- 1Department of Nutrition and Dietetics, Jimma University, Jimma, Ethiopia
- 2Department of Pediatrics and Child Health, Jimma University, Jimma, Ethiopia
Background: Undernutrition is an insufficient intake of energy and nutrients to meet an individual's needs to maintain good health. Undernutrition during pregnancy severely affects the health of mothers and her baby. Globally it contributes directly or indirectly to 3.5 million maternal deaths annually. This study aimed to determine the level of undernutrition and identify factors associated with undernutrition among pregnant women attending public health facilities in the East Shoa Zone, Central Ethiopia.
Methods: Institution-based cross-sectional study was conducted among 472 randomly selected pregnant women from June to August 2021. Sociodemographic, obstetrics, and knowledge related data were collected using a structured interviewer-administered questionnaire, and maternal nutritional status was measured using the Mid Upper Arm Circumference (MUAC). The collected data were entered to EPI-info version 3.5.4 and then exported to SPSS for windows version 26.0 software for analysis. Multivariable regression analysis was fitted to identify determinants of undernutrition. An adjusted odds ratio with 95% confidence intervals and a p-value < 0.05 was considered a statistically significant.
Results: The prevalence of undernutrition among pregnant women was 13.9% [95% CI: 11.0–17.4]. On multivariable logistic regression model after adjusting background variables, wealth (AOR: 4.9, 95% CI 1.34–18.20), women's decision making power (AOR: 3.31, 95% CI 1.18–7.79), and nutritional counseling (AOR: 3.53, 95% CI 1.29–9.60) were independently associated with nutritional status of pregnant women.
Conclusion: Findings indicated that significant number of pregnant women in the study were undernourished. Higher wealth index, nutritional counseling, and women's decision-making power were inversely associated with undernutrition. The findings imply the need for economic empowerment of women, enhancing decision-making ability of women and routine and consistent nutritional counseling to decrease undernutrition among pregnant women.
Introduction
The first 1,000 days (the period from conception through the first 2 years after birth) is a critical period for the future growth and development of a child (1). Pregnant women should get optimum nutrients for good perinatal outcomes. Taking the right balance of micronutrients at an early stage of pregnancy prevents complications due to malnutrition (2, 3). Undernutrition, energy and nutrients intake insufficient to maintain good health (4), contributes to 3.5 million global maternal deaths annually (5). It remains a significant public health problem in Africa, especially in sub-Sahara countries (6).
Undernutrition during pregnancy severely affects physical and mental health of children. There is a 64 percent probability that women delivering a low birth weight (LBW) infant would have a lower MUAC level than those delivering a normal birthweight infant (7). A systematic review conducted by Han et al. revealed that women with undernutrition had more than 60% increased risk of giving birth to LBW babies (8).
Pregnant women's knowledge about nutrition during pregnancy is a critical nexus in good pregnancy outcomes and improving children's nutritional status (9). Nutritional knowledge and attitude are essential for good dietary practices and are, thus, potential targets for appropriate planning of nutrition interventions for vulnerable population groups like pregnant and lactating women (10–12).
In Ethiopia, undernutrition among pregnant women ranges from 21.8 to 43.1%, with a higher prevalence among rural women (13, 14). Factors that are associated with maternal undernutrition include young age, low educational attainment, low socio-economic status, large family size, low income, poor women's decision-making power, household food insecurity, low nutrition knowledge, residence, dietary diversity, absence of latrine, and unintended pregnancy (13–16).
Risk factors for undernutrition vary by context due to differences in socioeconomic characteristics, culture, ethnicity, and geographical location. The magnitude of undernutrition and associated factors among pregnant women in East Shoa zone are not known. Therefore, this study aimed to determine the level of undernutrition and identify factors associated with undernutrition among pregnant women attending public health facilities in the East Shoa zone, Oromia Region, Ethiopia.
Methods and materials
Study area and period
According to the East Shoa zone health office, the health service delivery is organized under 3 hospitals, 59 health centers, and 290 health posts. All the facilities are expected to provide maternal and neonatal health care services based on the National Essential Health Services Packages (EHSP) for different levels of health care. According to the zonal report of 2020, the facilities in the zone provided antenatal care service (ANC) for more than 54,408 pregnant women. The food production system in the district is characterized by mixed crop-livestock farming, with predominant crop production. The community is also known for cultivating different fruits and vegetables, which are considered cash crops. Teff is the principal crop produced in the area. This study was conducted from June to August 2021.
Study design and population
Institution-based cross-sectional study design was used. All pregnant women who came for ANC service at selected health institutions in Eastern Shoa Zone during the study period were considered the study population.
Inclusion and exclusion criteria
Pregnant women living in Eastern Shoa Zone and attending ANC service at the selected health center during the study period were given a chance to be included in the study. Severely sick women were not eligible.
Sample size and sampling procedure
The sample size was calculated by using OpenEpi version 3.01 software (OpenSource.org/licenses). The minimum sample size was calculated using a single population proportion formula. Assuming standard error corresponding to a 95% confidence level (Z) = 1.96, the proportion of undernourished pregnant women from the previous study (p = 19.1), (17), margin of error (d) = 5% and design effect 2, the estimated sample size was 475. Multistage stratified sampling techniques was used to select study participants. Of a total of health centers in the east Shoa zone, six health centers from urban and eight health centers were included from rural kebele by using the lottery method. The total sample size was allocated to each health center based on the number of women who visited the health center in the preceding year in the same month. Finally, a systematic random sampling technique was used to select participants by following the Kth value. The Kth value was calculated by taking the total number of pregnant women on ANC during the study period and dividing it by the sample size, and it was found to be three. Then, lottery methods was used to choose the first case within the interval, which turned out to be 1.The first comer was considered as the first participants, and participants who came at the third interval were interviewed until the determined sample size was achieved.
Measurement and data collection procedure
A structured and pretested questionnaire was used to collect information on sociodemographic and obstetrics characteristics, women autonomy, Household Food Insecurity Access Scale (HHFIAS), and knowledge of women. The data collectors were trained nurses and midwives recruited for this study. Participants were invited to the survey when they came to receive ANC service at the selected health institution. All the participants completed the survey questions.
Mid upper arm circumference of pregnant women was measured by using inelastic MUAC tape. The midpoint of the left upper arm was located by flexing the women's elbows to 900 with the palm facing upwards and the midpoint between acromion to olecranon processes was marked. After this, measuring tape was placed around the arm at the midpoint. Two measurements was taken and reported to the nearest 0.1 cm. Women with MUAC < 22 cm were considered undernourished, and ≥ 22 cm were considered well-nourished (7). The household food security status in the past 4 weeks before data collection was assessed by using the Food Insecurity Access Scale (HFIAS) measurement tool. The score was calculated for each household by summing up the nine food insecurity-related conditions' frequency of occurrence. A household that obtained < 2 scores were considered food secured and those that obtained ≥ 2 scores were considered food insecure (18). Women's decision-making power was assessed using six questions adapted from previous literature (19). For each question, three options were presented, and one score was given when a decision was made by the woman alone or jointly with her husband, or zero was given if the decision did not involve women. Gravidity is number of times that a women get pregnant. Parity is the number of times that a woman had given birth to a fetus with a gestational age of 24 weeks or more, regardless of the child was born alive or was stillbirth.
A total of 16 questions focusing on nutrition knowledge were presented to participants of this study. For knowledge questions, respondents with an average score greater than or equal to mean score were categorized as having adequate knowledge about nutrition during pregnancy and respondents with average score less than mean value were classified as having inadequate knowledge (20).
Data quality assurance
To ensure the quality of the data, local languages were used for understanding of the questions. In addition, pre-test of research instruments and thorough training of data collectors and supervisors were done before the actual data collection. The supervisors provided on-site support to data collectors daily. All completed questionnaires were collected by respective supervisors and checked overnight to ensure completeness and consistencies. Regular meetings were held to provide feedback on issues of concern identified from data collected the next day.
Data processing and analysis
The data were entered to EPI-info version 3.5.4 and then exported to SPSS version 26.0 software for analysis. Binary logistic regression was used to check the association between explanotory variables and undernutrition. All variables with a p-value < 0.25 in bivariate analyses remained in the model as potential confounders for multivariable analysis. Hosmer and Lemeshow's goodness-of-fit test was performed to assess whether the required assumption was fulfilled, and variance inflation factors were checked to assess for multi-collinearity. The strength of association was expressed as adjusted odds ratio with 95% confidence intervals. A p-value < 0.05 was considered a statistically significant association with undernutrition. Multicolliniarity was checked using standard error of >2.
Results
Characteristics of respondents
Of 475 participants approached, 472 (99.4%) responded. The mean age of the respondents was 25.8 (SD ± 4.6) years, 465(98.5%) were married, 235(49.8%) Orthodox Christians, and 296 (62.7%) from Oromo ethnic group (Table 1). One-fourth, 119 (25.2%) of the respondents were unable to read and write, followed by those who attended primary education 117(24.8%) (Table 1).
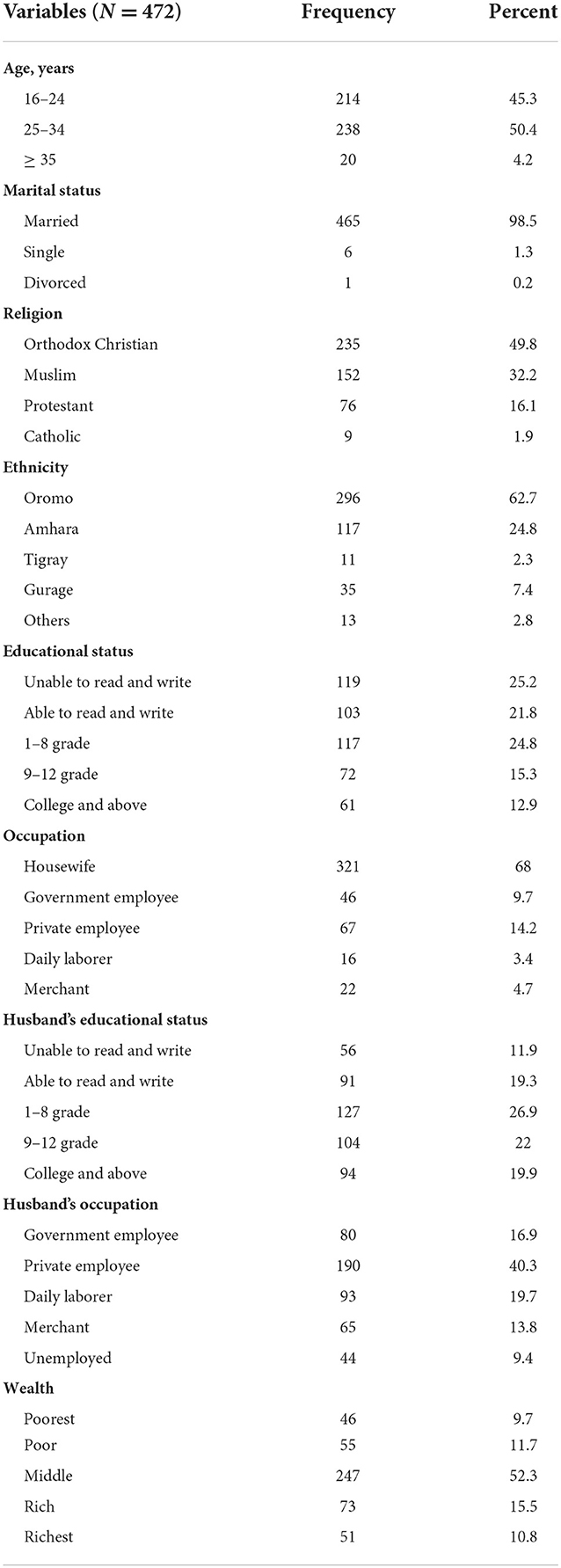
Table 1. Socio-demographic characteristics of pregnant women attending ANC service in East Shoa zone, Ethiopia, from June to August 2021.
More than two-thirds of respondents' maximum gravidity was two, and 80% gave birth once or twice. For the current pregnancy, 224(47.5) were in the third trimester, 431(91.3%) was planned and 207(84.8%) have nutritional counseling during their ANC follow-up. Of the respondents, 246 (52.1) took 21–30 iron-folate pills in the preceding 1 month, and the primary reason for missing the pills was forgetfulness 144 (30.5%) (Table 2).
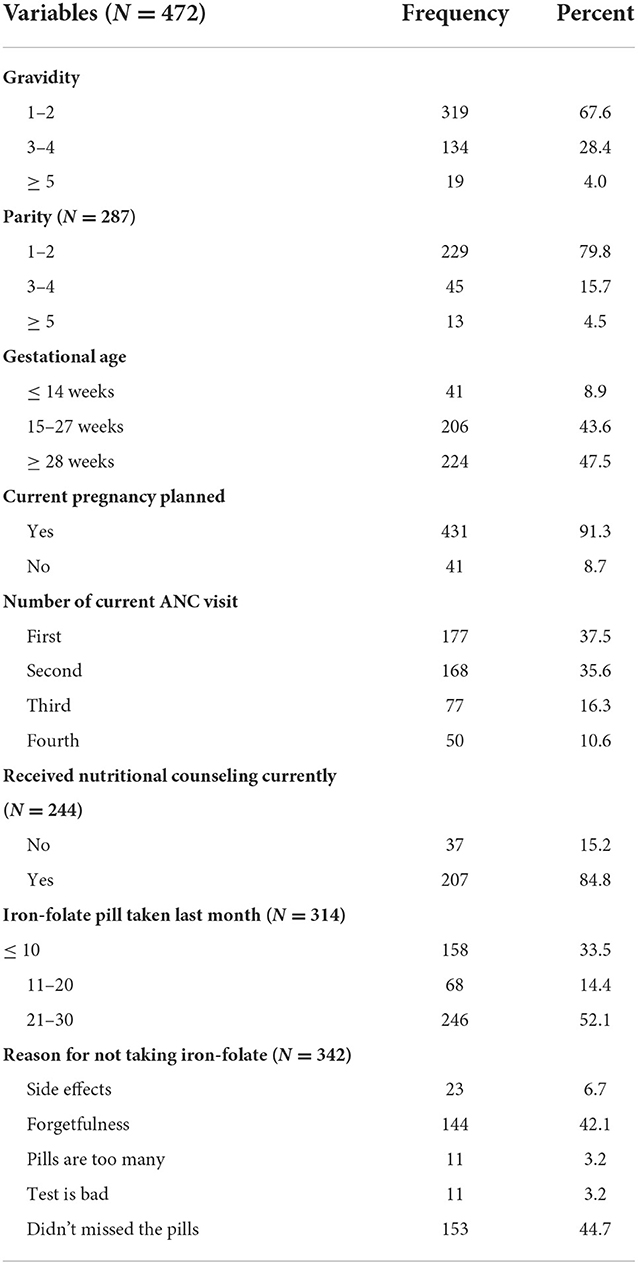
Table 2. Obstetrics and other related characteristics of pregnant mothers attending ANC service in East Shoa zone, Ethiopia, from June to August 2021.
Household food security
The majority of the participants, 374 (79.2%), were from food secured households. Seventy-two (15.3%) and 67(14.2%) of women were either unable to prefer food or ate a limited variety of food at least once in 4 weeks preceding the study period. A significant proportion of women, 61(12.9%), ate fewer meals per day, which happened at least once a month before the data collection period (Figure 1).
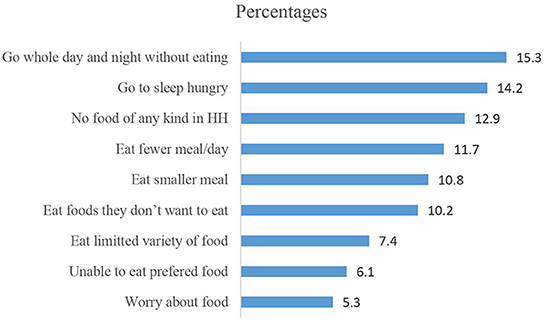
Figure 1. Distribution of household food insecurity based on the HIFAS scale among pregnant women attending ANC in East Shao zone, Ethiopia, from June to August 2021.
Knowledge of mothers on source of important nutrients
The knowledge assessment revealed that 150 (32.8%) women had poor knowledge about appropriate nutrition during pregnancy; 263 (55.7%), mentioned meat, poultry, and fish as a component of a balanced diet. The participants cited preventing pregnancy complications, 153(32.4), and brain and cognitive development, 179 (37.9%), as the significant advantages of a balanced diet. On the other hand, anemia 178 (37.7%) and LBW 117(24.8%) were the negative consequences mentioned by the respondents. Almost half of the study participants, 232(49.2%), know that they have to use iodized salt while 120 (25.4%) have no idea about the importance of iodized salt and 143 (30.3%) didn't know why iron folate pills are given (Table 3).
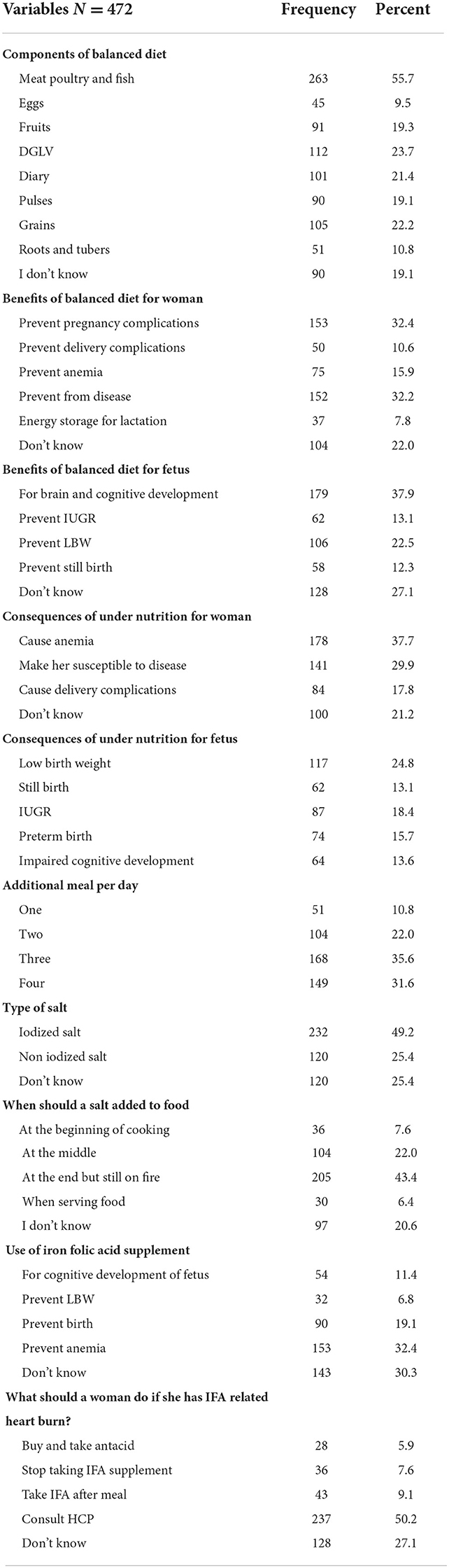
Table 3. Knowledge of pregnant mothers attending ANC service on optimal nutrition during pregnancy in East Shoa zone, Ethiopia, from June to August 2021.
Regarding iron, 152 (32.2%) did not know the food sources, and 56 (11.9%) reported meat, poultry, and fish as a source of iron. None of the participants were able to answer a single source of vitamin 147(31.1%) and protein 142 (30.1%). Dairy products were mentioned as sources of calcium by 168 (35.6%) women (Table 4).
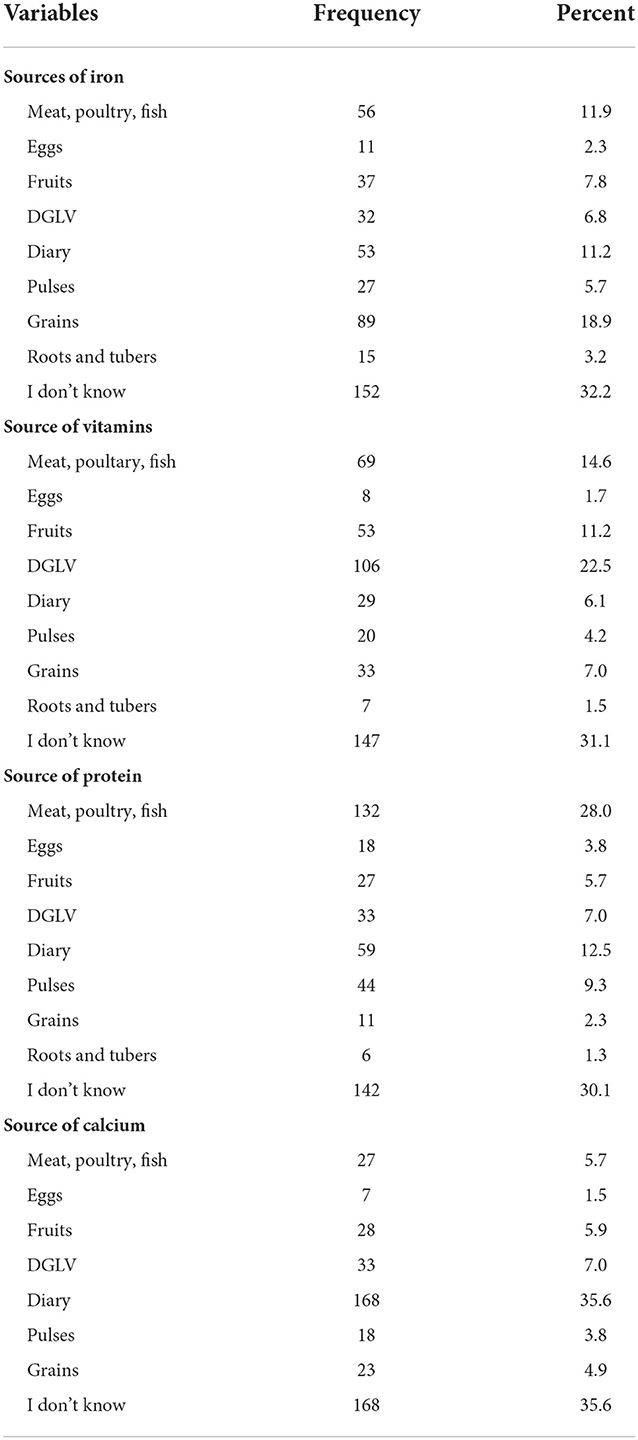
Table 4. Knowledge of mothers on source of important nutrients in East Shoa zone, from June to August 2021.
Nutritional status of pregnant women
In the current study, 405 (85.8%) of the women were well-nourished. Wealth, women's decision-making power, and nutritional counseling were independently associated with the nutritional status of pregnant women (Table 5). Poor women had 4.9 times higher odds of undernutrition compared with rich women (AOR: 4.9, 95% CI 1.3–18.2). Women with poor decision-making power had 3.3 higher odds of undernutrition than their counterparts (AOR: 3.3, 95% CI 1.2–7.8). Pregnant women who haven't received nutritional counseling during ANC follow-up had 3.5 higher odds of undernutrition than the women who received the counseling (AOR: 3.5, 95% CI 1.3–9.6) (Table 5).
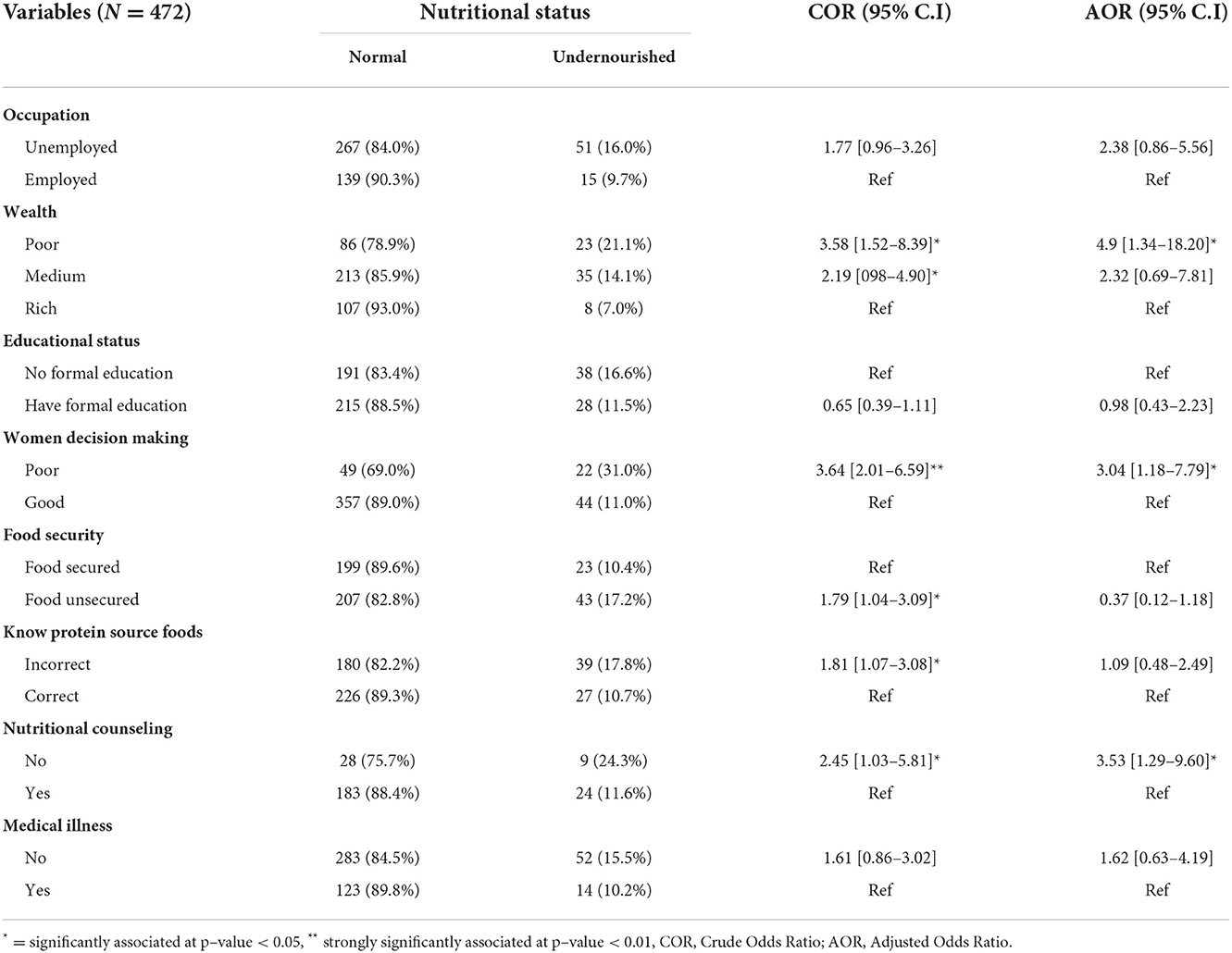
Table 5. Binary and multivariable logistic regression analysis showing the association of undernutrition among pregnant women attending ANC service in East Shoa zone, Ethiopia, from June to August 2021.
Discussion
This study assessed the nutritional status and associated factors among pregnant women attending ANC follow-up in East Shoa Zone, central Ethiopia. The study revealed that factors like wealth, women's decision-making power, and nutritional counseling were significantly associated with the nutritional status of pregnant women.
The effect of food insecurity appears significant during pregnancy. Because it compromises the quantity and quality of food intake, it causes adverse feto-maternal health outcomes and congenital disabilities (21). We found that 20.8% of women came from food-insecure households in the current study, consistent with the study done in northwest Ethiopia, where 20.6% came from food-insecure households (22). However, the result is lower than the report from a rural community in southern Ethiopia, where 38.6% of participants were from food-insecure households (23). The difference might be due to socioeconomic status, population density, and other geographical characteristics.
Pregnant women need to get a variety of food to meet the high need for energy and minerals due to increased maternal metabolic activity and the growing fetal tissue in her womb. In this study, around one in seven women ate a limited variety of foods at least once in the preceding month. This indicates a significant number of women were facing a challenge to get variety of foods during pregnancy in the study area. Which is similar to the report of previous studies in Ethiopia (22, 24).
Improving the women's knowledge is effective to modify the dietary practices of pregnant women (25). In Ethiopia, previous studies revealed that many pregnant women had poor knowledge of appropriate nutrition for pregnant women (24, 26, 27). Similarly, in our study, nearly one-third of the respondents had poor knowledge about appropriate nutrition during pregnancy. Among this, a significant proportion of participants could not cite a single protein, vitamins or iron food source. This finding pointed out the high need for establishing appropriate monitoring and feedback mechanisms on antenatal nutrition education and counseling for health care providers as this could improve the knowledge of women about appropriate nutrition.
Different interventions have been undertaken to curb the high prevalence of maternal undernutrition in the past years by the Ethiopian Federal Ministry of Health and other stakeholders (28, 29). However, high maternal undernutrition is still a challenge in many parts of the country (15, 23). We found that 14 percent of women were undernourished which is less than what was reported in the previous studies (24, 26, 30). The difference could be due to access to food, socioeconomic status, and awareness about nutrition during pregnancy. Effective implementation of strategies and evidence-based interventions such as; micronutrient supplementation, nutritional counseling, deworming prophylaxis, environmental and personal hygiene promotion could alleviate maternal undernutrition during pregnancy.
Access to variety of foods is possible when the women have enough money to purchase these foods and individuals' purchasing capacity determines the type of foods they consume (31–33). Higher odds of undernutrition observed among poor women in the present study are consistent with the previous study of young pregnant women from Ethiopia (34). In developing countries like Ethiopia, women have less access to jobs and unable to support their daily needs and the needs of their families. Hence, it logically follows that investment in women's economic empowerment would have a beneficial effect on the nutritional status of pregnant women.
Women's decision-making autonomy is the base for women's empowerment, and it ensures that women to have a good dietary diversity (19). Subsequently, having dietary diversity will help the women be in good nutritional status. In the present study, the odds of undernutrition was three times higher among women with poor decision-making power. This finding was supported by evidence from eastern Ethiopia, where the risk of malnutrition increased by more than double in pregnant women with low and medium levels of autonomy than in those who had a high level of autonomy (17). Programs working to improve the nutritional status of pregnant women should focus on increasing women's decision-making power.
Antenatal nutrition counseling and education (NEC) is one of the widely utilized strategies to improve women's nutritional status during pregnancy. NEC's goal is to improve maternal dietary quality by increasing the diversity and amount of foods consumed, and desired weight gain through the consumption of a sufficient and balanced diet. According to Girard &Olude, NEC improved gestational weight gain by 0.45 kg and reduced the risk of anemia by 30 percent (24). Lack of nutritional counseling was also significantly associated with low birthweight (35). In the present study, the odds of undernutrition are 3.5 times higher among women who haven't received nutritional counseling during pregnancy than those who received the counseling.
Though the evidence revealed that nutritional counseling during pregnancy improves the nutritional status of women and birth outcomes, the emphasis given to this intervention in developing countries is still low. For instance, majority of pregnant women who participated in the study done in Addis Ababa believe nutrition counseling provided to expectant mothers is not adequate and is neglected by most stake holders (36). Therefore, healthcare providers and hospital administrators should emphasize nutritional counseling and commit themselves to provide nutritional counseling to all women coming for ANC service.
This study included adequate sample size and assessed a range of determinants based on the constructed conceptual framework. The high response rate in this study minimizes the risk of non-response bias. The study only relied on MUAC to identify the nutritional status of women, and the limitations of this measurement could affect the findings of this study.
Conclusion
Findings indicated that a significant number of pregnant women in the study area were undernourished. It was also observed that higher wealth index, nutritional counseling, and women's decision-making power were inversely associated with undernutrition. Based on these findings, women's economic empowerment and increasing decision-making ability through direct and indirect interventions were recommended to decrease the magnitude of undernutrition. Additionally, routine and consistent nutritional counseling, establishing regular monitoring, and feedback mechanism are recommended to improve the nutritional status of women.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) of Jimma University, College of Health Sciences. The patients/participants provided their written informed consent to participate in this study.
Author contributions
EW, TB, and TG participated in the conception, study design, acquisition of data, analysis, interpretation, drafted, and critically reviewed the article. All authors have agreed on the journal to which the article will be submitted, reviewed, and agreed on all versions of the article before submission and during revision. All authors agree to take responsibility and be accountable for the contents of the article.
Funding
Institute of Health, Jimma University funded this research.
Acknowledgments
Authors would like to acknowledge Jimma University for funding this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Martorell R. Improved nutrition in the first 1000 days and adult human capital and health. Am J Hum Biol. (2017) 29:22952. doi: 10.1002/ajhb.22952
2. Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, et al. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet (London, England). (2013) 382:452–77. doi: 10.1016/S0140-6736(13)60996-4
3. Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet (London, England). (2013) 382:427–51. doi: 10.1016/S0140-6736(13)60937-X
4. Young MF, Ramakrishnan U. Maternal undernutrition before and during pregnancy and offspring health and development. Annal Nutr Metab. (2020) 76(Suppl. 3):41–53. doi: 10.1159/000510595
5. Black RE, Allen LH, Bhutta ZA, Caulfield LE, de Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet (London, England). (2008) 371:243–60. doi: 10.1016/S0140-6736(07)61690-0
6. Lartey A. Maternal and child nutrition in Sub-Saharan Africa: challenges and interventions. Proc Nutr Soc. (2008) 67:105–8. doi: 10.1017/S0029665108006083
7. Tang AM, Chung M, Dong K, Terrin N, Edmonds A, Assefa N, et al. Determining a global mid-upper arm circumference cutoff to assess malnutrition in pregnant women. Public Health Nutr. (2016) 23:3104–13. doi: 10.1017/S1368980020000397
8. Han Z, Mulla S, Beyene J, Liao G, McDonald SD. On behalf of the Knowledge synthesis G. Maternal underweight and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. Int J Epidemiol. (2011) 40:65–101. doi: 10.1093/ije/dyq195
9. Popa AD, Nită O, Graur LI, Popescu RM, Botnariu GE, Mihalache L, et al. Nutritional knowledge as a determinant of vitamin and mineral supplementation during pregnancy. BMC Public Health. (2013) 13:1–10. doi: 10.1186/1471-2458-13-1105
10. Tessema DG, Girma E, Mekonnen TC, Mebratu W. The extent of maternal nutritional knowledge and practice during lactation in kombolcha town, South Wollo Zone, Ethiopia: a mixed study design. Int J Womens Health. (2020) 12:79–87. doi: 10.2147/IJWH.S234398
11. Al-Shookri A, Al-Shukaily L, Hassan F, Al-Sheraji S, Al-Tobi S. Effect of mothers nutritional knowledge and attitudes on omani children's dietary intake. Oman Med J. (2011) 26:253–7. doi: 10.5001/omj.2011.61
12. Katenga-Kaunda LZ, Kamudoni PR, Holmboe-Ottesen G, Fjeld HE, Mdala I, Shi Z, et al. Enhancing nutrition knowledge and dietary diversity among rural pregnant women in Malawi: a randomized controlled trial. BMC Pregnancy Childbirth. (2021) 21:644. doi: 10.1186/s12884-021-04117-5
13. Muze M, Yesse M, Kedir S, Mustefa A. Prevalence and associated factors of undernutrition among pregnant women visiting ANC clinics in Silte zone, Southern Ethiopia. BMC Pregnancy Childbirth. (2020) 20:707. doi: 10.1186/s12884-020-03404-x
14. Ayele E, Gebreayezgi G, Mariye T, Bahrey D, Aregawi G, Kidanemariam G. Prevalence of undernutrition and associated factors among pregnant women in a public general hospital, tigray, Northern Ethiopia: a cross-sectional study design. J Nutr Metab. (2020) 2020:2736536. doi: 10.1155/2020/2736536
15. Gelebo DG, Gebremichael MA, Asale GA, Berbada DA. Prevalence of undernutrition and its associated factors among pregnant women in Konso district, southern Ethiopia: a community-based cross-sectional study. BMC Nutr. (2021) 7:32. doi: 10.1186/s40795-021-00437-z
16. Dadi AF, Desyibelew HD. Undernutrition and its associated factors among pregnant mothers in Gondar town, Northwest Ethiopia. PLoS ONE. (2019) 14:e0215305. doi: 10.1371/journal.pone.0215305
17. Kedir H, Berhane Y, Worku A. Magnitude and determinants of malnutrition among pregnant women in eastern Ethiopia: evidence from rural, community-based setting. Matern Child Nutr. (2016) 12:51–63. doi: 10.1111/mcn.12136
18. Gebreyesus SH, Lunde T, Mariam DH, Woldehanna T, Lindtjørn B. Is the adapted Household Food Insecurity Access Scale (HFIAS) developed internationally to measure food insecurity valid in urban and rural households of Ethiopia? BMC Nutr. (2015) 1:2. doi: 10.1186/2055-0928-1-2
19. Amugsi DA, Lartey A, Kimani-Murage E, Mberu BU. Women's participation in household decision-making and higher dietary diversity: findings from nationally representative data from Ghana. J Health, Population Nutr. (2016) 35:16. doi: 10.1186/s41043-016-0053-1
20. Blondin JH, LoGiudice JA. Pregnant women's knowledge and awareness of nutrition. Appl Nurs Res. (2018) 39:167–74. doi: 10.1016/j.apnr.2017.11.020
21. Iqbal S, Ali I. Maternal food insecurity in low-income countries: revisiting its causes and consequences for maternal and neonatal health. J Agri Food Res. (2021) 3:100091. doi: 10.1016/j.jafr.2020.100091
22. Demilew YM, Alene GD, Belachew T. Dietary practices and associated factors among pregnant women in West Gojjam Zone, Northwest Ethiopia. BMC Pregnancy Childbirth. (2020) 20:18. doi: 10.1186/s12884-019-2702-z
23. Zewdie S, Fage SG, Tura AK, Weldegebreal F. Undernutrition among pregnant women in rural communities in southern Ethiopia. Int J Womens Health. (2021) 13:73–9. doi: 10.2147/IJWH.S285132
24. Diddana TZ. Factors associated with dietary practice and nutritional status of pregnant women in Dessie town, northeastern Ethiopia: a community-based cross-sectional study. BMC Pregnancy Childbirth. (2019) 19:517. doi: 10.1186/s12884-019-2649-0
25. Girard AW, Olude O. Nutrition education and counselling provided during pregnancy: effects on maternal, neonatal and child health outcomes. Paediatr Perinat Epidemiol. (2012) 26:191–204. doi: 10.1111/j.1365-3016.2012.01278.x
26. Tsegaye D, Tamiru D, Belachew T. Factors associated with dietary practice and nutritional status of pregnant women in rural communities of Illu Aba Bor Zone, Southwest Ethiopia. Nutr Diet Suppl. (2020) 12:103–12. doi: 10.2147/NDS.S257610
27. Zerfu TA, Biadgilign S. Pregnant mothers have limited knowledge and poor dietary diversity practices, but favorable attitude towards nutritional recommendations in rural Ethiopia: evidence from community-based study. BMC Nutr. (2018) 4:43. doi: 10.1186/s40795-018-0251-x
28. FDRE-Ethiopia. National Nutrition Programme June 2013-June 2015. (2013). Available online at: http://www.usaid.gov/sites/default/files/documents/1867/National Nutrition Programme.pdf. (accessed June 28, 2022).
29. FMOH-Ethiopia. National Nutriton Strategy. Addis Ababa, Ethiopia: Ministry of Health (MoH), Federal Democratic Republic of Ethiopia. Addis Ababa, Ethiopia. (2008).
30. Lama N, Lamichhane R. C S, Bhandari G, Wagle R. Determinants of nutritional status of pregnant women attending antenatal care in Western Regional Hospital, Nepal. Int J Commun Med Public Health. (2018) 5:5045. doi: 10.18203/2394-6040.ijcmph20184776
31. Masters WA, Eggersdorfer M, Cordaro J, Fanzo J, Gibney M, Kennedy E, et al. The economic causes of malnutrition. Good Nutr. (2016):92–104. doi: 10.1159/000452378
32. French SA, Tangney CC, Crane MM, Wang Y, Appelhans BM. Nutrition quality of food purchases varies by household income: the SHoPPER study. BMC Public Health. (2019) 19:231. doi: 10.1186/s12889-019-6546-2
33. Ver Ploeg M, Breneman V, Farrigan T, Hamrick K, Hopkins D, Kaufman P, et al. Access to Affordable and Nutritious Food: Updated Estimates of Distance to Supermarkets Using 2010 Data. (2012).
34. Workicho A, Belachew T, Ghosh S, Kershaw M, Lachat C, Kolsteren P. Burden and determinants of undernutrition among young pregnant women in Ethiopia. Matern Child Nutr. (2019) 15:e12751. doi: 10.1111/mcn.12751
35. Deriba BS, Jemal K. Determinants of low birth weight among women who gave birth at public health facilities in North Shoa Zone: unmatched case-control study. Inquiry. (2021) 58:00469580211047199. doi: 10.1177/00469580211047199
Keywords: nutrition, determinants, pregnant women, undernutrition, Ethiopia
Citation: Wakwoya EB, Belachew T and Girma T (2022) Determinants of nutritional status among pregnant women in East Shoa zone, Central Ethiopia. Front. Nutr. 9:958591. doi: 10.3389/fnut.2022.958591
Received: 31 May 2022; Accepted: 28 November 2022;
Published: 15 December 2022.
Edited by:
Romanus Osabohien, Covenant University, NigeriaReviewed by:
Mahdi Shadnoush, Shahid Beheshti University of Medical Sciences, IranS. M. Tafsir Hasan, International Centre for Diarrhoeal Disease Research (ICDDR), Bangladesh
Copyright © 2022 Wakwoya, Belachew and Girma. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ermias Bekele Wakwoya, ZXJtaTM1NzdAZ21haWwuY29t
 Ermias Bekele Wakwoya
Ermias Bekele Wakwoya Tefera Belachew1,2
Tefera Belachew1,2