 48–59 months (Figure 2).
The trends of WaSt were declining, with a percent change of −57.51% between 2000 and 2019 in Ethiopia (Figure 3). Trends in stunting, wasting, and WaSt from 2000 to 2030 (forecasted for 2030) were presented in Figure 4.
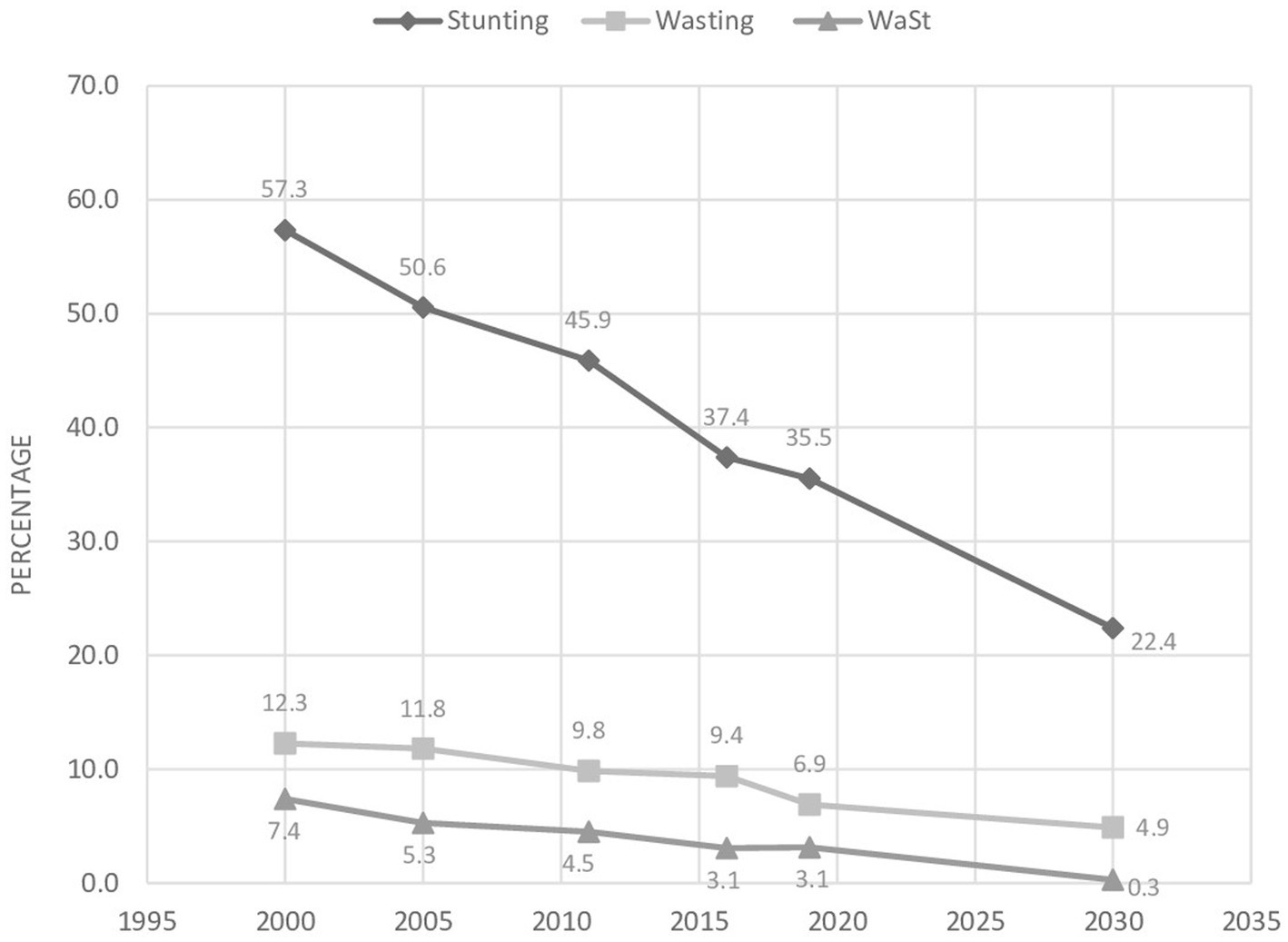
Figure 4. Trends and forecasting of stunting, wasting, and WaSt among children 6–59 months in Ethiopia; data from EDHS 2000–2019.
The factors associated with WaSt in Ethiopia include child sex and age, preceding birth interval, birth size, time of initiation of complementary foods, diarrhea, fever, and anemia, education and occupation of the mother, wealth index, residence, time spent to obtain water, and media exposure. At the individual-level factors, the likelihood of WaSt was high among boys (aOR 1.81, 95% CI 1.49–2.20), children aged 12–23 months (aOR 4.56, 95% CI 3.20–6.50), 24–35 months (aOR 3.51, 95% CI 2.39–5.15), 36–47 months (aOR 2.44, 95% CI 1.65–3.61), and 48–59 months (aOR 1.85, 95% CI 1.22–2.80) compared to children 6–11 months. Shorter preceding birth intervals of less than 2 years (aOR 1.83, 95% CI 1.34–2.49) and 2 years (aOR 1.59, 95% CI 1.20–2.08) were more likely to be associated with concurrent wasting and stunting when compared to preceding birth interval of 4 years/more. Similarly, small/very small children were twice (aOR 2.51, 95% CI 2.05–3.08) higher odds of concurrent wasting and stunting than average/larger birth size children. Timely initiation of complementary foods in 6–8 months had 38% (aOR 0.62, 95% CI 0.49–0.79) lower odds of concurrent wasting and stunting than their counterparts. Children who had diarrhea (aOR 1.57, 95% CI 1.22–2.03) and fever (aOR 1.68, 95% CI 1.25–2.20) in the last two weeks before the survey had higher odds of concurrent wasting and stunting than their counterparts. Children with severe anemia (aOR 4.70, 95% CI 2.91–7.59), moderate anemia (aOR 2.51, 95% CI 1.96–3.21), and mild anemia (aOR 1.88, 95% CI 1.47–2.42) were higher odds of concurrent wasting and stunting than those with no anemia. Lack of formal maternal education (aOR 1.68, 95% CI 1.28–2.19) and being a farmer (aOR 1.39, 95% CI 1.01–1.92) were associated with concurrent wasting and stunting. Also, being from a poor household (aOR 1.98, 95% CI 1.47–2.68) and middle wealth index (aOR 1.70, 95% CI 1.23–2.33) had higher odds of concurrent wasting and stunting than wealthy households. A child from a mother who can decide on health, purchases, and visits to health institutions alone or jointly with the partner had 32% (aOR 0.68, 95% CI 0.56–0.84) lower odds of WaSt than their counterparts.
At the community-level factors, children from households with no access to newspaper, radio, or TV at least once per week had more than twice (aOR 2.55, 95% CI 1.78–3.65) increased odds of concurrent wasting and stung than their counterparts. Being from a rural residence, drinking water not on the premises, and defecating in the open field increase the odds of WaSt in model III but were not significantly associated in the adjusted model (Table 4).
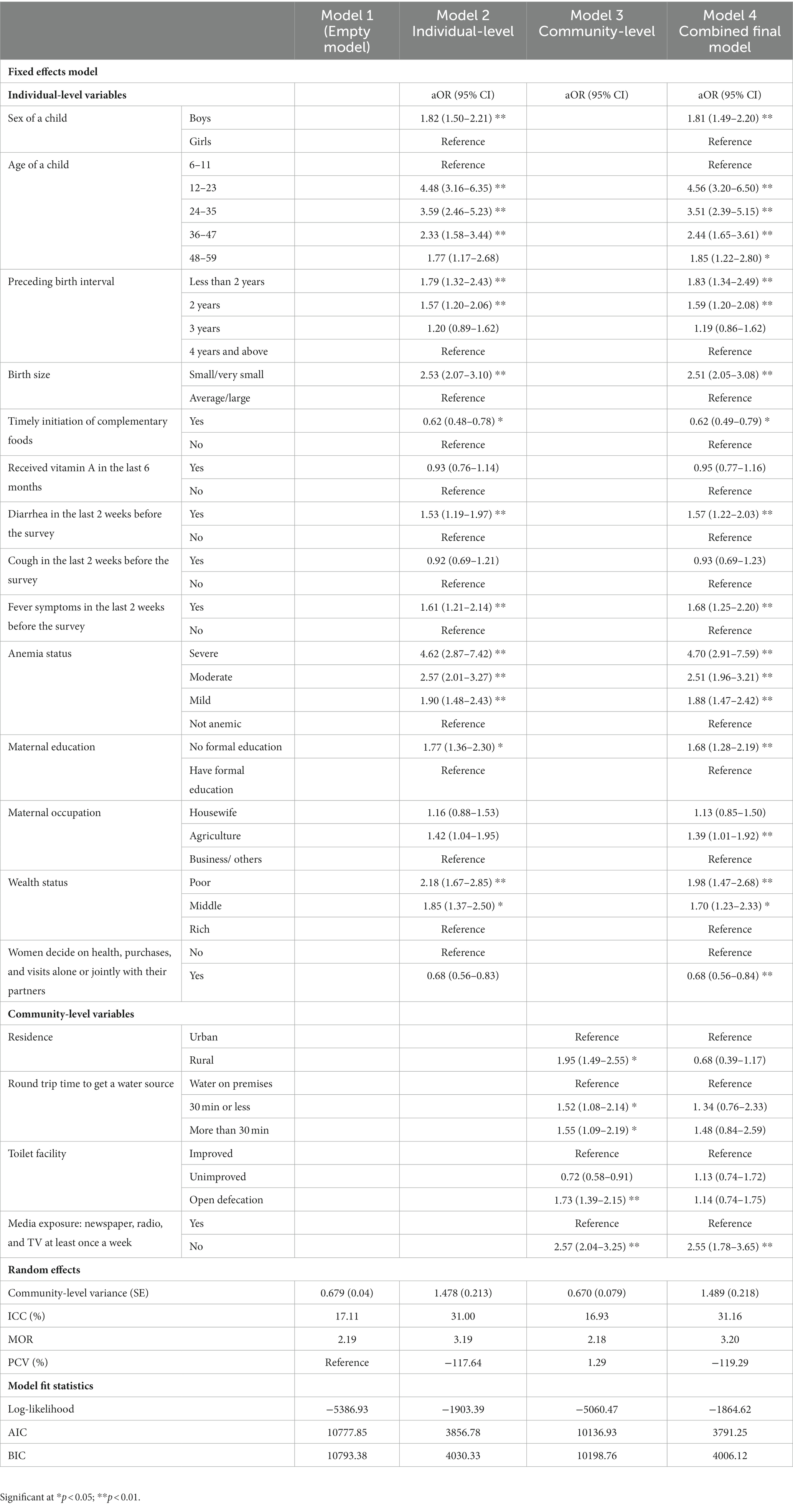
Table 4. Effect of individual and community level factors on concurrent wasting and stunting among children 6–59 months in Ethiopia; data from EDHS 2000–2019.
The empty model depicts that 17.11% of the variance in the odds of WaSt in Ethiopia could be attributed to variation between the clusters (ICC = 0.1711). The variation increased to 31% (ICC = 0.3100) in model-2 when only individual-level variables were fitted. The variation decreased to 16.93% (ICC = 0.1693) in model-3 with only community-level variables and finally increased to 31.16% (ICC = 0.3116) in model-4, which was adjusted for individual and community-level predictors. Model-4, the AIC and BIC values were lower than the previous three models, whereas the Log-likelihood ratio was the highest. Thus, model-4 is the best-fitted model to predict the likelihood of WaSt in Ethiopia. The median odds ratio (MOR) in the best-fitted model (model-4) showed that if a child moved from a cluster with a low risk of WaSt to a cluster with a high risk of WaSt, the median increase in the odds of WaSt would increase by three-fold (MOR = 3.20).
The prevalence of WaSt was 4.82% in Ethiopia. It was comparable with other studies in sub-Saharan Africa: 5% in Karamoja, Uganda (8), 6.2% in Niakhar, Senegal (4), less than 3.5% in Mozambique (5), and 5.8% in Kersa, Ethiopia (7). The trends of WaSt were declining from 7.69% in 2000 to 3.75% in 2019, with a percent change of −57.49% in Ethiopia. However, the percent change was slow from 2016 to 2019 (−1.5%). Based on the data from 2000 to 2019, the prevalence of WaSt, stunting, and wasting by 2030 is forecasted to be 0.28%, 22.4%, and 4.9%, respectively. Thus, with the current rate of reduction and the remaining 8 years (although the achievement is enormous), it’s impractical to end all forms of malnutrition by 2030.
In this study, boys were more likely to be concurrently wasted and stunted than girls. This is compatible with findings from Demographic and Health Surveys of Sub-Saharan Africa (33), a systematic review and meta-analysis (34), and other studies on wasting and stunting (11, 35–38). Some evidence in Ethiopia especially from rural communities shows that boys are preferred over girls and this is reflected in mothers’ health-seeking behavior and contraceptive utilization (39, 40). However, its effect on child-feeding behavior is unknown. Also, the exact cause linking child sex with malnutrition remains unclear. Biologically, hormonally, and immunologically boys are highly susceptible to undernutrition than girls. In terms of biology, boys have higher fat-free mass and a lower fat mass than girls which increases energy demands (4). Also, girls have thicker triceps and subscapular skinfolds than boys, while boys have a lower MUAC-for-age z score than girls, which makes boys more susceptible to undernutrition (4). Others associate gender-based variations with hormonal, immunological, and social factors (41, 42). For example, boys have low levels of growth hormones since the intrauterine life than girls which make them more susceptible to adverse events (43, 44). Similarly, hormones from the hypothalamic-pituitary-gonadal axis (testosterone, early disappearance of luteinizing hormone, and follicle-stimulating hormone) increase the susceptibility of boys to undernutrition than girls (4, 45, 46). However, gender-based variations were not reflected in nutrition policies and programs. Therefore, further studies are needed to understand the linkages and implications for nutrition policy that fill the gap related to sex variations.
WaSt decreases with rising age, suggesting that stunting is a persisting factor while wasting decreases with increasing age; the highest odd was at 12–23 months. This agrees with similar studies conducted elsewhere (4, 8). Since sub-optimal birth outcomes play a significant role in the development of WaSt, the timing of drivers of WaSt is important for preventive measures, including pre-birth and maternal health. A short preceding birth interval of less than or equal to 2 years was associated with WaSt in this study. Research findings showed that children with a short preceding birth interval had increased odds of multiple malnutrition (47), stunting (35, 47, 48), and wasting (49). The shorter birth interval may deplete maternal nutritional stores (both at macronutrient and micronutrient levels), which can negatively affect the health of the mother and child (47, 50). The recovery to the optimal status may be difficult if the mother is malnourished, breastfed the preceding child for an extended period, and carry out energy-demanding laborious work (51).On the other hand, the risk of WaSt increase with the competition between the preceding young child and succeeding infant for available resources, including breast milk, care, and attention from the mother/parents (52). Therefore, all stakeholders should encourage mothers to use modern contraception as early as possible to delay unintended pregnancy and have optimum child spacing.
In the current study, the odds of WaSt for small/very small children were twice higher than their average/larger counterparts. Small birth size may be associated with constrained intrauterine growth due to maternal, placental, fetal, genetic, or a combination of these factors (53). Besides, environmental factors such as smoking, indoor air pollution, and infections were linked with small birth sizes or low birth weight (54). Besides short-term complications, these children suffer from long-term health sequels, including abnormal physical growth and neurodevelopmental outcome (53, 54). Improvement of maternal nutrition and health during pregnancy that can be translated to adequate birth weight is vital to prevent intergenerational malnutrition (55). Antenatal visits are a massive window of opportunity to transmit health and nutrition messages and nutrition-based interventions.
Timely initiation of complementary foods (solid, semi-solid, and soft foods) in 6–8 months reduced the odds of WaSt by 29% in this study. Our study shows the proportion of children who started complementary foods within 6–8 months in Ethiopia was 74.56%. This indicates still one in four children had no access to complementary food. The household structure and composition can influence delayed initiation by influencing resources to the primary caregivers (56). As the child reaches 6 months, nutrient demands exceed what breast milk alone can satisfy. Therefore, the introduction of solid, semi-solid, and soft foods is required at this stage while continuing breastfeeding (57).
In this study, anemic children (severe, moderate, and mild) were at higher odds of WaSt than their non-anemic counterparts. The study also showed a high prevalence (51.17%) of anemia in children, where 28.17% were either moderate or severe anemia. According to the WHO classification (≥40% prevalence), anemia is a severe public health problem in Ethiopia among children (58). Children are at high risk for anemia due to high physiologic demands for growth and development, low iron stores, inadequate dietary intake of bioavailable iron, and iron depletion with frequent infections (59). Besides, poor socio-economic status, maternal anemia, birth spacing, multiple births, preterm and low birth weight, large family size, higher-order birth, rural residence, and low maternal literacy (60–64). Anemia results in growth retardation, impaired motor, and cognitive development, and increased morbidity and mortality (65, 66).
WaSt was associated with the mother’s lack of formal education in this study. This is compatible with a similar study conducted in Uganda (8). Maternal education affects child feeding and caring behavior (67). Similarly, maternal education broadens the knowledge base of optimal child feeding, dietary choices, seeking treatment from health institutions at times of illness, and better decision-making (25, 68–70). On the other hand, women’s age at first marriage, place of residence, and family’s wealth index were significant predictors of women’s education in Ethiopia (71). Thus, addressing the challenges of early marriage and establishing a system that improves their economic status such as access to financial resources, especially for rural uneducated mothers could influence child nutrition. Furthermore, as the mother’s education is an underlying determinant of malnutrition (72), promoting inclusive and equitable quality education by all girls is required according to the fourth sustainable development goal (73).
Children from a low/middle socio-economic status had higher odds of concurrent wasting and stunting compared to wealthy households. This is compatible with previous studies (74, 75). Mothers/parents with lower purchasing power may defer the initiation of complementary feeding, have inadequate access to high-quality and quantity of foods, increased exposure to health risks, compromised hygienic practices, and delay treatment-seeking from appropriate health institutions (76).
Media access to newspaper, radio, or TV at least once a week had 55% lower odds of concurrent wasting and stunting. In Ethiopia, most mothers had no formal education (71.04%) and lived in rural areas (87.33%). Exposure to mass media plays a vital role in reaching mothers with less education, rural residents, and hard-to-transfer health message in person (77). Media access increases mothers’/household members’ knowledge of WASH variables, optimal child feeding, child caring, and appropriate treatment seeking (78).
To the best of our knowledge, this is the first study to assess trends and predictors of WaSt at the national level in Ethiopia. Using multi-level analysis provides information about the efficacy of focusing intervention on clusters instead of individual-level variables only. This study also has a few limitations. First, as DHS data uses a cross-sectional study design, establishing a causal connection between the predictors and WaSt is impossible. Second, since the survey assessed the variables retrospectively, it may be prone to recall bias. Finally, the prevalence data (rather than the incidence rate) underestimate the real burden of wasting and WaSt in the community because a child can experience several acute episodes during a year (2, 79). Therefore, the true burden of WaSt may be much higher than the one reported in cross-sectional studies.
In this study, both individual and community-level factors were associated with concurrent wasting and stunting among children 6–59 months. Our analysis showed that the trends in WaSt are decreasing in Ethiopia. The study highlights the importance of considering individual and community-level factors to address WaSt, such as extra attention to boys and small size birth, empowering women to use family planning to prevent short birth intervals, and encouraging timely initiation of complementary feeding. Likewise, preventing diarrhea, fever, and anemia reduces the odds of WaSt. Furthermore, interventions are required to increase media access to health and nutrition information and improve girls’ education and income/wealth status.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/supplementary material.
The studies involving humans were approved by National Research Ethics Review Committee. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
AR conceptualized the study, obtained and analyzed the data, drafted the manuscript, interpreted the results and critically revised the manuscript. ÖB contributed to the conception of the idea, reviewed the manuscript and provided comments during the manuscript write-up. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AOR, Adjusted Odds Ratio; DHS, Demographic and Health Survey; EDHS, Ethiopia Demographic and Health Survey; ICC, Intra-Correlation coefficient; MOR, Median Odd Ratio; PCV, proportional change in variance; SE, Standard Error; SF, Supplementary File; SGD, Sustainable Development Goal.
1. World Health Organization. Malnutrition, key facts (2021) Available at: https://www.who.int/news-room/fact-sheets/detail/malnutrition (Accessed June 9, 2021).
2. Sadler, K, James, PT, Bhutta, ZA, Briend, A, Isanaka, S, Mertens, A, et al. How can nutrition research better reflect the relationship between wasting and stunting in children? Learnings from the wasting and stunting project. J Nutr. (2022) 152:2645–51. doi: 10.1093/jn/nxac091
3. WHO, UNICEF, International Bank for Reconstruction and Development, The World Bank. Levels and trends in child malnutrition: key findings of the 2021 edition of the joint child malnutrition estimates. Geneva: World Health Organization (2021).
4. Garenne, M, Myatt, M, Khara, T, Dolan, C, and Briend, A. Concurrent wasting and stunting among under-five children in Niakhar, Senegal. Matern Child Nutr. (2019) 15:e12736. doi: 10.1111/mcn.12736
5. Zaba, T, Conkle, J, Nyawo, M, Foote, D, and Myatt, M. Concurrent wasting and stunting among children 6–59 months: an analysis using district-level survey data in Mozambique. BMC Nutr. (2022) 8:15. doi: 10.1186/s40795-022-00508-9
6. Waterlow, J. Classification and definition of protein-calorie malnutrition. Br Med J. (1972) 3:566–9. doi: 10.1136/bmj.3.5826.566
7. Roba, AA, Assefa, N, Dessie, Y, Tolera, A, Teji, K, Elena, H, et al. Prevalence and determinants of concurrent wasting and stunting and other indicators of malnutrition among children 6-59 months old in Kersa, Ethiopia. Matern Child Nutr. (2021) 17:e13172. doi: 10.1111/mcn.13172
8. Obeng-Amoako, GAO, Karamagi, CAS, Nangendo, J, Okiring, J, Kiirya, Y, Aryeetey, R, et al. Factors associated with concurrent wasting and stunting among children 6-59 months in Karamoja, Uganda. Matern Child Nutr. (2021) 17:e13074. doi: 10.1111/mcn.13074
9. McDonald, CM, Olofin, I, Flaxman, S, Fawzi, WW, Spiegelman, D, Caulfield, LE, et al. The effect of multiple anthropometric deficits on child mortality: meta-analysis of individual data in 10 prospective studies from developing countries. Am J Clin Nutr. (2013) 97:896–901. doi: 10.3945/ajcn.112.047639
10. Harding, KL, Aguayo, VM, and Webb, P. Factors associated with wasting among children under five years old in South Asia: implications for action. PLoS One. (2018) 13:e0198749. doi: 10.1371/journal.pone.0198749
11. Khara, T, Mwangome, M, Ngari, M, and Dolan, C. Children concurrently wasted and stunted: a meta-analysis of prevalence data of children 6-59 months from 84 countries. Matern Child Nutr. (2018) 14:e12516. doi: 10.1111/mcn.12516
12. Angood, C, Khara, T, Dolan, C, and Berkley, JA, WaSt Technical Interest Group. Research priorities on the relationship between wasting and stunting. PLoS One. (2016) 11:e0153221. doi: 10.1371/journal.pone.0153221
13. Scrimshaw, NS. Historical concepts of interactions, synergism and antagonism between nutrition and infection. J Nutr. (2003) 133:316S–21S. doi: 10.1093/jn/133.1.316S
14. Myatt, M, Khara, T, Dolan, C, Garenne, M, and Briend, A. Improving screening for malnourished children at high risk of death: a study of children aged 6-59 months in rural Senegal. Public Health Nutr. (2019) 22:862–71. doi: 10.1017/S136898001800318X
15. Government of Ethiopia FMoH. National guideline for the management of acute malnutrition. Addis Ababa: FMOH (2019).
16. Rutstein, SO, and Rojas, G. Guide to DHS statistics. Demographic and Health Surveys. Calverton, MD: ORC Macro (2006).
17. Central Statistical Authority [Ethiopia] and ORC Macro. Ethiopia Demographic and Health Survey 2000. Addis Ababa, Ethiopia and Calverton, MD, USA: Central Statistical Authority and ORC Macro (2001).
18. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, MD, USA: CSA and ICF (2016).
19. Zewude, BT, Debusho, LK, and Diriba, TA. Multilevel logistic regression modelling to quantify variation in malaria prevalence in Ethiopia. PLoS One. (2022) 17:e0273147. doi: 10.1371/journal.pone.0273147
20. Bolarinwa, OA, Tessema, ZT, Frimpong, JB, Babalola, TO, Ahinkorah, BO, and Seidu, AA. Spatial distribution and factors associated with adolescent pregnancy in Nigeria: a multi-level analysis. Arch Public Health. (2022) 80:43. doi: 10.1186/s13690-022-00789-3
22. Yeshaneh, A, Mulu, T, Gasheneit, A, and Adane, D. Prevalence of wasting and associated factors among children aged 6-59 months in Wolkite town of the Gurage zone, southern Ethiopia, 2020. A cross-sectional study. PLoS One. (2022) 17:e0259722. doi: 10.1371/journal.pone.0259722
23. Habtamu, E, Chilo, D, and Desalegn, D. Determinants of wasting among children aged 6-59 months in Wonago woreda, South Ethiopia. A facility-based unmatched case-control study. PLoS One. (2022) 17:e0269380. doi: 10.1371/journal.pone.0269380
24. Chekol, YT, Arefaynie, M, Kassa, AA, Alene, TD, and Ngusie, HS. Determinants of wasting among children aged 6-59 months in north-East Ethiopia: a community-based case-control study. BMJ Open. (2022) 12:e057887. doi: 10.1136/bmjopen-2021-057887
25. Hiruy, AF, Xiong, Q, Jin, Q, Zhao, J, Lin, X, He, S, et al. The association of feeding practices and sociodemographic factors on underweight and wasting in children in Ethiopia: a secondary analysis of four health surveys from 2000 to 2016. J Trop Pediatr. (2021) 67:fmab047. doi: 10.1093/tropej/fmab047
26. Motbainor, A, Worku, A, and Kumie, A. Stunting is associated with food diversity while wasting with food insecurity among underfive children in east and West Gojjam zones of Amhara region, Ethiopia. PLoS One. (2015) 10:14. doi: 10.1371/journal.pone.0133542
27. Tesfaye, A, and Egata, G. Stunting and associated factors among children aged 6-59 months from productive safety net program beneficiary and non-beneficiary households in meta district, east Hararghe zone, eastern Ethiopia: a comparative cross-sectional study. J Health Popul Nutr. (2022) 41:13. doi: 10.1186/s41043-022-00291-0
28. Ayelign, A, and Zerfu, T. Household, dietary and healthcare factors predicting childhood stunting in Ethiopia. Heliyon. (2021) 7:e06733. doi: 10.1016/j.heliyon.2021.e06733
29. Midi, H, Sarkar, SK, and Rana, S. Collinearity diagnostics of binary logistic regression model. J Interdiscip Math. (2010) 13:253–67. doi: 10.1080/09720502.2010.10700699
30. Austin, PC, and Merlo, J. Intermediate and advanced topics in multilevel logistic regression analysis. Stat Med. (2017) 36:3257–77. doi: 10.1002/sim.7336
31. Merlo, J, Chaix, B, Ohlsson, H, Beckman, A, Johnell, K, Hjerpe, P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. (2006) 60:290–7. doi: 10.1136/jech.2004.029454
32. Larsen, K, Petersen, JH, Budtz-Jørgensen, E, and Endahl, L. Interpreting parameters in the logistic regression model with random effects. Biometrics. (2000) 56:909–14. doi: 10.1111/j.0006-341X.2000.00909.x
33. Garenne, M, Thurstans, S, Briend, A, Dolan, C, Khara, T, Myatt, M, et al. Changing sex differences in undernutrition of African children: findings from demographic and health surveys. J Biosoc Sci. (2021) 54:847–57. doi: 10.1017/S0021932021000468
34. Susan, T, Charles, O, Andrew, S, Jonathan, W, Tanya, K, Carmel, D, et al. Boys are more likely to be undernourished than girls: a systematic review and meta-analysis of sex differences in undernutrition. BMJ Glob Health. (2020) 5:e004030. doi: 10.1136/bmjgh-2020-004030
35. Yaya, S, Oladimeji, O, Odusina, EK, and Bishwajit, G. Household structure, maternal characteristics and children's stunting in sub-Saharan Africa: evidence from 35 countries. Int Health. (2020) 14:381–9. doi: 10.1093/inthealth/ihz105
36. Ali, Z, Saaka, M, Adams, A-G, Kamwininaang, SK, and Abizari, A-R. The effect of maternal and child factors on stunting, wasting and underweight among preschool children in northern Ghana. BMC Nutr. (2017) 3:1–13. doi: 10.1186/s40795-017-0154-2
37. Bork, KA, and Diallo, A. Boys are more stunted than girls from early infancy to 3 years of age in rural Senegal. J Nutr. (2017) 147:940–7. doi: 10.3945/jn.116.243246
38. Samuel, A, Osendarp, SJM, Feskens, EJM, Lelisa, A, Adish, A, Kebede, A, et al. Gender differences in nutritional status and determinants among infants (6-11 m): a cross-sectional study in two regions in Ethiopia. BMC Public Health. (2022) 22:12. doi: 10.1186/s12889-022-12772-2
39. Gelaw, YA, Biks, GA, and Alene, KA. Effect of residence on mothers’ health care seeking behavior for common childhood illness in Northwest Ethiopia: a community based comparative cross – sectional study. BMC Res Notes. (2014) 7:705. doi: 10.1186/1756-0500-7-705
40. Tilahun, T, Coene, G, Temmerman, M, and Degomme, O. Spousal discordance on fertility preference and its effect on contraceptive practice among married couples in Jimma zone, Ethiopia. Reprod Health. (2014) 11:27. doi: 10.1186/1742-4755-11-27
41. van Lunzen, J, and Altfeld, M. Sex differences in infectious diseases-common but neglected. J Infect Dis. (2014) 209:S79–80. doi: 10.1093/infdis/jiu159
42. Garenne, M. Demographic evidence of sex differences in vulnerability to infectious diseases. J Infect Dis. (2015) 211:331–2. doi: 10.1093/infdis/jiu448
43. Alur, P. Sex differences in nutrition, growth, and metabolism in preterm infants. Front Pediatr. (2019) 7:22. doi: 10.3389/fped.2019.00022
44. Geary, MP, Pringle, PJ, Rodeck, CH, Kingdom, JC, and Hindmarsh, PC. Sexual dimorphism in the growth hormone and insulin-like growth factor axis at birth. J Clin Endocrinol Metabol. (2003) 88:3708–14. doi: 10.1210/jc.2002-022006
45. Renault, CH, Aksglaede, L, Wøjdemann, D, Hansen, AB, Jensen, RB, and Juul, A. Minipuberty of human infancy – a window of opportunity to evaluate hypogonadism and differences of sex development? Ann Pediatr Endocrinol Metab. (2020) 25:84–91. doi: 10.6065/apem.2040094.047
46. Bizzarri, C, and Cappa, M. Ontogeny of hypothalamus-pituitary gonadal axis and minipuberty: an ongoing debate? Front Endocrinol (Lausanne). (2020) 11:187. doi: 10.3389/fendo.2020.00187
47. Shifti, DM, Chojenta, C, Holliday, EG, and Loxton, D. Maternal anemia and baby birth size mediate the association between short birth interval and under-five undernutrition in Ethiopia: a generalized structural equation modeling approach. BMC Pediatr. (2022) 22:108. doi: 10.1186/s12887-022-03169-6
48. Dessie, ZB, Fentie, M, Abebe, Z, Ayele, TA, and Muchie, KF. Maternal characteristics and nutritional status among 6-59 months of children in Ethiopia: further analysis of demographic and health survey. BMC Pediatr. (2019) 19:83. doi: 10.1186/s12887-019-1459-x
49. Darsene, H, Geleto, A, Gebeyehu, A, and Meseret, S. Magnitude and predictors of undernutrition among children aged six to fifty nine months in Ethiopia: a cross sectional study. Arch Public Health. (2017) 75:29. doi: 10.1186/s13690-017-0198-4
50. Dewey, KG, and Cohen, RJ. Does birth spacing affect maternal or child nutritional status? A systematic literature review. Matern Child Nutr. (2007) 3:151–73. doi: 10.1111/j.1740-8709.2007.00092.x
51. Aizenman, D. Impact of family planning on maternal-child health. The future of humanity depends on our children. Profamilia. (1988) 4:28–33.
52. Ronsmans, C. Birth spacing and child survival in rural Senegal. Int J Epidemiol. (1996) 25:989–97. doi: 10.1093/ije/25.5.989
53. Sharma, D, Shastri, S, and Sharma, P. Intrauterine growth restriction: antenatal and postnatal aspects. Clin Med Insights Pediatr. (2016) 10:67–83. doi: 10.4137/CMPed.S40070
54. Ramakrishnan, U. Nutrition and low birth weight: from research to practice. Am J Clin Nutr. (2004) 79:17–21. doi: 10.1093/ajcn/79.1.17
55. Rahman, MS, Howlader, T, Masud, MS, and Rahman, ML. Association of low-birth weight with malnutrition in children under five years in Bangladesh: do mother’s education, socio-economic status, and birth interval matter? PLoS One. (2016) 11:e0157814. doi: 10.1371/journal.pone.0157814
56. Irenso, AA, Zheng, M, Campbell, KJ, Chamberlain, D, and Laws, R. The influence of household structure and composition on the introduction of solid, semisolid and soft foods among children aged 6–8 months: an analysis based on Ethiopia Demographic and Health Surveys. Matern Child Nutr. 19:e13429. doi: 10.1111/mcn.13429
57. WHO, UNICEF. Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF) (2021).
58. World Health Organization. Prevalence of anaemia in children aged 6–59 months (%) [Internet]. The Global Health Observatory. (2021) [citado el 28 de julio de 2021]. 2022.
59. Ramakrishnan, U. Functional consequences of nutritional anemia during pregnancy and early childhood. Boca Raton, FL: CRC Press LLC (2001).
60. Tesema, GA, Worku, MG, Tessema, ZT, Teshale, AB, Alem, AZ, Yeshaw, Y, et al. Prevalence and determinants of severity levels of anemia among children aged 6–59 months in sub-Saharan Africa: a multilevel ordinal logistic regression analysis. PLoS One. (2021) 16:e0249978. doi: 10.1371/journal.pone.0249978
61. Gebrie, A, and Alebel, A. A systematic review and meta-analysis of the prevalence and predictors of anemia among children in Ethiopia. Afr Health Sci. (2020) 20:2007–21. doi: 10.4314/ahs.v20i4.59
62. Pasricha, S-R, Black, J, Muthayya, S, Shet, A, Bhat, V, Nagaraj, S, et al. Determinants of anemia among young children in rural India. Pediatrics. (2010) 126:e140–9. doi: 10.1542/peds.2009-3108
63. Salah, RW, Hasab, AAH, El-Nimr, NA, and Tayel, DI. The prevalence and predictors of iron deficiency anemia among rural infants in nablus governorate. J Res Health Sci. (2018) 18:e00417
64. Lweno, O, Hertzmark, E, Darling, AM, Noor, R, Bakari, L, Sudfeld, C, et al. The high burden and predictors of anemia among infants aged 6 to 12 months in Dar Es Salaam. Tanzania Food Nutr Bull. (2022) 43:68–83. doi: 10.1177/03795721211007009
65. Grantham-McGregor, S, and Ani, C. A review of studies on the effect of iron deficiency on cognitive development in children. J Nutr. (2001) 131:649S–68S. doi: 10.1093/jn/131.2.649S
66. Phiri, KS, Calis, JC, Faragher, B, Nkhoma, E, Ng'oma, K, Mangochi, B, et al. Long term outcome of severe anaemia in Malawian children. PLoS One. (2008) 3:e2903. doi: 10.1371/journal.pone.0002903
67. Akombi, BJ, Agho, KE, Hall, JJ, Wali, N, Renzaho, AM, and Merom, D. Stunting, wasting and underweight in sub-Saharan Africa: a systematic review. Int J Environ Res Public Health. (2017) 14:863. doi: 10.3390/ijerph14080863
68. Oyekale, AS. Factors explaining acute malnutrition among under-five children in sub-Sahara Africa (SSA). Life Sci J. (2012) 9:2101–7.
69. Keats, A. Women's schooling, fertility, and child health outcomes: evidence from Uganda's free primary education program. J Dev Econ. (2018) 135:142–59. doi: 10.1016/j.jdeveco.2018.07.002
70. Birungi, A, Koita, Y, Roopnaraine, T, Matsiko, E, and Umugwaneza, M. Behavioural drivers of suboptimal maternal and child feeding practices in Rwanda: an anthropological study. Matern Child Nutr. (2022) 19:e13420. doi: 10.1111/mcn.13420
71. Hussen, NM, and Workie, DL. Multilevel analysis of women’s education in Ethiopia. BMC Womens Health. (2023) 23:197. doi: 10.1186/s12905-023-02380-6
72. Bhutta, ZA, Ahmed, T, Black, RE, Cousens, S, Dewey, K, Giugliani, E, et al. What works? Interventions for maternal and child undernutrition and survival. Lancet. (2008) 371:417–40. doi: 10.1016/S0140-6736(07)61693-6
74. Gwatkin, DR, Rutstein, S, Johnson, K, Suliman, E, Wagstaff, A, and Amouzou, A. Socio-economic differences in health, nutrition, and population. Washington, DC: The World Bank. (2007):1–301.
75. Van de Poel, E, Hosseinpoor, AR, Speybroeck, N, Van Ourti, T, and Vega, J. Socioeconomic inequality in malnutrition in developing countries. Bull World Health Organ. (2008) 86:282–91. doi: 10.2471/BLT.07.044800
76. Victora, CG, Wagstaff, A, Schellenberg, JA, Gwatkin, D, Claeson, M, and Habicht, J-P. Applying an equity lens to child health and mortality: more of the same is not enough. Lancet. (2003) 362:233–41. doi: 10.1016/S0140-6736(03)13917-7
77. Fatema, K, and Lariscy, JT. Mass media exposure and maternal healthcare utilization in South Asia. SSM Popul Health. (2020) 11:100614. doi: 10.1016/j.ssmph.2020.100614
78. Alexander, CC, Shrestha, S, Tounkara, MD, Cooper, S, Hunt, L, Hoj, TH, et al. Media access is associated with knowledge of optimal water, sanitation and hygiene practices in Tanzania. Int J Environ Res Public Health. (2019) 16:1963. doi: 10.3390/ijerph16111963
79. Huybregts, L, Le, PA, Becquey, E, Zongrone, A, Barba, FM, Rawat, R, et al. Impact on child acute malnutrition of integrating small-quantity lipidbased nutrient supplements into community-level screening for acute malnutrition: a cluster-randomized controlled trial in Mali. PLoS Med. (2019) 16:e1002892. doi: 10.1371/journal.pmed.1002892
Keywords: Trends, predictors, concurrent wasting and stunting, multi-level analysis, DHS
Citation: Roba AA and Başdaş & (2023) Multilevel analysis of trends and predictors of concurrent wasting and stunting among children 6–59 months in Ethiopia from 2000 to 2019. Front. Nutr. 10:1073200. doi: 10.3389/fnut.2023.1073200
Received: 18 October 2022; Accepted: 10 August 2023;
Published: 01 September 2023.
Edited by:
Julie Hess, Grand Forks Human Nutrition Research Center, Agricultural Research Service (USDA), United StatesReviewed by:
Devika Suri, University of Wisconsin-Madison, United StatesCopyright © 2023 Roba and Başdaş. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aklilu Abrham Roba, YWtsaWx0aW1uYXRoc2VyYWhAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.