
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Nutr., 09 September 2022
Sec. Nutritional Epidemiology
Volume 9 - 2022 | https://doi.org/10.3389/fnut.2022.952665
This article is part of the Research TopicDiet and Nutrition for Non-communicable Diseases in Low and Middle-Income CountriesView all 30 articles
Introduction: Obesity and its association with socioeconomic factors are well-established. However, the gradient of this relationship among rural populations in low- and middle-income countries such as Nepal is not fully understood. We sought to assess the association of socioeconomic factors (education, income, and employment status) with overweight/obesity.
Methods: This cross-sectional study analyzed data from 260 participants aged ≥18 years and attending a rural health center in Dolakha, Nepal. Self-reported data on demographic, socioeconomic, and lifestyle factors was collected, and weight and height were measured for all the study participants. Those with a body mass index of <25 kg/m2 were regarded as non-overweight/obese and those with ≥25 kg/m2 were regarded as overweight/obese. Poisson regression models were used to estimate prevalence ratios and corresponding 95% confidence intervals to assess the association between socioeconomic factors and overweight/obesity. In addition, we assessed the effect of modification by age and gender to study the effect of socioeconomic factors on overweight/obesity.
Results: The age-standardized prevalence of overweight/obesity was higher for individuals with higher education (23%) and high-income (32%) and those who were unemployed (42%). Compared to the low-income and no formal education groups, the prevalence ratio of overweight/ obesity was 1.69 and 2.27 times more for those belonging to the high-income and high school and above groups, respectively. No evidence of effect modification by gender and age was observed.
Conclusions: Socioeconomic factors, education, and income were positively associated with overweight/obesity prevalence in rural Nepal. Further large studies using longitudinal settings are necessary to replicate our findings.
Obesity, a common risk factor for major non-communicable diseases (NCDs) has tripled in the last 4 decades (1–3). In 2016, more than 1.9 billion adults were overweight worldwide (4), and the number is still increasing. In Nepal, the prevalence of overweight and obesity (OWOB) also increased from 21% in 2013 to 29% in 2019 (5, 6). Therefore, understanding the burden of OWOB is important to develop effective strategies to halt obesity-associated several adverse health outcomes.
In low-income countries like Nepal, socioeconomic development drives food choices and diet pattern (7), and as a country progresses, obesity burden shifts from high to low income groups (8–10). Gradual economic prosperity has triggered nutrition transition shifting dietary patterns from home-produced food to easily available processed food contributing to the burden of OBOW and NCDs in Nepal (11).
Understanding the role of socioeconomic status (SES) in explaining food behavior that determines an individual's body weight is important (7). Individuals with low SES status is associated with increased risk of obesity in high-income nations (12, 13) while in LMICs (14, 15) results are mixed. For instance, findings from cross-sectional studies suggested that educated and affluent Nepalese (16), South Asian women (17), and Indians (18) were more likely to be overweight or obese. Likewise, being employed was positively associated with OWOB in Nepal (19), Mexico (20), and South India (21). On the other hand, obesity was reported to be inversely associated with education level and income in Argentina (22) and Iran (23). Furthermore, a national survey conducted in Nepal suggested that the prevalence of OWOB was more among affluent individuals living in urban hills (5), while a survey conducted among 341 Nepalese bureaucrats reported 33.4% of the participants to be either overweight or obese (24). The possible reason of higher OWOB prevalence in urban Nepal could be high consumption of energy-dense and cheap fatty foods as well as being physically less active (25, 26), whereas the lower prevalence of obesity seen among rural individuals might be due to engagement in physically demanding jobs (27).
Nepal has experienced considerable economic growth in recent years, and in 2015, the average income was $2,500 GDP per capita (gross domestic product per capita) (28). The impact of economic growth on obesity in different SES groups remains unclear. Compared to the rural women of Sherpa ethnicity, urban women had higher body mass index (BMI) (29), and this difference is the result of increase in income and less energy expenditure in the urban population (26). Therefore, a study to assess the association between SES and OWOB in rural Nepal, where 80% of the Nepalese population reside, is necessary. We recently published an article reporting a positive association between SES and hypertension (30). In this study, we used data from the same study (30) on individuals visiting a primary health center in rural Nepal to assess the association between SES and two other highly prevalent comorbid conditions, i.e., overweight and obesity.
The detail of the study design and the methodology used for this study are published elsewhere (30).
The study was conducted in Kirnetar health center in Dolakha district in Nepal, providing primary health services to eight rural villages in its proximity. It was an opportunistic screening. The health center, established in 2012, provides primary-level health services 6 days a week including 24-h emergency services.
A cross-sectional study was conducted among 260 individuals who visited the health center for clinical examination or to purchase medicine from October to December 2016. Participants over 18 years were included in the study, but those who were pregnant were excluded.
All the recruited participants were interviewed by trained enumerators. Self-reported data on demographic and socioeconomic factors, clinical history, lifestyle, and dietary factors were collected using a validated STEPS questionnaire (5). The participants were asked to stand (without footwear, jackets, and sweaters) on an instrument placed on a flat floor to measure weight (in kg) using BOSCH Electronic Scale PPWA4201. Similarly, the participants were asked to stand tall with heels and head against the measuring tape placed on the wall (without footwear, cap and hat) and the lineal measurement on the top point of the head was measured to the nearest 0.05 cm (5).
BMI was computed by dividing the weight (in kg) by the squared value of height (in m) and categorized as underweight or normal weight (<25 kg/m2), overweight (25–29.9 kg/m2), or obese (≥30 kg/m2) according to WHO recommendation. For analyses, we collapsed BMI categories into two groups, i.e., non-obese (BMI <25 kg/m2) and overweight and obese (BMI ≥25 kg/m2).
Per capita annual income was calculated by asking the total combined household income (in Nepalese rupee) in the year preceding the survey and dividing it by the total number of household members. Annual income was categorized into tertiles (low: 0–6,000, middle: 6,250–32,571, and high: 33,333–625,000 Nepalese Rupees).
Participants who reported that they did not attend school were confined to the “no formal education” group; those who had at least 1 year of formal school including those who did not complete high school were confined to the “less than high school” group, and those who had completed high school or beyond were confined to the “high school and above” group.
Employment status: this variable was classified into three groups: farming (agricultural task), employed (government/non-government employees, self-employed people), or unemployed (retired, students, unpaid, unable to work, unemployed, homemakers).
Sociodemographic variables include age (in years), gender (males, females), marital status (yes, no), and ethnicity (Dalit, Brahmin, Chettri, others). Lifestyle-related variables include both smoke or smokeless tobacco use (never-users, current, former users); alcohol intake (drinking <1 glass per week, 1–3 glasses/week, >3 standard drinks/week were categorized as “low drinkers,” “moderate drinkers,” or “heavy drinkers,” respectively). Physical activity was assessed using Global Physical Activity Questionnaire (31) (≥ 600 metabolic equivalent minutes (MET) and < 600 MET were categorized as adequate and inadequate, respectively), as well as fruits and vegetables servings (<2, 2–4, and >4 servings per day).
The descriptive data were presented as frequencies and percentages for categorical variables and mean and SD for continuous variables. To assess the association between socioeconomic positions and prevalence of OWOB, we used modified Poisson regression models with robust standard errors (32) to estimate prevalence ratio (PR) with corresponding 95% CI. We fitted the Poisson regression models to estimate PR because odds ratio provides an overestimated approximation of the risk when the prevalence of outcome of interest is common (≥10%) (33). Two models were constructed. Model 1 was unadjusted, and model 2 was adjusted for age (in years), gender (male, female), marital status (married, unmarried), and ethnicity (Brahmin, Chettri, Dalits, Other). The analyses of the association between SES and OWOB was stratified by gender (male vs. female) and age (<50 vs. ≥50 years). The statistical interaction was assessed by likelihood ratio test incorporating product terms of (1) categories of SES × age and (2) categories of SES × gender in the model. All the statistical analyses were performed using Stata/IC 14 (Stata Corp, College Station, TX, United States).
The sociodemographic and lifestyle characteristics of the 260 participants are presented in Table 1. The mean age of the study population was 45 years, 48.5% were women and 24.5% were OWOB. The prevalence of OWOB were higher among males, Dalit ethnicity, married, high level of education, high income and employed. Furthermore, the prevalence of OWOB were higher among those who consumed <2 servings of fruits and vegetables per day and those who were non-tobacco users, moderate drinkers, and less physically active.
The distribution of sociodemographic and lifestyle factors in relation to education and income are presented in Table 2. Sex and age group were significantly different across different levels of education and income categories. Alcohol consumption and tobacco use were significantly different across education categories.
In Table 3, the age-standardized prevalence of OWOB was higher among the high-income group, those who attained high school or had higher education, and the unemployed group. In the adjusted model, we observed that the prevalence of OWOB was 1.69 and 2.27 times greater in the high-income group and those with education of high school and above, respectively, compared to individuals in the low-income group and those with no formal education. Although the prevalence ratio was >1, there was uncertainty of the point estimates due to wide confidence interval. Furthermore, compared to the unemployed individuals, the farmers had significantly lower prevalence of OWOB (PR 0.5 and 95% CI 0.28–0.9). Furthermore, we found no evidence of effect modification on the outcome by age and sex. The p-value for interaction was not significant (results not shown).
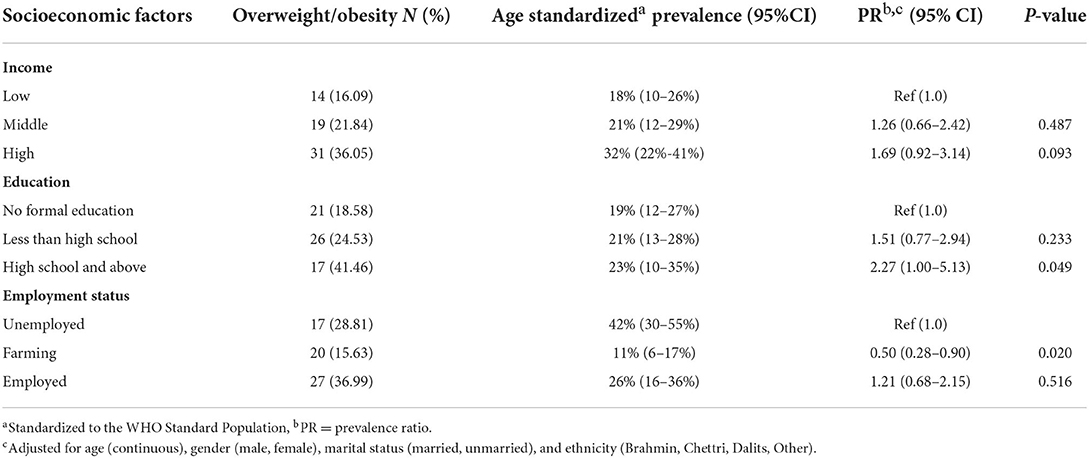
Table 3. Multivariable modified Poisson regression analyses between socioeconomic positions and OWOB.
In this cross-sectional study, we assessed the effect of SES on OWOB among participants from rural Nepal. We found that OWOB was predominant among men, young adults, those married, moderate alcohol drinkers, non-tobacco users, and those less physically active. We observed a positive association between SES (education, income, employment status) and prevalence of OWOB, while the group of farmers had significantly lower prevalence of being overweight or obese compared to the unemployed group. Furthermore, we found no evidence of effect modification by sex and age.
In line with our findings, nationally representative surveys from Nepal (6, 34) and studies from other low-income countries (35–38) reported a positive SES and OWOB association. The prevalence of OWOB was reported to be higher among affluent and educated individuals in Nepal (6), Bangladesh (39) and South Asia (40).
On the contrary, studies from developed countries reported an inverse association between SES (education level and income level) and obesity (8, 15, 41). Nevertheless, a meta-analysis of prospective cohort studies from high-income countries suggested that the inverse association observed between SES and obesity was inconclusive after correcting for publication bias and reverse causality (that obese people were less likely to earn) (42). A systematic review from a developing country reported mixed results by gender, i.e., positive association for men and inverse for women (43).
The positive association observed between SES and obesity might be explained by the high-SES group having access to surplus food (44), and change in dietary pattern to consumption of high-fat and sugar-containing foods (8, 14, 45–47). Occupation is related to physical activity, and many jobs in Nepal are still labor-intensive (27); however, those with high SES in rural Nepal seem more likely to be OWOB, as they are often engaged in sedentary jobs (48). The high prevalence of obesity can also be explained by preference for large body sizes in some countries (8, 49–51), including Nepal (24) where large body size is considered a sign of economic prosperity, thus high SES may gain weight to maintain a status quo. On the other hand, the lower prevalence of obesity among those with low SES might be explained by poor availability of nutritious food (44) and engagement in high energy-expending jobs (48, 52).
Furthermore, the inconsistent results observed between the studies might also be due to different categorizations of variables such as obesity, income and education, heterogeneity of the study population, variables included in the model, and, more importantly, the different economic development stages of the countries (43). As a country's economy progresses, SES and obesity associations might also tend to be reversed (15). Moreover, studies from high- and middle-income countries achieving economic prosperity have shown the reversal of obesity gradient with increase in income occurring more swiftly (43). The difference in obesity and SES association in high- and low-income countries is determined by lifestyle choices; high-SES individuals in LMICs consume high-calorie foods and avoid physically demanding tasks while high-SES individuals in high-income countries tend to eat a healthy diet and regularly exercise (53). Nepal has achieved a moderate reduction in poverty with a steady increase in gross domestic product (35). Evidence suggests obesity is rising in low-resource settings including Nepal, with a higher increase reported among the rural population (18, 54). Therefore, Nepal needs to understand that obesity is no longer confined to affluent populations in urban areas.
The government of Nepal monitors obesity trends through routine surveys and tackles it through broader NCD policies and programming (55). However, unclear implementation mechanisms and being under resourcing of these policies hamper effective implementation (56). Furthermore, the association of obesity with adverse events such as stroke, cardiovascular events, and diabetes (57, 58) makes it urgent to address modifiable risk factors by launching an obesity prevention and management program in rural Nepal where primary healthcare facilities are not well-equipped and are in a tattered state.
Our study has a few strengths. First, a validated questionnaire was used for the data collection. Second, we measured weight and height instead of relying on self-reported measures for computing BMI.
Our study also has some limitations. First, our analysis was based on a relatively small sample size with reasonable statistical power limiting our ability to perform further sub-group analyses. Second, due to the cross-sectional nature of the study design, we cannot rule out the possibility of reverse causality. Third, the self-reported questionnaire on physical activity, alcohol use, and income data might have introduced recall bias (59). Lastly, we cannot rule out the possibility of residual confounding because of some unmeasured and incorrectly specified adjusted confounders.
Overall, the findings from this study suggest that high-SES individuals had higher prevalence of OWOB. However, the results were based on participants who visited one health center in rural Nepal, limiting its generalizability even within regional Nepal.
We recommend studies to understand how the SES and obesity relationship changes with socioeconomic development in Nepal. Similarly, larger studies are required to replicate our findings, preferably a large prospective cohort study from rural Nepal to demonstrate the SES and OWOB association among different population groups, and needed for timely identification of high-risk groups that will allow for efficient use of scarce health resources to develop effective and personalized interventions to prevent obesity in rural Nepal.
• The show cards shown to the respondents during data collection were same as the one used in the Non-Communicable Diseases Risk Factors: STEPS Survey Nepal 2013
° to identify the type of tobacco the respondents used
° to determine the amount of alcohol the respondents consumed
° to identify the type of fruits the respondents ate
° to identify the type of physical activity the respondents were engaged in.
The raw data supporting the conclusions of this article will be made available by the authors upon receiving request and approval to share from the ethics committee.
Ethical approval from the Regional Ethical Committee in Central Norway and Institutional Review Committee of Kathmandu University School of Medical Sciences Nepal was obtained. Informed consent was obtained before the start of data collection. The enumerators were trained in ethical consideration of human subject research to minimize breach in confidentiality. The data were de-identified for analysis. The identifiers were stored for 5 years in a locked cabinet.
SB performed the analysis and drafted the manuscript. RN conceived the study, collected the data, and contributed to the draft. ASh and BK provided input during study design and on the drafting manuscript. ASe provided suggestions on data analysis and presentation, edited the draft of the manuscript, and approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
The authors would like to thank Dhulikhel Hospital, Dhulikhel, and the Kirnetar Health Center, Dolakha Nepal for facilitating the data collection and Norwegian University of Science and Technology, Trondheim, Norway for providing fund to RN.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2022.952665/full#supplementary-material
1. Peters R, Ee N, Peters J, Beckett N, Booth A, Rockwood K, Anstey KJ. Common risk factors for major noncommunicable disease, a systematic overview of reviews and commentary: the implied potential for targeted risk reduction. Ther Adv Chronic Dis. (2019) doi: 10.1177/2040622319880392
2. Sharma SR, Mishra SR, Wagle K, Page R, Matheson A, Lambrick D, et al. Social determinants of common metabolic risk factors (high blood pressure, high blood sugar, high body mass index and high waist-hip ratio) of major non-communicable diseases in South Asia region: a systematic review protocol. Syst Rev. (2017) 6:183. doi: 10.1186/s13643-017-0576-6
3. Fitzmaurice C, Abate DM, Abbasi N, Abbastabar H, Abd-Allah F, Abdel-Rahman, et al. Global burden of disease cancer collaboration global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: a systematic analysis for the global burden of disease study. JAMA Oncol. (2019) 5:1749–68. doi: 10.1001/jamaoncol.2019.2996
4. Available online at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight downloaded (accessed March 31, 2021).
5. Aryal KK, Mehata S, Neupane S, Vaidya A, Dhimal M, Dhakal P, et al. The Burden and determinants of non-communicable diseases risk factors in Nepal: findings from a nationwide steps survey. PLoS ONE. (2015) 10:e0134834. doi: 10.1371/journal.pone.0134834
6. Dhimal M, Bhattarai S, Dixit L, Hyder M, Agrawal N, Rani M, et al. Report of non-communicable disease risk factors: steps survey Nepal 2019. Kathmandu: Nepal Health Research Council. (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/ncds/ncd-steps-survey-2019-compressed.pdf
7. Delavari M, Sønderlund AL, Swinburn B, Mellor D, Renzaho A. Acculturation and obesity among migrant populations in high income countries–a systematic review. BMC Public Health. (2013) 13:458. doi: 10.1186/1471-2458-13-458
8. Dinsa GD, Goryakin Y, Fumagalli E, Suhrcke M. Obesity and socioeconomic status in developing countries: a systematic review. Obes Rev. (2012) 13:1067–79. doi: 10.1111/j.1467-789X.2012.01017.x
9. Yadav S, Arokiasamy P. Understanding epidemiological transition in India. Glob Health Action. (2014) 7:23248. doi: 10.3402/gha.v7.23248
10. Dutta A, Kavitha AK, Samal S, Panigrahi P, Swain S, Nanda L, et al. Independent urban effect on hypertension of older Indians: identification of a knowledge gap from a study on global ageing and health. J Am Soc Hypertens. (2018) 12:e9–17. doi: 10.1016/j.jash.2018.09.004
11. Subedi YP, Marais D, Newlands D. Where is Nepal in the nutrition transition? Asia Pac J Clin Nutr. (2017) 26:358–67. doi: 10.6133/apjcn.112015.10
12. Wang Y, Beydoun MA. The obesity epidemic in the United States–gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis Epidemiol Rev. (2007) 29:6–28. doi: 10.1093/epirev/mxm007
13. Lamerz A, Kuepper-Nybelen J, Wehle C, Brunin N, Trost-Brinkhues G, Brenner H, et al. Social class, parental education, and obesity prevalence in a study of 6-year-old children in Germany. Int J Obes. (2005) 29:373–80. doi: 10.1038/sj.ijo.0802914
14. Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: a review. Bull World Health Organ. (2004) 82:940–6.
15. McLaren L. Socioeconomic status and obesity. Epidemiol Rev. (2007) 29:29–48. doi: 10.1093/epirev/mxm001
16. Rawal LB, Kanda K, Mahumud RA, Joshi D, Mehata S, Shrestha N, et al. Prevalence of underweight, overweight and obesity and their associated risk factors in Nepalese adults: data from a nationwide survey, 2016. PLoS ONE. (2018) 13:e0205912. doi: 10.1371/journal.pone.0205912
17. Biswas T, Townsend N, Magalhaes R, Hasan MM, Al Mamun A. Geographical and socioeconomic inequalities in the double burden of malnutrition among women in Southeast Asia: a population-based study. Lancet Reg Health - Southeast Asia. (2022) 1:100007. doi: 10.1016/j.lansea.2022.04.003
18. Luhar S, Mallinson PA, Clarke L, Kinra S. Trends in the socioeconomic patterning of overweight/obesity in India: a repeated cross-sectional study using nationally representative data. BMJ Open. (2018) 8:e023935. doi: 10.1136/bmjopen-2018-023935
19. Balarajan Y, Villamor E. Nationally representative surveys show recent increases in the prevalence of overweight and obesity among women of reproductive age in Bangladesh, Nepal, and India. J Nutr. (2009) 139:2139–44. doi: 10.3945/jn.109.112029
20. Fernald LCH. Socio- economic status and body mass index in low- income Mexican adults. Soc Sci Med. (2007) 64:2030–42. doi: 10.1016/j.socscimed.2007.02.002
21. Samuel P, Antonisamy B, Raghupathy P, Richard J, Fall CH. Socio-economic status and cardiovascular risk factors in rural and urban areas of Vellore, Tamilnadu, South India. Int J Epidemiol. (2012) 41:1315–27. doi: 10.1093/ije/dys001
22. Jiwani SS, Carrillo-Larco RM, Hernández-Vásquez A, Barrientos-Gutiérrez T, Basto-Abreu A, Gutierrez L, et al. The shift of obesity burden by socioeconomic status between 1998 and 2017 in Latin America and the Caribbean: a cross-sectional series study. Lancet Glob Health. (2019) 7:e1644–54. doi: 10.1016/S2214-109X(19)30421-8
23. Dastgiri S, Mahdavi R, TuTunchi H, Faramarzi E. Prevalence of obesity, food choices and socio-economic status: a cross-sectional study in the north-west of Iran. Public Health Nutr. (2006) 9:996–1000. doi: 10.1017/PHN2006982
24. Simkhada P, Poobalan A, Simkhada PP, Amalraj R, Aucott L. Knowledge, attitude, and prevalence of overweight and obesity among civil servants in Nepal Asia. Pac J Public Health. (2011) 23:507–17. doi: 10.1177/1010539509348662
25. Mishra SR, Kallestrup P, Neupane D. Country in Focus: confronting the challenge of NCDs in Nepal. Lancet Diab Endocrinol. (2016) 4:979–80. doi: 10.1016/S2213-8587(16)30331-X
26. Vaidya A, Shakya S, Krettek A. Obesity prevalence in Nepal: public health challenges in a low-income nation during an alarming worldwide trend. Int J Environ Res Public Health. (2010) 7:2726–44. doi: 10.3390/ijerph7062726
27. Pedisic Z, Shrestha N, Loprinzi PD, Mehata S, Mishra SR. Prevalence, patterns, and correlates of physical activity in Nepal: findings from a nationally representative study using the global physical activity questionnaire (GPAQ). BMC Public Health. (2019) 19:864. doi: 10.1186/s12889-019-7215-1
28. Website. Nepal GDP - per capita (PPP): Index Mundi 2016. Available online at: http://www.indexmundi.com/nepal/gdp_per_capita_(ppp).html (accessed May 26, 2017).
29. Smith C. Prevalence of obesity and contributing factors among Sherpa women in urban and rural Nepal. Am J Human Biol.. (1998) 10:519–28. doi: 10.1002/(SICI)1520-6300(1998)10:4<519::AID-AJHB12>3.0.CO;2-B
30. Bhattarai S, Tandstad B, Shrestha A, Karmacharya B, Sen A. Socioeconomic status and its relation to hypertension in rural Nepal. Int. J. Hypertens. (2021) 3:5542438. doi: 10.1155/2021/5542438
31. Organization WH Others. Global Physical Activity Questionnaire (GPAQ) Analysis Guide (2012). Available online at: http://www.who.int/chp/steps
32. Martinez BA, Leotti VA, eSilva GS, Nunes LN, Machado G, Corbellini LG. Odds ratio or prevalence ratio? an overview of reported statistical methods and appropriateness of interpretations in cross-sectional studies with dichotomous outcomes in veterinary medicine. Front Vete Sci. (2017) 4:193. doi: 10.3389/fvets.2017.00193
33. Spiegelman D. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. (2005) 162:199–200. doi: 10.1093/aje/kwi188
34. Shrestha N, Mishra SR, Ghimire S, Gyawali B, Pradhan PM, Schwarz D. Application of single-level and multi-level modeling approach to examine geographic and socioeconomic variation in underweight, overweight and obesity in Nepal: findings from NDHS 2016. Scient Rep. (2020) 10:318. doi: 10.1038/s41598-019-56318-w
35. Bishwajit G. Household wealth status and overweight and obesity among adult women in Bangladesh and Nepal. Obes Sci Pract. (2017) 3:185–92. doi: 10.1002/osp4.103
36. Gebremedhin S. Prevalence and differentials of overweight and obesity in preschool children in Sub-Saharan Africa. BMJ Open. (2015) 5:e009005. doi: 10.1136/bmjopen-2015-009005
37. Kandala NB, Stranges S. Geographic variation of overweight and obesity among women in Nigeria: a case for nutritional transition in sub-Saharan Africa. PLoS ONE. (2014) 9:e101103. doi: 10.1371/journal.pone.0101103
38. Janjua NZ, Iqbal R, Mahmood B. Association of socioeconomic position with under- and overnutrition in Pakistan. Ann Epidemiol. (2011) 21:884–91. doi: 10.1016/j.annepidem.2011.08.006
39. Biswas T, Garnett SP, Pervin S, Rawal LB. The prevalence of underweight, overweight and obesity in Bangladeshi adults: data from a national survey. PLoS ONE. (2017) 12:e0177395. doi: 10.1371/journal.pone.0177395
40. Jayawardena R, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence, trends, and associated socio-economic factors of obesity in South Asia Obesity Facts. (2013) 6:405–14. doi: 10.1159/000355598
41. Stunkard AJ. Socioeconomic Status and Obesity. Ciba Foundation Sympos 201 - Orig Conseq Obes. (2007) 3:174–93. doi: 10.1002/9780470514962.ch11
42. Kim TJ, von dem Knesebeck O. Income and obesity: what is the direction of the relationship? A systematic review and meta-analysis. BMJ Open. (2018) 8:e019862. doi: 10.1136/bmjopen-2017-019862
43. Monteiro CA, Conde WL, Lu B, Popkin BM. Obesity and inequities in health in the developing world. Int J Obes. 28:1181–1186 (2004). doi: 10.1038/sj.ijo.0802716
44. Block J, Scribner R, Desalvo K. Fast food, race/ethnicity, and incomeA geographic analysis. Am J Prevent Medicine. (2004) 27:2117. doi: 10.1016/S0749-3797(04)00139-4
45. Samal S, Panigrahi P, Dutta A. Social epidemiology of excess weight and central adiposity in older Indians: analysis of study on global AGEing and adult health (SAGE). BMJ Open. (2015) 5 e008608. doi: 10.1136/bmjopen-2015-008608
46. Gouda J, Prusty RK. Overweight and obesity among women by economic stratum in urban India. J Health Popul Nutr. (2014) 32:79–88.
47. Khandelwal S, Reddy KS. Eliciting a policy response for the rising epidemic of overweight-obesity in India. Obes Rev. (2013) 14(Suppl 2) 114–125. doi: 10.1111/obr.12097
48. Haenel H. Diet, Nutrition, and The Prevention of Chronic Diseases (Technical Report Series 797). 203 Seiten, zahlr. Abb. und Tab. Geneva: World Health Organization (1990).
49. Rguibi M, Belahsen R. Body size preferences and sociocultural influences on attitudes towards obesity among Moroccan Sahraoui women. Body Image. (2006) 3:395–400. doi: 10.1016/j.bodyim.2006.07.007
50. Fernald LCH. Perception of body weight: a critical factor in understanding obesity in middle-income countries. J Women's Health. (2009) 18:1121–2. doi: 10.1089/jwh.2009.1625
51. Gulati S, Misra A, Colles SL, Kondal D, Gupta N, Goel K, et al. Dietary intakes and familial correlates of overweight/obesity: a four-cities study in India. Ann Nutr Metab. (2013) 62:279–29. doi: 10.1159/000346554
52. Schwinger C, Chandyo RK, Ulak M, Hysing M, Shrestha M, Ranjitkar S, et al. Prevalence of underweight, overweight, and obesity in adults in Bhaktapur, Nepal in 2015–2017. Front Nutri. (2020) 7:7164. doi: 10.3389/fnut.2020.567164
53. Pampel FC, Denney JT, Krueger PM. Obesity, SES, and economic development: a test of the reversal hypothesis. Soc Sci Med. (2012) 74:1073–81. doi: 10.1016/j.socscimed.2011.12.028
54. Mishra SR, Neupane D, Bhandari PM, Khanal V, Kallestrup P. Burgeoning burden of non-communicable diseases in Nepal: a scoping review. Global Health. (2015) 11:32. doi: 10.1186/s12992-015-0119-7
55. Organization WH Others. Global Action Plan for the Prevention and Control of Non-communicable Diseases 2013–2020. Geneva: World Health Organization (2013). Available online at: https://www.who.int/publications/i/item/9789241506236
56. Available online at: https://crehpa.org.np/wp-content/uploads/2020/01/Nepal-Whats-in-your-NCD-Policy.pdf
57. Kivimäki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. (2017) 2:e277–85. doi: 10.1016/S2468-2667(17)30074-9
58. Babu GR, Murthy GVS, Ana Y, Patel P, Deepa R, Neelon SEB, et al. Association of obesity with hypertension and type 2 diabetes mellitus in India: a meta-analysis of observational studies. World J Diab. (2018) 9:40–52. doi: 10.4239/wjd.v9.i1.40
Keywords: obesity, epidemiology - descriptive, rural, Nepal, socioeconomic
Citation: Bhattarai S, Nerhus Larsen R, Shrestha A, Karmacharya B and Sen A (2022) Association between socioeconomic positions and overweight/obesity in rural Nepal. Front. Nutr. 9:952665. doi: 10.3389/fnut.2022.952665
Received: 25 May 2022; Accepted: 29 July 2022;
Published: 09 September 2022.
Edited by:
Farhana Akter, Chittagong Medical College, BangladeshReviewed by:
Kona Chowdhury, Gonoshathaya Samaj Vittik Medical College, BangladeshCopyright © 2022 Bhattarai, Nerhus Larsen, Shrestha, Karmacharya and Sen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sanju Bhattarai, c2FuanUuYmhhdHRhcmFpQG50bnUubm8=; c2FuanV3YWdsZUBnbWFpbC5jb20=; Abhijit Sen, YWJoaWppdC5zZW5AbnRudS5ubw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.