- 1Global Health Institute, School of Public Health, Wuhan University, Wuhan, China
- 2School of Public Health, Zhejiang University, Hangzhou, China
- 3Nanjing Lishui District Hospital of Traditional Chinese Medicine, Nanjing, China
Background: Lower health-related quality of life (HRQoL) can result in adverse effects on the health of older people. This study aims to explore the relationship between personal social capital (PSC) and HRQoL among Chinese elderly people from rural-and-urban perspective.
Materials and methods: 4,802 samples were included from China’s health-related quality of life Survey for Older Adults 2018 (CHRQLS-OA 2018). The PSC, including bonding and bridging social capital (BOC and BRC), was measured by the Chinese version of the Personal Social Capital Scale (PSCS-16). The HRQoL was evaluated by the European Five Dimensions Questionnaire (EQ-5D-3L). Linear and Tobit regression models were conducted to examine the relationship between PSC and HRQoL.
Results: The BOC and BRC of rural older people were significantly lower than those of urban older people. Pain/discomfort and anxiety/depression were the most significant health problems affecting the older samples. In the five dimensions, the proportion of rural older people with problems was higher than that of urban older people. Among rural older people, BOC was significantly related to self-rated health and EQ-5D utility index (p < 0.05); while BRC was insignificantly associated with self-rated health (p > 0.05) but related to EQ-5D utility index (p < 0.05). Both BOC and BRC were significantly correlated with self-rated health and EQ-5D utility index (p < 0.05) among urban older people.
Conclusion: Our study reveals older people’s worrying PSC and HRQoL status. The relationship between PSC and HRQoL suggested that more social support and care of intimates should be encouraged to increase the PSC of older people, especially rural older people.
Introduction
Aging has become a major global public health issue, with an estimated 1.5 billion people aged 60 and over worldwide by 2030 (1). As one low-and middle-income country with the largest population globally, the aging process in China is much faster than in many other countries worldwide in terms of growth rate and proportion (2). The Chinese population over 60 years old has been to 264.02 million, accounting for about 18.70% of the total population in 2020 (3). In contrast, the number of people over 60 years old in China is estimated to increase to 420 million by 2035 (4), indicating that China’s aging situation is becoming increasingly severe. Besides, due to the deterioration of the physical functions of the older people with ages, most of them may suffer from certain kinds of diseases, especially chronic diseases (5–7), which will directly affect their health-related quality of life (HRQoL).
According to World Health Organization (WHO), HRQoL refers to that individuals’ perception of their position in life in the context of the culture and value systems in which they live and concerning their goals, expectations, standards, and concerns (8). HRQoL reflects the multi-dimensions of health, including physiology, psychology, social function, subjective judgment, and life satisfaction (9). Developed countries first researched HRQoL and mainly focused on the population of children (10, 11), women (12, 13), and patients (14, 15). However, they pay more attention to the older people currently because aging has become one of the global public issues (16–18). Most researchers studied HRQoL of the older people on influencing factors, and have proven that demographic factors (e.g., gender, age, marital status, and living areas) (19–22), health-related behaviors (e.g., drinking, smoking) (23, 24), and chronic diseases (25) can affect the HRQoL of the older people. With the development of the economy and the change in social perception, researchers also found that socioeconomic factors such as income, educational levels, and employment were related to the HRQoL of older people (26). In addition, previous studies have also proved that social relationships (e.g., social capital) were associated with individual health (27–29).
Social capital is regarded as the sum of resources and values based on a network of personal and organizational relationships (30). It describes the characteristics of a society that can achieve common goals (31). Considering the difficulty of collecting collective social capital, most studies focus on personal social capital (PSC). PSC can be further distinguished into two dimensions: bonding social capital (BOC) and bridging social capital (BRC) (32). BOC refers to the trust and cooperation between similar members with some social demographic factors (such as age, social status, etc.), while BRC means connections between community residents whose status and power are different (30). Social capital, as a kind of actual or potential resource, many studies have proved that it plays a key role whether on a personal or collective level (33). To date, current studies have found that collective-level social capital was positive associated with HRQoL (34, 35), but limited research exists on the relationship between PSC and HRQoL of the older people. Due to the tremendous socioeconomic and health disparities between urban and rural areas in China, this study was conducted from the perspective of urban-rural differences. The hypothesis of this study is that the PSC (BOC and BRC) is related to HRQoL positively among rural and urban older people. Moreover, rare studies distinguish between BOC and BRC while elaborating on the association between PSC and HRQoL. Thus, this study aimed to explore the relationship between PSC (BOC and BRC) and HRQoL among Chinese older people. Considering the other developing countries with huge populations, such as India, Brazil, and so on, Chinese experience on the suggestions about the relationship between HRQoL and PSC among older people can offer certain reference.
Materials and methods
Design and participants
The date of this study was obtained from China’s Health-Related Quality of Life Survey for Older Adults 2018 (CHRQLS-OA 2018) (36). This cross-sectional survey was conducted during the Spring Festival in 2018, and intended to explore the health status of the Chinese older people aged 60 years old and above. We used convenient sampling to collect data and the survey sites including Henan province, Hubei province, Fujian province, Jiangsu province, etc. According to the study design, volunteers met the following inclusion criteria were considered as our target population: (1) individuals aged 60 years old or above, (2) individuals who voluntarily participated in our survey. But not all participants were included. Therefore, the excluded criteria were (1) individuals who could not conduct normal conversation because of aphasia, deafness, or other critical body illnesses, (2) individuals who had severe mental disorders or had been diagnosed with cognitive impairment, (3) individuals who had lost their daily living abilities. The questionnaire included participants’ sociodemographic characteristics, personal social capital, behaviors, lifestyles, mental health, HRQoL, coping styles, etc. Overall, we collected 5,638 questionnaires and 5,442 were valid after data quality control, of which 4,807 were offline samples with an effective rate of 85.26%.
Since the purpose of this study was to explore the relationship between the personal social capital of the elderly and HRQoL, respondents with missing values on personal social capital and EQ-5D were excluded. Finally, 4,802 samples of the older people aged 60 years and above were included in the study.
Measures
Assessment of personal social capital
The Chinese Version of the Personal Social Capital Scale (PSCS-16) was adopted to measure PSC (37). The PSCS-16 contains 16 questions, composed of two sub-scales: BOC and BRC, both are formed from four sub-items and each sub-item contains two questions. The BOC contains (a) the perceived social network size, (b) the number of trusted social network members, (c) the number of social network members with resources (such as professional work and social influence), and (d) the number of reciprocal social network members; similarly, the BRC contains (a) perceived group size, (b) whether the group represents an individual, (c) resources owned by these groups and (d) the likelihood of getting help from the group on request (38). These response options of 16 questions were assessed using a five points Likert scale (1 = all, 2 = most, 3 = some, 4 = a few, and 5 = none). The average of two related questions’ score is the score for this sub-item, with an overall range of 8–40 points. To be consistent with the EQ-5D scores, the PSCS adopted reverse–code statistically. A higher score indicated that participants possessed more personal social capital.
The PSCS-16 has proven reliable and valid in China (19). In this study, Cronbach’s alpha of PSCS-16 total scale, BOC and BRC were 0.965, 0.932, and 0.965, and Kaiser-Meyer-Olkin (KMO) were 0.855, 0.919, and 0.953, respectively.
Assessment of health-related quality of life
Health-related quality of life was measured using the European Five Dimensions Questionnaire (EQ-5D-3L), which consisted of the EQ-5D descriptive system, the European Five Dimensions Questionnaire Visual Analogue Scale (EQ- VAS) and the Utility Index. The EQ-5D descriptive system measured participants’ health status in three levels of severity (no problems, moderate problems, and extreme problems) with five dimensions: Mobility (MO), Self-care (SC), Usual activities (UA), Pain/discomfort (PD), Anxiety/depression (AD) (39). The EQ-VAS score was recorded on a scale with anchor points 0 (worst health state) and 100 (best health state), which reflected their knowledge of health (40).
The EQ-5D utility index system refers to converting the combination of problems in the five dimensions of EQ-5D into a total utility score to evaluate the overall quality of life of the sample population. A higher EQ-5D utility index indicated higher levels of HRQoL (41). This study adopted the utility index system developed by Zhuo et al. (42), a model ranging from 0.1702 to 1.0000.
Previous studies have confirmed EQ-5D-3L’s reliability and validity in China (25). The Cronbach’s alpha of EQ-5D-3L was 0.786, and KMO was 0.788 in the study.
Basic demographic characteristics
The basic demographic information of this study included participants’ sociodemographic characteristics (gender, age, marital status, residence), socioeconomic status (annual family income per capita, educational levels, employment), number of chronic diseases and healthy behaviors (smoking, drinking, exercise, number of chronic diseases).
Statistical analysis
Data were analyzed using Statistical Package for the Social Sciences (SPSS) version 22.0 (SPSS Inc., Chicago, IL, USA) and Stata SE 16.0, with a 95% Confidence Interval (CI) and a statistical significance level of 0.05.
Categorical variables were represented by frequencies and proportions, while metric variables were expressed as mean and standard deviation. The chi-square test was used to test whether there was a difference in sociodemographic characteristics between urban and rural areas and univariate analysis of five dimensions in EQ-5D-3L. Differences in each dimension of personal social capital between rural and urban areas, single factor analysis of EQ-VAS and EQ-5D utility index score among samples with different demographic characteristics were carried out using T-test and Analysis of Variance (ANOVA). The association between personal social capital and five dimensions of EQ-5D was examined by multiple linear regression, which included one initial model and four adjusted models. Linear regression and Tobit regression were, respectively used to analyse the relationship between the social capital of the older people and EQ-VAS and EQ-5D utility scores.
Results
General sociodemographic characteristics of respondents
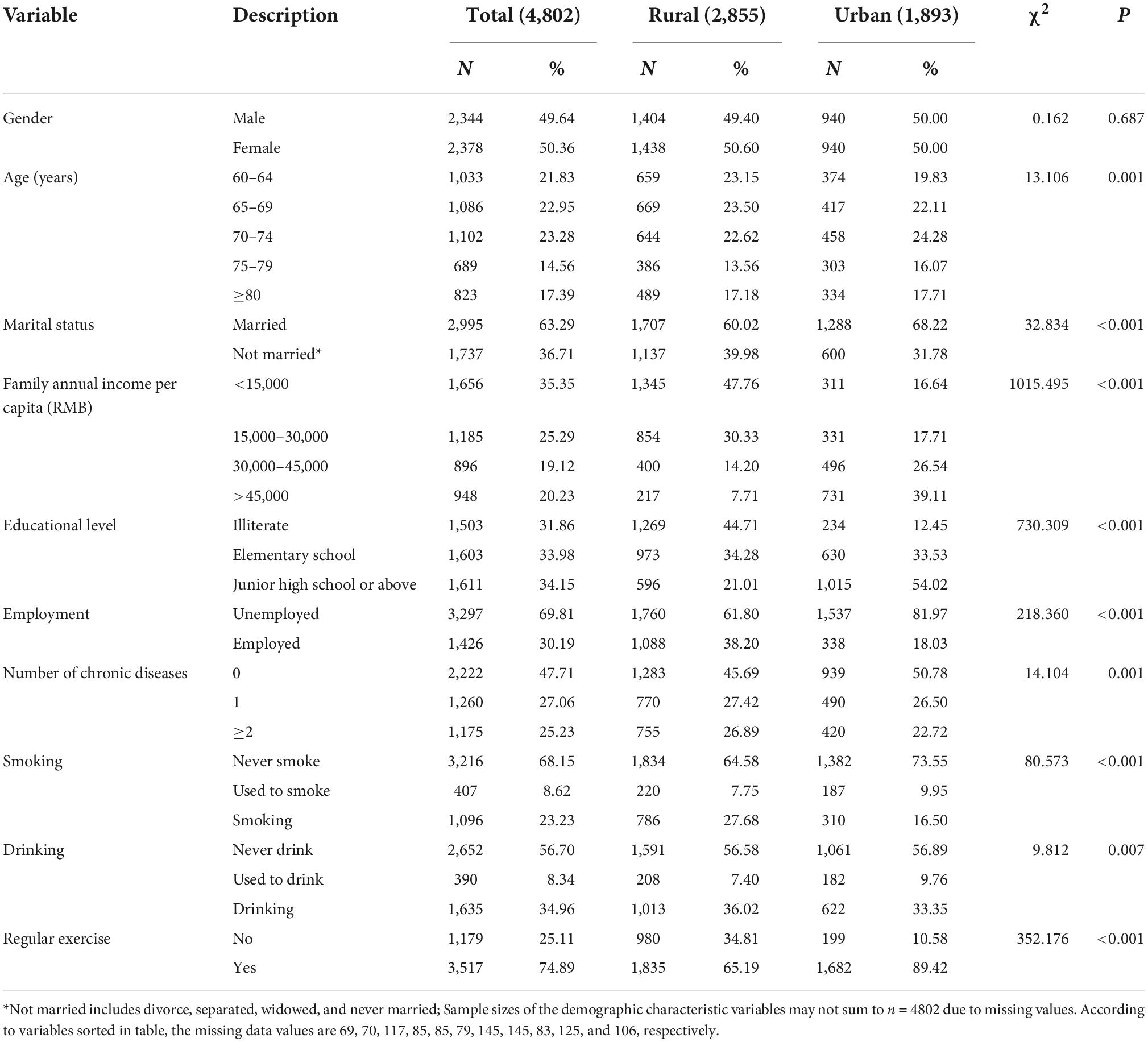
As shown in Table 1, this study consisted of 4,802 older adults; all samples were divided into two groups, among whom 59.45% (n = 2,855) were from rural areas and 40.54% (n = 1,893) were from urban areas.
Overall, of the participants, 49.64% were males and 50.36% were females. Nearly half of older people (44.78%) were under 70 years old, while 17.39% were over 80 years old. Most respondents (63.29%) were currently married. The annual family income per capita of less than 15,000 yuan accounted for the majority of the respondents (35.35%). Over half of the participants had received an education (68.13%), and 69.81% were reported without occupations. There were 52.29% of the samples suffered from chronic diseases, and the proportion of both non-smokers and non-drinkers was over 50% (68.15%, 56.70%, respectively). 74.89% of older people do regular exercise.
The following characteristics were found to be significant statistically differences across these two groups: age (χ2 = 13.106, p = 0.011), marital status (χ2 = 32.834, p < 0.001), family annual income per capita (χ2 = 1015.495, p < 0.001), educational level (χ2 = 730.309, p < 0.001), employment (χ2 = 218.360, p < 0.001), number of chronic diseases (χ2 = 14.104, p = 0.001), smoking (χ2 = 80.673, p < 0.001), drinking (χ2 = 9.812, p = 0.007), and regular exercise (χ2 = 352.176, p < 0.001).
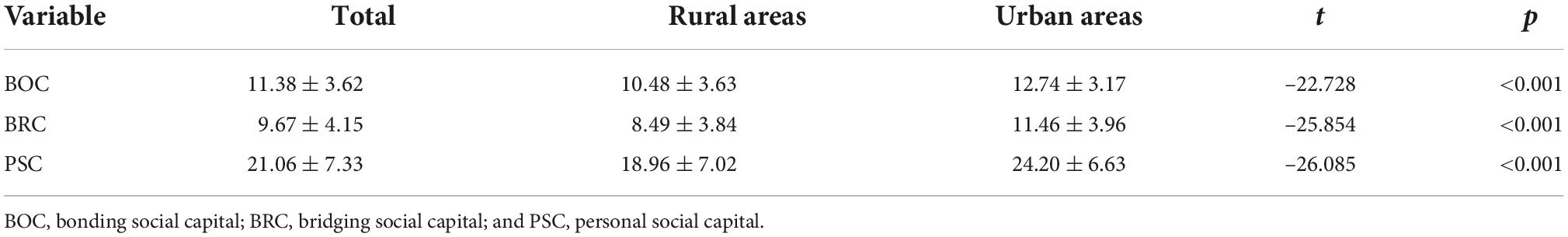
Scores of personal social capital of the elderly
Table 2 shows the scores of personal social capital among the participants. The respondents’ total score of personal social capital was 21.06 ± 7.33, while the score of two dimensions of personal social capital (BOC and BRC) were 11.38 ± 3.62 and 9.67 ± 4.15, respectively. The scores of the BOC and BRC among older people in rural areas were significantly lower than those in urban areas (p < 0.001).
Health status distribution on the five dimensions of European Five Dimensions Questionnaire
In this study, pain/discomfort was the most common problem among the older people: 51.52% in rural areas compared with 40.67% in urban areas (p < 0.001). While self-care was the least frequently reported problem: 20.91% in rural areas compared with 13.63% in urban areas (p < 0.001). Five dimensions of EQ-5D-3L were all statistically significant between rural and urban areas (p < 0.001) (Table 3).
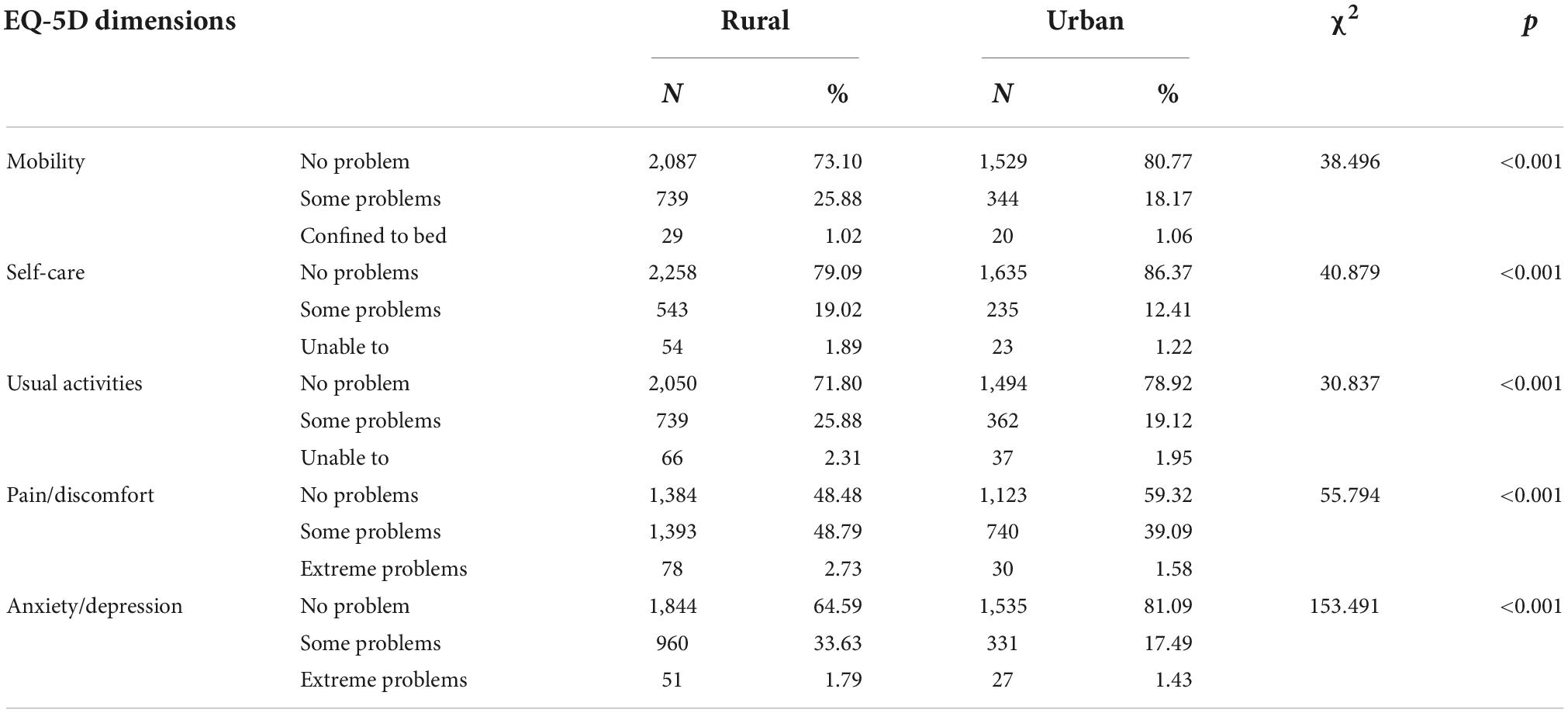
Table 3. Health status distribution on the five dimensions of European Five Dimensions Questionnaire (EQ-5D-3L).
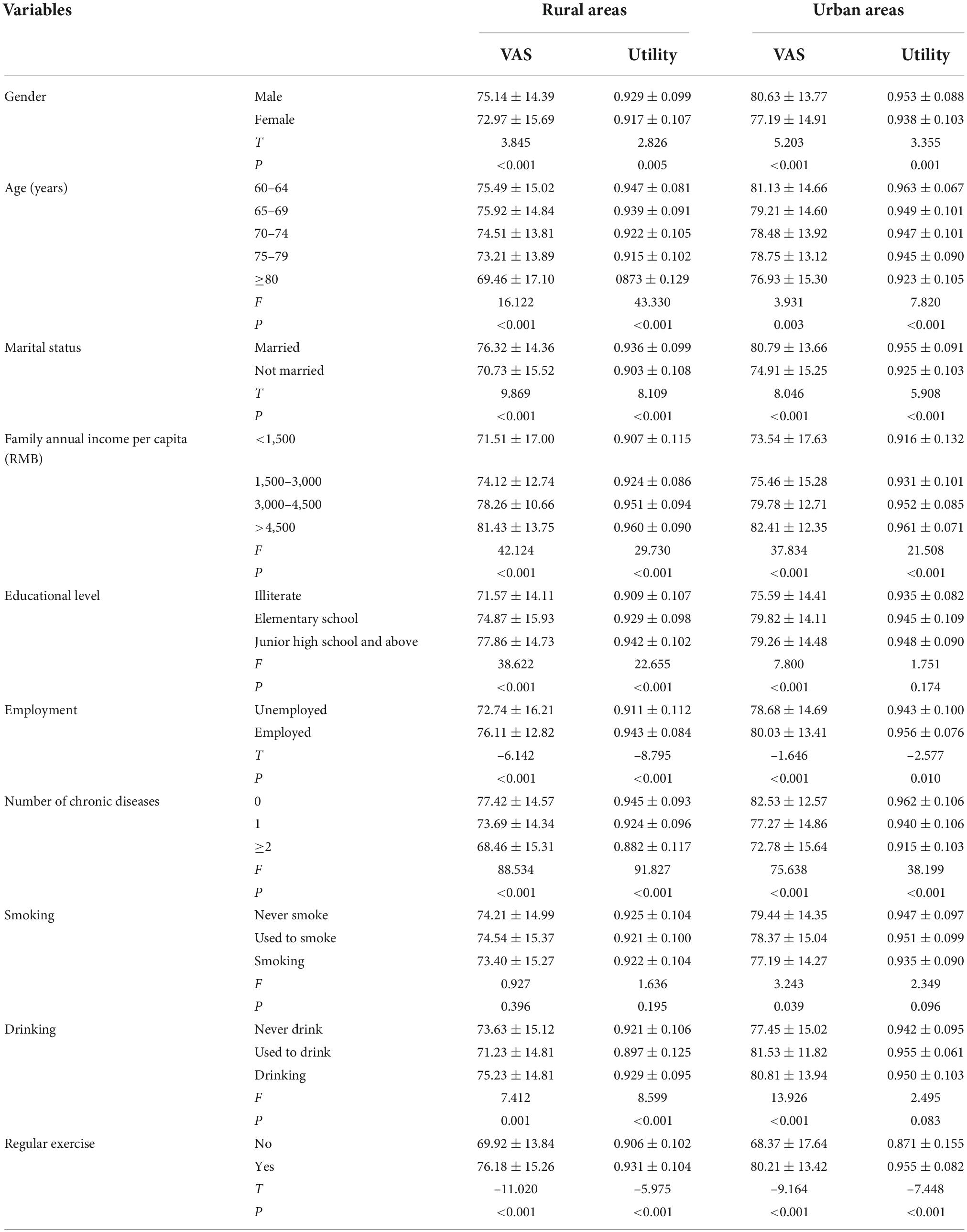
Distribution of VAS scores and utility index among older people
Table 4 shows the scores of the samples’ self-rated health and utility index. The following characteristics were significantly different among the rural participants in both VAS and utility index scores: gender, age, marital status, annual family income per capita, educational attainment, employment, number of chronic diseases, drinking, and regular exercise (p < 0.05). Significant differences were found in VAS scores in urban samples in age, marital status, annual family income per capita, educational level, employment, number of chronic diseases, smoking, drinking, and regular exercise (p < 0.05). While in utility index scores only age, marital status, annual family income per capita, employment, number of chronic diseases, and regular exercise were found to be significantly different among urban samples (p < 0.05).
The relationship between personal social capital and European Five Dimensions Questionnaire Visual Analogue Scale
As shown in Table 5, for the rural sample, in model 1, only BOC was positively correlated with the EQ-VAS score of the older people (B = 0.977, 95% CI = 0.75–1.21). After adjusting for sociodemographic characteristics, socioeconomic status, number of chronic diseases, and healthy behaviors, in model 5, BOC was still positively related to the EQ-VAS score of the older people (B = 0.567, 95% CI = 0.32–0.81), and BRC had nothing to do with the EQ-VAS score of the elderly (p > 0.05).
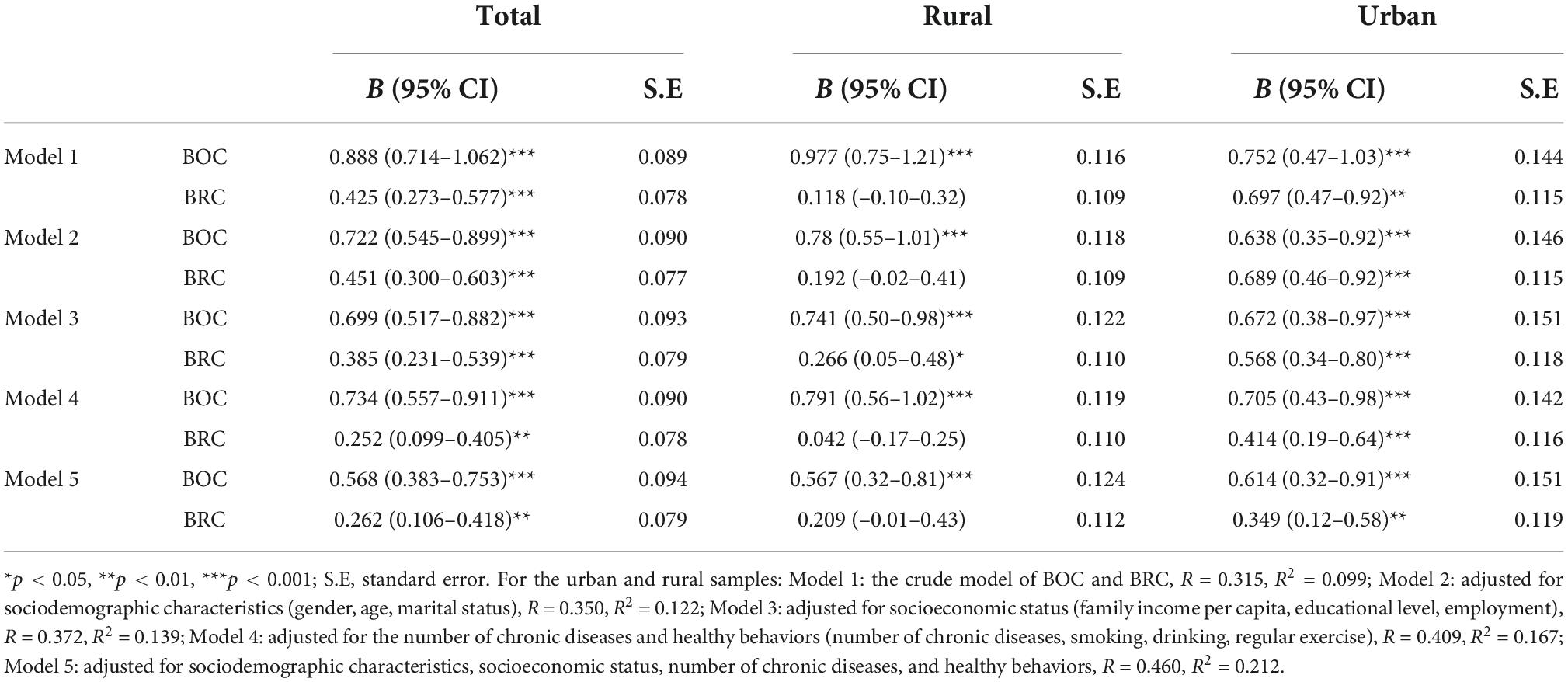
Table 5. The relationship between personal social capital and European Five Dimensions Questionnaire Visual Analogue Scale (EQ-VAS).
For the urban sample, in model 1, both the BOC (B = 0.752, 95% CI = 0.47–1.03) and the BRC (B = 0.697, 95% CI = 0.47–0.92) were related to the EQ-VAS score of the elderly positively. After adjusting for sociodemographic characteristics, socioeconomic status, number of chronic diseases, and healthy behaviors, in model 5, both the BOC (B = 0.614, 95% CI = 0.32–0.91) and the BRC (B = 0.349, 95% CI = 0.12–0.58) were still positively correlated with the EQ-VAS score of the participants.
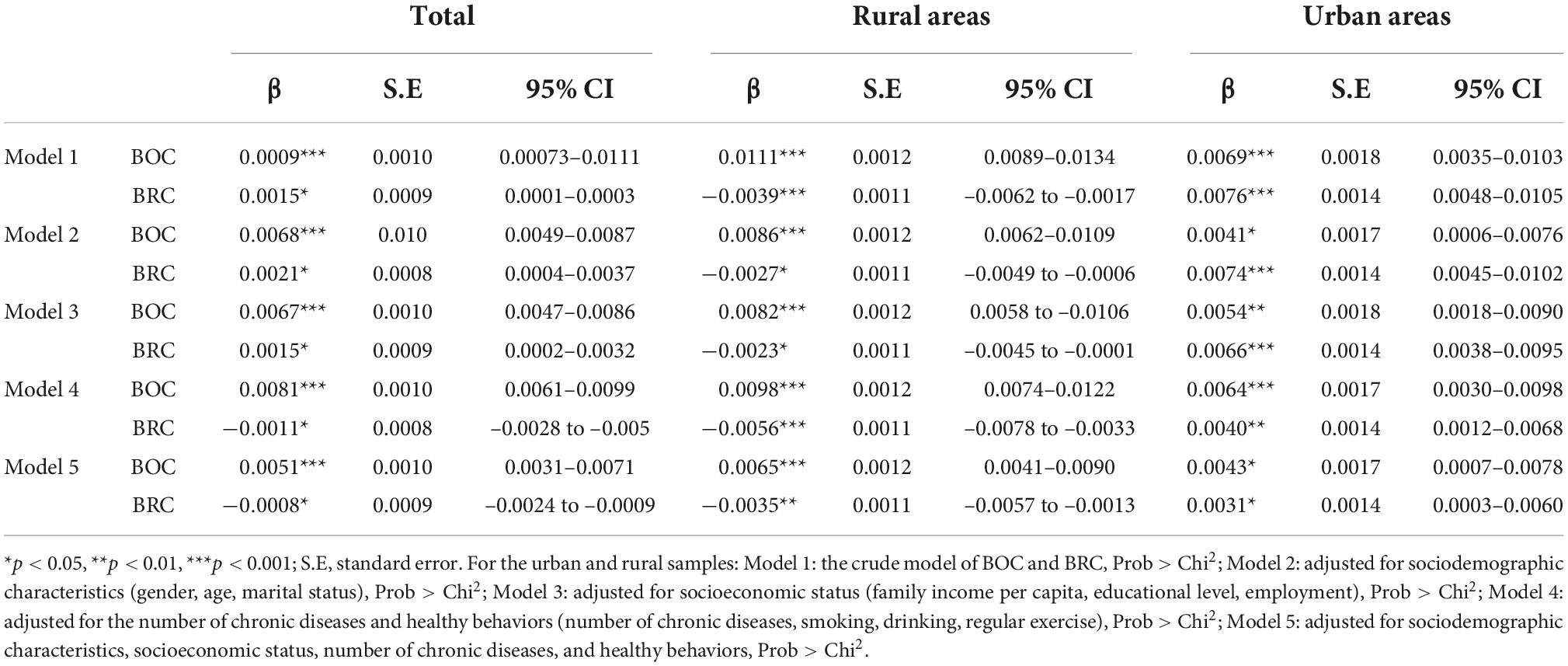
The relationship between personal social capital and EQ-5D utility index
As shown in Table 6, for the rural sample: in Model 1, the BOC was positively correlated with the utility score of the older people (β = 0.0111, 95% CI = 0.0089–0.0134), while the BRC was negatively correlated with the utility score of the older people (β = –0.0039, 95% CI = –0.0062–0.0017). After adjusting for sociodemographic characteristics, socioeconomic status, number of chronic diseases, and healthy behaviors, in model 5, the BOC was positively correlated with the EQ-5D utility score of the older people (β = 0.0065, 95% CI = 0.0041–0.0090), while the BRC was negatively correlated with the EQ-5D utility score of the older people (β = –0.0035, 95%-CI = –0.0057–0.0013).
For the urban sample: in Model 1, both the BOC (β = 0.0069, 95% CI = 0.0035–0.0103) and the BRC (β = 0.0076, 95% CI = 0.0048–0.0105) were positively correlated with the utility score of the older people. After adjusting for sociodemographic characteristics, socioeconomic status, number of chronic diseases, and healthy behaviors, in model 5, both the BOC (β = 0.0043, 95% CI = 0.0007–0.0078) and the BRC (β = 0.0031, 95% CI = 0.0003–0.0060) were still positively correlated with the EQ-5D utility score of the elderly.
Discussion
To our knowledge, this is the first study that measures the relationship between personal social capital and HRQoL among Chinese older people from an urban-rural perspective. This cross-sectional study found that personal social capital was significantly associated with HRQoL among rural and urban older people. Moreover, the correlation still existed after adjusting the sociodemographic characteristics, socioeconomic status, number of chronic diseases, and healthy behaviors.
Our data showed that the total score of PSC among older people in rural areas was significantly lower than those in urban areas, which was different from a previous study (43). We speculated that the Chinese urban-rural dual structure might cause the discrepancy. In Chinese traditional culture, rural areas are more likely to be an “acquaintance society” than urban areas. On the one hand, with the development of urbanization, the young migrate to urban areas for work; on the other hand, the intimates and friends of older people start to die, resulting in the PSC of the older people in rural areas are gradually losing (44). In addition, our study also found that BRC among older people was lower than BOC both in urban and rural areas. According to the definition of BRC and BOC, it means that rural and urban areas were facing the dilemma of community or village hollowing out (45). Because there is less social participation and lacking organizations/groups that could provide community public services such as medical services and cultural services for older people (46), which may make them feel less BRC than BOC subjectively. Therefore, the government must encourage the community or village to provide services for the older people by establishing more care facilities and volunteer organizations/groups which can improve the bridge social capital of the older people and give them a sense of belonging in these social organizations or groups. Consistent with previous studies (47, 48), pain/discomfort and anxiety/depression were the most significant health problems affecting older people. In this study, the average EQ-VAS score of the older people was 76.01 ± 14.99, lower than the result of the Fifth National Health Service Survey (80.91 ± 13.7) (49), indicating that the older people were not optimistic about their self-rated health. The average utility index score was 0.9323 ± 0.1016, lower than the fifth National Health Service Survey (0.985 ± 0.056) (39), indicating the urgency of further HRQoL improvement among older adults. In addition, our study found that the utility index score of the rural sample was lower than urban samples, which calls for more attention to the HRQoL of the rural older people.
Our results showed that only BOC was positively correlated with self-rated health for the rural samples. Understandably, neighborhood mutual assistance is a normal situation, even in the current rapid economic and social development, this tradition has not died out in rural areas. Rural older people were affected by traditional values, which emphasize more on the family relationship that emphasizes the family relationship more than in urban areas. At the same time, family relationships play an essential role in the health of family members. Moreover, Stafford et al. (50) found that neighborhood relationships’ cohesion is positively related to self-rated health. Therefore, older people with more BOC have a higher level of self-rated fitness. Given that most older people in rural areas were engaged in agricultural production activities and lacked social organizations or groups, their communication scope was narrow and social participation was low (51). Another reason is that the self-esteem of rural older people is high (52), leading them to be unwilling to resort to help from social organizations/groups when experiencing health issues, which may also result in the insignificant relationship between BRC and self-rated health. In our study, both BOC and BRC were associated with self-rated health among urban older people. A previous study has proven that good interpersonal relationships and more social participation can improve the health of old citizens (53). Compared with the rural older people, the urban older people had a higher socioeconomic status and more resources to cope with adversity, which could increase their mutual communication, exchange and support, got help and encouragement from others, met their needs of economic and emotional support, relieving psychological pressure, and provided indirect protection for health (54, 55).
Our study indicated that the BOC was positively correlated with the EQ-5D utility index of all older people in rural and urban areas. That might be related to Chinese Confucianism’s filial piety and family culture (56). Traditional values have a deep-rooted influence on the Chinese, especially older people. They attach more importance to their relationship with their family, relatives, and friends (57), the support and reciprocal network provided by people close to them and their living environment had a significant role in meeting their psychological and emotional needs and promoting the quality of life of the older people (58–60). Interestingly, the BRC was negatively correlated with the utility score of the rural older people, while it was positively correlated with the EQ-5D utility score of the urban older people. The BRC was generated from the weak network between the older people and the surrounding social organizations or groups. It improved the actual value of interpersonal communication among older people through individual participation in social activities (61). Compared with older people in urban areas, due to the influence of factors such as traffic, economic conditions, ideas, and consciousness, the rural older people had relatively weak connections with the outside world, rarely participated in social activities, and had a relatively simple social network, with limited help resources available. Urban older people could get help from communities and various social organizations. In addition, as more and more older people started to use smartphones and the Internet (62, 63), especially urban older people, they had more channels to contact the outside world and obtain information. Organizational participation and citizen participation can not only help the elderly to obtain a sense of belonging and self-worth and even directly promote their physical exercise, which is conducive to health promotion. Therefore, it is suggested that government should provide social assistance for older people in multi-levels and various forms; increase health education and promotion in healthy aging; and improve physical facilities, expand coverage of old-age care.
Limitations
There are still several limitations in our study. First, this is a cross-sectional study, which can only reflect the association between PSC and the HRQoL among older Chinese people. Therefore, causality cannot be determined. Second, this study is based on self-reported questionnaires, leading to some bias due to inaccurate responses. Third, the concept and measurement of PSC are still controversial. Though there are many ways to measure social capital, each instrument has its limitations and cannot cover all areas of social capital. For future studies, all the limitations should try to avoid. Four, we did not consider the regional and economical difference, although we conducted the survey in Henan province, Hubei province, Fujian province, Jiangsu province, etc., because we used the convenient sampling, indicating the limited representation of samples.
Conclusion
In Conclusion, our study found that (1) the PSC of the older people needs to improve further, and the PSC level of the rural older people was lower than that of the urban areas. (2) Pain/discomfort and anxiety/depression were the most significant health problems affecting older people. Older people in rural areas were more likely to have problems than older people in urban areas, and the level of health of rural older people was worse than urban older people. (3) The PSC of the older people was related to the HRQoL. The BOC was positive associated with the rural older people’s HRQoL, while the BRC was negatively associated with the rural older people’s HRQoL. BOC and the BRC were both positively correlated with the HRQoL of urban older people. Therefore, to improve the HRQoL of the older people, we should increase the BOC of the elderly in rural areas, and the BOC and BRC of the elderly in urban areas.
Data availability statement
The original contributions presented in this study are all included in the article. Further inquiries can be directed to the first or corresponding authors. The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board, School of Public Health, and Faculty of Medical Sciences, Wuhan University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
QW and DJ contributed to the study conception and design. DJ, YY, and HZ performed the material preparation, data collection, and analysis. DJ and YY wrote the first draft of the manuscript. QW revised and edited the draft. All authors commented on previous versions of the manuscript, read, and approved the final manuscript.
Acknowledgments
The Global Health Institute of Wuhan University lead the study. We thank Zhaoxun Hou from Harvard University for English language editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Plath D. International policy perspectives on independence in old age. J Aging Soc Policy. (2009) 21:209–23. doi: 10.1080/08959420902733173
2. Cui S, Yu Y, Dong W, Xu T, Huang Y, Zhang X, et al. Are there gender differences in the trajectories of self-rated health among Chinese older adults? An analysis of the Chinese longitudinal healthy longevity survey (CLHLS). BMC Geriatr. (2021) 21:563. doi: 10.1186/s12877-021-02484-4
3. National Statistical Bureau of China. Bulletin of the Seventh National Census. (2021). Available online at: http://www.gov.cn/guoqing/2021-05/13/content_5606149.htm (accessed May 23, 2021).
4. National Health Commission of the People’s Republic of China. Report of the State Council on the Progress of Strengthening and Advancing the Work on Aging. (2022). Available online at: http://www.nhc.gov.cn/wjw/mtbd/202209/2ca97b572ee34a38819cceaf5207dd1a.shtml (accessed November 11, 2022).
5. Anderson H, Atkinson R, Bremner S, Marston L. Particulate air pollution and hospital admissions for cardiorespiratory diseases: are the elderly at greater risk? Eur Respir J Suppl. (2003) 40:39–46s. doi: 10.1183/09031936.03.00402203
6. Fong J. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. (2019) 19:323. doi: 10.1186/s12877-019-1348-z
7. Moore P, Ortega J, Saldías F, Oyarzún M. Ambulatory management of community acquired pneumonia in the elderly. Rev Med Chil. (2006) 134:1568–75. doi: 10.4067/s0034-98872006001200013
8. The WHOQOL Group. The world health organization quality of life assessment (WHOQOL): position paper from the world health organization. Soc Sci Med. (1995) 41:1403–9. doi: 10.1016/0277-9536(95)00112-k
9. Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. (2016) 34:645–9. doi: 10.1007/s40273-016-0389-9
10. Wu X, Han L, Zhang J, Luo S, Hu J, Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: a systematic review. PLoS One. (2017) 12:e0187668. doi: 10.1371/journal.pone.0187668
11. Grange A, Bekker H, Noyes J, Langley P. Adequacy of health-related quality of life measures in children under 5 years old: systematic review. J Adv Nurs. (2007) 59:197–220. doi: 10.1111/j.1365-2648.2007.04333.x
12. Lagadec N, Steinecker M, Kapassi A, Magnier A, Chastang J, Robert S, et al. Factors influencing the quality of life of pregnant women: a systematic review. BMC Pregnancy Childbirth. (2018) 18:455. doi: 10.1186/s12884-018-2087-4
13. Schneider H, Birkhäuser M. Quality of life in climacteric women. Climacteric. (2017) 20:187–94. doi: 10.1080/13697137.2017.1279599
14. Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. (2018) 16:189. doi: 10.1186/s12955-018-1021-9
15. Carvalho W, Alves Maria G, Gonçalves K, Miranda A, Moreira M. Health-related quality of life of heart transplant recipients living in a developing country. Transplant Proc. (2021) 53:358–63. doi: 10.1016/j.transproceed.2020.05.027
16. Chen C, Liu G, Shi Q, Sun Y, Zhang H, Wang M, et al. Health-related quality of life and associated factors among oldest-old in China. J Nutr Health Aging. (2020) 24:330–8. doi: 10.1007/s12603-020-1327-2
17. Jalenques I, Rondepierre F, Rachez C, Lauron S, Guiguet-Auclair C. Health-related quality of life among community-dwelling people aged 80 years and over: a cross-sectional study in France. Health Qual Life Outcomes. (2020) 18:126. doi: 10.1186/s12955-020-01376-2
18. Kosilov K, Amedzawa H, Kuzina I, Kuznetsov V, Kosilova L. The impact of variable factors on the health-related quality of life in the elderly in Japan and Russia. Curr Aging Sci. (2020) 13:119–28. doi: 10.2174/1874609812666191105141438
19. Wong E, Xu R, Cheung A. Health-related quality of life among patients with hypertension: population-based survey using EQ-5D-5L in Hong Kong SAR, China. BMJ Open. (2019) 9:e032544. doi: 10.1136/bmjopen-2019-032544
20. Hajek A, Brettschneider C, Mallon T, Ernst A, Mamone S, Wiese B, et al. The impact of social engagement on health-related quality of life and depressive symptoms in old age - evidence from a multicenter prospective cohort study in Germany. Health Qual Life Outcomes. (2017) 15:140. doi: 10.1186/s12955-017-0715-8
21. Assari S, Smith J, Bazargan M. Health-related quality of life of economically disadvantaged African American older adults: age and gender differences. Int J Environ Res Public Health. (2019) 16:1522. doi: 10.3390/ijerph16091522
22. Freitas J, Silva J, Nóbrega J, Simões R, Medeiros J, Alves R, et al. Health-related quality of life and associated factors: regional differences among oldest-old in Brazil. Inquiry. (2022) 59:469580221086922. doi: 10.1177/00469580221086922
23. Sarna L, Bialous S, Cooley M, Jun H, Feskanich D. Impact of smoking and smoking cessation on health-related quality of life in women in the Nurses’ Health Study. Qual Life Res. (2008) 17:1217–27. doi: 10.1007/s11136-008-9404-8
24. Essex H, White I, Khadjesari Z, Linke S, McCambridge J, Murray E, et al. Quality of life among hazardous and harmful drinkers: EQ-5D over a 1-year follow-up period. Qual Life Res. (2014) 23:733–43. doi: 10.1007/s11136-013-0521-7
25. Yao Q, Liu C, Zhang Y, Xu L. Health-related quality of life of people with self-reported hypertension: a National Cross-Sectional Survey in China. Int J Environ Res Public Health. (2019) 16:1721. doi: 10.3390/ijerph16101721
26. Nedjat-Haiem F, Cadet T, Parada H Jr, Jones T, Jimenez E, Thompson B, et al. Financial hardship and health related quality of life among older Latinos with chronic diseases. Am J Hosp Palliat Care. (2021) 38:938–46. doi: 10.1177/1049909120971829
27. Abbott S, Freeth D. Social capital and health: starting to make sense of the role of generalized trust and reciprocity. J Health Psychol. (2008) 13:874–83. doi: 10.1177/1359105308095060
28. Ziersch A, Baum F, Darmawan I, Kavanagh A, Bentley R. Social capital and health in rural and urban communities in South Australia. Aust N Z J Public Health. (2009) 33:7–16. doi: 10.1111/j.1753-6405.2009.00332.x
29. Norstrand J, Xu Q. Social capital and health outcomes among older adults in China: the urban-rural dimension. Gerontologist. (2012) 52:325–34. doi: 10.1093/geront/gnr072
30. Chen X, Stanton B, Gong J, Fang X, Li X. Personal social capital scale: an instrument for health and behavioral research. Health Educ Res. (2009) 24:306–17. doi: 10.1093/her/cyn020
31. McKenzie K, Whitley R, Weich S. Social capital and mental health. Br J Psychiatry. (2002) 181:280–3. doi: 10.1192/bjp.181.4.280
32. Salehi A, Ehrlich C, Kendall E, Sav A. Bonding and bridging social capital in the recovery of severe mental illness: a synthesis of qualitative research. J Ment Health. (2019) 28:331–9. doi: 10.1080/09638237.2018.1466033
33. Westphaln K, Fry-Bowers E, Georges J. Social capital: a concept analysis. ANS Adv Nurs Sci. (2020) 43:E80–111. doi: 10.1097/ans.0000000000000296
34. Lamarca G, Leal Mdo C, Leao A, Sheiham A, Vettore M. The different roles of neighbourhood and individual social capital on oral health-related quality of life during pregnancy and postpartum: a multilevel analysis. Community Dent Oral Epidemiol. (2014) 42:139–50. doi: 10.1111/cdoe.12062
35. Kim D, Kawachi I. U.S. state-level social capital and health-related quality of life: multilevel evidence of main, mediating, and modifying effects. Ann Epidemiol. (2007) 17:258–69. doi: 10.1016/j.annepidem.2006.10.002
36. Liu X, Chen J, Zhou J, Liu J, Lertpitakpong C, Tan A, et al. The relationship between the number of daily health-related behavioral risk factors and sleep health of the elderly in China. Int J Environ Res Public Health. (2019) 16:4905. doi: 10.3390/ijerph16244905
37. Fu C, Wang C, Yang F, Cui D, Wang Q, Mao Z. Association between social capital and physical activity among community-dwelling elderly in Wuhan, China. Int J Gerontol. (2018) 12:155–9. doi: 10.1016/j.ijge.2017.10.001
38. Wang P, Chen X, Gong J, Jacques-Tiura A. Reliability and validity of the personal social capital scale 16 and personal social capital scale 8: two short instruments for survey studies. Soc Indic Res. (2014) 119:1133–48.
39. Yao Q, Liu C, Zhang Y, Xu L. Changes in health-related quality of life of Chinese populations measured by the EQ-5D-3 L: a comparison of the 2008 and 2013 National Health Services Surveys. Health Qual Life Outcomes. (2019) 17:43. doi: 10.1186/s12955-019-1109-x
40. Sun S, Chen J, Johannesson M, Kind P, Xu L, Zhang Y, et al. Population health status in China: EQ-5D results, by age, sex and socio-economic status, from the National Health Services Survey 2008. Qual Life Res. (2011) 20:309–20. doi: 10.1007/s11136-010-9762-x
41. Haridoss M, Bagepally B, Natarajan M. Health-related quality of life in rheumatoid arthritis: systematic review and meta-analysis of EuroQoL (EQ-5D) utility scores from Asia. Int J Rheum Dis. (2021) 24:314–26. doi: 10.1111/1756-185x.14066
42. Zhuo L, Xu L, Ye J, Sun S, Zhang Y, Burstrom K, et al. Time trade-off value set for EQ-5D-3L based on a nationally representative Chinese population survey. Value Health. (2018) 21:1330–7. doi: 10.1016/j.jval.2018.04.1370
43. Sørensen J. Rural–urban differences in bonding and bridging social capital. Reg Stud. (2016) 50:391–410. doi: 10.1080/00343404.2014.918945
44. Bai Y, Bian F, Zhang L, Cao Y. The impact of social support on the health of the rural elderly in China. Int J Environ Res Public Health. (2020) 17:2004. doi: 10.3390/ijerph17062004
45. Liu C, Xu M. Characteristics and influencing factors on the hollowing of traditional villages-taking 2645 villages from the Chinese traditional village catalog (batch 5) as an example. Int J Environ Res Public Health. (2021) 18:12759. doi: 10.3390/ijerph182312759
46. Yang Y, Wang S, Chen L, Luo M, Xue L, Cui D, et al. Socioeconomic status, social capital, health risk behaviors, and health-related quality of life among Chinese older adults. Health Qual Life Outcomes. (2020) 18:291. doi: 10.1186/s12955-020-01540-8
47. Zhang T, Shi W, Huang Z, Gao D, Guo Z, Liu J, et al. Influence of culture, residential segregation and socioeconomic development on rural elderly health-related quality of life in Guangxi, China. Health Qual Life Outcomes. (2016) 14:98. doi: 10.1186/s12955-016-0499-2
48. Wang H, Kindig D, Mullahy J. Variation in Chinese population health related quality of life: results from a EuroQol study in Beijing, China. Qual Life Res. (2005) 14:119–32. doi: 10.1007/s11136-004-0612-6
49. Jia X, Hu H, Wang X, Zhuo L, Xu L, Zhang Y, et al. Analysis on self-rated health status and its influencing factors among Chinese residents aged 15 and above. Chinese J Health Policy. (2016) 9:6.
50. Stafford M, Bartley M, Boreham R, Thomas R, Wilkinson R, Marmot M. Neighbourhood social cohesion and health: investigating associations and possible mechanisms. In: Morgan A, Swann C editors. Social Capital and Health. Issues of Definition, Measurement and Links to Health. London: Health Development Agency (2004). doi: 10.1109/CDC.2006.377003
51. Ibrahim N, Din N, Ahmad M, Ghazali S, Said Z, Shahar S, et al. Relationships between social support and depression, and quality of life of the elderly in a rural community in Malaysia. Asia Pac psychiatry. (2013) 5(Suppl. 1):59–66. doi: 10.1111/appy.12068
52. Sun Y, Zhang D, Yang Y, Wu M, Xie H, Zhang J, et al. Social support moderates the effects of self-esteem and depression on quality of life among Chinese rural elderly in nursing homes. Arch Psychiatr Nurs. (2017) 31:197–204. doi: 10.1016/j.apnu.2016.09.015
53. Lee H, Jang S, Lee S, Cho S, Park E. The relationship between social participation and self-rated health by sex and age: a cross-sectional survey. Int J Nurs Stud. (2008) 45:1042–54. doi: 10.1016/j.ijnurstu.2007.05.007
54. Gupta R, Kaur M, Islam S, Mohan V, Mony P, Kumar R, et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am J Hypertens. (2017) 30:373–81. doi: 10.1093/ajh/hpw169
55. Cao J, Rammohan A. Social capital and healthy ageing in Indonesia. BMC Public Health. (2016) 16:631. doi: 10.1186/s12889-016-3257-9
56. Lo M, Russell C. Family care: an exploratory study of experience and expectations among older Chinese immigrants in Australia. Contemp Nurse. (2007) 25:31–8. doi: 10.5172/conu.2007.25.1-2.31
57. Lou C, Lou K, Ridley J. Exploring the meaning of dignity at end of life for Chinese Canadians caregivers: a qualitative cross-cultural study. Palliat Med. (2021) 35:142–50. doi: 10.1177/0269216320956809
58. Lee H, Yun J. Health-related quality of life in South Korean community-dwelling older adults with multimorbidity: a convergent parallel mixed-methods approach. Qual Life Res. (2020) 29:721–32. doi: 10.1007/s11136-019-02360-0
59. Routasalo P, Tilvis R, Kautiainen H, Pitkala K. Effects of psychosocial group rehabilitation on social functioning, loneliness and well-being of lonely, older people: randomized controlled trial. J Adv Nurs. (2009) 65:297–305. doi: 10.1111/j.1365-2648.2008.04837.x
60. Nilsson J, Rana A, Kabir Z. Social capital and quality of life in old age: results from a cross-sectional study in rural Bangladesh. J Aging Health. (2006) 18:419–34. doi: 10.1177/0898264306286198
61. Jiang D, Hou Y, Hao J, Zhou J, Jiang J, Wang Q. Association between personal social capital and loneliness among widowed older people. Int J Environ Res Public Health. (2020) 17:5799. doi: 10.3390/ijerph17165799
62. Wong C, Yeung D, Ho H, Tse K, Lam C. Chinese older adults’ internet use for health information. J Appl Gerontol. (2014) 33:316–35. doi: 10.1177/0733464812463430
Keywords: Chinese elderly people, personal social capital, health-related quality of life, urban-rural distribution, sociocultural aspects of health and wellbeing
Citation: Jiang D, Yan Y, Zhou H and Wang Q (2022) The association between personal social capital and health-related quality of life among Chinese older people: A cross-sectional study. Front. Nutr. 9:995729. doi: 10.3389/fnut.2022.995729
Received: 16 July 2022; Accepted: 22 November 2022;
Published: 08 December 2022.
Edited by:
Yuxuan Gu, Nanjing Normal University, ChinaCopyright © 2022 Jiang, Yan, Zhou and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Quan Wang, d2FuZ3F1YW43M0B3aHUuZWR1LmNu
 Dongdong Jiang
Dongdong Jiang Yajie Yan
Yajie Yan Han Zhou
Han Zhou Quan Wang
Quan Wang