- 1Institute of Child and Adolescent Health, School of Public Health, Peking University, Beijing, China
- 2National Health Commission Key Laboratory of Reproductive Health, Peking University, Beijing, China
Background: Cardio-metabolic risk factors (CMRFs) represent the accumulation of metabolic abnormalities, significantly increasing the likelihood of cardiovascular diseases. Although studies assessed the independent association of single-child status and lifestyle risk factors with components of CMRFs or clustered CMRFs, little has been known about the combined effect of single-child status and lifestyles on clustered CMRFs as well as sex differences.
Materials and methods: Data was collected from a cross-sectional survey conducted in September 2013 in China. A total of 13,859 children and adolescents aged 7–18 years with blood samples were included. Anthropometric measurements and serum biochemical indexes were collected to assess clustered CMRFs, while questionnaires were used to obtain single-child status, lifestyle information, and characteristics of children and their parents. Mixed effect logistic regression was applied to analyze the independent and the combined effects of single-child status and ideal lifestyle category on clustered CMRFs.
Results: The prevalence of clustered CMRFs was 3.4%, with a higher prevalence in boys (4.0%) than girls (2.7%). Children and adolescents with clustered CMRFs had a higher proportion of single children (76.6 vs. 69.7%) and unfavorable lifestyles (62.1 vs. 29.2%) compared with their peers with non-clustered CMRFs. Both single children (OR = 1.67, 95% CI: 1.32–2.11) and unfavorable lifestyles (OR = 9.03, 95% CI: 6.26–13.02) were associated with an increased risk of clustered CMRFs. The risk of clustered CMRFs increased significantly (OR = 12.79, 95% CI: 6.67–24.52) when single children and an unfavorable lifestyle were combined, which was almost neutralized (OR = 1.33, 95% CI: 0.63–2.82) when single children adhered to a favorable lifestyle. However, no sex differences were observed in this study.
Conclusion: Single children with unfavorable lifestyles were associated with an obvious risk of clustered CMRFs, which might be partially offset by expanding family size (the number of siblings) or establishing a favorable lifestyle. A birth-friendly social environment as well as a family environment with a favorable lifestyle are encouraged in China.
Introduction
Cardiovascular diseases (CVDs) are the leading cause of death globally, accounting for 32% of all deaths (1), while in China this proportion has exceeded 40%, accompanied by an age-standardized mortality rate for males being 1.5 times higher than females (2). Cardio-metabolic risk factors (CMRFs) represent the accumulation of metabolic abnormalities, including hypertension, dyslipidemia, hyperglycemia, and abdominal obesity, while clustered CMRFs are defined as meeting at least three of these four abnormalities, significantly increasing the likelihood of CVDs (3). Although CMRFs are more common in adults, a substantial body of research indicated that pre-CMRFs and behavioral patterns were formed in childhood and adolescence (4–6), and that adverse levels of clustered CMRFs often coexisted in the same individual (7). Therefore, identifying modifiable factors for clustered CMRFs in children and adolescents is becoming to be recognized as a useful strategy to reduce the lifetime incidence of CVDs.
In the past few decades, China has undergone a remarkable shift in family structure under the implementation of the one-child policy since 1979, which resulted in the birth of more than 100 million families with single children (8). At the same time, the prevalence of cardiovascular and metabolic diseases skyrocketed (9). Based on this, many studies have noted the impact of different family structures on CMRFs, as well as sex differences. Recent studies provided evidence for the association of single children with components of CMRFs such as dyslipidemia (10), abdominal obesity (11), and hypertension (12) in children and adolescents, however, the findings were inconsistent in the direction of the association and sex differences. In addition, only one Iranian study explored the association between single children and all components of CMRFs, and this positive association was mainly manifested in abdominal obesity (13). These evidences suggested that single-child status might play an important role in CMRFs, with varied effects in different sexes. However, so far, studies have focused on the effects of single-child status on the single/multiple components of CMRFs rather than clustered CMRFs.
Furtherly, previous studies found that alcohol intake (14), sedentary behavior (15), insufficient sleep duration (16) and dairy intake (17) all played a significant role in clustered CMRFs. The high prevalence of these behavioral risk factors in childhood and adolescence has been a major concern because they are often maintained to adulthood (18, 19). However, the majority of CVDs can be avoided by addressing behavioral risk factors like tobacco and alcohol consumption, unhealthy diet, obesity, and lack of physical activity (1), which epidemiological studies has validated (20, 21), and so did expect to work for clustered CMRFs.
Although studies have shown that single children are more likely to establish an unfavorable lifestyle (22, 23), little has been known about the interaction of single-child status and lifestyles on clustered CMRFs as well as sex differences. In the real world, it is critical to comprehend the combined impact of disease risk factors, particularly those that coexist or cluster in the same individual, such as CMRFs. In this case, determining the combined impact of its risk factors enables a greater emphasis on controlling modifiable risks and, as a result, better prevention. Therefore, in this study, we hypothesized that there was a combined effect of single children and lifestyles on clustered CMRFs in children and adolescents, and this effect differed by sex. We aimed to investigate the independent and combined effects of two risk factors, single-child status and lifestyles, on clustered CMRFs among children and adolescents aged 7–18 years and the sex differences in these effects using data from a cross-sectional study in China in 2013.
Materials and methods
Study design and participants
Data was collected from a cross-sectional survey conducted in September 2013 with multi-stage cluster random sampling method, involving seven provinces (Liaoning, Ningxia, Tianjin, Shanghai, Hunan, Chongqing, and Guangdong) in China. The specific sampling and implementation methods have been described previously (24). A total of 15,733 children and adolescents aged 7–18 years with blood samples were included. Participants with missing data about anthropometric measurements and failed imputation of missing variables were excluded. The remaining 13,859 children and adolescents were included in the final analysis (Figure 1).

Figure 1. Flow chart of participants’ inclusion. SBP, systolic blood pressure; DBP, diastolic blood pressure; WC, waist circumference; CMRFs, cardio-metabolic risk factors.
Data collection and questionnaire survey
Anthropometric measurements
All anthropometric measurements were carried out by trained investigators using standardized instruments and procedures, which was described in detail in previous study (24). Briefly, children and adolescents needed to wear light clothing and no shoes when having their body height, weight and waist circumference (WC) measured. Height and WC were measured to the nearest 0.1 cm, and weight was measured to the nearest 0.1 kg. Prior to measuring systolic blood pressure (SBP) and diastolic blood pressure (DBP), participants were required to mediate for 5 mins. All indicators were measured twice, with the mean value being used as the final value.
Blood sample collection and detection
After 12 h of fasting, venipuncture was used to draw blood from the veins. Serum was then extracted after centrifugation at 3,000 rpm for 10 min and brought to the testing facility at low temperature (−80°C). A biomedical analysis company with Peking University certification carried out blood biochemical analysis (25). Finally, fasting blood glucose (FBG) and four lipid indicators, including total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C), were collected.
Questionnaire survey
A questionnaire for children and adolescents was used to collect sociodemographic characteristics (age, sex, residence, and school) and lifestyle information such as tobacco and alcohol consumption in the last 30 days, dietary consumption (meat, sugar-sweetened beverage, fruit, and vegetable), physical activity and screen time in the last 7 days, and daily sleep duration. The frequency (day) and amount (servings)/duration (h) were collected for the average daily consumption of each food, as well as daily physical activity and screen time using the following equation: (day × quantity for each day)/7.
A parental questionnaire was used to assess single-child status, which was divided into two categories: single children and non-single children. In addition, a family history of diseases (obesity, hypertension, diabetes, or cerebrovascular disease), parental education, parental tobacco, and alcohol consumption were also gathered.
Definition and categorization of indicators
Clustered cardio-metabolic risk factors
Cardio-metabolic risk factors were defined as hypertension, dyslipidemia, hyperglycemia, and abdominal obesity (26). Hypertension was considered as SBP and/or DBP ≥ the 95th percentile of blood pressure sex- and age-specific group (27). Dyslipidemia was considered as abnormal in any of the following four indicators (28): (I) TC ≥ 5.2 mmol/L; (II) In 0–9 age group, TG ≥ 1.1 mmol/L; In 10–18 age group, TG ≥ 1.5 mmol/L; (III) LDL-C ≥ 3.4 mmol/L; (IV) HDL-C ≤ 1.0 mmol/L. Hyperglycemia was considered as FBG ≥ 5.6 mmol/L (29). Abdominal obesity was considered as WC ≥ the 90th percentile of WC sex- and age-specific group (30). Clustered CMRFs was termed as meeting at least three of the above four items (31).
Ideal lifestyle category
Current smoking, current alcohol, dietary consumption, physical activity, sleep duration, screen time and healthy body mass index (BMI) were included to construct an ideal lifestyle score according to the definition of ideal cardiovascular health from the American Heart Association (32) and the Dietary Guidelines for School-age Children in China (33). Current smoking status was classified as smoking in the past 30 days (Yes/No), and current alcohol consumption was similar to smoking. The optimal dietary composition was defined as ≥3 servings of fruit per day (about 100 g per serving), ≥4 servings of vegetables (about 100 g per serving), 2–3 servings of meat products (about 50 g per serving), and <1 serving of sugar-sweetened beverage per week (about 250 mL per serving) according to the Dietary Guidelines for School-age Children in China (33). A healthy diet was described as the consumption of at least three or more foods in prescribed amounts. Adequate physical activity was characterized as 1 h or more of moderate to vigorous activity per day. The cut-off for sleep duration and screen time were 9 and 2 h, respectively. A healthy BMI was classified as lower than the 85th percentile of BMI for sex- and age-specific group (34). Children and adolescents who met each of the seven specified ideal lifestyles were given one point, and the total scores were 7. The ideal lifestyle scores were further divided into three groups as unfavorable lifestyles (0–3 points), intermediate lifestyles (4 points) and favorable lifestyles (5–7 points).
The combined subgroups
The single-child status was divided into single children and non-single children. Combining the single-child status and ideal lifestyle category, they can be further divided into six groups, namely the single children and favorable lifestyles, single children and intermediate lifestyles, single children and unfavorable lifestyles, non-single children and favorable lifestyles, non-single children and intermediate lifestyles, and non-single children and unfavorable lifestyles.
Covariates
In this study, age, residence, family history of diseases, parental education, parental tobacco, and alcohol consumption were considered as context covariates. A family history of the disease was considered a history of obesity, hypertension, diabetes or cerebrovascular disease in either parent. Parental education level was recorded by the highest educational level of the parents and divided into primary or below, secondary or equivalent and junior college or above. Parental tobacco consumption (Yes/No) was defined as smoking by either parent and parental alcohol consumption (Yes/No) was similar.
Statistics analysis
Hot-deck Imputation method was used for missing variables (e.g., lifestyle information), and background variables were set as school, grade, urban and rural area, and sex. The quantitative variables were described by median (interquartile spacing), and group differences were tested by Mann-Whitney U test according to the normality of distribution. Qualitative variables were described by frequency (percentage) and group differences were tested by Chi-square test. Mixed effect logistic regression was applied to analyze the independent and the combined effects of single-child status and ideal lifestyle category on clustered CMRFs. Only the random effect of schools was adjusted for all crude models. The fixed effect of covariates and the random effect of schools were adjusted in all adjusted models. We also constructed sex interaction terms and conducted stratified analysis to explore sex differences between these association. All analyses were performed in SPSS 26.0 and GraphPad Prism 9. A two-tailed P value < 0.05 was considered statistically significant.
We also analyzed the independent and combined effects of single-child status and ideal lifestyle category on components of CMRFs, including hyperglycemia, hypertension, dyslipidemia, and abdominal obesity as a supplementary result.
Results
Characteristics of participants
The characteristics of participants and their parents were showed in Table 1 and Supplementary Table 1. Overall, the prevalence of clustered CMRFs was 3.4%, with a higher prevalence in boys (4.0%) than girls (2.7%). Children and adolescents with clustered CMRFs had a higher proportion of single children (76.6 vs. 69.7%) and unfavorable lifestyles (62.1 vs. 29.2%) compared with their peers with non-clustered CMRFs. Children and adolescents with clustered CMRFs were more likely than those without clustered CMRFs to be male (61.1 vs. 50.8%), rural (50.2 vs. 41.1%), have a family history of diseases (18.9 vs. 12.5%), and have parents with lower proportion of high education level (24.9 vs. 30.3% for junior college or above).
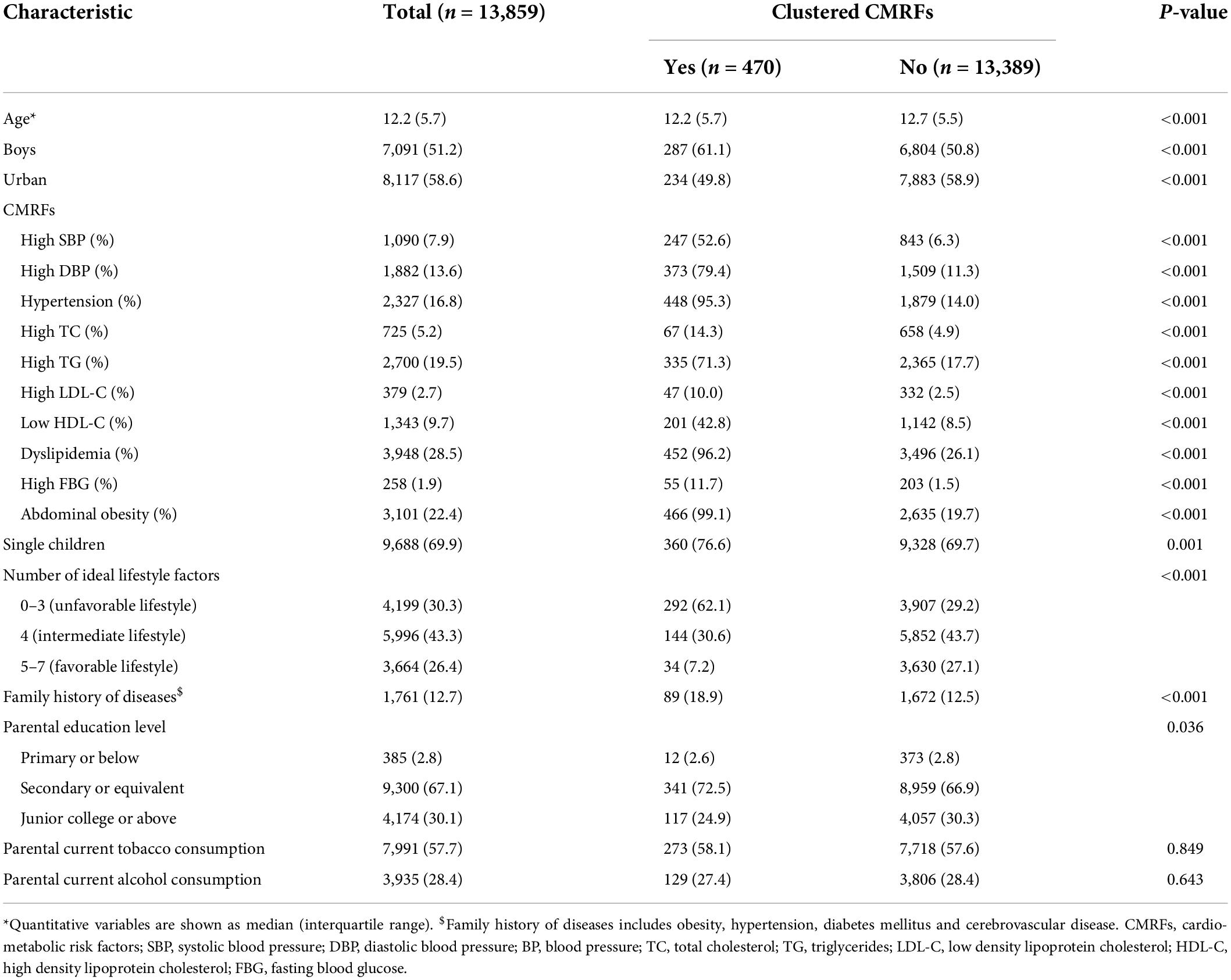
Table 1. Demographic characteristics of eligible children and adolescents and their parents, stratified by clustered cardio-metabolic risk factors (CMRFs).
Children who were included in the final sample (n = 13,859) were more likely than those in the primary sample (n = 15,733) to be rural (41.4 vs. 38.2%). There were no statistically significant differences in age group and sex between the primary sample and the final sample (Supplementary Table 2).
The independent effects of single-child status and lifestyle category on clustered cardio-metabolic risk factors
As presented in Figure 2, single children had a higher risk of CMRFs (adjusted model: OR = 1.67, 95% CI: 1.32–2.11) than non-single children in both crude and adjusted models. Although the sex interaction was not statistically significant, we stratified it by sex and found that this effect remained statistically significant for both boys (OR = 1.59, 95% CI: 1.16–2.20) and girls (OR = 1.48, 95% CI: 1.04–2.12). In the total population, participants engaged in intermediate (OR = 2.81, 95% CI: 1.92–4.12) and unfavorable lifestyles (OR = 9.03, 95% CI: 6.26–13.02) had a higher risk of clustered CMRFs compared to favorable lifestyles after adjusting for covariates (Figure 3). When stratified by sex, slightly higher OR values were observed in the unfavorable lifestyle group of boys (boys: OR = 9.42, 95% CI: 5.80–15.33 vs. girls: OR = 8.92, 95% CI: 5.08–15.67), although the difference was not statistically significant. The independent effects of single-child status and ideal lifestyle category on components of CMRFs have been shown in Supplementary Tables 3, 4.
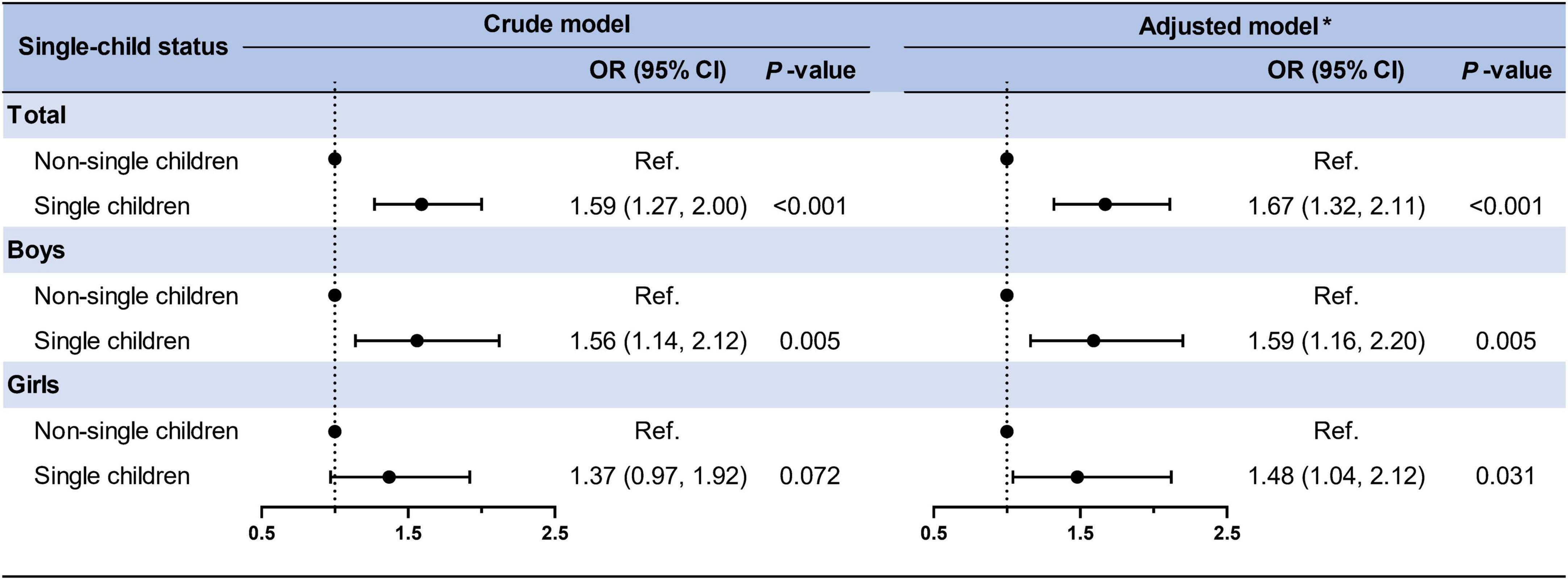
Figure 2. Association between single-child status and clustered CMRFs in children and adolescents. *Adjusted for age, residence, family history of diseases (obesity, hypertension, diabetes mellitus, and cerebrovascular disease), parental education level, parental tobacco, and alcohol consumption and the clustered effect of schools.
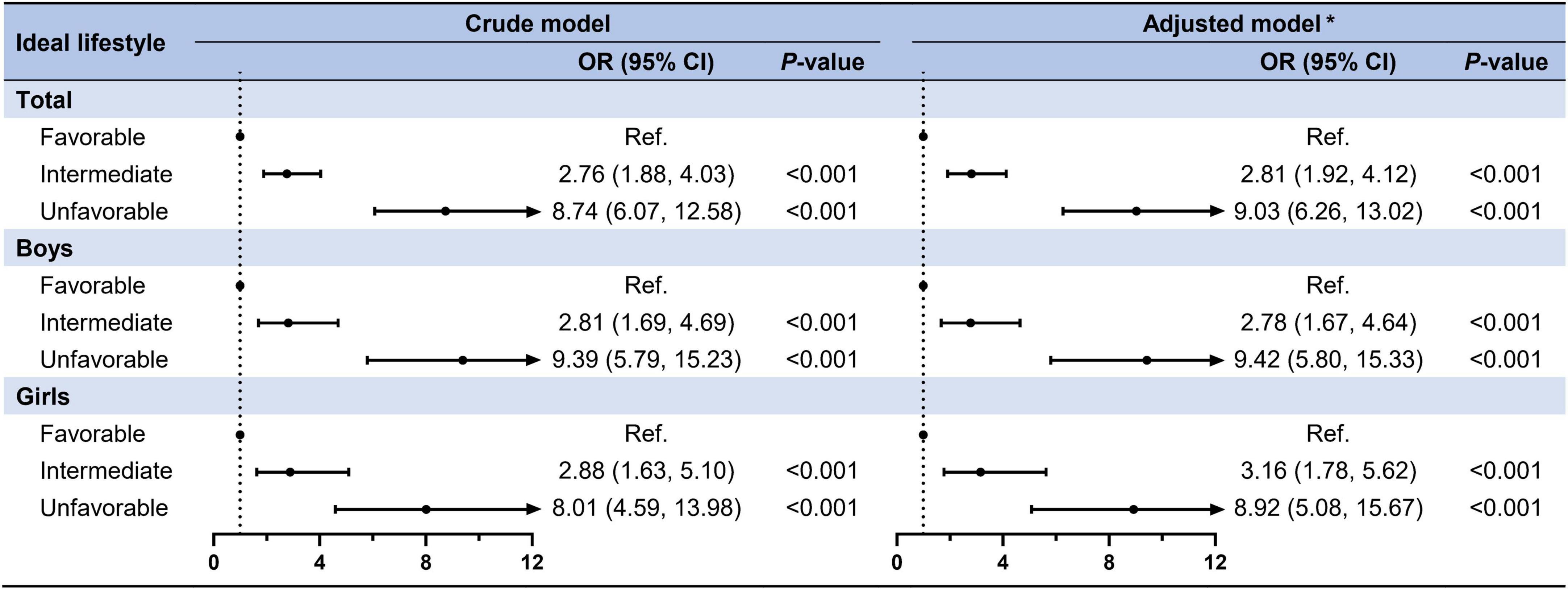
Figure 3. Association between ideal lifestyle factors and clustered CMRFs in children and adolescents. *Adjusted for age, residence, family history of diseases (obesity, hypertension, diabetes mellitus, and cerebrovascular disease), parental education level, parental tobacco, and alcohol consumption and the clustered effect of schools.
The combined effect of single-child status and lifestyle category on clustered cardio-metabolic risk factors
As shown in Figure 4, a stronger combined effect of single children and ideal lifestyle category was found in clustered CMRFs. Compared to children and adolescents in the non-single children and favorable lifestyle group, an extremely high risk of clustered CMRFs was observed among those in the non-single children and unfavorable lifestyle group (OR = 7.60, 95% CI: 3.85–14.96) and single children and unfavorable lifestyle group (OR = 12.79, 95% CI: 6.67–24.52). No statistical significance was found in the single children and favorable lifestyle group (OR = 1.33, 95% CI: 0.63–2.82). When stratified by sex, these relationships remained consistent with the total population but with no statistical difference between boys and girls in the OR values of each subgroup. Supplementary Table 5 shows the combined effect of single-child status and ideal lifestyle category on components of CMRFs. In addition to high FBG, the combined effect of single children and ideal lifestyle category was statistically significant for hypertension, dyslipidemia and abdominal obesity, with the largest OR for abdominal obesity.
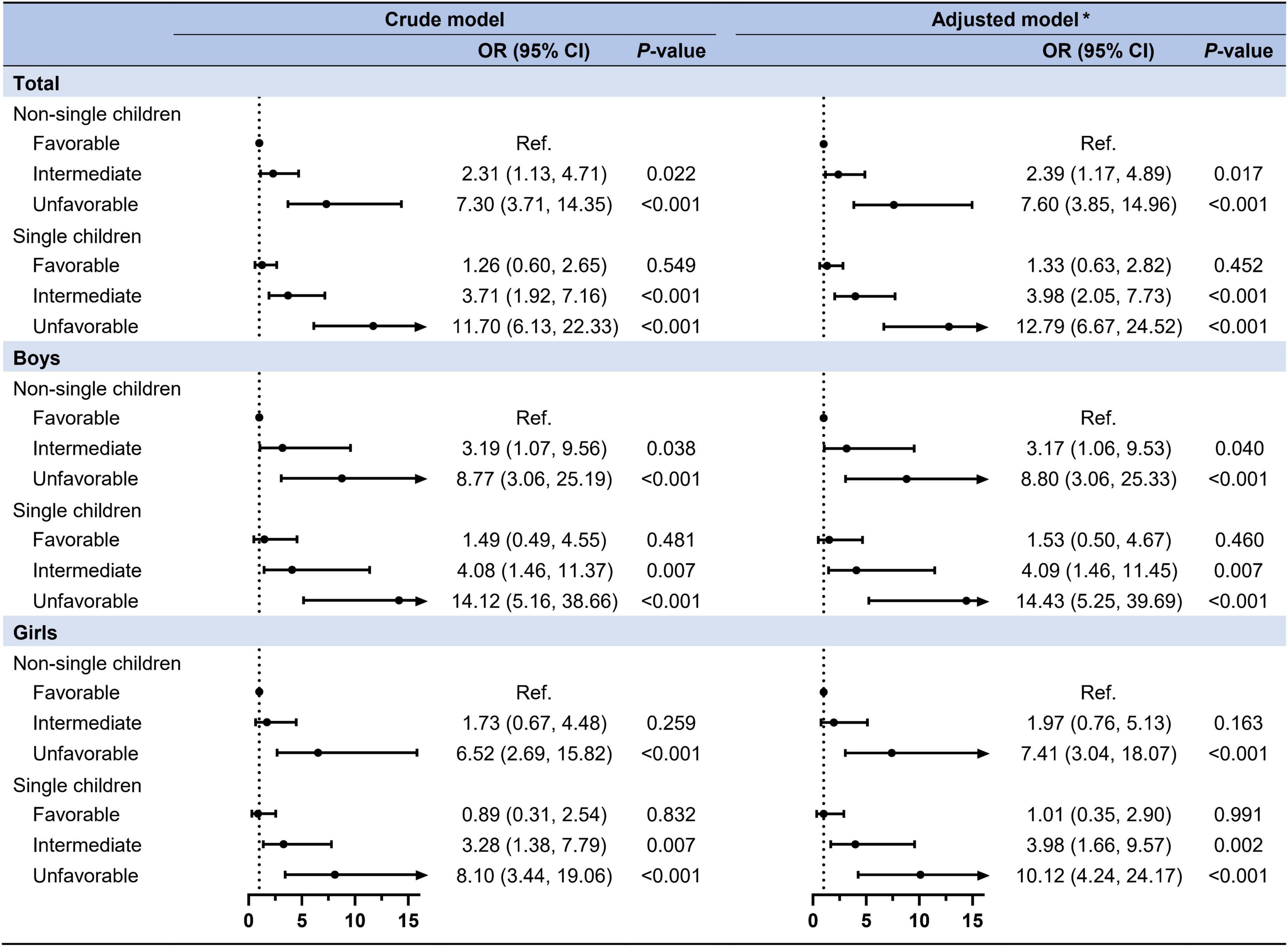
Figure 4. The combined effect of single-child status and ideal lifestyle on clustered CMRFs. *Adjusted for age, residence, family history of diseases (obesity, hypertension, diabetes mellitus, and cerebrovascular disease), parental education level, parental tobacco, and alcohol consumption and the clustered effect of schools.
Discussion
To the best of our knowledge, this study is the first to evaluate the combined effect of single children and lifestyle category on clustered CMRFs. According to the findings of this study, both single children and unfavorable lifestyles were associated with an increased risk of clustered CMRFs. The risk of clustered CMRFs increased significantly when single children and an unfavorable lifestyle were combined, which was almost neutralized when single children adhered to a favorable lifestyle. However, no sex difference was observed in this study.
The associations between the single children and an increased risk of elevated blood pressure (35), dyslipidemia (10), hypertension (13), abdominal obesity (11, 35), overweight and obesity (36, 37) were confirmed in China and European countries. However, one study found the opposite results that children with siblings were associated with a higher risk of hypertension (12), which the authors believed was likely attributed to adjustments for BMI or obesity status. The results of existing studies on lifestyles on CMRFs were more consistent, finding that an unfavorable lifestyle increased the risk of CMRFs or CVDs (38–40). Moreover, a meta-analysis showed that for each increase in ideal cardiovascular health as defined by the American Heart Association, cardiovascular mortality decreased by 19% (41). This present study added to the evidence that further emphasized the importance of adhering to a favorable lifestyle. No sex differences were found in this study, most likely due to the low prevalence of clustered CMRFs (3.4%) and, as a result, the relatively small number of children in each subgroup when stratified by sex, but indicated that intervention developed from single-child status or lifestyle perspectives or both would work for both sexes under such level of CMRFs.
Previous studies have identified an association between single-child families and components of CMRFs, however, the underlying mechanisms remain unknown. Even though the resource dilution theory (42, 43) contended that single children received more resources and care than children with siblings, the current nutritional and social environment may encourage the adoption of unhealthy lifestyles, which in turn resulted in metabolic abnormalities. Notably, this study discovered that when single children maintained a healthy lifestyle, the negative effect of single children on clustered CMRFs appeared to be offset, implying that the mechanism of health risks caused by single children was most likely due to their tendency to unfavorable lifestyles, such as fast food over intake (22), sugar excessive consumption (36), and physical inactivity (23). Based on the available evidence, the risks of being a single child might be mitigated by diluting the allocation of resources by expanding the family. On the other hand, children and adolescents should be encouraged to cultivate and maintain a healthy lifestyle, whether from single child or non-single child families.
To cope with the challenge of aging issue, the Chinese government ended one-child policy with the two-child policy in Zeng and Hesketh (44), and opened up the three-child policy in Jing et al. (45). However, the increasingly open policy has not improved China’s low fertility rate as expected (46, 47). According to the China Women’s Federation, the intention rate of parents to have a second child was 20.5% in 2017 (48), significantly lower than the 61.25% recorded under the one-child policy (49). Single children made up a large proportion of all structural families in an international environment of high income and low fertility (50). The level of delaying childbearing has been increasing, especially with the emergence of the second demographic transition (51), which suggested that this proportion was likely to increase in the future, and the resulting health problems should not be ignored. This study highlighted the need for the government and society to increase support for the birth of second and third children, such as reducing the financial burden and relieving the pressure of childrearing, and increasing couples’ free time. The findings of this study provided new evidence that single children with unfavorable lifestyles might be an important target group for future clustered CMRFs interventions, and it was necessary to strengthen the establishment of a friendly birth environment and health education at the family level to guide children toward a favorable lifestyle.
There were several limitations to the study. Firstly, this was a cross-sectional study with limited causal inference. Secondly, the lifestyle information of children and adolescents was entirely based on a questionnaire survey, which had a certain recall bias. Thirdly, although the method of imputation was used for missing variables, 12% of the samples were still excluded in this study, and thus there may be some selection bias in the final analyzed samples. However, when the background variables of the initial and final samples were compared, only urban and rural differences were discovered in this study. Fourthly, although some confounding factors were adjusted in this study, there was still residual confounding. Lastly, adding BMI as a scoring indicator in the definition of a healthy lifestyle may improve the correlation of lifestyle with clustered CMRFs, especially since abdominal obesity was included as a component of CMRFs in this study.
Conclusion
Single children with unfavorable lifestyles were associated with an obvious risk of clustered CMRFs, which might be partially offset by expanding family size (the number of siblings) or establishing a favorable lifestyle. A birth-friendly social environment as well as a family environment with a favorable lifestyle are encouraged in China.
Data availability statement
The data supporting the conclusions of this article can be made available from the corresponding author upon request.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking University (NO.IRB0000105213034). Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
YD, ZZ, YM, YS, and JM conducted data collection and data management. JD and YS conducted manuscript design. JD, NM, and YL conducted statistical analysis. JD, NM, YL, PZ, DS, SC, YD, ZZ, and YM wrote and finalized the manuscript. YS and JM reviewed and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This research was supported by funding from the Natural Science Foundation of Beijing (Grant No. 7222247 to YS).
Acknowledgments
The authors gratefully acknowledge all the schoolteachers and doctors for their assistance in data collection and all students and their guardians for participating in the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.987334/full#supplementary-material
References
2. Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, et al. Cause-specific mortality for 240 causes in China during 1990-2013: A systematic subnational analysis for the global burden of disease study 2013. Lancet. (2016) 387:251–72. doi: 10.1016/S0140-6736(15)00551-6
3. Griffin BA. Optimal diet and lifestyle strategies for the management of cardio-metabolic risk. Proc Nutr Soc. (2020) 79:1–3. doi: 10.1017/S0029665119001149
4. Martin-Diener E, Meyer J, Braun J, Tarnutzer S, Faeh D, Rohrmann S, et al. The combined effect on survival of four main behavioural risk factors for non-communicable diseases. Prev Med. (2014) 65:148–52. doi: 10.1016/j.ypmed.2014.05.023
5. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/S0140-6736(12)61766-8
6. Ford ES, Bergmann MM, Boeing H, Li C, Capewell S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med. (2012) 55:23–7. doi: 10.1016/j.ypmed.2012.04.016
7. Chen W, Srinivasan SR, Li S, Xu J, Berenson GS. Clustering of long-term trends in metabolic syndrome variables from childhood to adulthood in blacks and whites: The Bogalusa heart study. Am J Epidemiol. (2007) 166:527–33. doi: 10.1093/aje/kwm105
9. Motlagh ME, Ziaodini H, Qorbani M, Taheri M, Aminaei T, Goodarzi A, et al. Methodology and early findings of the fifth survey of childhood and adolescence surveillance and prevention of adult noncommunicable disease: The CASPIAN-V study. Int J Prev Med. (2017) 8:4. doi: 10.4103/2008-7802.198915
10. Cai L, Ma B, Lin L, Chen Y, Yang W, Ma J, et al. The differences of lipid profiles between only children and children with siblings: A national survey in China. Sci Rep. (2019) 9:1441. doi: 10.1038/s41598-018-37695-0
11. Gao D, Li Y, Yang Z, Ma Y, Chen M, Dong Y, et al. The association between single-child status and risk of abdominal obesity: Result from a cross-sectional study of China. Front Pediatr. (2021) 9:697047. doi: 10.3389/fped.2021.697047
12. Deng R, Lou K, Zhou S, Li X, Zou Z, Ma J, et al. Exploring the associations between single-child status and childhood high blood pressure and the mediation effect of lifestyle behaviors. Nutrients. (2022) 14:500. doi: 10.3390/nu14030500
13. Kelishadi R, Qorbani M, Rezaei F, Motlagh ME, Djalalinia S, Ziaodini H, et al. Is single-child family associated with cardio-metabolic risk factors: The CASPIAN-V study. BMC Cardiovasc Disord. (2018) 18:109. doi: 10.1186/s12872-018-0844-y
14. Du D, Bruno R, Dwyer T, Venn A, Gall S. Associations between alcohol consumption and cardio-metabolic risk factors in young adults. Eur J Prev Cardiol. (2017) 24:1967–78. doi: 10.1177/2047487317724008
15. Healy GN, Winkler EA, Owen N, Anuradha S, Dunstan DW. Replacing sitting time with standing or stepping: Associations with cardio-metabolic risk biomarkers. Eur Heart J. (2015) 36:2643–9. doi: 10.1093/eurheartj/ehv308
16. Yiallourou SR, Carrington MJ. Improved sleep efficiency is associated with reduced cardio-metabolic risk: Findings from the MODERN trial. J Sleep Res. (2021) 30:e13389. doi: 10.1111/jsr.13389
17. Johansson I, Nilsson LM, Esberg A, Jansson JH, Winkvist A. Dairy intake revisited – Associations between dairy intake and lifestyle related cardio-metabolic risk factors in a high milk consuming population. Nutr J. (2018) 17:110. doi: 10.1186/s12937-018-0418-y
18. Craigie AM, Lake AA, Kelly SA, Adamson AJ, Mathers JC. Tracking of obesity-related behaviours from childhood to adulthood: A systematic review. Maturitas. (2011) 70:266–84. doi: 10.1016/j.maturitas.2011.08.005
19. Back IC, Barros NF, Caramelli B. Lifestyle, inadequate environments in childhood and their effects on adult cardiovascular health. J Pediatria. (2022) 98(Suppl. 1):S19–26. doi: 10.1016/j.jped.2021.09.005
20. Chomistek AK, Chiuve SE, Eliassen AH, Mukamal KJ, Willett WC, Rimm EB. Healthy lifestyle in the primordial prevention of cardiovascular disease among young women. J Am Coll Cardiol. (2015) 65:43–51. doi: 10.1016/j.jacc.2014.10.024
21. Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, et al. Impact of healthy lifestyle factors on life expectancies in the US population. Circulation. (2018) 138:345–55. doi: 10.1161/CIRCULATIONAHA.117.032047
22. Jing J. Feeding China’s little emperors: Food, children, and social change. 46. Chicago, IL: The University of Chicago Press (2001). doi: 10.2307/2659515
23. Li M, Xue H, Wang W, Wen M, Wang Y. Increased obesity risks for being an only child in China: Findings from a nationally representative study of 19,487 children. Public Health. (2017) 153:44–51. doi: 10.1016/j.puhe.2017.07.002
24. Dang J, Chen T, Ma N, Liu Y, Zhong P, Shi D, et al. Associations between breastfeeding duration and obesity phenotypes and the offsetting effect of a healthy lifestyle. Nutrients. (2022) 14:1999. doi: 10.3390/nu14101999
25. Chen Y, Ma L, Ma Y, Wang H, Luo J, Zhang X, et al. A national school-based health lifestyles interventions among Chinese children and adolescents against obesity: Rationale, design and methodology of a randomized controlled trial in China. BMC Public Health. (2015) 15:210. doi: 10.1186/s12889-015-1516-9
26. Dou Y, Jiang Y, Yan Y, Chen H, Zhang Y, Chen X, et al. Waist-to-height ratio as a screening tool for cardiometabolic risk in children and adolescents: A nationwide cross-sectional study in China. BMJ Open. (2020) 10:e037040. doi: 10.1136/bmjopen-2020-037040
27. Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. (2017) 140:e20171904. doi: 10.1542/peds.2017-1904
28. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics. (2011) 128(Suppl. 5):S213–56. doi: 10.1542/peds.2009-2107C
29. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. (2014) 37(Suppl. 1):S81–90. doi: 10.2337/dc14-S081
30. National Health Commission of the People’s Republic of China. High waist circumference screening threshold among children and adolescents aged 7 18 years. Beijing: National Health Commission of the People’s Republic of China (2018).
31. Chen R, Ji L, Chen Y, Meng L. Weight-to-height ratio and body roundness index are superior indicators to assess cardio-metabolic risks in Chinese children and adolescents: Compared with body mass index and a body shape index. Transl Pediatr. (2022) 11:318–29. doi: 10.21037/tp-21-479
32. Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American heart association’s strategic impact goal through 2020 and beyond. Circulation. (2010) 121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703
33. Chinese Nutrition Society. Dietary guidelines for school age children in China. Beijing: People’s Health Publishing House (2022).
34. National Health Commission of the People’s Republic of China. Screening for overweight and obesity among school-age children and adolescents. Beijing: National Health Commission of the People’s Republic of China (2018).
35. Chen M, Li Y, Chen L, Gao D, Yang Z, Ma Y, et al. Associations between single-child status and metabolic syndrome in children and adolescents in China. Front Pediatr. (2021) 9:661164. doi: 10.3389/fped.2021.661164
36. Hunsberger M, Formisano A, Reisch LA, Bammann K, Moreno L, De Henauw S, et al. Overweight in singletons compared to children with siblings: The IDEFICS study. Nutr Diabetes. (2012) 2:e56. doi: 10.1038/nutd.2012.28
37. Min J, Xue H, Wang VHC, Li M, Wang Y. Are single children more likely to be overweight or obese than those with siblings? The influence of China’s one-child policy on childhood obesity. Prev Med. (2017) 103:8–13. doi: 10.1016/j.ypmed.2017.07.018
38. Mechanick JI, Zhao S, Garvey WT. The adipokine-cardiovascular-lifestyle network: Translation to clinical practice. J Am Coll Cardiol. (2016) 68:1785–803. doi: 10.1016/j.jacc.2016.06.072
39. Patterson KAE, Ferrar K, Gall SL, Venn AJ, Blizzard L, Dwyer T, et al. Cluster patterns of behavioural risk factors among children: Longitudinal associations with adult cardio-metabolic risk factors. Prev Med. (2020) 130:105861. doi: 10.1016/j.ypmed.2019.105861
40. Guasch-Ferré M, Li Y, Bhupathiraju SN, Huang T, Drouin-Chartier JP, Manson JE, et al. Healthy lifestyle score including sleep duration and cardiovascular disease risk. Am J Prev Med. (2022) 63:33–42. doi: 10.1016/j.amepre.2022.01.027
41. Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: A meta-analysis of prospective studies. Clin Cardiol. (2017) 40:1339–46. doi: 10.1002/clc.22836
42. Blake J. Family size and the quality of children. Demography. (1981) 18:421–42. doi: 10.2307/2060941
43. Downey DB. Number of siblings and intellectual development. The resource dilution explanation. Am Psychol. (2001) 56:497–504. doi: 10.1037//0003-066X.56.6-7.497
44. Zeng Y, Hesketh T. The effects of China’s universal two-child policy. Lancet. (2016) 388:1930–8. doi: 10.1016/S0140-6736(16)31405-2
45. Jing W, Liu J, Ma Q, Zhang S, Li Y, Liu M. Fertility intentions to have a second or third child under China’s three-child policy: A national cross-sectional study. Hum Reprod. (2022) 37:1907–18. doi: 10.1093/humrep/deac101
46. Li M, Xu X. Fertility Intentions for a second child and their influencing factors in contemporary China. Front Psychol. (2022) 13:883317. doi: 10.3389/fpsyg.2022.883317
47. Zhu C, Yan L, Wang Y, Ji S, Zhang Y, Zhang J. Fertility intention and related factors for having a second or third child among childbearing couples in Shanghai, China. Front Public Health. (2022) 10:879672. doi: 10.3389/fpubh.2022.879672
48. China Women’s Federation. Two-child policy’s impact on family education. Beijing: China Women’s Federation (2017).
49. Zheng Y, Yuan J, Xu T, Chen M, Liang H, Connor D, et al. Socioeconomic status and fertility intentions among Chinese women with one child. Hum Fertil. (2016) 19:43–7. doi: 10.3109/14647273.2016.1154988
50. Präg P, Choi S, Monden C. The sibsize revolution in an international context: Declining social disparities in the number of siblings in 26 countries. Demogr Res. (2020) 43:461–500. doi: 10.4054/DemRes.2020.43.17
Keywords: single-child, ideal lifestyle, clustered CMRFs, children, adolescents
Citation: Dang J, Ma N, Liu Y, Zhong P, Shi D, Cai S, Dong Y, Zou Z, Ma Y, Song Y and Ma J (2022) The independent and combined effects of single-child status and ideal lifestyle on clustered cardio-metabolic risk factors among Chinese children and adolescents. Front. Nutr. 9:987334. doi: 10.3389/fnut.2022.987334
Received: 06 July 2022; Accepted: 01 August 2022;
Published: 29 August 2022.
Edited by:
Yong Zhao, Chongqing Medical University, ChinaReviewed by:
Mingzhi Zhang, Soochow University, ChinaLinghui Meng, Independent Researcher, Beijing, China
Copyright © 2022 Dang, Ma, Liu, Zhong, Shi, Cai, Dong, Zou, Ma, Song and Ma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yi Song, c29uZ3lpQGJqbXUuZWR1LmNu; Jun Ma, bWFqdW50QGJqbXUuZWR1LmNu
 Jiajia Dang
Jiajia Dang Ning Ma
Ning Ma Yunfei Liu
Yunfei Liu Panliang Zhong
Panliang Zhong Di Shi1,2
Di Shi1,2 Shan Cai
Shan Cai Yanhui Dong
Yanhui Dong Zhiyong Zou
Zhiyong Zou Yi Song
Yi Song Jun Ma
Jun Ma