
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr. , 06 October 2022
Sec. Nutritional Epidemiology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.993180
This article is part of the Research Topic Food Cognition: The Crossroads of Psychology, Neuroscience and Nutrition View all 12 articles
A healthy diet and lifestyle may protect against adverse mental health outcomes, which is especially crucial during stressful times, such as the COVID-19 pandemic. This preregistered longitudinal online study explored whether diet and lifestyle (physical activity, sleep, and social interactions) were associated with wellbeing and mood during a light lockdown in Germany. Participants (N = 117, 72 males; 28 ± 9 years old) answered mental health and lifestyle questionnaires (social connections, sleep, activity) followed by submitting 1 week of food and mood-lifestyle diary (food intake, positive and negative mood, mental wellbeing, sleep quality, physical activity level, quantity and quality of social interactions) via a smartphone app. We used multivariate linear and mixed-effects models to associate mood and wellbeing with dietary components and lifestyle factors. Interindividual analyses revealed that sleep and social interaction significantly impacted mood and wellbeing. Interestingly, fruit and vegetable intake correlated with wellbeing, even when controlling for all lifestyle factors. Fruit and vegetable intake also significantly correlated with daily fluctuations in wellbeing within individuals next to sleep, physical activity, and social interactions. We observed gender differences in fruit and vegetable intake and anxiety levels. Our results emphasize the importance of diet contributing to individual wellbeing, even in the challenging times of a pandemic. Future research is necessary to test if our findings could extend to other populations.
COVID-19 lockdowns and social isolation have taken a toll on mental wellbeing (1–3). Lifestyle factors, including diet and physical activity, are shown to effectively reduce the risk of mental health disorders (4). However, it is unclear whether and how such lifestyle factors contribute to mental wellbeing during the pandemic.
A diet high in fruit and vegetables reduced depression risk (5–7) and anxiety (8). On the other hand, diets high in trans fatty acids from processed foods (9) and fast food increased depression risk over 6-years (10, 11). Dietary intake can have relatively instant effects on mood and wellbeing. Studies investigating daily associations found that higher fruit and vegetable intake was associated with wellbeing (12) and positive mood the same day or the next day (13). While eating salty snacks correlated with higher negative mood the next day in people with a high Body Mass Index (BMI) (13). Similarly, higher saturated fat intake correlated with negative mood 2 days later in college students (14).
Importantly, diet-induced neuroinflammation is a key mechanism linking diet, cognitive function, and even gray matter volume loss (15). The dietary inflammatory index (DII) estimates a diet’s inflammatory potential (16), and at least two meta-analyses have established a link with depression (17, 18), depressive symptoms, anxiety, and psychological distress (19, 20). Importantly, DII and mental health profiles were less associated in men than in women (19), pointing to gender differences.
Besides diet, physical activity and sleep play a major role in wellbeing (21, 22), depression (23), anxiety (24, 25) and sleep quality (26). However, the pandemic has impacted lifestyle behaviors. For example, a recent study demonstrated that roughly 53% of 5,000 participants reported a change in activity level during the COVID-19 pandemic (27). Sleep disturbances were reliably associated with the risk for depressive symptoms and clinical depression (4) and correlated positively with mental health issues (28), suggesting that physical activity and sleep quality majorly contribute to wellbeing and mood during the pandemic.
Managing the COVID-19 pandemic required social distancing, making the link between social interaction and mental health outcomes of high interest. Social interaction is vital for mental health outcomes, including wellbeing and symptoms of depression or anxiety (29–31). For example, loneliness, the subjective feeling of the absence of a social network or a companion, is associated with adverse physical and mental health outcomes (30) and low physical activity levels in mental health patient groups (32, 33). During COVID-19-lockdown, social distancing restrictions led to increased feelings of social isolation, which coincided with more severe mental health outcomes (34). At the same time, a good relationship quality was crucial in maintaining mental health (3). Furthermore, wellbeing during the pandemic was associated with satisfaction of psychological needs at an inter- and intrapersonal level (35). Data from an Italian study during lockdown and when some restrictions were lifted showed that both emotional eating and binge-eating were increased in the presence of emotional distress, including higher levels of anxiety and depression, but also partially correlated with relationship quality and quality of life (36). An interesting question that remains is to what extent dietary intake can ameliorate the negative consequences of living through a pandemic in the context of physical activity, sleep, and social interaction quality.
In this preregistered online study,1 we investigated whether diet, lifestyle factors, and social interaction were associated with wellbeing, anxiety, and feeling of excitement during COVID-19 lockdown. We hypothesized that food intake (i.e., fat, carbohydrates, fruit and vegetables) contributes significantly to (1) individual wellbeing, (2) anxiety, and (3) excitement, even when controlling for lifestyle factors. Next to these preregistered analyses, we tested whether inflammation, as a possible mechanism, plays a role in the relationship between food intake and wellbeing.
We recruited participants via the online research platform Prolific. German-speaking individuals without prior mental health diagnoses, residing in Germany at the time of the study, with an Apple or Android smartphone for using the FoodApp, were eligible to participate. We excluded participants who showed above-threshold depressive symptoms (i.e., above 30, which is classified as “severe”) determined by the Beck Depression Inventory [BDI; German version (37)]. Questionnaires were completed online on the SoSci Survey platform. The food and mood diary records were recorded using the FoodApp available for Android and Apple smartphones. Participants provided informed consent and received £28 for participation. Ethical approval was obtained from the Humboldt University of Berlin.
We conducted an online study using questionnaires assessing mental health, wellbeing, and lifestyle factors. Afterward, participants kept a food and mood diary and a record of sleep quality, activity, and social interactions for 7 days (Figure 1). In particular, in this study we wanted to investigate the relationship between food intake as independent variables (i.e., fruit and vegetable, fat and carbohydrate intake) and mood (i.e., wellbeing, anxiety, excitement) as dependent variables while controlling for lifestyle factors (i.e., activity, sleep and social interaction quality and quantity). Data were collected between 11 and 24 November 2020 at which time there was a light lockdown in Germany. During this time, people were asked to reduce social contacts to the minimum. In public, one was only allowed to meet with people of one’s household and one additional household (from: 28.10.2020).2
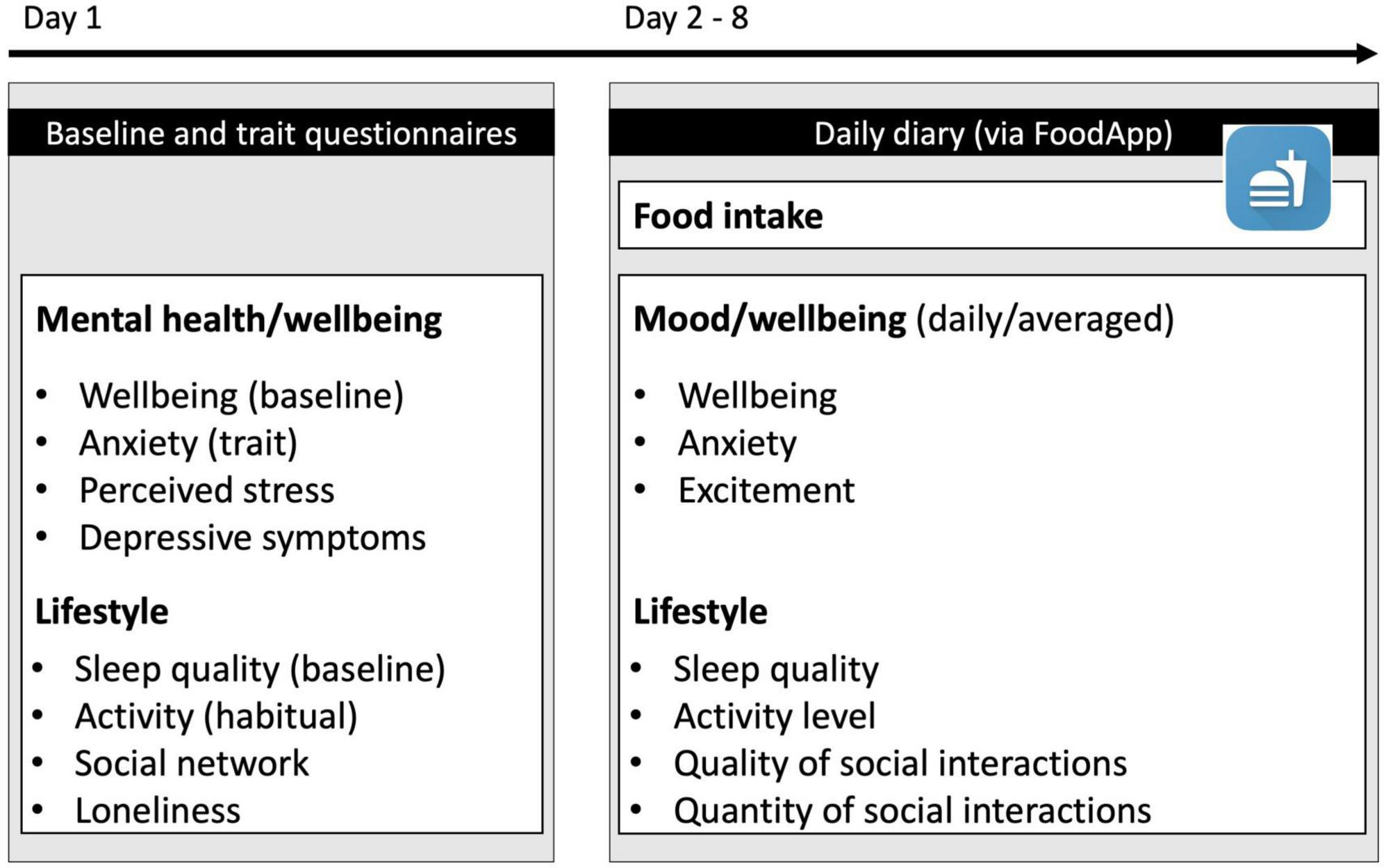
Figure 1. Study outline. Participants first answered questionnaires assessing baseline mental health and wellbeing as well as lifestyle-related questionnaires. Next, they completed a daily food, mood, and lifestyle diary for 7 days via a smartphone app.
The food-mood and lifestyle diaries were completed using a smartphone FoodApp for 7 days [following (14)]. For food intake, we recorded the following information: date, time, type of meal, companionship during the meal, food items, and weight consumed. Food items could be chosen from a list of about 10,000 food and beverage items commonly available in Germany, for example, “potatoes peeled boiled” or “wholemeal bread with margarine and currant jam.” Participants chose the food item matching their consumption along with an estimate of how much they consumed in grams or milliliters. Participants were free to log their food intake after a meal, or later during the day. A reminder was sent to participants who did not submit their data by 7 p.m. that day. Dietary intake was evaluated using the German Federal Food Key data table [Bundeslebensmittelschlüssel (38)] made available by the Max-Rubner Institut (MRI). Data from days with extreme daily caloric intake were excluded from analysis (for women: < 500 or > 3,500 kcal/day, for men: < 800 and > 4,000 kcal/day considered as unrealistic amounts) following (39).
For dietary intake, we calculated energy-adjusted (ea) values to account for an individual’s total energy intake (i.e., g/1,000 kcal/day) as suggested by Agnoli et al. (40). Additionally, we computed daily energy derived from each macronutrient. For this, we multiplied the daily intake of carbohydrate and protein (g/d) by 4 kcal, and fat intake by 9 kcal (Table 1). Outliers in dietary data were winsorized separately for men and women.
Finally, we calculated the Dietary Inflammatory Index (DII) score for each participant following (16). First, we selected the nutrients available to us, then we calculated z-scores by subtracting the standard global mean and dividing by the global standard deviation (the standard global mean and deviation are both found in Table 2 of Shivappa et al. (16). Then, we converted these z-scores to normal percentiles and multiplied them by 2, and subtracted them by 1. Each score was multiplied by its respective inflammatory effect score. Lastly, all scores were summed up to derive the overall DII score for each participant.
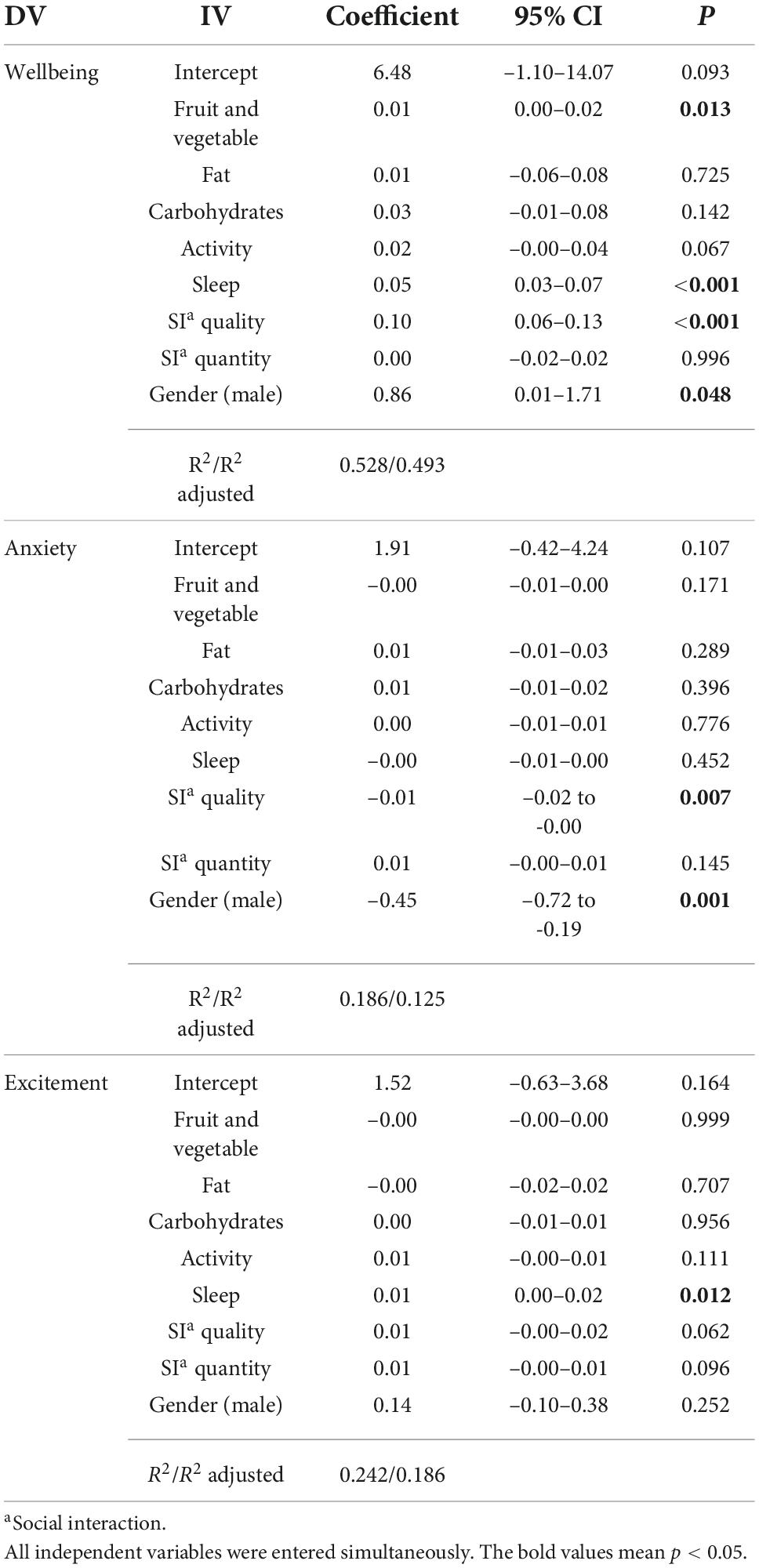
Table 2. Association between diet and lifestyle factors and measures of wellbeing and mood, using multiple linear regression models.
Mood and lifestyle ratings were unlocked after 5 p.m. each day. Participants rated their wellbeing [using the short Warwick-Edinburgh Mental Wellbeing Scale (41)], anxiety, and excitement levels on a 5-point Likert scale. We added excitement and anxiety to daily measures to supplement functional wellbeing. Finally, sleep quality, activity level, quantity, and quality of social interactions were rated on a scale from 1 to 100.
We used the Warwick Edinburgh Mental Wellbeing Scale [WEMWBS (41)] to assess baseline wellbeing. This 14-item questionnaire assesses different aspects of positive mental health including balance of feeling and functioning. Example items include, “I’ve been feeling optimistic about the future” and “I’ve been thinking clearly.” We used the 7-item short form of the WEMWBS to assess daily wellbeing during the week of food-mood-lifestyle diary entries. This scale emphasizes functioning items over feeling items. Both versions are responsive to change (42).
Participants also completed mental health and lifestyle questionnaires, including trait anxiety [STAI (43)], depressive symptoms [BDI; German version (37)], and perceived stress [PSQ (44)]. Finally, the Community Assessment of Psychic Experiences (45) was analyzed as part of a separate study.
All data was downloaded from the FoodApp server, Prolific, and SoSci survey and imported into R studio. Plots were made using ggstatsplot (46). We reported descriptive statistics for demographic characteristics, food intake, daily ratings as well as baseline and trait questionnaire scores.
First, we examined between-person relationships with each averaged daily dependent variable (wellbeing, anxiety, and excitement) separately. Independent variables were fruit and vegetable, fat and carbohydrate intake and lifestyle behaviors (i.e., activity, sleep, social interaction). We performed multiple linear regression using the stats package (47). The full models were specified as shown in equation (1). Gender was dummy-coded.
To investigate if averaged daily measures of lifestyle mediated an effect of fruit and vegetable intake on wellbeing, we performed simple mediation analyses using the MeMoBootR package (48). We wanted to conduct three separate mediation analyses for the outcome variable wellbeing. The mediator variables were averaged from the daily diary; (1) physical activity, (2) sleep, and (3) social behavior. Covariates were, fat, carbohydrate, sleep, quality and quantity of social interaction, and gender.
Next, we performed same-day and 1- and 2-day lagged analyses to test intra-individual relationships between dependent variables (daily wellbeing, anxiety, excitement) and independent variables (i.e., fruit and vegetable, fat and carbohydrate intake) using multilevel modeling using the lme4 package (49). We included fruit and vegetable, fat and carbohydrate each as the level-1 independent variables and daily wellbeing, anxiety, excitement each as the level-1 outcome. We also included the dependent variable’s score of the previous day as a covariate (DVT0).
We assessed same-day associations between fruit and vegetable, fat and carbohydrate intake, wellbeing, anxiety and excitement along with lifestyle covariates [T1; see equation (2)].
One-day lagged associations tested whether eating fruit and vegetable, fat or carbohydrate intake on 1 day (T0) correlated with changes in wellbeing, anxiety and excitement the next day (T1) while controlling for mood on the first day. Lifestyle variables (i.e., activity, sleep, social interactions) were entered as covariates and not lagged [see Equation (3)].
Similarly, 2-day lagged analyses tested whether eating fruit and vegetables, carbohydrates, or dietary fats on 1 day (T0) were associated with wellbeing, anxiety or excitement 2 days later [T2; see Equation (4)]. Gender was dummy-coded.
Exploratory associations between self-reported average fruit and vegetable, fat and carbohydrate intake, sleep, activity, social interaction quality and quantity and mental health questionnaires were tested with Pearson correlations. Significance levels were Bonferroni-corrected for multiple comparisons for each DV separately. Estimated marginal means analysis allowed us to test independent variable × gender effects on wellbeing and were carried out using the emmeans package (50). Mediation with covariates was conducted using the MeMoBootR package (48).
Preregistered hypotheses and analyses are available on the public data repository Open Science Framework (see text footnote 1). We had not preregistered analysis by gender initially, however, after a more in-depth literature analysis it became clear, that gender differences play a larger role than we had previously assumed (8, 19). Therefore, we included gender as a covariate in all models, and tested correlations between wellbeing and (a) fruit and vegetable intake; and (b) social interaction quality stratified by gender.
We intended to include baseline wellbeing as a covariate in the wellbeing model, and similarly, perceived stress (PSQ) and trait anxiety (STAI) as covariates in the anxiety weekly averaged models. However, after observing high correlation between these measures we decided not to include these to avoid biased coefficients (51). In the mixed-effects models we included their wellbeing, anxiety, or excitement levels of the previous day as a covariate following (13) to test associations with daily wellbeing, anxiety, and excitement.
Finally, we originally wanted to use difference scores between habitual and concurrent lifestyle behaviors as mediators. However, at the time of conducting the study, light lockdown had been re-instated for more than 2 weeks. We reasoned that habitual data would reflect lockdown habits rather than pre-lockdown behaviors. Therefore, we used concurrent data of lifestyle behaviors instead.
A total of 135 individuals participated in the study. After data collection, we excluded participants with severe symptom severity on the BDI (> 30, N = 3) as well as participants who logged fewer than 4 days of food intake and mood diary (N = 15). This resulted in a total sample of 117 participants (women N = 45, men N = 72, other = 0). Prior to the study, a power analysis based on a small effect size (f = 0.15), alpha = 0.05, and power of 0.95, estimated a required sample size of 119. Our final sample of N = 117 would deem sufficient.
Averages of daily mood ratings and lifestyle factors are reported alongside baseline and trait questionnaire scores in Table 1. As shown in this table, in our sample women were significantly older than men, and had a lower BMI on average. Intake of kilocalories also differed between men and women (Figure 2A), whereby men had a higher total energy intake and consumed more protein than women. However, women had a significantly higher intake of fruit and vegetables (Figure 2B).
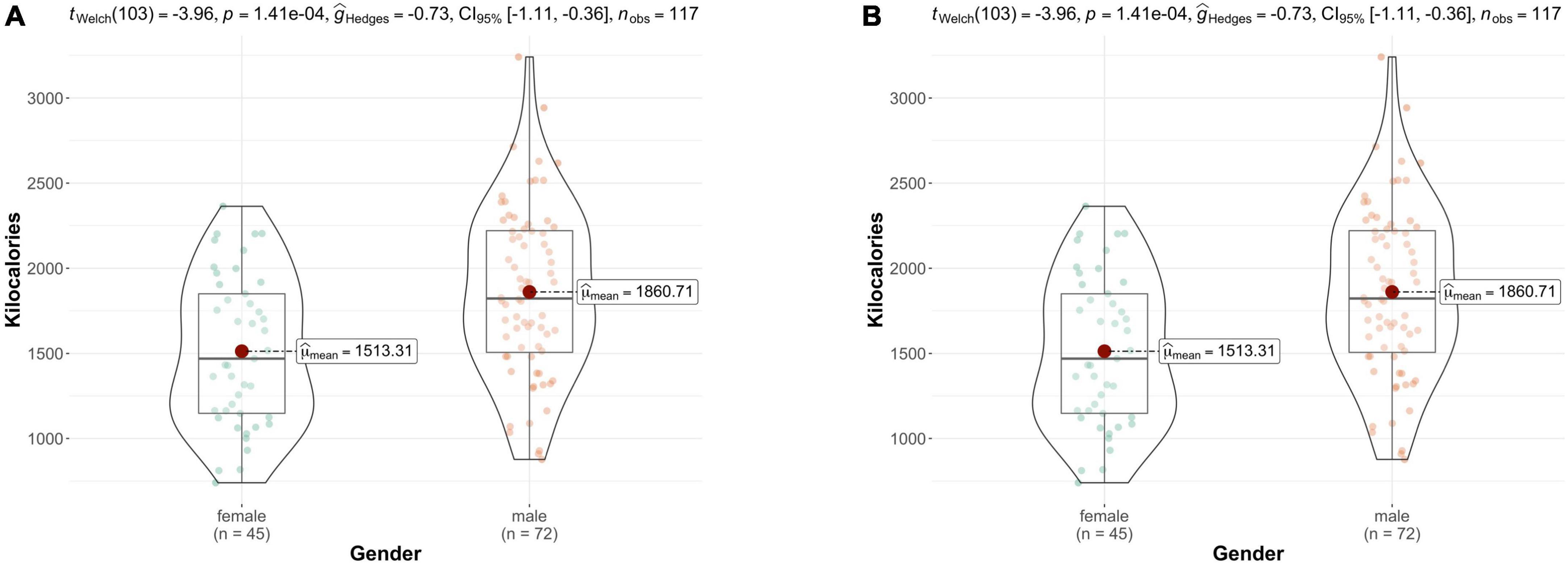
Figure 2. (A) Intake of kilocalories by gender; (B) energy adjusted fruit and vegetable intake by gender. Female participants consumed significantly more fruit and vegetables adjusted for total energy intake. Bars represent the interquartile range, with the median drawn in the middle. Whiskers depict the minimum and maximum values.
Daily mood and lifestyle ratings differed insofar that women reported higher levels of anxiety but also rated their social interactions of a higher quality. Trait anxiety levels were also higher in women than in men. No other significant differences between men and women were found.
We investigated whether wellbeing, anxiety and excitement was associated with averages of the diary data in inter-individual models. Based on the multiple regression models, and as shown in Table 2, we found that fruit and vegetable intake correlated with wellbeing (B = 0.01, CI = 0.00–0.02, p = 0.013) alongside sleep (B = 0.05, CI = 0.03–0.07, p < 0.001), social interaction quality (B = 0.10, CI = 0.06–0.13, p < 0.001) and male gender (B = 0.86, CI = 0.01–1.71, p = 0.048). Anxiety was significantly associated with social interaction quality (B = –0.01, CI = –0.02 to –0.00, p = 0.007) and male gender (B = –0.45, CI = –0.72 to –0.19, p = 0.001). Finally, excitement correlated with sleep quality (B = 0.01, CI = 0.00–0.02, p = 0.012).
Next, we tested if concurrent lifestyle (activity, sleep, social interactions) mediated the effect of food intake on wellbeing while controlling for all other lifestyle factors. To validate using a mediation model, we first tested if fruit and vegetable, fat and carbohydrate intake each regress onto wellbeing, which revealed that only fruit and vegetable intake significantly correlated with wellbeing (B = 0.02, SE = 0, t = 3.20, p = 0.002). Next, we tested whether the independent variable fruit and vegetable intake regressed onto the mediators (activity, sleep, social interactions). Fruit and vegetable intake correlated with activity (B = 0.14, SE = 0.04, t = 3.35, p = 0.001) but neither sleep (B = –0.02, SE = 0.041, t = –0.51, p = 0.614) nor quality of social interaction (B = –0.00, SE = 0.03, t = –0.05, p = 0.960). Thus, we ran a mediation model to test whether activity mediated the effect of fruit and vegetable intake on wellbeing (Figure 3). Indeed, this model revealed that the difference in activity partially mediated the direct effect of fruit and vegetable intake on wellbeing (c’, B = 0.01, SE = 0.01, t = 2.52, p = 0.013) compared to the total effect (c, B = 0.02, SE = 0, t = 3.20, p = 0.002; bootstrapped indirect effect (B = 0.03, SE = 0, 95% CI –0.00–0.01).
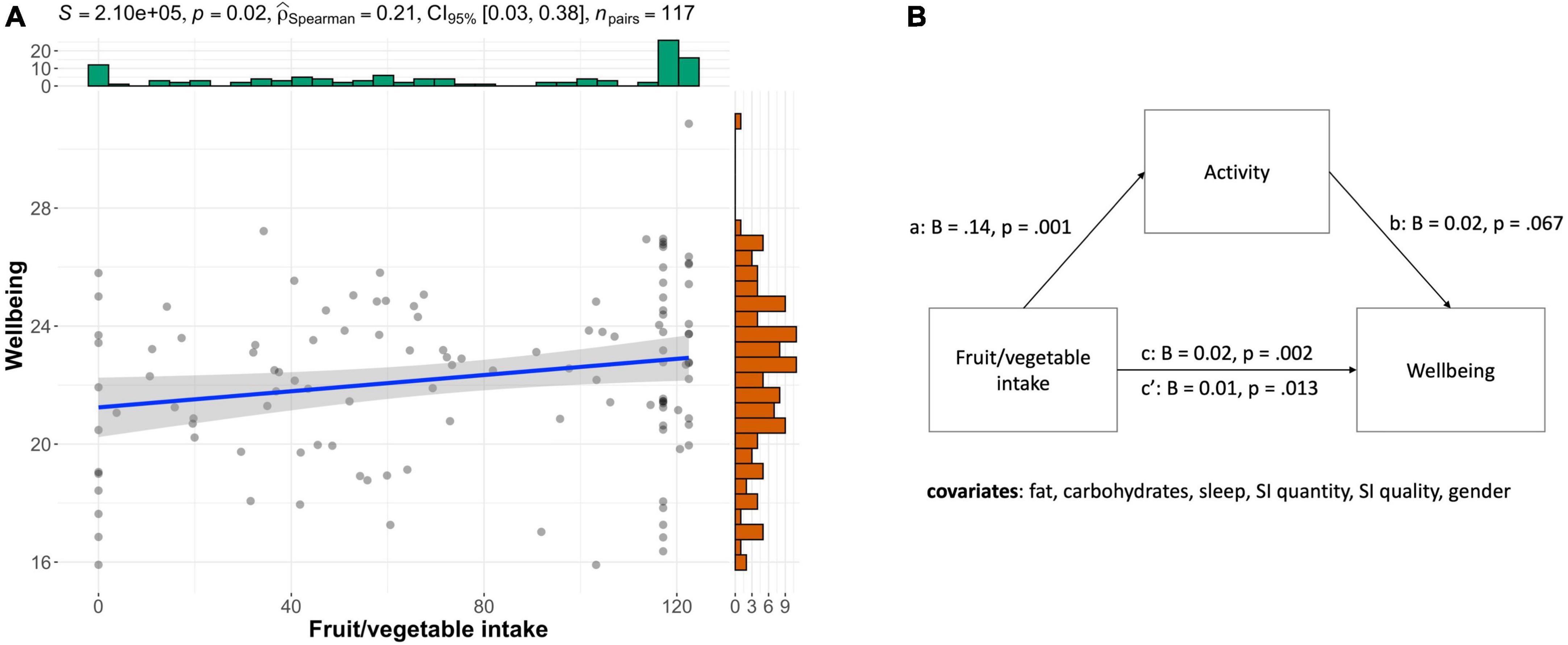
Figure 3. Fruit and vegetable intake affects wellbeing which is partially mediated by activity. (A) Scatterplot showing that fruit and vegetable intake correlates positively with wellbeing (rho = 0.21, p = 0.021). (B) Mediation model, illustrates that higher levels of fruit and vegetable intake were associated with more activity on average (a) and a higher level of wellbeing (c). Activity showed a non-significant positive trend for wellbeing (b). After accounting for the indirect effect, the direct effect remained significant, meaning fruit/veg intake contributes to wellbeing independently of activity (c’).
We also tested intra-individual associations between daily fruit and vegetable, fat and carbohydrate intake and changes in wellbeing using linear mixed-effects models controlling for wellbeing, anxiety, or excitement of the same day, respectively. The results for same-day analyses are shown in Table 3. Same-day wellbeing correlated with fruit and vegetable intake while controlling for same-day sleep, activity and quality, and quantity of social interactions and the previous day’s wellbeing. Neither anxiety nor excitement were associated with diet, but by same-day lifestyle factors.
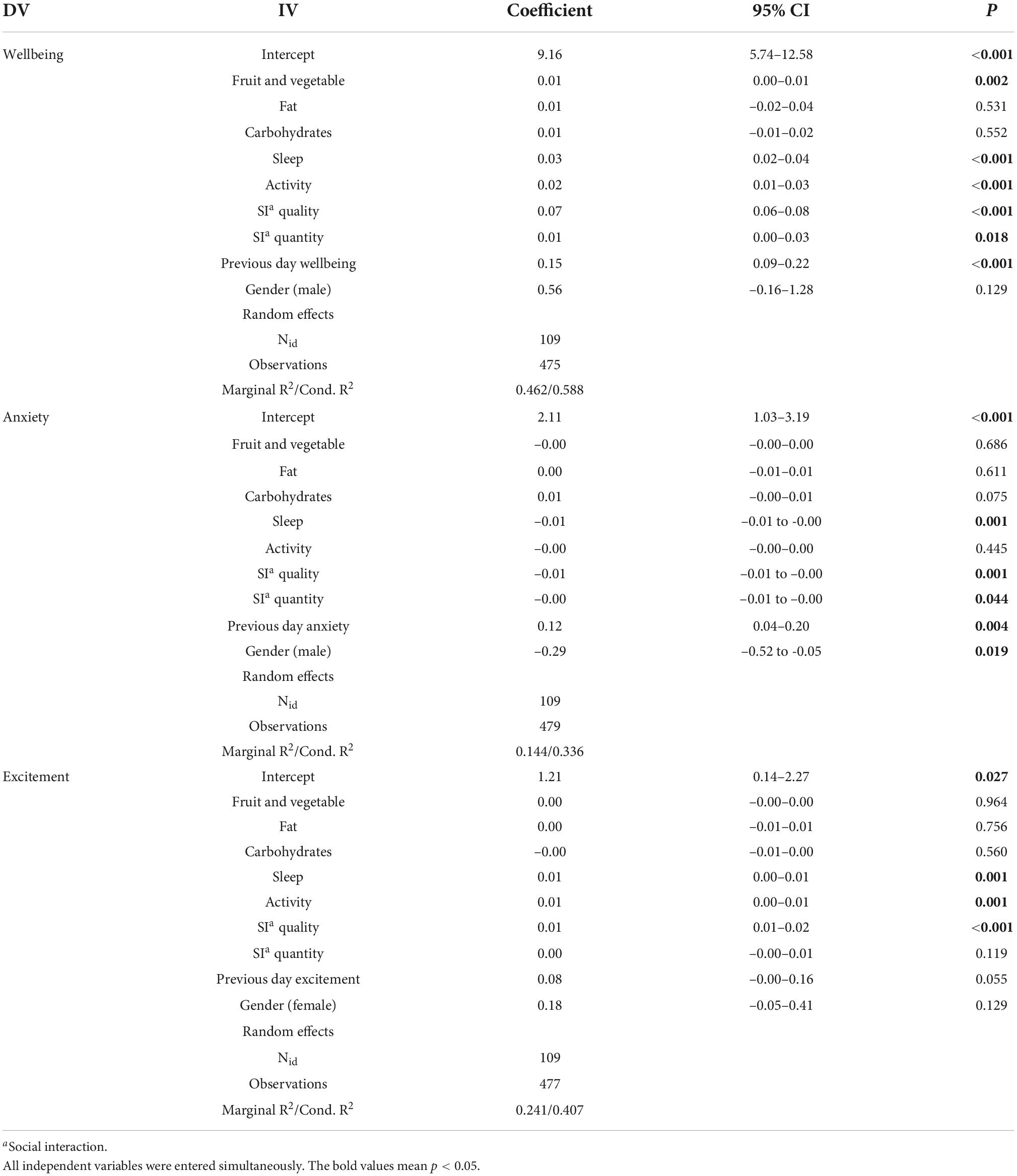
Table 3. Same-day associations between diet and lifestyle factors and measures of wellbeing and mood, using linear mixed-effects models.
We also tested 1-day (Supplementary Table 1) and 2-day-lagged (Supplementary Table 2) associations of fruit and vegetable, fat and carbohydrate intake on wellbeing, anxiety, and excitement each controlling for same-day lifestyle factors revealing similar patterns. For 1-day lags none of the dietary components correlated with wellbeing, anxiety or excitement (all p > 0.296). Instead, daily wellbeing was significantly associated with lifestyle factors sleep, activity, social interaction quality, and the previous day’s level of wellbeing (all p = 0.001 or < 0.001). Anxiety was correlated with sleep and quality of social interactions (all p < 0.001), the previous day’s level of anxiety (p = 0.002) as well as male gender (p = 0.029). Finally, excitement was associated with sleep, activity, social interaction quality (all p = 0.001 or < 0.001), and the previous day’s level of excitement (p = 0.018). Two-day lagged associations did not reveal any significant diet associations when accounting for lifestyle factors in the same model (all p > 0.184).
We explored correlations between mental health questionnaires and individuals’ average dietary and lifestyle behaviors. In Table 4 we report Pearson correlations between baseline mental health and wellbeing questionnaires (as dependent variables) and diet and lifestyle variables. We found that fat intake correlates positively with trait anxiety (r = 0.30, p = 0.007). In addition, self-rated sleep quality and social interaction quality significantly correlate with all dependent variables.
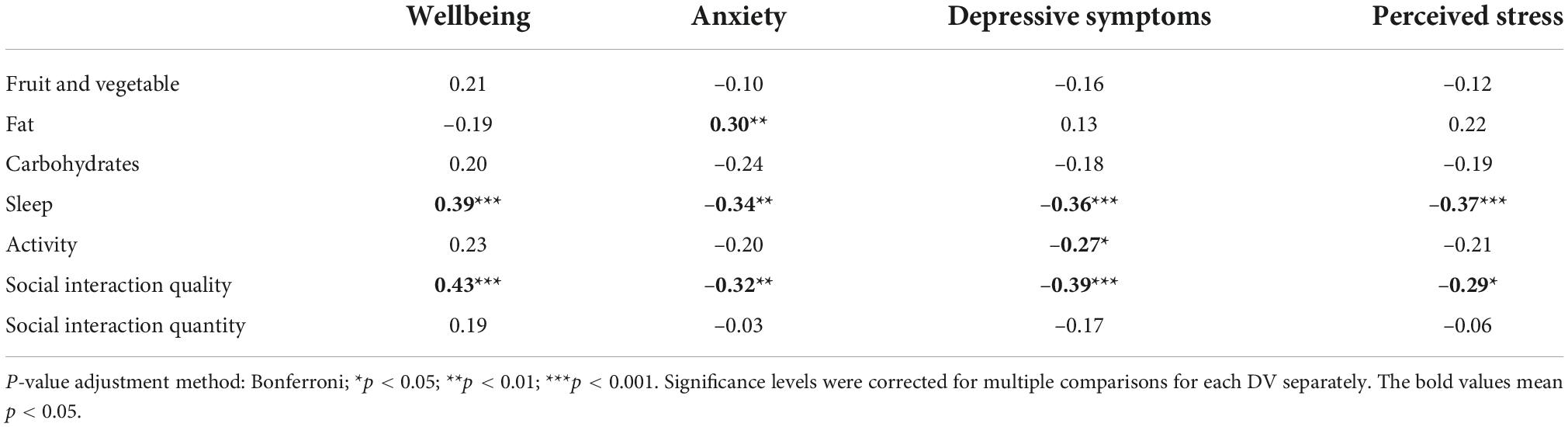
Table 4. Pearson correlations between baseline mental health and wellbeing questionnaires and diet and lifestyle outcomes.
As inflammation is a possible mechanism by which diet affects mental wellbeing, we tested if a high Dietary Inflammatory Index (DII) is associated with lower wellbeing and higher levels of anxiety. DII score correlated significantly with averaged daily wellbeing (r = –0.20, p = 0.027, Figure 4A) but not with anxiety (r = 0.17, p = 0.063) or excitement (r = –0.09, p = 0.332).
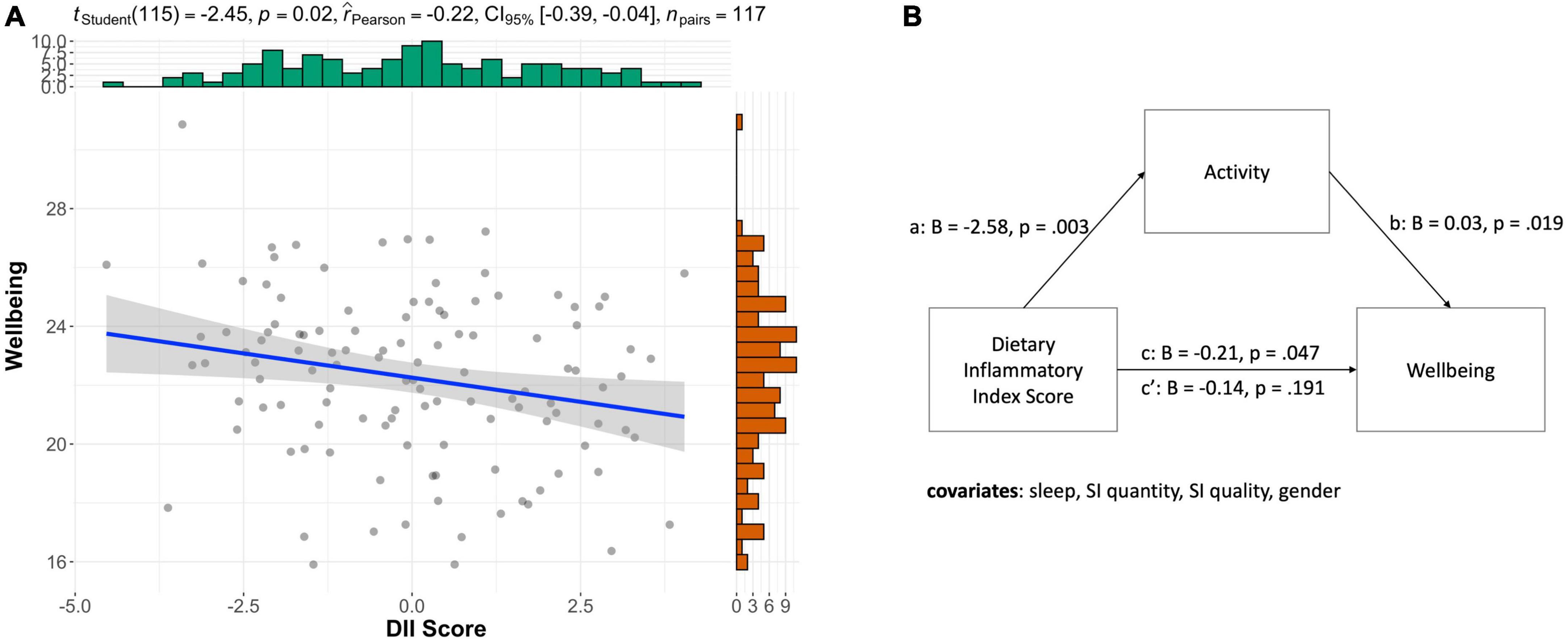
Figure 4. Dietary inflammatory index, wellbeing, and activity. (A) Negative correlation between DII and average wellbeing (r = 0.22, p = 0.016). (B) Mediation model illustrating that a more inflammatory diet was associated with being less active (a) and reporting lower levels of wellbeing (c). While more activity was also associated with higher wellbeing (b).
Based on the mediation effect we found above, we also tested if average daily lifestyle (i.e., activity, sleep, social interactions) mediated the effect of an inflammatory diet on wellbeing. DII negatively correlated with wellbeing (B = –0.20, SE = 0.10, t = –2.00, p = 0.047). As for possible mediators, DII negatively correlated with activity (B = –2.58, SE = 0.86, t = –3.00, p = 0.003) but neither sleep (B = –0.37, SE = 0.84, t = –0.44, p = 0.658) nor social interaction quality (B = –0.15, SE = 0.62, t = –0.23, p = 0.815). Therefore, we tested for a mediation of activity only. We found that activity fully mediated the direct effect (c’) of the dietary inflammatory score on wellbeing (B = –0.14, SE = 0.11, t = –1.32, p = 0.191) compared to the total effect (c, B = –0.21, SE = 0.10, t = –2.00, p = 0.047; bootstrapped indirect effect (B = –0.07, SE = 0.04, 95% CI –0.15 to 0.00) as shown in Figure 4B.
Given that female participants consumed significantly more fruits and vegetables compared to men [Mfemale = 91.96 (35.17), Mmale = 62.48 (44.89), p = 0.009], we explored if the strength of the association between fruit and vegetable intake and wellbeing differed depending on gender. However, as shown in Figure 5, an estimation of the marginal means of linear trends did not show that the interaction between gender and fruit/vegetable intake was significantly different (B = –0.01, p = 0.409).
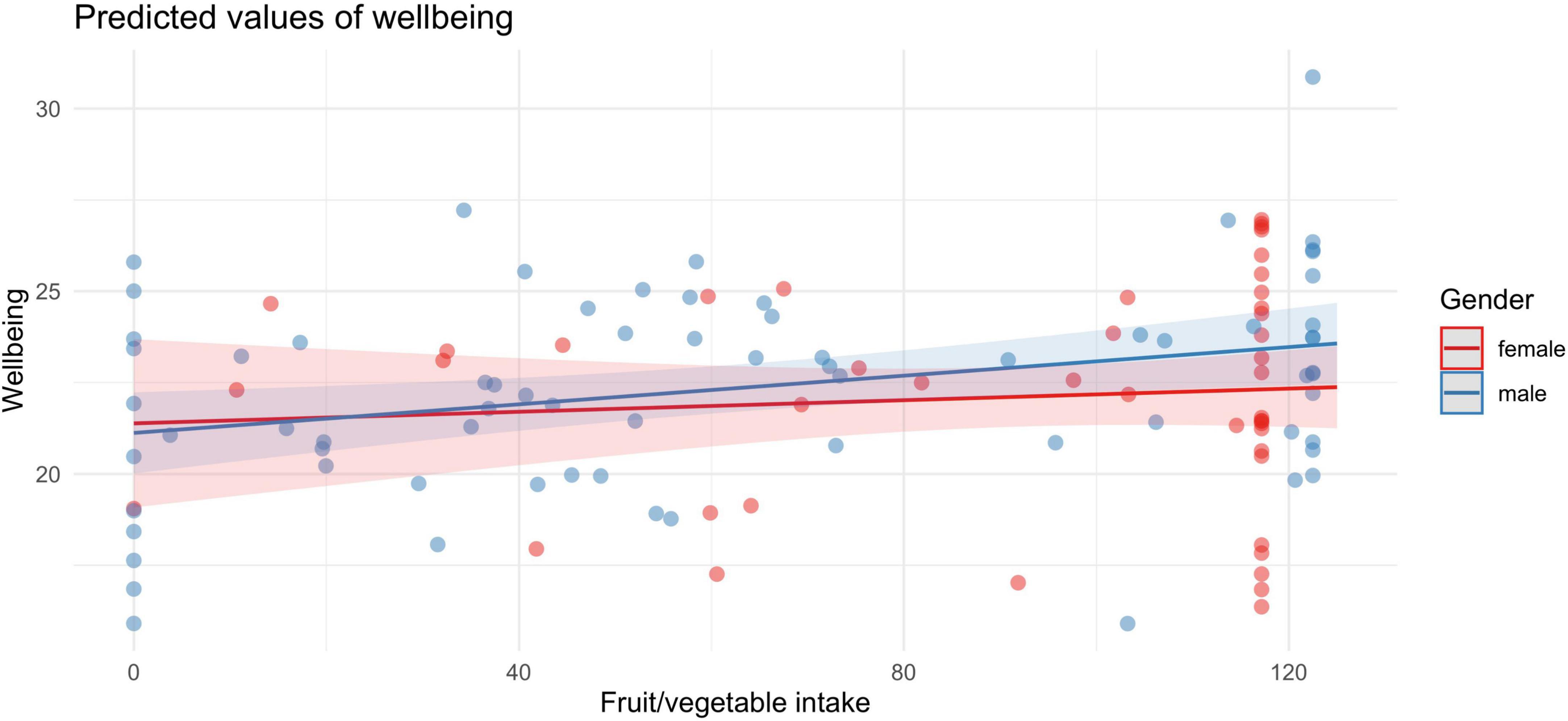
Figure 5. Both men (blue) and women (red) showed a positive association between fruit and vegetable intake and wellbeing.
Given that age and BMI significantly differed between male and female participants (see Table 1), we wondered if these variables could account for the gender effects we found. While fruit and vegetable intake correlated negatively with BMI (r = –0.18, p = 0.048), wellbeing did not (r = –0.07, p = 0.440). However, age did not correlate with either wellbeing (r = 0.05, p = 0.575) or fruit and vegetable intake (r = 0.13, p = 0.166).
The effect of Dietary Inflammatory Index on wellbeing was also independent of gender (B = –0.10, p = 0.732). Furthermore, we were curious as to whether gender differently interacted with social interaction quality and wellbeing. This was not the case (B = 0.05, p = 0.126); for both genders, social interaction quality positively affected wellbeing (for women: B = 0.15, p < 0.001; for men: B = 0.10, p < 0.001). Likewise, sleep was positively associated with wellbeing in both genders (overall contrast: B = 0.07, p = 0.007, for women: B = 0.12, p < 0.001; for men: B = 0.05, p = 0.003).
This preregistered study investigated how dietary intake affected mood and wellbeing alongside lifestyle factors during COVID-19-lockdown. Previous studies showed that dietary components (7, 13, 14), exercise and sleep impacted on mental health and wellbeing (4). We were also interested in social interaction as a contributor to wellbeing (29), since social distancing measures were so prominent during lockdowns.
We hypothesized that food intake was associated with (1) wellbeing; (2) anxiety; and (3) excitement and tested between- and within-person relationships while controlling for concurrent lifestyle factors. Both in our regression models, as well as mediation analysis, we observed that fruit and vegetable intake correlated with wellbeing, while this was partially mediated by physical activity.
The pandemic context brought about changes in diet, sleep, and activity (52), which brought about increased negative mood (52–55) and lower wellbeing (1). Lower dietary quality was associated with poor mood and may have been used to regulate emotions (55). The present findings complement this by providing evidence that inversely, consuming healthier foods, i.e., fruit and vegetable, were linked with more wellbeing. Work by Cecchetto and colleagues’ investigated whether social factors (amongst others) contributed to dysfunctional eating habits during the pandemic (36). However, a more holistic approach of lifestyle factors that include physical activity, sleep, dietary intake and social interaction to investigate their joint effect on wellbeing, anxiety and excitement had thus far been lacking.
Undergoing lockdown may have undermined the impact of diet on mood when accounting for other healthful behaviors. For example, mood affects the likelihood of making healthy food choices mediated by physical activity (56). The authors suggest that people engage in healthy lifestyles rather than isolated health behaviors, i.e., being physically active goes together with making healthier dietary choices (56). Our data support this notion; high intakes of fruit and vegetable as well as physical activity were associated with increased levels of wellbeing.
Additionally, other lifestyle factors may have gained importance during this period. Highly active people experienced significant declines in quality of sleep and wellbeing during lockdown as compared to sedentary individuals (2). Furthermore, dramatic declines in physical activity, especially walking, were recorded due to lockdown restrictions and increased home-office hours or job termination in this period (57). Being active outdoors compared to indoors may contribute further to mental wellbeing in addition to the exercise itself (58). The more time spent outdoors in daylight lowered the risk of depression, low mood and added to happiness (59). Thus, lockdown restrictions may have magnified beneficial effects of physical activity during lockdown, and even more so when activity happened outdoors.
Finally, social interactions were greatly affected by social distancing measures. For example, social media use increased during the pandemic (60) and was linked to poor mental health in a large cross-country sample (61), and increased the odds of experiencing anxiety in a Chinese (62) and American sample (60). While greater social connectedness was associated with less perceived stress during the pandemic (63). In line with the existing literature, we found that the quality but not quantity of social interactions correlated with mood and wellbeing in almost all analyses, echoing previous findings (64). To our knowledge, social interactions have not yet been considered in models alongside diet, sleep, and activity. Our findings suggest that during lockdown the quality of social interactions plays a key role when examining the relationship between diet, wellbeing, and mood.
Dietary intake can be analyzed in many different ways. Here we focused on specific dietary components. Fat, carbohydrates, and fruit and vegetable intake had been identified in the literature to play a key role in mood and wellbeing (13, 14, 65). Our findings supported the role of fruit and vegetable intake in concurrent wellbeing. Furthermore, we found an association between trait anxiety and fat intake, whereby higher fat intake correlated with greater state anxiety. However, we did not find that total fat intake correlated with daily anxiety levels when controlling for other lifestyle factors.
Additionally, we calculated the dietary inflammatory index—a well-established measure of a diet’s inflammatory potential (16). We found that DII score correlated negatively with average wellbeing but not with anxiety or excitement. DII score has been found to correlate with wellbeing before (66). We also found that the effect of DII on wellbeing was fully mediated by activity.
We examined whether dietary intake was associated with wellbeing, anxiety, and excitement. However, vice versa, it is an interesting question whether negative mood and mental health issues can drive low-quality food intake. Neither longitudinal (67) nor short-term evidence, 1- or 2-day lagged associations (13, 14) support this idea. However, a recent study conducted during COVID-19-lockdown found that mood states were linked to the intake of fruit, vegetables, and fish, which were partially mediated by physical exercise load (56). The authors suggested that some participants may have actively changed their exercise and food intake behavior to deal with the anticipated challenges on mental health during lockdown (56). Importantly, these authors included exercise as a lifestyle factor to investigate the relationship between mood and diet. In sum, the differences between studies may be due to the unusual circumstances of the pandemic as well as the mediating factor of physical exercise, which was affected by pandemic restrictions (27, 57). Finally, Amatori et al. did not report testing the reverse direction, i.e., whether dietary intake was correlated with mood states (56).
Here we found gender differences in food intake, anxiety levels, and quality of social interaction. In particular, women consumed more fruit and vegetables but fewer calories from protein than men. This is in line with previous work demonstrating gender differences in dietary intake (68–70). For instance, women across 23 countries showed greater beliefs in the importance of healthy eating as evident by higher intake of fruit and fiber-rich foods (70). In this study, women reported higher baseline and concurrent anxiety levels than men in this study, consistent with previous findings (71). But we did not find that higher fruit and vegetable intake was associated with lower anxiety ratings, contrary to what has been reported elsewhere (8). Eating more fruit and vegetables also did not affect wellbeing to a greater extent than men. It is currently unclear why women’s mood did not benefit from fruit and vegetable intake more so than men despite higher intake, or why anxiety levels were unaffected by higher fruit and vegetable intake. Thus, more research is needed to better understand mechanistic links between diet, body, brain, and gender interactions.
A few limitations need to be considered. First, due to the acute nature of the pandemic, we lack a baseline dietary assessment, and cannot make claims whether dietary intake has changed in response to the lockdown. Second, as with any self-report study, these measures underlie self-reporting biases. For example, self-reported caloric intake is likely underreported. Underreporting is a common problem in self-reported dietary data (72). Note that we also chose to exclude individuals with mental health diagnoses and severe depressive symptoms, therefore our findings cannot be generalized to subclinical and clinical populations.
Strengths of this study include the use of preregistration of hypotheses and analyses before data collection. Considering that dietary intake alongside multiple lifestyle factors and social aspects is still understudied, highlights the need for a holistic approach to assess lifestyle with mood and mental health outcomes. Furthermore, we were able to collect a rich data set by assessing baseline parameters of mental health and lifestyle followed by a 7-day diary of food intake. Using such a food diary, rather than a 24-hr recall, alongside concurrent mood and lifestyle factors allowed us to explore both inter- and intra-individual fluctuations of these variables. The findings of this study are limited to a relatively young German population, and further research would be needed to determine if the same effects can be found for different age groups and specific health groups. An interesting avenue for future studies would be to investigate whether the dynamic between mood, diet, lifestyle, and social interactions still holds beyond the acute lockdown situation observed in this study, and whether this extends to different individuals such as clinical populations.
Our results showed that, on average, fruit and vegetable intake contributed to wellbeing alongside sleep and social interaction quality. Examining day-to-day associations showed that fruit and vegetable intake on the same day promoted wellbeing, while this was not the case for the next day or second day time lags. Instead, sleep, activity, and social interactions were associated with wellbeing in the context of lockdown during the COVID-19 pandemic. Importantly, associations between fruit and vegetable intake were partially mediated by physical activity. These findings highlight the need for an integrated way of assessing lifestyle factors and gender in future studies. As pandemics are thought to appear more frequently due to diminishing biodiversity (73), strategies to protect mental health and wellbeing become more important than ever, especially because access to mental health care remains limited for many. Therefore, reducing the risk for adverse psychological effects via lifestyle behaviors such as diet, activity, and sleep remains a promising strategy [for a meta-review on lifestyle psychiatry see Firth et al. (4)].
In conclusion, a combination of physical activity, good sleep, and daily high-quality social interactions as well as a diet rich in fruit and vegetables and a low inflammatory potential (i.e., diets high in minerals and vitamins, such as fruit and vegetables, but low in saturated fats) appears to promote better mood and wellbeing in stressful circumstances such as a lockdown during a global pandemic. Our research result offers a novel perspective of dietary and lifestyle recommendations that can be provided in times of high uncertainty, such as pandemic situation.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Humboldt University of Berlin. The patients/participants provided their written informed consent to participate in this study.
A-KM and SP: conceptualization and project administration. A-KM: investigation, visualization, and writing—original draft preparation. A-KM, AL, and SP: methodology and formal analysis. A-KM, AL, DT, and SP: writing—review and editing. AL and SP: supervision. SP: funding acquisition. All authors have read and agreed to the published version of the manuscript.
This research was funded by the German Ministry of Education and Research (BMBF), the State of Brandenburg and the German Center for Diabetes Research (DZD, 82DZD00302).
We would like to thank Vadim Schäfer and Zen Melzer for the development and maintenance of the FoodApp without which we could not have collected the food-mood data.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.993180/full#supplementary-material
1. Hu Z, Lin X, Kaminga AC, Xu H. Impact of the covid-19 epidemic on lifestyle behaviors and their association with subjective well-being among the general population in mainland China: cross-sectional study. J Med Internet Res. (2020) 22:e21176. doi: 10.2196/21176
2. Martínez-de-Quel Ó, Suárez-Iglesias D, López-Flores M, Pérez CA. Physical activity, dietary habits and sleep quality before and during covid-19 lockdown: a longitudinal study. Appetite. (2021) 158:105019. doi: 10.1016/j.appet.2020.105019
3. Pieh C, Budimir S, Probst T. The effect of age, gender, income, work, and physical activity on mental health during coronavirus disease (covid-19) lockdown in Austria. J Psychosom Res. (2020) 136:110186. doi: 10.1016/j.jpsychores.2020.110186
4. Firth J, Solmi M, Wootton RE, Vancampfort D, Schuch FB, Hoare E, et al. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in the prevention and treatment of mental disorders. World Psychiatr. (2020) 19:360–80. doi: 10.1002/wps.20773
5. Lai JS, Hiles S, Bisquera A, Hure AJ, McEvoy M, Attia J. A systematic review and meta-analysis of dietary patterns and depression in community-dwelling adults. Am J Clin Nutr. (2013) 99:181–97. doi: 10.3945/ajcn.113.069880
6. Psaltopoulou T, Sergentanis TN, Panagiotakos DB, Sergentanis IN, Kosti R, Scarmeas N. Mediterranean diet, stroke, cognitive impairment, and depression: a meta-analysis. Ann Neurol. (2013) 74:580–91. doi: 10.1002/ana.23944
7. Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and vegetable intake and mental health in adults: a systematic review. Nutrients. (2020) 12:115. doi: 10.3390/nu12010115
8. Jacka FN, Pasco JA, Mykletun A, Williams LJ, Hodge AM, O’Reilly SL, et al. Association of western and traditional diets with depression and anxiety in women. Am J Psychiatr. (2010) 167:305–11. doi: 10.1176/appi.ajp.2009.09060881
9. Berdanier C, Zempleni J. Advanced Nutrition Macronutrients, Micronutrients, and Metabolism. Boca Raton, FL: CRC Press (2009).
10. Sánchez-Villegas A, Verberne L, Irala JD, Ruíz-Canela M, Toledo E, Serra-Majem L, et al. Dietary fat intake and the risk of depression: the sun project. PLoS One. (2011) 6:e16268. doi: 10.1371/journal.pone.0016268
11. Sánchez-Villegas A, Toledo E, Irala JD, Ruiz-Canela M, Pla-Vidal J, Martínez-González MA. Fast-food and commercial baked goods consumption and the risk of depression. Public Health Nutr. (2012) 15:424–32. doi: 10.1017/s1368980011001856
12. Conner TS, Brookie KL, Richardson AC, Polak MA. On carrots and curiosity: eating fruit and vegetables is associated with greater flourishing in daily life. Br J Health Psychol. (2015) 20:413–27. doi: 10.1111/bjhp.12113
13. White BA, Horwath CC, Conner TS. Many apples a day keep the blues away – daily experiences of negative and positive affect and food consumption in young adults. Br J Health Psychol. (2013) 18:782–98. doi: 10.1111/bjhp.12021
14. Hendy HM. Which comes first in food–mood relationships, foods or moods? Appetite. (2012) 58:771–5. doi: 10.1016/j.appet.2011.11.014
15. Muth A-K, Park SQ. The impact of dietary macronutrient intake on cognitive function and the brain. Clin Nutr. (2021) 40:3999–4010. doi: 10.1016/j.clnu.2021.04.043
16. Shivappa N, Steck SE, Hurley TG, Hussey JR, Hébert JR. Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr. (2014) 17:1689–96. doi: 10.1017/s1368980013002115
17. Wang J, Zhou Y, Chen K, Jing Y, He J, Sun H, et al. Dietary inflammatory index and depression: a meta-analysis. Public Health Nutr. (2019) 22:654–60. doi: 10.1017/s1368980018002628
18. Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, et al. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatr. (2019) 24:965–86. doi: 10.1038/s41380-018-0237-8
19. Haghighatdoost F, Feizi A, Esmaillzadeh A, Feinle-Bisset C, Keshteli AH, Afshar H, et al. Association between the dietary inflammatory index and common mental health disorders profile scores. Clin Nutr. (2019) 38:1643–50. doi: 10.1016/j.clnu.2018.08.016
20. Salari-Moghaddam A, Keshteli AH, Afshar H, Esmaillzadeh A, Adibi P. Association between dietary inflammatory index and psychological profile in adults. Clin Nutr. (2019) 38:2360–8. doi: 10.1016/j.clnu.2018.10.015
21. Fox KR. The influence of physical activity on mental well-being. Public Health Nutr. (1999) 2:411–8. doi: 10.1017/s1368980099000567
22. Stephens T. Physical activity and mental health in the United States and Canada: evidence from four population surveys. Prevent Med. (1988) 17:35–47. doi: 10.1016/0091-7435(88)90070-9
23. Schuch FB, Vancampfort D, Firth J, Rosenbaum S, Ward PB, Silva ES, et al. Physical activity and incident depression: a meta-analysis of prospective cohort studies. Am J Psychiatr. (2018) 175:631–48. doi: 10.1176/appi.ajp.2018.17111194
24. Schuch FB, Stubbs B, Meyer J, Heissel A, Zech P, Vancampfort D, et al. Physical activity protects from incident anxiety: a meta-analysis of prospective cohort studies. Depress Anxiety. (2019) 36:846–58. doi: 10.1002/da.22915
25. McDowell CP, Dishman RK, Gordon BR, Herring MP. Physical activity and anxiety: a systematic review and meta-analysis of prospective cohort studies. Am J Prevent Med. (2019) 57:545–56. doi: 10.1016/j.amepre.2019.05.012
26. Youngstedt SD, O’Connor PJ, Dishman RK. The effects of acute exercise on sleep: a quantitative synthesis. Sleep. (1997) 20:203–14. doi: 10.1093/sleep/20.3.203
27. Busse H, Buck C, Stock C, Zeeb H, Pischke CR, Fialho PMM, et al. Engagement in health risk behaviours before and during the covid-19 pandemic in German university students: results of a cross-sectional study. Int J Environ Res Public Health. (2021) 18:1410. doi: 10.3390/ijerph18041410
28. Wu X, Tao S, Zhang Y, Zhang S, Tao F. Low physical activity and high screen time can increase the risks of mental health problems and poor sleep quality among Chinese college students. PLoS One. (2015) 10:e0119607. doi: 10.1371/journal.pone.0119607
29. Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. (2001) 78:458–67. doi: 10.1093/jurban/78.3.458
30. Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. (2017) 152:157–71. doi: 10.1016/j.puhe.2017.07.035
31. Terenzi D, Liu L, Bellucci G, Park SQ. Determinants and modulators of human social decisions. Neurosci Biobehav Rev. (2021) 128:383–93. doi: 10.1016/j.neubiorev.2021.06.041
32. Vancampfort D, Knapen J, Probst M, Scheewe T, Remans S, Hert MD. A systematic review of correlates of physical activity in patients with schizophrenia. Acta Psychiatr Scand. (2012) 125:352–62. doi: 10.1111/j.1600-0447.2011.01814.x
33. Vancampfort D, Probst M, Skjaerven LH, Catalán-Matamoros D, Lundvik-Gyllensten A, Gómez-Conesa A, et al. Systematic review of the benefits of physical therapy within a multidisciplinary care approach for people with Schizophrenia. Phys Ther. (2012) 92:11–23. doi: 10.2522/ptj.20110218
34. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students’ social networks and mental health before and during the covid-19 crisis in Switzerland. PLoS One. (2020) 15:e0236337. doi: 10.1371/journal.pone.0236337
35. Dimmock J, Krause AE, Rebar A, Jackson B. Relationships between social interactions, basic psychological needs, and wellbeing during the covid-19 pandemic. Psychol Health. (2022) 37:457–69. doi: 10.1080/08870446.2021.1921178
36. Cecchetto C, Aiello M, Gentili C, Ionta S, Osimo SA. Increased emotional eating during covid-19 associated with lockdown, psychological and social distress. Appetite. (2021) 160:105122. doi: 10.1016/j.appet.2021.105122
37. Hautzinger M, Beiler M, Worall H, Keller F. Beck-Depressions-Inventar (BDI). Bern, Switzerland: Huber Verlag (1994).
38. Dehne LI, Klemm Ch, Henseler G, Bögl KW, Hermann-Kunz E. Der Bundeslebensmittelschlüssel (BLS II.2). Bundesgesundheitsblatt. (1997) 40:203–6. doi: 10.1007/bf03044213
39. Banna JC, McCrory MA, Fialkowski MK, Boushey C. Examining plausibility of self-reported energy intake data: considerations for method selection. Front Nutr. (2017) 4:45. doi: 10.3389/fnut.2017.00045
40. Agnoli C, Pounis G, Krogh V. Dietary Pattern Analysis. In: G Pounis editor. Analysis in Nutrition Research: Principles of Statistical Methodology and Interpretation of the Results. Cambridge, MA, USA: Academic Press (2019) 75–101. doi: 10.1016/b978-0-12-814556-2.00004-x
41. Tennant R, Hiller L, Fishwick R, Platt S, Joseph S, Weich S, et al. The warwick-edinburgh mental well-being scale (WEMWBS): development and UK validation. Health Qual Life Outcomes. (2007) 5:63. doi: 10.1186/1477-7525-5-63
42. Maheswaran H, Weich S, Powell J, Stewart-Brown S. Evaluating the responsiveness of the warwick edinburgh mental well-being scale (WEMWBS): group and individual level analysis. Health Qual Life Outcomes. (2012) 10:156. doi: 10.1186/1477-7525-10-156
43. Grimm J. State-Trait-Anxiety Inventory nach Spielberger. Deutsche Lang- und Kurzversion. Vienna: Methodenforum der UniversitätWien (2009).
44. Levenstein S, Prantera C, Varvo V, Scribano ML, Berto E, Luzi C, et al. Development of the perceived stress questionnaire: a new tool for psychosomatic research. J Psychosom Res. (1993) 37:19–32. doi: 10.1016/0022-3999(93)90120-5
45. Schlier B, Jaya ES, Moritz S, Lincoln TM. The Community Assessment of Psychic Experiences measures nine clusters of psychosis-like experiences: a validation of the German version of the CAPE. Schizophr Res. (2015) 169:274–9. doi: 10.1016/j.schres.2015.10.034
46. Patil I. Visualizations with statistical details: the “ggstatsplot” approach. J Open Source Software. (2021) 6:3167. doi: 10.21105/joss.03167
47. R Core Team.R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing (2012).
48. Buchanan E. MeMoBootR: Mediation-Moderation with Bootstrapping in R. R package version 0.0.0.7001. (2021).
49. Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Statis Software. (2015) 67:1–48. doi: 10.18637/jss.v067.i01
50. Lenth R. emmeans: Estimated Marginal Means, Aka Least-Squares Means. R Package Version 1.7.0. Vienna: CRAN (2021).
51. Vermeer ABL, Muth A, Terenzi D, Park SQ. Curiosity for information predicts wellbeing mediated by loneliness during covid-19 pandemic. Sci Rep. (2022) 12:7771. doi: 10.1038/s41598-022-11924-z
52. Ingram J, Maciejewski G, Hand CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during covid-19 lockdown. Front Psychol. (2020) 11:588604. doi: 10.3389/fpsyg.2020.588604
53. McAtamney K, Mantzios M, Egan H, Wallis DJ. Emotional eating during covid-19 in the United Kingdom: exploring the roles of alexithymia and emotion dysregulation. Appetite. (2021) 161:105120. doi: 10.1016/j.appet.2021.105120
54. Renzo LD, Gualtieri P, Cinelli G, Bigioni G, Soldati L, Attinà A, et al. Psychological aspects and eating habits during covid-19 home confinement: results of ehlc-covid-19 italian online survey. Nutrients. (2020) 12:2152. doi: 10.3390/nu12072152
55. Marty L, Lauzon-Guillain BD, Labesse M, Nicklaus S. Food choice motives and the nutritional quality of diet during the covid-19 lockdown in France. Appetite. (2021) 157:105005. doi: 10.1016/j.appet.2020.105005
56. Amatori S, Zeppa SD, Preti A, Gervasi M, Gobbi E, Ferrini F, et al. Dietary habits and psychological states during covid-19 home isolation in italian college students: the role of physical exercise. Nutrients. (2020) 12:3660. doi: 10.3390/nu12123660
57. Hunter RF, Garcia L, de Sa TH, Zapata-Diomedi B, Millett C, Woodcock J, et al. Effect of covid-19 response policies on walking behavior in US cities. Nat Commun. (2021) 12:3652. doi: 10.1038/s41467-021-23937-9
58. Coon JT, Boddy K, Stein K, Whear R, Barton J, Depledge MH. Does participating in physical activity in outdoor natural environments have a greater effect on physical and mental wellbeing than physical activity indoors? A systematic review. Environ Sci Technol. (2011) 45:1761–72. doi: 10.1021/es102947t
59. Burns AC, Saxena R, Vetter C, Phillips AJK, Lane JM, Cain SW. Time spent in outdoor light is associated with mood, sleep, and circadian rhythm-related outcomes: a cross-sectional and longitudinal study in over 400,000 UK biobank participants. J Affect Disord. (2021) 295:347–52. doi: 10.1016/j.jad.2021.08.056
60. Drouin M, McDaniel BT, Pater J, Toscos T. How parents and their children used social media and technology at the beginning of the covid-19 pandemic and associations with anxiety. Cyberpsychol Behav Soc Netw. (2020) 23:727–36. doi: 10.1089/cyber.2020.0284
61. Geirdal AØ, Ruffolo M, Leung J, Thygesen H, Price D, Bonsaksen T, et al. Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the covid-19 outbreak. A cross-country comparative study. J Ment Health. (2021) 30:148–55. doi: 10.1080/09638237.2021.1875413
62. Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during covid-19 outbreak. PLoS One. (2020) 15:e0231924. doi: 10.1371/journal.pone.0231924
63. Nitschke JP, Forbes PAG, Ali N, Cutler J, Apps MAJ, Lockwood PL, et al. Resilience during uncertainty? Greater social connectedness during covid-19 lockdown is associated with reduced distress and fatigue. Br J Health Psychol. (2021) 26:553–69. doi: 10.1111/bjhp.12485
64. Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. (2000) 15:187–224. doi: 10.1037//0882-7974.15.2.187
65. Ugartemendia L, Bravo R, Castaño MY, Cubero J, Zamoscik V, Kirsch P, et al. Influence of diet on mood and social cognition: a pilot study. Food Func. (2020) 11:8320–30. doi: 10.1039/d0fo00620c
66. Phillips CM, Shivappa N, Hébert JR, Perry IJ. Dietary inflammatory index and mental health: a cross-sectional analysis of the relationship with depressive symptoms, anxiety and well-being in adults. Clin Nutr. (2018) 37:1485–91. doi: 10.1016/j.clnu.2017.08.029
67. Port AL, Gueguen A, Kesse-Guyot E, Melchior M, Lemogne C, Nabi H, et al. Association between dietary patterns and depressive symptoms over time: a 10-year follow-up study of the gazel cohort. PLoS One. (2012) 7:e51593. doi: 10.1371/journal.pone.0051593
68. Bates C, Prentice A, Finch S. Gender differences in food and nutrient intakes and status indices from the national diet and nutrition survey of people aged 65 years and over. Eur J Clin Nutr. (1999) 53:694–9. doi: 10.1038/sj.ejcn.1600834
69. Fagerli RA, Wandel M. Gender differences in opinions and practices with regard to a “healthy diet”>. Appetite. (1999) 32:171–90. doi: 10.1006/appe.1998.0188
70. Wardle J, Haase AM, Steptoe A, Nillapun M, Jonwutiwes K, Bellisie F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med. (2004) 27:107–16. doi: 10.1207/s15324796abm2702_5
71. Hallers-Haalboom ET, Maas J, Kunst LE, Bekker MHJ. Chapter 22 The role of sex and gender in anxiety disorders: being scared “like a girl”? Handbook Clin Neurol. (2020) 175:359–68. doi: 10.1016/b978-0-444-64123-6.00024-2
72. Ravelli MN, Schoeller DA. Traditional self-reported dietary instruments are prone to inaccuracies and new approaches are needed. Front Nutr. (2020) 7:90. doi: 10.3389/fnut.2020.00090
Keywords: eating behavior, mental health, COVID-19, gender, activity
Citation: Muth A-K, Losecaat Vermeer A, Terenzi D and Park SQ (2022) The impact of diet and lifestyle on wellbeing in adults during COVID-19 lockdown. Front. Nutr. 9:993180. doi: 10.3389/fnut.2022.993180
Received: 13 July 2022; Accepted: 23 September 2022;
Published: 06 October 2022.
Edited by:
Carol Coricelli, Western University, CanadaReviewed by:
Laura Maria König, University of Bayreuth, GermanyCopyright © 2022 Muth, Losecaat Vermeer, Terenzi and Park. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Damiano Terenzi, ZGFtaWFub3RlcmVuemlAZ21haWwuY29t; Soyoung Q. Park, U295b3VuZy5xLnBhcmtAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.